Abstract
Increased consumption of unhealthy processed foods, particularly those high in sodium, is a major risk factor for cardiovascular diseases. The nutrition information on packaged foods can help guide consumers toward products with less sodium and support government actions to improve the healthiness of the food supply. The aims of this study were to estimate the proportion of packaged foods displaying nutrition information for sodium and other nutrients specified by Nigerian nutrition labelling regulations and to determine the amount of sodium in packaged foods sold in Nigeria using data from the nutritional information panel. Data were collected from November 2020 to March 2021 from in-store surveys conducted in supermarkets in three states. A total of 7039 products were collected. Overall, 91.5% (n = 6439) provided only partial nutrition information, 7.0% (n = 495) provided no nutritional information, and only 1.5% (n = 105) displayed a nutrient declaration that included all nutrients specified by 2019 Nigerian regulations. Some form of sodium content information was displayed for 86% of all products (n = 6032), of which around 45% (n = 2689) expressed this as ‘salt’ and 59% (n = 3559) expressed this as ‘sodium’, while a small number of food products had both ‘salt’ and ‘sodium’ content (3.6%). Provision of sodium or salt information on the label varied between food categories, ranging from 50% (vitamins and supplements, n = 2/4) to 96% (convenience foods, n = 44/46). Food categories with the highest median sodium content were ‘meat and meat alternatives’ (904 mg/100 g), ‘sauces, dressings, spreads, and dips’ (560 mg/100 g), and ‘snack foods’ (536 mg/100 g), although wide variation was often observed within categories. These findings highlight considerable potential to improve the availability and consistency of nutrition information on packaged products in Nigeria and to introduce further policies to reduce the amount of sodium in the Nigerian food supply.
Keywords: sodium, salt, nutritional labelling, packaged foods, hypertension, cardiovascular diseases, Nigeria
1. Background
Excess dietary intake of sodium increases the risk of high blood pressure, a major, modifiable risk factor for cardiovascular diseases (CVDs) [1,2]. CVDs and other diet-related non-communicable diseases (NCDs), including obesity, type 2 diabetes mellitus, and some cancers, are among the leading causes of global mortality in both high-income and low- and middle-income countries (LMIC) alike [3]. In Nigeria, the most populous country in Africa, high blood pressure is the leading cause of CVDs [4]. As in other LMIC contexts, Nigeria has experienced a nutrition transition over the past few decades, whereby traditional diets high in vegetables, fruits, and pulses have been replaced by an increasing proportion of highly processed and packaged foods [5]. The mean salt intake for Nigerian adults has been reported to be 7 g per day, which exceed the World Health Organization (WHO) daily recommendation of 2 grams (g) of sodium per day, which is equivalent to 5 g of salt per day [6,7]. The beneficial effects of reducing sodium intake on the prevention and control of high blood pressure are clear [8,9], yet the average global sodium intake is approximately 4 g per day or 10 g of salt per day [10]. Further, reducing sodium intake is a highly cost-effective strategy to control high blood pressure and prevent CVDs [11].
As part of the WHO Global Action Plan on the Prevention and Control of NCDs, WHO Member States have endorsed a global target of a 30% relative reduction in mean population intake of sodium, intending to achieve a target of less than 2 g of sodium (i.e., <5 g of salt) per day by 2025 [12]. Among its ‘best-buy’ strategies for highly cost-effective and feasible approaches to reducing population sodium intake, the WHO includes nutrition labelling reforms including back-of-pack nutrition information to quantify sodium content, and front-of-pack nutrition labelling to improve understanding and use of this information. Other ‘best-buy’ strategies include sodium reformulation targets for processed and packaged foods, provision of low sodium options in public settings such as schools and hospitals, and behaviour change through mass media campaigns [13]. In the context of sodium reduction specifically, WHO has synthesised these strategies through the SHAKE package (Surveillance of salt intake, Harness industry, Adopt standards for labelling and marketing, Knowledge to empower consumers, and Environments to promote healthy eating) to support a comprehensive approach for governments to maximise public health impact.
In 2019, Nigeria announced its National Multi-sectoral Action Plan (NMSAP) for NCDs, which included a target to reduce the mean population dietary sodium intake by at least 30% by 2025 in alignment with the WHO global target [14,15]. Meeting this target will require implementing the relevant WHO best buys and associated SHAKE strategies. In the area of nutrition labelling, Nigerian regulations, introduced in 2019, only require mandatory nutrient declarations on the back of pre-packaged foods and beverages that make a health or nutrient claim [16]. Where nutrient declarations are provided, the regulation specifies that this information can be provided per 100 g, per 100 mL, or per serving but should contain information on energy value, amounts of fat (specifying saturated and trans fat), carbohydrate (specifying the quantity from total sugars), protein, salt, and the amount of any other nutrient for which a nutrition or health claim is made [16]. While elements of these updated regulations are promising in that salt is now included as a required nutrient for the first time, the law still falls short of the international Codex Alimentarius Commissions Guidelines on Nutrition Labelling, [17], which recommend nutrient declarations be mandatory on all pre-packaged foods. The Codex Alimentarius also suggest nutrient declarations generally be presented on a standardised per 100 g or 100 mL basis to facilitate comparison and avoid confusion if based on serving size. This differs from Nigeria’s current allowance for manufacturers to provide nutrient declarations on a per serving basis.
