Abstract
Rationale, aims, and objectives
Chronic pain is a global public health problem that negatively impacts individuals' quality of life and imposes a substantial economic burden on societies. The use of medicinal cannabis (MC) is often considered by patients to help manage chronic pain as an alternative or supplement to more conventional treatments, given enabling legalization in a number of countries. However, healthcare professionals involved in providing guidance for patients related to MC are often doing so in the absence of strong evidence and clinical guidelines. Therefore, it is crucial to understand their perspectives regarding the clinical use and relevance of MC for chronic pain. As little is known about attitudes of HCPs with regard to MC use for chronic pain specifically, the aim of this review was to identify and synthesize the published evidence on this topic.
Methods
A systematic search was conducted across six databases: MEDLINE, EMBASE, CINAHL, Scopus, Web of Science, and PubMed from 2001 to March 26, 2021. Three authors independently performed the study selection and data extraction. Thematic analysis was undertaken to identify key themes.
Results
A total of 26 studies were included, involving the United States, Israel, Canada, Australia, Ireland, and Norway, and the perspectives of physicians, nurses, and pharmacists. Seven key themes were identified: MC as a treatment option for chronic pain, and perceived indicated uses; willingness to prescribe MC; legal issues; low perceived knowledge and the need for education; comparative safety of MC versus opioids; addiction and abuse; and perceived adverse effects;
Conclusion
To support best practice in the use of MC for chronic pain, healthcare professionals require education and training, as well as clinical guidelines that provide evidence‐based information about efficacy, safety, and appropriate dosage of products for this indication. Until these gaps are addressed, healthcare professionals will be limited in their capacity to make treatment recommendations about MC for people/patients with chronic pain.
Keywords: chronic pain, healthcare professionals, medicinal cannabis, narrative review, perspectives
INTRODUCTION
Chronic pain is a global public health problem that can restrict an individual's physical activity and reduce their quality of life. 1 It also places a substantial economic burden on individuals, healthcare systems, and societies due to the costs of pharmaceuticals, healthcare, productivity loss, and absenteeism. 2 Due to the complex nature of chronic pain, the clinical management often involves a range of treatment modalities, including pharmaceutical and psychological treatments, but is often insufficient to provide enough relief. 3 Thus, many people living with chronic pain have turned to novel and alternative approaches, such as medicinal cannabis (MC), to manage their pain. Ineffective analgesia and a preference for nonopioid treatment are known precipitators for patients to explore the use of MC. 4 Chronic pain is one of the major reasons for MC use. 5 , 6 , 7 , 8
Within this context, several countries have introduced legislation in the past two decades to legalize cannabis for therapeutic use. Despite the evident shifts in legislation internationally, there has not been the same progress in building the evidence base of randomized clinical trials to support the use of MC for chronic pain. 9 Several studies have gathered patient perspectives regarding the benefits of MC for pain control. 10 , 11 , 12 , 13 While patient perspectives provide important experiential evidence, gaps remain in the scientific evidence related to MC's effectiveness as a pharmacological treatment for chronic pain. Systematic reviews of placebo‐controlled trial data point out the difficulties in comparisons across clinical trials due to, for example, small sample sizes and short duration of studies to measure the outcome of pain control. 14 , 15 , 16 , 17 , 18 It was also noted that studies used different MC products which varied in cannabinoid content and formulation, and studied different chronic pain phenotypes, which make it inappropriate to directly compare data. There is a need for high‐quality randomized controlled trials which use a standardized MC product in a defined pain phenotypic population. However, there are unique ethical factors involved in MC research in humans due to its classification as a prohibited drug across much of the world. 19 In summary, the limitations of the existing evidence coupled with the growth in demand pose a dilemma for healthcare professionals who are caught between patient reports of effectiveness and the absence of high‐quality clinical trials and clinical guidance.
As healthcare professionals are essential for the delivery of healthcare services, their views on the appropriateness of MC use for chronic pain will affect their provision of MC to their patients. Several systematic reviews have been published regarding the effectiveness of MC for different types of pain, 20 , 21 , 22 but these did not elicit the views of the healthcare professionals tasked with prescribing, dispensing, or administering MC.
To date, one systematic review by Gardiner et al. 23 has been published on healthcare professionals' beliefs, knowledge, and concerns surrounding MC use, however, this considered medicinal use generally and did not focus on chronic pain. The authors concluded that healthcare professionals generally supported MC use in clinical practice but lacked confidence and self‐perceived competence; lacked self‐perceived knowledge about MC in legislative and clinical domains; and held concerns over psychiatric adverse effects and societal harm from recreational misuse of MC.
The aim of our systematic search and narrative review is to build on previous research to identify and synthesize the existing literature on the perspectives of healthcare professionals about the use of MC in the clinical management of chronic pain. For the purposes of this review, MC refers to cannabis that has been prescribed by a healthcare professional for medical purposes and excludes recreational use or self‐medication.
METHODS
To meet the aims of this study, we adopted a systematic search and narrative review approach to capture publications of interest from a broad range of published studies, 24 inclusive of study designs and methods, both quantitative and qualitative, that aimed to capture the perspectives of healthcare professionals.
Search strategy
The following databases were searched: MEDLINE, EMBASE, CINAHL, Scopus, Web of Science, and PubMed. Publications from 2001, the year of the first instance of legalization of cannabis for medicinal use in the world as introduced by Canada, to March 26, 2021 were included. A systematic search of the literature was conducted by creating search strategies for each database, which were modified in accordance with the subject headings and keywords specific to each database. Keywords used were “cannabis,” “marijuana,” “weed,” “hemp,” “CBD,” “THC,” and “chronic pain.” An example search strategy for MEDLINE can be seen in Figure 1. An academic health services librarian was engaged to help refine the search. Additionally, the reference lists of relevant articles were inspected to identify additional publications that were not retrieved via the database search.
FIGURE 1.
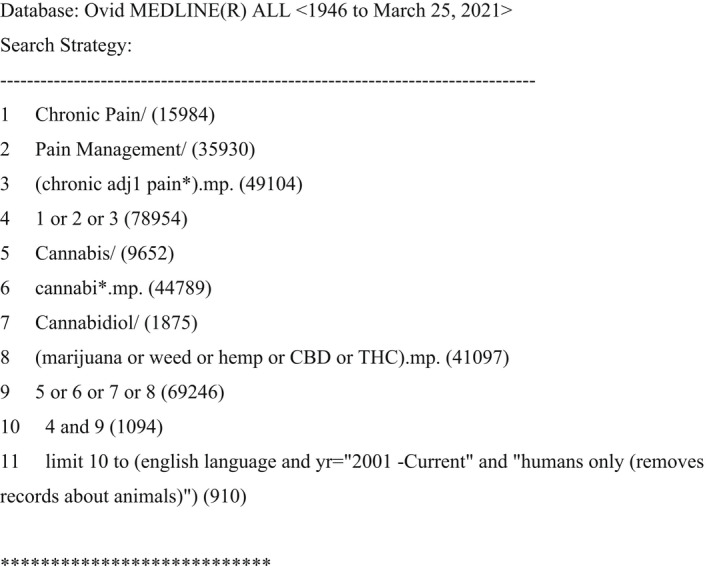
Unique search strategy applied to the MEDLINE database
Study screening
This systematic search followed the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) checklist (Figure 2). A screening of titles and abstracts was performed by KC to select potentially relevant publications. A second screening of full‐text articles was conducted by KC, LS, and JH to assess the eligibility for inclusion in the review and resolve any conflicts. Articles which contained limited data on chronic pain were discussed between the three authors to judge their eligibility for inclusion in this review. Inclusion criteria were: healthcare professional participants; related to “medicinal” cannabis; related to the indication of chronic pain; related to perspectives; of English language; human studies; publication date (2001 to March 26, 2021); journal articles or primary studies. Exclusion criteria were: participants did not involve healthcare professionals; related to “recreational” cannabis; contained insufficient information about chronic pain as an indication; non‐English publications; animal studies; reviews, meta‐analyses, gray literature, conference abstracts, editorials, commentaries, books, or book chapters.
