Abstract
Purpose of the Review
Neuro-ophthalmologists rapidly adopted telehealth during the COVID-19 pandemic to minimize disruption to patient care. This article reviews recent research on tele-neuro-ophthalmology adoption, current limitations, and potential use beyond the pandemic. The review considers how digital transformation, including machine learning and augmented reality, may be applied to future iterations of tele-neuro-ophthalmology.
Recent Findings
Telehealth utilization has been sustained among neuro-ophthalmologists throughout the pandemic. Adoption of tele-neuro-ophthalmology may provide solutions to subspecialty workforce shortage, patient access, physician wellness, and trainee educational needs within the field of neuro-ophthalmology. Digital transformation technologies have the potential to augment tele-neuro-ophthalmology care delivery by providing automated workflow solutions, home-based visual testing and therapies, and trainee education via simulators.
Summary
Tele-neuro-ophthalmology use has and will continue beyond the COVID-19 pandemic. Digital transformation technologies, when applied to telehealth, will drive and revolutionize the next phase of tele-neuro-ophthalmology adoption and use in the years to come.
Keywords: Telehealth, Telemedicine, Neuro-ophthalmology, Pandemic, Artificial intelligence, Augmented reality
Introduction
The coronavirus disease-19 (COVID-19) pandemic has indelibly altered medical care and global society. Within neuro-ophthalmology, a key shift has been the adoption of telemedicine services. Publications regarding telemedicine use in neuro-ophthalmology were scant until after the declaration of a Public Health Emergency in the USA (March 2020) [1••]. Since 2020, an exponential expansion of resources and research has demonstrated that tele-neuro-ophthalmology offers many benefits to patient care in selected situations, and attitudes towards the continued use of telemedicine remain positive [2••].
Tele-Neuro-Ophthalmology Utilization Before COVID-19
Historically, telehealth adoption in neuro-ophthalmology has been limited by existing technology, financial reimbursement, and governmental regulations [3•]. Prior to the COVID-19 pandemic, less than 4% of neuro-ophthalmologists within the North American Neuro-Ophthalmology Society (NANOS), the largest international organization of neuro-ophthalmologists in the world, utilized synchronous telehealth [1••]. Within the parent specialties of neuro-ophthalmology, telemedicine applications in neurology definitively established benefits in the management of stroke and other neurological disorders [4], while ophthalmology-based adoption focused on diagnostic test interpretation, such as in remote monitoring of diabetic retinopathy and retinopathy of prematurity [5, 6]. Prior to the COVID-19 pandemic, due to significant restrictions in telehealth reimbursement, utilization of telehealth within the US was very limited. Therefore, national advocacy efforts were underway to expand telehealth, including efforts that specifically impacted neurological patients. For example, in 2015, the American Academy of Neurology (AAN), the American Heart Association (AHA), and the American Stroke Association (ASA) successfully collaborated on the passage of the Furthering Access to Stroke Telemedicine (FAST) Act. In 2018, the FAST Act was signed into law, which requires Medicare to reimburse for telestroke services regardless of where a patient receives treatment, thereby expanding telestroke coverage to include urban and rural areas throughout the country [7].
Tele-Neuro-Ophthalmology Utilization During Early COVID-19
The policies precipitated by the COVID-19 Public Health Emergency (PHE) included lifting many regulatory barriers and promoting parity in reimbursement for telemedicine services [8]. This coverage expansion allowed many neuro-ophthalmologists to reimagine appropriate patient care delivery while navigating the constraints of a global health crisis [9•], including the adoption of synchronous and asynchronous telehealth, developing techniques for performing elements of the neuro-ophthalmic exam virtually, and scrutinizing triage protocols.
In May 2020, NANOS conducted a survey of its membership regarding telehealth use [1••]. The survey reported that before the pandemic, 3.9% of respondents used synchronized telehealth; by May 2020 (roughly 6 months after the initial cases of COVID-19 were reported), that number had increased to 68.3%, a 17.5-fold increase [1••]. Survey respondents cited telehealth benefits, including ensuring continuity of care, improving patient access to care, and patient convenience [1••]. Respondents also increased the adoption and utilization of asynchronous telehealth modalities, including remote interpretation of tests, second opinion record review, and interprofessional consultations (eConsults). Neuro-ophthalmology telehealth adopters and non-adopters responding to the survey noted the following barriers to telehealth use: concerns about data/physical exam quality, reimbursement, medical liability, and sufficient infrastructure support for telehealth implementation [1••]. Another study citing seismic tele-neuro-ophthalmic adoption shifts during the early pandemic includes a US-based, multicenter retrospective study of four academic and private-practice neuro-ophthalmologists [10]. Moss et al. reported no telemedicine use in 2019, compared to 39.8% of patients managed by telemedicine over the analogous period in 2020 [10].
Tele-Neuro-Ophthalmology Utilization One Year After Onset of COVID-19
In 2021, a follow-up survey of NANOS members demonstrated that 50.8% of respondents were still utilizing synchronized telehealth. Utilization of other telehealth modalities also sustained increased adoption. Despite concerns about continued reimbursement and regulatory support, 82.1% of synchronized telehealth users indicated interest in continued utilization [2••].
