Abstract
Background
Immune-based therapies are standard-of-care treatment for coronavirus disease 2019 (COVID-19) patients requiring hospitalization. However, safety concerns related to the potential risk of secondary infections may limit their use.
Methods
We searched OVID Medline, Ovid EMBASE, SCOPUS, Cochrane Library, clinicaltrials.gov, and PROSPERO in October 2020 and updated the search in November 2021. We included randomized controlled trials (RCTs). Pairs of reviewers screened abstracts and full studies and extracted data in an independent manner. We used RevMan to conduct a meta-analysis using random-effects models to calculate the pooled risk ratio (RR) and 95% CI for the incidence of infection. Statistical heterogeneity was determined using the I2 statistic. We assessed risk of bias for all studies and rated the certainty of evidence using the Grading of Recommendations Assessment, Development, and Evaluation methodology. We conducted a meta-regression using the R package to meta-explore whether age, sex, and invasive mechanical ventilation modified risk of infection with immune-based therapies. The protocol is registered with PROSPERO (CRD42021229406).
Results
This was a meta-analysis of 37 RCTs including 32 621 participants (mean age, 60 years; 64% male). The use of immune-based therapy for COVID-19 conferred mild protection for the occurrence of secondary infections (711/15 721, 4.5%, vs 616/16 900, 3.6%; RR, 0.82; 95% CI, 0.71–0.95; P = .008; I2 = 28%). A subgroup analysis did not identify any subgroup effect by type of immune-based therapies (P = .85). A meta-regression revealed no impact of age, sex, or mechanical ventilation on the effect of immune-based therapies on risk of infection.
Conclusions
We identified moderate-certainty evidence that the use of immune-based therapies in COVID-19 requiring hospitalization does not increase the risk of secondary infections.
Keywords: COVID-19, immunotherapy, secondary infection
The optimal management of coronavirus disease 2019 (COVID-19) has evolved with our understanding of the disease pathophysiology. Earlier in the pandemic, treatment focused on medications with antiviral properties, with formal recommendation against the routine use of systemic corticosteroids for COVID-19. This stemmed not only from prior data demonstrating lack of benefit in terms of mortality, length of hospitalization, and intensive care unit admission, but also from increased rates of adverse effects with the use of corticosteroids for severe Middle East respiratory syndrome coronavirus (MERS-CoV), severe acute respiratory syndrome (SARS), and COVID-19 [1, 2]. Moreover, corticosteroids increased the risk of secondary infections in hospitalized patients with influenza [3].
As the COVID-19 pandemic progressed, evidence suggested that an aberrant immune response is the key contributor to severe COVID-19. Consequently, immune-based therapies such as corticosteroids, tocilizumab (interleukin-6 inhibitor), and baricitinib (Janus Kinase inhibitor) were studied further for treatment of severe COVID-19. Furthermore, based on data showing a survival benefit of some of the immune-based therapies, their use is now supported by consensus guidelines [4].
As immune-based therapies are now the standard of care for treatment of severe COVID-19, the theoretical increased risk of hospital-acquired infections, especially in critically ill ventilated patients, is a matter of concern. The increased risk of secondary infections with the use of immune-based therapies is supported by the available evidence on their safety for the treatment of inflammatory disorders, mainly rheumatologic conditions, when compared with standard of care or placebo [5], but their impact in COVID-19 has not been appropriately rigorously evaluated.
The objective of this systematic review and meta-analysis was to assess the risk of secondary infections with the use of immune-based therapies in patients hospitalized with COVID-19.
METHODS
We registered the protocol for this systematic review and meta-analysis on the PROSPERO database (CRD42021229406), and the report was made following the guidelines from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; checklist included in Supplementary Data B) [6].
Eligibility Criteria
We included peer-reviewed randomized controlled trials (RCTs) published between January 2020 and November 2021 and excluded nonrandomized studies (NRS) and non-peer-reviewed manuscripts (eg, published in preprint servers), meeting abstracts, and thesis dissertations. RCTs including adult participants (≥18 years of age), diagnosed with reverse transcription polymerase chain reaction or antigen testing, and hospitalized with COVID-19 were included if they received immune-based therapy and were compared with participants who did not receive these treatments (received either placebo, standard of care, or antiviral therapy). We excluded studies evaluating interventions with no effect on the immune system such as antivirals, vaccines, passive antibodies, and traditional Chinese herbal remedies without immune-based therapies. Studies allowing co-treatment with other immune-based therapies were included if these co-treatments were administered in both experimental and control arms. The primary outcome of interest was the rate of secondary infections, defined as infections occurring after initiation of interventions for the management of COVID-19.
Information Sources
A search was executed by an expert searcher/librarian (S.C.) on OVID Medline, Ovid EMBASE, SCOPUS, Cochrane Library, and PROSPERO using controlled vocabulary (eg, MeSH, Emtree, etc.) and keywords representing the concepts “COVID-19” and “immunotherapies” and “outcomes including secondary infections.” Prognostic hedges from the McMaster Health Information Research Unit were applied to the EMBASE and Medline searches [7]. Searches were adjusted appropriately for different databases. Searches were conducted in October 2020 and updated on November 9, 2021. Update searches were limited to randomized controlled trials using RCT filters [8, 9]. No other limits were applied. Results (10 576) were exported to the COVIDence systematic review system. Duplicates (3413) were removed in COVIDence. Detailed search strategies are available in Appendix 1 in Supplementary Data C.
Study Selection
Using the web-based systematic review software COVIDence, pairs of reviewers (D.K., A.S., K.L., B.W.) independently screened all titles and abstracts, followed by full texts of potentially eligible articles. A third reviewer (C.C.) resolved conflicts. We performed training and a calibration exercise before each step.
Data Collection
Following training and calibration exercises, full data extraction was performed by 2 independent reviewers (D.K., A.S., K.L., B.W., M.R.). Data elements collected included: demographics and methodology for each study (country of the study, study size, year of the study, number of centers, funding source, trial registration numbers if applicable, and the study design), patient characteristics (age, sex, diabetes, body mass index, immunosuppression), setting, severity of COVID-19 (percentage requiring oxygen and mechanical ventilation), method of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection diagnosis, intervention details (immune-based therapy used, including route, dosing, treatment duration, and concomitant immune-based therapies), and all secondary infections reported in the outcomes (proportion of patients with bacteremia, pneumonia, urinary tract infection, sepsis, septic shock, invasive fungal infection, and viral infections). The definition used in each trial for secondary infection is listed in Supplementary Table 1. Time to infection was not collected as this information was missing from most studies.
Risk of Bias Assessment
To assess bias in randomized controlled trials, we used the Cochrane risk-of-bias tool for randomized trials, which includes selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. Each study was individually assessed by a minimum of 2 separate investigators, with any discrepancies resolved by an experienced senior investigator. Furthermore, a collective calibration exercise and training were provided before independent assessment of study biases. We used robvis (Risk Of Bias VISualization) to create the risk-of-bias plots [10].
Data Synthesis
Due to the heterogeneity among the studies in terms of study design and comparators, we used a random-effects model when conducting the meta-analyses. The primary analysis was the incidence of secondary infection in each group. Each outcome (including total infection, pneumonia, bacteremia, invasive fungal infection, sepsis, and septic shock) was analyzed separately. In studies that did not outline total infection in the RCT, we calculated the variable by adding different infectious syndromes with the exception of sepsis and septic shock. The unit of analysis was based on the aggregated outcome of secondary infections, as access to individual patient data was unavailable. Dichotomous data were analyzed using risk ratio (RR) with 95% CI. The weight in each trial was calculated using RevMan and represents the inverse of the variance (the square of the standard error) of the trial's summary statistic. This relates closely to the sample size and the number of events in each trial. Nonquantifiable data were narratively described. Statistical heterogeneity was determined using the I2 statistic to assess the appropriateness of performing a meta-analysis and was categorized as (1) 0%–40%, might not be important; (2) 30%–60%, moderate heterogeneity; (3) 50%–90%, substantial heterogeneity; 75%–100%, considerable heterogeneity. The statistical software RevMan 5.31 (The Cochrane Collaboration) was used to calculate and combine each outcome.
