Abstract
Background
Individuals with inflammatory bowel disease (IBD) have elevated symptoms of anxiety and depression. The burden of such symptoms, accompanied by functional impairment in IBD, is not well documented, nor is utilization of mental health care in this population.
Methods
Adults ≥18 years were identified in the cross-sectional 2015–2016 National Health Interview Survey. Responses from the Kessler Index were used to estimate the national prevalence of psychological distress with impairment and mental health-care use in IBD. Factors associated with psychological distress with impairment in IBD were analyzed using logistic regression.
Results
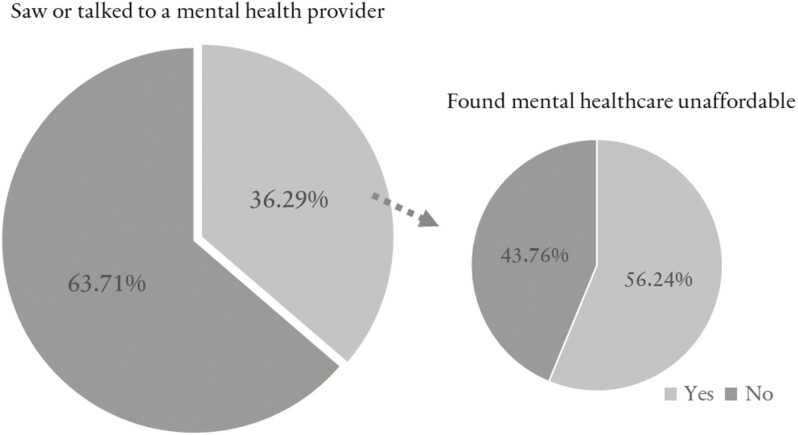
The prevalence of psychological distress with impairment was significantly higher in IBD than non-IBD adults (7.69% vs. 3.50%, respectively; P < .01). Among those with IBD and psychological distress with impairment, only a third (36.29%) had seen or talked to a mental health provider in the preceding 12 months. About half of these found the cost of mental health care unaffordable. On multivariable analysis, factors associated with psychological distress in IBD included increasing emergency room visits and trouble finding a health provider.
Conclusions
A significant number of adults with IBD in the United States have psychological distress accompanied by functional impairment. However, mental health care is underutilized in this population. Many of these individuals find the cost of mental health care unaffordable, struggle to find a health provider, and experience repeated emergency room visits. Ongoing efforts to improve mental health care in IBD should address issues of access and cost. Additionally, these efforts should seek to understand other barriers to mental health-care use.
Keywords: inflammatory bowel disease, mental health care, psychological distress
Introduction
Many individuals with inflammatory bowel disease (IBD) experience symptoms of psychological distress, such as anxiety and depression, which have been linked to increased disease activity.1–3 Recent studies describing a bidirectional relationship between IBD disease activity and psychological distress have highlighted the importance of recognizing and addressing psychological care for individuals with IBD, who may have higher levels of psychological distress than their non-IBD counterparts.4–8 A general limitation of pooled analyses of studies in estimating psychological distress is the variability in the screening measures and cutoffs used to identify clinically relevant symptoms. For example, there were over a dozen psychometric scales included in the meta-analysis by Barberio and colleagues.8 The thresholds for clinical relevance even with the commonly used Hospital Anxiety and Depression Scale ranged from >7 to ≥11, meaning scores in that range overlapped with what could be considered normal and abnormal. Thus, the prevalence beyond symptoms of psychological distress and inclusive of functional impairment (ie, symptoms interfering with or limiting 1 or more major life activities) in IBD is not well documented. Furthermore, despite the recognized importance of treating psychological distress in IBD, overall utilization and potential barriers to mental health care for IBD patients in the United States are not well described. The purpose of this study is to expand upon estimates of psychological distress in IBD to include functional impairment and mental health-care use. Understanding these issues can lead to interventions towards achieving holistic care in IBD.