To improve upon back-of-pack nutrition information, governments worldwide are following WHO recommendations to implement front-of-pack nutrition labelling (FOPNL) on packaged foods and beverages [8]. These simple, graphical labels use words and colours to provide at-a-glance information on nutritional quality to complement back-of-pack nutrient declarations. Existing authoritative guidance from both WHO and Codex support government action in this area [18], but provide limited detail on the appropriate content of national FOPNL regulation. In Nigeria, there have been efforts led by the Nigerian Heart Foundation to initiate a voluntary ‘Heart Tick’ style label on pre-packaged foods to identify heart-healthy foods [8], but there has yet to be any government-led FOPNL scheme developed or implemented in Nigeria.
Beyond these limited activities related to nutrition labelling, Nigeria has not yet commenced major policy activities in WHO’s other recommended areas of action on sodium. To provide a baseline estimate to guide national policy action, the objective of this study was to estimate the proportion of packaged foods and beverages displaying nutrition information for sodium and other nutrients specified by Nigerian nutrition labelling regulations and to determine the amount of sodium in packaged foods sold in Nigeria.
2. Methods
This study was a cross-sectional survey of all available commercially packaged foods and beverages in leading Nigerian retail stores in capital cities of the Federal Capital Territory, Kano, and Ogun states in Nigeria between November 2020 and March 2021. Using similar methods from previous studies [19,20], large and frequently visited retail supermarkets and stores were purposively chosen for data collection because these stores sell products that are widely sold and consumed. This retail survey is part of the larger, multi-faceted Nigeria Sodium Study, which seeks to evaluate Nigeria’s implementation of its dietary sodium policies, as detailed elsewhere [21].
2.1. Data Source
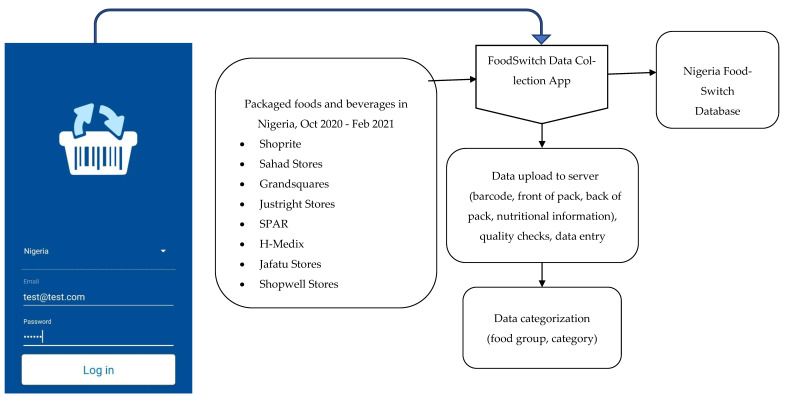
The George Institute for Global Health created its FoodSwitch system to collect information about the food supply in multiple jurisdictions worldwide. To support this study, we gained permission from store managers to collect data from leading retailers in three Nigerian states. The FoodSwitch Data Collector App was used by trained data collection officers who used study smartphones to scan the barcode and photograph the front- and back-of-food packaging, capturing information such as product names, nutrient declarations, ingredient lists, and manufacturer information. Photographs were uploaded into a cloud-based server, and then data were stored, extracted, and categorised using a standardised method by trained research staff [22] (Figure 1).
Figure 1.
Overview of the development of the Nigeria FoodSwitch Database, 2020.
2.2. Food Labelling and Food Composition Data
During data collection, we captured the presence or absence of a partial or complete nutrient declaration on pack. Where a nutrient declaration was present, we extracted available information on the following nutrients, where necessary converting information into the following standardised measurements: energy (kJ/100 g), protein (g/100 g), saturated fat (g/100 g), trans fat (g/100 g), carbohydrate (g/100 g), total sugar (g/100 g), sodium (mg/100 g), and salt (g/100 g). We defined a partial nutrient declaration as including information on at least one of the components specified in the Nigerian regulation, and a complete nutrient declaration as providing information on all components specified in the 2019 Nigerian regulation, i.e., energy, saturated fats, trans fats, carbohydrates, total sugars, protein, and either sodium or salt. We also extracted information on product manufacturers.
2.3. Data Categorisation
Products were grouped and categorised using the system developed by the Global Food Monitoring Group (GFMG) [19,20,21,22,23], which was based on previous reports, existing branded food databases, and expert consensus to optimise international comparison and interpretation by industry, and other stakeholders. This hierarchical system is designed to monitor the nutrient composition of food products globally [24]. Products were classified by trained dietitians and nutritionists into 16 major food categories: (a) bread and bakery products, (b) cereal and grain products, (c) confectionery, (d) convenience foods, (e) dairy, (f) edible oils and oil emulsions, (g) alcohol, (h) foods for specific dietary use, (i) fruits, vegetables, nuts and legumes, (j) meat and meat alternatives, (k) non-alcoholic beverages, (l) sauces, dressings, spreads, and dips, (m) seafood and seafood products, (n) snack foods, (o) sugars, honey and related products, and (p) vitamins and supplements. Products were identified by their unique barcode.
2.4. Statistical Analyses
The number and percentage of products displaying partial and complete nutrient declarations were reported, along with the number and percentage of products that displayed sodium information expressed either as sodium or salt, overall and by category. Salt per 100 g was converted to sodium per 100 mg by multiplying salt figure by 400. Descriptive statistics (i.e., medians, interquartile ranges, and ranges of sodium levels per 100 g) were also calculated and presented for each sub-category. All statistical analyses were conducted using SAS version 9.4 (The SAS Institute, Cary, NC, USA).