FIGURE 2.
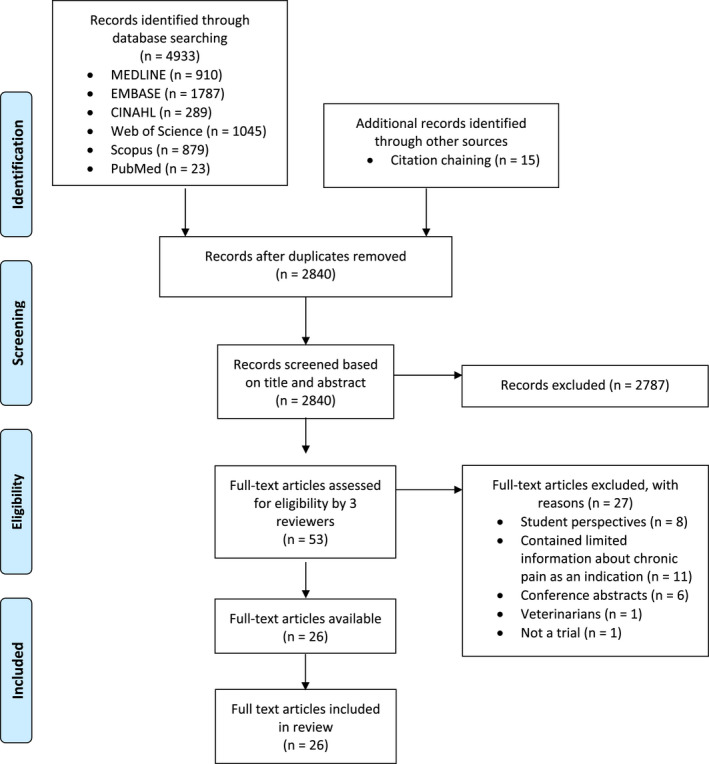
PRISMA flow chart of included and excluded publications regarding the use of medicinal cannabis in chronic pain management.
Data analysis
Data analysis was carried out by first organizing the included studies into a table showing authors, publication year, country, aims, study design, sample size, and relevant study findings (Tables 1 and 2). Next, the studies' findings were systematically and thematically analyzed by discussion between the authors to identify common topics and patterns of meaning, as well as negative or deviant cases (viewpoints that deviated from the main body of evidence). 25
TABLE 1.
Studies included in this review about chronic noncancer pain
| Author (Year), Country | Aims | Study design | Sample | Study findings |
|---|---|---|---|---|
| Ablin et al. (2016) 37 , Israel | Achieve a cross‐cultural comparison with Canada on rheumatologists' confidence of knowledge of MC | Survey from Fitzcharles et al. (2014) 43 study | N = 23 rheumatology specialists and residents | 78% rheumatologists were not confident in writing prescriptions for MC, 48% believed in its therapeutic role for rheumatic diseases, 51% have previously prescribed it. MC would be considered if patients were refractory to conventional treatment by 82.6% |
| Abo Ziad et al. (2020) 40 , Israel | Assess the attitudes and beliefs of Israeli family physicians on the use of MC and their knowledge on adverse effects and barriers to use | Survey | N = 152 physicians (97 specialists, 48 residents, three general practitioners) | High proportions of family physicians believed MC is effective in cancer pain (84.2%) and chronic pain (82.2%). They generally believed specialists in pain medicine and oncology should recommend it. They themselves were not willing to prescribe or only willing to a small extent |
| Arnfinsen et al. (2021) 50 , Norway | Assess Norwegian physicians' perceived knowledge of, experience with, and attitudes toward MC | Survey | N = 102 physicians | Of the physicians who were asked to choose justifications for why MC should be available by prescription in Norway, the majority stated that MC can improve the quality of life for patients with chronic pain and MC may reduce unnecessary use of opioids |
| Bega et al. (2017) 51 , International | Assess MC‐related practices, experiences, beliefs, and attitudes of neurologists across National Parkinson's Foundation Center of Excellence | Survey | N = 56 neurologists | Physicians described a lack of formal education on MC, reported obtaining their information from medical literature and personal experience, and wanted more attention to MC in the curricula. Concerning side effects noted include negative impact on memory, executive function, driving, and addiction |
| Carlini et al. (2015) 29 , U.S.A. | Assess Washington State's healthcare providers' MC knowledge, beliefs, clinical practices, and training needs | Survey | N = 494 healthcare providers (physicians, physician assistants, nurses, pharmacists) | Intractable pain was the leading indication for written authorizations. Despite healthcare providers' eligibility to write MC authorizations, the majority has not issued one. There was general support for formal training and concerns for addiction and psychiatric side effects |
| Collister et al. (2021) 45 , Canada | Elicit Canadian nephrologists' views regarding the use and study of MC in patients with kidney disease | Survey | N = 154 nephrologists | Chronic pain was one of the major indications for a MC prescription but only 19% of nephrologists have prescribed MC for it. Greater support for MC use in chronic pain if symptoms were refractory to or patients could not tolerate conventional treatment. However, nephrologists did not feel comfortable prescribing MC themselves and preferred someone else do it with more prescribing expertise and a license. Concerns expressed include the lack of evidence for safety and efficacy and uncertainty with dosing |
| Cooke et al. (2019) 26 , U.S.A. | Present patients' and clinicians' perspectives on the co‐use of MC and opioid among chronic noncancer pain patients with a history of a substance‐use disorder and their clinicians | Semistructured interviews | N = 23 primary care providers (18 physicians, four nurse practitioners, one physician assistant) | Clinicians did not routinely discuss MC with patients, but noted that MC was helpful to their patients in managing pain symptoms while on opioids. Clinicians were not comfortable to discuss and/or provide MC in clinical settings and expressed concerns about potential exacerbation of mental health issues with MC use |
| Crowley et al. (2017) 49 , Ireland | Investigate attitudes of Irish General Practitioners (GPs) attitudes toward decriminalization of MC and assess levels of support for use of MC | Survey | N = 565 GPs | >60% Irish GPs agreed that MC has a role in pain management and 58.6% supported legalization for medical use. Support for legalization was higher in those who were trained in addiction treatment (e.g., managing opioid users). Majority of Irish GPs did not support decriminalization of MC for recreational use but GPs with more advanced addiction specialist training supported decriminalization of MC |
| Ebert et al. (2015) 39 , Israel | Examine the experience, knowledge, and attitudes of Israeli physicians of different specialties toward MC, and assess whether physicians with more knowledge or experience have different attitudes than those who are less knowledgeable and experienced | Survey | N = 72 physicians (28 oncology, five pain, 20 psychiatry, 13 neurology, six rehabilitation) | Pain was two of the four most prevalent indications for MC use (chronic pain, cancer pain, chemotherapy‐induced symptoms, palliative care). Oncologists and pain physicians generally disagreed that MC undermined mental health. Physicians who recommended MC reported themselves having greater knowledge. Physicians unanimously agreed that more education on MC should be available to physicians and specific training should precede ability to recommend MC |
| Fitzcharles et al. (2014) 43 , Canada | Examine rheumatologists' confidence about cannabinoids in general and their ability to advise patients about MC | Survey | N = 128 rheumatologists | 45% rheumatologists believed there is no therapeutic role for MC in the management of rheumatic diseases, 70% have never previously recommended any form of MC for patients and 60% currently would not recommend a trial of any MC |
| Irvine et al. (2006) 46 , Australia | Obtain information about GPs' views on potential legalization of MC | Survey | N = 32 GPs | GPs generally regarded chronic pain as a MC‐treatable condition. They would prescribe MC if it was legal, backed up by research, and under a legalized regulatory scheme for indications. There was concern of bureaucracy of paperwork with the public knowing about MC access |
| Jacobs et al. (2019) 48 , Australia | Assess Australia psychiatrists' and psychiatry trainees' knowledge, attitudes, and concerns about MC | Survey | N = 23 psychiatrists | >2/3 respondents believed there was evidence for use of CBD and THC in treating chronic pain. They generally could not differentiate between CBD and THC indications. 55% were open to prescribing MC if it were legal. Greatest concerns regarded psychotic symptoms, recreational use (for intoxication), apathy, addiction, and dependence |
| Karanges et al. (2018) 47 , Australia | Examine the knowledge and attitudes of Australian GPs toward MC | Survey | N = 640 GPs | 61.5% GPs have fielded at least one enquiry about MC in the last 3 months, but half were not comfortable dealing with enquiries. They believed in the utility of MC, but generally did not want to prescribe MC, citing risk of abuse and dependence as primary concerns. GPs preferred training and accreditation or a shared care arrangement with a specialist instead of a specialist‐only prescribing approach. Most rated themselves having poor perceived knowledge of MC. There was a contrast in support for MC for patients with chronic cancer pain (80.2%) and chronic noncancer pain (39.1%) |