Methods
Data Source
The National Health Interview Survey (NHIS) is conducted annually by the US Census Bureau on behalf of the Centers for Disease Control and Prevention (CDC) as a cross-sectional sample of all noninstitutionalized civilians. The NHIS is administered as a face-to-face, computer-assisted personal interview conducted by Census Bureau representatives. A wide range of data are collected, from basic demographics and medical conditions to health-care access, utilization, and quality-of-life assessments. Additional questions are periodically added to the survey. In the 2015 and 2016 surveys, data about an IBD diagnosis were collected. The NHIS deidentified data files, questionnaires, and related documentation are publicly available and accessible through the National Center for Health Statistics on the CDC website.9,10 National Health Interview Survey data have been cited in various previous IBD publications.11–14
Study Population
The NHIS uses geographically clustered sampling techniques so that each month’s sample is nationally representative. A sample adult is randomly selected from each household and separately interviewed. All sample adults aged 18 years and older who were interviewed in the 2015 and 2016 NHIS were included in this study. An affirmative response to the question “have you ever been told by a doctor or other health professional that you had Crohn’s disease or ulcerative colitis?” was the definition of an IBD diagnosis.
Outcome
Mental health-care use was defined as an affirmative answer to the question “during the past 12 months, have you seen or talked to any of the following health-care providers about your own health: a mental health professional such as a psychiatrist, psychologist, psychiatric nurse, or clinical social worker?” An assessment of psychological distress was based on the Kessler Index (K6), which is a validated 6-item scale measuring the frequency of specific psychological symptoms over the preceding 30 days: feeling so sad nothing could cheer you up; nervous; restless or fidgety; hopeless; that everything was an effort; or worthless. The K6 is part of the annual NHIS survey and was designed and validated to be sensitive in discriminating cases of psychological distress with functional impairment (ie, a mental, behavioral, or emotional disorder that substantially interferes with or limits 1 or more major life activities)15 from noncases based on the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders criteria.16,17 Responses are coded on a scale of total scores ranging from 0 to 24, with values ≥13 indicating psychological distress with impairment. The validity and reliability of the K6 in IBD has been previously reported.18 The K6 and its related 10-item scale are available in multiple languages and have been applied within diverse communities, including the World Health Organization’s World Mental Health surveys.19
Statistical Analysis
Survey sampling weights were used to calculate nationally representative estimates. Age standardization of the weighted prevalences and 95% confidence intervals (CIs) of participant characteristics were calculated based on the 2000 US census (distribution 8). To estimate the prevalence of psychological distress, the total K6 score was dichotomized, with scores ≥13 indicating psychological distress with impairment. The prevalence of psychological distress with impairment was compared between those with and without IBD. The non-IBD cohort includes all adults in the study who did not have IBD, although they could have another chronic condition.
To identify factors associated with psychological distress in IBD, covariates were first individually analyzed for an association with IBD using logistic regression. Variables of interest included sociodemographic factors (age group, sex, race and ethnicity, geographic region, marital status, educational attainment, employment status); lifestyle and comorbidity factors (smoking status; current heavy alcohol intake, defined as >14 drinks per week in the past year for males and >7 for females; comorbidities of hypertension, coronary heart disease, stroke, arthritis, asthma, cancer, weak or failing kidneys, chronic obstructive pulmonary disease, diabetes, or a liver condition); and health-care access and utilization factors (over the past 12 months: health insurance coverage, trouble finding a health provider, number of emergency room visits). Variables associated with IBD at a P value < .25 were included for multivariable modeling of the odds of psychological distress with impairment with an a priori adjustment for age and with IBD as the exposure variable of interest. Sequential models were adjusted for (1) sociodemographic factors, (2) plus lifestyle and comorbidity factors, (3) plus health-care access and utilization factors.
To analyze characteristics associated with mental health-care use in the IBD cohort with psychological distress with impairment, logistic regression was performed to compare characteristics between those who did and did not use mental health care over the preceding 12 months. To identify factors associated with psychological distress with impairment among the overall IBD population, logistic regression was performed to analyze the individual associations between psychological distress with impairment and each of the above covariates. Variables associated with psychological distress with impairment at a P value < .25 were also assessed in a multivariable model with backward elimination until all variables in the model were statistically significant, defined as having a P value < .05. All statistical analyses were performed with Stata 16.1 (College Station, Texas).
Ethical Considerations
This study used deidentified secondary data and received an exemption from full board review by the Einstein-Montefiore Institutional Review Board.
Results
Of the adults sampled in the 2015 (n = 33 672) and 2016 (n = 33 028) NHIS, there were 951 with a reported history of IBD (2015: n = 454; 2016: n = 497), corresponding to approximately 3.1 million individuals with IBD nationally. There was a significantly higher prevalence of psychological distress with impairment in adults with IBD compared to those without IBD (7.69% vs. 3.50%, respectively; P < .01).
