Abstract
Background
Clinical data are needed on long‐term outcomes of removable implant‐supported prostheses in the fully edentulous maxilla as a function of the number of implants, effects of the attachment system and other clinical variables.
Objective
To restore individuals with an edentate maxilla with a metal‐reinforced removable prosthesis without palatal coverage retained by low‐profile stud attachments on three implants.
Methods
The regional ethics committee approved a prospective cohort study that included all consecutive patients treated in a private speciality clinic. Primary outcomes were patients reported, that is denture satisfaction scale and oral health‐related quality of life – OHIP‐20. Secondary outcomes were implant‐ (bone loss, implant complications and peri‐implant conditions) and prosthesis‐related (prosthesis complications, maintenance needs and mucosa condition).
Results
Thirty‐two study participants were recruited between March 2007 and October 2016 and followed for a minimum of five years. According to Kruskal–Wallis tests, the OHIP‐20 and Denture Satisfaction Scale questionnaire pre‐treatment scores differed significantly. After an average of 6.7 years, peri‐implant bone loss of more than 2 mm was observed on 17% of all implants, while no or minor bone loss was seen on 38%. The estimated success of implants was 0.95 at 168 months. The estimated success of the prosthesis, that is no adverse events or need for any repairs, was 0.55 at 156 months.
Conclusion
The positive findings in the current clinical study strengthen the notion that for many individuals with an edentulous maxilla, a removable prosthesis retained by three implants fitted with low‐profile stud‐attachment is a reliable technical solution.
Keywords: edentulous, oral implant, patient satisfaction, prospective studies, quality of life, self report
Many individuals with an edentulous maxilla are satisfied with using a removable palate‐free metal‐reinforced prosthesis retained three low‐profile stud‐attachments fitted on dental implants placed to form a triangular support zone. The solution is a less costly alternative than fixed or bar‐retained removable prosthetics and appears to function satisfactorily over several years.

1. INTRODUCTION
Individuals with an edentulous maxilla suffer from loss of stomatognathic functions and aesthetics, at times leading to physical and psychological impairments. A properly designed and fitted conventional prosthesis can partially restore functions and aesthetics, as reflected by regained patient‐reported oral health‐related quality of life. 1 A premise, however, is that the individual must be capable of stabilising a relatively moveable prosthesis by orofacial muscular activity during stomatognathic functions. 2 The ability may be compromised for different reasons, including a resorbed alveolar ridge, unfavourable maxilla‐mandibular dimensional relationship and a frail or dry mucosa. 3 Although many consider that a conventional prosthesis restores their oral functions and aesthetics adequately, others experience that the solution does not align with their expectations.
The alternative solutions rely on the surgical placement of dental implants to support a fixed or removable prosthesis. Already in 1986, expert clinicians emphasised the need to adopt ‘overdenture principles…necessitated by either economic considerations or patient compromise’. 4 Similar sentiments are repeated today, with the additional knowledge that a removable solution may be more cost‐effective than a fixed solution 5 and show comparable peri‐implant marginal bone loss. 6 Other arguments demonstrate high implant and prosthesis survival 7 , 8 and satisfy many patients' expectations and desires. 9 However, the proportion of clinical studies that describe long‐term outcomes of overdentures is modest amongst the currently ~1300 publications on implant‐supported maxillary complete prostheses. 10 , 11
More robust clinical data are needed on long‐term outcomes of removable implant‐supported prostheses in the fully edentulous maxilla as a function of a minimum number of implants, 12 , 13 attachment system 14 and other clinical variables, 15 to estimate the value for money and contingent valuation of alternative prosthesis modalities. 16 , 17
The current investigators have previously described the clinical experiences of patients receiving a palate‐free metal‐reinforced maxillary overdenture retained by three implants fitted with low‐profile stud attachments. 18 It was recognised that more long‐term prospective data were required to determine this technical solution's potential merits and disadvantages. Hence, the objective of the current cohort study is to present the long‐term data over a minimum of five years of clinical observation.
