Abstract
Although youth anxiety treatment research has focused largely on severe and impairing anxiety levels, even milder anxiety levels including levels that do not meet full criteria for a diagnosis can be impairing and cause for concern. There is need to develop and test viable treatments for these concerning anxiety levels to improve functioning and reduce distress. We present findings from a randomized controlled efficacy trial of attention bias modification treatment (ABMT) and attention control training (ACT) for youths with concerning anxiety levels. Fifty-three clinic-referred youths (29 boys; M age=9.3 years, SD age=2.6) were randomized to either ABMT or ACT. ABMT and ACT consisted of attention-training trials in a dot-probe task presenting angry and neutral faces; probes appeared in the location of neutral faces in 100% of ABMT trials and 50% of ACT trials. Independent evaluators provided youth anxiety severity ratings; youths and parents provided youth anxiety severity and global impairment ratings; and youths completed measures of attention bias to threat and attention control at pretreatment, posttreatment, and two-month follow-up. In both arms, anxiety severity and global impairment were significantly reduced at posttreatment and follow-up. At follow-up, anxiety severity and global impairment were significantly lower in ACT compared with ABMT. Attention control, but not attention bias to threat, was significantly improved at follow-up in both arms. Changes in attention control and attention focusing were significantly associated with changes in anxiety severity. Findings support the viability of attention training as a low intensity treatment for youth with concerning anxiety levels, including levels that do not meet full criteria for a diagnosis. Superior anxiety reduction effects in ACT highlight the critical need for mechanistic research on attention training in this population.
Keywords: Anxiety, Children, Adolescents, Treatment, Attention bias modification
The youth anxiety randomized controlled treatment literature is dominated by samples of severe and diagnosable cases, which has significantly advanced knowledge about treating anxiety disorders in children and adolescents (hereon “youth”) (Higa-McMillan, Francis, Rith-Najarian, & Chorpita, 2016; Silverman, Pina, & Viswesvaran, 2008). Far less advancement has occurred in treating less severe yet concerning levels of youth anxiety. Emanating from the anxiety stepped care literature, in this article for brevity we use the term “concerning anxiety” to refer to such levels (Kendall et al., 2016; Silverman, Pettit, & Lebowitz, 2016). Concerning anxiety includes mild to moderate anxiety levels that meet for diagnosis, as well as mild to moderate levels that do not meet the number, duration, and/or severity of symptoms required for diagnosis. Concerning anxiety, too, is associated with impairment and distress and is the focus of the current treatment study.
Angold, Costello, Farmer, Burns, and Erkanli (1999) were among the first to shine a light on these understudied though prevalent “impaired but undiagnosed” youth with concerning anxiety. Additional supportive data from large U.S. and European samples have since appeared (Balàzs et al., 2013; Roberts, Fisher, Turner, & Tang, 2015). In a sample of 4,975 youths in the U.S., the Teen Health 2000 Study found about a three-fold rate of concerning anxiety cases that did not meet full criteria for a diagnosis (5.9%) compared with diagnosable anxiety cases (2.0%) (Roberts et al., 2015). Close to 40% (37.8%) of these cases were highly impaired -- a sizable proportion given 49.6% of diagnosable cases were highly impaired. In 12,395 youths, the Saving and Empowering Young Lives in Europe Study also showed high rates of concerning anxiety, high impairment, and increased disease burden and suicide risk (Balàzs et al., 2013).
Using Attention Training as a Low Intensity Treatment Approach to Target Attention Bias
With the cumulative knowledge concerning prevalence, impairment, and increased disease burden and suicide risk, there is need for evidence-based treatments that can allay concerning anxiety. A key consideration for such treatment is access and use of mental health services. Access and use of services are key because only 22% of anxiety disorder cases access services, lowest of all psychiatric disorders (Costello, He, Sampson, Kessler, & Merikangas, 2014). When youth with anxiety disorders and their families do access mental health services, they attend on average four sessions and up to 50% drop out of treatment (de Haan, Boon, de Jong, Hoeve, & Vermeiren, 2013; Harpaz-Rotem, Leslie, & Rosenheck, 2004).
Given the above, attention bias modification treatment (ABMT) seems like an especially viable low intensity treatment for youth with concerning anxiety. This is because ABMT is inexpensive (does not require skilled clinicians), brief (8 15-minute sessions), and can allay participants’ privacy, stigma, and personal disclosure concerns (Yeguez, Page, Rey, Silverman, & Pettit, 2020). ABMT is based on converging behavioral and neuroscience research establishing that attention processes among anxious individuals, including youth with concerning anxiety, are characterized by perturbations in attention allocation to threat (Abend et al., 2018; Dudeney, Sharpe, & Hunt, 2015). Although low intensity prevention programs show small positive effects for nonreferred youth at risk for anxiety (e.g., Waters et al., 2019; Werner-Seidler, Perry, Calear, Newby, & Christensen, 2017), it is unknown whether these or other low intensity treatment approaches are efficacious for clinic-referred anxious youth who do not meet full criteria for a diagnosis. Having such treatments available has the potential to improve early intervention and stepped care approaches.
In ABMT, attention perturbations are targeted directly as participants complete hundreds of computer-based training trials of a dot-probe task. In each trial, a pair of threatening and neutral stimuli is presented simultaneously, followed immediately by a probe. The probe always appears in the location of the neutral stimulus, establishing a contingency between the neutral stimulus and probe location, facilitating reductions in attention allocation to threat. Studies demonstrate feasibility and acceptability and largely demonstrate significant ABMT effects in adults and youth with anxiety disorders and youth at temperamental risk for anxiety (Chang et al., 2019; Eldar et al., 2012; Liu, Taber-Thomas, Fu, & Perez-Edgar, 2018; Price et al., 2016). Of note, not all studies find superior effects for ABMT relative to comparator attention training arms, as we elaborate in the following section (de Voogd, Wiers, & Salemink, 2017; Fodor et al., 2020; Grist, Croker, Denne, & Stallard, 2019).
Using Attention Control Training as a Comparator to Target Attention Focusing and Shifting
The most widely used comparator in youth and adult ABMT randomized controlled trials is Attention Control Training (ACT) (Price et al., 2016). In ACT, participants complete the same dot-probe task as in ABMT, with the key exception that the probe appears with equal frequency in the locations of the neutral stimulus and threatening stimulus. By having no contingency between stimulus valence and probe location, ACT is designed to control for nonspecific effects on focusing and shifting attention. Although designed as a comparator control, data from samples of youth and adults with anxiety disorders show significant anxiety-reduction effects in both ABMT and ACT (Heeren, Mogoase, McNally, Schmitz, & Philippot, 2015; Pergamin-Hight, Pine, Fox, & Bar-Haim, 2016; Pettit et al., 2020). Data from youth and adults with anxiety disorders further show that ABMT and ACT both significantly increase attention control, the ability to focus strategically and shift attention voluntarily (Heeren et al., 2015; Linetzky, Pettit, Silverman, Pine, & Bar-Haim, 2020; Pettit et al., 2020). Whether this is true with concerning anxiety in youth is unknown; our examining this issue is therefore another important contribution of our study.
Our study further contributes and extends past research by evaluating attention training’s effects on attention control components, focusing and shifting. Focusing refers to maintaining attention on a stimulus; shifting refers to redirecting attention from one stimulus to another. By evaluating attention control as well as its components, our study is an important step in developing more nuanced understanding of mechanisms of anxiety reduction effects found in ABMT and ACT.