As noted in Table 1, those with IBD tended to be older and majority female. They were also significantly more likely to have other chronic conditions compared to those without IBD (for 4+ conditions: 9.10% vs. 4.19%, respectively). While health insurance status did not differ significantly between those with and without an IBD diagnosis, those with IBD had more trouble finding a health provider (8.19% vs. 3.14%, respectively) and a greater number of emergency room (ER) visits (1 visit: 19.82% vs. 12.14%, respectively) than those without IBD.
Table 1.
Characteristics of US adults by IBD diagnosis.a
| Characteristic | IBDb | Non-IBDc | P value |
|---|---|---|---|
| Age-adjusted %d | Age-adjusted %d | ||
| Sociodemographic variables | |||
| Age group, years | |||
| 18-24 | 4.87 | 12.32 | <.01 |
| 25-44 | 25.57 | 34.27 | |
| 45-64 | 44.67 | 34.10 | |
| ≥65 | 24.89 | 19.32 | |
| Sex | |||
| Female | 62.01 | 51.53 | <.01 |
| Male | 37.99 | 48.47 | |
| Race and ethnicity | |||
| Hispanic | 15.37 | 16.35 | .04 |
| Non-Hispanic Asian | 2.83 | 5.89 | |
| Non-Hispanic Black | 5.86 | 11.96 | |
| Non-Hispanic Other | 2.76 | 2.20 | |
| Non-Hispanic White | 73.18 | 63.60 | |
| Region | |||
| Northeast | 19.66 | 17.69 | .28 |
| Midwest | 23.81 | 22.28 | |
| South | 34.93 | 36.36 | |
| West | 21.60 | 23.67 | |
| Marital status | |||
| Married/cohabitating | 55.44 | 60.53 | .19 |
| Widowed/divorced/separated | 21.27 | 15.88 | |
| Never married | 23.29 | 23.59 | |
| Educational attainment | |||
| Less than high school | 15.26 | 12.21 | .13 |
| High school/GED | 23.29 | 24.56 | |
| Some college/Associate degree | 32.06 | 31.30 | |
| Bachelor’s degree | 18.16 | 20.23 | |
| Master’s/Professional/Doctoral | 11.23 | 11.70 | |
| Employed or working | 54.84 | 63.20 | <.01 |
| Lifestyle factors and comorbidity | |||
| Smoking status | |||
| Current | 18.04 | 15.44 | <.01 |
| Former | 26.04 | 21.04 | |
| Never | 55.92 | 63.52 | |
| Heavy alcohol intakee | 6.14 | 5.11 | .21 |
| Other chronic conditionsf | |||
| None | 36.73 | 52.95 | <.01 |
| 1 | 24.89 | 24.06 | |
| 2–3 | 29.28 | 18.80 | |
| 4+ | 9.10 | 4.19 | |
| Health-care access and utilization | |||
| Health insurance | |||
| Private | 64.38 | 64.56 | .90 |
| Publicg | 21.60 | 19.88 | |
| Other | 5.45 | 4.96 | |
| Uninsured | 8.57 | 10.60 | |
| Trouble finding a health provider | 8.19 | 3.14 | <.01 |
| Emergency room visits | |||
| None | 66.58 | 81.14 | <.01 |
| 1 | 19.82 | 12.14 | |
| 2–3 | 10.05 | 4.84 | |
| 4+ | 3.55 | 1.87 | |
Source: NCHS, National Health Interview Survey, 2015–2016. Abbreviations: IBD, inflammatory bowel disease; NCHS, National Center for Health Statistics
Unweighted total, N = 951; estimated total, N = 3 121 000.
Unweighted total, N = 65 749; estimated total, N = 240 700 000.
Age-adjusted (except for age groups) percentages of total.
Heavy alcohol intake was defined as >14 drinks per week in the past year for males and >7 for females.
Comorbidities included hypertension, coronary heart disease, stroke, arthritis, asthma, cancer, weak or failing kidneys, chronic obstructive pulmonary disease, diabetes, or a liver condition.
Public insurance refers to any Medicaid or Medicare plan.
After adjusting for the aforementioned sociodemographic factors, psychological distress with impairment was over 2 times higher in adults with IBD than those without IBD (odds ratio [OR], 2.32; 95% CI, 1.62–3.31). Psychological distress with impairment remained significantly higher in the IBD cohort after adjusting for chronic comorbidities and lifestyle factors (OR, 1.78; 95% CI, 1.18–2.66). After additionally adjusting for health-care access and utilization factors, psychological distress with impairment was approximately 50% higher in IBD than non-IBD adults (OR, 1.54; 95% CI, 1.04–2.29).