2. MATERIALS AND METHODS
This clinical study is reported according to the STROBE guidelines (Strengthening the Reporting of Observational Studies in Epidemiology) (https://www.strobe‐statement.org). 19
2.1. Study design, setting and participants
A prospective cohort study was conducted strictly to all ethical research principles. The Norwegian regional research ethics board approved the research protocol, invitation letter for study participation and case‐report forms (ref. 2013/1446/REK Nord). Questionnaire response data were managed according to directives established by the Norwegian patient privacy ombudsperson.
The clinical study was conducted in a single private specialist clinic in Drammen, Norway.
The study cohort consisted of all consecutive patients with an edentate maxilla that received implants before 2017 and subsequently were restored with a metal‐reinforced removable prosthesis without palatal coverage retained by low‐profile stud attachments. All patients were invited to participate in annual follow‐up examinations without any costs. Study participation received no additional fiduciary benefits. A request was also made for permission to contact their referring dentist for updated status information.
The study inclusion criteria were a need for full‐arch reconstruction in an edentulous maxilla, general health adequate to tolerate surgery physically, sufficient bone quantity and quality for the placement of three implants with at least 8 mm length without the need for any further bone augmentation, provision of written informed consent to the planned treatment. The participants were requested to sign an informed consent form for participation and permission to use obtained data for research purposes. There was no age limitation or restriction regarding current and past smoking history. Exclusion criteria were previous radiation therapy or prior bone grafting in the maxilla.
2.2. Pre‐treatment examination
All study participants provided information on their general health status, specifically systemic diseases, smoking status and medications that could risk‐averse treatment outcomes. Recordings were made of other general and local factors that could affect the prognosis of the implants or prostheses.
Clinical examinations included adverse oral mucosal findings in the maxilla, including cheilitis, flabby ridge, hyperplasia, sore spots (decubitus) or ulcers. The dentition in the mandible was examined for caries and marginal periodontitis using a manual periodontal probe (American Eagle 2‐12B probe, Young Innovations, Germany). The clinical examination was combined with a panoramic radiograph to detect pathological conditions and local bone availability. Any oral hygiene limitations, high plaque and bleeding scores and active periodontitis in the mandible or local inflammation or mucosal diseases in the maxilla were managed before active implant prosthetic treatment.
The study participants reported their experiences with the existing maxillary prosthesis by completing the Denture Satisfaction Scale questionnaire, 20 and a short‐form version of the Oral Health Impact Profile questionnaire (OHIP‐20). 21 The denture satisfaction scale reflects the individuals' opinions on general satisfaction, retention, comfort, stability, speech, appearance and occlusion using a Likert response format scale ranging from 1 to 5 (‘totally satisfied’ to ‘not at all satisfied’, respectively). The OHIP‐20 questionnaire consists of twenty questions with the response options ‘never’ (0), ‘hardly ever’ (1), ‘occasionally’ (2), ‘fairly often’ (3) or ‘very often’ (4). In addition to a total score, the scores are detailed in seven subscales: that is functional limitation, physical pain/discomfort, psychological discomfort, physical disability, psychological disability, social disability and handicap.
2.3. Surgical procedures
The surgical procedures involved local anaesthetics and full flap incisions. Antibiotics were used at the discretion of the oral surgeon. Two implants with at least 8 mm length were placed posteriorly in bone bilaterally as far as possible, considered radiographically acceptable quantitatively and qualitatively. Attention was made to not enter the sinus cavity without intentionally distally tilting the implants. So, the most distally placed implants were in the 15 and 25 regions. A third implant with relative parallelism to the two posterior implants was placed anteriorly in the bone, considered to be the best quantitatively and qualitatively. The implants were placed surgically by a certified oral surgeon strictly according to the manufacturer's instructions regarding the osteotomy approach with rotating instruments, torque recommendations and minimum primary stability.
