Abstract
Coffee may protect against non-alcoholic fatty liver disease (NAFLD), but the roles of the caffeine and non-caffeine components are unclear. Coffee intake by 156 overweight subjects (87% with Type-2-Diabetes, T2D) was assessed via a questionnaire, with 98 subjects (all T2D) also providing a 24 h urine sample for quantification of coffee metabolites by LC–MS/MS. NAFLD was characterized by the fatty liver index (FLI) and by Fibroscan® assessment of fibrosis. No associations were found between self-reported coffee intake and NAFLD parameters; however, total urine caffeine metabolites, defined as Σcaffeine (caffeine + paraxanthine + theophylline), and adjusted for fat-free body mass, were significantly higher for subjects with no liver fibrosis than for those with fibrosis. Total non-caffeine metabolites, defined as Σncm (trigonelline + caffeic acid + p-coumaric acid), showed a significant negative association with the FLI. Multiple regression analyses for overweight/obese T2D subjects (n = 89) showed that both Σcaffeine and Σncm were negatively associated with the FLI, after adjusting for age, sex, HbA1c, ethanol intake and glomerular filtration rate. The theophylline fraction of Σcaffeine was significantly increased with both fibrosis and the FLI, possibly reflecting elevated CYP2E1 activity—a hallmark of NAFLD worsening. Thus, for overweight/obese T2D patients, higher intake of both caffeine and non-caffeine coffee components is associated with less severe NAFLD. Caffeine metabolites represent novel markers of NAFLD progression.
Keywords: non-alcoholic fatty liver disease, fatty liver index, type 2 diabetes, caffeine, fibrosis
1. Introduction
As a result of societal changes in diet and lifestyle, there has been an increase in obesity rates, with the incidence of non-alcoholic fatty liver disease (NAFLD) rapidly increasing in many Western countries. NAFLD can ultimately progress to severe and irreversible conditions such as cirrhosis and hepatocellular carcinoma, which generate enormous societal and healthcare burdens. Recent observational studies suggest that coffee consumption protects against NAFLD development and progression [1,2].
To date, these studies have relied on either self-reported information via questionnaires or interviews to evaluate coffee consumption. Aside from uncertainties arising from possible bias and/or misclassification in self-reporting, these data do not inform the intake of different coffee components, such as caffeine and polyphenols: this may be important in explaining the relationship between coffee intake and NAFLD, as both caffeine and non-caffeine metabolites may contribute to protection against NAFLD through independent mechanisms. Caffeine intake has been shown to be associated with decreased liver fibrosis in NAFLD and other chronic liver disease settings [3,4,5,6]. This effect may in part be mediated by inhibition of adenosine A2A receptor-mediated induction of collagen production in hepatic stellate cells [4,7,8]. Adenosine A2A and A2B receptor signaling also contribute to regulating β-cell insulin secretion, as well as influencing insulin sensitivity in several tissues, including the liver [9,10], but the effects of caffeine on these parameters in relation to NAFLD are currently not known. In preclinical studies, other coffee components, such as trigonelline, chlorogenic acid and melanoidins have been shown to independently ameliorate NAFLD co-morbidities such as hepatic autophagy, oxidative stress, inflammation and intestinal barrier function [11,12,13,14,15], as well as improving systemic glucose homeostasis in both healthy and overweight subjects [16,17].
To date, almost all studies on the effects of coffee intake on human health have relied on self-reported coffee intake information. Given the inherent limitations and uncertainties of this approach, there have been efforts to obtain more defined and quantitative data on coffee intake, by measuring its major metabolites in urine collected over a 24 h interval [18,19]. With the exception of advanced cirrhosis and/or kidney dysfunction, coffee metabolites are cleared relatively quickly [20]: a 24 h urine sample, timed from before breakfast the preceding day to before breakfast on collection day, captures the majority of coffee metabolites that would be cleared over a typical day. To our knowledge, this approach has not yet been applied to study of the effects of coffee intake on markers of NAFLD severity.
The effective dose of coffee metabolites seen by liver and other tissues not only depends on coffee intake, but also on the individual’s body mass. To date, correction for body mass has not been applied to any coffee intake study. Our study population had a wide range of body mass, with obesity also prevalent. As coffee metabolites are assumed to distribute predominantly in aqueous rather than lipid constituents, the amounts of recovered urinary coffee metabolites for each subject were adjusted for fat-free mass.
2. Materials and Methods
2.1. Materials
Caffeine (1 mg/mL), theobromine (0.1 mg/mL), theophylline (1 mg/mL), paraxanthine (1 mg/mL), 13C3-caffeine (1 mg/mL) stock solutions and theobromine-d6 (98% purity) were purchased from Sigma-Aldrich, St. Louis, MO, USA. Trigonelline, p-coumaric acid and catechin-2,3,4-13C3 in solid state were purchased from Sigma-Aldrich, while trans-caffeic acid was purchased from Fluka. Acetonitrile, methanol and water were LC–MS grade from VWR. Formic acid was LC–MS grade, and was purchased from Amresco.
2.2. Clinical Studies
Ethical permits were obtained from the Ethics Committee of Associação Protetora dos Diabéticos de Portugal (APDP). All subjects were volunteers, and written informed consent was obtained from all participants. The study protocol adhered to the Declaration of Helsinki. Subjects were recruited via the APDP clinic and, after providing informed consent, each subject was instructed to provide a 24 h urine sample, and to record their coffee and food intake over this period. The subjects were also requested to fill out a questionnaire on their customary consumption of beverages and caffeine-rich foods other than coffee, such as chocolate, based on that used by Modi et al. in their study of caffeine intake and liver fibrosis [21]. Within 24 h of finishing the urine collection, the subjects were admitted to the APDP clinic for anthropometric measurements, blood collection and assessment of liver steatosis and fibrosis with Fibroscan®. A subsection of subjects underwent the protocol without urine collection. Exclusion criteria included bowel disease or surgery, kidney disease, alcohol intake of >30 g per day for men and >20 g per day for women, and other chronic liver diseases, such as hepatitis A, B, C and Wilson’s disease.
2.3. Analysis of Urine Coffee Metabolites
Urine caffeine metabolites were analysed by LC–MS/MS, as described [22,23]. A similar protocol was developed for the non-caffeine metabolites. The detailed procedures are described in Appendix A.
2.4. Analysis of Blood Components, Body Composition and Fatty Liver Index
From the collected blood, plasma and serum were obtained. Clinical chemistry analyzers were used to assay glucose, HDL-cholesterol, LDL-cholesterol, total cholesterol, triglycerides, alanine aminotransferase (ALT), aspartate aminotransferase (AST) and γ-glutamyl transferase (GGT) (Beckman Coulter AU480), HbA1c (Menarini Hb 9210 Premier), and insulin (Architect Plus i1000SR), in accordance with standard operating procedures. Body composition, including fat-free body mass, was measured by bioimpedance, using a Body Composition Monitor (OMRON BF511). The fatty liver index (FLI) was calculated from triglyceride and GGT levels and from anthropometric parameters, according to the following formula [24]:
| FLI = (e0.953 × ln (triglycerides) + 0.139 × BMI + 0.718 × ln (GGT) + 0.053 × waist circumference − 15.745)/(1 + e0.953 × ln (triglycerides) + 0.139 × BMI + 0.718 × ln (GGT) + 0.053 × waist circumference − 15.745) × 100 |
Zonulin, a marker for intestinal barrier status [25,26], was measured from thawed serum samples with an ELISA kit (Immunodiagnostik AG, Bensheim, Germany), in accordance with the manufacturer’s instructions.