We screened for clinical trial registration on the international clinical trials registry platform of the World Health Organization (http://apps.who.int/trialssearch). Publication biases were evaluated using a funnel plot (Figure 12 in Supplementary Data A).
Moderator and Sensitivity Analysis
To try to explain potential sources of heterogeneity, we performed subgroup analysis according to the different drugs used in these clinical trials. In addition, and although we predefined 3 subgroup analyses in our protocol (age, severity of illness, and immunosuppression), we used meta-regression to explore the potential impact of age and invasive mechanical ventilation as a surrogate of severity of illness on the (log) RR of infection with immune-based therapies. For the meta-regression, we conducted the analysis using the R package meta [11]. We could not perform a subgroup analysis on immunosuppression as most RCTs excluded these patients.
To assess the impact of potential publication-related confounding factors on the overall outcome, we used a sensitivity analysis. More specifically, we omitted studies with high rates of participant attrition, other missing data, and those judged to have high risks of bias. Furthermore, a sensitivity analysis was also conducted excluding studies where total infection was calculated or only infection leading to death was presented.
Certainty of the Evidence
We used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) working group methodology to assess the certainty of evidence across the domains of risk of bias: consistency, directness, precision, outcome, and publication bias [12].
RESULTS
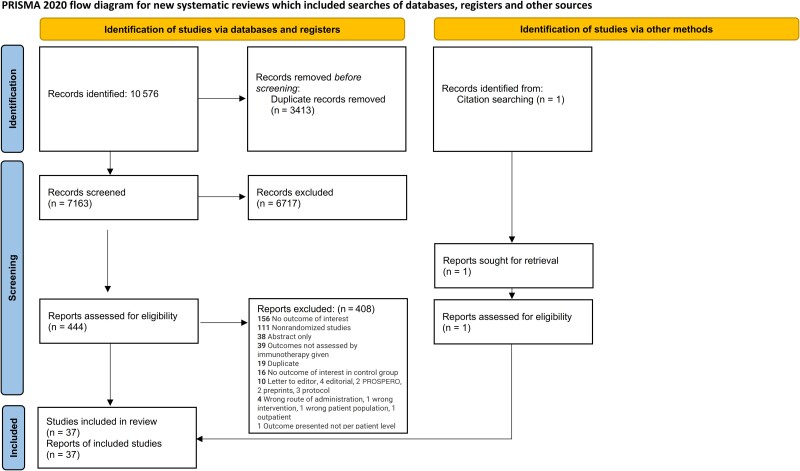
After screening 7163 titles and abstracts and 444 full texts published between January 2020 and November 8, 2021, we identified 37 RCTs that fulfilled our eligibility criteria (Figure 1). The characteristics of the RCTs are summarized in Table 1 and Table 1 in Supplementary Data A.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart.
Table 1.
Characteristics of Patients and Interventions Used in Randomized Clinical Trials
| Author-Year Trial Name | Design and Setting | Participants | Intervention Dose/Route and Duration | SOC | Co-intervention (%) | Outcomes |
|---|---|---|---|---|---|---|
| Salama 2021 EMPACTA |
Double-blind Multicenter |
I: 249, C: 128 |
Tocilizumab IV 8 mg/kg 1–2 doses |
Antiviral RDV: I: 131 (52.6), C: 75 (58.6) |
Steroids I: 200 (80.3), C: 112 (87.5) |
Total infection: I: 25/250, C: 16/127 |
| Stone 2020 BACC Bay Tocilizumab |
Double-blind Multicenter |
I: 161, C: 81 |
Tocilizumab IV 8 mg/kg (max 800 mg), 1 dose | Antiviral, HCQ RDV: I: 53 (33), C: 24 (29) | Steroids: I: 18 (11%), C: 5 (6%) | Total infection: I: 13/161, C: 14/82 |
| Veiga 2021 | Open-label Multicentre |
I: 65, C: 64 |
Tocilizumab IV 8 mg/kg (max 800 mg), 1 dose | HCQ, AZM, antibiotics | Steroids: I: 45 (69), C: 47 (73) | Total infection: I: 10/65, C: 10/64 |
| Salvarani 2021 | Open-label Multicenter |
I: 60, C: 66 |
Tocilizumab IV 8 mg/kg (max 800 mg), 2 doses | Varied as per treatment protocol of each center | Steroids: I: 7 (11.7), C: 5 (8.3) | Total infection: I: 1/6°C: 2/63 |
| Hermine 2021 CORIMUNO-TOCI1 |
Open-label Multicenter |
I: 63, C: 67 |
Tocilizumab 8 mg/kg (1st dose); 400 mg (2nd dose), 1 or 2 doses |
AZM, HCQ, LPV/r, LPV, RDV, oseltamivir | Steroids: I: 21 (33), C: 41 (61) Anakinra: I: 1 (2), C: 3 (4.4) Eculizimab: I: 0, C: 1 (1.6) |
Total infection: I: 2/63, C: 14/67 |
| Dequin 2020 CAPE-COD |
Double-blind Multicenter |
I: 76, C: 73 |
Hydrocortisone IV 200 mg/d × 7 d, 100 mg/d × 4 d, 50 mg/d × 3 d | HCQ, AZM, LPV/r, RDV | Tocilizumab: I: 1 (1.3), C: 2 (2.7) Eculizumab: I: 3 (3.9), C: 2 (2.7) |
Total infection: I: 28/76, C: 30/73 |
| Angus 2020 REMAP-CAP |
Open-label Multicenter |
I: 278, C: 101 |
Hydrocortisone IV 50 mg q6 h, 7 d or shock resolved, vasopressors off 24 h, max 28 d | … | … | Total infection: I: 1/278, C: 0/101 |
| Edalatifard 2020 | Single-blind Multicenter |
I: 34, C: 24 |
Methylprednisolone IV 250 mg/d × 3 d (3 doses) | HCQ, LPV, naproxen | … | Total infection: I: 1/34, C: 0/28 |
| Tomazini 2020 Codex |
Open-label Multicentre |
I: 151, C: 148 |
Dexamethasone IV 20 mg × 5 d; then 10 mg × 5 d 10 doses | AZM, antibiotics, HCQ | Steroids: C: 52 (35.1) | Total infection: I: 33/151, C: 43/148 |
| Jeronimo 2020 MetCOVID |
Double-blind Single-center |
I: 199, C: 194 |
Methylprednisolone IV: 0.5 mg/kg BID × 5 d 10 doses |
Antibiotics | … | Total infection: I: 9/108, C: 7/88 |
| Corral-Gudino 2021 GLUCOCOVID |
Open-label Multicentre |
I: 35, C: 29 |
Methylprednisolone IV 40 mg BID × 3 d, then 20 mg BID × 3 d 12 doses | Antibiotics, AZM, HCQ, LPV/r | … | Total infection: I: 5/35, C: 1/29 |
| Vlaar 2020 PANAMO |
Open-label Multicentre |
I: 15, C: 15 |
Anti-C5a Ab (IFX-1) IV 800 mg up to 7 doses | HCQ | … | Total infection: I: 3/15, C: 4/15 |
| Rahmani 2020 | Open-label Single-center |
I: 33, C: 33 |
Interferon SQ B-1b 250 mcg every 2nd day for 2 wk | LPV/r or ATV/r, HCQ | Steroids: I: 5 (15.15), C: 9 (27.27) | Total infection: I: 1/33, C: 5/33 |
| Davoudi-Monfared 2020 | Open-label Single-center |
I: 42, C: 39 |
Interferon B-1a 44 mcg/mL SQ (12 MIU/mL) 3x/wk for 2 wk | HCQ, LPV/r, ATV/r | Steroids: I: 26 (61.9), C: 17 (43.58) | Total infection: I: 11/42, C: 5/39 |