Attitudes and Perception of Telehealth Among Neuro-Ophthalmologists
In the 2020 and 2021 surveys, neuro-ophthalmologists expressed positive sentiments toward patient-centered benefits (access and continuity of care, patient efficiency) [1••, 2••]. However, over 90% of participants in the 2021 survey reported patient technology barriers and exam data limitations [2••]. The survey found that while there was heterogeneity in the opinions of exam element suitability performed during synchronous video exams, data elements collected outside of the video visit and ancillary testing review were uniformly considered suitable for tele-neuro-ophthalmology. The survey responses for remote interpretation of test data suitability correlated with other studies demonstrating safety and feasibility of remote interpretation of visual fields [11•]. The 2021 survey noted that nearly half of participants incorporated remote interpretation into their practice [2••].
Neuro-Ophthalmologists' Interest in Future Telehealth Use
Data from the 2021 survey indicates that neuro-ophthalmologists, especially from neurology-based training, generally follow neurology practice utilization of telehealth, rather than ophthalmology practice [2••]. A year into the pandemic, 49.6% still utilized synchronous telehealth, indicating the establishment of tele-neuro-ophthalmology as a common practice [2••]. However, 30% of participants did not perform synchronous video telemedicine visits during any of the surveyed periods, suggesting utilization remains heterogeneous [2••].
Of surveyed neuro-ophthalmologists utilizing synchronous telehealth in 2021, 82.1% planned to continue offering video visits [2••]. Despite the continued interest, concerns of reimbursement and regulatory changes may impact sustainability [2••]. This uncertainty is recognized by US healthcare leaders, despite the acknowledgment of telehealth’s promotion of patient equity and access to healthcare [12].
Can Tele-Neuro-Ophthalmology Be Useful Beyond the Pandemic?
Neuro-ophthalmology can benefit from synchronous telehealth by addressing workforce shortages, expanding access to care for patients limited by geographical distance, accommodating patients with physical impairment, offering neuro-ophthalmic education and training to a broader audience, and improving efficiency of care delivery for applicable neuro-ophthalmic conditions [13••].
Tele-Neuro-Ophthalmology Addresses Neuro-Ophthalmology Workforce Shortages and Expands Access to Neuro-Ophthalmic Care
Within the USA, there is an alarming shortage of neuro-ophthalmologists, with a projected need for an additional 180 neuro-ophthalmologists (working 0.5 clinical full-time equivalent) to meet the population demands of the country [14••]. This workforce shortage has resulted in prolonged wait times and geographic limitations in access to neuro-ophthalmic care, with pre-COVID median wait times of 6 weeks for new appointments [14••]. Telehealth services offer partial amelioration by affording patients in geographically distant regions access to neuro-ophthalmic care without requiring exhaustive commutes [13••]. Triaging suitable conditions and shifting established patients not requiring an internal eye examination to telemedicine vacates limited in-person clinic slots in favor of patients needing direct examination [13••]. Telemedicine also offers stable established patients the opportunity to address their concerns without waiting for an in-person visit [13••].
Asynchronous Tele-Neuro-Ophthalmology Improves Patient Access
Time-sensitive patient access to neuro-ophthalmology from specialists who frequently request our diagnostic testing and interpretation of tests is a common conundrum. Oftentimes, our colleagues from neurosurgery, otolaryngology, and endocrinology urgently seek visual fields to triage if a skull-base or sellar mass is sight-threatening and therefore requires emergent surgery. Pre-pandemic, some neuro-ophthalmic practices employed specific procedure-only slots within a weekly clinic template to accommodate these urgent requests whereby the ophthalmic technician performs the diagnostic testing and electronically sends the imaging for the neuro-ophthalmologist to interpret formally without having to physically examine the patient.
Kung et al. recently performed a retrospective chart review of their remote interpretation of visual fields performed in 2012 (n = 180), well before the COVID-19 pandemic. They found that the most frequent referring departments were endocrinology (79; 44%), neurology (51; 28%), and neurosurgery (43; 24%) [11•]. Indications for the visual field included parasellar lesion (107; 59%), seizure disorder (26; 14%), meningioma (19; 11%), vascular lesion (11; 6%), and other (17; 9%). Seventy-eight patients (43%) had an intervention prior to the VF, while 49 (27%) were preoperative VFs. Eighty-seven (48%) of the VFs were interpreted as abnormal [11•].
Of all the 180 remote interpretations of visual fields, 87% had VF interpretations consistent with the clinical question posed by the referring provider based on prior clinical history and imaging. The median wait time for patients receiving remote VF interpretations was 1 day at this single institution [11•]. With such rapid turnaround, remote interpretation of visual fields may offer specific referring departments an efficient method of obtaining visual field interpretations than in-office neuro-ophthalmology examinations. This can improve timely multi-disciplinary decision-making, particularly in brain tumor operative management cases. Other practices have utilized remote interpretation of data workflows whereby the visual fields are performed off-site at the referring physician’s office (e.g., neurosurgery practices). Then, the visual fields are remotely sent via the electronic medical record to the neuro-ophthalmologist for interpretation (H Moss, Personal Communication, February 2021).
eConsults (also called interprofessional consults) are another form of asynchronous communication utilized within neuro-ophthalmology. Like remote interpretation of testing, the neuro-ophthalmologist does not see or examine the patient. Rather, the requesting physician asks the neuro-ophthalmologist a specific clinical question via review of the clinical records. While this can be accomplished in formal written form, within the digital age, the requesting physician often utilizes an EMR platform to send the neuro-ophthalmologist their query for back-and-forth response.