Present Study
Based on the conceptualization that reducing attention bias to threat is critical to the anxiety-reduction effects of attention training (e.g., MacLeod & Clarke, 2015), we designed our randomized controlled trial to test the hypotheses that ABMT would result in significantly lower levels of attention bias to threat and anxiety severity at posttreatment and at the follow-up evaluation two months after treatment, compared with ACT. Under this conceptualization, decreases in attention bias to threat would be associated with decreases in anxiety severity. However, as our summary reveals, it cannot be taken for granted that ABMT will produce superior outcome compared with ACT. Based on data suggesting that increases in attention control may be critical to the anxiety-reduction effects of attention training (Heeren et al., 2015; Linetzky et al., 2020; Pettit et al., 2020), it is plausible that levels of attention control would be significantly higher, and levels of anxiety severity significantly lower at posttreatment and follow-up relative to pretreatment in both ABMT and ACT, and that increases in attention control would be associated with decreases in anxiety. Given that youth with concerning anxiety are impaired despite not necessarily meeting full criteria for a diagnosis of an anxiety disorder (Angold et al., 1999), we evaluated youth global impairment as well. We expected that findings for global impairment would parallel those for anxiety severity.
Method
Participants
Participants were 53 clinic-referred youths ages 7 to 15 years (mean age = 9.3 years, SD = 2.6; 54.7% boys; 66.0% Hispanic; see Table 1) recruited from two university-based anxiety disorder specialty clinics, one at Florida International University and the other at Yale University. We recruited from anxiety specialty clinics because, as noted, concerning anxiety is impairing and prompts parents to seek clinical intervention. Inclusion criteria were either youths or parents endorsing concerning anxiety, defined as (a) the presence of at least 3 anxiety symptoms across the most common youth anxiety disorders, generalized anxiety disorder, separation anxiety disorder, and social anxiety disorder, and (b) global anxiety impairment ratings of either 4 or 5 (mild to moderate) on the 0–8 point scale on the Anxiety Disorder Interview Schedule for Children-IV: Child and Parent Versions (ADIS-IV: C/P; Silverman & Albano, 1996). Global anxiety impairment ratings were obtained by asking parents and children to provide an overall severity rating based on all anxiety symptoms endorsed across all diagnostic modules on the ADIS-IV: C/P. We derived a composite rating for each participant using the highest overall severity rating from the youth and parent interviews. These inclusion criteria ensured all participants experienced anxiety-related impairment. Of note, baseline attention bias to threat was not an inclusion criterion because there is insufficient evidence that it either predicts or moderates ABMT outcome (e.g., Pergamin-Hight et al., 2016; Shechner et al., 2014). Exclusion criteria were global impairment ratings of 6 or higher, developmental disabilities, psychosis, or current involvement in another treatment; all can be ruled in/out with the ADIS-IV: C/P.
Table 1.
Participant Sociodemographic and Diagnostic Characteristics at Pretreatment
| ABMT (n = 27) |
ACT (n = 26) |
|
|---|---|---|
| Age, mean (SD) | 9.67 (2.68) | 8.85 (2.53) |
| Male gender, n (%) | 17 (63.0) | 12 (46.2) |
| Hispanic ethnicity, n (%) | 19 (70.4) | 16 (61.5) |
| Annual family income, n (%) | ||
| 0-20,999 | 2 (7.4) | 2 (7.7) |
| 21,000--60,999 | 10 (37.0) | 9 (34.6) |
| 61,000--99,999 | 4 (14.8) | 1 (3.8) |
| Over 100,000 | 8 (29.6) | 10 (38.5) |
| Not reported | 3 (11.1) | 4 (15.4) |
| Primary Diagnosis, n (%) | ||
| No Diagnosis | 14 (51.9) | 19 (73.1) |
| Generalized Anxiety Disorder | 6 (22.2) | 2 (7.7) |
| Separation Anxiety Disorder | 6 (22.2) | 2 (7.7) |
| Social Anxiety Disorder | 0 (0.0) | 1 (3.8) |
| Specific Phobia | 1 (3.7) | 2 (7.7) |
Note. ABMT = attention bias modification treatment; ACT = attention control training.
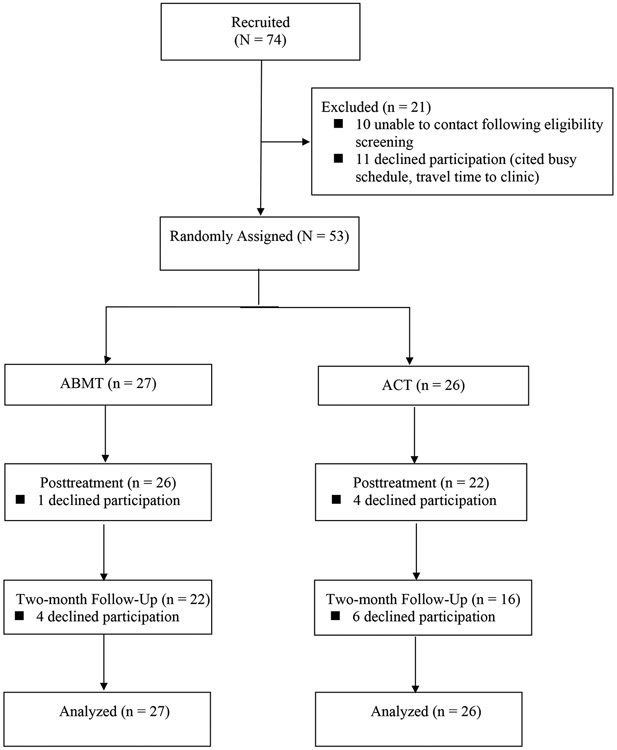
As shown in Figure 1, 74 youths were recruited for this study. Of these 74, 53 (71.6%) parents provided informed consent and youths provided informed assent. After we obtained consent/assent, participants were then enrolled. All 53 participants met criteria for concerning anxiety as defined above; of these 53, 20 (37.7%) met for an anxiety disorder diagnosis and 33 (62.2%) experienced impairing anxiety that did not meet full criteria for a diagnosis (see Table 1). Four participants (2 in ABMT; 2 in ACT) met criteria for Attention Deficit /Hyperactivity Disorder (ADHD), Combined Type and were on a stable dose of medication for ADHD.
Figure 1.
CONSORT Diagram
Materials and Task
All measures described below have been validated and used widely in samples of youth ages 7 to 15 years.
Diagnostic Interview.
We administered the ADIS-IV: C/P (Silverman & Albano, 1996) to youths and parents, respectively. The ADIS-IV: C/P yields retest reliability kappas between .80 and .92 for diagnoses, interrater reliability kappas between .57 and .86 for specific anxiety diagnoses, and significant associations with youth anxiety ratings (Silverman, Saavedra, & Pina, 2001).
Pediatric Anxiety Rating Scale (PARS; RUPP Anxiety Study Group, 2002).
We measured primary outcome using independent evaluator (IE) ratings of youth anxiety symptom severity on the six-item version of the PARS. Using information obtained in separate interviews with youths and parents, an IE masked to participants’ assigned study arm scored each of 50 anxiety symptoms as either present or absent during the past week. IEs then rated endorsed symptoms on six dimensions of global severity and impairment. A clinical cutoff for the six-item PARS has not been established. To characterize the study’s sample, we compared scores on the six-item PARS with established clinical cutoffs for the five-item PARS (11.5) and the seven-item PARS (17.5) (Ginsburg, Keeton, Drazdowski, & Riddle, 2011). The PARS has adequate coefficient alphas (between .64 and .91) and interrater reliability (intraclass correlation coefficients between .78 and .97), treatment sensitivity, and convergent validity through significant correlations with youth self-ratings and parent ratings on youth anxiety scales (RUPP Anxiety Study Group, 2002). In this sample, the omega coefficient was .83 (Revelle & Condon, 2019).