3. Results
Data were collected from retail outlets in Federal Capital Territory (n = 16), Kano (n = 17), and Ogun (n = 12) states.
3.1. Labelling Completeness of Packaged Food Products in Nigeria
A total of 7039 packaged foods and beverages made by 1089 unique manufacturers across 16 major food groups and 89 food categories were identified in the Nigerian supermarkets surveyed. The major food groups with the largest number of products were ‘bread and bakery products’ (n = 1352, 19.2%), followed by ‘fruits, vegetables, nuts, and legumes’ (n = 1015, 14.4%) and ‘non-alcoholic beverages’ (n = 889, 12.6%) (Table 1).
Table 1.
Overview of sodium labelling and content of packaged foods by major food group, and food categories in Nigeria, 2021.
| Food Group | Food Category | Total Number of Products | Products Displaying Sodium Content Information (%) | Sodium Content | ||
|---|---|---|---|---|---|---|
| Median (mg/100 g) |
IQR (mg/100 g) |
Range (mg/100 g) |
||||
| Bread and bakery products | Biscuits/cookies/crackers | 1240 | 80.9 | 273.0 | 186 | 0–40,000 |
| Bread | 20 | 90.0 | 568.5 | 1114.1 | 274.8–4000 | |
| Cakes, muffins, and pastries | 92 | 82.6 | 385.5 | 861.0 | 30–1533 | |
| Cereal and grain products | Breakfast cereals | 373 | 90.6 | 198.0 | 387.0 | 0–6800 |
| Couscous | 8 | 75.0 | 9.0 | 6.0 | 0–38 | |
| Miscellaneous cereal and grain products | 183 | 78.7 | 35.0 | 400.0 | 0–38,500 | |
| Noodles | 59 | 91.5 | 760.0 | 1342.0 | 0–1900 | |
| Pasta | 143 | 92.3 | 4.0 | 7.8 | 0–1029 | |
| Rice and rice products | 74 | 90.5 | 2.0 | 12.0 | 0–2000 | |
| Confectionery | Chewing gum | 46 | 95.7 | 8.0 | 16.0 | 0–505.8 |
| Chocolate and sweets/candy | 592 | 91.7 | 96.0 | 116.0 | 0–31,000 | |
| Cough lozenges | 1 | 100.0 | 21.5 | 0.0 | 21.5–21.5 | |
| Jelly (Jell-O) | 28 | 96.4 | 12.0 | 12.0 | 0–120 | |
| Convenience foods | Frozen Asian dumplings and similar products | 3 | 66.7 | 509.0 | 262.0 | 378–640 |
| Pre-prepared salads and sandwiches | 4 | 100.0 | 360.0 | 480.0 | 320–1200 | |
| Ready meals | 12 | 91.7 | 320.0 | 170.0 | 40–512 | |
| Soup | 27 | 100.0 | 236.0 | 68.0 | 21–5600 | |
| Seafood and seafood products | Canned seafood | 117 | 83.8 | 383.0 | 60.0 | 80–6360 |
| Dried seafood | 12 | 58.3 | 400.0 | 408.0 | 11–784 | |
| Fish spread | 2 | 100.0 | 400.0 | 160.0 | 320–480 | |
| Frozen seafood | 4 | 100.0 | 488.5 | 507.5 | 360–1160 | |
| Seafood and seafood products not otherwise specified | 4 | 75.0 | 1107.0 | 980.0 | 180–1160 | |
| Dairy | Cheese | 49 | 91.8 | 776.0 | 360.0 | 14–1800 |
| Cream | 19 | 94.7 | 32.0 | 30.0 | 0–248 | |
| Desserts | 59 | 81.4 | 71.1 | 178.0 | 4–762 | |
| Ice cream/edible ices | 21 | 90.5 | 100.0 | 108.0 | 12–241 | |
| Milk | 224 | 78.6 | 56.0 | 188.0 | 0–1221 | |
| Probiotic drinks | 2 | 100.0 | 8.0 | 0.0 | 8–8 | |
| Yoghurt/yoghurt drinks | 38 | 78.9 | 36.0 | 16.0 | 8–113 | |
| Foods for specific dietary use | Baby and infant foods | 146 | 90.4 | 146.0 | 167.0 | 0–367 |
| Diet drink mixes (meal replacements) | 13 | 100.0 | 89.0 | 162.0 | 0.4–360 | |
| Foods for specific dietary use not otherwise specified | 16 | 75.0 | 1.8 | 270.0 | 0–2280 | |
| Sports products | 4 | 50.0 | 124.0 | 212.0 | 18–230 | |
| Fruits, vegetables, nuts, and legumes | Fruit and fruit products | 91 | 95.6 | 5.9 | 40.0 | 0–5533 |
| Herbs and spices | 136 | 60.3 | 200.0 | 4983.0 | 0–35,833 | |
| Jam (jelly in the US) and marmalades | 64 | 81.3 | 8.0 | 40.0 | 0–195 | |
| MSG | 1 | 100.0 | 12,000.0 | 0.0 | 12,000–12,000 | |
| Nuts and seeds | 154 | 87.0 | 166.0 | 412.0 | 0–11,000 | |