| Kondrad and Reid (2013) 28 , U.S.A. | Gather information about Colorado family physicians' experience with and attitudes toward MC | Survey | N = 520 family physicians | Despite Colorado having the highest per‐capita number of patients using MC, 31% of family physicians never recommended MC. Most physicians did not think there are significant health benefits to MC. Those who have not recommended MC before cited news media, practice policy, personal opinion, concerns of legal liability, and a lack of evidence as influencing factors. Physicians believed MC is predominantly used by people who want legal protection for recreational cannabis. They expressed a strong desire for educational opportunities |
| Mitchell et al. (2016) 44 , Canada | Determine hospital pharmacists' opinions about MC and their level of comfort in providing advice about MC to patients and other healthcare professionals | Survey | N = 769 hospital pharmacists | Majority obtained self‐directed education on MC. Despite limited education, 53.8% of hospital pharmacists have been confronted with questions about its use. 67% disagreed that they were knowledgeable about MC, and 50% completely disagreed that they were comfortable in providing advice to patients |
| Narouze et al. (2020) 31 , U.S.A. | Characterize pain physicians' advocacy and concerns regarding MC | Survey | N = 30 pain physicians | Pain physicians believed in the legitimacy and benefits of MC for physical symptoms and 76% have cared for patients on MC. However, 13% participants were actually registered in an MC program |
| Philpot et al. (2019) 36 , U.S.A. | Understand the attitudes, beliefs, and knowledge of primary care providers and identify ongoing barriers, biases, and knowledge gaps relating to MC | Survey | N = 62 primary care providers (physicians, nurse practitioners, physician assistants) | Providers believed that MC is a legitimate medical therapy for intractable pain but did not believe it can improve patient's quality of life. One third were concerned about significant drug interactions with MC. 50% were not ready or did not want to answer patient questions regarding MC |
| Sharon et al. (2018) 38 , Israel | Examine the attitudes, beliefs, and personal experiences of Israeli pain specialists regarding the MC | Survey | N = 50 pain specialists | 95% prescribed MC in their pain practice, 63% found it moderately to highly effective in treating patients with intractable chronic pain, 81% felt that they have not received adequate education regarding MC during their specialty training. There was general agreement that MC has a favorable side effect profile compared to opiates yet most preferred trialing opiate therapy before initiating MC. Doctors favored chronic pain states with a clear etiology and viewed psychiatric morbidity, breastfeeding, and young age to be leading contraindications. Most physicians overestimated addiction rates |
| Sideris et al. (2018) 30 , U.S.A. | Assess New York's physicians' comfort level, opinions, and experience in recommending or supporting patient use of MC | Survey | N = 164 physicians (primary care, anesthesiology, pain medicine, surgery, psychiatry) | 87% respondents were not registered with New York's MC program, but majority were willing to recommend patients to registered physicians. Pain symptom control was the most common symptom qualifying for MC. ~75% opioid prescribers considered recommending MC as an adjuvant in pain |
| Starrels et al. (2020) 27 , U.S.A. | Generate consensus among clinicians expert in chronic pain and opioid prescribing about how to respond to MC use among patients on long‐term opioid therapy (LTOT) | Analysis from an online Delphi study | N = 42 clinicians (physicians, nurse practitioners, clinical pharmacologist, registered nurse, clinical nurse specialist) | There was expert consensus about initiating monitoring strategies in response to MC use among patients prescribed LTOT; tapering or discontinuation of LTOT was not important for one‐time or occasional MC users. There was disagreement as to whether to taper or discontinue opioids for patients with a pattern of repeated use and a suspicion of a cannabis use disorder |
Note: This review uses the standardized abbreviation to encompass “medical cannabis,” “medicinal cannabis,” “medical marijuana,” “cannabis for therapeutic purposes,”, “cannabis,” “cannabinoids,” and “marijuana.”
Abbreviation: MC, medicinal cannabis.
TABLE 2.
Studies included in this review about chronic cancer pain
| Author (Year), Country | Aims | Study design | Sample | Study findings |
|---|---|---|---|---|
| Braun et al. (2017) 33 , U.S.A. | Investigate the extent to which oncology experts view marijuana as having medical value and the range of approaches to clinical decision making around MC | Semistructured interviews | N = 15 oncology experts (10 oncologists, two palliative care physicians, one psychiatrist, one surgeon) | 13 of 15 of oncology experts endorsed MC for the indication of pain. Expert opinion was divided on MC's position in medicine with about half who believed MC to have efficacy comparable to conventional management strategies. Nearly as many viewed it as an adjunct, capable of reducing benzodiazepine and opioid loads |
| Braun et al. (2018) 32 , U.S.A. | Examine beliefs, knowledge, and practices of oncologists regarding MC | Survey | N = 237 oncologists | There was a lack of consensus among oncologists regarding MC as the primary treatment for pain, but >2/3 supported its use as an adjunct to standard pain management strategies. 45.9% reported discussing about MC with patients in the past year, 56.7% of them did not consider themselves sufficiently knowledgeable to make MC recommendations |
| Luba et al. (2018) 34 , U.S.A. | Examine the attitudes, beliefs, and practices of palliative and hospice care providers regarding the use of MC for terminally ill patients | Survey | N = 426 palliative and hospice care providers (345 doctors, 58 nurses) | Majority of palliative and hospice care providers saw MC as helpful in treating pain and end of life generally, and useful as an adjuvant medicine. However, fewer than half (46.4%) have recommended MC in the past. 61% indicated that they would recommend MC for terminal illness regardless of legality |
| Uritsky et al. (2011) 35 , U.S.A. | Assess the knowledge, experience, and views of hospice professionals regarding the use of MC in terminally ill patients | Survey | N = 209 hospice professionals (13 medical doctors, 131 nurses, 34 social workers) | 90% hospice care professionals supported the legalization of MC for palliative symptoms. Pain control was the most commonly perceived reason for marijuana use though not a currently FDA‐approved indication. Majority would neglect ethical implications with smoking MC if it was controlling symptoms |
| Zolotov et al. (2018) 41 , Israel | Understand the views of physicians who regularly encounter cancer and chronic pain patients on MC and its possible integration into their clinic, and identify potential underlying factors that influence these perceptions | Semiconstructed interviews | N = 24 physicians (six pain medicine, nine oncology, nine family medicine) | On one hand, physicians abiding by the evidence‐base paradigm of healthcare did not see MC as a conventional medicine. Some physicians viewed patients as drug addicts and feared recreational use of medically acquired cannabis. On the other hand, physicians saw MC as a viable treatment for pain and suffering especially for cancer patients |
| Zolotov et al. (2019) 42 , Israel | Identify underlying factors that influence physicians' intentions to recommend MC to patients | Survey and some interviews | N = 247 physicians (98 family physicians, 80 oncologists, 69 pain medicine) | Respondents had higher intentions to recommend MC to the cancer patient than the chronic pain patient. There were more psychosocial (nonmedical) factors associated with intentions to recommend MC to the chronic pain patient |
Note: This review uses the standardized abbreviation to encompass “medical cannabis,” “medicinal cannabis,” “medical marijuana,” “cannabis for therapeutic purposes,” “cannabis,” “cannabinoids,” and “marijuana.”
