Abstract
Background
COVID-19 vaccination is the latest preventive intervention strategy in an attempt to control the global pandemic. Its efficacy has come under scrutiny because of break through infections among the vaccinated and need for booster doses. Besides, although health workers were prioritized for COVID-19 vaccine in most countries, anecdotal evidence points to high levels of reluctance to take the vaccine among health workers. We assessed COVID-19 vaccine hesitancy among health workers in Dokolo district, northern Uganda.
Methods
This was a mixed-method, cross-sectional descriptive study. A customised self-administered data collection tool was used to collect quantitative data on characteristics, vaccination status and factors for or rejection of vaccine uptake. We conducted multivariable logistic regression to assess the association between selected exposures and vaccine hesitancy using Stata version 15. Conversely, qualitative data were collected using key informant interviews (KIIs) among 15 participants that were purposively selected. Data were analysed using thematic content analysis with the help of NVivo 12.0.
Results
Of the 346 health workers enrolled, (13.3% [46/346]) were vaccine hesitant. Factors associated with vaccine hesitancy included fear of side effects (Adjusted Odds Ratio [AOR]: 2.55; 95% Confidence Interval [95%CI]: 1.00, 6.49) and health workers’ lack of trust in the information provided by health authorities (AOR: 6.74; 95% CI: 2.43, 18.72). Similar factors were associated with vaccine hesitancy when we used the vaccine hesitancy score. Fear of side effects, distrust in vaccine stakeholders, and lack of trust in the vaccine were barriers to COVID-19 vaccination among health workers.
Conclusion
A small proportion of health workers were found to be hesitant to take the COVID-19 vaccine in this study. The paucity of COVID-19 vaccine safety information, which eroded the health workers’ trust in the information they received on the vaccine, was responsible for health workers hesitancy to take up the vaccine in Uganda.
Keywords: COVID-19, Vaccine hesitancy, Health workers, SARS-CoV-2, Unwillingness, Uganda
1. Introduction
Uganda recorded its first COVID-19 case on March 22nd, 2020, 11 days after the World Health Organization declared COVID-19 a global pandemic, and since then, the cases of COVID-19 have peaked with seasonal variations that correspond with infection waves [1]. The Government of Uganda instituted stringent measures to contain the COVID-19 spread at the population level by applying the longest country wide lockdown in the world [2]. These measures included restricting public transport and other movements, instituting prohibition of social gathering, closedown all institutions of learning, wearing of masks and social distancing among others [3]. However, the safety and effectiveness of these measures remain doubtful as the infection continued unabated [4].
With the development of the COVID-19 vaccines, the WHO recommended COVID-19 vaccination under emergency use regulation, initially as a novel measure to mitigate the COVID-19 pandemic. Earlier studies had indicated that vaccination significantly lowered the burden of COVID-19, with lower infection rates recorded in vaccinated populations [5]. However, latter published data that show breakthrough infections among vaccinated also indicated that COVID-19 variably responded to available vaccines [6], even in communities with high acceptance and uptake [7] Pharmaceutical companies are working around to improve on the safety and efficacy of COVID-19 vaccines with inclusion of components that target as many variants of public concern as possible [8], [9]. The evaluation of uptake or acceptance of vaccines need to be done for the current vaccines and this may inform future vaccine responses [10].
Anecdotal and emerging studies suggest high rates of COVID-19 vaccine hesitancy even among at-risk groups [10], [11], [12], [13]. For instance, a study in Uganda by Kanyike et al 2021 revealed 30.7% prevalence of vaccine hesitancy among medical students in Uganda [14]. Data on COVID-19 vaccine hesitancy among health workers in Uganda is still lacking and the picture is not complete. In this study, we assessed COVID-19 vaccine hesitancy among health workers in Dokolo district so as to inform the implementation of COVID-19 health promotional programs in the district and similar settings.
2. Methods
2.1. Study design
This study was a mixed-methods sequential explanatory design, consisting of two distinct phases: a quantitative phase, followed by a qualitative phase. Quantitative data on vaccine uptake and vaccine hesitancy were collected first followed by qualitative data collection.
2.2. Study setting
The study was conducted in Dokolo district in Northern Uganda. Dokolo district has a total population of 215,500 with 109,300 males and 106,200 females [15]. It has 1 (health sub-district) HSD of Dokolo, 2 constituencies of Dokolo North and Dokolo South, 17 public health facilities (1 HCIV, 7 HC IIIs, and 9 HCIIs), 102 private health facilities (PFP & PNFP). At the time of the study, there were 350 health workers in public and private health facilities; 14 administrative units (4 Town councils and 10 sub-counties); 69 parishes and 484 villages. The principal investigator was a member of the district health team and the focal person for COVID-19 surveillance in Dokolo district thus had access to all the health workers in the district.
In this study we used the Theoretical Domains Framework (TDF). The TDF includes 14 domains to explain how individuals’, communities’, or populations’ decisions are shaped by past and present experiences, resources, and restrictions. These domains are categorized into three constructs: capability (knowledge, skills, behavior regulation, memory and attention, decision-making), opportunity (environmental context and resources, social influences), and motivation (goals, social/professional role/identity, beliefs about capabilities, beliefs about consequences, optimism, reinforcement, emotions)[16]. These factors are hypothesized to directly affect vaccine hesitancy. The framework was adopted from Crawshaw et al 2021[17].
2.3. Quantitative component
2.3.1. Study population
All registered and practicing health workers in Dokolo district from both government and private health facilities were eligible for this study. We excluded those who were too sick to communicate and those unwilling to participate.
2.3.2. Sample size
We recruited 346 out of the 350 registered health workers in Dokolo district. This represented 98.9% of the study population and was deemed adequate.