Screen for Child Anxiety Related Emotional Disorders – Child and Parent versions (SCARED-C/P; Birmaher et al., 1997).
We measured secondary outcomes using youth self-ratings and parent ratings of youth anxiety symptom severity on the SCARED-C/P. The SCARED-C/P consists of 41 items on which youth or parents rate youth anxiety symptoms. A score of 25 or higher indicates clinical levels of anxiety severity. The SCARED-C/P has adequate test-retest reliability (ranging from .70 to .90) and convergent and divergent validity through expected patterns of correlations with other screening scales (Birmaher et al., 1997). In this sample, the omega coefficient was .93 for the SCARED-C and .94 for the SCARED-P.
Columbia Impairment Scale – Child and Parent versions (CIS-C/P; Bird et al., 1993).
We also measured secondary outcomes using youth self-ratings and parent ratings of youth global impairment on the CIS-C/P. The CIS-C/P consists of 13 items on which youth or parents rate youth global impairment on a 5-point Likert scale, ranging from “no problem” to “very bad problem.” Higher scores indicate greater impairment, with scores above 15 indicating “high” impairment (Bird et al., 1993). The CIS has adequate test-retest reliability (ranging from .63 to .89) and convergent validity through significant correlations with other measures of impairment (Winters, Collett, & Myers, 2005). In this sample, the omega coefficient was .78 for the CIS-C and .88 for the CIS-P.
Attention Bias to Threat.
Consistent with past studies on attention training for anxiety (e.g., Price et al., 2016), we used the standardized emotional faces dot-probe task from the Tel Aviv University – National Institute of Mental Health ABMT Initiative (http://people.socsci.tau.ac.il/mu/anxietytrauma/research/) to measure attention bias to threat (Abend, Pine, & Bar-Haim, 2014). In each of 120 trials, a white fixation cross appeared for 500 milliseconds (ms) in the center of the screen, followed by a pair of faces (one neutral, one angry) appearing for 500 ms. Immediately following the faces, a probe (“<” or “>”) appeared in the location of one of the faces. Participants indicated the orientation of the probe by clicking the left or right mouse button (left for “<”, right for “>”). Responses on the dot-probe task were used to calculate attention bias scores. Trials in which the probe replaced the angry face were considered congruent trials; trials in which the probe replaced the neutral face were considered incongruent trials. Bias scores were computed as reaction time differences of incongruent minus congruent trials. Positive attention bias scores indicate a bias toward angry faces (i.e., threat) and negative scores indicate a bias away from threat. Inaccurate responses, trials with response latencies shorter than 150 ms and longer than 1,200 ms, and trials with response latencies plus or minus 2.5 SDs from the participant’s mean were excluded (Abend et al., 2018; Eldar, Yankelevitch, Lamy, & Bar-Haim, 2010).
Attentional Control Scale for Children (ACS-C; Muris, de Jong, & Engelen, 2004).
We measured youth attention control using a 15-item version of the ACS-C (Melendez, Bechor, Rey, Pettit, & Silverman, 2017; van Son et al., 2021). The original ACS-C consists of 20 items on which youth rate their ability to maintain attentional focus on a stimulus and shift attention from one stimulus to another. Multiple independent validation studies in anxious youth support a 15-item version that excludes 5 poorly performing items from the original version (Melendez et al., 2017; van Son et al., 2021). On the 15-item version, 9 items comprise a Focusing subscale and 6 items comprise a Shifting subscale. The 15-item ACS-C total scale score and subscale scores have demonstrated good psychometric properties and concurrent validity through significant correlations with anxiety and depression severity (Melendez et al., 2017; van Son et al., 2021). In this sample, the omega coefficient was .74 for the total scale, .79 for Focusing, and .73 for Shifting.
Procedure
The present study received approval from the universities’ institutional review boards (ClinicalTrials.gov identifier: NCT02410967). The study was conducted at Florida International University and Yale University from April 2015 to June 2018. All measures were completed at pretreatment (PRE), posttreatment (POST), and a follow-up (Follow-Up) evaluation two months after POST. Following PRE, participants were randomized in equal proportion to ABMT or ACT. Participants and researchers were masked to study arm assignment. Six masters- and doctoral-level graduate students served as IEs and administered ABMT and ACT sessions. Before conducting interviews, IEs received extensive training in administering and scoring the protocol and met reliability criteria on five video-recorded youth–parent assessments. Supervision was provided by a licensed clinical psychologist at weekly meetings. For each participant, one IE administered the PRE evaluation and a different IE administered the POST and Follow-Up evaluations.
ABMT.
Consistent with past attention training studies and following the standardized Tel Aviv University – National Institute of Mental Health ABMT Initiative (http://people.socsci.tau.ac.il/mu/anxietytrauma/research/), youths completed two weekly sessions of ABMT in the clinic over four weeks, for a total of eight sessions (e.g., Pergamin-Hight et al., 2016; Pettit et al., 2020). At each session, participants completed 160 trials of the ABMT protocol, for a total of 1,280 trials. Trials of the ABMT protocol were identical to trials of the attention bias to threat assessment task except that a unique set of faces was used (i.e., different from those used in the assessment task) and the probe replaced the neutral face on 100% of the trials. Data demonstrate that this standardized ABMT protocol, including stimuli, number of sessions, and number of trials, produces anxiety-reduction effects (Pergamin-Hight et al., 2016; Price et al., 2017).
ACT.
ACT was identical to the ABMT protocol except for the frequency with which the probe replaced the neutral face. Eighty percent of trials included one neutral face and one angry face. On these trials, angry face location, probe location, and actor were fully counterbalanced. Probe type appeared with equal probability for angry face location, probe location, and actor. The other 20% of trials included neutral-neutral face pairs.
Statistical Analysis
We used power analyses to determine sample size. With alpha at .05 and power at 0.80, we introduced covariates (age, study site, and the PRE-score on the outcome variable) to reduce within-subject error and thus increase the precision of estimated between-group differences (Belin & Normand, 2009; Pocock, Assmann, Enos, & Kasten, 2002). This allowed us to detect medium-sized effects between treatment arms, which is in line with meta-analyses that show small to medium effects (e.g., Hakamata et al., 2010; Price et al., 2016).
To examine the influence of treatment on anxiety, impairment, and attention, we used two-way analyses of covariance in a structural equation modeling (SEM) framework (Rausch, Maxwell, & Kelley, 2003). We used a maximum likelihood estimator with robust standard errors (MLR) as implemented in the MPlus 6.12 statistical software program. In each model, participant age, study site, and the PRE-score on the outcome variable were included as covariates. Robust likelihood ratio tests were used to examine differences between PRE and POST mean scores and POST and Follow-Up mean scores (collapsing across treatment arms). We calculated reliable change indices for primary and secondary anxiety outcomes, with RCIs greater than or equal to 1.96 indicating clinically significant change at p < 0.05 (RCI; Jacobson & Truax, 1991).
To examine the associations between changes in anxiety variables and changes in attention variables, we used fixed effects regression analyses for panel data at PRE, POST, and Follow-Up (Allison, 2009). This approach regressed anxiety variables onto attention variables on a within-person basis, documenting how much anxiety changed given a one-unit change in attention variables.