Abbreviation: MC, medicinal cannabis.
RESULTS
Study selection and characteristics
As shown in the PRISMA flow chart (Figure 2), the database search yielded 4933 records. Following the removal of duplicates, 2840 records were screened by title and abstract, resulting in 53 full‐text articles being further assessed against our inclusion and exclusion criteria. A total of 26 studies met the criteria for inclusion (Tables 1 and 2). As shown in Figures 3 and 4, the 26 articles included studies from the United States of America, 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 Israel, 37 , 38 , 39 , 40 , 41 , 42 Canada, 43 , 44 , 45 Australia, 46 , 47 , 48 Ireland, 49 and Norway. 50 One study was conducted across five countries. 51 Healthcare professionals represented in the studies were predominantly physicians, 28 , 30 , 39 , 40 , 41 , 42 , 46 , 47 , 49 , 50 but also palliative care providers, 34 , 35 rheumatologists, 37 , 43 pain medicine specialists, 31 , 38 neurologists, 51 nephrologists, 45 psychiatrists, 48 pharmacists, 44 and oncologists. 32 Some studies included a mixed cohort of healthcare providers, 26 , 27 , 29 , 33 , 36 including physicians, physician assistants, osteopathic physicians, osteopathic physician assistants, naturopathic physicians, advanced registered nurse practitioners, registered nurses, licensed nurses, pharmacists, oncologists, palliative care physicians, a psychiatrist, a surgeon, and a clinical nurse specialist. Methods for data collection included surveys, 28 , 29 , 30 , 31 , 32 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 semistructured interviews asking open‐ended questions, 26 , 33 , 41 , 42 and a Delphi study analysis. 27 The sample sizes of studies ranged from 15 to 749 healthcare professionals.
FIGURE 3.
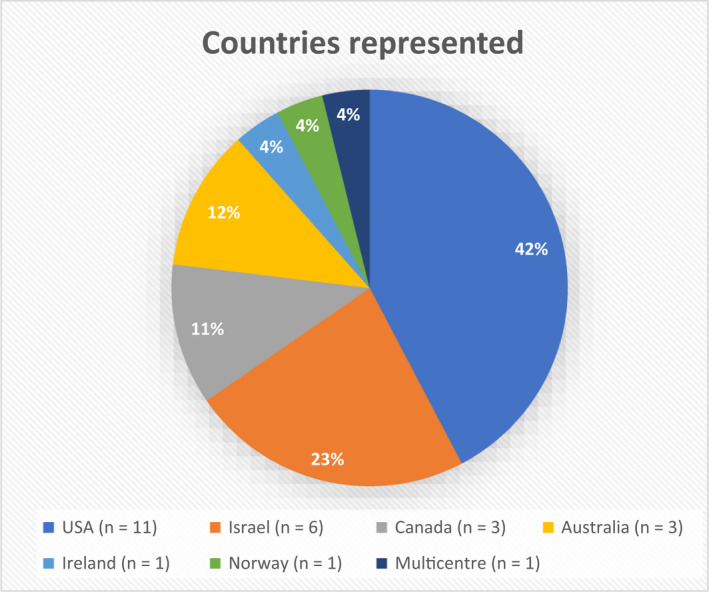
Countries represented in this systematic search and narrative review
FIGURE 4.
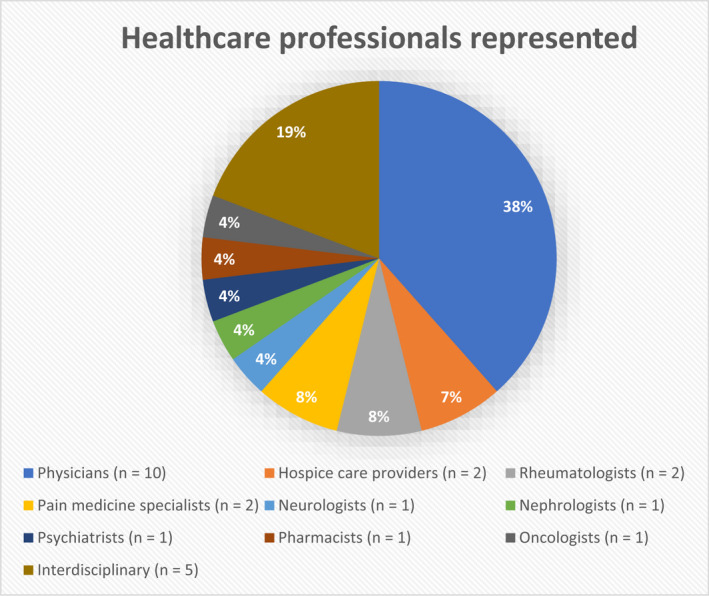
Types of healthcare professionals represented in this systematic search and narrative review. “Interdisciplinary” combines the studies which used a mixed cohort of healthcare providers.
Thematic analysis
The study findings are presented under the following seven themes: MC as a treatment option for chronic pain and perceived indicated uses; willingness to prescribe MC for patients with chronic pain; legal issues affecting use of MC in patients with chronic pain; low perceived knowledge in and the need for education for healthcare professionals supplying MC for chronic pain; comparative safety of MC versus opioids; potential for addiction and abuse in patients with chronic pain; perceived adverse effects.
