Abstract
Porphyromonas gingivalis, a gram-negative anaerobe, is implicated in the etiology of adult periodontitis. P. gingivalis fimbriae are one of several critical surface virulence factors involved in both bacterial adherence and inflammation. P. gingivalis fimbrillin (FimA), the major subunit protein of fimbriae, is considered an important antigen for vaccine development against P. gingivalis-associated periodontitis. We have previously shown that biologically active domains of P. gingivalis fimbrillin can be expressed on the surface of the human commensal bacterium Streptococcus gordonii. In this study, we examined the effects of oral coimmunization of germfree rats with two S. gordonii recombinants expressing N (residues 55 to 145)- and C (residues 226 to 337)-terminal epitopes of P. gingivalis FimA to elicit FimA-specific immune responses. The effectiveness of immunization in protecting against alveolar bone loss following P. gingivalis infection was also evaluated. The results of this study show that the oral delivery of P. gingivalis FimA epitopes via S. gordonii vectors resulted in the induction of FimA-specific serum (immunoglobulin G [IgG] and IgA) and salivary (IgA) antibody responses and that the immune responses were protective against subsequent P. gingivalis-induced alveolar bone loss. These results support the potential usefulness of the S. gordonii vectors expressing P. gingivalis fimbrillin as a mucosal vaccine against adult periodontitis.
Porphyromonas gingivalis is a pathogen strongly associated with some forms of adult periodontitis, a chronic infection of the periodontium which causes destruction of the alveolar bone, leading to tooth loss (40). P. gingivalis is armed with a number of virulence factors that enable this organism to cause disease (15). Among these, P. gingivalis fimbriae are one of the critical cell surface virulence factors operative at early, as well as later, stages of infection (10). The major fimbrial subunit protein (fimbrillin, FimA) plays an important role in the progression of disease. The FimA protein mediates bacterial colonization through binding to saliva-coated pellicles (2, 16, 17), other bacteria (1, 13), epithelial cells (14, 24, 36), and endothelial cells (3). FimA is also a potent inducer of proinflammatory cytokines involved in tissue destruction and loss of alveolar bone (25, 26). Further, immunization with FimA protein has been shown to reduce P. gingivalis-induced alveolar bone loss in experimental rats (6–8) and confer protection against subsequent lethal infection with P. gingivalis in mice (4). Thus, P. gingivalis FimA protein is considered an important candidate antigen for vaccine development.
To develop live vectors for delivery of FimA antigen to a host mucosal immune system, we have genetically engineered Streptococcus gordonii strains that surface express biologically active N (residues 55 to 145)- and C (residues 226 to 337)-terminal polypeptide domains of P. gingivalis fimbrillin (31–33). S. gordonii is a human oral commensal that is currently being developed as a vector for delivery of vaccines against viral and bacterial pathogens (5, 9, 20–22, 27, 29). These studies have demonstrated the feasibility of utilizing an S. gordonii vector for induction of systemic and local immune responses against heterologous antigens expressed on the surface of S. gordonii by colonizing the host mucosal surfaces such as the oral, gut, and vaginal mucosal surfaces.
The present study was undertaken to test the ability of oral immunization with S. gordonii recombinants surface expressing P. gingivalis FimA polypeptides to induce specific immune responses in rats. Further, the efficacy of oral immunization in conferring protection against P. gingivalis-induced alveolar bone loss was evaluated. Here we show that oral coimmunization with the S. gordonii recombinants expressing N- and C-terminal functional domains of P. gingivalis fimbrillin in germfree rats is effective in inducing specific antibodies in serum and saliva and in conferring protection against P. gingivalis-induced alveolar bone loss.
MATERIALS AND METHODS
Bacterial strains, media, and culture conditions.
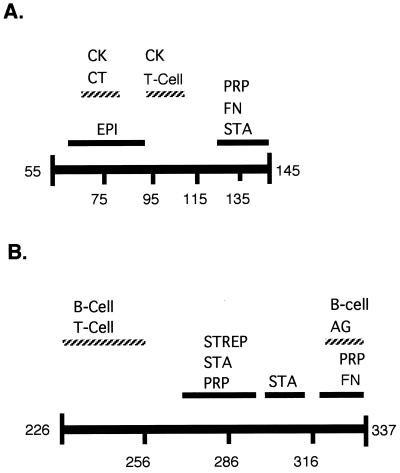
S. gordonii strain GP251 and recombinant strains SgFimN and SgFimC2 have been described previously (31, 32). Briefly, S. gordonii GP251 is the vaccine carrier strain used for construction of two FimA-expressing recombinants, SgFimN (expressing residues 55 to 145 of FimA) and SgFimC233+322 (expressing residues 226 to 337 of FimA), respectively. SgFimC233+322 (renamed SgFimC2) was constructed after modification of cysteine residues in the C-terminal FimA domain (residues 226 to 337) to facilitate its expression on the surface of S. gordonii (31). SgFimN and SgFimC2 are stable transformants that express FimA polypeptides by chromosome-integrated fimA gene fragments. S. gordonii was grown in Todd-Hewitt broth containing 0.2% yeast extract with or without 1.5% agar under anaerobic conditions and harvested at the late log phase (optical density at 600 nm of 1.0). Bacterial suspensions were washed and resuspended in phosphate-buffered saline (PBS). Each bacterial suspension was then diluted to obtain approximately 2 × 1010 cells/ml (optical density at 600 nm of 1.0 = 109 cells/ml). The N (residues 55 to 145)- and C (residues 226 to 337)-terminal domains of P. gingivalis fimbrillin selected for expression on SgFimN and SgFimC2, respectively, are shown in Fig. 1. These domains of the P. gingivalis FimA protein were selected based on their role in adherence to host surfaces (epitopes involved in binding to salivary components, fibronectin, fibrinogen, and epithelial cells) and their role in modulation of the host immune response (epitopes involved in B-cell and T-cell recognition and epitopes involved in cytokine induction). P. gingivalis 381, used for challenge infection in germfree rats, was cultured according to previously described procedures (18). Briefly, P. gingivalis 381 was grown in half-strength brain heart infusion (18 mg/ml; Difco) supplemented with 5 mg of yeast extract per ml, 5 μg of hemin per ml, and 0.2 μg of menadione per ml and buffered at pH 7.4 under anaerobic conditions (anaerobic chamber; Forma Scientific, Marietta, Ohio) for 48 h. Cells were harvested after 2 days and washed with PBS, and a bacterial suspension for inoculation was made in 5% carboxymethyl cellulose.