Six different implant types from four manufacturers were used. The implants were made from commercially pure titanium, that is Osseospeed (n = 14 × 3 implants) (Astra Tech), Bone level SLA (n = 10 × 3 imp.) and Tissue level SLA (n = 2 × 3 imp.) (Straumann), and Osstem (n = 1 × 3 imp.) (Osstem), or from a zirconium‐titanium alloy, that is Tissue level Roxolid (n = 1 × 3 imp.) and Bone level Roxolid (n = 1 × 3 imp.) (Straumann, Waldenburg, Switzerland). All implants had a microrough surface, and the diameter ranged between ø3.3 and ø4.5 mm, with implant lengths varying between 8 and 13 mm (Table 1).
TABLE 1.
Implant lengths and diameters (mm) (n = 32 study participants × 3 implants)
| L (mm) ø (mm) | 8 or 9 | 10 | 11 | 12 or 13 | Total |
|---|---|---|---|---|---|
| 3.3 | 0 | 30 | 0 | 5 | 35 |
| 3.5 | 1 | 0 | 9 | 12 | 22 |
| 4.0/4.1 | 6 | 13 | 2 | 0 | 21 |
| 4.5 | 0 | 0 | 13 | 5 | 18 |
| Total | 7 | 43 | 24 | 22 | 96 |
A two‐stage approach was adopted with submerged implants. At the same time, the existing removable prosthesis was relieved and lined with a soft silicone‐based reline material (G.C. Reline Soft, G.C. Corp.) when necessary. Post‐operative panoramic radiographs were taken on the day of implant surgery, complemented with radiographs taken at the second‐stage surgery.
2.4. Prosthodontic procedures
After approximately 3–4 months of healing, the implants were fitted to low‐profile stud attachments (Locator, ZEST Anchors LLC). The attachment cuff height was selected to match the mucosa thickness, so only the male seating area extended above the mucosa (Figure 1). New prostheses were made from heat‐cured poly‐methyl‐methacrylate (PMMA) reinforced with a metal alloy framework created from cobalt‐chromium. The matrix housings were attached to the prosthesis by being wholly incorporated into the PMMA, that is not connected to the metal framework. All prostheses included prefabricated acrylic teeth (Premium and Mondial PALA Teeth, Heraeus Kulzer GmbH) that were carefully adjusted for a balanced occlusion bilaterally and in protrusion and with no anterior contacts in habitual occlusion. All study participants were instructed on best practices for maintaining good oral health and motivated to uphold good oral hygiene, according to the specialist clinic's routine protocols. They were also advised to seek regular maintenance care. All study participants were offered to return to the specialist clinic for follow‐up examinations. The referring dentists received a written treatment history synopsis, prognosis estimate and a summary of the oral health guidance provided to the study participants.
FIGURE 1.

Three representative patients with an edentate maxilla with three implants spread anteriorly–posteriorly to form a triangular support zone for a full removable prosthesis. Top and centre row, one week following prosthesis delivery, bottom row, 14 months following prosthesis delivery
2.5. Data collection and follow‐up consultations
All follow‐up consultations included a clinical and radiological examination to assess the implants and the prosthesis status. The study participants were invited to complete the denture satisfaction scale questionnaire and the OHIP‐20 questionnaire.
2.6. Implant outcomes
The stability of all implants was assessed, and signs of mobility, pain or discomfort were defined as an implant failure. Measurements were made of the presence or absence of peri‐implant suppuration or fistula, the modified plaque and sulcus bleeding indices, 22 and the probing depth. 23
The clinical examination was complemented with a radiographic examination of an orthopantomogram. Reference bone levels on the mesial and distal sides were determined by measuring the distance between the implant platform and the most apical point of the alveolar crestal bone surrounding the implant. The loss in crestal bone height over the observation period was calculated relative to the bone level measured on the radiographs made at implant placement.