| Kalil 2020 ACTT-2 |
Double-blind Multicenter |
I: 515, C: 518 |
Barcitinib: PO 4 mg/d × 14 d or until d/c, RDV IV 200 mg × 1 d, then 100 mg × 9d or until d/c | RDV: 200 mg × 1 d, then 100 mg × 9 d or until discharge | Steroids: I: 87 (16.9), C: 104 (20) | Total infection: I: 30/515, C: 57/518 |
| Cao 2020 | Single-blind Multicenter |
I: 20, C: 21 |
Ruxolitinib PO 5 mg BID 56 doses |
Antivirals, antibiotics Placebo: Vit C PO BID 56 doses |
Steroids: I: 14 (70), C: 15 (71.4) | Total infection: I: 0/2°C: 2/21 |
| Lopes 2021 | Double-blind Single-center |
I: 38, C: 37 |
Colchicine 0.5 mg TID × 5 d then 0.5 mg BID × 5 d | AZM, HCQ, UHeparin | Steroids: I: 25 (69), C: 24 (67) | Total infection: I: 3/36, C: 5/36 |
| Caballero-Bermejo 2021 SARTRE |
Open-label Multicentre |
I: 99, C: 102 |
Sarilumab 200 mg IV × 1 or 400 mg IV × 1 if >75 kg | Antibiotics, antivirals, anticoagulants | Steroids: I: 99 (100), C: 102 (100) | Total infection: 1: 1/99, C: 3/102 |
| Soin 2021 COVINTOC |
Open-label Multicentre |
I: 91, C: 89 |
Tocilizumab 6 mg/kg IV (max 480 mg) + another dose >12 h prn | RDV: I: 31 (43), C: 36 (41) | Steroids: I: 83 (91), C: 80 (91) | Total infection: I: 6/91, C: 5/89 |
| Kyriazopoulou 2021 SAVE- MORE |
Double-blind Multicentre |
I: 405, C: 189 |
Anakinra 100 mg SC daily × 7–10 d | RDV: I: 298 (73), C: 141 (74.6) LMWH, antibiotics |
Steroids: I: 342 (84.4), C: 168 (88.9) | Total infection: I: 34/405, C: 30/189 |
| Caricchio 2021 CAN-COVID |
Double-blind Multicenter |
I: 224, C: 223 |
Canakinumab 450–750 mg IV × 1 | Convalescent plasma, antivirals, anticoagulants RDV: I: 49 (22), C: 45 (20) |
Steroids: I: 92 (41), C: 73 (32) Tocilizumab: I 5 (2.2), C: 20 (8.8) Anakinra: I: 2 (1) |
Total infection: I: 23/225, C: 43/223 |
| Mariette 2021 CORIMUNO-ANA-1 |
Open-label Mulicenter |
I: 59, C: 55 |
Anakinra: 200 mg IV BID × 3 d then EITHER 100 mg IV BID × 1 d then 100 mg IV QD × 1 d OR if necessary 400 mg × 3 d then 200 mg × 1 d then 100 mg × 1 d | Antibiotics, antivirals, anticoagulants | Steroids: I: 30 (51), C: 29 (53) Tocilizumab: I: 1 (2) C: 0 (0) |
Total infection: I: 11/59, C: 4/55 |
| Guimaraes 2021 STOP-COVID |
Double-blinded Multicentre |
I: 144, C: 145 |
Tofacitinib: PO 10 mg BID × 14 d | Antibiotics, anticoagulants, antivirals | Steroids: I: 128 (88.9), C: 130 (89.7) | Total infection: I: 7/142, C: 8/142 |
| Kumar 2021 | Open-label Multicentre |
I: 22, C: 10 |
Itolizumab: IV 1.6 mg/kg + if deemed necessary IV 0.8 mg/kg weekly up to total of 4 doses | Antibiotics, HCQ, antivirals, LMWH, and vitamin supplements | Hydrocortisone 100 mg + pheniramine 30 mg IV: I: 22 (100), C: 0 (0), steroids | Total infection: I: 1/22, C: 3/10 |
| Rosas 2021 | Double-blinded Multicentre |
I: 434, C: 215 |
Tocilizumab: IV 8 mg/kg + if necessary a second 8 mg/kg | Antibiotics RDV: I: 434 (100), C: 213 (100) |
Low-dose corticosteroids | Total infection: I: 131/429, C: 71/213 |
| Aman 2021 | Double-blind Multicentre |
I: 197, C: 188 |
Imatinib PO: 800 mg × 1 d then 400 mg × 9 d | Anticoagulants, antibiotics RDV: I: 40 (20), C: 40 (21) |
Steroids: I: 143 (73), C: 133 (71) | Total infection: I: 12/197, C: 16/188 |
| Tang 2021 | Single -blind Multicenter |
I: 43, C: 43 |
Methylprednisolone 1 mg/kg | Antivirals, antibiotics, immunoglobulin | … | Total infection: I: 2/43, C: 1/43 |
| Kalil 2021 ACTT-3 |
Double-blinded Multicentre |
I (RDV + IFN): 487 C (RDV): 482 |
44 μg interferon beta-1a sc q2d × 4 doses RDV (all pts): 200 mg IV × 1, 100 mg IV × 9 d | … | Steroids | Total infection: I: 5/477, C: 3/468 |
| REMAP-CAP Investigators 2021 | Open-label Multicenter |
I (toci): 353 (29% 2 doses), I (sari): 48, C: 402 |
Toci: 8 mg/kg IV (max 800) over 1 h, could be repeated 12–24 h later Sari: 400 mg IV once only |
Immunoglobulin, antivirals, anticoagulation RDV: T: 107/341 (31.4), S: 21/48 (43.8), C: 133/389 (34.2) |
Steroids: T: 252/272 (92.7), S: 46/48 (95.8), C: 293/312 (93.9) |
Total infection: Toc: 1/353, Sari: 0, C: 0 |
| Lomakin 2021 | Double-blind Multicenter |
I: 103, C: 103 |
LVL 324 mg sq + single open-label LVL 324 mg rescue therapy |
Antibiotics, HCQ, anticoagulants | Steroids: I: 5/103 (4.9), C: 10/103 (9.7) |
Total infection: I: 1/103, C: 1/101 |
| Cremer 2021 MASH-COVID |
Double-blind Multicenter |
I: 21, C: 19 |
Mavrilimumab 6 mg/kg | Antivirals, antimicrobials, convalescent plasma RDV: I: 18 (85), C: 15 (79) |
Steroids: I: 16 (76), C: 15 (79) | Total infection: I: 2/21, C: 1/19 |
| Marconi 2021 COV-BARRIER |
Double-blind Multicenter |
I: 764, C: 761 |
4 mg/d oral baricitinib × 14 d or until discharge, 2 mg if GFR <30 | RDV: I: 18% (140/762), C: 19% (147/756) |
Steroids: I: 612/762 (80), C: 592/756 (78) | Total infection: I: 119/750, C: 123/752 |
| Recovery 2 | Open-label Multicenter |
I: 5610, C: 5730 |
Colchicine 1 mg, then 500 μg 12 h later, then 500 μg po/NG q12h × 10 d or until d/c dose adjusted for wt and GFR | RDV: I: 1235/5610 (22), C: 1251/5730 (22) |
Steroids: I: 5243/5610 (93), C: 5360 (94) |
Infection as cause of death: I: 6/5610, C: 2/5730 |
| Recovery 1 | Open-label Multicenter |
I: 2104, C: 4321 |
Dexamethasone: 6 mg oral or IV daily × 10 d (or until d/c) | Antibiotics, LPV/RTV <1% HCQ: I: 1 (16), C: 1 (24) RDV: I: <1 (2), C: 0 |