FIG. 1.
Domain structures of FimA segments expressed on the surfaces of SgFimN (A) and SgFimC2 (B) recombinants. These data were compiled from a review (15) and our previous studies (31, 32). Abbreviations: AG, immunodominant; B-Cell, stimulation of B cells; CK, stimulation of cytokines; CT, chemotaxis; EPI, binding to epithelial cells; FN, binding to fibronectin; PRP, binding to salivary PRPs; STA, binding to statherin; STREP, binding to Streptococcus oralis; T-Cell, stimulation of T cells.
Protocol for animal experiments. (i) Vector control.
To determine if the vaccine carrier strain (S. gordonii GP251) used for construction of FimA-expressing recombinants would itself colonize germfree rats without causing alveolar bone loss, a condition important for the subsequent evaluation of a recombinant S. gordonii vaccine utilizing the germfree-rat model of P. gingivalis-associated alveolar bone loss, the following protocol was performed. The following groups of rats (eight per group) were infected: group 1 (GF), germfree control group (sham colonized and sham infected); group 2 (Sg), S. gordonii (GP251) colonized; group 3 (PgINF, monoinfected), P. gingivalis infected; group 4 (Sg/PgINF, dually infected), S. gordonii colonized and challenged with P. gingivalis. The experimental protocol was as follows. Three-week-old male Sprague-Dawley germfree rats (Taconic Farm, Germantown, N.Y.) were maintained under sterile conditions, and all food, bedding, and water was sterilized. Animals belonging to a group were housed together in a single isolator. Oral colonization with S. gordonii was carried out by administering two inoculations 24 h apart, each with a total of 200 μl of a bacterial suspension (109 CFU), into the oral cavity. To assess S. gordonii colonization, oral swabs were taken at regular weekly intervals and cultured by plating on blood agar plates containing erythromycin (5 μg/ml for SgFimN and SgFimC2) or chloramphenicol (5 μg/ml for S. gordonii GP251) as a selection marker. Plates displaying two or more colonies with characteristic streptococcal morphology (gram-positive bacterial chains) were considered positively colonized. Group 3 was infected with P. gingivalis alone, and group 4 was infected with P. gingivalis 2 weeks following administration of the last S. gordonii dose. P. gingivalis infection was carried out by oral gavage three times at 48-h intervals. Each P. gingivalis dose consisted of 0.5 ml of a bacterial suspension (1012 bacteria) in 5% carboxymethyl cellulose (low viscosity; Sigma Chemical Co., St. Louis, Mo.). Microbiological samples were taken from the oral cavity and feces to evaluate P. gingivalis infection status. Animals were sacrificed 42 days following the last P. gingivalis infection dose. On termination, the rat jaws were defleshed and stained with 1% methylene blue to delineate the cementoenamel junction (CEJ). The distance from the CEJ to the alveolar bone crest (ABC) was measured at 14 sites on the mandible using a calibrated dissecting microscope (magnification, ×30). All measurements are made in triplicate by two individuals in a blinded fashion. The results were averaged and expressed as the mean number of millimeters of bone loss per site for each animal. The number of millimeters of bone loss per group was derived by taking the average of the individuals in that group.
(ii) Kinetics of the FimA-specific immune response following oral coimmunization with recombinant S. gordonii vectors (SgFimN and SgFimC2).
To determine the kinetics of the FimA-specific immune response in serum and saliva following coimmunization with the two S. gordonii recombinant vectors expressing N- and C-terminal epitopes of the P. gingivalis FimA protein (SgFimN and SgFimC2, respectively), the following procedures were employed. Two groups of 18 rats each were colonized with a vaccine combination (group 1, coimmunized with SgFimN and SgFimC2) or with the carrier S. gordonii strain (group 2, S. gordonii GP251). Oral immunization was carried out by administering two inoculations 24 h apart, each with a total of 50 μl of a bacterial suspension (109 CFU of each strain), into the oral cavity. This was followed by a second immunization with a similar dose 3 weeks following the first immunization. Rats were maintained as described above and sacrificed (six rats at each time point) at weeks 3, 6, and 9 to determine the kinetics of the serum and salivary FimA-specific immune responses. To assess colonization by SgFimN and SgFimC2, oral swabs were taken at regular intervals and cultured by plating on blood agar plates containing erythromycin. The expression of fimbrillin polypeptides by recombinants recovered from the oral cavity was determined by Western immunoblot analyses using N terminus-specific or full-length-specific antifimbrillin antibodies (31).
Antibody analyses.
Blood and saliva samples were collected for antibody measurements. Approximately 0.5 ml of saliva was obtained from each rat after subcutaneous injection of 1% pilocarpine nitrate (0.1 ml/100 g of body weight). Blood was obtained by cardiac puncture, and the serum was separated by centrifugation and stored at −20°C. The FimA-specific serum immunoglobulin G (IgG) and IgA titers were determined by a two-step fluorescent enzyme-linked immunosorbent antibody (ELISA) technique (particle concentration fluorescence immunoassay [PCFIA]) described previously (7). Briefly, recombinant fimbrillin was purified according to our previously described procedure (34) and used to coat polystyrene beads. FimA-coated beads were incubated for 30 min with diluted serum (1:100 to 1:500) in blocking buffer (1% bovine serum albumin in PBS). The beads were washed with PBS, and the bound primary antibody was reacted with a fluorescein isothiocyanate-labeled goat anti-rat IgG secondary antibody or the goat anti-rat IgA antibody (Southern Biotechnologies). The bound fluorescence was measured after washing of the beads with PBS containing 0.05% Tween 20, and the serum antibody titers were expressed as relative fluorescent units after subtraction of the background (7).