Complete data were obtained from 90.6% of participants at POST and 71.7% at Follow-Up. To examine missing-data bias, a dummy variable was created that indicated the presence or absence of missing data on each variable in the analyses. Associations between the dummy variables and other study variables were examined. No meaningful bias was observed and the extent of missing data did not differ between study arms. Missing data were accommodated using full information maximum likelihood for the two-way analyses of covariance (Enders, 2010). For the fixed effects regressions, missing data were accommodated using multiple imputation (chained equations) (Van Buuren, 2007). Across all analyses, significant effects were detected at α < 0.05. All tests were two-sided.
Results
We present a CONSORT diagram in Figure 1. Attrition did not differ significantly between study arms at POST or Follow-Up. Forty-eight (90.6%) participants completed all 8 training sessions as scheduled, supporting the feasibility and acceptability of the attention training protocols in this sample of youths with concerning anxiety. There were no statistically significant differences between study completers and non-completers at PRE on any study variables. Outcome analyses included all participants (study completers and non-completers), allowing intent-to-treat analyses. We determined maintenance of masked assignment to study arm by asking youths and their parents at Follow-Up to indicate to which study arm the youth was assigned (ABMT or ACT). Youths’ and parents’ ability to identify study arm assignment did not exceed chance.
Outcomes Analyses
We present means and standard deviations on anxiety variables, impairment, and attention variables for each study arm in Table 2. Relative to prior RCTs of attention training for youth with anxiety disorders (see Hang, Zhang, Wang, Zhang, & Liu, 2021), the current sample’s mean anxiety severity levels at PRE were lower according to clinician ratings on the PARS, which typically were above 16 in prior RCTs, and similar according to youth and parent ratings on the SCARED-C/P, which typically were between 25 and 30 in prior RCTs. Mean IE ratings of youth anxiety on the PARS were below clinical cutoff at PRE, POST, and Follow-Up. Mean youth and parent ratings of youth anxiety on the SCARED-C/P were above clinical cutoff at PRE, indicating they rated youth anxiety severity at clinical levels. Mean youth and parent ratings on the SCARED-C/P were below cutoff at POST and Follow-Up. Mean youth and parent ratings of youth global impairment on the CIS-C/P were slightly below the “high” cutoff at PRE and substantially below the cutoff at POST and Follow-Up.
Table 2.
Means and Standard Deviations for Anxiety Symptoms, Impairment, and Attention Variables at Pretreatment, Posttreatment, and Two-Month Follow-Up
| Measure | ABMT (n = 27) | ACT (n = 26) | |
|---|---|---|---|
| PARS | PRE | 10.30 (4.75) | 10.12 (4.97) |
| POST | 7.21 (5.66) | 7.73 (4.81) | |
| Follow-Up | 7.90 (6.19) | 5.69 (4.42) | |
| SCARED-C | PRE | 28.89 (14.77) | 22.00 (11.66) |
| POST | 17.88 (13.76) | 14.72 (10.61) | |
| Follow-Up | 20.41 (15.66) | 11.88 (10.88) | |
| SCARED-P | PRE | 28.31 (15.28) | 29.41 (13.29) |
| POST | 18.98 (13.70) | 20.16 (11.75) | |
| Follow-Up | 21.96 (16.82) | 17.13 (10.86) | |
| CIS-C | PRE | 12.03 (9.17) | 12.47 (6.65) |
| POST | 7.54 (8.86) | 6.71 (5.03) | |
| Follow-Up | 8.06 (8.17) | 5.62 (5.31) | |
| CIS-P | PRE | 12.60 (7.98) | 12.53 (10.85) |
| POST | 9.42 (8.86) | 9.47 (11.26) | |
| Follow-Up | 11.55 (6.79) | 6.00 (5.50) | |
| Attention bias to threat | PRE | 18.74 (54.54) | −5.02 (60.63) |
| POST | −10.04 (22.94) | −12.27 (63.76) | |
| Follow-Up | −2.86 (47.67) | 26.64 (64.43) | |
| ACS-C | PRE | 38.94 (7.15) | 40.25 (6.39) |
| POST | 40.87 (7.00) | 42.46 (9.36) | |
| Follow-Up | 43.05 (7.96) | 46.10 (8.12) |
Note. ABMT = attention bias modification treatment; ACT = attention control training; PARS = Pediatric Anxiety Rating Scale; SCARED – C = Screen for Child Anxiety and Related Disorders – Child Version; SCARED-P = Screen for Child Anxiety and Related Disorders – Parent Version; CIS-C = Columbia Impairment Scale – Child Version; CIS-P = Columbia Impairment Scale – Parent Version; ACS-C = Attentional Control Scale for Children. Means and standard deviations of Attention bias to threat are presented in milliseconds.
Primary Outcome.
The Time x Study Arm interaction effect was statistically significant for IE ratings of youth anxiety on the PARS; youth in ACT had significantly lower PARS scores at Follow-Up than youth in ABMT, controlling for scores at POST (z = 1.99, p < .05; Cohen’s d = 0.44). The difference between study arms at POST for the PARS was not statistically significant (z = −.47, p = .64; Cohen’s d = 0.07). Collapsing across study arms, mean scores on the PARS were significantly lower at POST than PRE (z = 3.70, p < .001; Cohen’s d = 0.51) and mean scores at POST were not significantly different from mean scores at Follow-Up. RCI analyses indicated significant reliable PRE to POST change on the PARS in 29.3% of participants.
Secondary Outcomes.
The Time x Study Arm interaction effects were statistically significant for youth self-ratings of anxiety on the SCARED-C and parent ratings of youth impairment on the CIS-P, but not parent ratings of youth anxiety on the SCARED-P or youth self-ratings of impairment on the CIS-C. Youth in ACT had significantly lower youth SCARED-C (z = 2.29, p < .05; Cohen’s d = 0.72) and CIS-P (z = 2.50, p < .05; Cohen’s d = 0.69) scores at Follow-Up than youth in ABMT, controlling for scores at POST. The differences between study arms at POST was not statistically significant for the SCARED-C (z = −.37, p = .71; Cohen’s d = 0.17), SCARED-P (z = −.32, p = .75; Cohen’s d = 0.13), CIS-P (z = −.02, p = .98; Cohen’s d = 0.01), or CIS-C (z = −.02, p = .98; Cohen’s d = 0.04). Collapsing across study arms, mean scores were significantly lower at POST than PRE for the SCARED-C (z = 4.33, p < .001; Cohen’s d = 0.66), SCARED-P (z = 5.05, p < .001; Cohen’s d = 0.96), CIS-C (z = 4.78, p < .001; Cohen’s d = 0.88) and CIS-P (z = 3.57, p < .001; Cohen’s d = 0.49). Mean scores at POST were not significantly different from mean scores at Follow-Up. RCI analyses indicated significant reliable PRE to POST change on the SCARED-C in 46.7% of participants and on the SCARED-P in 39.1% of participants.
Attention Bias and Attention Control Analyses
Mean levels of attention bias to threat and attention control were similar to those in prior trials of attention training in anxious youth (e.g., Pergamin-Hight et al., 2016; Pettit et al., 2020). The Time x Study Arm interaction effect was not statistically significant for attention bias scores at POST (z = .34, p = .73; Cohen’s d = 0.22) or Follow-Up (z = −.28, p = .78; Cohen’s d = 0.29), indicating no significant differences between study arms. Collapsing across study arms, mean attention bias scores did not significantly differ between PRE and POST, nor between POST and Follow-Up. In fixed effects panel regression analyses, changes in attention bias scores were not significantly associated with changes in anxiety severity.