Steroids: I: 95, C: 8 IL-6 inhibitors: I: 2 (45), C: 3 (132) |
Infection as cause of death: I: 6/2104, C: 9/4321 |
| Lescure 2021 | Double-blind Placebo-controlled Multicenter |
I: 173 + 159, C: 84 |
Sarilumab IV 400 mg or Sarilumab IV 200 mg second dose could be given |
Antivirals, antibacterials, HCQ, CQ | Steroids: I: 200 mg 25 (16), I: 400 mg 42 (24), C: 16 (19) | Total infection: I: 40/332 (12), C: 10/84 (12) |
| Rosas 2021 COVACTA |
Double-blind Placebo-controlled Multicenter |
I: 294, C: 144 |
Tocilizumab IV 8 mg/kg × 1 and second dose could be given 8–24 h after | Antiviral treatment, low-dose glucocorticoids, convalescent plasma | Steroids: I: 57 (19.4), C: 41 (28.5) | Total infection: I: 126/295 (42.7), C: 62/143 (43.4) |
| Recovery 3 | Open-label Multicenter |
I: 2022, C: 2094 |
Tocilizumab IV 400–800 mg; a second dose could be given 12–24 h later | SOC evolved over the study | Steroids: I: 82%, C: 82% | Infections as cause of death: I: 2022, C: 6/2094 |
Abbreviations: ATV/r, atazanavir/ritonavir; AZM, azithromycin; C, control; CQ, Chloroquine; GFR, glomerular filtration rate; HCQ, hydroxychloroquine; I, intervention; IV, intravenous; LPV/r, lopinavir/ritonavir; LVL, levilimab; RDV, remdesivir; RTV, ritonavir; SOC, standard of care; wt, wild-type.
The immune-based therapies used in the RCTs consisted of corticosteroids in 8 studies [13–20], tocilizumab in 10 [21–30], interferon in 3 [31–33], sarilumab in 3 [21, 34, 35], baricitinib in 2 [36, 37], anakinra in 2 [38, 39], colchicine in 2 [40, 41], ruxolitinib in 1 [42], tofacinib in 1 [43], imatinib in 1 [44], levilimab in 1 [45], mavrilimumab in 1 [46], itolizumab in 1 [47], canakinumab in 1 [48], and vilobelimab in 1 [49]. Most RCT protocols were registered online (36/37, 97%). A total of 32 621 subjects were randomized (15 721 to immunotherapy and 16 900 to standard of care or placebo). The participant's mean age (SD, range) was 60 (3.9, 49–70) years, and 64% were male. In most RCTs, participants with moderate to severe COVID-19 were randomized to immune-based therapies vs placebo or standard of care, while in 11 RCTs [20, 22, 28, 30, 33, 36, 37, 40, 41, 43, 45, 50], patients who did not require oxygen supplementation were also included. At the time of randomization, 19 RCTs [13, 15, 17–24, 28–31, 35, 41, 49–51] had patients who required invasive mechanical ventilation with or without extracorporeal membrane oxygenation (ECMO). Concurrent treatment with steroids and antivirals varied between trials (Table 1).
Risk of Bias in Included Studies
The Supplementary Data contains the assessment of risk of bias for RCTs. Eleven studies were judged low risk in all domains (Aman, Dequin, Guimaraes, Jeronimo, Kalil, Lescure, Marconi, Rosas 2021a 2021b, Salama, and Stone), 13 studies were open-label and were judged high risk in the domain of blinding (Angus, Cao, Corral-Gudino, Caballero-Bermejo, Mariette 3 Recovery, REMAP CAP investigators, Salvarani, Soin, Tomazini, and Veiga), 3 had either a physician or statistician unblinded (Carchio, Kalil 2021, Tang), and 6 had high risk of bias in several domains (Davoudi-Monfared, Edalatifard, Hermine, Rahmani, Kumar, and Vlaar) (Table 2; Figure 9 in Supplementary Data A).
Risk of Total Infections With Immune-Based Therapy
Out of the 37 RCTs included in this systematic review, 22 collected total infection as a secondary outcome or adverse effect (Cao, Caricchio, Caballero-Bermejo, Davoudi-Monfared, Dequin, Edalatifard, Guimaraes, Kalil 2020, Kyriazopoulou, Kumar, Lescure, Marconi, Rahmani, Rosas 2021a, 2021b, Salama, Salvarini, Stone, Soin, Tomazini, Veiga, and Vlaar). In the RECOVERY trials, infection was included as a cause of death. Hermine et al. presented infection outcomes as bacterial sepsis, fungal sepsis, and viral sepsis, and Mariette et al. presented infection outcomes as bacterial and fungal sepsis, which we combined to get total infection. Angus et al. presented only invasive fungal infection, which we included as total infection. Cremer et al., Lopes et al., and Tang et al. presented only pneumonia, which we included as total infection. The REMAP-CAP investigators presented bacterial infection, which we included as total infection. Lomakin presented opportunistic infection, which we included as total infection. In the trial by Aman et al., we included lip infection, lung infection, and other as total infection and analyzed sepsis separately. In the trial Khalil et al. (2021), we included cellulitis, bacterial pneumonia, and Aspergillus as total infection and analyzed sepsis and septic shock separately. In the trial by Jerenimo et al., we included bacteremia as total infection and analyzed sepsis separately. Finally, for the trial by Corral-Gudino et al., we combined pneumonia and invasive fungal infections as total infection.
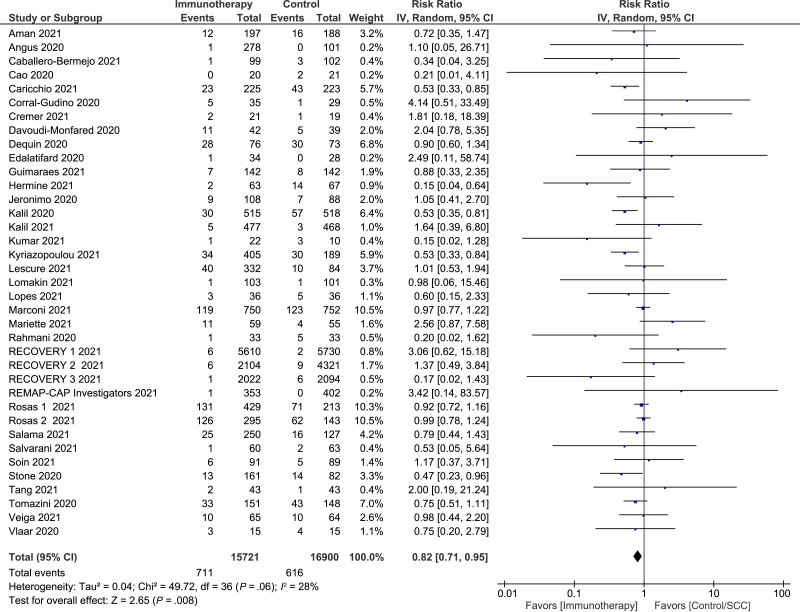
There were 711 infections identified in 15 721 patients receiving immune-based therapy (4.5%) and 616 infections in 16 900 patients receiving placebo or standard of care (3.6%). Based on a random-effects meta-analysis, the summary RR was 0.82 (95% CI, 0.71–0.95; P = .008). There was little inconsistency between the trial results (I2 = 28%; Pheterogeneity = .06) (Figure 2).