Due to the variable flow rates encountered during saliva collection, saliva samples were assayed for both total IgA concentration and fimbrillin-specific IgA antibody. The amount of rat IgA in saliva was estimated by utilizing a commercially available rat IgA quantitation kit (Bethyl Laboratories, Montgomery, Tex.). This was carried out by first establishing a rat IgA standard curve on a plate in a capture ELISA format. Briefly, ELISA plates were coated with affinity-purified goat anti-rat IgA antibody. This was followed by incubation with a rat IgA standard or saliva and then goat anti-rat IgA coupled to horseradish peroxidase and subsequent color development with horseradish peroxidase-substrate reagent. The dilution of saliva which fell on the linear portion of the IgA standard curve was used to determine the total IgA in that sample. Specific IgA in saliva directed to P. gingivalis fimbrillin protein was measured on plates coated with the recombinant P. gingivalis protein. Each microtiter plate well was coated with 5 μg of recombinant fimbrillin protein, and the saliva was diluted 1:5 prior to incubation. The concentration of FimA-specific IgA was expressed as the amount of specific IgA per milligram of total IgA in each saliva sample.
(iii) Assessment of protection against P. gingivalis-induced alveolar bone loss.
The efficacy of the FimA-specific antibody response elicited by coimmunization with S. gordonii recombinants against P. gingivalis-induced alveolar bone loss was evaluated in a separate experiment. For this purpose, groups of eight rats were immunized as described above and then challenged at week 6 by oral gavage with P. gingivalis. At the termination of the experiment (6 weeks following the last P. gingivalis injection), the mean alveolar bone levels of the groups were compared. The groups were as follows: group 1, sham immunized and P. gingivalis infected; group 2, control (GP251) immunized (oral) and P. gingivalis infected; group 3, orally coimmunized with vaccine strains (SgFimN and SgFimC2) and P. gingivalis infected.
Statistics.
Differences between groups were analyzed by the Student t test, and a one-way analysis of variance with multiple comparisons among groups was done with Tukey's test using software from InStat (San Diego, Calif.). A P value of less than 0.05 was considered statistically significant.
RESULTS
Colonization of germfree rats by S. gordonii vector.
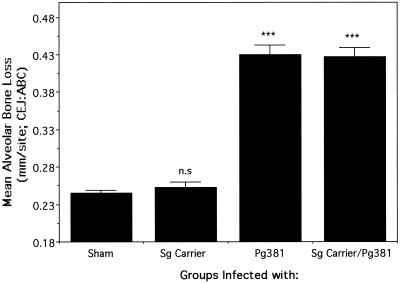
An animal model of P. gingivalis-induced alveolar bone loss utilizing germfree rats has been in use in our laboratory for the past several years (7, 8, 19). In this model, monoinfection with P. gingivalis by oral gavage causes significant reproducible induction of alveolar bone loss. Studies were first carried out to determine (i) if the S. gordonii carrier used to deliver the P. gingivalis FimA antigen would colonize the oral cavities of germfree rats and whether this infection alone would induce alveolar bone loss and (ii) if rats once colonized with S. gordonii would be altered in their ability to support a subsequent infection with P. gingivalis. The results of this study (data not shown) showed that in groups 2 and 4, which were inoculated orally, S. gordonii colonized the oropharyngeal cavity within a week following administration of the initial inoculating dose in 100% of the rats and the colonization continued until the end of the experiment (12 weeks). P. gingivalis was recovered from groups 3 and 4 following infection until the end of the experiment. Moreover, as we have shown previously, monoinfection with P. gingivalis (group 3) reproducibly caused alveolar bone loss (Fig. 2). S. gordonii GP251 colonized germfree rats and did not cause alveolar bone loss. There was no significant difference in alveolar bone loss between the monoinfected (group 3) and dually (S. gordonii and P. gingivalis) infected (group 4) groups of rats. These results demonstrated that S. gordonii was able to successfully colonize rats without causing significant alveolar bone loss and furthermore allowed cocolonization with P. gingivalis. Most importantly, the S. gordonii carrier strain by itself did not cause alveolar bone loss and did not inhibit or enhance P. gingivalis-induced alveolar bone loss when used in combination with P. gingivalis. The germfree-rat model was thus utilized to determine if S. gordonii-delivered P. gingivalis fimbrillin would act as a protective vaccine.
FIG. 2.
Validation of the germfree-rat model of P. gingivalis-induced alveolar bone loss in rats dually infected with P. gingivalis 381 (Pg381) and the S. gordonii carrier strain (Sg Carrier, Pg251). The mean alveolar bone loss (CEJ:ABC) was calculated as the mean difference between the CEJ and the ABC in millimeters per site for each group ± the standard error of the mean (n = 8). Groups infected with P. gingivalis 381 alone (Pg381) or P. gingivalis and the S. gordonii carrier (Sg Carrier/Pg381) showed significant alveolar bone loss compared to groups colonized with the S. gordonii carrier alone (Sg Carrier) or sham infected (***, P < 0.001). Colonization with the S. gordonii carrier did not cause alveolar bone loss (n.s, not significantly different from sham-infected rats).
Kinetics of the FimA-specific immune response by coimmunization with S. gordonii recombinants.