| Salt, plain and flavoured | 21 | 47.6 | 29,125.0 | 26,256.0 | 0–39,680 | |
| Seasoning | 183 | 65.0 | 21,910.0 | 14,500.0 | 0–37,500 | |
| Vegetables | 365 | 92.9 | 268.0 | 565.0 | 0–24,000 | |
| Non-alcoholic beverages | Beverage mixes | 154 | 79.9 | 133.0 | 279.0 | 0–10,500 |
| Breakfast beverages | 24 | 100.0 | 145.0 | 160.0 | 46–710 | |
| Coffee and tea | 284 | 87.7 | 0.0 | 107.0 | 0–37,000 | |
| Cordials (syrups) | 7 | 100.0 | 0.0 | 0.0 | 0–24 | |
| Electrolyte (sports) drinks | 7 | 100.0 | 0.0 | 0.0 | 0–53 | |
| Energy drinks | 48 | 91.7 | 40.0 | 51.5 | 0–125 | |
| Fermented beverages (e.g., Kombucha) | 2 | 50.0 | 66.0 | 0.0 | 66–66 | |
| Fruit and vegetable juices | 218 | 78.9 | 4.0 | 10.0 | 0–9100 | |
| Non-alcoholic beverages not otherwise specified | 9 | 77.8 | 10.0 | 383.0 | 0–2000 | |
| Soft drinks | 111 | 74.8 | 4.0 | 8.2 | 0–21,000 | |
| Waters | 25 | 48.0 | 16.0 | 18.0 | 0–600 | |
| Sauces, dressings, spreads and dips | Mayonnaise/salad dressings | 153 | 98.0 | 535.0 | 385.0 | 0–1867 |
| Sauces | 367 | 84.2 | 680.0 | 974.0 | 0–22,000 | |
| Spreads and dips | 88 | 96.6 | 391.0 | 448.0 | 0–1640 | |
| Alcohol | Alcohol not otherwise specified | 1 | 100.0 | 0.0 | 0.0 | 0–0 |
| Beer | 3 | 33.3 | 0.0 | 0.0 | 0–0 | |
| Cordial, mixers and syrups (integrated alcoholic beverages) | 3 | 66.7 | 41.5 | 77.0 | 3–80 | |
| Liquor (distilled spirits) | 11 | 54.5 | 21.5 | 37.0 | 0–60 | |
| Wine | 28 | 92.9 | 0.0 | 4 | 0–18,800 | |
| Edible oils and oil emulsions | Cooking oils | 155 | 86.5 | 0.0 | 0.0 | 0–11,100 |
| Edible oils | 58 | 77.6 | 470.0 | 981.0 | 0–1870 | |
| Meat and meat alternatives | Meat alternatives | 2 | 100.0 | 0.0 | 0.0 | 0–0 |
| Processed meat | 79 | 53.2 | 912.0 | 460.0 | 85.1–7360 | |
| Sugars, honey and related products | Condensed caramel | 1 | 100.0 | 60.0 | 0.0 | 60–60 |
| Dessert additions (e.g., sprinkles) | 1 | 100.0 | 48.0 | 0.0 | 48–48 | |
| Dessert toppings (e.g., caramel sauce) | 5 | 100.0 | 163.0 | 175.0 | 4–200 | |
| Food essence and colouring | 13 | 92.3 | 0.0 | 300.0 | 0–6360 | |
| Honey and pollen | 37 | 94.6 | 3.0 | 12.0 | 0–40 | |
| Icing | 6 | 83.3 | 0.0 | 4.0 | 0–258 | |
| Sugar | 16 | 87.5 | 5.2 | 15.0 | 0–120 | |
| Sugars, honey, and related products not otherwise specified | 6 | 100.0 | 30.5 | 80.0 | 0–240 | |
| Sweeteners | 27 | 77.8 | 0.0 | 36.0 | 0–9120 | |
| Syrups | 48 | 97.9 | 23.0 | 166.1 | 0–333 | |
| Snack foods | Cassava chips | 6 | 100.0 | 394.0 | 331.0 | 308–679 |
| Cereal/nut-based snack bars | 35 | 94.3 | 228.0 | 250.4 | 12–756.4 | |
| Corn-based snacks/chips | 20 | 75.0 | 476.0 | 290.8 | 76.1–1067 | |
| Extruded snacks | 1 | 100.0 | 1200.0 | 0.0 | 1200–1200 | |
| Legume-based snacks/chips (e.g., Wasabi peas) |
9 | 77.8 | 413.6 | 633.0 | 0–1040 | |
| Noodle-based snacks/chips | 3 | 100.0 | 401.0 | 621.0 | 357–978 | |
| Popcorn | 37 | 64.9 | 490.5 | 698.5 | 3.6–1188 | |
| Potato-based snacks and chips/crisps | 137 | 92.7 | 640.0 | 326.0 | 40–1887 | |
| Pretzels | 2 | 100.0 | 850.0 | 100.0 | 800–900 | |
| Rice-based snacks | 12 | 91.7 | 113.0 | 485.0 | 47.5–1182 | |
| Salt and vinegar flavoured snacks (excl. Potato chips) | 7 | 85.7 | 762.5 | 719.0 | 40–2000 | |
| Snack foods not otherwise specified | 76 | 77.6 | 474.0 | 642.0 | 0–1900 | |
| Snack packs | 21 | 85.7 | 736.0 | 285.0 | 0–1087 | |
| Vegetable-based snacks/chips | 9 | 88.9 | 519.5 | 342.5 | 140–1040 | |
| Wholegrain chips | 2 | 100.0 | 930.0 | 340.0 | 760–1100 | |
| Vitamins and supplements | – | 4 | 50.0 | 2.0 | 4.0 | 0–4 |
11 products were excluded from the table as they were unable to be categorised.