The Time x Study Arm interaction effect was not statistically significant for total attention control, Attention Focusing, or Attention Shifting scores at POST or Follow-Up, indicating no significant differences between study arms. Collapsing across study arms, mean total attention control scores were significantly higher at Follow-Up than PRE (z = 4.24, p < .001; Cohen’s d = 0.73) and POST (z = 2.38, p < .05; Cohen’s d = 0.37). Collapsing across study arms, mean Attention Focusing scores were significantly higher at Follow-Up than PRE (z = 2.71, p = .007; Cohen’s d = −0.52) and POST (z = 2.50, p = .012; Cohen’s d = −0.29), and the Attention Shifting scores were significantly higher at Follow-Up than PRE (z = 2.00, p = .045; Cohen’s d = −0.29) but not POST (z = .76, p = .45; Cohen’s d = 0.13).
In fixed effects panel regression analyses, changes in total attention control (coefficient = −0.52, z = 2.91, p < .01) and Attention Focusing (coefficient = −0.69, z = 3.26, p = .001), but not Attention Shifting, were significantly associated with changes in anxiety severity on the SCARED-C. These coefficients indicate that SCARED-C scores decreased on average by 0.52 units for every one unit increase in attention control and by 0.69 units for every one unit increase in Attention Focusing. Changes in total attention control, Attention Focusing, or Attention Shifting scores were not significantly associated with changes in anxiety severity on the PARS or SCARED-P.
Discussion
In this sample of clinic-referred youths with concerning anxiety, we found statistically significant reductions in anxiety severity and global impairment from PRE to POST in both ABMT and ACT, with medium to large effect sizes for independent evaluator ratings, youth self-ratings, and parent ratings and reliable change in 29% to 47% of participants. These reductions were maintained at a two-month Follow-Up. Contrary to hypotheses, we found significantly greater reductions in youth anxiety severity and global impairment at Follow-Up in ACT compared with ABMT, again with medium to large effect sizes. These data therefore reveal successful anxiety reduction effects using low intensity treatment in clinic-referred youths with concerning anxiety.
These data and revelation are important because they support the viability of attention training, a low intensity treatment, to reduce concerning youth anxiety levels – impairing problems that have been sorely under-researched. We acknowledge though that our data raise tantalizing questions that require further research. We highlight these questions below and suggest possible answers. We hope this discussion will spark increased “attention on attention training” approaches and enhance conceptual understanding of these treatments including mechanisms of action, and lead to more efficacious and efficient treatments.
Two tantalizing and intertwined questions relate to the optimal contingencies to use in attention training for concerning anxiety in youth and the mechanisms by which attention training reduces concerning anxiety in youth. The current findings raise the possibility that the 50% neutral training contingency in ACT may produce superior effects compared with the 100% neutral training contingency in ABMT. These findings were statistically significant using youth self-ratings of anxiety and parent ratings of youth impairment, although the pattern of lower anxiety and impairment in ACT was present across all informants (albeit not always statistically significant). When a threat appears, it is adaptive to rapidly orient attention to the threat to evaluate for potential relevance and initiate cognitive-affective processes related to defense or escape, as needed. If the threat is not relevant, attention control is needed to disengage attention from the threat, shift attention to back task-relevant stimuli, and maintain attentional focus on task-relevant stimuli (Shi, Sharpe, & Abbott, 2019). The balanced contingency in ACT may train more flexible deployment of attention by requiring participants to maintain focus on task-relevant stimuli and ignore distracting threatening stimuli that are irrelevant to efficient completion of the task (Badura-Brack et al., 2015; Lazarov et al., 2019), possibly resulting in more reductions in anxiety and related impairment.
Our finding that the focusing component of attention control was associated with reductions in anxiety severity is also consistent with this possibility that sustaining attention in the presence of a distracting threat is a key mechanism in attention training’s anxiety-reducing effects. Our finding that total attention control and focusing, but not shifting, were significantly associated with reductions in anxiety severity represents an important and initial step in developing mechanistic understanding of attention training’s anxiety-reduction effects. For example, improvements in the ability to maintain focus on task-relevant stimuli in the presence of distracting threats may be central to anxiety reductions. Further research is needed to test this idea.
Overall, the current findings contribute to the growing evidence supporting attention control as critical to the anxiety-reduction effects of attention training, dampening the earlier conceptualization of decreases in attention bias to threat as a key mechanism to anxiety reductions (Heeren et al., 2015; Linetzky et al., 2020; Pettit et al., 2020). The lack of significant effects of treatment arm on attention control, however, is consistent with findings of some prior RCTs in youth with anxiety disorders, highlighting the need for further mechanistic research before concluding attention control is indeed a key mechanism of anxiety reduction (de Voogd et al., 2016; Linetzky et al., 2020; Pettit et al., 2020).
Overall, these findings highlight the need for more research on the optimal attention training schedules for enhancing attention control and its components among youth with concerning anxiety. This includes research that systematically manipulates both the training contingencies (e.g., 10% neutral versus 50% neutral vs. 90% neutral), and the presence versus absence of distracting threat stimuli to test whether balanced contingencies result in more flexible deployment of attention, and whether effects on attention are most salient in the presence of a distracting threat.
Another tantalizing question pertains to what the optimal approach to help clinic-referred youth with concerning anxiety might be, especially when considered within the context of the observed effect sizes. The medium to large effect sizes for reductions in anxiety severity and impairment support the viability of low intensity treatment. The size of anxiety- and impairment-reduction effects is encouraging given the resource-light features (e.g., time, personal investment) of attention training. Also encouraging is that over 90% of participants attended all 8 training sessions, further supporting the viability of low intensity treatment. As we noted earlier, identifying efficacious, resource-light treatments is critical given data showing only 22% of youths with diagnosable anxiety disorders access mental health services (Costello et al., 2014). Lengthy, resource-heavy treatments perhaps could be reserved for severe cases and/or for youths with concerning anxiety who have completed but not benefited from attention training. Importantly, our prior research supports not only the promise but also the cost-effectiveness of attention training as a low intensity treatment in a stepped care approach in youths with anxiety disorders, with higher intensity cognitive behavioral therapy delivered to the subset of youth who did not benefit from attention training (Pettit et al., 2017; Yeguez et al., 2020). Further development and evaluation of this and other strategies for leveraging attention training to treat concerning anxiety is warranted to improve efforts to reduce youth’s distress and impairment while using limited resources efficiently. As such development and evaluation work progresses, a key consideration will be ensuring access to treatment without compromising anxiety-reduction effects. Recent efforts to deliver attention training in schools and remotely under clinician supervision represent promising steps in this direction (Alon, Azriel, Pine, & Bar-Haim, 2022; Waters et al., 2019).
This study has several strengths and limitations. Strengths include the double-blind, randomized controlled design, the multi-informant assessment approach, the use of independent evaluators, and the assessment of global impairment. Another strength is our focus on clinic-referred youths with concerning anxiety, as noted a prevalent and understudied population. Further, the high representation of Hispanic/Latino youth in this sample (66%) is a strength given the longstanding underrepresentation of such youth in anxiety treatment research in general (Pina, Polo, & Huey, 2019; Pina, Silverman, Fuentes, Kurtines, & Weems, 2003) and attention training research specifically. We know of only two prior trials of attention training in predominantly Hispanic/Latino youth samples with anxiety disorders, both of which supported attention training’s anxiety-reducing effects (Pettit et al., 2020; Pettit et al., 2017). We were unable to examine the influence of youth ethnicity on response to attention training in this study, although others have noted it is possible the use of non-linguistic training stimuli (i.e., faces) may make it amenable to youth from diverse ethnic and linguistic backgrounds (Amir, Taylor, & Donohue, 2011).