Xu et al. published a retrospective review of a single institution’s experience with eConsults (n = 80) during a 3-year study period [15•]. The median time from eConsult request to completion was 4 days (range 0–34 days). The most frequent eConsult questions were vision/visual field disturbances (35.0%) cases, optic neuropathies (32.5%), and optic disc edema (21.3%). At the time of eConsult, 44% of cases provided sufficient prior information for the neuro-ophthalmologist to provide a definitive management decision. In over 56% of the eConsults, further diagnostic testing was recommended. In-person neuro-ophthalmology consultation was recommended in 30.0% of cases. Sixty-one (76.3%) eConsults provided diagnostic and/or treatment direction, and 12 (15.0%) provided reassurance. eConsults increase access to timely neuro-ophthalmic care and provide diagnostic and treatment direction to requesting physicians when sufficient information is provided at the time of eConsult. In addition, with 15% of cases providing reassurance, this, in essence, triages otherwise referred in-person visits and opens additional scheduling template slots for the most appropriate patient cases.
Elements of the Neuro-Ophthalmic Exam Amenable to Synchronous Telehealth
A prospective survey was conducted on patient and physician experiences with consecutive tele-neuro-ophthalmology visits at three tertiary care academic institutions in the USA during the early COVID period [16•]. Neuro-ophthalmologists generally indicated that the synchronous telehealth history and examination were sufficient for decision-making (87% of visits) [15•]. Exam elements indicated by neuro-ophthalmologists that were easy to conduct include.
Range of eye movements
Visual acuity
Ishihara color plate assessment
Amsler grid testing
Red desaturation evaluation
These impressions were corroborated by the 2021 NANOS survey, which found similar results [2••].
Tele-Neuro-Ophthalmology Expands Neuro-Ophthalmic Education Opportunities
The Accreditation Council for Graduate Medical Education (ACGME) requires neurology and ophthalmology training programs to provide sufficient training in subspecialties applicable to their respective fields, including neuro-ophthalmology [17, 18]. Because of the workforce shortages in neuro-ophthalmology, some US training programs have had to obtain neuro-ophthalmology faculty from outside institutions to satisfy ACGME requirements [13••]
Synchronous telemedicine offers trainees from remote institutions exposure to geographically distant neuro-ophthalmologists [13••]. Asynchronous telehealth curricula such as the Neuro-Ophthalmology Virtual Education Library (NOVEL) and the Eccles Health Sciences Library at the University of Utah and the Neuro-Ophthalmology Illustrated Curriculum developed by NOVEL and NANOS fill curriculum gaps and provide education to learners across a broad range of interests [19].
Tele-Neuro-Ophthalmology and Physician Wellness
The American Medical Association (AMA) conducted a survey to evaluate relationships between pandemic-related stress and work intentions in a sample of US health care workers [20]. Among 2914 physician respondents at 124 institutions, approximately 1 in 3 physicians surveyed intend to reduce work hours. One in 5 physicians intend to leave their practice altogether within the next 2 years. Burnout, fear of exposure, COVID-19-related anxiety/depression, and workload were predictors of intent to leave [20]. Medscape examined burnout rates in over 13,000 physicians and noted that burnout among neurologists and ophthalmologists was 46% and 40%, respectively [21]. The top cited reasons for burnout among physicians included bureaucratic tasks, lack of respect from administrators/employees, too many hours at work, and lack of control/autonomy over one’s life. When asked what would help improve burnout, respondents stated that a more manageable work schedule, lighter work schedule, more autonomy/control over life, and increased compensation would help [21].
While it has been suggested in opinion pieces that telemedicine may provide a reduction in physician burnout and improve wellness, few studies have been performed. Aklureishi et al. performed an observational, cross-sectional study of healthcare providers (nearly 75% of physicians). They noted that video visits took longer to prepare (33%) and conduct (62/200, 32%) than in-person visits [22]. Clinicians who conducted a higher percentage of their telemedicine by video were less likely to feel overwhelmed, with no difference in reported burnout. Interestingly, clinicians 50 or older were “less overwhelmed” than those younger than 50 years, which may be related to clinical experience. Clinicians who received more video visit training modalities were less likely to feel overwhelmed by the conversion to video visits (P = 0.007) or burnt out (P = 0.009). In addition, those reporting a higher ability to navigate a video visit were also less likely to feel overwhelmed by video visits (P = 0.02) or burned out (P = 0.001). More than half “enjoyed conducting video visits” (60%) and wanted to continue using video visits in the future (75%) [23]. Similar to the neuro-ophthalmology surveys cited above, the top telemedicine barriers were patient-related: lack of technology access, lack of skill, and reluctance, with clinicians noting an increased need for increased support staff to ease the workflow. More research is required to understand if telehealth facilitates physician wellness. Nonetheless, Aklureishi’s study suggests that experienced clinicians and those with sufficient telehealth training and operational support are less likely to experience burnout [22].