We identified 6439 (91.5%) products with a partial or incomplete nutrient declaration; however, only 105 products (1.5%) displayed complete nutrient declaration in compliance with the 2019 update to Nigeria’s nutrition labelling regulation. The remaining 495 (7.0%) products displayed no nutrient information (Table 2). The information most frequently missing from incomplete nutrient declarations was trans fats (only present on 26% of products) and sodium expressed as ‘salt’ as per the requirements of regulation (only present on 38% of all products) (Supplementary Figure S1).
Table 2.
Nutrition labelling of foods and beverages in the Nigerian food supply.
| Total Number of Products (N) |
Percent of Food Supply (%) |
|
|---|---|---|
| Complete nutrient declaration: provides a nutrient declaration with information on all food components required by 2019 regulation | 105 | 1.5 |
| Partial nutrient declaration: provides a nutrient declaration with at least one nutrient from energy, saturated fat, trans fat, carbohydrates, sugars, protein, salt. | 6439 | 91.5 |
| No nutrient declaration | 495 | 7.0 |
| 7039 |
MSG: Monosodium glutamate.
Information on sodium content was obtained from the labels of 6032 (85.7%) products. Of these, 59.0% (n = 3559) provided this information expressed as sodium, and 44.6% (n = 2689) displayed this information as ‘salt’. A small number of products (n = 216; 3.6%) provided information as both sodium and salt (Supplementary Table S1). The form of presenting this information in the nutrient declaration also varied, with 61.4% (n = 3704) products providing information on both a standardised per 100 g/mL basis and per serving, 37.1% (n = 2238) presenting information based on per 100 g only, and 1.5% (n = 90) presenting information on a per serving basis only (Supplementary Figure S2).
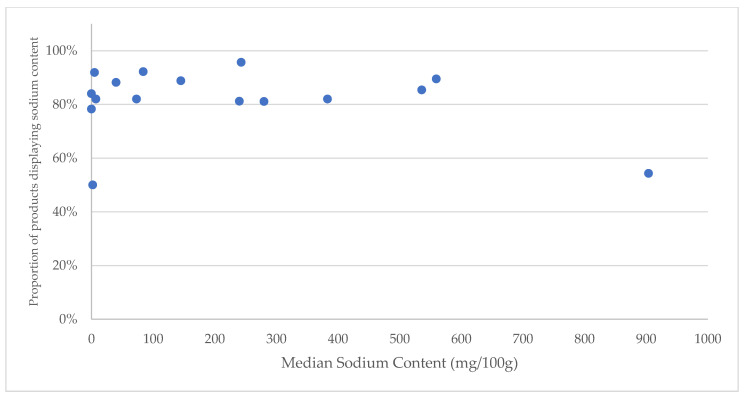
Provision of sodium information varied by category and was most prevalent in the categories of ‘convenience foods’ (n = 42/44, 96%), ‘confectionary’ (n = 566/615, 92%), ‘sugars, honey, and related products’ (n = 135/147, 92%), and ‘sauces, dressings, spreads, and dips’ (n = 484/544, 89%). Provision of sodium information was lowest in the categories of ‘meat and meat alternatives’ (n = 24/44, 55%) and ‘vitamins and supplements’ (n = 2/4, 50%) (Figure 2).
Figure 2.
Prevalence of sodium labelling and median sodium content reported for the 16 defined categories of packaged foods and beverages in Nigerian retail stores by median sodium context, 2020–2021.
Provision of sodium information also varied by manufacturer. Of the 1089 unique manufacturers, 430 (39.5%) displayed sodium or salt information on all products, 209 (19.2%) had sodium or salt information on some products, and 449 (41.2%) did not present sodium or salt information at all (Supplementary Table S2).
3.2. Sodium Content of Packaged Foods Available in Nigeria
The declared sodium content was highly variable between food groups and categories (Figure 2). The major food groups with the highest median sodium content were ‘meat and meat alternatives’ (904 mg/100 g), ‘sauces, dressings, spreads, and dips’ (559.5 mg/100 g) and ‘snack foods’ (536 mg/100 g). Major food groups with the lowest median sodium content (mg/100 g) were ‘vitamins and supplements (2 mg/100 g), ‘sugars, honey, and related products’ (5 mg/100 g) and ‘non-alcoholic beverages’ (7.2 mg/100 g).
For some high sodium food groups, information on sodium content was more limited; for example, sodium labelling was only present on 54% (n = 44) of ‘meat and meat alternatives’ despite this being the group with the highest median content. Similarly, products such as ‘edible oils and oil emulsion’ and alcohol displayed labels with zero sodium content among 84% (n = 179) and 78% (n = 36) of products, respectively. Packaged foods and beverages with zero sodium content had about 50% sodium labeling, and this was similar to products reported with about 900 mg/100g; whereas, products reported with sodium content between 200 mg/100g and 300 mg/100g were reported to have highest sodium labeling (Figure 2).