2.3.3. Variables
The outcome variable was vaccine hesitancy, which was defined as unwillingness of a health worker to take a COVID-19 vaccine. According to the World Health Organization, a health worker is a person who provides preventive, curative, rehabilitative and promotional health services based on an extensive body of theoretical and factual knowledge in diagnosis and treatment of disease and other health problems. As a form of sensitivity analysis, we constructed a vaccine hesitancy index by conducting principal component analysis of five related variables (unwillingness to receive COVID-19 vaccine, never been vaccinated with any vaccine, ever refused any vaccination, no intention to get COVID-19 vaccine, and unlikeliness to get COVID-19 vaccine). We used the first principal component as an index of vaccine hesitancy. We defined vaccine hesitancy as a vaccine hesitancy score greater than two standard deviations above the mean vaccine hesitancy score.
The independent variables included socio-demographic characteristics, history of comorbidities, vaccination history; previous history of allergies to vaccination, fear of side effects, confidence and trust in the capacity of the health services and information provided by the health authorities and perceived risk of getting COVID-19. Using principal component analysis, we generated a variable called wealth tertiles to measure the participants’ socio-economic status from an asset-based index. The following assets were considered: television, mobile phone, motorcycle, car, cooker, washing machine, refrigerator, computer, and piped water.
2.3.4. Data analysis
We summarized categorical variables as proportions while continuous variables as mean (standard deviation). We determined the proportion of health workers who were vaccine hesitant (defined as unwillingness to take a COVID-19 vaccine). We conducted multivariable logistic regression to determine the factors associated with vaccine hesitancy among health workers. Factors known to be associated with vaccine hesitancy from the literature and factors from the bi-variable analysis with a p-value<0.25 were included in the multivariable analysis. Data were analyzed using Stata V.15.0. (StataCorp LLC, College Station, Texas, United States of America).
2.3.5. Sensitivity analyses
To check whether an individual’s unwillingness to get the COVID-19 vaccine was a good proxy for assessing vaccine hesitancy, we collected variables similar to unwillingness (never been vaccinated with any vaccine, ever refused any vaccination, no intention to get COVID-19 vaccine, and unlikeliness to get COVID-19 vaccine). We then conducted a principal component analysis with these variables (unwillingness to receive COVID-19 vaccine, ever been vaccinated with any vaccine, ever refused any vaccination, intention to get COVID-19 vaccine, and unlikeliness to get COVID-19 vaccine (reverse coded)) and used the first principal component as an index of vaccine hesitancy. This was because the first component correlated with the variables unwillingness to get COVID-19 vaccine, intention to get COVID-19 vaccine, and unlikeliness to get COVID-19 vaccine (reverse coded)). We considered vaccine hesitancy, as a vaccine hesitancy score>2 standard deviation above the mean. We then conducted logistic regression analysis of the vaccine hesitancy score with all covariates and obtained similar results to the initial analysis (i.e. analysis that defined vaccine hesitancy with only the unwillingness to get COVID-19 vaccine variable).
2.4. Qualitative component
2.4.1. Study population
We interviewed members of the district health team (DHT) and immunization focal persons at the COVID-19 vaccination sites for the qualitative component.
2.4.2. Participants’ selection
Five DHT members and ten immunization focal point persons from the ten COVID-19 vaccination sites were purposively selected as key informants (KIs). The DHTs were the leads in training of the health workers on COVID-19 vaccination, mobilization and sensitization for the vaccination, planning and management of vaccine supplies and playing the overall supervisory role at the district level. The site focal persons were selected on the basis that they were the managers of the COVID-19 vaccination program at the sub-county and at health facility level; they managed supplies, records, sensitization and mobilization of health workers for COVID-19 vaccination.
2.4.3. Data collection
Data were collected using key informant interview guides from the district health team and immunization focal persons at COVID-19 vaccination sites. The topics included in the interview guide were; willingness to take the COVID-19 vaccine, known risks associated with the vaccine, concerns regarding vaccine safety and efficacy, views on mandatory vaccination and trust in the government regarding COVID-19 vaccination. The interview guide was developed basing on the quantitative findings, the qualitative findings were meant to elaborate on the factors associated with vaccine hesitancy. The interviews were conducted face to face in a quiet environment to avoid interruptions and allow a free interaction between the interviewer and the participant. After seeking permission from the participants, we audio recorded the interviews, transcribed them verbatim and translated those conducted in Lango to English.
2.4.4. Data analysis
Data were analyzed by the principal investigator and a qualitative research expert following thematic content analysis. Transcripts were read for familiarization, and the team coded two to three interviews together, to share conceptual thoughts, and increase coding rigor. The same interview was then coded by each individual and discussed, to improve coding standardization. A coding template and codebook were developed in NVivo 12.0.0 (QRS International, Cambridge, MA). The codebook was modified as inductive codes emerged. Teams held regular meetings, to check each other's coding, and the final coding was proofread, to increase credibility between the two coders. This was an ongoing process until all the transcripts were coded, and the coding framework was continually adapted. We aggregated similar codes to develop themes and finally wrote down qualitative findings while quoting participants’ responses.
2.5. Ethics approval and informed consent
Ethical approval for this study was sought from Mbale Regional Referral Hospital Research and Ethics Committee, approval number (MRRH-2021-86). A letter of permission to collect data in the institutions was granted by the Chief Administrative Officer, Dokolo District Local Government. Personal identifiers were not captured, and transcripts were anonymized. Informed consent was sought, and participation was voluntary.