2.5. Alcohol Intake Measurement
Alcohol intake was calculated in terms of alcohol units per week, where 1 unit = 10 mL of pure ethanol. In the questionnaire information, it was designated that one small beer (200 mL, 5% alcohol) = 1 unit, one medium beer (330 mL, 5% alcohol) = 1.65 units, one large beer (500 mL, 5% alcohol) = 2.5 units, one glass of red or white wine (125 mL, 13% alcohol) = 1.625 units, and one measure of spirits (25 mL, 40% alcohol) = 1 unit.
2.6. Data Analysis and Presentation
Statistical tests and correlation analyses were performed with Microsoft Excel and GraphPad Prism 8.0.1. Statistical significance was defined as a p value ≤ 0.05. Data were presented as means ± standard deviations in tables, and as box and whisker plots in graphs where, for a given data set, the box spanned the second and third quartile boundaries, with the horizontal line representing the median, and the whisker line spanned the maximum and minimum values.
3. Results
3.1. Study Cohort Characteristics
The study cohort was composed of almost equal proportions of overweight middle-aged males and females with high incidence of T2D (Table 1). The lipid profile was atherogenic, with above-normal triglyceride and total cholesterol levels, and with LDL-cholesterol well above the healthy range. The controlled attenuation parameter (CAP) and transient elastography (TE) measured by Fibroscan® were consistent with moderate steatosis and mild fibrosis, respectively. Levels of circulating GGT, ALT and AST were at the upper limits of their normal ranges. The mean FLI score of 60 was at the cut-off value for ruling in NAFLD [24]. Mean alcohol intake was within the current 14 units per week guideline recommended by the NHS [27]. The subgroup of subjects that provided urine samples for determination of 24 h coffee metabolite amounts had identical characteristics, with the exception of T2D.
Table 1.
Population characteristics. Characteristics of the total subject population and the subset of subjects that provided urine for analysis of coffee metabolites. Values are expressed as mean ± standard deviation.
| Parameters | Values | |
|---|---|---|
| Total (n = 156) |
With Urine Data (n = 98) | |
| Age (yr) | 59 ± 9 | 60 ± 6 |
| Sex distribution (F/M) | 76/80 | 52/46 |
| Type 2 Diabetes incidence & duration (yr) | 135/156 (87%), 11 ± 7 | 98/98 (100%), 11 ± 6 |
| Body mass index (BMI, kg·m−2) | 29 ± 5 | 30 ± 4 |
| Aspartate aminotransferase (AST, U·L−1) | 23 ± 6 | 22 ± 4 |
| Alanine aminotransferase (ALT, U·L−1) | 27 ± 12 | 26 ± 7 |
| γ-glutamyltransferase (GGT, U·L−1) | 31 ± 21 | 31 ± 14 |
| Fibrosis (transient elastography, kPa) | 5.7 ± 2.9 | 6.1 ± 2.1 |
| Steatosis (controlled attenuation parameter, dB·m−1) | 283 ± 56 | 290 ± 44 |
| Fatty liver index (FLI) score | 60 ± 26 | 63 ± 20 |
| Total Cholesterol (mg·dL−1) | 180 ± 39 | 178 ± 32 |
| HDL-Cholesterol (mg·dL−1) | 51 ± 11 | 49 ± 9 |
| LDL-Cholesterol (mg·dL−1) | 121 ± 32 | 120 ± 27 |
| Triglyceride (mg·dL−1) | 141 ± 66 | 149 ± 53 |
| Glucose (mg·dL−1) | 145 ± 41 | 153 ± 31 |
| Insulin (µU·mL−1) | 11 ± 10 | 11 ± 7 |
| Zonulin (ng·mL−1) | 46 ± 10 | 48 ± 7 |
| Alcohol intake (alcohol units per week) | 8 ± 14 | 10 ± 16 |
Abbreviations: high-density lipoprotein (HDL); low-density lipoprotein (LDL).
3.2. Urinary Coffee Metabolite Profile
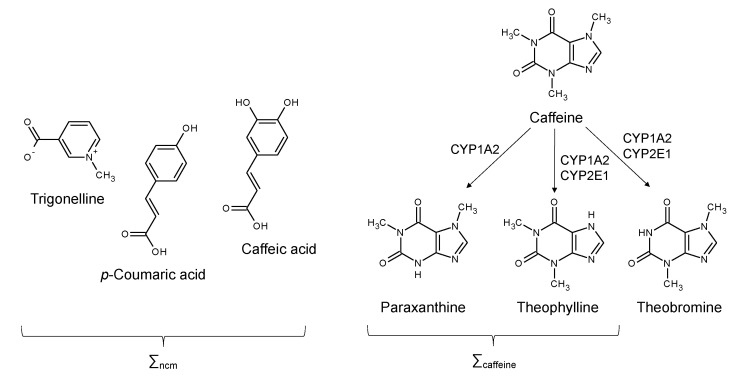
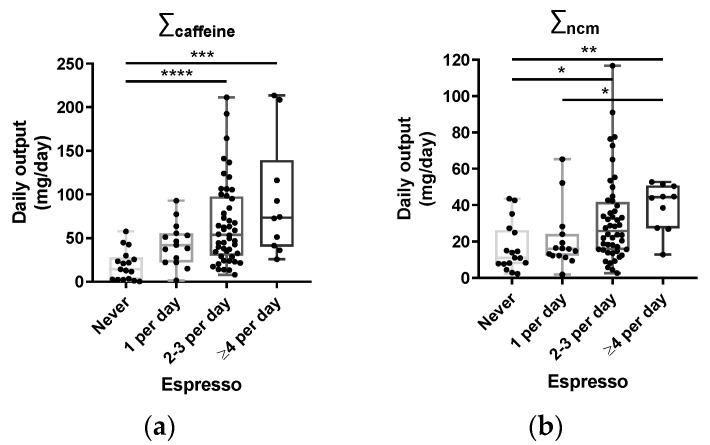
The caffeine component of coffee can be metabolized via cytochrome P450 enzymes to paraxanthine, theophylline and theobromine (Figure 1). Since theobromine is also a constituent of tea and chocolate, it was excluded from the calculation of total caffeine metabolites. The remaining caffeine metabolites were dominated by paraxanthine, accounting for ~90% of the total, with caffeine and theophylline accounting for ~5–10% and ~1–5%, respectively (Table S1). Of the non-caffeine components that were measured, trigonelline accounted for ~95% of the total, with caffeic acid and p-coumaric acid contributing about 4% and 1%, respectively. For both caffeine and non-caffeine metabolites, there was a robust association between their 24 h urine amounts and reported coffee consumption, as shown in Figure 2. Individual metabolites also showed a strong association with reported intake, with the exception of p-coumaric acid (Table S2).
Figure 1.
Caffeine metabolites that were analyzed in the subject urine samples, including caffeine and two of its secondary metabolites—paraxanthine and theophylline (∑caffeine)—and the non-caffeine metab-olites, trigonelline, p-coumaric acid and caffeic acid (∑ncm). Also shown are the cytochrome P450 mixed-function oxidases (CYP1A2 and CYP2E1) that convert caffeine to these secondary metabo-lites.
Figure 2.
Reported coffee consumption associated with 24 h urine amounts of coffee components: (a) relationship between coffee metabolites measured in the 24 h urine samples and reported espresso intake for total caffeine metabolites (∑caffeine); (b) total non-caffeine metabolites (∑ncm). * = significant difference (p ≤ 0.05, Kruskal–Wallis test with Dunn’s multiple comparisons); ** = significant difference (p ≤ 0.01, Kruskal–Wallis test with Dunn’s multiple comparisons); *** = significant difference (p ≤ 0.001, Kruskal–Wallis test with Dunn’s multiple comparisons); **** = significant difference (p ≤ 0.0001, Kruskal–Wallis test with Dunn’s multiple comparisons).