4. Discussion
In this study, we assessed the prevalence and completeness of the nutrient declaration, the prevalence of sodium labelling on the pack, and the reported sodium content of food and beverage products available in Nigerian retail markets in three major cities. This is the largest retail survey of its kind in Nigeria to date, and so while the sampling frame may not have been representative, it is likely to have captured the most commonly sold and consumed packaged foods and beverages. Overall, 91.5% (n = 6439) provided only partial nutrition information, 7.0% (n = 495) provided no nutritional information, and only 1.5% (n = 105) displayed a nutrient declaration that included all nutrients specified by 2019 Nigerian regulations. Sodium content of packaged foods and beverage were found to be highest for ‘meat and meat alternatives’, ‘sauces, dressings, spreads, and dips’, and ‘snack foods’.
Our investigation revealed that very limited packaged foods and beverages provided complete nutritional information with reference to the 2019 Nigeria food labelling regulations. Food products and beverages were more likely to have partial nutritional information available on the pack of the products. The 2019 Nigeria food labelling regulations required that salt should be displayed on the product package, but less than half of the packaged food products and beverages met this regulation. The overall sodium labelling of packaged foods and beverages in Nigeria (sodium = 45%; salt 59%) was found to be higher compared to what was previously reported in a study conducted in Kenya, where 39% of packaged food products displayed sodium content; this was also the same for another study conducted in India, where only 32% sodium labelling was reported. Sodium content of packaged foods and beverage were found to be highest for ‘meat and meat alternatives’, ‘sauces, dressings, spreads, and dips’, and ‘snack foods’.
Provision of consistent and understandable nutrient information through accurate and complete back-of-pack nutrient declarations is important to inform consumer choice and promote transparency in the food supply. Our results show that very few products in Nigeria displayed nutrient declarations that fully comply with the information required by the 2019 nutrition labelling regulations, though the vast majority of products provided at least partial information. This may be in part related to the relatively recent introduction of new regulations, and also related to those regulations only requiring nutrient declarations to be provided on a mandatory basis on products which make a health or nutrient claim, but also suggests significant scope to improve uptake.
Other elements of our analysis of nutrition labelling information also suggest areas for improving the utility of Nigeria’s food labels for consumers. Among Nigerian products currently displaying a partial or complete nutrient declaration, inconsistencies in the way this information is provided, for example as both salt and sodium, and not consistently using a per 100 g or 100 mL standardised presentation, also limit the usability of this information to consumers. At a minimum, Nigeria could strengthen front-of-pack nutrition labelling requirements to be consistent with international Codex Alimentarius which require mandatory nutrient declarations for all pre-packaged foods and suggest that nutrient declarations be generally presented using a standardised per 100 g or 100 mL basis to facilitate comparisons between foods.
Improved back-of-pack nutrient declarations are also necessary to support a variety of other WHO ‘best-buy’ policies to address unhealthy diets and prevent and control NCDs. These policies include reformulation programs and targets, procurement standards for public settings such as schools and hospitals, and front-of-pack nutrition labelling systems, each of which relies on information drawn from accurate nutrient declarations for effective implementation [25,26]. For Nigeria to make progress toward its National Multi-Sectoral Action Plan target to reduce the mean population′s dietary sodium intake by at least 30% by 2025, further action should be considered to improve nutrition labelling to facilitate the implementation of these policies. Nigeria can learn from other countries that have developed sodium reduction policies, such as the UK that has successful implemented a reformulation program on salt reduction strategies, and nearby South Africa which has implemented mandatory sodium limits in regulation for certain food categories [27].
Our study findings on reported sodium content are consistent with previous studies which have identified the food groups that have the highest levels and concentrations of sodium content in the food supply [28]. For example, in South Africa, snack foods, meat and meat alternatives, and sauces and spreads were similarly reported to be food groups with the highest median sodium content. Similarly, confectionary foods and dairy were both reported in Nigeria and South Africa as the food groups with the lowest sodium content. Variability in sodium content within categories of foods highlights the potential for reformulation programs to reduce the sodium content [29].
To reduce the burden of CVDs, sodium reduction is one of the major priority actions globally [30,31]. In Nigeria, there is an urgent need for the adoption of a sodium reduction strategy incorporating a range of WHO best-buy policies. Without stronger action to improve the food environment, there is unlikely to be meaningful progress towards reducing population sodium intake.
The strength of this study is the fact that it included a large number of packaged products in the Nigerian food and beverage supply with data captured directly from retail stores using a structured and widely reported approach. An important limitation of the current study is that data were collected from supermarkets and stores from three cities; thus, these results may not be nationally representative of all food and beverage products sold in Nigeria but likely provide the best estimate of commonly available packaged foods and beverages. Future research from this study will collect and evaluate information on unpackaged and street/restaurant foods and beverages. Another limitation in this study was that we relied on the validity and accuracy of the nutritional information displayed on the NIP of the food products. While it may be possible the chemical analysis of food products may provide more precision information about the nutritional content of packaged foods and beverages, this approach is expensive and was outside the scope of the current study. Finally, the lack of sales data to understand the potential impact of findings was also a challenge.