Among the cohort of those with IBD and psychological distress with impairment, around a quarter (23.32%) found mental health care unaffordable. As depicted in Figure 1, about a third had seen or talked to a mental health provider in the preceding 12 months, of which about half still found the cost of mental health care unaffordable. Of sociodemographic factors associated with mental health-care use in those with elevated psychological distress, utilization was significantly higher in the Western United States compared to the Southern United States (OR, 7.01; 95% CI, 1.13–43.34) and significantly lower in those employed or working (OR, 0.19; 95% CI, 0.05–0.80). None of the lifestyle and comorbidity factors were significantly associated with mental health care in this subgroup.
Figure 1.
Mental health-care use and affordability among those with IBD and psychological distress with impairment. In a nationally representative population of US adults with IBD who met the criteria for psychological distress that substantially interferes with or limits 1 or more major life activities, only about a third of individuals had seen or talked to a mental health provider in the preceding 12 months. Of these, over half found the cost of care unaffordable. Abbreviation: IBD, inflammatory bowel disease.
In the overall IBD population, there were several factors associated with psychological distress with impairment on univariable logistic analysis: seeing a mental health provider; finding mental health care unaffordable; being widowed, divorced, or separated; being a current smoker; having nonprivate health insurance; having trouble finding a health provider; and having 2 or more ER visits in the past 12 months. On multivariable analysis, factors that remained associated with increased psychological distress with impairment in those with IBD were seeing a mental health provider (OR, 2.25; 95% CI, 1.06–4.77); finding mental health care unaffordable (OR, 6.96; 95% CI, 2.85–16.95); having 2 or more ER visits (for 4 ER visits, OR, 4.83; 95% CI, 1.63–14.28); and having trouble finding a health provider (OR, 4.14; 95% CI, 1.71–10.06) in the past 12 months.
Discussion
In this nationally representative sample of US adults, approximately 1 in 13 of those with IBD had psychological distress with impairment, which was significantly higher than the non-IBD population (7.69% vs. 3.50%, respectively; P < .01). Recent estimates from the National Institute of Mental Health report a 5.2% overall prevalence of psychological distress with impairment in US adults.15 The estimated prevalence in our study is based on a validated screening measure specifically designed to differentiate psychological distress that substantially interferes with or limits 1 or more major life activities from less severe, nonspecific psychological symptoms. Compared to their non-IBD counterparts, adults with IBD had a significantly greater burden of psychological distress with impairment even after adjusting for sociodemographic, lifestyle, comorbidity, and health-care access and utilization factors.
Among those with IBD, the factors most associated with psychological distress with impairment were trouble finding a health provider, increasing ER visits, having seen or talked to a mental health provider, and finding mental health care unaffordable. The fact that having seen or talked to a mental health provider was also associated with increased psychological distress with impairment among IBD adults presumably reflects that those struggling with psychological distress with impairment are more likely to engage with mental health services. It should be noted, however, that the CI for the association between psychological distress with impairment and mental health care was close to 1 or nonsignificance, though still statistically significant.