Figure 2.
Risk of infection with immune-based therapy in randomized controlled trials.
We performed a subgroup analysis using immunotherapy mostly used in clinical practice in the management of COVID-19 including only steroids, tocilizumab, and baricitinib. There were 550 infections identified in 11 389 patients receiving immune-based therapy (4.8%) and 464 infections in 10 854 patients receiving placebo or standard of care (4.3%). Based on a random-effects meta-analysis, the summary RR was 0.85 (95% CI, 0.72–0.99; P = .04). There was little inconsistency between the trial results (I2 = 26%; Pheterogeneity = .03).
Influence of Drug Type, Age, Sex, and Need for Invasive Mechanical Ventilation in RCTs
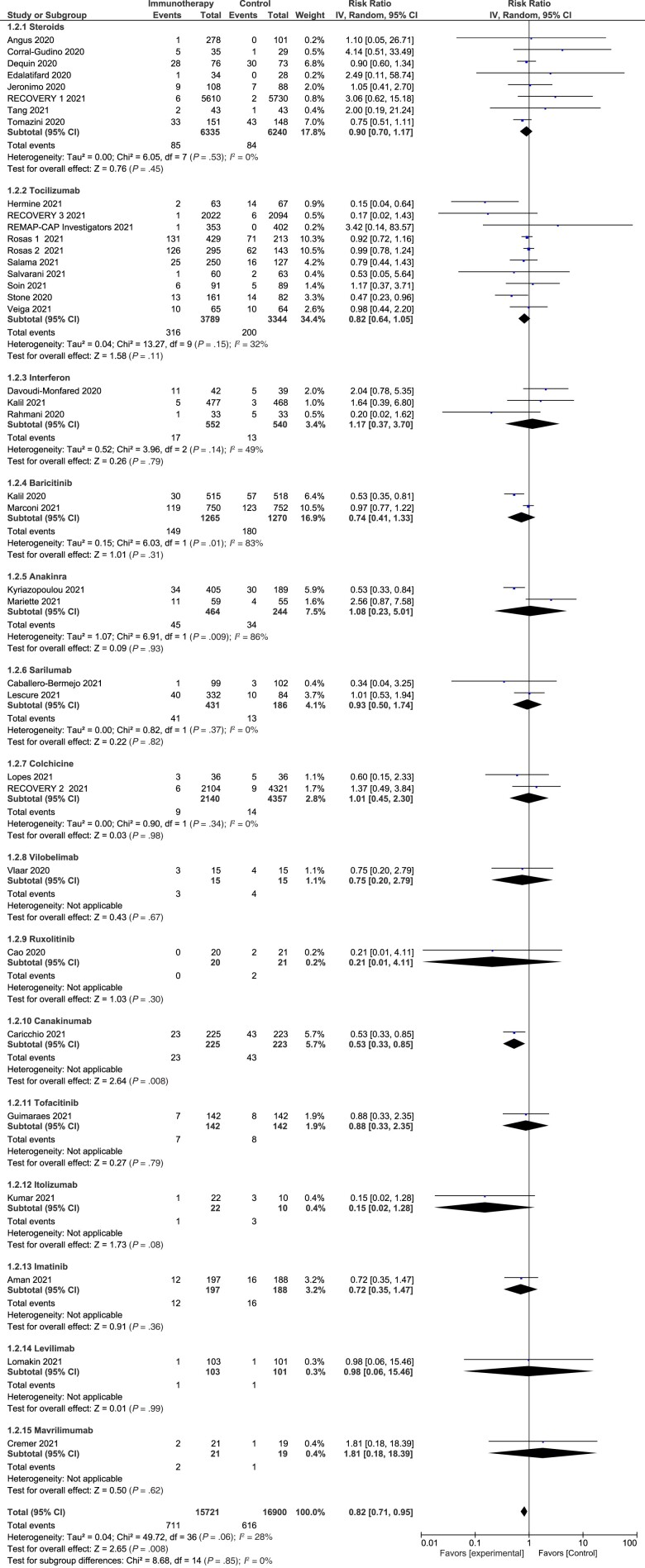
We explored subgroup analysis by immune-based drugs and found no significant difference (P = .85; I2 = 0%) (Figure 3). Meta-regression revealed no impact of age, percentage of female sex, or percentage of participants on mechanical ventilation on the effect of immune-based therapies on the risk of infection (Figures 6, 7, and 8 in Supplementary Data A).
Figure 3.
Risk of infection with different immune-therapeutic agents in randomized controlled trials.
Sensitivity Analysis
By omitting studies with high rates of participant attrition or other missing data or studies that were judged to be at high risk of bias (Davoudi-Monfared, Edalatifard, Hermine, Rahmani, Kumar, and Vlaar), the summary RR remained in favor of immune-based therapy (RR, 0.84; 95% CI, 0.74–0.95; P = .0040) (Figure 10 in Supplementary Data A). Moreover, when omitting studies where the total number of infections was calculated or only infections leading to death were included (Angus, Aman, Corral-Gudino, Cremer, Hermine, Jeronimo, Kalil 2021, Lomakin Lopes, Mariette, RECOVERY 1, 2, 3, REMAp-CAP, Tang), the results were not altered (RR, 0.80; 95% CI, 0.69–0.92; P = .002) (Figure 11 in Supplementary Data A).
Risk of Pneumonia, Bacteremia, Invasive Fungal Infection, Sepsis, and Septic Shock With Immune-Based Therapy in RCTs
Twenty trials assessed the risk of secondary pneumonia in hospitalized patients with COVID-19 treated with immune-based therapy, and based on a random-effects meta-analysis, the summary RR was 0.70 (95% CI, 0.53–0.93; P = .01). There was little inconsistency between the trial results (I2= 19%; Pheterogeneity = .22) (Supplementary A, Figure 1). The risk of bacteremia was assessed in 9 trials [15, 17, 18, 23, 29, 32, 36, 39, 52], and based on a random-effects meta-analysis, the summary RR was 0.80 (95% CI, 0.54–1.19; P = .27), with low inconsistency between the trial results (I2 = 0%; Pheterogeneity = .92) (Figure 2 in Supplementary Data A). Nine trials assessed the risk of invasive fungal infections [13, 14, 25, 33, 36–38, 47, 48], and based on a random-effects meta-analysis, the summary RR was 1.12 (95% CI, 0.46–2.74; P = .80), with low inconsistency between the trial results (I2 = 0%; Pheterogeneity = .78) (Figure 3 in Supplementary Data A). Fourteen trials assessed the risk of sepsis [14, 17, 23–25, 27, 30, 33, 36, 42–44, 48, 49] and 10 trials septic shock [23, 24, 26, 31–33, 36, 39, 43, 48]. Based on a random-effects meta-analysis, the summary RR for sepsis and septic shock was 0.73 (95% CI, 0.45–1.20; P = .21) and 0.60 (95% CI, 0.39–0.93; P = .02), respectively. There was low inconsistency between the trial results (sepsis: I2 = 29%; Pheterogeneity = .15; septic shock: I2 = 27%; Pheterogeneity = .20) (Figures 4 and 5 in Supplementary Data A).