3.3. Coffee Metabolites and NAFLD Severity
To determine if there was a relationship between coffee metabolite output and NAFLD profile for this population, we examined the correlations between total urinary caffeine and non-caffeine metabolite levels, adjusted for fat-free mass, and three parameters associated with NAFLD: the FLI score, and fibrosis and steatosis readouts from Fibroscan® (Table 2). There were no significant correlations of total urinary caffeine metabolites with any of the NAFLD parameters, or with zonulin, a serum marker of intestinal barrier function [28]. The total non-caffeine metabolites showed a significant negative correlation with the FLI but not with any other NAFLD parameters, nor with zonulin. We did not find any significant associations between self-reported coffee consumption, either adjusted or non-adjusted for fat-free mass, and any NAFLD parameter, either for the cohort that provided the 24 h urine samples or for the entire study population (Figure S1).
Table 2.
Non-caffeine metabolites correlated with the FLI. Correlations, expressed as Pearson coefficients, of total urinary coffee metabolites [(caffeine metabolites (Σcaffeine) and non-caffeine metabolites (Σncm)], expressed per kg of fat-free mass, with the fatty liver index (FLI), fibrosis and steatosis parameters measured by Fibroscan®, and with serum zonulin levels. The p value for each Pearson coefficient is shown alongside in parentheses.
| Liver Parameter | Correlation with Σcaffeine |
Correlation with Σncm |
|---|---|---|
| FLI | −0.1783 (p = 0.0789) | −0.2266 * (p = 0.0249) |
| Fibrosis (kPa) | −0.1090 (p = 0.2852) | −0.0646 (p = 0.5271) |
| Steatosis (CAP, db·m−1) | −0.0734 (p = 0.4728) | −0.0860 (p = 0.3996) |
| Zonulin (ng·mL−1) | −0.0804 (p = 0.4510) | 0.06918 (p = 0.5171) |
* = significant difference (p ≤ 0.05, Pearson correlation). Abbreviations: Controlled attenuation parameter (CAP).
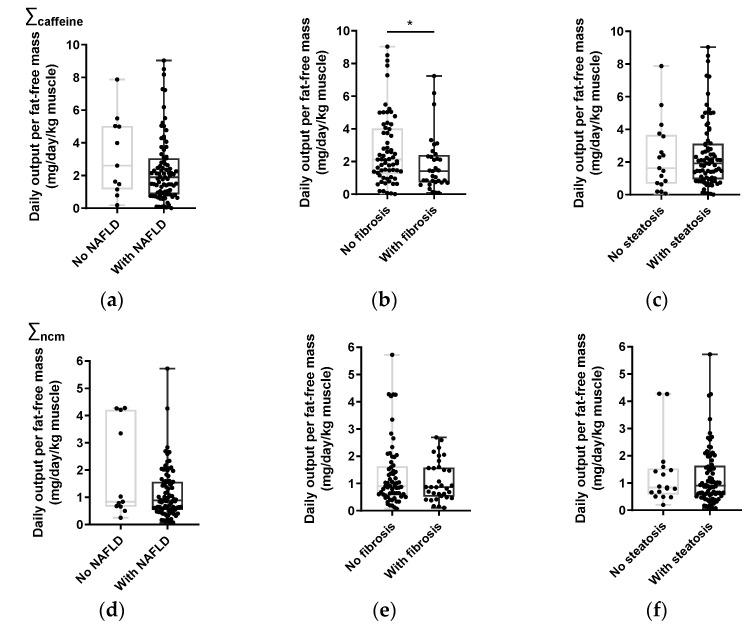
As the FLI, steatosis and fibrosis scores were each categorized according to NAFLD severity, we also examined the relationships between coffee metabolite amounts adjusted for fat-free mass and the different NAFLD categories (Figure 3). There were no significant differences between either total caffeine or total non-caffeine metabolites for subjects with (S1 + S2 + S3) or without (S0) steatosis, or for subjects where NAFLD could be ruled out (FLI < 30) vs. those where NAFLD was probable (FLI ≥ 30). Total caffeine metabolites were significantly higher for subjects with no fibrosis (F0), compared to those with fibrosis (F1–F4). There was no significant difference in total non-caffeine metabolites between these categories. For self-reported coffee intake adjusted for fat-free mass, no significant differences were found between any of the NAFLD categories (Figure S2).
Figure 3.
High total caffeine metabolites are associated with less fibrosis. Levels of total caffeine metabolites (a–c) and total non-caffeine metabolites (d–f), adjusted for fat-free mass with different categories of the fatty liver index (FLI) (a,d), scores of fibrosis (b,e) and steatosis (c,f). * = significant difference (p ≤ 0.05, Mann–Whitney test).
To account for possible confounding factors in the relationship between coffee metabolites and FLI scores, a multiple regression analysis was performed. As the body mass index (BMI) is an important confounder of NAFLD, but is not a variable independent from the FLI (because the BMI is a component of the FLI formula), the subjects were stratified according to normal weight (BMI < 25 kg/m2) and overweight and obese (BMI ≥ 25 kg/m2). For overweight and obese T2D subjects (n = 86), both total caffeine metabolites and total non-caffeine metabolites retained a significant negative correlation with FLI scores after adjusting for age, sex, ethanol intake, glomerular filtration rate (GFR) and glycated hemoglobin (HbA1c)—a marker of T2D severity (Table S3). The same relationships between coffee metabolites and NAFLD parameters were also found when metabolite levels were normalized to total body mass (Table S4).
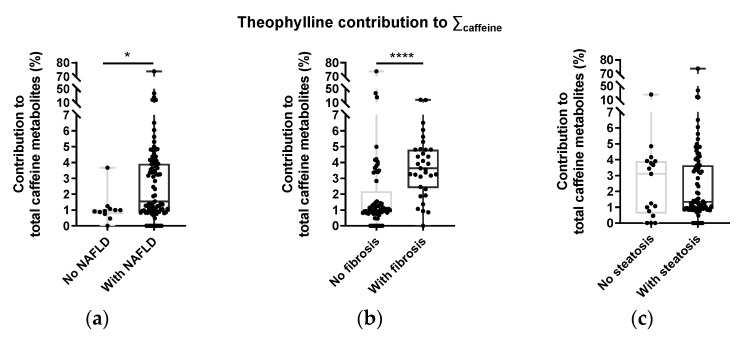
3.4. Caffeine Metabolite Profiles and NAFLD Status
For the measured secondary metabolites of caffeine (paraxanthine and theophylline), there was a significant positive relationship between the fraction of caffeine metabolites accounted for by theophylline and some parameters of NAFLD severity (Figure 4). The theophylline fraction was significantly higher for subjects with either mild or moderate/severe fibrosis, relative to no fibrosis. It was also significantly higher for subjects with FLI scores ruling in vs. FLI scores ruling out NAFLD. The ratio of theophylline to paraxanthine also followed the same pattern (Figure S3). There was no relationship between the proportion of caffeine metabolites and steatosis severity.
Figure 4.
Theophylline was higher in subjects with NAFLD and fibrosis. Theophylline fraction of total caffeine metabolites and categories of the fatty liver index (FLI) (a) and scores of fibrosis (b) and steatosis (c). * = significant difference (p ≤ 0.05, Mann–Whitney test); **** = significant difference (p ≤ 0.0001, Mann–Whitney test).