Reimbursement and regulations on telehealth services vary from country to country. In the USA, the Centers for Medicare and Medicaid Services (CMS) determine the parameters of telehealth eligibility for Medicare patients. Private insurers and state Medicaid programs may have different requirements and fee schedules.
Prior to the COVID-19 pandemic, CMS allowed telehealth in restricted contexts, only allowing patients to receive synchronous telehealth care if they lived in designated “Healthcare Provider Shortage Areas” [23], and both the physician and patient were located in approved facilities. Other triage-associated telehealth services, such as eConsults, remote interpretation of diagnostic tests, and short synchronous and asynchronous physician–patient communications (phone, video, or electronic) were also available [24].
The COVID-19 PHE temporary waivers removed restrictions on some interstate licensure requirements, geographic restrictions on eligible patients, added reimbursement for audio-only synchronous telehealth, and waived location requirements for medical professionals and patients. These waivers allowed tele-neuro-ophthalmic care for patients living hours away from a neuro-ophthalmologist [10]. There are continued advocacy efforts to codify these changes to improve access to care.
The Future of Tele-Neuro-Ophthalmology
The practice of neuro-ophthalmology will never return to pre-pandemic patterns. Based on the authors’ 2021 survey of neuro-ophthalmologists 1 year into the pandemic, utilization of tele-neuro-ophthalmology continued despite lower COVID case numbers, lower COVID-related hospitalizations, and the advent of the COVID vaccination [2••]. While 30% of respondents never utilized telehealth, over 60% adopted tele-neuro-ophthalmology. Eighty-two percent of adoptees indicated that they plan to continue, but the survey did not directly query respondents as to their rationale for continued telehealth use [2••].
Digital Transformation: Tele-Neuro-Ophthalmology 2.0 and Beyond
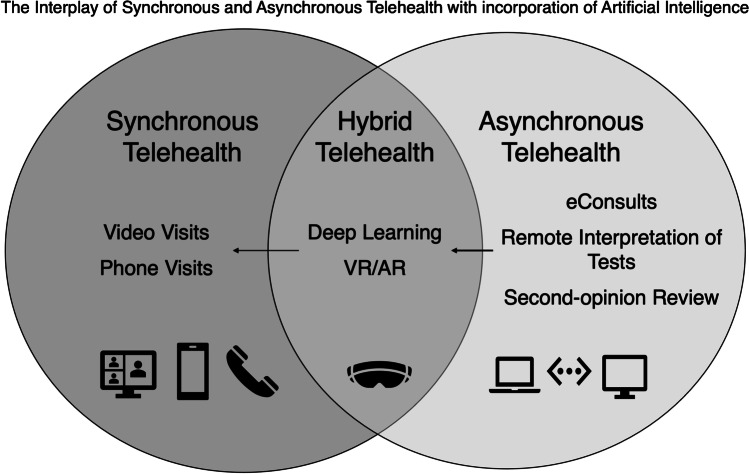
As tele-neuro-ophthalmology enters its next iteration, incorporating other digital technologies is expected to enhance healthcare and its intersection with telehealth delivery (Fig. 1). Digital transformation is defined as the process of improving an entity through the combination of digital technologies, including information, computing, communication, and connectivity [25]. Within ophthalmology and, by extension, neuro-ophthalmology, digital transformation can potentially improve patient access and healthcare delivery through artificial intelligence (AI), machine learning, deep learning (DL), and virtual reality and augmented reality (VR and AR) [26]. Through these digital transformation technologies, some existing barriers within current tele-neuro-ophthalmology delivery may be surmountable, including improving physician workflow and utilizing forms of deep learning for screening and triaging patient based on DL analysis of ophthalmic images and using augmented reality for home monitoring of vision field progression.
Fig. 1.
The interplay of synchronous and asynchronous telehealth with incorporation of artificial intelligence. Synchronous telehealth is live/interactive telehealth that can be either clinic or home based. It includes video or phone visits. Asynchronous telehealth is a “store-and-forward” approach where testing/information is obtained and then shared through a portal for a physician to review later. Hybrid telehealth incorporates both synchronous and asynchronous modalities including capturing a visual field or fundus photograph asynchronously for the neuro-ophthalmologist to review at a later time point. A video visit is then scheduled for the neuro-ophthalmologist to synchronously review with the patient the testing results and care management plan. An example of a potential artificial intelligence (AI)-driven future state of neuro-ophthalmology is where asynchronous data is obtained via augmented reality (AR) home monitoring of a visual field defect. Deep learning (DL) algorithms then interpret the change in the visual field defect from previously obtained visual fields of the patient. If there are significant changes, DL can then pivot to either alert scheduling of an urgent synchronous video visit or a routine video visit with the patient
Artificial Intelligence and Deep Learning
AI is the broad umbrella concept under which machine and deep learning reside (Fig. 2). AI is defined as any technique that is used to mimic sentient behavior [27]. AI is utilized in everyday life, from voice commands on smart devices to robotic vacuum cleaners.