Medicinal cannabis as a treatment option for chronic pain
The majority of healthcare professionals recognized that MC is a legitimate treatment option for the indication of either chronic pain, 26 , 27 , 28 , 30 , 31 , 32 , 33 , 34 , 35 , 38 , 39 , 40 , 41 , 42 , 44 , 45 , 46 , 48 , 49 , 51 intractable pain (pain that is refractory to conventional treatments), 29 , 36 or rheumatic diseases, 37 , 50 while one study of rheumatologists showed that they generally did not believe that MC has a role in therapeutic management in their practice. 43 Some healthcare professionals indicated more support for MC use in chronic cancer pain 36 , 40 , 41 , 47 , 50 or palliative care 41 , 46 than general chronic pain. There were mixed views regarding whether MC improves a patient's quality of life. 36 , 50
Perspectives on MC as a treatment option were influenced by the lack of quality control testing of MC products on the market, the particular formulations of MC products available to the healthcare professional, and the healthcare professional's clinical training and experience. Of the 15 oncology experts in one study, almost half expressed reservations regarding the efficacy of MC due to the varied constituents and content between MC products on the market which can result in variations in pharmacological effects and therefore unpredictable therapeutic outcomes. 33 In terms of the formulation of the products, some Israeli physicians considered smoking as an inappropriate delivery mechanism as the dose delivered cannot be ascertained and the act of smoking is associated with morbidities. 41 Senior healthcare professionals in another study indicated they would choose to neglect the ethical implications and potential health consequences relating to the act of smoking a medicine if it was controlling the patient's symptoms. 35 Healthcare professionals who showed a greater endorsement of MC as a treatment option were those who had additional addiction training, and they also showed a greater support for cannabis to be decriminalized for recreational use. 49 MC as a treatment option was also endorsed by healthcare professionals who had greater accumulated clinical experience with MC. In an Israeli interview, an oncologist said, “I think that we see in the clinic much more efficacy of cannabis than what has been proven in the literature.” 41 Clinical experience was regarded significantly more influential by physicians who had recommended MC in the past compared to those who had not. 39 Healthcare professionals who had recommended MC were generally more likely to be convinced of its benefits and less concerned of its risks 28 , 29 , 38 or had greater perceived knowledge of MC. 44
Physicians' perspectives on appropriate indications for initiating MC were varied. In a Norwegian study, chronic pain was ranked lower as an indication than cancer, multiple sclerosis, rheumatic disease, and Parkinson's disease. 50 Likewise, few Australian general practitioners supported the use of MC in chronic noncancer pain. 47 Pain medicine specialists in Israel judged that neuropathic pain, oncological pain, and arthralgias related to rheumatic diseases were the most suitable indications to start MC, with the least suitable being chronic low back pain and chronic postoperative pain. 38 Almost half (47%) of this sample of 50 pain specialists considered a lack of a clear diagnosis as a contraindication. Israeli family physicians indicated during interviews that it was easier for them to recommend MC to cancer patients because the diagnosis is confirmed, whereas reports of other pain are more subjective. 41 , 42
Few studies have investigated the use of MC for end‐of‐life care. Israeli physicians indicated they were not concerned by the lack of sufficient scientific evidence supporting MC and the potential harms of use (eg, addiction, side effects) as long as it helps the suffering patient. 35 , 41 Oncology experts regarded those at end of life requiring palliation as the population in which it is most appropriate to use MC. 33
Willingness to prescribe MC for chronic pain
Willingness to prescribe MC among physicians varied. There were higher prescribing rates reported via pain specialists, and rheumatologists from Israel, 37 , 38 but most Israeli family physicians were not at all willing or only willing to a small extent to prescribe MC. 40 As most American physicians were not registered with the state's MC program – the only way can they legally recommend MC to patients 30 , 36 – they preferred to refer patients to another physician or specialist with MC prescribing expertise and licensure, 40 , 45 or to prescribe after consulting a specialist. 43 , 46 , 47 Barriers to prescribing included: a lack of evidence for use 28 , 29 , 30 , 34 , 41 , 44 , 45 , 46 , 50 ; concerns of abuse 40 , 41 , 43 , 50 ; bureaucracy involved with getting approval 30 , 36 , 40 , 46 ; lack of training and knowledge 29 , 44 ; lack of algorithms or endorsed clinical guidelines 29 , 41 ; federal status of cannabis or political resistance 29 , 30 , 33 , 50 ; legal liability or licensure. 28 , 30 Rheumatologists were willing to consider a trial period for MC if patients had failed conventional treatments, but were less willing if patients requested the substance. 37 , 43
Legal issues affecting prescribing of MC for chronic pain
The legal boundaries governing access to MC affected its actual and perceived prescribing for chronic pain. Access varied from country to country, for example, in the United States, cannabis is a prohibited (Schedule I [controlled]) substance at a federal level according to the Controlled Substances Act (1970); however, individual states legally permit the use of cannabis for medicinal purposes if a registered healthcare professional certifies a user's eligibility. Federal and state differences in the legal status of MC were a primary barrier for New York physicians to register into the state program to certify patients for use. 30 Washington healthcare providers' (including physicians, nurses, and pharmacists) reported a lack of comfort when recommending MC, and expressed that they should not have to fear legal action when allowing a patient to access use. 29 Hospice care providers and neurologists agreed that MC should be reclassified as a controlled substance in order to change their views on its utility in palliative care and Parkinson's disease, respectively. 34 , 51 However, almost half of the surveyed Colorado family physicians (n = 520) were not in favor of decriminalizing cannabis and would rather it remain as a controlled drug. 28 In Norway, MC was legalized in 2016 but has not been readily available for patients due to the strictly regulated approval process and the small number of physicians who can prescribe MC. Norwegian physicians supporting MC on prescription believe that the current legislation prevents optimal quality of care where MC could improve the quality of life for patients with chronic pain. 50 An Australian study published in 2006 found that 75% of rural general practitioners (n = 32) felt prepared to prescribe MC with the only barrier being its status as an illegal drug. 46
Low perceived knowledge and the need for education
Generally, across all disciplines, healthcare professionals involved in managing patients with pain reported being not ready or comfortable to answer patients' questions regarding MC, 36 , 37 , 43 discuss MC with patients or other healthcare professionals, 26 , 44 , 47 write a prescription for MC, 40 , 43 , 45 , 47 or issue a written authorization for a patient to possess MC. 29 Related to this finding, few healthcare professionals received formal training or MC‐related education during their undergraduate degree. A total of 48% of Australian general practitioners (n = 640) rated their knowledge of MC as poor. 47 Of Israeli pain specialists (n = 50), 81% did not receive adequate education during specialty training. 38 Insufficient knowledge played into the self‐perceived low ability of oncologists to make a recommendation for MC use. 32 The majority of healthcare professionals engaged in self‐directed education 44 with sources of information being medical literature, 29 , 50 , 51 clinical experience, 29 , 51 news and media, 29 , 50 and colleagues. 29 , 50 Despite such patterns of use of information sources, more than 70% of doctors (n = 25) perceived that clinical practice guidelines served as a better educational format than peer‐reviewed literature. 48 There was almost unanimous endorsement of the need to pay more attention to MC in undergraduate curricula. 28 , 29 , 51 Many believed that formal training or a licensing procedure should precede the ability to authorize use for a patient. 28 , 29 , 39 , 47 A large proportion were interested in learning more about the topic or wanted to be trained to prescribe MC. 36 , 39 , 46 , 47
Comparative safety of MC versus opioids
Opioids have long been the mainstay in the treatment of refractory pain. The general view held by healthcare professionals in this review, for example, by Israeli physicians, 38 , 41 Australian general practitioners, 47 and American oncologists 32 is that MC is safer than opioids. MC was observed to have the advantages of being opioid sparing, 33 , 41 , 50 having less side effects, 41 and carrying lower risks of overdose death and addiction. 32 However, MC was also recognized to cause paranoia and confusion which opioids did not. 32 There was support for MC to be used as an adjunct to conventional chronic pain management strategies by New York physicians, 30 a mixed cohort of healthcare providers in Norway (mainly oncologists) 47 and Israeli oncology experts. 32 However, when asked about cannabis in practice, a majority of Israeli pain specialists thought that opioid therapy should be trialed prior to commencing cannabis. 38 A large proportion of the pain specialists preferred themselves and their families to be treated with opioids when given the choice against cannabis if a situation necessitated it. 38 Also, the majority of American hospice providers in one study (mainly physicians and nurses) was not sure or believed that MC was not as effective than conventional pain treatment. 34 Clinicians did not discuss MC with patients on long‐term opioid therapy for pain nor routinely perform urine toxicology testing due to the assumption that patients were using cannabis already, given the prevalent use of cannabis in the chronic pain patient population. 26
Addiction and abuse
Many healthcare providers held the view that cannabis was addictive. 29 , 35 , 47 , 48 , 51 This influenced some Australian general practitioners' decisions in one study (about 30% of those sampled; n = 640) to not prescribe MC. 47 Addiction concerns have manifested in physicians' fears that MC for recreational use would be disguised under legal protection. 28 , 41 There were unclear boundaries between recreational and medicinal use of cannabis reported by Israeli physicians where they related the therapeutic effect to “getting high.” 41 Australian rural doctors also feared burdening the healthcare system if patients sought prescriptions for recreational use once MC is legal. 46
As noted earlier, “when dealing with very sick patients, the lack of evidence and potential harms carried less weight” compared to relief of suffering. 41
Perceived adverse effects
Mental health risks including anxiety, psychosis, paranoia, hallucinations, and dysphoria were commonly cited adverse effects across studies. 28 , 29 , 33 , 39 , 47 , 48 , 50 One study highlighted the difficulty healthcare professionals had in distinguishing between cannabis‐induced psychosis and a patient's underlying psychiatric disorder. 26 This may be why Israeli pain specialists noted schizophrenia and previous psychosis as the leading contraindications to commencing MC. 38 Driving impairment 47 , 51 and cognitive impairment 47 , 51 were also noted as adverse effects of MC.