4. Discussion
4.1. Characterizing Coffee Consumption by 24 h Urine Analysis versus Self-Reporting
To date, most studies on the effects of coffee intake on the status of non-communicable chronic diseases, such as NAFLD and T2D, have relied on self-reported coffee intake; however, within the last few years, there has been an increasing shift to the analysis of coffee metabolites in plasma, serum and urine: this has been facilitated by the development of sensitive and robust LC– and UPLC–MS/MS methods for quantifying coffee metabolites in biofluids such as serum, plasma and cerebrospinal fluid [22,23,29], urine [30,31] and even fingertip sweat [32]. In five out of six measured urinary coffee metabolites (p-coumaric acid being the exception), we found robust and significant Pearson correlations, in the range of 0.29–0.43, with reported coffee intake (Table S2). This is consistent with other studies that looked at the association between self-reported coffee intake data and urinary caffeine metabolites. Vanderlee et al. reported similar Pearson correlations of urinary caffeine, paraxanthine and theophylline concentrations with self-reported coffee intake, for 79 healthy young adults [19], while Petrovic et al. also reported strong associations between self-reported coffee intake and these three metabolites, but not with theobromine [18]. Of the non-caffeine metabolites, trigonelline was found to have a robust correlation with reported coffee intake for a group of 39 healthy subjects [33]. As for the Southern Italian population studied by Anty et al. [34], coffee is habitually drunk as espresso in Portugal. This may have a significant impact on the amount of caffeine and non-caffeine metabolites that are extracted, in comparison to coffee brewed over longer periods with higher volumes of water [35,36].
In previous studies, urinary coffee metabolites were not adjusted for either total body mass or fat-free mass. In the current study, we applied both 24 h urinary coffee metabolite and self-reported coffee intake data, to look for associations between coffee intake and NAFLD parameters in T2D subjects. While coffee metabolites were shown to have modest but significant associations with NAFLD parameters (Figure 3), none were found with self-reported coffee intake data (Figure S1). On this basis, the analysis of urinary coffee metabolites is a more precise and informative approach for studying the effects of coffee intake on NAFLD status, in comparison to questionnaire information.
4.2. Coffee Intake and NAFLD Parameters
To date there have been several studies that have looked at the relationship between self-reported coffee intake and NAFLD status. In a cohort of subjects with NASH, coffee consumption was associated with a reduction in fibrosis risk [3]. Bambha et al. found that coffee consumption was associated with a lower risk of severe fibrosis in NAFLD patients that had preserved insulin sensitivity, but this effect was absent for insulin-resistant NAFLD subjects [37]. Veronese et al. did not find any association between coffee intake and the degree of steatosis in a Southern Italian population [38]. Anty et al. found that regular coffee, but not espresso, was protective against fibrosis in a group of morbidly obese European women [34]. Recent meta-analyses show a consensus that coffee intake protects against fibrosis for subjects with NAFLD [6,39,40,41,42,43], but there is a lack of agreement on whether coffee intake has any effect on NAFLD incidence in the general population, with three of these studies supporting an effect [40,42,43] and the other three concluding that there is no effect [6,39,41]. Our study found a significantly higher level of caffeine metabolites in subjects without fibrosis compared to those with fibrosis (Figure 3), but failed to find significant correlation between coffee metabolites and fibrosis, when studied as a continuous variable (Table 2).
In addition to anthropometric and lipid inputs, the FLI has a liver enzyme (GGT) component. We found that total non-caffeine metabolites were negatively associated with FLI scores (Table 2), and that for overweight/obese T2D subjects, both caffeine and non-caffeine metabolites were associated with better (i.e., lower) FLI scores after adjusting for potential confounders (Table S3). Xiao et al. also found an inverse relationship between coffee intake (including decaffeinated coffee) and circulating liver enzymes [44]. In subjects with liver cirrhosis, increased coffee consumption was related to lower prevalence of elevated aspartate and alanine aminotransferase levels [45].
4.3. Mechanisms by Which Coffee Metabolites May Protect against NAFLD
Coffee metabolites may protect against NAFLD development to more severe states. The risk factors for NAFLD and T2D are highly congruent, and include obesity, hypertriglyceridemia, insulin resistance and inflammation of both liver and adipose tissues [46,47,48]. More recently, intestinal microbiome dysbiosis and compromised intestinal barrier function have been implicated in disrupting hepatic nutrient metabolism via the generation of metabolites such as ethanol [49], through altering bile acid homeostasis [50,51], and by promoting visceral inflammation through the leakage of pro-inflammatory factors, such as endotoxin into the portal circulation [52].
To date, the best characterized direct effect of coffee on liver health is the attenuation of liver fibrosis by caffeine through its actions of antagonizing adenosine A2A and A1 receptors in hepatic stellate cells, thereby interrupting signaling pathways for collagen production [4,8] as well as vasoconstriction and inflammation [53]. The development of fibrosis and inflammation are key factors in the progression of benign NAFLD towards more irreversible and severe states, such as NASH and cirrhosis. Additionally, there are also a number of extra-hepatic actions by both caffeine and non-caffeine metabolites that oppose NAFLD progression. In preclinical models of NAFLD, de-caffeinated coffee was shown to attenuate the loss of intestinal barrier function [12,13], which was associated with a less severe NAFLD phenotype [12]. In our study, the status of intestinal integrity was assessed by measuring the levels of circulating zonulin. Previous studies have shown associations between zonulin and severity of fatty liver disease in overweight subjects [25,28,54], as well as in patients with magnetic resonance and biopsy-characterized NAFLD and NASH [55]. In our study, no association was found between serum zonulin levels and either caffeine or non-caffeine metabolites (Table 2). One possible explanation is that the NAFLD severity of our study cohort was relatively mild, as seen by circulating liver enzyme levels and fibrosis scores (Table 1). Hendy et al. found that amongst their NAFLD cohort, zonulin levels were significantly higher in subjects with NASH, compared to those with simple steatosis, whose values did not significantly differ from those of healthy controls [55]. To the extent that coffee intake associates with circulating zonulin through its effects on intestinal integrity, this might be easier to detect in subjects with more advanced NAFLD, where there is a clear perturbation of serum zonulin levels. In the setting of mild NAFLD, this does not rule out possible associations of coffee metabolites with other parameters of intestinal health, such as microbiome status [56] and gastrointestinal hormone secretion [16].
4.4. Caffeine Metabolite Profiles and CYP2E1
The liver has an array of cytochrome P-450 (CYP) enzymes that metabolize ethanol, eicosanoid fatty acids, and a wide range of xenobiotic compounds, including many drugs and plant-derived natural products [57]. Initially considered to be solely involved in the detoxification of xenobiotic molecules, CYP isoforms may have wider effects on liver metabolism, in part via their oxidation of physiologically active eicosanoids such as prostaglandins [57]. Caffeine is metabolized to paraxanthine via CYP1A2, while its conversion to theophylline or theobromine is mediated not only by this enzyme, but also by CYP2E1. Preclinical studies have shown that CYP2E1 expression is upregulated by chronic alcohol intake and by high fat intake [58,59,60], while biopsy studies have revealed upregulated CYP2E1 expression in livers of NAFLD patients, compared to those of healthy subjects [61]. Not only is increased CYP2E1 expression associated with NAFLD, but it is also implicated in its progression to more severe states, by contributing to increased hepatic oxidative stress [60,62]. Our observation of a significant positive correlation between the fraction of urinary caffeine metabolites represented by theophylline and FLI scores (Figure 4) is consistent with such upregulated CYP2E1 expression, and suggests that this measurement could be a useful non-invasive marker of hepatic CYP2E1 status.