A study limitation is the absence of a no treatment control arm and an alternative comparison arm. Only three trials of attention training for youth anxiety have included a no treatment control arm; each trial evaluated a remotely-administered visual search for positive stimuli training task, two among youth with anxiety disorders (Waters et al., 2015, 2016) and one among unselected youth (de Voogd et al., 2017). The two trials among youth with anxiety disorders found significantly enhanced anxiety reductions in the active arms compared with the no treatment control arm; the trial among unselected youth found comparable anxiety reductions in all arms. As noted by others (Chang et al., 2019; Mogg, Waters, & Bradley, 2017), a no treatment control arm would have allowed us to parse out effects due to repeated assessment, regression to the mean, and spontaneous remission in this sample of clinic-referred youth with concerning anxiety. An alternative comparator arm that did not target attention control would allow for firmer inferences about whether enhancements in attention control accounts for reductions in anxiety severity (Linetzky et al., 2020). Additional limitations include the relatively small sample, which hindered statistical power to detect small effects, an absence of an independent measure of attention to threat that does not use the dot-probe paradigm, and a reliance on a rating scale to measure attention control. In an ongoing trial of attention training (ClinicalTrials.gov Identifier: NCT03932032), we supplement rating scales with other tasks (e.g., antisaccade; Cardinale et al., 2019) and methods (e.g., electroencephalography; Bechor et al., 2019; Thai, Taber-Thomas, & Perez-Edgar, 2016) to measure attention control and attention allocation to threat. With the cumulation of data from multiple tasks and methodologies, researchers will be positioned to advance theory and treatment development by mapping patterns of attention onto neural circuitry and behavioral phenotypes of anxiety (Pettit & Silverman, 2020).
In summary, the current study supports the viability of low intensity treatments that involve attention training for youth with concerning anxiety. These novel data provide the impetus for further efforts to help this population of youth while maximizing use of limited treatment resources effectively and efficiently. This demonstration of anxiety reduction in a clinic setting also supports investigation of attention training in community or school settings where there are higher numbers of youth with concerning anxiety (e.g., de Voogd et al., 2017; Waters et al., 2019). The data further set the stage for additional mechanistic research on attention training protocols, using alternative comparison arms and investigating optimal training contingencies for targeting attention control.
Highlights.
Tested attention training for concerning anxiety in youth
Attention training led to reductions in anxiety severity and global impairment
Changes in attention control were associated with changes in anxiety
Findings support the viability of attention training for concerning anxiety
Acknowledgements:
We gratefully acknowledge Deepika Bose, MS, Victor Buitron, PhD, Yesenia Martinez, LMHC, Alyssa Martino, MS, Raquel Melendez, PhD, and Daniella Vaclavik, MS for their assistance in administering attention training sessions and collecting data.
Declarations:
This research was supported by National Institutes of Health grant UH MH101470 and NIMH-IRP Project ZIA-MH002781. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors report no financial interests or conflicts of interest.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abend R, de Voogd L, Salemink E, Wiers RW, Perez-Edgar K, Fitzgerald A, … Bar-Haim Y (2018). Association between attention bias to threat and anxiety symptoms in children and adolescents. Depression & Anxiety, 35(3), 229–238. doi: 10.1002/da.22706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abend R, Pine DS, & Bar-Haim Y (2014). The TAU-NIMH Attention Bias Measurement Toolbox. Available from: http://people.socsci.tau.ac.il/mu/anxietytrauma/research/. [Google Scholar]
- Allison P (2009). Fixed effects regression modeling. Thousand Oaks, CA: Sage. [Google Scholar]
- Alon Y, Azriel O, Pine DS, & Bar-Haim Y (2022). A randomized controlled trial of supervised remotely-delivered attention bias modification for posttraumatic stress disorder. Psychological Medicine, 1–10. doi: 10.1017/S003329172200023X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N, Taylor CT, & Donohue MC (2011). Predictors of response to an attention modification program in generalized social phobia. Journal of Consulting and Clinical Psychology, 79(4), 533–541. doi: 10.1037/a0023808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Farmer EM, Burns BJ, & Erkanli A (1999). Impaired but undiagnosed. Journal of the American Academy of Child & Adolescent Psychiatry, 38(2), 129–137. doi: 10.1097/00004583-199902000-00011 [DOI] [PubMed] [Google Scholar]
- Badura-Brack AS, Naim R, Ryan TJ, Levy O, Abend R, Khanna MM, … Bar-Haim Y (2015). Effect of attention training on attention bias variability and PTSD symptoms: randomized controlled trials in Israeli and U.S. combat veterans. American Journal of Psychiatry, 172(12), 1233–1241. doi: 10.1176/appi.ajp.2015.14121578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balàzs J, Miklosi M, Kereszteny A, Hoven CW, Carli V, Wasserman C, … Wasserman D (2013). Adolescent subthreshold-depression and anxiety: psychopathology, functional impairment and increased suicide risk. Journal of Child Psychology & Psychiatry, 54(6), 670–677. doi: 10.1111/jcpp.12016 [DOI] [PubMed] [Google Scholar]
- Bechor M, Ramos ML, Crowley MJ, Silverman WK, Pettit JW, & Reeb-Sutherland BC (2019). Neural correlates of attentional processing of threat in youth with and without anxiety disorders. Journal of Abnormal Child Psychology, 47(1), 119–129. doi: 10.1007/s10802-018-0424-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belin TR, & Normand SLT (2009). The Role of ANCOVA in analyzing experimental data. Psychiatric Annals, 39(7), 753-+. doi:Doi 10.3928/00485713-20090625-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird HR, Shaffer D, Fisher P, Gould MS, Staghezza B, Chen JY, & Hoven C (1993). The Columbia-Impairment-Scale (Cis) - pilot findings on a measure of global impairment for children and adolescents. International Journal of Methods in Psychiatric Research, 3(3), 167–176. [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, & Neer SM (1997). The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry, 36(4), 545–553. doi: 10.1097/00004583-199704000-00018 [DOI] [PubMed] [Google Scholar]
- Cardinale EM, Subar AR, Brotman MA, Leibenluft E, Kircanski K, & Pine DS (2019). Inhibitory control and emotion dysregulation: A framework for research on anxiety. Development & Psychopathology, 31(3), 859–869. doi: 10.1017/S0954579419000300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang SW, Kuckertz JM, Bose D, Carmona AR, Piacentini J, & Amir N (2019). Efficacy of attention bias training for child anxiety disorders: a randomized controlled trial. Child Psychiatry & Human Development, 50(2), 198–208. doi: 10.1007/s10578-018-0832-6 [DOI] [PubMed] [Google Scholar]