3. Results
3.1. Quantitative results
Nearly three-quarters of the respondents [74.9% (259/346)] were aged between 18 and 35 years, and the mean age ± standard deviation was 31.4 ± 6.9. More than half of the participants [56.4% (195/346)] were females. Most [61.9% (210/339)] respondents were married, and the majority 69.6% (240/345) had a certificate level of education. Almost all the participants [95.1% (329/346)] had ever been vaccinated with COVID-19 vaccine, and 16.7% (57/342) reported a history of allergies to vaccination. Participants’ cadres were nurses [(65.6%) 225/343] clinicians [(9.0%) 31/343], environmental health officers [(14.3%) 49/343], laboratory technicians [(6.7%) 23/343], and doctors [(4.4%) 15/343]. The rest of the participant characteristics are shown in Table 1, Table 2.
Table 1.
Characteristics of health workers in Dokolo district in Uganda.
| Variable (n = 346) | Frequency | Percentage |
|---|---|---|
| Age | ||
| 18–35 | 259 | 74.9 |
| >35 | 87 | 25.1 |
| Gender | ||
| Male | 151 | 43.6 |
| Female | 195 | 56.4 |
| Marital Status (n = 339) | ||
| Married | 210 | 61.9 |
| Single | 129 | 38.1 |
| Level of Education (n = 345) | ||
| Certificate | 240 | 69.6 |
| Diploma | 86 | 24.9 |
| Bachelor's Degree and above | 19 | 5.5 |
| Respondents Cadres (n = 343) | ||
| Doctor | 15 | 4.4 |
| Clinical Officer | 31 | 9.0 |
| Nurse/Midwife | 225 | 65.6 |
| Laboratory Technician | 23 | 6.7 |
| Environmental Health Officers | 49 | 14.3 |
| Wealth Tertiles(n=310) | ta | |
| Poorer | 169 | 54.5 |
| Middle | 43 | 13.9 |
| Richer | 98 | 31.6 |
| Ever been vaccinated | ||
| Yes | 329 | 95.1 |
| No | 17 | 4.9 |
| Previous allergies (n = 342) | ||
| Yes | 57 | 16.7 |
| No | 285 | 83.3 |
Table 2.
COVID-19 vaccine related aspects among health workers in Dokolo district in Uganda.
| Variable (n = 346) | Frequency (n) | Percentage (%) |
|---|---|---|
| Do you intend to get the COVID-19 vaccine (n = 341) | ||
| Yes | 266 | 78.0 |
| No | 75 | 22.0 |
| Fear of COVID-19 vaccine side effects (n = 343) | ||
| Yes | 134 | 39.1 |
| No | 209 | 60.9 |
| History of comorbidity | ||
| Yes | 73 | 21.1 |
| No | 273 | 78.9 |
| Ever been diagnosed with COVID-19 (n = 337) | ||
| Yes | 29 | 8.6 |
| No | 308 | 91.4 |
| Ever refused any vaccination other than COVID-19 (n = 343) | ||
| Yes | 48 | 14.0 |
| No | 295 | 86.0 |
| Living with old family members (n = 343) | ||
| Yes | 71 | 20.7 |
| No | 272 | 79.3 |
| Have school-age children (n = 341) | ||
| Yes | 174 | 51.0 |
| No | 167 | 49.0 |
| Confidence in the capacity of health services (n = 344) | ||
| Yes | 237 | 68.9 |
| No | 107 | 31.1 |
| Trust in the information provided by health authorities (n = 344) | ||
| Yes | 280 | 81.4 |
| No | 64 | 18.6 |
| Perceived risk of getting COVID-19 (n = 343) | ||
| Yes | 285 | 83.1 |
| No | 58 | 16.9 |
| Perceived risk of developing severe disease following COVID-9 infection (n = 345) | ||
| Yes | 80 | 23.2 |
| No | 265 | 76.8 |
| The government has put adequate measures toward COVID-19 prevention (n = 344) | ||
| Yes | 170 | 49.4 |
| No | 174 | 50.6 |
3.2. Prevalence of vaccine hesitancy among health workers
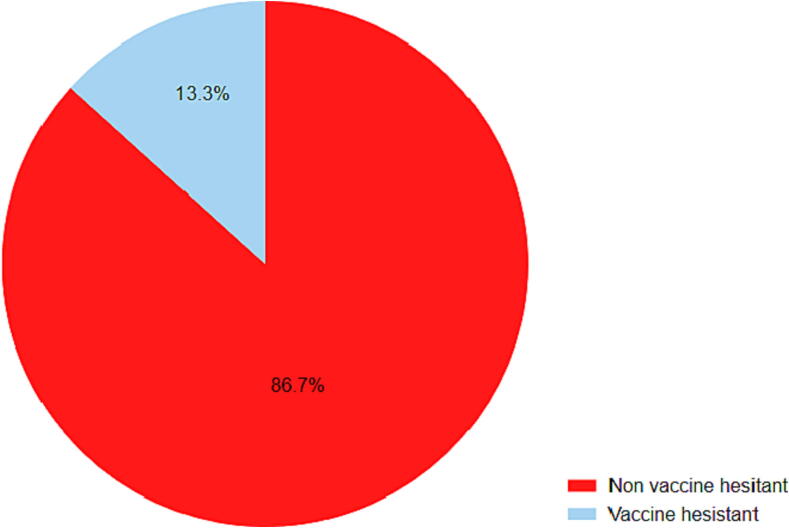
A total of 46 out of 346 health workers (13.3%) were vaccine hesitant as shown in Fig. 1 below.
Fig. 1.
Prevalence of vaccine hesitancy among health workers in Dokolo district in Uganda.
3.3. Factors associated with COVID-19 vaccine hesitancy
Table 3 shows factors associated with COVID-19 vaccine hesitancy among health workers. Health workers who had fear of the side effects were 2.55 times more likely to be vaccine-hesitant, in comparison to those with no fear of side effects (Adjusted Odds Ratio [AOR]: 2.55; 95% Confidence Interval [95% CI]: 1.00, 6.49). Those who did not have trust in the information provided by health authorities were 6.74 times more likely to be vaccine-hesitant than those who had trust in the information provided by health authorities (AOR: 6.74; 95% CI: 2.43, 18.72). The same factors were associated with vaccine hesitancy when we used the vaccine hesitancy index (Table 4).