Certainty of Evidence Using GRADE
In adults hospitalized with moderate to severe COVID-19, the certainty of evidence using GRADE to assess the risk of infection with immune-based therapy compared with controls was rated as moderate (Table 5 in Supplementary Data A). Although the evidence was derived from randomized controlled trials (which are considered high quality of evidence), it (the certainty of evidence) was downgraded because of the high risk of bias in 5 trials. Although we included different immune-based drug agents, we considered the indirectness to be low, as all these drugs target the aberrant immune system caused by SARS-CoV-2.
DISCUSSION
In this systematic review and meta-analysis of 37 randomized clinical trials that included 32 621 patients with COVID-19 requiring hospitalization, the use of immune-based therapies was not associated with increased risk of secondary infections from the time of randomization as compared with standard of care. We found a mild protective effect for secondary infections with the use of immunotherapy, this effect being higher for secondary pneumonia and septic shock than for other infectious syndromes. Although the percentage of infections was slightly higher in those who received immunotherapy, the adjusted analysis that considered the weight of each study showed slight protection, with an RR of 0.82. The effect of immune-based therapy on the risk of infection was not dependent on age, sex, or mechanical ventilation at inclusion.
The protective effect of immune-based therapies for secondary infections in COVID-19 seems initially counterintuitive, considering previously published data for each drug in a variety of clinical conditions. The use of short-course corticosteroids, generally prescribed for upper respiratory tract infections, acute spinal conditions, and allergies, was associated with a 5.3-fold increase in the risk of sepsis within 30 days of drug initiation in a large, population-based study in the United States [53]. A pooled analysis of 7 studies from a systematic review and meta-analysis that included 1 RCT and 29 observational studies evaluating the use of corticosteroids as adjunctive treatment for influenza requiring hospitalization showed a 2.7-fold increased risk of hospital-acquired infection [54]. In a meta-analysis including 6 RCTs from a systematic review on the use of tocilizumab for rheumatoid arthritis, the combination of tocilizumab at 8 mg/kg with methotrexate (odds ratio [OR], 1.3) mildly increased the risk of infection [55]. Baricitinib, a Janus Kinase (JAK) inhibitor, increased the risk of infections by 1.28-fold compared with placebo in patients with rheumatoid arthritis [56]. Ruxolitinib, another JAK inhibitor, increased the risk of opportunistic and nonopportunistic infections [57].
Available data from RCTs suggest that immune-based therapy for COVID-19 are not only not associated with increased risk of infections, but may also be associated with protective effect. Targeting the COVID-19-related inflammatory response with corticosteroids or tocilizumab leads to better clinical outcomes and survival [58–60]. Both corticosteroids and tocilizumab decreased the risk for mechanical ventilation (OR, 0.74 and 0.71, respectively) in a meta-analysis including 3 studies and 6873 patients treated with corticosteroids and another that included 6 studies and 771 patients treated with tocilizumab [60, 61]. As the protective effect conferred by immune-based therapy for COVID-19 is highest for secondary pneumonia, one can postulate that avoiding or decreasing the time on mechanical ventilation may decrease the occurrence of ventilator-associated pneumonia. In our meta-regression, mechanical ventilation at baseline did not influence the RR of secondary infection, indicating that preventing mechanical ventilation is not the only mechanism in decreasing hospital-acquired pneumonia. We did not have information on days of intubation in all studies, so we could not account for that in our analysis.
Patients with severe COVID-19 display either macrophage activation syndrome or very low human leucocyte antigen DR expression accompanied by a profound depletion of CD4 lymphocytes, CD19 lymphocytes, and natural killer cells that can be partially rescued with interleukin-6 blockage by tocilizumab [62]. Other drugs targeting different pathways of the inflammatory response may also partially revert the consequences of this aberrant immune response and restore optimal immune responses against other pathogens.
Immune-based therapies for severe COVID-19 have been the only treatments demonstrating survival benefit to date. The use of immune-based therapies in the most vulnerable population carries a hypothetical increased risk of secondary infections. However, our data show that this risk is absent (or even lower), and thus these treatments should not be delayed when indicated, including in older or mechanically ventilated patients.
Guidelines on the treatment of moderate to severe COVID-19 should reflect our findings and make appropriate recommendations against the routine use of preventive antibiotics and antifungals in those treated with immunomodulating drugs for severe COVID-19.
Limitations
This study has several limitations. First, the definitions and reporting of infectious adverse events were not consistent across the trials. While this lack of consistency precludes estimating the rates of infectious complications for each immune-based therapy compared with standard of care, there is no reason to believe that this will impact the protective association measures.
Second, although there are few missing outcome data, no follow-up was done after hospital discharge in most trials, and the rates of secondary infection after hospital discharge were not evaluated. The potential immunosuppressive effects for some of the evaluated drugs may persist over time. For instance, short-term use of corticosteroids increases the rates of sepsis by 2.5-fold between 31 and 90 days after discontinuation [53], and tocilizumab has a half-life of around 10 days [63].
Third, some trials allowed combination of the study drug with other immune-based therapies. All RCTs evaluating tocilizumab allowed the concomitant use of corticosteroids ranging from 11% to 90% of all participants included in the interventional arm, and 1 participant received at least tocilizumab plus anakinra. In 1 RCT evaluating hydrocortisone, 1 participant in the interventional arm received tocilizumab and 3 eculizumab. In the 2 RCTs evaluating interferon β, 15% and 62% of the participants randomized to interferon received corticosteroids. Seventy percent of the participants assigned to ruxolitinib received concomitant treatment with corticosteroids. Finally, 17% of the participants randomized to receive baricitinib plus remdesivir received corticosteroids. Despite the obvious limitation in the accuracy of the estimations, it is important to highlight that the high frequent co-administration reinforces the hypothesis of using immune-based therapies as the first-line therapy for severe COVID-19.
Fourth, we used mechanical ventilation as a surrogate marker for the severity of the disease. However, there are reasons to use mechanical ventilation for managing COVID-19 other than the severity of the disease. As an example, early intubation has been suggested by some authors to interrupt the progressive lung deterioration mediated by tissue stress, raised pulmonary transvascular pressures, vascular flows, and fluid leakage [64]. Although mechanical ventilation may not accurately reflect the severity of COVID-19, stratifying the risk according to this variable is highly relevant as orotracheal intubation is a major risk factor for hospital-acquired pneumonia.
Finally, the protective effect of immune-based therapies may not be generalized to all populations. The RCTs included in this meta-analysis were mostly done in high-income countries, in adults, in individuals without concomitant infections (or without previous specific infections such as tuberculosis or strongyloidiasis), and in those not previously on exogenous immunosuppression. More information is required to evaluate the protective effect of immune-based therapies for secondary infections in specific populations such as children and immunocompromised patients.
This systematic review and meta-analysis provides an evidence-based review that could support future guidelines on the management of hospitalized patients with COVID-19 treated with immune-based therapy.
Supplementary Material
Acknowledgments
Financial support . The research reported in this publication was supported by the Fogarty International Center and Office of Dietary Supplements of the National Institutes of Health under Award Number D43 TW009118.
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author contributions. D.K., C.C., and E.A.A. conceptualized the study. D.K., C.C., E.A.A., M.C., and T.L. developed the study protocol. D.K. and S.C. developed the search strategy and searched for relevant records. D.K., A.S., B.W., K.C.K.L., and M.R. assessed eligibility and extracted data under the supervision of C.C. D.K. and J.G.A. analyzed the data. D.K. and C.C. wrote the first draft of the manuscript, coordinated and integrated comments from co-authors, and approved the final version for publication. All the authors critically revised successive drafts of the manuscript, provided important intellectual input, and approved the final version of the manuscript. The corresponding author has full access to all the data in the study.