- Costello EJ, He JP, Sampson NA, Kessler RC, & Merikangas KR (2014). Services for adolescents with psychiatric disorders: 12-month data from the National Comorbidity Survey-Adolescent. Psychiatric Services, 65(3), 359–366. doi: 10.1176/appi.ps.201100518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Haan AM, Boon AE, de Jong JTVM, Hoeve M, & Vermeiren RRJM (2013). A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clinical Psychology Review, 33(5), 698–711. doi: 10.1016/j.cpr.2013.04.005 [DOI] [PubMed] [Google Scholar]
- de Voogd EL, Wiers RW, Prins PJM, de Jong PJ, Boendermaker WJ, Zwitser RJ, & Salemink E (2016). Online attentional bias modification training targeting anxiety and depression in unselected adolescents: Short- and long-term effects of a randomized controlled trial. Behaviour Research & Therapy, 87, 11–22. doi: 10.1016/j.brat.2016.08.018 [DOI] [PubMed] [Google Scholar]
- de Voogd EL, Wiers RW, & Salemink E (2017). Online visual search attentional bias modification for adolescents with heightened anxiety and depressive symptoms: A randomized controlled trial. Behaviour Research & Therapy, 92, 57–67. doi: 10.1016/j.brat.2017.02.006 [DOI] [PubMed] [Google Scholar]
- Dudeney J, Sharpe L, & Hunt C (2015). Attentional bias towards threatening stimuli in children with anxiety: A meta-analysis. Clinical Psychology Review, 40, 66–75. doi: 10.1016/j.cpr.2015.05.007 [DOI] [PubMed] [Google Scholar]
- Eldar S, Apter A, Lotan D, Edgar KP, Naim R, Fox NA, … Bar-Haim Y (2012). Attention bias modification treatment for pediatric anxiety disorders: a randomized controlled trial. American Journal of Psychiatry, 169(2), 213–220. doi: 10.1176/appi/ajp.2011/11060886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldar S, Yankelevitch R, Lamy D, & Bar-Haim Y (2010). Enhanced neural reactivity and selective attention to threat in anxiety. Biological Psychology, 85(2), 252–257. doi: 10.1016/j.biopsycho.2010.07.010 [DOI] [PubMed] [Google Scholar]
- Enders CK (2010). Applied missing data analysis. New York: Guilford Publications. [Google Scholar]
- Fodor LA, Georgescu R, Cuijpers P, Szamoskozi S, David D, Furukawa TA, & Cristea IA (2020). Efficacy of cognitive bias modification interventions in anxiety and depressive disorders: a systematic review and network meta-analysis. Lancet Psychiatry, 7(6), 506–514. doi: 10.1016/S2215-0366(20)30130-9 [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Keeton CP, Drazdowski TK, & Riddle MA (2011). The utility of clinicians ratings of anxiety using the Pediatric Anxiety Rating Scale (PARS). Child & Youth Care Forum, 40(2), 93–105. doi: 10.1007/s10566-010-9125-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grist R, Croker A, Denne M, & Stallard P (2019). Technology delivered interventions for depression and anxiety in children and adolescents: a systematic review and meta-analysis. Clinical Child & Family Psychology Review, 22(2), 147–171. doi: 10.1007/s10567-018-0271-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakamata Y, Lissek S, Bar-Haim Y, Britton JC, Fox NA, Leibenluft E, … Pine DS (2010). Attention bias modification treatment: a meta-analysis toward the establishment of novel treatment for anxiety. Biological Psychiatry, 68(11), 982–990. doi: 10.1016/j.biopsych.2010.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hang Y, Zhang G, Wang C, Zhang N, & Liu G (2021). Attention bias modification for anxiety disorders in children and adolescents: A systematic review and meta-analysis. Psychiatry Research, 300, 113896. doi: 10.1016/j.psychres.2021.113896 [DOI] [PubMed] [Google Scholar]
- Harpaz-Rotem I, Leslie D, & Rosenheck RA (2004). Treatment retention among children entering a new episode of mental health care. Psychiatric Services, 55(9), 1022–1028. doi: 10.1176/appi.ps.55.9.1022 [DOI] [PubMed] [Google Scholar]
- Heeren A, Mogoase C, McNally RJ, Schmitz A, & Philippot P (2015). Does attention bias modification improve attentional control? A double-blind randomized experiment with individuals with social anxiety disorder. Journal of Anxiety Disorders, 29, 35–42. doi: 10.1016/j.janxdis.2014.10.007 [DOI] [PubMed] [Google Scholar]
- Higa-McMillan CK, Francis SE, Rith-Najarian L, & Chorpita BF (2016). Evidence base update: 50 years of research on treatment for child and adolescent anxiety. Journal of Clinical Child and Adolescent Psychology, 45(2), 91–113. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, & Truax P (1991). Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. doi: 10.1037//0022-006x.59.1.12 [DOI] [PubMed] [Google Scholar]
- Kendall PC, Makover H, Swan A, Carper MM, Mercado R, Kagan E, & Crawford E (2016). What steps to take? How to approach concerning anxiety in youth. Clinical Psychology-Science and Practice, 23(3), 211–229. doi: 10.1111/cpsp.12156 [DOI] [Google Scholar]
- Lazarov A, Suarez-Jimenez B, Abend R, Naim R, Shvil E, Helpman L, … Neria Y (2019). Bias-contingent attention bias modification and attention control training in treatment of PTSD: a randomized control trial. Psychological Medicine, 49(14), 2432–2440. doi: 10.1017/S0033291718003367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linetzky M, Pettit JW, Silverman WK, Pine DS, & Bar-Haim Y (2020). What drives symptom reduction in attention bias modification treatment? A randomized controlled experiment in clinically anxious youths. Clinical Psychological Science, 8(3), 506–518. doi: 10.1177/2167702620902130 [DOI] [Google Scholar]
- Liu P, Taber-Thomas BC, Fu X, & Perez-Edgar KE (2018). Biobehavioral markers of attention bias modification in temperamental risk for anxiety: a randomized control trial. Journal of the American Academy of Child & Adolescent Psychiatry, 57(2), 103–110. doi: 10.1016/j.jaac.2017.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLeod C, & Clarke PJF (2015). The attentional bias modification approach to anxiety intervention. Clinical Psychological Science, 3(1), 58–78. [Google Scholar]
- Melendez R, Bechor M, Rey Y, Pettit JW, & Silverman WK (2017). Attentional Control Scale for Children: Factor structure and concurrent validity among children and adolescents referred for anxiety disorders. Journal of Clinical Psychology, 73(4), 489–499. doi: 10.1002/jclp.22346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogg K, Waters AM, & Bradley BP (2017). Attention bias modification (ABM): review of effects of multisession ABM training on anxiety and threat-related attention in high-anxious individuals. Clinical Psychological Science, 5(4), 698–717. doi: 10.1177/2167702617696359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, de Jong PJ, & Engelen S (2004). Relationships between neuroticism, attentional control, and anxiety disorders symptoms in non-clinical children. Personality and Individual Differences, 37(4), 789–797. doi: 10.1016/j.paid.2003.10.007 [DOI] [Google Scholar]
- Pergamin-Hight L, Pine DS, Fox NA, & Bar-Haim Y (2016). Attention bias modification for youth with social anxiety disorder. Journal of Child Psychology & Psychiatry, 57(11), 1317–1325. doi: 10.1111/jcpp.12599 [DOI] [PubMed] [Google Scholar]