4.5. Study Limitations
Our study has several limitations that need to be taken into consideration. While analysis of coffee metabolites from 24 h urine samples may provide a more informative indication of coffee intake, compared to questionnaire data, it is nevertheless based on intake over a single day. Whether this interval is truly representative of the subject’s habitual coffee intake is not known. Moreover, the urine metabolites that were measured can be derived from foods and beverages other than coffee. Finally, our measurement of NAFLD involved the use of serum markers and ultrasound/elastography, all of which are less precise than liver biopsy and magnetic resonance spectroscopy/imaging modalities in NAFLD diagnosis and staging.
Authors should discuss the results and how they can be interpreted from the perspective of previous studies and of the working hypotheses. The findings and their implications should be discussed in the broadest context possible. Future research directions may also be highlighted.
5. Conclusions
There is a general consensus that coffee intake is associated with modest but significant protection against NAFLD. To date, this has been entirely based on questionnaire data that, among other things, does not provide information on the role of different coffee components in protecting against NAFLD. Our study indicates that higher cumulative amounts of both caffeine and non-caffeine metabolites measured in a 24 h urine collection are associated with a less severe NAFLD profile. Finally, the profile of urine caffeine metabolites is sensitive to NAFLD severity, and may serve as a non-invasive marker of hepatic CYP2E1 expression, an important driver of NAFLD progression.
Acknowledgments
Sociedade Portuguesa de Diabetologia (SPD).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15010004/s1, Table S1: quantities of selected caffeine and non-caffeine metabolites measured from 24 h urine collections; Table S2: correlations, expressed as Pearson coefficients, of individual caffeine and non-caffeine metabolites (total amount recovered in 24 h urine) and reported espresso coffee consumption (cups per day); Table S3: multiple regression analysis for fatty liver index (FLI) and urinary coffee metabolites (total caffeine metabolites, top table, and total non-caffeine metabolites, bottom table) normalized to fat-free mass; Table S4: multiple regression analysis for fatty liver index (FLI) and urinary coffee metabolites (total caffeine metabolites, top table and total non-caffeine metabolites, bottom table), normalized to total body weight; Figure S1: no significant associations were found between self-reported coffee consumption, either adjusted or non-adjusted for fat-free mass, and any NAFLD parameter, either for the cohort that provided the 24 h urine samples or for the entire study population; Figure S2: levels of espresso consumption, adjusted for fat-free mass with different categories of the fatty liver index (FLI) and scores of fibrosis and steatosis obtained by Fibroscan®; Figure S3: ratio of theophylline abundance by paraxanthine with different categories of the fatty liver index (FLI) and scores of fibrosis and steatosis obtained by Fibroscan®.
Appendix A
LC–MS/MS analysis of coffee metabolites in urine: Urine caffeine-derived metabolites and non-caffeine-derived metabolites were analysed on an LC Nexera system (Shimadzu) coupled to a hybrid triple quadrupole/linear ion-trap 4000 QTrap mass spectrometer operated by Analyst 1.6.1 (Sciex). The injector was a CTC-xt (PAL System). The chromatographic separation was performed using the 3 μm Gemini C18 column (50 × 2.0 mm, 110Å, Phenomenex) with a 4 × 2.0 mm C18 guard-column (Phenomenex). The flow rate was set to 250 µL/min, and mobile phases A and B were 0.1% formic acid in water and 0.1% formic acid in acetonitrile, respectively. The LC program for coffee metabolites consisted of 2% of B (0–0.3 min), 2–10% of B (0.3–5.0 min), 10–90% of B (5.0–6.0 min), 90% of B (6.0–7.0 min), 90–2% of B (7.0–7.1 min) and 2% of B (7.1–9.0 min). The LC program for non-caffeine-derived metabolites consisted of 2–30% of B (0–9.0 min), 30–95% of B (9.0–10.0 min), 95% of B (10.0–12.0 min), 95–2% of B (12.0–12.1 min) and 2% of B (12.1–15.0 min). The ionization source (ESI Turbo V) was operated in the positive mode set to an ion spray voltage of 5500 V, 35 psi for nebulizer gas 1 (GS1) for caffeine metabolites and 30 psi for non-caffeine-derived metabolites, 20 psi for the nebulizer gas 2 (GS2), 30 psi for the curtain gas (CUR), and the temperature was 450 °C. All molecules were analysed by multiple reaction monitoring (MRM) setting Q1 and Q3 at unit resolution, the entrance potential (EP) was at 10 eV, and the collision gas (CAD) was at 8 psi. All metabolites had a dwell time of 80 ms, and caffeine metabolites had a cycle time of 1.2751 s, while non-caffeine-derived metabolites had a cycle time of 1.2750 s. The MRM transitions for each compound, and the parameters used, are shown in Table A1. For the preparation of calibration curves, standard solutions and mixtures were prepared in 2% acetonitrile and 0.1% formic acid in H2O, and calibration curves were constructed from these solutions’ dilutions with at least seven calibrants for each analyte. Each calibrant was spiked with 50 µL of the internal standard mixture (8 µM 13C3-catechin and 1.8 µM theobromine-d6 and 13C3-caffeine). After thawing, the urine samples were centrifuged at 4000× g for 5 min at 4 °C. A 100 µL volume of the supernatant was diluted with 400 µL of 2% acetonitrile and 0.1% formic acid in H2O. Samples were further diluted for injection by combining 50 µL of the previous dilution with 50 µL of the internal standard mixture.
Table A1.
Multiple reaction monitoring (MRM) transitions of the data acquisition method for coffee metabolites caffeine, theobromine, theophylline and paraxanthine, the internal standards 13C3-caffeine and theobromine-d6, and the non-caffeine metabolites trigonelline, p-coumaric acid, caffeic acid and the internal standard 13C3-catechin.
| Analyte | Q1 | Q3 | CE | CXP | DP |
|---|---|---|---|---|---|
| Caffeine | 195.2 | 138.0 | 27 | 8 | 71 |
| Paraxanthine | 181.1 | 124.1 | 27 | 10 | 90 |
| Theobromine | 181.1 | 138.1 | 25 | 10 | 66 |
| Theophylline | 181.1 | 124.1 | 27 | 10 | 90 |
| 13C3-Caffeine | 198.2 | 140.2 | 27 | 10 | 61 |
| Theobromine-d6 | 187.3 | 144.2 | 25 | 10 | 91 |
| Trigonelline | 138.1 | 94.3 | 29 | 6 | 86 |
| p-Coumaric acid | 165.2 | 147.3 | 15 | 12 | 61 |
| trans-Caffeic acid | 181.2 | 135.2 | 27 | 8 | 56 |
| 13C3-Catechin | 294.3 | 139.8 | 21 | 24 | 51 |
Abbreviations: Precursor ion m/z selected in the first quadrupole (Q1); fragment ion m/z selected in the third quadrupole (Q3); collision energy (CE); collision cell exit potential (CXP); and declustering potential (DP).
Author Contributions
Conceptualization, R.S.P., I.S.-L., R.T.R., J.F.R., M.P.M. and J.G.J.; Data curation, M.C., R.S.P., R.T.R., M.P.M. and J.G.J.; Formal analysis, M.C., R.S.P., I.S.-L., R.T.R., M.J.M., R.A. and V.M.M.; Investigation, M.C., R.S.P., M.P.M. and J.G.J.; Methodology, R.S.P., I.S.-L., R.T.R., J.F.R., M.P.M. and J.G.J.; Resources, B.M., J.F.R., M.P.M. and J.G.J.; Writing—original draft, M.C., R.S.P., I.S.-L., R.T.R. and J.G.J.; Writing—review and editing, M.C. and J.G.J. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available, due to restrictions presented in the informed consent, related to data storage.