It is notable that only about a third of IBD adults with psychological distress with impairment had seen or talked to a mental health provider in the preceding 12 months. This proportion of IBD patients engaging in mental health care is similar to findings in a small, retrospective study on psychotherapy use in IBD patients.20 Also notable is that almost 1 in 4 IBD adults with psychological distress with impairment found mental health care unaffordable. Of those who had seen a mental health provider, about half still found the cost unaffordable, which suggests they may have discontinued prematurely or not received an adequate dose of therapy. Thus, accessing and affording mental health care appears to be an area of unmet need in an IBD population with an increased burden of psychological distress. Recent efforts to address this issue have included offering telemedicine options to ease logistical barriers to mental health care.21,22 Further studies are needed, however, to determine the effectiveness and equitable implementation of this approach.23
Reasons for frequent ER visits are unknown, and it is not possible to determine from the data whether ER visits were due to IBD flares or whether psychological distress with impairment was a contributing etiology. It is notable, however, that negative perturbations to mental health have been demonstrated to precede IBD flares, while flares in IBD disease activity also negatively impact mental health.2 Poor mental health has also been linked to increased health-care utilization among IBD patients in other studies,24–28 and attention to mental health among IBD patients with risk factors for poor mental health has been shown to reduce ER visits and overall health-care costs.5,29,30
This study has many strengths, including the nationally representative sampling and validated assessment tool from which the estimates are derived. The study also focuses on psychological distress with functional impairment, which has not been well studied previously, and moves beyond describing prevalence to assessing mental health-care use as well. We do acknowledge there are inherent limitations to a cross-sectional study, such as unmeasured confounders and an inability to infer causality in the associations described. In addition, Crohn’s disease and ulcerative colitis diagnoses were self-reported and not based on clinical records. However, the overall prevalences of self-reported diagnoses were similar in the independent samples of both years of the survey, indicating reproducibility of the estimates. Data on comorbid psychiatric diagnoses were not available to adjust for in the model. However, the K6 index is designed to account for any psychological distress in the population, regardless of a formal clinical psychiatric diagnosis. Since IBD disease activity and severity were not captured in the data, it cannot be determined whether the estimates of psychological distress with impairment here are driven by those with more active or complicated IBD compared to those with quiescent disease. Regardless of disease activity, however, the finding that only about a third of those with IBD and psychological distress with impairment utilized mental health care is troubling.
Conclusions
In conclusion, although it has been recognized that many individuals with IBD experience a range of negative mental health symptoms, such as anxiety and depression, this study suggests a significant number of IBD adults in the United States meet the criteria for having psychological distress that substantially interferes with or limits 1 or more major life activities. Many of these individuals struggle to find a health provider, experience repeated ER visits, and find the cost of mental health care unaffordable. Future studies could focus not only on screening for symptoms of psychological distress in IBD but also developing accessible and affordable mental health interventions to address this important aspect of care.
Acknowledgements
We would like to thank Aileen McGinn, PhD, for her data analysis support for this study. Data analyses, interpretations, and conclusions are those of the authors and not the National Center for Health Statistics.
Contributor Information
Ruby Greywoode, Assistant Professor of Medicine, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, New York, USA.
Thomas Ullman, Professor of Medicine, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, New York, USA.
Laurie Keefer, Professor of Medicine, Icahn School of Medicine at Mount Sinai, New York, New York, USA.
Supported By
RG is supported by NIH/National Center for Advancing Translational Science (NCATS) Einstein Montefiore CTSA Grant Number UL1TR001073.
Financial disclosures
R.G. is supported by NIH/National Center for Advancing Translational Science (NCATS) Einstein Montefiore CTSA Grant Number UL1TR001073. L.K. is a consultant to Abbvie and Reckitt Health and has equity ownership and is a cofounder of Trellus Health. T.U. declares no conflicts.
References
- 1. Wintjens DSJ, de Jong MJ, van der Meulen-de Jong AE, et al. Novel perceived stress and life events precede flares of inflammatory bowel disease: a prospective 12-month follow-up study. J Crohns Colitis. 2019;13:410–416. [DOI] [PubMed] [Google Scholar]
- 2. Gracie DJ, Guthrie EA, Hamlin PJ, et al. Bi-directionality of brain-gut interactions in patients with inflammatory bowel disease. Gastroenterology. 2018;154:1635–1646.e3. [DOI] [PubMed] [Google Scholar]
- 3. Bernstein CN, Singh S, Graff LA, et al. A prospective population-based study of triggers of symptomatic flares in IBD. Am J Gastroenterol. 2010;105:1994–2002. [DOI] [PubMed] [Google Scholar]
- 4. Neuendorf R, Harding A, Stello N, et al. Depression and anxiety in patients with inflammatory bowel disease: a systematic review. J Psychosom Res. 2016;87:70–80. [DOI] [PubMed] [Google Scholar]
- 5. Szigethy EM, Allen JI, Reiss M, et al. White paper AGA: the impact of mental and psychosocial factors on the care of patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2017;15:986–997. [DOI] [PubMed] [Google Scholar]
- 6. Bernstein CN, Hitchon CA, Walld R, et al. Increased burden of psychiatric disorders in inflammatory bowel disease. Inflamm Bowel Dis. 2019;25:360–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mikocka-Walus A, Knowles SR, Keefer L, et al. Controversies revisited: a systematic review of the comorbidity of depression and anxiety with inflammatory bowel diseases. Inflamm Bowel Dis. 2016;22:752–762. [DOI] [PubMed] [Google Scholar]
- 8. Barberio B, Zamani M, Black CJ, et al. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:359–370. [DOI] [PubMed] [Google Scholar]
- 9. National Center for Health Statistics. National Health Interview Survey, 2015. Public-use data file and documentation. 2016. https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm. Accessed November 3, 2020.