5. Conclusions
These findings highlight considerable potential to improve the availability and consistency of nutrition information on packaged products in Nigeria and to introduce further actions to reduce the amount of sodium in the Nigerian food supply. Low nutrient declaration and sodium labelling of packaged foods and beverages call for interventions of the relevant stakeholders in Nigeria. To improve the utility of food labels for consumers and improve transparency in the food supply, further action could be considered by the Nigerian stakeholders to strengthen nutrition labelling by requiring complete nutrient declarations for all packaged products. Taking this step will also facilitate the implementation of other recommended policies for sodium reduction, including reformulation programs and front-of-pack nutrition labelling to work towards Nigeria’s targeted 30% reduction in population sodium intake by 2025.
Acknowledgments
The authors wish to acknowledge Nadia Laznik from The George Institute for Global Health for her contributions to the data collection and quality assurance in this current study. The authors also wish to thank Aiyedun Oluwatumininu, Ikechukwu-Orji Mercy, and Ibukunoluwa Owoade who supervised the data collection at the study sites.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/nu15010027/s1, Table S1: Provision of sodium and/or salt information on packaged foods in Nigeria. Table S2: Distribution of packaged foods products in Nigeria by the compliance of sodium labelling by manufacturers. Figure S1: Presentation of information on specific nutrients required by Nigerian regulation within the nutrient declaration of foods and beverages in the Nigerian food supply. Figure S2: Sodium/Salt content of foods and beverages in the Nigerian food supply, 2020–2021.
Author Contributions
M.D.H., D.B.O. and B.N. conceptualised the idea of this study; A.E.O., A.J., C.E.O., V.O.A., R.O., G.L.S., I.A.O., S.O., A.C., L.V.V.H., L.R.H., K.T., F.T., K.H., M.I., M.J.W., V.T.-T., B.N., M.D.H. and D.B.O. contributed to the design of the study; A.E.O. and V.O.A. conducted the study with oversight support from F.T., B.N., M.D.H. and D.B.O.; A.C. and A.E.O. analysed the data with support from A.J. and K.T.; A.E.O. and D.B.O. drafted the first draft of the paper. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Restricted data were accessed remotely through the FoodSwitch database.
Conflicts of Interest
AEO was supported through the PhD global health fellowship program of the University Medical Centre, Utrecht University, Julius Centre for Global Health, The Netherlands.
Funding Statement
National Heart, Lung, and Blood Institute (UG3HL152381).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.He F.J., Li J., Macgregor G.A. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst. Rev. 2013;2013:CD004937. doi: 10.1002/14651858.CD004937.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amine E.K., Baba N.H., Belhadj M., Deurenberg-Yap M., Djazayery A., Forrestre T., Galuska D.A., Herman S., James W.P.T., M’Buyamba Kabangu J.R., et al. Diet, Nutrition and the Prevention of Chronic Diseases. WHO; Geneva, Switzerland: 2003. (WHO Technical Report Series). [DOI] [Google Scholar]
- 3.Young F., Critchley J.A., Johnstone L.K., Unwin N.C. A review of co-morbidity between infectious and chronic disease in Sub Saharan Africa: TB and Diabetes Mellitus, HIV and Metabolic Syndrome, and the impact of globalization. Glob. Health. 2009;5:1–9. doi: 10.1186/1744-8603-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akinlua J.T., Meakin R., Umar A.M., Freemantle N. Current prevalence pattern of hypertension in Nigeria: A systematic review. PLoS ONE. 2015;10:e0140021. doi: 10.1371/journal.pone.0140021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ronto R., Wu J.H.Y., Singh G.M. The global nutrition transition: Trends, disease burdens and policy interventions. Public Health Nutr. 2018;21:2267–2270. doi: 10.1017/S1368980018000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van de Vijver S., Akinyi H., Oti S., Olajide A., Agyemang C., Aboderin I., Kyobutungi C. Status report on hypertension in Africa—Consultative review for the 6th Session of the African Union Conference of Ministers of Health on NCD’s. Pan Afr. Med. J. 2013;16:1–17. doi: 10.11604/pamj.2013.16.38.3100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . Noncommunicable Diseases Country Profiles. WHO; Geneva, Switzerland: 2018. [(accessed on 2 February 2022)]. Available online: https://apps.who.int/iris/handle/10665/274512. [Google Scholar]
- 8.Jones A., Neal B., Reeve B., Ni Mhurchu C., Thow A.M. Front-of-pack nutrition labelling to promote healthier diets: Current practice and opportunities to strengthen regulation worldwide. BMJ Glob. Health. 2019;4:e001882. doi: 10.1136/bmjgh-2019-001882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tekle D.Y., Santos J.A., Trieu K., Thout S.R., Ndanuko R., Charlton K., Hoek A.C., Huffman M.D., Jan S., Webster J. Monitoring and implementation of salt reduction initiatives in Africa: A systematic review. J. Clin. Hypertens. 2020;22:1355–1370. doi: 10.1111/jch.13937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Odili A.N., Chori B.S., Danladi B., Nwakile P.C., Okoye I.C., Abdullahi U., Zawaya K., Essien I., Sada K., Nwegbu M.M., et al. Urinary sodium excretion and its association with blood pressure in Nigeria: A nationwide population survey. J. Clin. Hypertens. 2020;22:2266–2275. doi: 10.1111/jch.14069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cappuccio F.P., Capewell S., Lincoln P., McPherson K. Policy options to reduce population salt intake. BMJ. 2011;343 doi: 10.1136/bmj.d4995. [DOI] [PubMed] [Google Scholar]