Table 3.
Factors associated with COVID-19 vaccine hesitancy among health workers in Dokolo district in Uganda.
| Variable | Percentage reporting vaccine hesitancy, n (%) | Crude Odds Ratio (COR) | 95% Confidence Interval (95% CI) | p-value | Adjusted Odds Ratio (AOR) | 95% CI | p-value |
|---|---|---|---|---|---|---|---|
| Age | |||||||
| ≤35 | 34 (73.9) | 1.00 | 1.00 | ||||
| >35 | 12 (26.1) | 1.06 | 0.52, 2.15 | 0.874 | 0.31 | 0.06, 1.52 | 0.148 |
| Sex | |||||||
| Male | 20 (43.5) | 1.00 | 1.00 | ||||
| Female | 26 (56.5) | 1.01 | 0.54, 1.88 | 0.981 | 2.50 | 0.84, 7.43 | 0.100 |
| Education | |||||||
| Certificate | 24 (53.3) | 0.42 | 0.23, 0.80 | 0.008 | 1.14 | 0.36, 3.56 | 0.822 |
| ≥Diploma | 21 (46.7) | 1.00 | 1.00 | ||||
| Previous allergies | |||||||
| Yes | 14 (31.8) | 1.00 | 1.00 | ||||
| No | 30 (68.2) | 0.36 | 0.18, 0.74 | 0.005 | 0.539 | 0.159, 1.82 | 0.321 |
| Fear of side effects | |||||||
| Yes | 35 (76.1) | 0.16 | 0.08, 0.32 | <0.001 | 2.55 | 1.00, 6.49 | 0.050* |
| No | 11 (23.9) | 1.00 | 1.00 | ||||
| Trust in the information provided by health authorities | |||||||
| Yes | 18 (40.0) | 1.00 | 1.00 | ||||
| No | 27 (60.0) | 10.62 | 5.55, 21.15 | <0.001 | 6.74 | 2.43, 18.72 | <0.001* |
| Wealth Tertiles | |||||||
| Poorer | 11 (40.7) | 1.00 | 1.00 | ||||
| Middle | 2 (7.4) | 0.70 | 0.15, 3.29 | 0.625 | 1.093 | 0.21, 5.53 | 0.916 |
| Richer | 14 (51.9) | 2.39 | 1.04, 5.51 | 0.040 | 2.78 | 0.96, 8.03 | 0.059 |
| Perceived risk of contracting COVID-19 | |||||||
| Yes | 38 (82.6) | 1.04 | 0.46, 2.36 | 0.925 | 1.42 | 0.36, 5.53 | 0.605 |
| No | 8 (17.4) | 1.00 | 1.00 |
COR, Crude Odds Ratio; CI, Confidence interval; AOR, Adjusted Odds Ratio; *statistically significant at a p-value < 0.05.
Table 4.
Factors associated with COVID-19 vaccine hesitancy among health workers in Dokolo district in Uganda using a PCA generated vaccine hesitancy score.
| Variable | Crude Odds Ratio (COR) | 95% Confidence Interval (95% CI) | p-value | Adjusted Odds Ratio (AOR) | 95% CI | p-value |
|---|---|---|---|---|---|---|
| Age | ||||||
| ≤35 | 1.00 | 1.00 | ||||
| >35 | 1.52 | 0.76, 3.03 | 0.234 | 1.02 | 0.33, 3.24 | 0.963 |
| Sex | ||||||
| Male | 1.00 | 1.00 | ||||
| Female | 0.57 | 0.30, 1.08 | 0.981 | 1.23 | 0.48, 3.28 | 0.641 |
| Education | ||||||
| Certificate | 0.36 | 0.19, 0.69 | 0.002 | 1.11 | 0.38, 3.28 | 0.850 |
| ≥Diploma | 1.00 | 1.00 | ||||
| Previous allergies | ||||||
| Yes | 1.00 | 1.00 | ||||
| No | 0.44 | 0.21, 0.93 | 0.030 | 0.68 | 0.2, 2.35 | 0.547 |
| Fear of side effects | ||||||
| Yes | 4.94 | 2.43, 10.0 | <0.001 | 1.84 | 0.73, 4.64 | 0.194 |
| No | 1.00 | 1.00 | ||||
| Trust in the information provided by health authorities | ||||||
| Yes | 1.00 | 1.00 | ||||
| No | 9.91 | 4.91, 20.0 | <0.001 | 5.64 | 2.09, 15.2 | 0.001* |
| Wealth Tertiles | ||||||
| Poorer | 1.00 | 1.00 | ||||
| Middle | 1.33 | 0.35, 5.15 | 0.677 | 1.66 | 0.38, 7.21 | 0.496 |
| Richer | 2.72 | 1.12, 6.62 | 0.028 | 2.69 | 0.93, 7.83 | 0.068 |
| Perceived risk of contracting COVID-19 | ||||||
| Yes | 0.74 | 0.33, 1.63 | 0.453 | 0.83 | 0.25, 2.70 | 0.752 |
| No | 1.00 | 1.00 |
COR, Crude Odds Ratio; CI, Confidence interval; AOR, Adjusted Odds Ratio; *statistically significant at a p-value < 0.05.
3.4. Sensitivity analyses
We conducted a sensitivity analysis using a vaccine hesitancy score created by principal component analysis and found that fear of the side effects and lack of trust in information provided by health authorities were still significantly associated with vaccine hesitancy (Table 4). The first principal components were used as an index of vaccine hesitancy since it correlated with unwillingness to get COVID-19 vaccine, intention to get COVID-19 vaccine (0.5313), and unlikeliness to get COVID-19 vaccine (reverse coded). We defined vaccine hesitancy as a vaccine hesitancy score greater than two standard deviations above the mean vaccine hesitancy score.