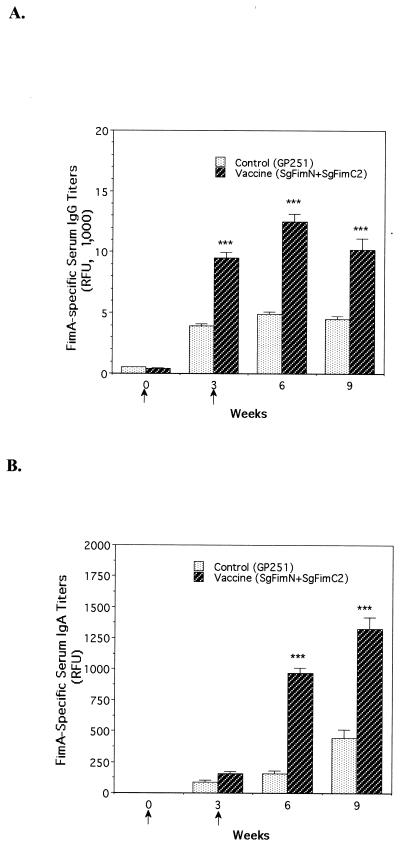
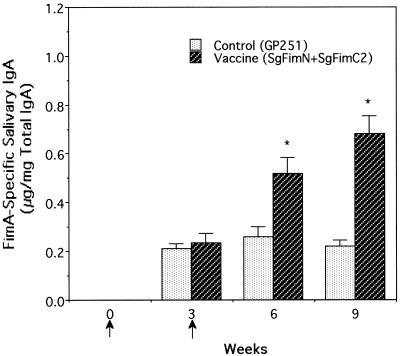
Next, we determined the ability of oral immunization with recombinant S. gordonii surface expressing P. gingivalis fimbrillin to elicit FimA-specific serum and salivary antibodies. Oral coimmunization with two S. gordonii recombinants (SgFimN and SgFimC2) was carried out as described above. Microbiological sampling of the oral cavity showed that S. gordonii recombinants colonized 100% of the immunized animals and continued to express fimbrillin polypeptides during the course of the experiment, as judged by immunoblot analyses of the recovered S. gordonii recombinants (data not shown). The kinetics of the serum and salivary FimA-specific antibodies was monitored for 9 weeks. The results (Fig. 3A) showed a significant increase in the FimA-specific serum IgG titers at week 3 in rats coimmunized with vaccine (SgFimN and SgFimC2) compared to rats colonized with the vector alone (GP251), which was used as a control. The titers reached maximal levels by week 6 and remained elevated by week 9. A similar trend was also observed with FimA-specific serum IgA titers (Fig. 3B). There was also an increase in the FimA-specific salivary IgA antibody at week 6 in the vaccine-immunized rats and a further increase at week 9 (Fig. 4). Thus, coimmunization with the two S. gordonii recombinants (SgFimN and SgFimC2) was able to elicit significant serum and salivary antibody responses specific against P. gingivalis FimA. The vector alone elicited only modest IgG and IgA responses against the FimA antigen at weeks 3, 6, and 9 compared to those of germfree animals (week 0). The explanation for this observation is not known, but it may be due to the presence of one or more cross-reactive epitopes on the surface of the GP251 vector. Although the ELISA-based PCFIA is specific for the FimA protein, possibilities exist for recognition of FimA-cross-reactive epitopes. The cross-reactive FimA antibodies (IgG and IgA) were elevated following control immunization with the vector at weeks 3, 6, and 9 compared to those of germfree animals (week 0).
FIG. 3.
FimA-specific serum IgG (A) and IgA (B) titers following coimmunization with recombinant S. gordonii. Rats were orally inoculated with the live recombinant S. gordoni vaccine strains (SgFimN and SgFimC2) or the control GP251 strain at weeks 0 and 3. Each inoculation consisted of two doses (48 h apart) of 109 CFU of live cells instilled into the oral cavity. Serum and saliva were collected at weeks 3, 6, and 9, and FimA-specific antibody titers in serum were determined by PCFIA. Serum antibody titers (relative fluorescence units [RFU]) are expressed as the mean ± the standard error (n = 6). ∗∗∗, P < 0.001 versus control-immunized group.
FIG. 4.
FimA-specific salivary IgA antibody levels following coimmunization with SgFimN and SgFimC2. The amount of FimA-specific IgA was normalized to the concentration of total IgA and expressed in micrograms of specific IgA per milligram of total IgA. Bars indicate antibody levels (mean ± standard error, n = 6). Significant anti-FimA IgA levels were elicited in animals immunized with vaccine (SgFimN plus SgFimC2) at week 6 and remained elevated at week 9 (*, P < 0.05 versus control).
Assessment of protective immune responses against P. gingivalis-induced alveolar bone loss.
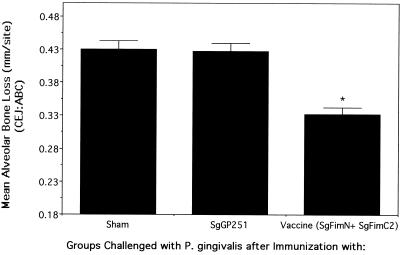
The effectiveness of the immune response elicited by coimmunization with S. gordonii-FimA vaccine in conferring protection against P. gingivalis-induced alveolar bone loss was evaluated next. Rats were orally immunized with S. gordonii-FimA vaccine as in the studies described above and challenged with P. gingivalis by oral gavage at week 6. FimA-specific antibody responses reached significantly elevated levels after coimmunization with the vaccine at that point (Fig. 3 and 4). The results of the protection study showed that animals coimmunized with SgFimN and SgFimC2 were significantly protected from subsequent alveolar bone loss caused by infection with P. gingivalis compared with sham-immunized rats (group 1) or with the control-immunized and P. gingivalis-infected group (group 2) (Fig. 5). An approximately 60% reduction in P. gingivalis-induced alveolar bone loss was caused by this coimmunization strategy (a mean alveolar bone level of 0.24 ± 0.02 mm per site, as in non-P. gingivalis-infected animals [Fig. 2], was taken as 100% reduction). All of the groups tested positive for the presence of cultivable S. gordonii and P. gingivalis throughout the experiment (data not shown).
FIG. 5.
Assessment of protection against P. gingivalis-induced alveolar bone loss in rats by coimmunization with SgFimN and SgFimC2. Results are expressed as the mean difference between the CEJ and the ABC in millimeters per site (average of 14 sites per mandible) for each group ± the standard error of the mean (n = 8). Coimmunization with vaccine strains (SgFimN and SgFimC2) prior to P. gingivalis challenge caused significant protection (*, P < 0.05 versus the control-immunized [SgGP251] or sham-immunized group).