- 12.WHO . Action Plan for the Prevention and Control of Noncommunicable Diseases in the WHO European Region. WHO; Geneva, Switzerland: 2016. pp. 12–15. [Google Scholar]
- 13.WHO . ‘Best Buys’ and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases. WHO; Geneva, Switzerland: 2017. pp. 65–70. The Updated Appendix 3 of the WHO Global NCD Action Plan 2013–2020. [Google Scholar]
- 14.Ncdsng B. National Multi-Sectoral Action Plan for the Non-Communicable Diseases. Federal Ministry of Health; Abuja, Nigeria: 2019. [Google Scholar]
- 15.Organization World Health . World Health Organization Guideline: Sodium Intake for Adults and Children. WHO; Geneva, Switzerland: 2012. pp. 1–56. [PubMed] [Google Scholar]
- 16.National Agency for Food and Drug Administration and Control (NAFDAC) Pre-Packaged Food, Water and Ice Labelling Regulations. NAFDAC; Abuja, Nigeria: 2019. [Google Scholar]
- 17.Ipa P., Di S. Guidelines on Nutrition Labelling CXG 2-1985 Adopted. Volume 4 Food and Agriculture Organization of the United Nations; Rome, Italy: World Health Organization; Geneva, Switzerland: 2017. Codex Alimentarius International Food Standards. [Google Scholar]
- 18.Naidoo P., Foundation S., Africa S., Popkin B.M. World Heart Federation Policy Brief: Front-of-Pack Labelling. Glob. Heart. 2020;15:70. doi: 10.5334/gh.935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ndanuko R., Maganja D., Kibet A., Coyle D.H., Kimiywe J., Raubenheimer D., Marklund M., Wu J.H.Y. Sodium content and labelling completeness of packaged foods and beverages in Kenya. Nutrients. 2021;13:1385. doi: 10.3390/nu13041385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dunford E.K., Farrand C., Huffman M.D., Raj T.S., Shahid M., Ni Mhurchu C., Neal B., Johnson C. Availability, healthiness, and price of packaged and unpackaged foods in India: A cross-sectional study. Nutr. Health. 2022;28:571–579. doi: 10.1177/02601060211039124. [DOI] [PubMed] [Google Scholar]
- 21.Ojji D. Developing long-term strategies to reduce excess salt consumption in Nigeria. Eur. Heart J. 2022;43:1277–1279. doi: 10.1093/eurheartj/ehac025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunford E., Trevena H., Goodsell C., Ng K.H., Webster J., Millis A., Goldstein S., Hugueniot O., Neal B. FoodSwitch: A mobile phone app to enable consumers to make healthier food choices and crowdsourcing of national food composition data. JMIR mHealth uHealth. 2014;2:e37. doi: 10.2196/mhealth.3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Powles J., Fahimi S., Micha R., Khatibzadeh S., Shi P., Ezzati M., Engell R.E., Lim S.S., Danaei G., Mozaffarian D. Global, regional and national sodium intakes in 1990 and 2010: A systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3:e003733. doi: 10.1136/bmjopen-2013-003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elizabeth K Dunford International collaborative project to compare and track the nutritional composition of fast foods. BMC Public Health. 2012;12:559. doi: 10.1186/1471-2458-12-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dunford E.K., Guggilla R.K., Ratneswaran A., Webster J.L., Maulik P.K., Neal B.C. The adherence of packaged food products in Hyderabad, India with nutritional labelling guidelines. Asia Pac. J. Clin. Nutr. 2015;24:540–545. doi: 10.6133/apjcn.2015.24.3.08. [DOI] [PubMed] [Google Scholar]
- 26.Ministry of Health . Reducing Salt Intake in Malaysia: An Interim Evaluation of What Works. WHO; Geneva, Switzerland: 2019. pp. 1–33. [Google Scholar]
- 27.Trevena H., Neal B., Dunford E., Wu J.H.Y. An evaluation of the effects of the Australian food and health dialogue targets on the sodium content of bread, Breakfast cereals and processed meats. Nutrients. 2014;6:3802–3817. doi: 10.3390/nu6093802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gillespie C., Maalouf J., Yuan K., Cogswell M.E., Gunn J.P., Levings J., Moshfegh A., Ahuja J.K.C., Merritt R. Sodium content in major brands of US packaged foods, 2009. Am. J. Clin. Nutr. 2015;101:344–353. doi: 10.3945/ajcn.113.078980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peters S.A.E., Dunford E., Ware L.J., Harris T., Walker A., Wicks M., van Zyl T., Swanepoel B., Charlton K.E., Woodward M., et al. The sodium content of processed foods in South Africa during the introduction of mandatory sodium limits. Nutrients. 2017;9:404. doi: 10.3390/nu9040404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mozaffarian D., Fahimi S., Singh G.M., Micha R., Khatibzadeh S., Engell R.E., Lim S., Danaei G., Ezzati M., Powles J. Global Sodium Consumption and Death from Cardiovascular Causes. N. Engl. J. Med. 2014;371:624–634. doi: 10.1056/NEJMoa1304127. [DOI] [PubMed] [Google Scholar]
- 31.Bertram M.Y., Steyn K., Wentzel-Viljoen E., Tollman S., Hofman K.J. Reducing the sodium content of high-salt foods: Effect on cardiovascular disease in South Africa. S. Afr. Med. J. 2012;102:743–745. doi: 10.7196/SAMJ.5832. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Restricted data were accessed remotely through the FoodSwitch database.