- Pettit JW, Bechor M, Rey Y, Vasey MW, Abend R, Pine DS, … Silverman WK (2020). A randomized controlled trial of attention bias modification treatment in youth with treatment-resistant anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 59(1), 157–165. doi: 10.1016/j.jaac.2019.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettit JW, Rey Y, Bechor M, Melendez R, Vaclavik D, Buitron V, … Silverman WK (2017). Can less be more? Open trial of a stepped care approach for child and adolescent anxiety disorders. Journal of Anxiety Disorders, 51, 7–13. doi: 10.1016/j.janxdis.2017.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettit JW, & Silverman WK (2020). Editorial: Attention to threat in child anxiety: gazing into the future while keeping sight of the past. Journal of the American Academy of Child & Adolescent Psychiatry, 59(1), 33–35. doi: 10.1016/j.jaac.2019.09.019 [DOI] [PubMed] [Google Scholar]
- Pina AA, Polo AJ, & Huey SJ (2019). Evidence-based psychosocial interventions for ethnic minority youth: the 10-year update. Journal of Clinical Child and Adolescent Psychology, 48(2), 179–202. doi: 10.1080/15374416.2019.1567350 [DOI] [PubMed] [Google Scholar]
- Pina AA, Silverman WK, Fuentes RM, Kurtines WM, & Weems CF (2003). Exposure-based cognitive-behavioral treatment for phobic and anxiety disorders: Treatment effects and maintenance for Hispanic/Latino relative to European-American youths. Journal of the American Academy of Child and Adolescent Psychiatry, 42(10), 1179–1187. doi: 10.1097/01.chi.0000081804.49840.02 [DOI] [PubMed] [Google Scholar]
- Pocock SJ, Assmann SE, Enos LE, & Kasten LE (2002). Subgroup analysis, covariate adjustment and baseline comparisons in clinical trial reporting: current practice and problems. Statistics in Medicine, 21(19), 2917–2930. doi: 10.1002/sim.1296 [DOI] [PubMed] [Google Scholar]
- Price RB, Kuckertz JM, Amir N, Bar-Haim Y, Carlbring P, & Wallace ML (2017). Less is more: Patient-level meta-analysis reveals paradoxical dose-response effects of a computer-based social anxiety intervention targeting attentional bias. Depression & Anxiety, 34(12), 1106–1115. doi: 10.1002/da.22634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price RB, Wallace M, Kuckertz JM, Amir N, Graur S, Cummings L, … Bar-Haim Y (2016). Pooled patient-level meta-analysis of children and adults completing a computer-based anxiety intervention targeting attentional bias. Clinical Psychology Review, 50, 37–49. doi: 10.1016/j.cpr.2016.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rausch JR, Maxwell SE, & Kelley K (2003). Analytic methods for questions pertaining to a randomized pretest, posttest, follow-up design. Journal of Clinical Child & Adolescent Psychology, 32(3), 467–486. doi: 10.1207/S15374424JCCP3203_15 [DOI] [PubMed] [Google Scholar]
- Revelle W, & Condon DM (2019). Reliability from alpha to omega: A tutorial. Psychological Assessment, 31(12), 1395–1411. doi: 10.1037/pas0000754 [DOI] [PubMed] [Google Scholar]
- Roberts RE, Fisher PW, Turner JB, & Tang M (2015). Estimating the burden of psychiatric disorders in adolescence: the impact of subthreshold disorders. Social Psychiatry & Psychiatric Epidemiology, 50(3), 397–406. doi: 10.1007/s00127-014-0972-3 [DOI] [PubMed] [Google Scholar]
- RUPP Anxiety Study Group. (2002). The Pediatric Anxiety Rating Scale (PARS): development and psychometric properties. Journal of the American Academy of Child & Adolescent Psychiatry, 41(9), 1061–1069. [DOI] [PubMed] [Google Scholar]
- Shechner T, Rimon-Chakir A, Britton JC, Lotan D, Apter A, Bliese PD, … Bar-Haim Y (2014). Attention bias modification treatment augmenting effects on cognitive behavioral therapy in children with anxiety: randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), 61–71. doi: 10.1016/j.jaac.2013.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi R, Sharpe L, & Abbott M (2019). A meta-analysis of the relationship between anxiety and attentional control. Clinical Psychology Review, 72, 101754. doi: 10.1016/j.cpr.2019.101754 [DOI] [PubMed] [Google Scholar]
- Silverman WK, & Albano AM (1996). Anxiety Disorders Interview Schedule for Children-IV (Child and Parent Versions). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Silverman WK, Pettit JW, & Lebowitz ER (2016). Stepping toward making less more for concerning anxiety in children and adolescents. Clinical Psychology-Science and Practice, 23(3), 234–238. doi: 10.1111/cpsp.12158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, Pina AA, & Viswesvaran C (2008). Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 37(1), 105–130. doi: 10.1080/15374410701817907 [DOI] [PubMed] [Google Scholar]
- Silverman WK, Saavedra LM, & Pina AA (2001). Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. Journal of the American Academy of Child & Adolescent Psychiatry, 40(8), 937–944. doi: 10.1097/00004583-200108000-00016 [DOI] [PubMed] [Google Scholar]
- Thai N, Taber-Thomas BC, & Perez-Edgar KE (2016). Neural correlates of attention biases, behavioral inhibition, and social anxiety in children: An ERP study. Developmental Cognitive Neuroscience, 19, 200–210. doi: 10.1016/j.dcn.2016.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Buuren S (2007). Multiple imputation of discrete and continuous data by fully conditioned specification. Statistical methods in medical research, 16(3), 219–242. [DOI] [PubMed] [Google Scholar]
- van Son D, Marin CE, Boutris P, Rey Y, Lebowitz ER, Pettit JW, & Silverman WK (2021). Attending to the Attentional Control Scale for Children: Confirming its factor structure and measurement invariance. Journal of Anxiety Disorders, 80, 102399. doi: 10.1016/j.janxdis.2021.102399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters AM, Candy SG, Zimmer-Gembeck MJ, Groth TA, Craske MG, Bradley BP, & Mogg K (2019). A school-based comparison of positive search training to enhance adaptive attention regulation with a cognitive-behavioural intervention for reducing anxiety symptoms in children. Journal of Abnormal Child Psychology, 47(11), 1821–1840. doi: 10.1007/s10802-019-00551-4 [DOI] [PubMed] [Google Scholar]
- Waters AM, Zimmer-Gembeck MJ, Craske MG, Pine DS, Bradley BP, & Mogg K (2015). Look for good and never give up: A novel attention training treatment for childhood anxiety disorders. Behaviour Research and Therapy, 73, 111–123. doi: 10.1016/j.brat.2015.08.005 [DOI] [PubMed] [Google Scholar]
- Waters AM, Zimmer-Gembeck MJ, Craske MG, Pine DS, Bradley BP, & Mogg K (2016). A preliminary evaluation of a home-based, computer-delivered attention training treatment for anxious children living in regional communities. Journal of Experimental Psychopathology, 7(3), 511–527. doi: 10.5127/jep.053315 [DOI] [Google Scholar]
- Werner-Seidler A, Perry Y, Calear AL, Newby JM, & Christensen H (2017). School-based depression and anxiety prevention programs for young people: A systematic review and meta-analysis. Clinical Psychology Review, 51, 30–47. doi: 10.1016/j.cpr.2016.10.005 [DOI] [PubMed] [Google Scholar]
- Winters NC, Collett BR, & Myers KM (2005). Ten-year review of rating functional scales, VII: Scales assessing impairment. Journal of the American Academy of Child and Adolescent Psychiatry, 44(4), 309–338. doi: 10.1097/01.chi.0000153230.57344.cd [DOI] [PubMed] [Google Scholar]
- Yeguez CE, Page TF, Rey Y, Silverman WK, & Pettit JW (2020). A cost analysis of a stepped care treatment approach for anxiety disorders in youth. Journal of Clinical Child & Adolescent Psychology, 49(4), 549–555. doi: 10.1080/15374416.2018.1539913 [DOI] [PMC free article] [PubMed] [Google Scholar]