Conflicts of Interest
The authors received funding from the Institute for Scientific Information on Coffee (ISIC), to perform the studies.
Funding Statement
This research was financed by a grant from the Institute for Scientific Information on Coffee (ISIC), by the European Regional Development Fund (ERDF), through the Centro 2020 Regional Operational Programme, the COMPETE 2020-Operational Programme for Competitiveness and Internationalization, and by Portuguese national funds via Fundação para a Ciência e Tecnologia (FCT): UIDB/04539/2020, UIDP/04539/2020, LA/P/0058/2020 and iNOVA4Health (UIDB/Multi/04462/2020). The National Mass Spectrometry Network (RNEM) provided funding under the contract POCI-01-0145-FEDER-402-022125 (ref.: ROTEIRO/0028/2013). M.C. was supported by PhD fellowship PD/BD/135178/2017, co-financed by the European Social Fund (ESF), through the POCH-Programa Operacional do Capital Humano, and national funds via FCT.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Hodge A., Lim S., Goh E., Wong O., Marsh P., Knight V., Sievert W., de Courten B. Coffee intake is associated with a lower liver stiffness in patients with non-alcoholic fatty liver disease, hepatitis C, and hepatitis B. Nutrients. 2017;9:56. doi: 10.3390/nu9010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marventano S., Salomone F., Godos J., Pluchinotta F., Del Rio D., Mistretta A., Grosso G. Coffee and tea consumption in relation with non-alcoholic fatty liver and metabolic syndrome: A systematic review and meta-analysis of observational studies. Clin. Nutr. 2016;35:1269–1281. doi: 10.1016/j.clnu.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 3.Molloy J.W., Calcagno C.J., Williams C.D., Jones F.J., Torres D.M., Harrison S.A. Association of coffee and caffeine consumption with fatty liver disease, nonalcoholic steatohepatitis, and degree of hepatic fibrosis. Hepatology. 2012;55:429–436. doi: 10.1002/hep.24731. [DOI] [PubMed] [Google Scholar]
- 4.Wang Q., Dai X.F., Yang W.Z., Wang H., Zhao H., Yang F., Yang Y., Li J., Lv X.W. Caffeine protects against alcohol-induced liver fibrosis by dampening the cAMP/PKA/CREB pathway in rat hepatic stellate cells. Int. Immunopharmacol. 2015;25:340–352. doi: 10.1016/j.intimp.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Khalaf N., White D., Kanwal F., Ramsey D., Mittal S., Tavakoli-Tabasi S., Kuzniarek J., El-Serag H.B. Coffee and caffeine are associated with decreased risk of advanced hepatic fibrosis among patients with hepatitis C. Clin. Gastroenterol. Hepatol. 2015;13:1521–1531. doi: 10.1016/j.cgh.2015.01.030. [DOI] [PubMed] [Google Scholar]
- 6.Shen H.F., Rodriguez A.C., Shiani A., Lipka S., Shahzad G., Kumar A., Mustacchia P. Association between caffeine consumption and nonalcoholic fatty liver disease: A systemic review and meta-analysis. Ther. Adv. Gastroenterol. 2016;9:113–120. doi: 10.1177/1756283X15593700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan E.S.L., Montesinos M.C., Fernandez P., Desai A., Delano D.L., Yee H., Reiss A.B., Pillinger M.H., Chen J.F., Schwarzschild M.A., et al. Adenosine A(2A) receptors play a role in the pathogenesis of hepatic cirrhosis. Br. J. Pharmacol. 2006;148:1144–1155. doi: 10.1038/sj.bjp.0706812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang H., Guan W.J., Yang W.Z., Wang Q., Zhao H., Yang F., Lv X.W., Li J. Caffeine inhibits the activation of hepatic stellate cells induced by acetaldehyde via adenosine A2A receptor mediated by the cAMP/PKA/SRC/ERK1/2/P38 MAPK signal pathway. PLoS ONE. 2014;9:e92482. doi: 10.1371/journal.pone.0092482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Antonioli L., Blandizzi C., Csoke B., Pacher P., Hasko G. Adenosine signalling in diabetes mellitus-pathophysiology and therapeutic considerations. Nat. Rev. Endocrinol. 2015;11:228–241. doi: 10.1038/nrendo.2015.10. [DOI] [PubMed] [Google Scholar]
- 10.Csoka B., Toro G., Vindeirinho J., Varga Z.V., Koscso B., Nemeth Z.H., Kokai E., Antonioli L., Suleiman M., Marchetti P., et al. A(2A) adenosine receptors control pancreatic dysfunction in high-fat-diet-induced obesity. Faseb J. 2017;31:4985–4997. doi: 10.1096/fj.201700398R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vitaglione P., Morisco F., Mazzone G., Amoruso D.C., Ribecco M.T., Romano A., Fogliano V., Caporaso N., D’Argenio G. Coffee reduces liver damage in a rat model of steatohepatitis: The underlying mechanisms and the role of polyphenols and melanoidins. Hepatology. 2010;52:1652–1661. doi: 10.1002/hep.23902. [DOI] [PubMed] [Google Scholar]
- 12.Brandt A., Nier A., Jin C.J., Baumann A., Jung F., Ribas V., Garcia-Ruiz C., Fernandez-Checa J.C., Bergheim I. Consumption of decaffeinated coffee protects against the development of early non-alcoholic steatohepatitis: Role of intestinal barrier function. Redox Biol. 2019;21:101092. doi: 10.1016/j.redox.2018.101092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mazzone G., Lembo V., D’Argenio G., Vitaglione P., Rossi A., Guarino M., Caporaso N., Morisco F. Decaffeinated coffee consumption induces expression of tight junction proteins in high fat diet fed rats. Funct. Foods Health Dis. 2016;6:602–611. [Google Scholar]
- 14.Shi A.M., Li T., Zheng Y., Song Y.H., Wang H.T., Wang N., Dong L., Shi H.T. Chlorogenic acid improves NAFLD by regulating gut microbiota and GLP-1. Front. Pharmacol. 2021;12:693048. doi: 10.3389/fphar.2021.693048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma L., Lone N.A., Knott R.M., Hassan A., Abdullah T. Trigonelline prevents high cholesterol and high fat diet induced hepatic lipid accumulation and lipo-toxicity in C57BL/6J mice, via restoration of hepatic autophagy. Food Chem. Toxicol. 2018;121:283–296. doi: 10.1016/j.fct.2018.09.011. [DOI] [PubMed] [Google Scholar]
- 16.Johnston K.L., Clifford M.N., Morgan L.M. Coffee acutely modifies gastrointestinal hormone secretion and glucose tolerance in humans: Glycemic effects of chlorogenic acid and caffeine. Am. J. Clin. Nutr. 2003;78:728–733. doi: 10.1093/ajcn/78.4.728. [DOI] [PubMed] [Google Scholar]