Implant success was defined as the absence of persistent subjective complaints, absence of recurrent peri‐implant infection with suppuration, absence of mobility, lack of continuous radiolucency around the implant and the possibility for restoration. 23
2.7. Prosthetic outcomes
The prosthesis was carefully examined for technical flaws, and the mucosa was inspected for signs of rubor or inflammation. Adverse technical events were defined as poor retention, fracture or chipping of the removable prosthesis. Adverse mechanical events included loosening the attachment or an implant's fracture. Any flaws were corrected by repairing or relining the prosthesis or replacing worn nylon ring inserts. Prosthesis success was defined according to the most relevant Cochrane systematic review criteria. 14 I.e., no occurrence of patrix or matrix becoming dislodged, worn, or loose, nor any need to be activated, replaced, or fractured more than twice in the first year or more than five replacements in the first five years. Repair includes replacement of worn or fractured overdenture teeth/fractured overdentures, relining of overdenture more than once in 5 years, or excision of patrix‐associated mucosal enlargement because of infringement on the shoulder/undersurface of the patrix. Retreatment denotes the need for a replacement prosthesis if part or all the implant overdenture is no longer serviceable because of either loss of implants or irreparable mechanical breakdown.
2.8. Patient‐reported outcomes
The study participants reported their experiences with the new implant‐supported prosthesis by completing the Denture Satisfaction Scale questionnaire, 20 and the short‐form version of the Oral Health Impact Profile questionnaire (OHIP‐20). 21
2.9. Statistical analyses
The success and survival estimates of implants and removable prostheses were based on Kaplan–Meier survival statistics. Nonparametric Kruskal–Wallis tests were used to compare group medians of prosthesis satisfaction and OHIP scores before the treatment started and after delivery of the implant‐stabilised prostheses. Statistical analysis was performed using SPSS software version 28 (SPSS Inc.).
3. RESULTS
3.1. Demographics
Thirty‐two study participants received three maxillary implants between March 2007 and October 2016. The baseline data of the study participants are shown in Table 2.
TABLE 2.
Baseline data, n = 32 study participants
| Variable | Categories | Number (%) |
|---|---|---|
| Gender | Male | 13 |
| Female | 19 | |
| Age (years) | Mean (SD) | 65 (9.2) |
| Min‐max | 38–83 | |
| Edentulous (months) | Mean (SD) | 4 (9) |
| Min‐max | 3–540 | |
| Smoking habits | Never/previous smoke | 23 |
| Smoke | 9 | |
| Mucosal health | Healthy | 14 |
| Stomatitis | 18 | |
| Oral/Denture hygiene | Good | 3 |
| Adequate | 17 | |
| Poor | 12 | |
| Denture use during sleep | Yes | 25 |
| No | 7 | |
| Sign of bruxism | Yes | 2 |
| No | 30 | |
| Chronic systemic condition | Yes | 20 |
| No | 12 | |
| Prescribed medication | Yes > 5 (polypharmacy) | 7 |
| Yes | 11 | |
| No | 14 | |
| Mandible dentition | Natural teeth 35–45 | 8 |
| Partial, no prosthesis | 4 | |
| Partial, fixed | 5 | |
| Partial, removable | 2 | |
| Full, implant‐denture | 10 | |
| Full, implant‐fixed | 3 |
Since the treatment completion, six study participants have passed away (after 9, 10, 19, 21, 72 and 107 months). Contact has been lost with three participants (after 33, 57 and 87 months), likely attributed to age and frailty (aged 81, 75 and 65 years). None of the study participants has declined to undergo annual clinical examinations.
3.2. Implant outcomes
Three study participants have lost implants after 75, 83 and 97 months. Two lost implants were in quadrant one and one in the anterior region. Kaplan–Meier statistics indicate an estimated survival and success at 168 months of 0.95 (SE 0.03) (Figure 2). All three felt no need to replace the implant and continued to use the prosthesis supported by only two implants. Peri‐implant bone loss of more than 2 mm was observed on 17% of all implants, while no or minor bone loss occurred on 38% of the implants after an average of 6.7 years (range 11–5 years) (Figure 3). The peri‐implant bone loss did not differ between the anterior and posterior implants (Table 3).
FIGURE 2.