- 10. National Center for Health Statistics. National Health Interview Survey, 2016. Public-use data file and documentation. 2017. https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm.
- 11. Longobardi T. Work losses related to inflammatory bowel disease in the United States results from the National Health Interview Survey. Am J Gastroenterol. 2003;98:1064–1072. [DOI] [PubMed] [Google Scholar]
- 12. Nguyen GC, Chong CA, Chong RY.. National estimates of the burden of inflammatory bowel disease among racial and ethnic groups in the United States. J Crohns Colitis. 2014;8:288–295. [DOI] [PubMed] [Google Scholar]
- 13. Xu F, Dahlhamer JM, Terlizzi EP, et al. Receipt of preventive care services among US adults with inflammatory bowel disease, 2015-2016. Dig Dis Sci. 2019;64:1798–1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nguyen NH, Khera R, Ohno-Machado L, et al. Prevalence and effects of food insecurity and social support on financial toxicity in and healthcare use by patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2021;19:1377–1386.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. National Institute of Mental Health. Mental Illness. Accessed July 7, 2021. https://www.nimh.nih.gov/health/statistics/mental-illness
- 16. Kessler RC, Barker PR, Colpe LJ, et al. Screening for psychological distress with impairment in the general population. Arch Gen Psychiatry. 2003;60:184–189. [DOI] [PubMed] [Google Scholar]
- 17. Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184–189. [DOI] [PubMed] [Google Scholar]
- 18. Bernstein CN, Zhang L, Lix LM, et al. The validity and reliability of screening measures for depression and anxiety disorders in inflammatory bowel disease. Inflamm Bowel Dis. 2018;24: 1867–1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kessler RC, Green JG, Gruber MJ, et al. Screening for psychological distress with impairment in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19(Suppl 1):4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Craven MR, Quinton S, Taft TH.. Inflammatory bowel disease patient experiences with psychotherapy in the community. J Clin Psychol Med Settings. 2019;26:183–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Webb CA, Rosso IM, Rauch SL.. Internet-based cognitive-behavioral therapy for depression: current progress and future directions. Harv Rev Psychiatry. 2017;25:114–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mikocka-Walus A, Bampton P, Hetzel D, et al. Cognitive-behavioural therapy for inflammatory bowel disease: 24-month data from a randomised controlled trial. Int J Behav Med. 2017;24:127–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wegermann K, Patel Y, Wilder J.. Health equity and telemedicine in gastroenterology and hepatology. Clin Gastroenterol Hepatol. 2021;19:1516–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. van Langenberg DR, Lange K, Hetzel DJ, et al. Adverse clinical phenotype in inflammatory bowel disease: a cross sectional study identifying factors potentially amenable to change. J Gastroenterol Hepatol. 2010;25:1250–1258. [DOI] [PubMed] [Google Scholar]
- 25. Click B, Ramos Rivers C, Koutroubakis IE, et al. Demographic and clinical predictors of high healthcare use in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22:1442–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Limsrivilai J, Stidham RW, Govani SM, et al. Factors that predict high health care utilization and costs for patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2017;15: 385–392.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Navabi S, Gorrepati VS, Yadav S, et al. Influences and impact of anxiety and depression in the setting of inflammatory bowel disease. Inflamm Bowel Dis. 2018;24:2303–2308. [DOI] [PubMed] [Google Scholar]
- 28. Nguyen NH, Khera R, Ohno-Machado L, et al. Annual burden and costs of hospitalization for high-need, high-cost patients with chronic gastrointestinal and liver diseases. Clin Gastroenterol Hepatol. 2018;16:1284–1292.e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mittermaier C, Dejaco C, Waldhoer T, et al. Impact of depressive mood on relapse in patients with inflammatory bowel disease: a prospective 18-month follow-up study. Psychosom Med. 2004;66:79–84. [DOI] [PubMed] [Google Scholar]
- 30. Lores T, Goess C, Mikocka-Walus A, et al. Integrated psychological care reduces health care costs at a hospital-based inflammatory bowel disease service. Clin Gastroenterol Hepatol. 2021;19: 96–103.e3. [DOI] [PubMed] [Google Scholar]