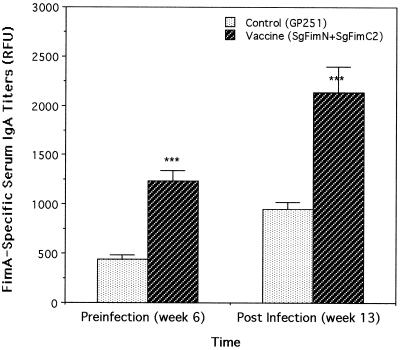
Serum IgA titers against P. gingivalis FimA were found to be significantly elevated at the termination of the experiment (42 days following P. gingivalis infection, a total of 13 weeks) in immunized rats, compared to those of control-immunized and P. gingivalis-infected animals (Fig. 6). However, no significant differences in FimA-specific IgG titers were noted at the end of the experiment (13 weeks) between P. gingivalis-infected groups immunized with the vaccine and control strains (data not shown).
FIG. 6.
Titers of IgA antibody to FimA in serum at termination of the experiment in rats coimmunized with recombinant S. gordonii and infected with P. gingivalis. Animals were immunized at weeks 0 and 3 with recombinant S. gordonii and infected at week 6 with P. gingivalis by oral gavage (three doses given at 48-h intervals at 1012 CFU per dose). Bars indicate antibody titers (mean ± standard error, n = 8) in each group. ***, P < 0.001 versus the control, RFU, relative fluorescence units.
DISCUSSION
The purpose of this study was to assess the potential of immunization with recombinant S. gordonii vectors expressing P. gingivalis fimbrillin (S. gordonii-FimA) epitopes in inducing FimA-specific immune responses protective against P. gingivalis-induced alveolar bone loss in rats. The presentation of an antigen at a specific mucosal site results in a higher-level local antibody response at that site compared to distant locations (11, 12, 23). S. gordonii vectors for delivery of P. gingivalis FimA antigen into the oral cavity offer an attractive strategy for induction of immunity against P. gingivalis infection. The rat model of P. gingivalis-induced alveolar bone loss was utilized to assess the efficacy of S. gordonii vectors delivering FimA vaccine. The results presented here showed that the S. gordonii carrier strain (GP251) used for delivery of the FimA antigen was able to colonize rats and did not cause alveolar bone loss. Further, the amount of alveolar bone loss caused by dual infection with P. gingivalis and the carrier S. gordonii strain was not significantly different from that in rats monoinfected with P. gingivalis alone.
The prototype S. gordonii recombinants (SgFimA) that express biologically important epitopes of P. gingivalis fimbrillin have been described earlier (31–33). An oral coimmunization strategy involving simultaneous immunization with the SgFimN and SgFimC2 recombinants was utilized in the present study. The SgFimN recombinant expresses amino acid residues 55 to 145 of P. gingivalis fimbrillin, and the SgFimC2 recombinant expresses amino acid residues 226 to 337 of P. gingivalis fimbrillin on its surface (31, 32). The domains of the P. gingivalis FimA protein used for expression on the surface of S. gordonii were selected on the basis of their roles in bacterial adherence and in triggering host immune responses (summarized in Fig. 1).
The results presented above show that oral coimmunization with SgFimN and SgFimC2 recombinants elicited FimA-specific serum and salivary antibody responses. FimA-specific serum IgG and IgA responses reached maximim levels at week 6 following coimmunization with vaccine. The salivary IgA response to FimA was significantly elevated at week 6 and continued to increase until week 9. Control (S. gordonii vector alone) immunization of animals, on the other hand led to the induction of FimA-cross-reactive antibodies. The likely presence of one or more epitopes on the surface of S. gordonii that potentially share homology with P. gingivalis FimA is responsible for a level of induction of cross-reactive antibodies that is elevated at weeks 3, 6, and 9 compared to that of germfree animals.
Coimmunization strategies have been used by several investigators to enhance the immunogenicity and efficacy of subunit vaccines (28, 35, 37). These studies have demonstrated the effectiveness of the coimmunization strategy in enhancing the immunogenicity of peptides that lack major T-cell or B-cell epitopes or to which there is genetically regulated unresponsiveness. In a recent study, coimmunization with complementary glucosyltransferase peptides of Streptococcus mutans resulted in enhanced immunogenicity and protection against dental caries (37).
To determine if the induced immune response to FimA was also protective against P. gingivalis-induced alveolar bone loss, rats were challenged at week 6 with P. gingivalis following coimmunization. As mentioned above, both the serum and salivary antibodies against P. gingivalis fimbrillin reached significant levels at this point. At the termination of the experiment (6 weeks following administration of the last P. gingivalis dose), mean alveolar bone levels and FimA-specific antibody levels were determined. The results showed a significant reduction in P. gingivalis-induced alveolar bone loss in vaccine (SgFimN and SgFimC2)-immunized animals compared to that in animals immunized with the carrier strain (GP251) alone. These cross-reactive antibodies to FimA were not protective in vector-immunized animals and were thus likely directed toward nonprotective epitopes of FimA.
The rats coimmunized with SgFimN and SgFimC2 were presented with FimA epitopes (residues 55 to 145 and 226 to 337, respectively) via surface expression on S. gordonii, as well as the native fimbriae during a challenge with P. gingivalis. The control-immunized or sham-immunized rats were presented only with native fimbriae as a result of P. gingivalis infection. Thus, the specific immune response in vaccine-immunized animals was sufficient to confer protection from P. gingivalis-induced alveolar bone loss. In this regard, the presence of FimA-specific serum and salivary antibodies prior to infection could have had an adherence-blocking effect via inhibition of fimbria-mediated binding of the bacterium to oral surfaces. Additionally, the protective effect of the anti-FimA antibody induced in immunized animals may be also due to specific-antibody-mediated neutralization of the functional key P. gingivalis fimbrial epitope(s).