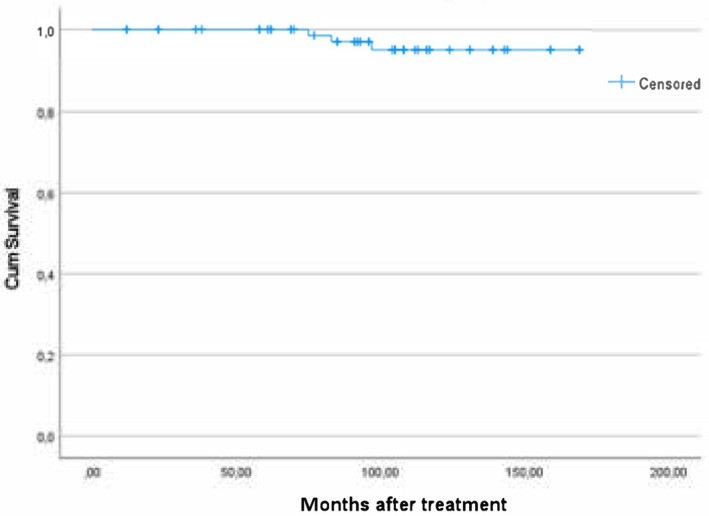
The success and survival of the implants (n = 32 patients × 3 implants)
FIGURE 3.
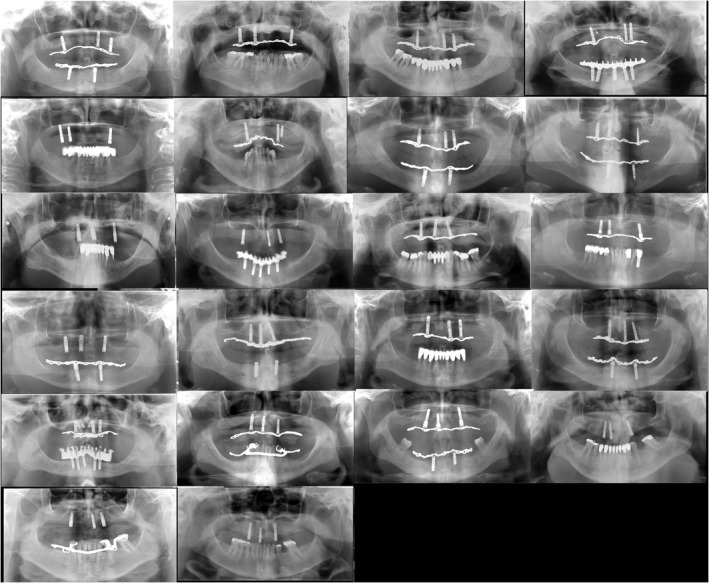
Panoramic radiographs from the latest clinical follow‐up examination (n = 23, mean, 6.7 years (range 11–5 years). Radiographs are sorted by the extent of the anterior–posterior spread of the three supporting implants (one flawed X‐ray not shown)
TABLE 3.
Marginal bone change at latest follow‐up examination with radiographs (mean, 6.7 years (range 11–5 years)
| Bone change | Frequency Q1–Anter.–Q2 | Per cent Q1–Anter.–Q2 | Total (%) |
|---|---|---|---|
| Bone gain/no loss (<0.1 mm) | 7–10–8 | 32–45–38 | 25 (38) |
| 0.1–≤2 mm bone loss | 12–9–8 | 54–41–38 | 29 (45) |
| >2 mm bone loss | 3–3–5 a | 14–14–24 | 11 (17) |
| Total | 22–22–21 a | 100–100–100 | 65 |
Note: Mean of mesial and distal measurements around implants in quadrants 1 and 2 and anteriorly (n = 22 study participants ×3 implants).
One implant lost, last measurement before implant loss was 2.1 mm.
3.3. Prosthetic outcomes
Oral stomatitis was observed for n = 15 study participants (47%), but none reported that the condition was considered bothersome. Twenty‐five participants reported that they did not store the overdenture extraorally while sleeping.