Fig. 2.
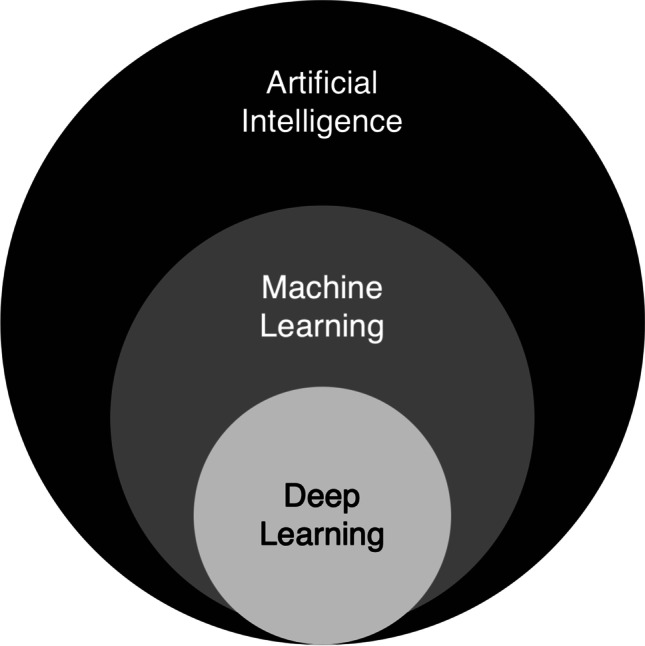
Artificial intelligence, machine learning, and deep learning defined. AI is the broad umbrella concept under which machine and deep learning reside. AI is defined as any technique that is used to mimic sentient behavior. Machine learning (ML) is a form of AI focused on data analysis by the construction and study of algorithms that process data to develop prediction or decision models. Deep learning (DL) is a form of machine learning that mimics human learning by layering multiple automated learning algorithms over the data in an iterative process to achieve the desired level of accuracy
Machine learning (ML) is a form of AI focused on data analysis. ML is the construction and study of algorithms that process data to develop prediction or decision models. Unlike traditional computer programming, ML does not need programmers to write step-by-step scripting for a computer to follow. Instead, they train computers to recognize patterns based on data [28]. One example of ML is the spam filter on e-mail systems, which can learn by direct input from humans and from automated pattern-recognition algorithms.
Deep learning (DL) is a form of machine learning that mimics human learning by layering multiple automated learning algorithms over the data in an iterative process to achieve the desired level of accuracy (Fig. 1) [29]. As a result, DL is especially powerful with image recognition and highly applicable to image-heavy specialties, including ophthalmology. Within neuro-ophthalmology, DL applications can analyze ophthalmic images, including digital fundus photography, visual fields, and optical coherence tomography. DL can assist in automated screening and diagnosis. DL has been utilized to distinguish abnormal optic discs from normal controls, including papilledema and the degree of optic nerve swelling, and to differentiate various forms of non-glaucomatous optic neuropathies [30, 31••, 32–34]. Recently, DL applications were proven to be at least as accurate as expert neuro-ophthalmologists in identifying papilledema [35]. Given the current workforce challenges within neuro-ophthalmology, one can envision a future practice model in which mature DL applications triage screening fundus photographs of referred patients to prioritize the most severe cases of papilledema over mild cases. Additionally, patients with anomalous but normal optic nerves may not even require a referral to neuro-ophthalmology. With direct ophthalmoscopy instruction declining in medical school curricula, many non-ophthalmology-based physicians lack confidence in viewing the fundus [36]. Proven DL applications may support non-ophthalmology-based doctors by funneling patients with potential sight-threatening papilledema to the neuro-ophthalmologist and deferring those with normal optic nerves to comprehensive ophthalmology. Automated DL telescreening is already utilized by non-eye health professionals in diabetic retinopathy screening [37••]. This workflow integrates virtual technologies throughout a patient’s continuum of care: patient visit registration, digital capture of the funduscopic images, DL-guided screening algorithms, and then synchronous video telemedicine to communicate the results to the patient.
Virtual and Augmented Reality
Virtual reality (VR) and its subset, augmented reality (AR), comprise another aspect of digital transformation that will impact Tele-Neuro-Ophthalmology 2.0 [37••]. VR is where the user, via a wrap-around headset, is fully immersed in a virtual environment. VR is used in ophthalmology for patients with visual loss/impairment where an attached camera records the patient’s environment and displays or magnifies that image into the patient’s visible visual field. Safety concerns are a limitation; patients can not see their real environment while ambulating because the headsets are fully occlusive and immersive [37••].