Patient consent. As this is a systematic review and unidentified data were collected from published manuscripts, no patient consent or local ethical board review was obtained.
Contributor Information
Dima Kabbani, Department of Internal Medicine, American University of Beirut, Beirut, Lebanon; Department of Medicine, University of Alberta, Edmonton, Alberta, Canada.
Ashlesha Sonpar, Department of Medicine, University of Alberta, Edmonton, Alberta, Canada.
Benson Weyant, Department of Medicine, University of Alberta, Edmonton, Alberta, Canada.
Keith C K Lau, Department of Medicine, University of Alberta, Edmonton, Alberta, Canada.
Mark Robbins, Department of Medicine, University of Alberta, Edmonton, Alberta, Canada.
Sandra Campbell, John W. Scott Health Sciences Library, University of Alberta, Edmonton, Canada.
Karen Doucette, Department of Medicine, University of Alberta, Edmonton, Alberta, Canada.
Juan G Abraldes, Department of Medicine, University of Alberta, Edmonton, Alberta, Canada.
Tamara Lotfi, Department of Health Research Methods, Evidence, and Impact (HEI), McMaster University, Hamilton, Ontario, Canada.
Marlene Chaktoura, Department of Internal Medicine, American University of Beirut, Beirut, Lebanon.
Elie A Akl, Department of Internal Medicine, American University of Beirut, Beirut, Lebanon; Department of Health Research Methods, Evidence, and Impact (HEI), McMaster University, Hamilton, Ontario, Canada.
Carlos Cervera, Department of Medicine, University of Alberta, Edmonton, Alberta, Canada.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
References
- 1. Stockman LJ, Bellamy R, Garner P. SARS: systematic review of treatment effects. PLoS Med 2006; 3:e343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Li H, Chen C, Hu F, et al. Impact of corticosteroid therapy on outcomes of persons with SARS-CoV-2, SARS-CoV, or MERS-CoV infection: a systematic review and meta-analysis. Leukemia 2020; 34:1503–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ni YN, Chen G, Sun J, Liang BM, Liang ZA. The effect of corticosteroids on mortality of patients with influenza pneumonia: a systematic review and meta-analysis. Crit Care 2019; 23:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bhimraj A, Morgan R, Shumaker A, et al. Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients With COVID-19. Version 4.2.0. Infectious Diseases Society of America; 2021. Available at: https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/. Accessed May 9, 2021. [DOI] [PMC free article] [PubMed]
- 5. Singh JA, Wells GA, Christensen R, et al. Adverse effects of biologics: a network meta-analysis and Cochrane overview. Cochrane Database Syst Rev 2011; 2011:CD008794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wilczynski NL, Haynes RB. Developing optimal search strategies for detecting clinically sound prognostic studies in MEDLINE: an analytic survey. BMC Med 2004; 2:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lefebvre CGJ, Briscoe S, Littlewood A, et al. Technical supplement to chapter 4: searching for and selecting studies. In: Higgins JPT, Thomas J, Chandler J, Cumpston MS, Li T, Page MJ, and Welch VA, eds. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; 2020. [Google Scholar]
- 9. Glanville JM, Lefebvre C, Miles JN, Camosso-Stefinovic J. How to identify randomized controlled trials in MEDLINE: ten years on. J Med Libr Assoc 2006; 94:130–6. [PMC free article] [PubMed] [Google Scholar]
- 10. McGuinness LA, Higgins JPT. Risk-of-bias visualization (robvis): an R package and shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 2020; 12:55–61. [DOI] [PubMed] [Google Scholar]
- 11. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw 2010; 36:1–48. [Google Scholar]
- 12. Guyatt G, Oxman AD, Sultan S, et al. GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J Clin Epidemiol 2013; 66:151–7. [DOI] [PubMed] [Google Scholar]
- 13. Angus DC, Derde L, Al-Beidh F, et al. Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: the REMAP-CAP COVID-19 corticosteroid domain randomized clinical trial. J Am Med Assoc 2020; 324:1317–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Corral-Gudino L, Bahamonde A, Arnaiz-Revillas F, et al. Methylprednisolone in adults hospitalized with COVID-19 pneumonia: an open-label randomized trial (GLUCOCOVID). Wien Klin Wochenschr 2021; 133:303–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dequin PF, Heming N, Meziani F, et al. Effect of hydrocortisone on 21-day mortality or respiratory support among critically ill patients with COVID-19: a randomized clinical trial. JAMA 2020; 324:1298–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Edalatifard M, Akhtari M, Salehi M, et al. Intravenous methylprednisolone pulse as a treatment for hospitalised severe COVID-19 patients: results from a randomised controlled clinical trial. Eur Respir J 2020; 56:2002808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jeronimo CMP, Farias MEL, Val FFA, et al. Methylprednisolone as adjunctive therapy for patients hospitalized with coronavirus disease 2019 (COVID-19; MetCOVID): a randomized, double-blind, phase IIb, placebo-controlled trial. Clin Infect Dis 2021; 72:e373–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tomazini BM, Maia IS, Cavalcanti AB, et al. Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe acute respiratory distress syndrome and COVID-19: the CoDEX randomized clinical trial. JAMA 2020; 324:1307–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tang X, Feng YM, Ni JX, et al. Early use of corticosteroid may prolong SARS-CoV-2 shedding in non-intensive care unit patients with COVID-19 pneumonia: a multicenter, single-blind, randomized control trial. Respiration 2021; 100:116–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Horby P, Lim WS, Emberson JR, et al. Dexamethasone in hospitalized patients with COVID-19—preliminary report. N Engl J Med. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gordon AC, Mouncey PR, Al-Beidh F, et al. Interleukin-6 receptor antagonists in critically ill patients with COVID-19. N Engl J Med 2021; 384:1491–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. RECOVERY Collaborative Group . Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 2021; 397:1637–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rosas IO, Bräu N, Waters M, et al. Tocilizumab in hospitalized patients with severe COVID-19 pneumonia. N Engl J Med 2021; 384:1503–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rosas IO, Diaz G, Gottlieb RL, et al. Tocilizumab and remdesivir in hospitalized patients with severe COVID-19 pneumonia: a randomized clinical trial. Intensive Care Med 2021; 47:1258–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hermine O, Mariette X, Tharaux PL, Resche-Rigon M, Porcher R, Ravaud P. Effect of tocilizumab vs usual care in adults hospitalized with COVID-19 and moderate or severe pneumonia: a randomized clinical trial. JAMA Int Med 2021; 181:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Salama C, Han J, Yau L, et al. Tocilizumab in patients hospitalized with COVID-19 pneumonia. N Engl J Med 2021; 384:20–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Salvarani C, Dolci G, Massari M, et al. Effect of tocilizumab vs standard care on clinical worsening in patients hospitalized with COVID-19 pneumonia: a randomized clinical trial. JAMA Int Med 2021; 181:24–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stone JH, Frigault MJ, Serling-Boyd NJ, et al. Efficacy of tocilizumab in patients hospitalized with COVID-19. N Engl J Med 2020; 383:2333–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Veiga VC, Prats JAGG, Farias DLC, et al. Effect of tocilizumab on clinical outcomes at 15 days in patients with severe or critical coronavirus disease 2019: randomised controlled trial. BMJ 2021; 372:n84. doi: 10.1136/bmj.n84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Soin AS, Kumar K, Choudhary NS, et al. Tocilizumab plus standard care versus standard care in patients in India with moderate to severe COVID-19-associated cytokine release syndrome (COVINTOC): an open-label, multicentre, randomised, controlled, phase 3 trial. Lancet Respir Med 2021; 9:511–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Davoudi-Monfared E, Rahmani H, Khalili H, et al. Efficacy and safety of interferon β-1a in treatment of severe COVID-19: a randomized clinical trial. Antimicrob Agents Chemother. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rahmani H, Davoudi-Monfared E, Nourian A, et al. Interferon beta-1b in treatment of severe COVID-19: a randomized clinical trial. Int Immunopharmacol 2020; 88:106903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kalil AC, Mehta AK, Patterson TF, et al. Efficacy of interferon beta-1a plus remdesivir compared with remdesivir alone in hospitalised adults with COVID-19: a double-bind, randomised, placebo-controlled, phase 3 trial. Lancet Respir Med 2021; 9:1365–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sancho-López A, Caballero-Bermejo AF, Ruiz-Antorán B, et al. Efficacy and safety of sarilumab in patients with COVID19 pneumonia: a randomized, phase III clinical trial (SARTRE study). Infect Dis Ther 2021; 10:2735–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lescure FX, Honda H, Fowler RA, et al. Sarilumab in patients admitted to hospital with severe or critical COVID-19: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir Med 2021; 9:522–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kalil AC, Patterson TF, Mehta AK, et al. Baricitinib plus remdesivir for hospitalized adults with COVID-19. N Engl J Med. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Marconi VC, Ramanan AV, de Bono S, et al. Efficacy and safety of baricitinib for the treatment of hospitalised adults with COVID-19 (COV-BARRIER): a randomised, double-blind, parallel-group, placebo-controlled phase 3 trial. Lancet Respir Med 2021; 9:1407–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. CORIMUNO-19 Collaborative Group . Effect of anakinra versus usual care in adults in hospital with COVID-19 and mild-to-moderate pneumonia (CORIMUNO-ANA-1): a randomised controlled trial. Lancet Respir Med 2021; 9:295–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kyriazopoulou E, Poulakou G, Milionis H, et al. Early treatment of COVID-19 with anakinra guided by soluble urokinase plasminogen receptor plasma levels: a double-blind, randomized controlled phase 3 trial. Nat Med 2021; 27:1752–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lopes MI, Bonjorno LP, Giannini MC, et al. Beneficial effects of colchicine for moderate to severe COVID-19: a randomised, double-blinded, placebo-controlled clinical trial. RMD Open 2021; 7:e001455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. RECOVERY Collaborative Group . Colchicine in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet Respir Med 2021; 9:1419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cao Y, Wei J, Zou L, et al. Ruxolitinib in treatment of severe coronavirus disease 2019 (COVID-19): a multicenter, single-blind, randomized controlled trial. J Allergy Clin Immunol 2020; 146:137–46.e133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Guimarães PO, Quirk D, Furtado RH, et al. Tofacitinib in patients hospitalized with COVID-19 pneumonia. N Engl J Med 2021; 385:406–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Aman J, Duijvelaar E, Botros L, et al. Imatinib in patients with severe COVID-19: a randomised, double-blind, placebo-controlled, clinical trial. Lancet Respir Med 2021; 9:957–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lomakin NV, Bakirov BA, Protsenko DN, et al. The efficacy and safety of levilimab in severely ill COVID-19 patients not requiring mechanical ventilation: results of a multicenter randomized double-blind placebo-controlled phase III CORONA clinical study. Inflamm Res 2021; 70(10–12):1233–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cremer PC, Abbate A, Hudock K, et al. Mavrilimumab in patients with severe COVID-19 pneumonia and systemic hyperinflammation (MASH-COVID): an investigator initiated, multicentre, double-blind, randomised, placebo-controlled trial. Lancet Rheumatol 2021; 3:e410–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kumar S, De Souza R, Nadkar M, et al. A two-arm, randomized, controlled, multi-centric, open-label phase-2 study to evaluate the efficacy and safety of itolizumab in moderate to severe ARDS patients due to COVID-19. Expert Opin Biol Ther 2021; 21:675–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Caricchio R, Abbate A, Gordeev I, et al. Effect of canakinumab vs placebo on survival without invasive mechanical ventilation in patients hospitalized with severe COVID-19: a randomized clinical trial. JAMA 2021; 326:230–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Vlaar APJ, de Bruin S, Busch M, et al. Anti-C5a antibody IFX-1 (vilobelimab) treatment versus best supportive care for patients with severe COVID-19 (PANAMO): an exploratory, open-label, phase 2 randomised controlled trial. Lancet Rheumatol 2020; 2:e764–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kalil AC, Patterson TF, Mehta AK, et al. Baricitinib plus remdesivir for hospitalized adults with COVID-19. N Engl J Med 2021; 384:795–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Rahmani H, Davoudi-Monfared E, Nourian A, et al. Interferon β-1b in treatment of severe COVID-19: a randomized clinical trial. Int Immunopharmacol 2020; 88:106903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Caballero A, Filgueira LM, Betancourt J, et al. Treatment of COVID-19 patients with the anti-CD6 antibody itolizumab. Clin Transl Immunol 2020; 9:e1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Waljee AK, Rogers MA, Lin P, et al. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ 2017; 357:j1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lansbury L, Rodrigo C, Leonardi-Bee J, Nguyen-Van-Tam J, Lim WS. Corticosteroids as adjunctive therapy in the treatment of influenza. Cochrane Database Syst Rev 2019; 2:CD010406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Campbell L, Chen C, Bhagat SS, Parker RA, Östör AJ. Risk of adverse events including serious infections in rheumatoid arthritis patients treated with tocilizumab: a systematic literature review and meta-analysis of randomized controlled trials. Rheumatology (Oxford) 2011; 50:552–62. [DOI] [PubMed] [Google Scholar]
- 56. Wang F, Sun L, Wang S, et al. Efficacy and safety of tofacitinib, baricitinib, and upadacitinib for rheumatoid arthritis: a systematic review and meta-analysis. Mayo Clin Proc 2020; 95:1404–19. [DOI] [PubMed] [Google Scholar]
- 57. Lussana F, Cattaneo M, Rambaldi A, Squizzato A. Ruxolitinib-associated infections: a systematic review and meta-analysis. Am J Hematol 2018; 93:339–47. [DOI] [PubMed] [Google Scholar]
- 58. RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med 2021; 384(8):693–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Sterne JAC, Murthy S, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA 2020; 324:1330–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Tleyjeh IM, Kashour Z, Damlaj M, et al. Efficacy and safety of tocilizumab in COVID-19 patients: a living systematic review and meta-analysis. Clin Microbiol Infect 2021; 27:215–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Pasin L, Navalesi P, Zangrillo A, et al. Corticosteroids for patients with coronavirus disease 2019 (COVID-19) with different disease severity: a meta-analysis of randomized clinical trials. J Cardiothorac Vasc Anesth 2021; 35:578–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Giamarellos-Bourboulis EJ, Netea MG, Rovina N, et al. Complex immune dysregulation in COVID-19 patients with severe respiratory failure. Cell Host Microbe 2020; 27:992–1000e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sebba A. Tocilizumab: the first interleukin-6-receptor inhibitor. Am J Health Syst Pharm 2008; 65:1413–8. [DOI] [PubMed] [Google Scholar]
- 64. Marini JJ, Gattinoni L. Management of COVID-19 respiratory distress. JAMA 2020; 323:2329–30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.