None of the study participants developed any adverse oral mucosal findings. Three study participants had their prostheses relined to correct for local ridge resorption.
Five study participants had a new prosthesis made after dropping their prosthesis during extraoral cleaning or fall accidents. Discounting these five replacements, the survival of the overdentures was 100%. Eleven individuals required repairs of the prosthesis. In order of frequency, these were due to a delaminated acrylic tooth (n = 4), a partial fracture of the prostheses that was repairable (n = 2), a matrix housing becoming loose (n = 2) and one attachment was replaced due to retention loss caused by wear. Several study participants elected to replace worn nylon ring inserts during their annual clinical consultation to improve prosthesis retention. No inserts were replaced due to breakage.
Since delivery of the prosthesis, the mean observation period is 111 months (range 9–154 months). According to Kaplan–Meier calculations, the estimated success of the prosthesis, that is no need for any repairs or retreatments, is 0.55 (SE 0.10) at 156 months (Figure 4).
FIGURE 4.
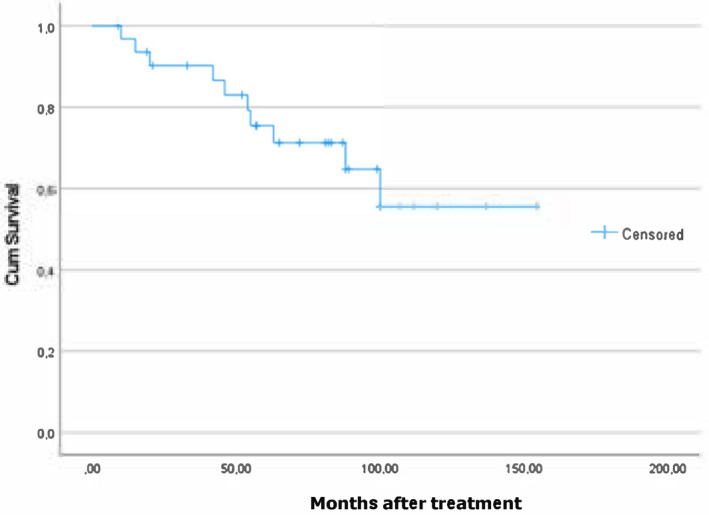
The success of prosthesis, that is prosthesis with no complications or need for any repairs (n = 32 patients)
3.4. Patient‐reported outcomes
The study participants reported significant statistical differences in OHIP scores between the pre‐ and post‐treatment. The OHIP scores remained high when the participants completed the subsequent questionnaire after several years (Figure 5). The patients also reported high denture satisfaction scores with their new maxillary overdenture, which remained high over the following 4–5 years (Figure 6)
FIGURE 5.
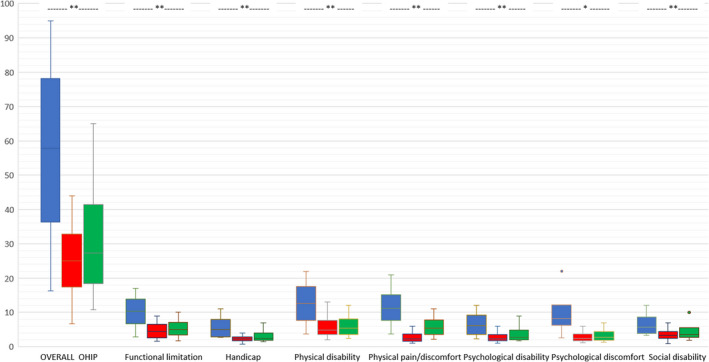
OHIP‐20 total and subscale scores. n = 12, n = 32 and n = 22 study participants reported OHIP, respectively pre‐, 0.5–1 year post‐ and 4–5 years post‐treatment. Statistically significant differences between post and pre‐treatment OHIP scores according to the Kruskal–Wallis tests marked * denotes p < .01 and **p < .001.
FIGURE 6.