An interesting observation was the fact that although there was no significant difference in the FimA-specific IgG levels in serum between vaccine (SgFimN plus SgFimC2)-immunized and sham-immunized animals at termination (7 weeks following P. gingivalis infection), the level of IgA to FimA in serum was significantly elevated only in the immunized animals. It remains to be determined if the IgA to FimA in serum played any role in mediating protection, perhaps by blocking key FimA epitopes or by anti-inflammatory effects of IgA (30, 38). Monitoring of the kinetics of the anti-FimA response at shorter intervals following a P. gingivalis challenge may be required to detect early differences in serum IgG and salivary IgA to FimA between immunized and sham-immunized groups. As P. gingivalis fimbriae by themselves elicit antibody responses (10), the immune response to FimA reached maximal levels at 7 weeks after P. gingivalis infection. In any event, these data indicate that the P. gingivalis-induced alveolar bone loss was reduced in vaccine-coimmunized animals. Although, the vaccinated animals protected from P. gingivalis-induced alveolar bone loss still showed the presence of P. gingivalis at termination, there exists a possibility that there was a reduction in the number of infecting P. gingivalis bacteria. Further studies enumerating the flora will help explain the differences.
Taken together, the reduction in alveolar bone loss by FimA-specific serum and salivary immune responses by coimmunization may be due to (i) blocking of fimbria-mediated colonization of the oral cavity by the bacterium and/or (ii) blocking of inflammatory cytokine release from host immune cells by P. gingivalis fimbriae, and/or (iii) induction of cell-mediated immunity which confers protection. A recent study has shown that intranasal immunization with P. gingivalis FimA antigen together with cholera toxin induced FimA-specific salivary IgA responses and the FimA-specific IgA monoclonal antibodies generated from submandibular glands of nasally immunized mice inhibited P. gingivalis attachment to and reduced subsequent inflammatory cytokine production from epithelial cells (39). Additionally, IgA has also been shown to possess anti-inflammatory activity (30). In this study, IgA down regulated the release of inflammatory cytokines (tumor necrosis factor alpha and interleukin-6) and induced interleukin-1 receptor antagonist production (38).
The previous studies by Evans et al. (6, 7, 8) have demonstrated the efficacy of parenteral immunization with the FimA protein or its synthetic peptides against P. gingivalis-induced alveolar bone loss in rats. These studies showed that subcutanous immunization with the P. gingivalis fimbrillin protein in the presence of a synthetic adjuvant was able to induce FimA-specific antibodies in serum and saliva. Significantly elevated serum and salivary anti-FimA IgG antibody titers were elicited in immunized and P. gingivalis-infected animals compared to animals that were infected with P. gingivalis alone. FimA-specific IgA levels were not determined in the above-mentioned studies. FimA immunization caused protection from P. gingivalis-induced alveolar bone loss in rats, whereas sham-immunized animals were not protected. The alveolar bone levels in protected animals were comparable to those of noninfected germfree animals, indicating that a nearly 100% reduction in P. gingivalis-induced alveolar bone loss was achieved following FimA immunization.
The approach described in the present study, on the other hand, utilizes oral immunization with FimA antigen delivered via an S. gordonii vector. Oral immunization with an S. gordonii-FimA vaccine resulted in the induction of a significant anti-FimA response in serum (IgG and IgA) and saliva (IgA), and the response peaked around week 6 following immunization. As mentioned above, only FimA-specific serum IgA was found to be elevated in S. gordonii-FimA-immunized and protected animals at termination after P. gingivalis infection and the S. gordonii-FimA-vaccinated animals were significantly protected from P. gingivalis-induced alveolar bone loss. However, unlike those in rats protected by parenteral FimA immunization (7), the alveolar bone levels in S. gordonii-FimA-vaccinated animals (0.33 ± 0.02 mm) did not reach the baseline levels seen in noninfected animals (0.24 ± 0.02 mm). This corresponds to an about 60% reduction caused by S. gordonii vaccine immunization against P. gingivalis-induced alveolar bone loss. We do not know if the difference in efficacy between the two approaches is due to the difference between the titers and/or the nature of the anti-FimA responses elicited by the two approaches. Examination of the protective mechanisms of the immune response against P. gingivalis-induced alveolar bone loss would, however, aid in the design of better intervention strategies.
In summary, this study suggests that the S. gordonii recombinants expressing P. gingivalis fimbrillin could be utilized for development of a mucosal vaccine against P. gingivalis-associated periodontal disease. Moreover, since coimmunization with N- and C-terminal antigenic epitopes of FimA was effective in eliciting a protective immune response against P. gingivalis, development of vectors that express multiple hybrid epitopes of the P. gingivalis FimA protein on the surface of a single S. gordonii vector would be beneficial. This will allow simultaneous delivery of multiple FimA epitopes by a single S. gordonii vector.
ACKNOWLEDGMENTS
We thank Kevin F. Jones of SIGA Research Laboratories for helpful advice during the course of this work and Cornelia Sfintescu for expert technical assistance.
This work was supported in part by U.S. Public Health Service grant DE 12320 and a grant from SIGA Technologies Inc., Corvallis, Oreg.