- 17.van Dijk A.E., Olthof M.R., Meeuse J.C., Seebus E., Heine R.J., van Dam R.M. Acute effects of decaffeinated coffee and the major coffee components chlorogenic acid and trigonelline on glucose tolerance. Diabetes Care. 2009;32:1023–1025. doi: 10.2337/dc09-0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Petrovic D., Younes S.E., Pruijm M., Ponte B., Ackermann D., Ehret G., Ansermot N., Mohaupt M., Paccaud F., Vogt B., et al. Relation of 24-hour urinary caffeine and caffeine metabolite excretions with self-reported consumption of coffee and other caffeinated beverages in the general population. Nutr. Metab. 2016;13:81. doi: 10.1186/s12986-016-0144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vanderlee L., Reid J.L., White C.M., Acton R.B., Kirkpatrick S.I., Pao C.L., Rybak M.E., Hammond D. Evaluation of a 24-hour caffeine intake assessment compared with urinary biomarkers of caffeine intake among young adults in Canada. J. Acad. Nutr. Diet. 2018;118:2245–2253.E1. doi: 10.1016/j.jand.2018.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martinez-Lopez S., Sarria B., Baeza G., Mateos R., Bravo-Clemente L. Pharmacokinetics of caffeine and its metabolites in plasma and urine after consuming a soluble green/roasted coffee blend by healthy subjects. Food Res. Int. 2014;64:125–133. doi: 10.1016/j.foodres.2014.05.043. [DOI] [PubMed] [Google Scholar]
- 21.Modi A.A., Feld J.J., Park Y., Kleiner D.E., Everhart J.E., Liang T.J., Hoofnagle J.H. Increased caffeine consumption is associated with reduced hepatic fibrosis. Hepatology. 2010;51:201–209. doi: 10.1002/hep.23279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mendes V.M., Coelho M., Tome A.R., Cunha R.A., Manadas B. Validation of an LC-MS/MS method for the quantification of caffeine and theobromine using non-matched matrix calibration curve. Molecules. 2019;24:2863. doi: 10.3390/molecules24162863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Travassos M., Santana I., Baldeiras I., Tsolaki M., Gkatzima O., Genc S., Yener G.G., Simonsen A., Hasselbalch S.G., Kapaki E., et al. Does caffeine consumption modify cerebrospinal fluid amyloid-beta levels in patients with alzheimer’s disease? J. Alzheimers Dis. 2015;47:1069–1078. doi: 10.3233/JAD-150374. [DOI] [PubMed] [Google Scholar]
- 24.Bedogni G., Bellentani S., Miglioli L., Masutti F., Passalacqua M., Castiglione A., Tiribelli C. The Fatty Liver Index: A simple and accurate predictor of hepatic steatosis in the general population. Bmc Gastroenterol. 2006;6:33. doi: 10.1186/1471-230X-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pacifico L., Bonci E., Marandola L., Romaggioli S., Bascetta S., Chiesa C. Increased circulating zonulin in children with biopsy-proven nonalcoholic fatty liver disease. World J. Gastroenterol. 2014;20:17107–17114. doi: 10.3748/wjg.v20.i45.17107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang D., Zhang L., Zheng Y., Yue F., Russell R.D., Zeng Y. Circulating zonulin levels in newly diagnosed Chinese type 2 diabetes patients. Diabetes Res. Clin. Pract. 2014;106:312–318. doi: 10.1016/j.diabres.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 27.Wood A.M., Kaptoge S., Butterworth A.S., Willeit P., Warnakula S., Bolton T., Paige E., Paul D.S., Sweeting M., Burgess S., et al. Risk thresholds for alcohol consumption: Combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. 2018;391:1513–1523. doi: 10.1016/S0140-6736(18)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim J.H., Heo J.S., Baek K.S., Kim S.Y., Baek K.H., Kim K.E., Sheen Y.H. Zonulin level, a marker of intestinal permeability, is increased in association with liver enzymes in young adolescents. Clin. Chim. Acta. 2018;481:218–224. doi: 10.1016/j.cca.2018.03.005. [DOI] [PubMed] [Google Scholar]
- 29.Renouf M., Guy P.A., Marmet C., Fraering A.L., Longet K., Moulin J., Enslen M., Barron D., Dionisi F., Cavin C., et al. Measurement of caffeic and ferulic acid equivalents in plasma after coffee consumption: Small intestine and colon are key sites for coffee metabolism. Mol. Nutr. Food Res. 2010;54:760–766. doi: 10.1002/mnfr.200900056. [DOI] [PubMed] [Google Scholar]
- 30.Rybak M.E., Pao C.I., Pfeiffer C.M. Determination of urine caffeine and its metabolites by use of high-performance liquid chromatography-tandem mass spectrometry: Estimating dietary caffeine exposure and metabolic phenotyping in population studies. Anal. Bioanal. Chem. 2014;406:771–784. doi: 10.1007/s00216-013-7506-9. [DOI] [PubMed] [Google Scholar]
- 31.Lang R., Yagar E.F., Eggers R., Hofmann T. Quantitative investigation of trigonelline, nicotinic acid, and nicotinamide in foods, urine, and plasma by means of LC-MS/MS and stable isotope dilution analysis. J. Agric. Food Chem. 2008;56:11114–11121. doi: 10.1021/jf802838s. [DOI] [PubMed] [Google Scholar]
- 32.Brunmair J., Niederstaetter L., Neuditschko B., Bileck A., Slany A., Janker L., Feuerstein M.L., Langbauer C., Gotsmy M., Zanghellini J., et al. Finger sweat analysis enables short interval metabolic biomonitoring in humans. Nat. Commun. 2021;12:5993. doi: 10.1038/s41467-021-26245-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rothwell J.A., Fillatre Y., Martin J.F., Lyan B., Pujos-Guillot E., Fezeu L., Hercberg S., Comte B., Galan P., Touvier M., et al. New biomarkers of coffee consumption identified by the non-targeted metabolomic profiling of cohort study subjects. PLoS ONE. 2014;9:e93474. doi: 10.1371/journal.pone.0093474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anty R., Marjoux S., Iannelli A., Patouraux S., Schneck A.S., Bonnafous S., Gire C., Amzolini A., Ben-Amor I., Saint-Paul M.C., et al. Regular coffee but not espresso drinking is protective against fibrosis in a cohort mainly composed of morbidly obese European women with NAFLD undergoing bariatric surgery. J. Hepatol. 2012;57:1090–1096. doi: 10.1016/j.jhep.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 35.Olechno E., Puscion-Jakubik A., Zujko M.E., Socha K. Influence of various factors on caffeine content in coffee brews. Foods. 2021;10:1208. doi: 10.3390/foods10061208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bell L.N., Wetzel C.R., Grand A.N. Caffeine content in coffee as influenced by grinding and brewing techniques. Food Res. Int. 1996;29:785–789. doi: 10.1016/S0963-9969(97)00002-1. [DOI] [Google Scholar]
- 37.Bambha K., Wilson L.A., Unalp A., Loomba R., Neuschwander-Tetri B.A., Brunt E.M., Bass N.M., Nonalcoholic S. Coffee consumption in NAFLD patients with lower insulin resistance is associated with lower risk of severe fibrosis. Liver Int. 2014;34:1250–1258. doi: 10.1111/liv.12379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Veronese N., Notarnicola M., Cisternino A.M., Reddavide R., Inguaggiato R., Guerra V., Rotolo O., Zinzi I., Leandro G., Correale M., et al. Coffee intake and liver steatosis: A population study in a mediterranean area. Nutrients. 2018;10:89. doi: 10.3390/nu10010089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kositamongkol C., Kanchanasurakit S., Auttamalang C., Inchai N., Kabkaew T., Kitpark S., Chaiyakunapruk N., Duangjai A., Saokaew S., Phisalprapa P. Coffee consumption and non-alcoholic fatty liver disease: An umbrella review and a systematic review and meta-analysis. Front. Pharmacol. 2021;12:786596. doi: 10.3389/fphar.2021.786596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hayat U., Siddiqui A.A., Okut H., Afroz S., Tasleem S., Haris A. The effect of coffee consumption on the non-alcoholic fatty liver disease and liver fibrosis: A meta-analysis of 11 epidemiological studies. Ann. Hepatol. 2021;20:100254. doi: 10.1016/j.aohep.2020.08.071. [DOI] [PubMed] [Google Scholar]