DISCUSSION
There is wide support among healthcare professionals for the inclusion of MC in the management of chronic pain. 33 , 34 , 35 , 36 , 38 , 39 , 40 , 41 , 44 , 45 , 46 , 50 , 51 Furthermore, chronic pain is the most common reason for authorization or recommendation of MC use. 28 , 29 , 30 , 45 Indeed our review found that healthcare professionals were frequently presented with inquiries, 30 , 44 , 47 , 50 requests to prescribe, 41 , 51 opportunities to recommend MC, 28 , 31 or were confronted with patients in their care who were already taking MC. 31 , 45 , 50 , 51 However, studies have suggested relatively low prescribing and recommending rates overall, complicated by legal issues, personal perspectives, a lack of education and formal training, and the absence of evidence‐based guidelines for healthcare professionals.
Since the legal use of the cannabis plant was prohibited globally in 1961, access to MC has been complex internationally despite prior traditional use. For some countries, the plant has remained prohibited for both medicinal and recreational purposes, whereas in others unique legal frameworks have been established to uphold the use of MC and/or recreational cannabis. 52 A variety of access models and regulatory experiences have emerged internationally. The latter occur in the United States where cannabis is illicit at the federal level but prescribers can be registered in state‐based programs to write a “recommendation” for the plant for a patient if the patient suffers from one of the conditions listed by the state. 53 It remains unclear why healthcare professionals in the United States fear legal action despite being covered by state policy, and this situation presents a barrier to prescribing. While the majority of literature reporting “regulatory experiences” associated with MC in our review is based in the United States, it is important to note such experiences will vary throughout the world. However, international research for MC is certainly hampered by the legalities of accessing it. 22
This review found a disconnect between healthcare professionals' views and actual practice in the treatment of chronic pain, in that MC was regarded as safer than opioids yet was not prescribed to the same extent as opioids. To date there is little evidence regarding interactions between the use of opioids and cannabis/cannabinoids concurrently. 54 Vaporized cannabis may reduce pain in chronic pain patients taking morphine or oxycodone without affecting the pharmacokinetics of these opioids. Additive sedation and CNS depression might occur with concurrent use of cannabis or cannabinoids with opioids. 54
In the last two decades, the world has seen an epidemic of opioid prescribing whereby prescription opioids have been associated with a large number of deaths and labeled a “public health problem.” 55 Healthcare professionals' positive views regarding cannabis' comparative risk profile to opioids may be shaped by the lives lost to opioid toxicity, such that not using opioids at all or reducing the opioid load are seen as favorable. However, our review saw reservations for MC to be used in practice expressed by Israeli pain specialists, American hospice providers, and American pain experts. This may be attributed to a recent shift toward opioid stewardship and deprescribing in practice, which has consequently seen the emergence of evidence‐based guidelines from public health agencies to address harms from the misuse of these pain medicines. 56 , 57 These guidelines serve as a means of dissemination of best clinical practices to prescribers. 58 One systematic review of 15 studies showed low to moderate evidence that opioid stewardship efforts have decreased the number of opioid prescriptions, number of patients on long‐term opioids, duration of prescribed treatment, and opioid dosages. 59 Until there are high‐quality randomized controlled trials for MC to test its efficacy and safety for the indication of chronic pain, and standardize the dose and administration for prescribing, local prescribing protocols cannot be evidence based. Meanwhile opioids appear to be the preferred treatment by physicians due to the presence of guidelines. This highlights the need for more funding and attention by regulatory authorities to increase the pace of research approval for MC and trial result turnover, which can be subsequently translated into evidence‐based guidelines to support the healthcare professional after the point of MC's legalization.
Health professionals in our review showed a preference for prescribing MC to patients with chronic pain associated with a clear etiology (eg, neuropathic pain, cancer‐related pain, rheumatic diseases), where the diagnosis is confirmed, as well as those at their end of life. The indication with the most robust evidence for MC is neuropathic pain with a number of double‐blind placebo‐control trials conducted. 17 However, there remains a lack of evidence for other pain phenotypes. 19 As there is no objective marker for diagnosis with chronic pain, diagnosis is reliant on the patient's report of their lived experience. This subjectivity of a chronic pain diagnosis may form the basis of physicians' concerns of abuse where they may perceive patients to be malingering under the indication of chronic pain in order to gain access to MC for recreational use. This review found lower intentions to prescribe MC for general chronic pain than in Gardiner et al.’s review, 23 but the latter was not focused on health professionals practicing in the sphere of chronic pain. There also appeared to be a compassionate stance toward the suffering patients experience in our study, causing physicians to be more permissive with palliative medications and overlook issues of addiction, side effects, and the reluctance to prescribe MC. Interestingly, there are few studies conducted on end‐of‐life care, yet it is the population that is considered the most appropriate to use MC. Perspectives on MC use in end‐of‐life care may therefore be a promising area of research.
While the prescription or approval of MC may currently be restricted to physicians, pharmacists and nurses also have roles in educating their prescribing colleagues, counseling patients about MC's safety and efficacy, staying informed about and interpreting emerging research, as well as dispensing or administering MC, respectively. Additionally, in some parts of the world, pharmacies serve as points of sale of MC (eg, Australia). 52 Understanding healthcare professionals' personal views regarding the efficacy of MC is crucial as these play into their provision of a perceived viable treatment option for chronic pain. Therefore, the views of other healthcare professionals regarding chronic pain and pain with underlying conditions could be a future research direction.
Finally, it is concerning that few healthcare professionals feel equipped to deal with people who use MC for chronic pain, due to limited opportunities for education and training around MC worldwide. This may be explainable due to the lack of supporting evidence for its efficacy. With the legalization of MC, healthcare professionals often enter practice without prior knowledge or guidance about the substance which has grown in public favor. Consequently, a high use of nonpeer‐reviewed information sources was reported by healthcare professionals in this review. It is encouraging that healthcare professionals expressed a strong desire for formal educational opportunities, which may suggest a willingness to undergo additional training. This review showed that those with more clinical experience have more permissive attitudes to prescribing or recommending MC for chronic pain. While scientific evidence accumulates to inform practice guidelines and educational curricula, healthcare professionals rely on their accumulated clinical experience to guide their present practice. This reinforces the need for safety and efficacy data to be gathered and disseminated, and clinical dosing guidelines to be developed to support the healthcare professional after the point of legalization and ensure the provision of MC to chronic pain patients where appropriate.