3.5. Qualitative results
Key informants described the barriers to COVID-19 vaccination to include; perception of vaccine effectiveness, the fear of side effects, mandatory vaccination, distrust in the health system and authorities, feeling coerced to take the COVID-19 vaccine, lack of trust in the vaccine, and Severe Adverse Events (SAEs) and information asymmetry. These barriers are presented in detail below.
3.6. Poor perceptions of the vaccine effectiveness
We found that participants’ poor perceptions of the effectiveness of the COVID-19 vaccine were a significant barrier to taking the COVID-19 vaccine. Key informants argued that getting vaccinated with the COVID-19 vaccine does not guarantee protection from the COVID-19 disease, as it only prevents the severity of the disease and hospitalization. They also reported that signing consent forms is like signing a death sentence, and this was perceived to be risky, as reflected.
“[…] the covid-19 vaccine does not prevent health workers from getting the infection and also have been hearing people getting the vaccine but still getting the infection which I think only reduces the severity of infection making me think there should be more research on COVID-19 vaccine that makes people gain trust in it like the rest of the antigens. And I don't like the fact that you still contract the disease after beingvaccinated.itmeans the vaccine is not safe and effective.”[34 year-old male…P01]
“People think that there is high risk in getting vaccination because by filling the consent form, it's like filling a death warrant.” [35 year-old female…P15]
3.7. Fear of the side effects
We also found the fear of side effects of the COIVID-19 vaccines to be an enabler of vaccine hesitancy. Participants alluded to fearing too many side effects associated with the vaccine, which they reported were very discomforting and, in some cases, life-threatening. They also argued that they would refuse to take the vaccine, because of its side effects, and the notion of having to sign an informed consent was also indicative that it might have safety issues. However, some participants admitted to weighing the risk of side effects and the risk of death and decided to take the vaccine. The quotes of participants concisely described this:
“I know that people develop high body temperature and headache and hear that you get blood clots once vaccinated, and others can react adversely to the vaccine.” [28 year-old female …P06]
“Yes, the vaccine has serious side effects that are life-threatening ranging from high fever, body allergies, headache, and serious fatigue. Sometimes people are even hospitalized after vaccination.” [42 year-old female…P11]
“Yes, the side effects of the vaccines are very bad, which you have to overcome. However, if I weigh the risk of death with the side effects, I prefer getting vaccinated.” [34 year-old male…P05]
3.8. The lack of trust in the vaccine
The lack of trust in the COVID-19 vaccine by the participants was also found to be another barrier to COVID19 vaccination. Participants reported no trust in COVID-19 vaccines, and by virtue of being health workers, they unveiled issues around the vaccination exercise. These included; having to sign consent forms, making vaccination mandatory, and the short duration of vaccine development. The lack of clear information about the process of vaccine research and development would only be greeted with hesitancy, due to a lack of trust. Also, the vaccine safety issues were another justification for the lack of trust, due to the vaccine being under trial. This was depicted by the following quotes, as noted below.
“The vaccine was also new, people were not sure of the vaccines and look like the health workers were being experimented on. Additionally, people should have been allowed to make decisions on whether to take the vaccine or not since there was little trust in the new vaccine.” [34 year-old male…P01]
“It is difficult to say the vaccine is safe because of the serious side effects people are getting and more so it is still on trial though released under emergency use listing.” [42 year-old female…P11]
“The vaccine is still on trial and people who are getting it are like guinea pigs, which is a big risk.” [34 year-old male…P05]
3.9. Feeling coerced to take the COVID-19 vaccine
Participants perceived the mandatory vaccination orders by the health authorities to all health workers as a sign of coercion. They argued that the COVID-19 vaccine should not be made mandatory for health workers, with a number of them equating it to a violation of their rights in deciding to uptake the vaccine. Therefore, this feeling of coercion invoked fears in them, and they became hesitant.
A 35 year-old female was quoted as saying “[…]To make vaccination mandatory would mean people’s rights are not considered, and I don't support that. COVID-19 vaccination should not be made mandatory. Health workers should get vaccinated voluntarily and not through coercion.”.
3.10. Severe adverse events and information asymmetry
We also found that the participants were in fear of Severe Adverse Events (SAEs) of the new COVID-19 vaccines. They reported that they had not fully understood the performance of the vaccine, as they did not have complete information on the development, effectiveness, and efficacy of the vaccines. Some of the key informants reported that the research and development cycle process of the vaccine was not clearly defined; there was conflicting information on the vaccine safety, which aggravated their fears to uptake the vaccine. Other health workers reported incomplete information on the general prognosis after taking the COVID-19 vaccine.
“[…] Those with chronic infections do not want to get vaccinated because of the fear of adverse events following vaccination often associated with COVID-19 vaccines. Some health workers refuse vaccination because of rumors that the vaccine has been brought to depopulate the world”. [42 year-old female…P04]
3.11. Distrust in vaccine stakeholders
Having undivided trust in the vaccine authority is also reflected in one of our sub-themes. Respondents argued that the trust they would usually give the government was not the same in regard to the COVID-19 vaccination. However, this time, they were highly skeptical about the implementation of COVID-19 vaccination programs, and the people around the vaccine. This, we understand, was created by passing a mandatory vaccination decree on health workers against their wishes, and the information they were getting at the time.
“There is a lot of misleading information in the media and others from the top government officials. Even the high Ministry officials are sometimes inconsistent with their information, making it hard to trust the vaccines and the government” [42 year-old female…P04]
Examples of meaning units, categories, and themes generated from the thematic content analysis of interviews about COVID-19 vaccination hesitancy among health workers in Dokolo district are shown in Table 5 below.