- 41.Ebadi M., Ip S., Bhanji R.A., Montano-Loza A.J. Effect of coffee consumption on non-alcoholic fatty liver disease incidence, prevalence and risk of significant liver fibrosis: Systematic review with meta-analysis of observational studies. Nutrients. 2021;13:3042. doi: 10.3390/nu13093042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen Y.P., Lu F.B., Hu Y.B., Xu L.M., Zheng M.H., Hu E.D. A systematic review and a dose-response meta-analysis of coffee dose and nonalcoholic fatty liver disease. Clin. Nutr. 2019;38:2552–2557. doi: 10.1016/j.clnu.2018.11.030. [DOI] [PubMed] [Google Scholar]
- 43.Wijarnpreecha K., Thongprayoon C., Ungprasert P. Coffee consumption and risk of nonalcoholic fatty liver disease: A systematic review and meta-analysis. Eur. J. Gastroenterol. Hepatol. 2017;29:E8–E12. doi: 10.1097/MEG.0000000000000776. [DOI] [PubMed] [Google Scholar]
- 44.Xiao Q., Sinha R., Graubard B.I., Freedman N.D. Inverse associations of total and decaffeinated coffee with liver enzyme levels in national health and nutrition examination survey 1999–2010. Hepatology. 2014;60:2091–2098. doi: 10.1002/hep.27367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Klatsky A.L., Morton C., Udaltsova N., Friedman G.D. Coffee, cirrhosis, and transaminase enzymes. Arch. Intern. Med. 2006;166:1190–1195. doi: 10.1001/archinte.166.11.1190. [DOI] [PubMed] [Google Scholar]
- 46.Saponaro C., Gaggini M., Gastaldelli A. Nonalcoholic fatty liver disease and type 2 diabetes: Common pathophysiologic mechanisms. Curr. Diabetes Rep. 2015;15:34. doi: 10.1007/s11892-015-0607-4. [DOI] [PubMed] [Google Scholar]
- 47.Luukkonen P.K., Qadri S., Ahlholm N., Porthan K., Mannisto V., Sammalkorpi H., Penttila A.K., Hakkarainen A., Lehtimaki T.E., Gaggini M., et al. Distinct contributions of metabolic dysfunction and genetic risk factors in the pathogenesis of non-alcoholic fatty liver disease. J. Hepatol. 2022;76:526–535. doi: 10.1016/j.jhep.2021.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Trico D., Caprio S., Umano G.R., Pierpont B., Nouws J., Galderisi A., Kim G., Mata M.M., Santoro N. Metabolic features of nonalcoholic fatty liver (NAFL) in obese adolescents: Findings from a multiethnic cohort. Hepatology. 2018;68:1376–1390. doi: 10.1002/hep.30035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhu L., Baker S.S., Gill C., Liu W., Alkhouri R., Baker R.D., Gill S.R. Characterization of gut microbiomes in nonalcoholic steatohepatitis (NASH) patients: A connection between endogenous alcohol and NASH. Hepatology. 2013;57:601–609. doi: 10.1002/hep.26093. [DOI] [PubMed] [Google Scholar]
- 50.Yang Q., Vijayakumar A., Kahn B.B. Metabolites as regulators of insulin sensitivity and metabolism. Nat. Rev. Mol. Cell Biol. 2018;19:654–672. doi: 10.1038/s41580-018-0044-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mouzaki M., Wang A.Y., Bandsma R., Comelli E.M., Arendt B.M., Zhang L., Fung S., Fischer S.E., McGilvray I.G., Allard J.P. Bile acids and dysbiosis in non-alcoholic fatty liver disease. PLoS ONE. 2016;11:e0151829. doi: 10.1371/journal.pone.0151829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Delzenne N.M., Neyrinck A.M., Baeckhed F., Cani P.D. Targeting gut microbiota in obesity: Effects of prebiotics and probiotics. Nat. Rev. Endocrinol. 2011;7:639–646. doi: 10.1038/nrendo.2011.126. [DOI] [PubMed] [Google Scholar]
- 53.Hsu S.J., Lee F.Y., Wang S.S., Hsin I.F., Lin T.Y., Huang H.C., Chang C.C., Chuang C.L., Ho H.L., Lin H.C., et al. Caffeine ameliorates hemodynamic derangements and portosystemic collaterals in cirrhotic rats. Hepatology. 2015;61:1672–1684. doi: 10.1002/hep.27679. [DOI] [PubMed] [Google Scholar]
- 54.Kim A.S., Ko H.J. Plasma concentrations of zonulin are elevated in obese men with fatty liver disease. Diabetes Metab. Syndr. Obes.-Targets Ther. 2018;11:149–157. doi: 10.2147/DMSO.S163062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hendy O.M., Elsabaawy M.M., Aref M.M., Khalaf F.M., Oda A.M.A., El Shazly H.M. Evaluation of circulating zonulin as a potential marker in the pathogenesis of nonalcoholic fatty liver disease. Apmis. 2017;125:607–613. doi: 10.1111/apm.12696. [DOI] [PubMed] [Google Scholar]
- 56.Mills C.E., Tzounis X., Oruna-Concha M.J., Mottram D.S., Gibson G.R., Spencer J.P.E. In vitro colonic metabolism of coffee and chlorogenic acid results in selective changes in human faecal microbiota growth. Br. J. Nutr. 2015;113:1220–1227. doi: 10.1017/S0007114514003948. [DOI] [PubMed] [Google Scholar]
- 57.Nebert D.W., Wikvall K., Miller W.L. Human cytochromes P450 in health and disease. Philos Trans R Soc Lond B Biol Sci. 2013;368:20120431. doi: 10.1098/rstb.2012.0431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Massart J., Begriche K., Hartman J.H., Fromenty B. Role of mitochondrial cytochrome P450 2E1 in healthy and diseased liver. Cells. 2022;11:288. doi: 10.3390/cells11020288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lieber C.S., Leo M.A., Mak K.M., Xu Y.Q., Cao Q., Ren C.L., Ponomarenko A., DeCarli L.M. Model of nonalcoholic steatohepatitis. Am. J. Clin. Nutr. 2004;79:502–509. doi: 10.1093/ajcn/79.3.502. [DOI] [PubMed] [Google Scholar]
- 60.Abdelmegeed M.A., Banerjee A., Yoo S.H., Jang S., Gonzalez F.J., Song B.J. Critical role of cytochrome P450 2E1 (CYP2E1) in the development of high fat-induced non-alcoholic steatohepatitis. J. Hepatol. 2012;57:860–866. doi: 10.1016/j.jhep.2012.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ma H.L., Chen S.D., Zheng K.I., Yu Y., Wang X.X., Tang L.J., Li G., Rios R.S., Huang O.Y., Zheng X.Y., et al. TA allele of rs2070673 in the CYP2E1 gene is associated with lobular inflammation and nonalcoholic steatohepatitis in patients with biopsy-proven nonalcoholic fatty liver disease. J. Gastroenterol. Hepatol. 2021;36:2925–2934. doi: 10.1111/jgh.15554. [DOI] [PubMed] [Google Scholar]
- 62.Leung T.M., Nieto N. CYP2E1 and oxidant stress in alcoholic and non-alcoholic fatty liver disease. J. Hepatol. 2013;58:395–398. doi: 10.1016/j.jhep.2012.08.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available, due to restrictions presented in the informed consent, related to data storage.