Limitations
First, we did not assess the quality of study methodologies included in this review, given the focus on the narrative and thematic synthesis of the included studies. 24 Second, we generalized all cannabis‐containing products mentioned in studies under the term “medicinal cannabis,” though perspectives may differ, for example, toward the cannabis plant versus manufactured cannabis products. Third, this review included articles of the English language only. Potential literature may have been missed from countries which are leading in the MC field, but whose scientists may not be publishing results in English. Additionally, this review reported on studies that largely consisted of physicians and specialists involved in the prescribing or recommendation of MC. Future studies could consider a deeper examination of the perspectives of pharmacists and nurses, who may be directly involved in the dispensing or administration of MC, respectively, regarding chronic pain versus pain associated with underlying conditions.
CONCLUSIONS
Healthcare professionals appear to rely on their clinical experiences of caring for people living with chronic pain to make decisions about MC use. Healthcare professionals require education and training, and clinical guidelines that provide evidence‐based information about efficacy and safety, and guidance related to dosage of MC products for chronic pain. Until these gaps are addressed, healthcare professionals are limited in making informed treatment recommendations about MC, may deny a potentially beneficial intervention, divert patients to inappropriate or unnecessary care, and may be unintentionally devaluing the lived experience and preferences of people with chronic pain.
AUTHOR CONTRIBUTIONS
All authors have made a significant contribution to this manuscript. LS, JH, and KC conceived the study, collected the data, performed data analysis, and drafted the manuscript. Critical revision of the manuscript was conducted by SD, DE, and SL.
CONFLICT OF INTEREST
The authors do not have any conflicts of interest to declare.
ACKNOWLEDGMENT
Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians.
Cheng KYC, Harnett JE, Davis SR, Eassey D, Law S, Smith L. Healthcare professionals' perspectives on the use of medicinal cannabis to manage chronic pain: A systematic search and narrative review. Pain Pract. 2022;22:718–732. 10.1111/papr.13161
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author, [author initials], upon reasonable request.
REFERENCES
- 1. Dueñas M, Salazar A, de Sola H, Failde I. Limitations in activities of daily living in people with chronic pain: identification of groups using clusters analysis. Pain Pract. 2020;20(2):179–87. [DOI] [PubMed] [Google Scholar]
- 2. Phillips CJ. The cost and burden of chronic pain. Rev Pain. 2009;3(1):2–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Turk DC, Wilson HD, Cahana A. Treatment of chronic non‐cancer pain. Lancet. 2011;377(9784):2226–35. [DOI] [PubMed] [Google Scholar]
- 4. Manning L, Bouchard L. Medical cannabis use: exploring the perceptions and experiences of older adults with chronic conditions. Clin Gerontol. 2021;44(1):32–41. [DOI] [PubMed] [Google Scholar]
- 5. Luque JS, Okere AN, Reyes‐Ortiz CA, Williams PM. Mixed methods study of the potential therapeutic benefits from medical cannabis for patients in Florida. Complement Ther Med. 2021;57:102669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Azcarate PM, Zhang AJ, Keyhani S, Steigerwald S, Ishida JH, Cohen BE. Medical reasons for marijuana use, forms of use, and patient perception of physician attitudes among the US population. J Gen Intern Med. 2020;35(7):1979–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Costales B, van Boemmel‐Wegmann S, Winterstein A, Segal R. Clinical conditions and prescription drug utilization among early medical marijuana registrants in Florida. J Psychoactive Drugs. 2021;1‐10:185–94. [DOI] [PubMed] [Google Scholar]
- 8. Bachhuber M, Arnsten JH, Wurm G. Use of cannabis to relieve pain and promote sleep by customers at an adult use dispensary. J Psychoactive Drugs. 2019;51(5):400–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sharon H, Brill S. Cannabis‐based medicines for chronic pain management: current and future prospects. Curr Opin Anaesthesiol. 2019;32(5):623–8. [DOI] [PubMed] [Google Scholar]
- 10. Wipfler K, Simon T, Katz P, Wolfe F, Michaud K. Cannabis use among patients in a large us rheumatic disease registry. Arthritis Rheumatol. 2019;71:5217–20. [Google Scholar]
- 11. Ware MA, Adams H, Guy GW. The medicinal use of cannabis in the UK: results of a nationwide survey. Int J Clin Pract. 2005;59(3):291–5. [DOI] [PubMed] [Google Scholar]
- 12. Swift W, Gates P, Dillon P. Survey of Australians using cannabis for medical purposes. Harm Reduct J. 2005;2:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bar‐Sela G, Vorobeichik M, Drawsheh S, Omer A, Goldberg V, Muller E. The medical necessity for medicinal cannabis: prospective, observational study evaluating the treatment in cancer patients on supportive or palliative care. Evid Based Complement Alternat Med. 2013;2013:510392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lynch ME, Ware MA. Cannabinoids for the treatment of chronic non‐cancer pain: an updated systematic review of randomized controlled trials. J Neuroimmune Pharmacol. 2015;10(2):293–301. [DOI] [PubMed] [Google Scholar]
- 15. Hauser W, Fitzcharles MA. The perils of overestimating the efficacy of cannabis‐based medicines for chronic pain management. Pain Physician. 2018;21(1):E79–80. [PubMed] [Google Scholar]
- 16. Hauser W, Petzke F, Fitzcharles MA. Efficacy, tolerability and safety of cannabis‐based medicines for chronic pain management ‐ an overview of systematic reviews. Eur J Pain. 2018;22(3):455–70. [DOI] [PubMed] [Google Scholar]
- 17. Mucke M, Phillips T, Radbruch L, Petzke F, Häuser W. Cannabis‐based medicines for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2018;3:CD012182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stockings E, Campbell G, Hall WD, Nielsen S, Zagic D, Rahman R, et al. Cannabis and cannabinoids for the treatment of people with chronic noncancer pain conditions: a systematic review and meta‐analysis of controlled and observational studies. Pain. 2018;159(10):1932–54. [DOI] [PubMed] [Google Scholar]
- 19. Andreae MH, Rhodes E, Bourgoise T, Carter GM, White RS, Indyk D, et al. An ethical exploration of barriers to research on controlled drugs. Am J Bioeth. 2016;16(4):36–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Aviram J, Samuelly‐Leichtag G. Efficacy of cannabis‐based medicines for pain management: a systematic review and meta‐analysis of randomized controlled trials. Pain Physician. 2017;20(6):E755–96. [PubMed] [Google Scholar]
- 21. Wang L, Hong PJ, May C, Rehman Y, Oparin Y, Hong CJ, et al. Medical cannabis or cannabinoids for chronic non‐cancer and cancer related pain: a systematic review and meta‐analysis of randomised clinical trials. BMJ. 2021;374:n1034. [DOI] [PubMed] [Google Scholar]
- 22. Nugent SM, Morasco BJ, O'Neil ME, Freeman M, Low A, Kondo K, et al. The effects of cannabis among adults with chronic pain and an overview of general harms: a systematic review. Ann Intern Med. 2017;167(5):319–31. [DOI] [PubMed] [Google Scholar]
- 23. Gardiner KM, Singleton JA, Sheridan J, Kyle GJ, Nissen LM. Health professional beliefs, knowledge, and concerns surrounding medicinal cannabis – A systematic review. PLoS One. 2019;14(5):e0216556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108. [DOI] [PubMed] [Google Scholar]