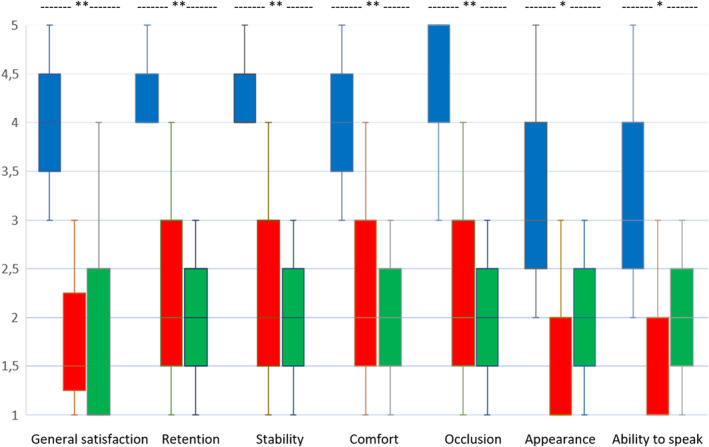
Denture Satisfaction Scale scores (median (range)). n = 12, n = 32 and n = 22 study participants reported OHIP, respectively pre‐, 0.5–1 year post‐ and 4–5 years post‐treatment. Statistically significant differences between post and pre‐treatment satisfaction scores according to the Kruskal–Wallis tests marked * denotes p < .01 and **p < .001.
4. DISCUSSION
4.1. Study design
Data obtained in a prospective single cohort study can indicate benefits and risks. However, it is acknowledged that it is risky to make robust statistical inferences. A strength of this study is a follow‐up period beyond five years of study participants that were not required to satisfy meticulous inclusion and exclusion criteria, which are otherwise often applied in more strictly controlled trials. Table 1 shows that a high proportion of the study participants had a chronic systemic condition and prescribed medication combined with a manifestation of stomatitis and inadequate oral and denture hygiene. The study participant cohort likely represents average patients seeking care in a private dental clinic. Therefore, despite the less‐than‐ideal intraoral situations, a superconstruction retained by stud attachments on two posterior plus one anterior implant with a good anterior–posterior spread appears to be a good solution – at least for some individuals with an edentulous maxilla.
4.2. Implant outcome
The implant outcomes in this study are comparable with the most favourable estimates of success and survival of implant‐supported maxillary overdentures, 13 and better than estimates based on pooled meta‐analyses of clinical studies on maxillary overdentures supported by three implants. 15 The precise reasons for the positive outcomes of this current clinical study remain uncertain. Still, the combination of some key elements may have been crucial.
The anterior–posterior spread of the implants was maximised to create the largest possible triangular support area. Determining the support zone is essential when planning for or addressing the prognosis of telescopic prostheses on very few remaining teeth. 24 , 25 The best prognosis is obtained when the support zone is triangular or quadrangular, that is corresponding to class E and class F, respectively, in the classification system intended to design removable partial prostheses. 26 Four individual attachments with a good anterior–posterior spread create a quadrangular support zone. In comparison, three attachments make a triangular support zone. No scientific literature shows that a quadrangular is superior to a triangular support zone regarding telescopic prostheses or removable partial prostheses on teeth. The same applies to the limited number of clinical studies that have examined combined maxillary tooth‐implant removable partial prostheses, 27 , 28 and telescopic solutions. 29 , 30 , 31 , 32 In these studies, implants are placed ‘in strategic positions to create a missing favorable support zone’, that is to create a quadrangular or triangular support zone.