REFERENCES
- 1.Amano A, Fujiwara T, Nagata H, Kuboniwa M, Sharma A, Sojar H T, Genco R J, Hamada S, Shizukuishi S. Prophyromonas gingivalis fimbriae mediate coaggregation with Streptococcus oralis through specific domains. J Dent Res. 1997;76:852–857. doi: 10.1177/00220345970760040601. [DOI] [PubMed] [Google Scholar]
- 2.Amano A, Sojar H T, Lee J Y, Sharma A, Levine M J, Genco R J. Salivary receptors for recombinant fimbrillin of Porphyromonas gingivalis. Infect Immun. 1994;62:3372–3380. doi: 10.1128/iai.62.8.3372-3380.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deshpande R G, Khan M B, Genco C A. Invasion of aortic and heart endothelial cells by Porphyromonas gingivalis. Infect Immun. 1998;66:5337–5343. doi: 10.1128/iai.66.11.5337-5343.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deslauriers M, Haque S, Flood P M. Identification of murine protective epitopes on the Porphyromonas gingivalis fimbrillin molecule. Infect Immun. 1996;64:434–440. doi: 10.1128/iai.64.2.434-440.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Fabio S, Medaglini D, Rush C M, Corrias F, Panzini G L, Pace M, Verani P, Pozzi G, Titti F. Vaginal immunization of Cynomolgus monkeys with Streptococcus gordonii expressing HIV-1 and HPV 16 antigens. Vaccine. 1998;16:485–492. doi: 10.1016/s0264-410x(97)80002-3. [DOI] [PubMed] [Google Scholar]
- 6.Evans R T, Klausen B, Genco R J. Immunization with fimbrial protein and peptide protects against Porphyromonas gingivalis-induced periodontal tissue destruction. Adv Exp Med Biol. 1992;327:255–262. doi: 10.1007/978-1-4615-3410-5_27. [DOI] [PubMed] [Google Scholar]
- 7.Evans R T, Klausen B, Sojar H T, Bedi G S, Sfintescu C, Ramamurthy N S, Golub L M, Genco R J. Immunization with Porphyromonas (Bacteroides) gingivalis fimbriae protects against periodontal destruction. Infect Immun. 1992;60:2926–2935. doi: 10.1128/iai.60.7.2926-2935.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Evans R T, Klausen B, Sojar H T, Ramamurthy M J, Evans M J, Genco R J. Immunization with Porphyromonas gingivalis fimbriae and a synthetic fimbrial peptide. In: Genco R J, Hamada S, Lehner T, McGhee J R, Mergenhagen S, editors. Molecular pathogenesis of periodontal disease. Washington, D.C.: American Society for Microbiology; 1994. pp. 267–277. [Google Scholar]
- 9.Fischetti V A, Medaglini D, Pozzi G. Gram-positive commensal bacteria for mucosal vaccine delivery. Curr Opin Biotechnol. 1996;7:659–666. doi: 10.1016/s0958-1669(96)80079-6. [DOI] [PubMed] [Google Scholar]
- 10.Genco R J, Sojar H T, Lee J-Y, Sharma A, Bedi G, Cho M C, Dyer D W. Porphyromonas gingivalis fimbriae: structure, function, and insertional inactivation mutants. In: Genco R J, Hamada S, Lehner T, McGhee J, Mergenhagen S, editors. Molecular pathogenesis of periodontal disease. Washington, D.C.: American Society for Microbiology; 1994. pp. 13–23. [Google Scholar]
- 11.Haneberg B, Kendall D, Amerongen H M, Apter F M, Kraehenbuhl J P, Neutra M R. Induction of specific immunoglobulin A in the small intestine, colon-rectum, and vagina measured by a new method for collection of secretions from local mucosal surfaces. Infect Immun. 1994;62:15–23. doi: 10.1128/iai.62.1.15-23.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haneberg B, Kendall D, Amerongen H M, Apter F M, Neutra M R. The colon and rectum as inductor sites for local and distant mucosal immunity. Adv Exp Med Biol. 1995;371A:107–109. doi: 10.1007/978-1-4615-1941-6_19. [DOI] [PubMed] [Google Scholar]
- 13.Lamont R J, Bevan C A, Gil S, Persson R E, Rosan B. Involvement of Porphyromonas gingivalis fimbriae in adherence to Streptococcus gordonii. Oral Microbiol Immunol. 1993;8:272–276. doi: 10.1111/j.1399-302x.1993.tb00573.x. [DOI] [PubMed] [Google Scholar]
- 14.Lamont R J, Chan A, Belton C M, Izutsu K T, Vasel D, Weinberg A. Porphyromonas gingivalis invasion of gingival epithelial cells. Infect Immun. 1995;63:3878–3885. doi: 10.1128/iai.63.10.3878-3885.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lamont R J, Jenkinson H F. Life below the gum line: pathogenic mechanisms of Porphyromonas gingivalis. Microbiol Mol Biol Rev. 1998;62:1244–1263. doi: 10.1128/mmbr.62.4.1244-1263.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee J-Y, Sojar H T, Bedi G S, Genco R J. Synthetic peptides analogous to the fimbrillin sequence inhibit adherence of Porphyromonas gingivalis. Infect Immun. 1992;60:1662–1670. doi: 10.1128/iai.60.4.1662-1670.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee J-Y, Sojar H T, Sharma A, Bedi G S, Genco R J. Active domains of fimbrillin involved in adherence of Porphyromonas gingivalis. J Periodontal Res. 1993;28:470–472. doi: 10.1111/j.1600-0765.1993.tb02105.x. [DOI] [PubMed] [Google Scholar]
- 18.Lee J-Y, Sojar H T, Bedi G S, Genco R J. Porphyromonas (Bacteroides) gingivalis fimbrillin: size, amino-terminal sequence, and antigenic heterogeneity. Infect Immun. 1991;59:383–389. doi: 10.1128/iai.59.1.383-389.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malek R, Fisher J G, Caleca A, Stinson M, van Oss C, Lee J Y, Cho M I, Genco R J, Evans R T, Dyer D W. Inactivation of the Porphyromonas gingivalis fimA gene blocks periodontal damage in gnotobiotic rats. J Bacteriol. 1994;176:1052–1059. doi: 10.1128/jb.176.4.1052-1059.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Medaglini D, Oggioni M R, Pozzi G. Vaginal immunization with recombinant gram-positive bacteria. Am J Reprod Immunol. 1998;39:199–208. doi: 10.1111/j.1600-0897.1998.tb00354.x. [DOI] [PubMed] [Google Scholar]