Table 5.
Examples of meaning units, categories, and themes from the thematic content analysis of interviews about COVID-19 vaccination hesitancy among health workers in Dokolo district.
| Meanings unit/ quote | Categories | Themes |
|---|---|---|
| “I know that people develop high body temperature and headaches and hear that you get blood clots once vaccinated and others can react adversely to the vaccine”. [28 year old female …P06] “Yes, the vaccine has serious side effects that are life-threatening ranging from high fever, body allergies, headache, and serious fatigue. Sometimes people are even hospitalized after vaccination”. [42 year old female…P11] “Yes, the side effects of the vaccines are very bad and you have to overcome them, however, weighing the risk of death with the side effects. We prefer to get vaccinated.” [34 year old male…P05] |
Fear of side effects | Barriers to COVID-19 Vaccine hesitancy |
| “I do trust the government but not 100% and the fact that vaccines are brought from outsides makes me doubt the government and the vaccines.” [42 year old female…P04] “There is a lot of misleading information on the media and others from the top government officials. Even the high ministry officials are sometimes inconsistent with their information making it hard to trust the vaccines and the government” [42-year-old female…P04] |
Distrust in vaccine stakeholders | |
| “The vaccine was also new, people were not sure of the vaccine, and look like the health workers were being experimented on also, people should have been allowed to make decisions on whether to take the vaccine or not since there was little trust in the new vaccine” [34 year old male…P01] “It's difficult to say the vaccine is safe because of the serious side effects people are getting and more so it's still on trials though released under emergency use listing”.[42 year old female…P11] “The vaccine is still on trial and people who are getting it are like guinea pigs which is a big risk”[34 year old male…P05] |
No trust in the vaccine |
4. Discussion
Our study found that 13.3% of health workers were unwilling to take the COVID-19 vaccine. This finding could have been due to issues around COVID-19 vaccinations like mandatory vaccination of all the health workers decreed by the health authorities, fear of side effects, and concerns regarding the safety of the vaccine that was a very heated debate during this time. However, this finding are in line with the findings of a comprehensive worldwide assessment of published evidence on COVID-19 vaccine hesitancy among healthcare workers which found vaccine hesitancy in healthcare workers to range from 4.3% to 72% [18].
The finding of another online survey in Malta amongst the adult population to explore attitudes and factors influencing attitudes towards the COVID-19 vaccine and to identify the reasons why individuals are unsure or unwilling to take the vaccine also concurred with our findings, where vaccine hesitancy was present in the study population, with 32.6% being unsure, and 15.6% declaring that they were not willing to take the vaccine [19].
We found that the fear of side effects was associated with COVID-19 vaccine hesitancy among health workers in the Dokolo district. This finding could have been because the COVID-19 vaccine side effects were still being documented at the time, and some studies had reported blood clots in COVID-19 vaccine recipients [20], [21]. There was also fear of multiple side effects like headache, nausea, allergies, and others that were being reported by people in the community. This finding was supported by the result of another study conducted by Rizwan et al 2021 to assess the reasons for vaccine hesitancy among Pakistanis, which found that fear of serious side effects was the most common issue associated with hesitancy in all groups of people, including the health workers [22]. However, this finding was in disagreement with the findings of a study conducted in Northern Italy to identify the predictors of vaccine hesitancy which established that between groups, the levels of vaccine safety (54%) and efficacy (27%) did not necessarily indicate hesitancy [23].
This study also found the lack of trust in the information provided by the health authorities regarding the COVID-19 vaccine to be associated with hesitancy among health workers. Health workers are known to rely on various information channels to deliver their diagnosis and treatment to patients. During COVID-19, there was a lot of information published on the internet about the COVID-19 vaccine safety, and the mismatch of their findings and the information provided by the health authority during this period could have contributed to their hesitancy. This finding was in line with that of another study on COVID-19 vaccine hesistancy by Chaudhuri et al which found individuals and groups who possessed a negative attitude towards public officials and the government were unwilling to be vaccinated most in most cases [24].
4.1. Barriers to COVID-19 vaccination
We found that lack of trust in the information regarding the efficacy and safety of the COVID-19 vaccines provided by the health authorities was a key barrier to taking the COVID-19 vaccine among health workers. This was because people didn’t trust the information they were getting regarding the vaccine safety and the idea of signing a consent form was associated with a death sentence by some participants. This was also worsened by the mandatory vaccination decree put on them to get the vaccine. This finding is in agreement with the findings from a study conducted among Egyptian medical students which found insufficient data regarding the vaccine’s adverse effects and insufficient information regarding the vaccine itself to be the most significant influencers of COVID-19 vaccination hesitancy [12].
Furthermore, we also found the fear of side effects by participants to be one of the barriers to COVID-19 vaccination. Participants reported that the COVID-19 vaccine had too many side effects like headache, pain at the injection sites, allergies, and some life-threatening effects that made them hesitant. Furthermore, the many of those that were vaccine-hesitant noted that they were willing to take the vaccine, if additional studies were available, documenting the safety and effectiveness of the vaccine, meaning the fear of side effects was key to their hesitancy. Our finding was in line with other findings that assessed the beliefs and barriers associated with COVID-19 vaccination uptake and found concerns about side effects as one of the key barriers to vaccine acceptance [25], [26], [27], [28]. Additionally, a rapid systematic review on healthcare workers attitude and related factors towards COVID-19 vaccination revealed that concerns about safety, efficacy and effectiveness were barriers to COVID-19 vaccination [29].
The lack of trust in the COVID-19 vaccine stakeholders also emerged strongly from our key informants as another key barrier to COVID-19 vaccination among health workers. Participants alluded to having little trust in the vaccine owing to the circumstances around the vaccine like signing consent forms, mandatory vaccination, coercion by health authorities, and the short duration of manufacturing COVID-19 vaccine. This finding is in line with findings from other studies which also found out that lack of trust in health authorities was a significant barrier to receiving the COVID-19 vaccine [24], [30], [31].