Augmented reality (AR), on the other hand, integrates technology with real life, for example, smartphone language applications projecting translations over the native text. A developing neuro-ophthalmology application of AR is glasses with embedded cameras that can map out a patient’s scotoma or visual field defect, create a custom remapping of the missing images, and overlay that image onto functioning areas of a patient’s vision dynamically, allowing the patient to continue functioning within the real environment [37••, 38]. Other uses of AR include home monitoring units developed for patients with age-related macular degeneration to detect retinal fluid changes with the data then transmitted via the cloud to healthcare providers for interpretation [37••]. These technologies present potential translation opportunities for neuro-ophthalmic patients from a diagnostic monitoring and therapeutic perspective by allowing patients to engage visually with their environment. Additional applications of AR that impact the neuro-ophthalmic surgeon include the development of 3D glasses (heads up surgery) to improve ergonomics and enhance visualization during ophthalmic surgery. This AR technology allows surgeons to view projected operative images directly in front of them, aiding greater maneuverability [37••]. Lastly, VR and AR applications have potential to extend into neuro-ophthalmic medical education by training medical students and residents in pertinent anatomy and surgical techniques through surgical simulators, which have already demonstrated efficacy and validity in improving surgical performance and reducing complication rates. Ophthalmoscopy simulators have also demonstrated efficacy and validity evidence in improving ophthalmoscopy skills in the clinical setting [39].
Conclusions
Telehealth and its applications and adoption within neuro-ophthalmology have accelerated since the pandemic’s onset, fundamentally shifting the delivery of neuro-ophthalmic care permanently. While the potential applications and innovations of digital transformation are exciting, Tele-Neuro-Ophthalmology 2.0 is not without challenges. Much work must be done to validate, adopt, and pay for these technologies. Additionally, challenges remain in protecting patient data privacy, narrowing the digital divide, increasing digital literacy, and securing permanent insurance coverage for telehealth services. Despite these current roadblocks, we are on the cusp of these virtual technologies becoming reality with transformative implications for our visually impaired patients.
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.•• Moss HE, Lai KE, Ko MW. Survey of telehealth adoption by neuro-ophthalmologists during the COVID-19 pandemic: benefits, barriers, and utility. J Neuroophthalmol. 2020;40(3):346–355. 10.1097/WNO.0000000000001051. The first global survey within the field of neuro-ophthalmology to study the benefits, barriers, and utility of tele-neuro-ophthalmology. [DOI] [PMC free article] [PubMed]
- 2.•• Moss HE, Lai KE, Ko MW. Tele-neuro-ophthalmology utilization, availability, and attitudes: update 1 year into the COVID-19 public health emergency. J Neuroophthalmol 2022; in press. 10.1097/WNO.0000000000001663. A follow up survey of the global utilization of tele-neuro-ophthalmology a year into the pandemic. [DOI] [PMC free article] [PubMed]
- 3.• Ko MW, Busis NA. Tele-neuro-ophthalmology: vision for 20/20 and beyond. J Neuroophthalmol. 2020;40(3):378–84. 10.1097/WNO.0000000000001038. This is a comprehensive state-of-the-art review on pre-COVID to early-COVID telehealth in neuro-ophthalmology, with perspectives on the potential applications of tele-neuro-ophthalmology.
- 4.Guzik AK, Switzer JA. Teleneurology is neurology. Neurology. 2020;94(1):16–17. doi: 10.1212/WNL.0000000000008693. [DOI] [PubMed] [Google Scholar]
- 5.Gupta A, Cavallerano J, Sun JK, Silva PS. Evidence for telemedicine for diabetic retinal disease. Semin Ophthalmol. 2017;32(1):22–28. doi: 10.1080/08820538.2016.1228403. [DOI] [PubMed] [Google Scholar]
- 6.Thanos A, Yonekawa Y, Todorich B, Moshfeghi DM, Trese MT. Screening and treatments using telemedicine in retinopathy of prematurity. Eye Brain. 2016;8:147–151. doi: 10.2147/EB.S94440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Telemedicine for Stroke Expanded with Passage of FAST ACT. American Academy of Neurology. Available at: https://www.aan.com/PressRoom/home/PressRelease/1618#:~:text=On%20Friday%2C%20February%209%2C%202018%2C%20President%20Trump%20signed,services%20regardless%20of%20where%20a%20patient%20receives%20treatment. Accessed November 18, 2022.
- 8.President Trump Expands Telehealth Benefits for Medicare Beneficiaries During COVID-19 Outbreak. Centers for Medicare and Medicaid Services. 2020. Available at: https://www.cms.gov/newsroom/press-releases/president-trump-expands-telehealth-benefits-medicare-beneficiaries-during-covid-19-outbreak. Accessed July 13, 2022.
- 9.• Lai KE, Ko MW, Rucker JC, Odel JG, Sun LD, Winges KM, Ghosh A, Bindiganavile SH, Bhat N, Wendt SP, Scharf JM, Dinkin MJ, Rasool N, Galetta SL, Lee AG. Tele-neuro-ophthalmology during the age of COVID-19. J Neuroophthalmol. 2020;40(3):292–304. 10.1097/WNO.0000000000001024. The authors provide practical clinical tips for tele-neuro-ophthalmology implementation. [DOI] [PMC free article] [PubMed]
- 10.Moss HE, Ko MW, Mackay DD, Chauhan D, Gutierrez KG, Villegas NC, Lai KE. The impact of COVID-19 on neuro-ophthalmology office visits and adoption of telemedicine services. J Neuroophthalmol. 2021;41(3):362–367. doi: 10.1097/WNO.0000000000001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.• Kung FF, Xu TT, Leavitt JA, Lossen VI, Lai KE, Ko MW, Bhatti MT, Chen JJ. Characterization and utility of remote interpretation of visual field diagnostic testing in an academic center. J Neuroophthalmol. 2022;42(1):e1–7. 10.1097/WNO.0000000000001481. The authors discuss the utility and efficiency of remote interpretation of visual fields. [DOI] [PubMed]
- 12.Dyrda L, Drees J, Adams K. Becker’s Hospital Review. Will health systems sustain telehealth if pandemic pay rates, coverage drop? Available at: Will health systems sustain telehealth if pandemic pay rates, coverage drop? (beckershospitalreview.com) Accessed January 8, 2022.