- 21.Medaglini D, Pozzi G, King T P, Fischetti V A. Mucosal and systemic immune response to a recombinant protein expressed on the surface of the oral commensal bacterium Streptococcus gordonii after oral colonization. Proc Natl Acad Sci USA. 1995;92:6868–6872. doi: 10.1073/pnas.92.15.6868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Medaglini D, Rush C M, Sestini P, Pozzi G. Commensal bacteria as vectors for mucosal vaccines against sexually transmitted diseases: vaginal colonization with recombinant streptococci induces local and systemic antibodies in mice. Vaccine. 1997;15:1330–1337. doi: 10.1016/s0264-410x(97)00026-1. [DOI] [PubMed] [Google Scholar]
- 23.Nedrud J G, Liang X P, Hague N, Lamm M E. Combined oral/nasal immunization protects mice from Sendai virus infection. J Immunol. 1987;139:3484–3492. [PubMed] [Google Scholar]
- 24.Njoroge T, Genco R J, Sojar H T, Hamada N, Genco C A. A role for fimbriae in Porphyromonas gingivalis invasion of oral epithelial cells. Infect Immun. 1997;65:1980–1984. doi: 10.1128/iai.65.5.1980-1984.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ogawa T, Uchida H. A peptide, ALTTE, within the fimbrial subunit protein from Porphyromonas gingivalis, induces production of interleukin 6, gene expression and protein phosphorylation in human peripheral blood mononuclear cells. FEMS Immunol Med Microbiol. 1995;11:197–205. doi: 10.1111/j.1574-695X.1995.tb00117.x. [DOI] [PubMed] [Google Scholar]
- 26.Ogawa T, Uchida H, Hamada S. Porphyromonas gingivalis fimbriae and their synthetic peptides induce proinflammatory cytokines in human peripheral blood monocyte cultures. FEMS Microbiol Lett. 1994;116:237–342. doi: 10.1111/j.1574-6968.1994.tb06707.x. [DOI] [PubMed] [Google Scholar]
- 27.Oggioni M R, Manganelli R, Contorni M, Tommasino M, Pozzi G. Immunization of mice by oral colonization with live recombinant commensal streptococci. Vaccine. 1995;13:775–779. doi: 10.1016/0264-410x(94)00060-z. [DOI] [PubMed] [Google Scholar]
- 28.Partidos C D, Obeid O E, Steward M W. Antibody responses to non-immunogenic synthetic peptides induced by co-immunization with immunogenic peptides. Immunology. 1992;77:262–266. [PMC free article] [PubMed] [Google Scholar]
- 29.Ricci S, Medaglini D, Rush C M, Marcello A, Peppoloni S, Manganelli R, Palú G, Pozzi G. Immunogenicity of the B monomer of Escherichia coli heat-labile toxin expressed on the surface of Streptococcus gordonii. Infect Immun. 2000;68:760–766. doi: 10.1128/iai.68.2.760-766.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Russell M W, Sibley D A, Nikolova E B, Tomana M, Mestecky J. IgA antibody as a non-inflammatory regulator of immunity. Biochem Soc Trans. 1997;25:466–470. doi: 10.1042/bst0250466. [DOI] [PubMed] [Google Scholar]
- 31.Sharma A, Honma K, Sojar H T, Hruby D E, Kuramitsu H K, Genco R J. Expression of saliva-binding epitopes of the Porphyromonas gingivalis FimA protein on the surface of Streptococcus gordonii. Biochem Biophys Res Commun. 1999;258:222–226. doi: 10.1006/bbrc.1999.0616. [DOI] [PubMed] [Google Scholar]
- 32.Sharma A, Nagata H, Hamada N, Sojar H T, Hruby D E, Kuramitsu H K, Genco R J. Expression of functional Porphyromonas gingivalis poypeptide domains on the surface of Streptococcus gordonii. Appl Environ Microbiol. 1996;62:3933–3938. doi: 10.1128/aem.62.11.3933-3938.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sharma A, Sojar H T, Hruby D E, Kuramitsu H K, Genco R J. Secretion of Porphyromonas gingivalis fimbrillin polypeptides by recombinant Streptococcus gordonii. Biochem Biophys Res Commun. 1997;238:313–316. doi: 10.1006/bbrc.1997.7306. [DOI] [PubMed] [Google Scholar]
- 34.Sharma A, Sojar H T, Lee J Y, Genco R J. Expression of a functional Porphyromonas gingivalis fimbrillin polypeptide in Escherichia coli: purification, physicochemical and immunochemical characterization, and binding characteristics. Infect Immun. 1993;61:3570–3573. doi: 10.1128/iai.61.8.3570-3573.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shaw D M, Stanley C M, Partidos C D, Steward M W. Influence of the T-helper epitope on the titre and affinity of antibodies to B-cell epitopes after co-immunization. Mol Immunol. 1993;30:961–968. doi: 10.1016/0161-5890(93)90121-q. [DOI] [PubMed] [Google Scholar]
- 36.Sojar H T, Han Y, Hamada N, Sharma A, Genco R J. Role of the amino-terminal region of Porphyromonas gingivalis fimbriae in adherence to epithelial cells. Infect Immun. 1999;67:6173–6176. doi: 10.1128/iai.67.11.6173-6176.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taubman M A, Smith D J, Holmberg C J, Eastcott J W. Coimmunization with complementary glucosyltransferase peptides results in enhanced immunogenicity and protection against dental caries. Infect Immun. 2000;68:2698–2703. doi: 10.1128/iai.68.5.2698-2703.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wolf H M, Hauber I, Gulle H, Samtag A, Fischer M B, Ahmad R U, Eibl M M. Anti-inflammtory properties of human serum IgA: induction of IL-1 receptor antagonist and FcαR(CD89)-mediated down-regulation of tumor necrosis factor-alpha (TNF-α) and IL-6 in human monocytes. Clin Exp Immunol. 1996;105:537–543. doi: 10.1046/j.1365-2249.1996.d01-793.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yanagita M, Hiroi T, Kitagaki N, Hamada S, Ito H O, Shimauchi H, Murakami S, Okada H, Kiyono H. Nasopharyngeal-associated lymphoreticular tissue (NALT) immunity: fimbriae-specific Th1 and Th2 cell-regulated IgA responses for the inhibition of bacterial attachment to epithelial cells and subsequent inflammatory cytokine production. J Immunol. 1999;162:3559–3565. [PubMed] [Google Scholar]
- 40.Zambon J J, Grossi S, Dunford R, Harazsthy V I, Preus H, Genco R J. Epidemiology of subgingival bacterial pathogens in periodontal diseases. In: Genco R J, Hamada S, Lehrer J R, McGhee J R, Mergenhagen S, editors. Molecular pathogenesis of periodontal disease. Washington, D.C.: American Society for Microbiology; 1994. pp. 3–12. [Google Scholar]