4.2. Strengths and limitations
We utilized a mixed-methods sequential explanatory design, combining both quantitative and qualitative methods of data collection. The use of the two approaches in this study increased the rigor, trustworthiness, and angles at which we investigated the outcomes. The quantitative phase was followed by a qualitative phase. The qualitative findings helped us make meaning of the quantitative results. For instance, the key informant interviews gave us meaningful insights into the factors associated with COVID-19 vaccine hesitancy among health workers in Dokolo district. To ensure trustworthiness in this study, we ensured that after transcribing the transcript and analyzing data, the results were read to a few participants for validation. The use of two coders also helped us to increase the coding rigor and credibility of our results. Since we recruited almost all the registered health workers from both private and public health facilities (3 5 0) and 346/350 participated in the study, we believe selection bias could be minimal in our study. Since we investigated outcomes like willingness to take COVID-19 vaccine, misclassification of the outcomes is probably minimal in the study. All the health workers interviewed were followed to their respective health facilities, this reduced selection bias. Additionally, the knowledge that the principal investigator in this study was a member of the district health team and the focal person for COVID-19 surveillance in Dokolo district and also played a key role in coordinating COVID-19 vaccination activities, could have biased the way health workers were recruited and also may have introduced a social desirability bias since at the time there were threats to terminate unvaccinated health workers all over the world [32]. Many health workers could have lied about their vaccination status to a DHT member. Lastly, varying statistics globally due to changes in trends of managing COVID-19, changes in the information, evidence and also changes in tools for measuring vaccine hesitancy. Our definition of COVID-19 vaccine hesitancy could have created an information bias. However, sensitivity analyses with a much more inclusive definition resulted into similar results.
5. Conclusions
The prevalence of COVID-19 vaccine hesitancy among health workers in Dokolo district was low at 13.3%. The factors associated with COVID-19 vaccine hesitancy were lack of trust in the information provided by the health authorities and fear of side effects. Qualitative participants identified fear of the side effects, distrust in vaccine stakeholders and feeling coerced to undergo COVID-19 vaccination as barriers to COVID-19 vaccination among health workers in Dokolo district. We therefore recommend that health stakeholders, including the Ministry of Health Uganda, the World Health Organization, and non-state actors should explain COVID-19 vaccine safety and embark on rigorous information dissemination on the known side effects and management strategies, to restore vaccine confidence among health workers and the public and also accurately packaging the information on COVID-19 vaccine from the national and sub-national level, and use correct and reliable channels to disseminate the information to erase distrust in the information passed out on COVID-19 vaccine.
Funding
There was no funding received for this study.
Data availability
Data will be made available on request.
CRedit Author Statement
Patrick DioxOuni: Conceptualization, Formal analysis, Funding acquistion, Investigation, Methodology, Project administration, Resources, Visualization, Original draft, Review. Racheal Namulondoa: Conceptualization, Data curation, Methodology, Review. Benon Wanume: Data curation, Formal analysis, Review. David Okia: Data curation, Formal analysis, Methodology, Review. Peter Olupot Olupot: Methodology, Review. Ritah Nantale: Project administration, Software, Supervision, Visualization, Original draft, Review. Joseph K.B. Matovu: Methodology, Validation, Review. Agnes Napyo: Methodology, Validation, Review. Yovani A.Moses Lubaale: Methodology, Validation, Review. Nathan Nshakira: Methodology, Review. David Mukunya: Conceptualization, Methodology, Project administration, Supervision, Original draft, Review.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
In a special way, we extend our heartfelt appreciation to Ms. Vivian Mutaki and Ms. Brendah Nambozo who were very helpful during the data collection process and qualitative data analysis. Our sincere gratitude also goes to all the study participants who willingly took time to provide the information needed to complete this study.
Data availability
Data will be made available on request.
References
- 1.Olum R., Bongomin F. Uganda’s first 100 COVID-19 cases: trends and lessons. Int J Infect Dis. 2020;96:517–518. doi: 10.1016/j.ijid.2020.05.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tallio V. Uganda’s Social Policy Response to Covid-19: Rudimentary Relief Measures. 2021.
- 3.Nabukeera MS. The Covid-19 Coronavirus Pandemic and theHealth Sector in Uganda. 2021.
- 4.Sarki A.M., Ezeh A., Stranges S. Uganda as a role model for pandemic containment in Africa. Am J Public Health. 2020;110(12):1800–1802. doi: 10.2105/AJPH.2020.305948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pritchard E, Matthews PC, Stoesser N, Eyre DW, Gethings O, Vihta K-D, et al. Impact of vaccination on SARS-CoV-2 cases in the community: a population-based study using the UK’s COVID-19 Infection Survey. medRxiv 2021.