- 25. Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320(7227):114–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cooke AC, Knight KR, Miaskowski C. Patients' and clinicians' perspectives of co‐use of cannabis and opioids for chronic non‐cancer pain management in primary care. Int J Drug Policy. 2019;63:23–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Starrels JL, Young SR, Azari SS, Becker WC, Jennifer Edelman E, Liebschutz JM, et al. Disagreement and uncertainty among experts about how to respond to marijuana use in patients on long‐term opioids for chronic pain: results of a Delphi study. Pain Med. 2020;21(2):247–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kondrad E, Reid A. Colorado family physicians' attitudes toward medical marijuana. J Am Board Fam Med. 2013;26(1):52–60. [DOI] [PubMed] [Google Scholar]
- 29. Carlini BH, Garrett SB, Carter GT. Medicinal cannabis: a survey among health care providers in Washington state. Am J Hosp Palliat Care. 2015;34(1):85–91. [DOI] [PubMed] [Google Scholar]
- 30. Sideris A, Khan F, Boltunova A, Cuff G, Gharibo C, Doan LV. New York physicians' perspectives and knowledge of the state medical marijuana program. Cannabis Cannabinoid Res. 2018;3(1):74–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Narouze S, Hakim SM, Kohan L, Adams D, Souza D. Medical cannabis attitudes and beliefs among pain physicians. Reg Anesth Pain Med. 2020;45(11):917–9. [DOI] [PubMed] [Google Scholar]
- 32. Braun IM, Wright A, Peteet J, Meyer FL, Yuppa DP, Bolcic‐Jankovic D, et al. Medical oncologists' beliefs, practices, and knowledge regarding marijuana used therapeutically: a nationally representative survey study. J Clin Oncol. 2018;36(19):1957–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Braun IM, Meyer FL, Gagne JJ, Nabati L, Yuppa DP, Carmona MA, et al. Experts' perspectives on the role of medical marijuana in oncology: a semistructured interview study. Psychooncology. 2017;26(8):1087–92. [DOI] [PubMed] [Google Scholar]
- 34. Luba R, Earleywine M, Farmer S, Slavin M. Cannabis in end‐of‐life care: examining attitudes and practices of palliative care providers. J Psychoactive Drugs. 2018;50(4):348–54. [DOI] [PubMed] [Google Scholar]
- 35. Uritsky TJ, McPherson ML, Pradel F. Assessment of hospice health professionals' knowledge, views, and experience with medical marijuana. J Palliat Med. 2011;14(12):1291–5. [DOI] [PubMed] [Google Scholar]
- 36. Philpot LM, Ebbert JO, Hurt RT. A survey of the attitudes, beliefs and knowledge about medical cannabis among primary care providers. BMC Fam Pract. 2019;20:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ablin JN, Elkayam O, Fitzcharles MA. Attitudes of Israeli rheumatologists to the use of medical cannabis as therapy for rheumatic disorders. Rambam Maimonides Med J. 2016;7(2):e0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sharon H, Goldway N, Goor‐Aryeh I, Eisenberg E, Brill S. Personal experience and attitudes of pain medicine specialists in Israel regarding the medical use of cannabis for chronic pain. J Pain Res. 2018;11:1411–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ebert T, Zolotov Y, Eliav S, Ginzburg O, Shapira I, Magnezi R. Assessment of Israeli physicians' knowledge, experience and attitudes towards medical cannabis: a pilot study. Isr Med Assoc J. 2015;17(7):437–41. [PubMed] [Google Scholar]
- 40. Abo Ziad R, Grynbaum MB, Peleg R, Treister‐Goltzman Y. The attitudes and beliefs of family physicians regarding the use of medical cannabis, knowledge of side effects, and barriers to use: a comparison between residents and specialists. Am J Ther. 2020;29:29. [DOI] [PubMed] [Google Scholar]
- 41. Zolotov Y, Vulfsons S, Zarhin D, Sznitman S. Medical cannabis: an oxymoron? Physicians' perceptions of medical cannabis. Int J Drug Policy. 2018;57:4–10. [DOI] [PubMed] [Google Scholar]
- 42. Zolotov Y, Vulfsons S, Sznitman S. Predicting physicians' intentions to recommend medical cannabis. J Pain Symptom Manage. 2019;58(3):400–7. [DOI] [PubMed] [Google Scholar]
- 43. Fitzcharles MA, Ste‐Marie PA, Clauw DJ, Jamal S, Karsh J, LeClercq S, et al. Rheumatologists lack confidence in their knowledge of cannabinoids pertaining to the management of rheumatic complaints. BMC Musculoskelet Disord. 2014;15:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mitchell F, Gould O, LeBlanc M, Manuel L. Opinions of hospital pharmacists in Canada regarding marijuana for medical purposes. Can J Hosp Pharm. 2016;69(2):122–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Collister D, Tennankore K, Davison SN, Wald R, Rabbat C, Walsh M. Nephrologist views regarding cannabinoid use in advanced chronic kidney disease and dialysis: a survey. J Pain Symptom Manage. 2021;61(2):237–45.e2. [DOI] [PubMed] [Google Scholar]
- 46. Irvine G. Rural doctors' attitudes to and knowledge of medicinal cannabis. J Law Med. 2006;14(1):135–42. [PubMed] [Google Scholar]
- 47. Karanges EA, Suraev A, Elias N, Manocha R, McGregor IS. Knowledge and attitudes of Australian general practitioners towards medicinal cannabis: a cross‐sectional survey. BMJ Open. 2018;8(7):e022101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jacobs NI, Montebello M, Monds LA, Lintzeris N. Survey of Australian psychiatrists' and psychiatry trainees' knowledge about and attitudes towards medicinal cannabinoids. Australas Psychiatry. 2019;27(1):80–5. [DOI] [PubMed] [Google Scholar]
- 49. Crowley D, Collins C, Delargy I, Laird E, van Hout MC. Irish general practitioner attitudes toward decriminalisation and medical use of cannabis: results from a national survey. Harm Reduct J. 2017;14(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Arnfinsen JL, Kisa A. Assessment of Norwegian physicians' knowledge, experience and attitudes towards medical cannabis. Drugs. 2021;28(2):165–71. [Google Scholar]
- 51. Bega D, Simuni T, Okun MS, Chen X, Schmidt P. Medicinal cannabis for Parkinson's disease: practices, beliefs, and attitudes among providers at national Parkinson foundation centers of excellence. Mov Disord Clin Pract. 2017;4(1):90–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Sofia A, Victor G, Lisa S, Nougier M. Medicinal cannabis policies and practices around the world. London: International Drug Policy Consortium; 2018. [Google Scholar]
- 53. Gregorio J. Physicians, medical marijuana, and the law. AMA J Ethics. 2014;16(9):732–8. [DOI] [PubMed] [Google Scholar]
- 54. Baxter K, Preston CL. Stockley's drug interactions. [online]. London: Pharmaceutical Press; 2013. [Google Scholar]
- 55. Humphreys K. Avoiding globalisation of the prescription opioid epidemic. Lancet. 2017;390(10093):437–9. [DOI] [PubMed] [Google Scholar]
- 56. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain ‐ United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. [DOI] [PubMed] [Google Scholar]
- 57. Manchikanti L, Kaye AM, Knezevic NN, McAnally H, Slavin K, Trescot AM, et al. Responsible, safe, and effective prescription of opioids for chronic non‐cancer pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines. Pain Physician. 2017;20(2s):S3–92. [PubMed] [Google Scholar]
- 58. Butler JC, Fraser MR. A public health guide to ending the opioid epidemic. Oxford: Oxford University Press; 2019. [Google Scholar]
- 59. Shoemaker‐Hunt SJ, Wyant BE. The effect of opioid stewardship interventions on key outcomes: a systematic review. J Patient Saf. 2020;16(3S Suppl 1):S36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, [author initials], upon reasonable request.