- 13.•• Lai KE, Ko MW: Tele-neuro-ophthalmology. In: Maa A, Ocular Telehealth. Philadelphia: Elsevier; 2022. The first textbook on ocular telehealth published in the peri/post-COVID era.
- 14.DeBusk A, Subramanian PS, Scannell Bryan M, Moster ML, Calvert PC, Frohman LP. Mismatch in supply and demand for neuro-ophthalmic care. J Neuroophthalmol. 2022;42(1):62–67. doi: 10.1097/WNO.0000000000001214. [DOI] [PubMed] [Google Scholar]
- 15.• Xu TT, Kung FF, Lai KE, Ko MW, Brodsky MC, Bhatt MT, Chen JJ. Interprofessional electronic consultations for the diagnosis and management of neuro-ophthalmic conditions. J Neuroophthalmol. 2022; in press. 10.1097/WNO.0000000000001643. The authors examine the use of electronic consultation to improve access and efficiency to neuro-ophthalmic care. [DOI] [PubMed]
- 16.• Conway J, Krieger P, Hasanaj L, Sun L, Scharf JM, Odel JG, Dinkin MJ, Oliveira C, Mackay DD, Rasool N, Ko M, Rucker JC, Galetta SL, Balcer LJ. Telemedicine evaluations in neuro-ophthalmology during the COVID-19 pandemic: patient and physician surveys. J Neuroophthalmol. 2021;41(3):356–61. 10.1097/WNO.0000000000001370. This is a pioneering prospective multicenter survey of patient and physician attitudes towards synchronous video telemedicine services in neuro-ophthalmology. [DOI] [PubMed]
- 17.Neurology. www.acgme.org. Available at: https://www.acgme.org/Specialties/Program-Requirements-and-FAQs-and-Applications/pfcatid/37/Neurology Accessed July 27, 2022.
- 18.Ophthalmology. www.acgme.org. Available at: https://www.acgme.org/Specialties/Program-Requirements-and-FAQs-and-Applications/pfcatid/13/Ophthalmology Accessed July 27, 2022.
- 19.NANOS Illustrated Curriculum for Neuro-Ophthalmology. NOVEL. Available at: https://www.tetondata.com/resources/srOnline/Handouts/NANOS_Overview_Handout_STAT!Ref.pdf Accessed July 27, 2022. [DOI] [PubMed]
- 20.Sinsky, Christine (2022) 1 in 5 doctors will leave medicine in the next 2 years Available at: https://www.mcpiqojournal.org/article/S2542-4548(21)00126-0/fulltext Accessed July 20, 2022.
- 21.Pearl, R. (2022) Physician burnout is increasing, Gender Inequality Is Making It Worse Available at: https://www.forbes.com/sites/robertpearl/2022/04/26/physician-burnout-is-increasing-gender-inequality-is-making-it-worse/?sh=288167cc6eab) Accessed July 20, 2022.
- 22.Alkureishi MA, Choo ZY, Lenti G, Castaneda J, Zhu M, Nunes K, Weyer G, Oyler J, Shah S, Lee WW. Clinician perspectives on telemedicine: observational cross-sectional study. JMIR Hum Factors. 2021;8(3):e29690. doi: 10.2196/29690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.HPSA Find. Health Resources and Services Administration. https://data.hrsa.gov/tools/shortage-area/hpsa-find. Accessed November 22, 2022.
- 24.Ko MW, Lai KE, Zimmer-Galler IE, Gold DR, Moss HE. Telemedicine and neuro-ophthalmology: 20/20 in 2020. Neuro-Ophthalmology Virtual Education Library [NOVEL], 2020:259–284. North American Neuro-Ophthalmology Society 46th Annual Meeting; March 9, 2020; Omni Amelia Island Plantation Resort, Amelia Island, FL. Available at: https://novel.utah.edu/collection/NAM/program/20200309_nanos_telemedicine_1/year/2020/.
- 25.Vial G. Understanding digital transformation: a review and a research agenda. J Strateg Inf Syst. 2019;28(2):118–144. doi: 10.1016/j.jsis.2019.01.003. [DOI] [Google Scholar]
- 26.Tan TF, Li Y, Lim JS, Gunasekeran DV, Teo ZL, Ng WY, Ting DS. Metaverse and virtual health care in ophthalmology: opportunities and challenges. Asia Pac J Ophthalmol (Phila) 2022;11(3):237–246. doi: 10.1097/APO.0000000000000537. [DOI] [PubMed] [Google Scholar]
- 27.McCarthy J, Minsky ML, Rochester N, Shannon CE. A Proposal for the Dartmouth Summer Research Project on Artificial Intelligence, August 31, 1955. AI Mag. 2006;27(4):12. doi: 10.1609/aimag.v27i4.1904. [DOI] [Google Scholar]
- 28.IBM Cloud Learn Hub. What is machine learning? Available at: https://www.ibm.com/cloud/learn/machine-learning Accessed August 19, 2022.