- 6.Parker E.P., Desai S., Marti M., Nohynek H., Kaslow D.C., Kochhar S., et al. Response to additional COVID-19 vaccine doses in people who are immunocompromised: a rapid review. Lancet Glob Health. 2022;10(3):e326–e328. doi: 10.1016/S2214-109X(21)00593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richterman A., Meyerowitz E.A., Cevik M. Indirect protection by reducing transmission: ending the pandemic with severe acute respiratory syndrome coronavirus 2 vaccination. Open Forum Infect Dis. 2021;9(2) doi: 10.1093/ofid/ofab259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Majeed A., Papaluca M., Molokhia M. Assessing the long-term safety and efficacy of COVID-19 vaccines. J R Soc Med. 2021;114(7):337–340. doi: 10.1177/01410768211013437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu Q., Qin C., Liu M., Liu J. Effectiveness and safety of SARS-CoV-2 vaccine in real-world studies: a systematic review and meta-analysis. Infect Dis Poverty. 2021;10(1):132. doi: 10.1186/s40249-021-00915-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maraqa B., Nazzal Z., Rabi R., Sarhan N., Al-Shakhra K., Al-Kaila M. COVID-19 vaccine hesitancy among health care workers in Palestine: a call for action. Prev Med. 2021;149:106618. doi: 10.1016/j.ypmed.2021.106618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biswas N., Mustapha T., Khubchandani J., Price J.H. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. 2021;46(6):1244–1251. doi: 10.1007/s10900-021-00984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saied S.M., Saied E.M., Kabbash I.A., Abdo S.A.E.F. Vaccine hesitancy: beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J Med Virol. 2021;93(7):4280–4291. doi: 10.1002/jmv.26910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agyekum M.W., Afrifa-Anane G.F., Kyei-Arthur F., Addo B. Acceptability of COVID-19 vaccination among health care workers in Ghana. Adv Public Health 2021. 2021 [Google Scholar]
- 14.Kanyike A.M., Olum R., Kajjimu J., Ojilong D., Akech G.M., Nassozi D.R., et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Tropical Med Health. 2021;49(1) doi: 10.1186/s41182-021-00331-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.POPULATION STATISTICS, CHARTS AND MAPS [Cited 2022 July 24]; Available from: https://www.citypopulation.de/en/uganda/northern/admin/074__dokolo/.
- 16.Lessard D., Ortiz-Paredes D., Park H., Varsaneux O., Worthington J., Basta N.E., et al. Barriers and facilitators to COVID-19 vaccine acceptability among people incarcerated in Canadian federal prisons: a qualitative study. Vaccine: X. 2022;10:100150. doi: 10.1016/j.jvacx.2022.100150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crawshaw A.F., Farah Y., Deal A., Rustage K., Hayward S.E., Carter J., et al. Defining the determinants of under-vaccination in migrant populations in Europe to improve routine and COVID-19 vaccine uptake: a systematic review. MedRxiv. 2021 doi: 10.1016/S1473-3099(22)00066-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Biswas B., Chattopadhyay S., Hazra S., Hansda A.K., Goswami R. COVID-19 pandemic: the delta variant, T-cell responses, and the efficacy of developing vaccines. Inflamm Res. 2022;71(4):377–396. doi: 10.1007/s00011-022-01555-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cordina M., Lauri M.A., Lauri J. Attitudes towards COVID-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharmacy Practice (Granada) 2021;19(1):2317. doi: 10.18549/PharmPract.2021.1.2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahase E. British Medical Journal Publishing Group; In.: 2021. Covid-19: US suspends Johnson and Johnson vaccine rollout over blood clots. [DOI] [PubMed] [Google Scholar]
- 21.Wise J: Covid-19: European countries suspend use of Oxford-AstraZeneca vaccine after reports of blood clots. In.: British Medical Journal Publishing Group; 2021. [DOI] [PubMed]
- 22.Rizwan W., Rana M.N., Bukhari M.H., Mushtaq A., Sadiq M. Reasons of vaccine hesitancy among Pakistanis with available COVID-19 vaccine: the next challenge in the fight against COVID-19. Nat Sci. 2021;13(6):211–217. [Google Scholar]
- 23.Reno C., Maietti E., Fantini M.P., Savoia E., Manzoli L., Montalti M., et al. Enhancing COVID-19 vaccines acceptance: results from a survey on vaccine hesitancy in Northern Italy. Vaccines. 2021;9(4):378. doi: 10.3390/vaccines9040378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chaudhuri K., Chakrabarti A., Chandan J.S., Bandyopadhyay S. COVID-19 vaccine hesitancy in the UK: a longitudinal household cross-sectional study. BMC Public Health. 2022;22(1):1–13. doi: 10.1186/s12889-021-12472-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Magadmi R.M., Kamel F.O. Beliefs and barriers associated with COVID-19 vaccination among the general population in Saudi Arabia. BMC Public Health. 2021;21(1):1–8. doi: 10.1186/s12889-021-11501-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yousif AA-b, Taha EES, Faragalla MME: Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among the general population in Sudan. Napata College; 2021.
- 27.Sharun K., Rahman C.K.F., Haritha C.V., Jose B., Tiwari R., Dhama K. COVID-19 vaccine acceptance: beliefs and barriers associated with vaccination among the general population in India. J Exp Biol Agric Sci. 2020;8(Spl-1-SARS-CoV-2):S210–S218. [Google Scholar]
- 28.Altulahi N., AlNujaim S., Alabdulqader A., Alkharashi A., AlMalki A., AlSiari F., et al. Willingness, beliefs, and barriers regarding the COVID-19 vaccine in Saudi Arabia: a multiregional cross-sectional study. BMC Fam Pract. 2021;22(1):1–11. doi: 10.1186/s12875-021-01606-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li M., Luo Y., Watson R., Zheng Y., Ren J., Tang J., et al. Healthcare workers’(HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review. Postgrad Med J. 2021 doi: 10.1136/postgradmedj-2021-140195. [DOI] [PubMed] [Google Scholar]
- 30.Fisk R.J. Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: experience from the United States. Global Health J. 2021;5(1):51–55. doi: 10.1016/j.glohj.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burke P.F., Masters D., Massey G. Enablers and barriers to COVID-19 vaccine uptake: an international study of perceptions and intentions. Vaccine. 2021;39(36):5116–5128. doi: 10.1016/j.vaccine.2021.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Northwell begins exiting unvaccinated team members [Cited 2022 July 24]; Available from: https://www.northwell.edu/news/in-the-news/new-york-hospitals-face-possible-mass-firings-as-workers-spurn-vaccines-.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.
Data will be made available on request.