- 29.IBM Cloud Learn Hub. What is deep learning? Available at: https://www.ibm.com/cloud/learn/deep-learning Accessed August 19, 2022.
- 30.Liu TYA, Wei J, Zhu H, Subramanian PS, Myung D, Yi PH, Hui FK, Unberath M, Ting DSW, Miller NR. Detection of optic disc abnormalities in color fundus photographs using deep learning. J Neuroophthalmol. 2021;41(3):368–374. doi: 10.1097/WNO.0000000000001358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.•• Milea D, Najjar RP, Zhubo J, Ting D, Vasseneix C, Xu X, Aghsaei Fard M, Fonseca P, Vanikieti K, Lagrèze WA, La Morgia C, Cheung CY, Hamann S, Chiquet C, Sanda N, Yang H, Mejico LJ, Rougier M-B, Kho R, Thi Ha Chau T, Singhal S, Gohier P, Clermont-Vignal C, Cheng C-Y, Jonas JB, Yu-Wai-Man P, Fraser CL, Chen JJ, Ambika S, Miller NR, Liu Y, Newman NJ, Wong TY, Biousse V; BONSAI Group. Artificial intelligence to detect papilledema from ocular fundus photographs. N Engl J Med. 2020 Apr 30;382(18):1687–1695. 10.1056/NEJMoa1917130. This is a seminal, global, multi-center study examining the use of AI to detect papilledema from fundus photographs. [DOI] [PubMed]
- 32.Vasseneix C, Najjar RP, Xu X, Tang Z, Loo JL, Singhal S, Tow S, Milea L, Ting DSW, Liu Y, Wong TY, Newman NJ, Biousse V, Milea D; BONSAI Group. Accuracy of a deep learning system for classification of papilledema severity on ocular fundus photographs. Neurology. 2021;97(4):e369-e377. 10.1212/WNL.0000000000012226. [DOI] [PMC free article] [PubMed]
- 33.Yang HK, Kim YJ, Sung JY, Kim DH, Kim KG, Hwang JM. Efficacy for differentiating nonglaucomatous versus glaucomatous optic neuropathy using deep learning systems. Am J Ophthalmol. 2020;216:140–146. doi: 10.1016/j.ajo.2020.03.035. [DOI] [PubMed] [Google Scholar]
- 34.Lee J, Kim JS, Lee HJ, Kim SJ, Kim YK, Park KH, Jeoung JW. Discriminating glaucomatous and compressive optic neuropathy on spectral-domain optical coherence tomography with deep learning classifier. Br J Ophthalmol. 2020;104(12):1717–1723. doi: 10.1136/bjophthalmol-2019-314330. [DOI] [PubMed] [Google Scholar]
- 35.Biousse V, Newman NJ, Najjar RP, Vasseneix C, Xu X, Ting DS, Milea LB, Hwang JM, Kim DH, Yang HK, Hamann S, Chen JJ, Liu Y, Wong TY, Milea D; BONSAI (Brain and Optic Nerve Study with Artificial Intelligence) Study Group. Optic Disc Classification by Deep Learning versus Expert Neuro-Ophthalmologists. Ann Neurol. 2020;88(4):785–795. 10.1002/ana.25839. [DOI] [PubMed]
- 36.Mackay DD, Garza PS, Bruce BB, Newman NJ, Biousse V. The demise of direct ophthalmoscopy: a modern clinical challenge. Neurol Clin Pract. 2015;5(2):150–157. doi: 10.1212/CPJ.0000000000000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.•• Li JO, Liu H, Ting DSJ, Jeon S, Chan RVP, Kim JE, Sim DA, Thomas PBM, Lin H, Chen Y, Sakomoto T, Loewenstein A, Lam DSC, Pasquale LR, Wong TY, Lam LA, Ting DSW. Digital technology, tele-medicine and artificial intelligence in ophthalmology: a global perspective. Prog Retin Eye Res. 2021;82:100900. 10.1016/j.preteyeres.2020.100900. The authors have written an extensive, forward-thinking review on the impact of digital transformation and its applications to the field of ophthalmology. [DOI] [PMC free article] [PubMed]
- 38.Sayed AM, Kashem R, Abdel-Mottaleb M, Roongpoovapatr V, Eleiwa TK, Abdel-Mottaleb M, Parrish RK, 2nd, Abou SM. Toward improving the mobility of patients with peripheral visual field defects with novel digital spectacles. Am J Ophthalmol. 2020;210:136–145. doi: 10.1016/j.ajo.2019.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ong CW, Tan MCJ, Lam M, Koh VTC. Applications of extended reality in ophthalmology: systematic review. J Med Internet Res. 2021;23(8):e24152. doi: 10.2196/24152. [DOI] [PMC free article] [PubMed] [Google Scholar]