While there is a lack of studies reporting on using three stud attachments with an anterior–posterior spread that creates a triangular support zone, several papers report using four stud attachments to create a quadrangular support zone. 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 Only one of these studies discussed the relevancy of implant number and forwarded the following: ‘Interestingly, the use of three implants may also provide sufficient retention to satisfy the patient during function, if the anterior‐posterior spread is large enough’. 40
4.3. Prosthetic outcomes
Low‐profile stud attachments do not require extensive hollowing out of the intaglio surface of the overdenture to create enough vertical space to accommodate the attachment components. A stud attachment metal housing containing a nylon insert requires ~3.2 mm, ball attachments require around ~6 mm and milled or cast bar solutions even more than 6 mm vertical space. The prostheses were reinforced by a metallic mesh made from cobalt‐chromium, increasing the stiffness. The improved flexural properties reduce the overdenture base deformation. It has been postulated that a metal reinforcement decreases and distributes evenly strains on the underlying supporting structures. 46 , 47
The occlusion of the overdentures was balanced to avoid tilting the prosthesis during biting off and eccentric chewing. Correctly adjusting the occlusion is crucial and requires clinical skill and competency.
Milled bars with or without additional stud attachments are optimal in several circumstances when there is extensive hard and soft tissue loss. At the same time, such solutions may be considered over‐engineered in other situations. In this perspective, an overruling consideration is that patients must maintain good oral hygiene and biofilm control to minimise the risk of developing peri‐implantitis 48 since peri‐implantitis is a biofilm‐associated pathological condition. 49 It follows that prosthesis elements or attachments that impede the patient's ability to remove biofilms from all surfaces are potentially detrimental. Daily peri‐implant cleaning under a fixed prosthesis or around a bar used as a mesostructure requires eye‐hand coordination ability, finger dexterity and correct use of specially designed intraoral cleaning instruments. Particularly, elderly individuals will experience difficulties with increased development of frailty. 50 On the other hand, most patients will use a conventional toothbrush to remove biofilms intraorally on individual attachments or copings, and the biofilm on the prosthesis surfaces extraorally.
In this context, the insertion path of an overdenture should facilitate easy removal and replacement of the prosthesis twice daily for extraoral cleaning. While magnets were favoured for this reason in the past, low‐profile stud attachments allow easy removal if the nylon ring retention level has been adjusted to the users' finger strength. 50
4.4. Maintenance needs
Clinical studies on stud‐attachments report different incidences of adverse events, complications and maintenance needs. The differences may be related to underlying clinical variables such as patient selection, the number of implants to retain the overdenture and support zone configurations. 51 However, it also seems that the estimates reflect the everlasting debate in prosthodontics on what constitutes a complication versus what should be expected maintenance. 5 , 7 , 52 , 53 The concept behind the Locator attachment system is that the nylon ring insert is the weakest part that needs to be replaced, as it gradually, after use, will exhibit wear while protecting the more costly stud attachment from wear. The nylon ring needs to be replaced because lost retention force varies from individual to individual. In this study, the replacement of nylon inserts was on average every two years, with further details presented in an earlier report. 18 The few situations in the current study that arguably could be labelled as complications were quickly correctable and did not entail remakes of the prosthesis.
4.5. Patient‐reported outcomes
Various factors determine patients' choice of implant‐supported prostheses. 54 One element is that patients' valuation of oral health outcomes differs, which is reflected in their decision of whether the perceived additional health benefits of a particular prosthetic solution outweigh the higher costs. 16 Another critical consideration in the treatment decision process is fear of pain or complications related to invasive surgery. 55 Patients' preferences are that any intraoral surgery should be minimally invasive. 56 Hence, it is not unexpected that patient‐reported outcome measures are inconsistent when comparing implant‐supported fixed versus removable prostheses for fully edentulous patients. 57
Several studies emphasise affordability and opportunity costs as core elements. 58 However, this assumption is disputed, and for patients needing maxillary implant‐supported prostheses, there are no contingent valuation studies. 17 This study findings indicate that the three stud retained solution results in clinical and patient‐reported outcomes comparable to those obtained with the alternative overdenture solutions on four implants, but at a lower cost. In Norway, the price for surgical placement of three versus four implants and the associated range of implant components creates a patient fee difference of around 20%. This difference increases further if a need is to graft an implant site to create a quadrangular support zone. Any bar solution increases the costs even further due to the additional expenses for dental laboratory services.
5. CONCLUSION
In many clinical situations, it is acknowledged that a bar‐splinted solution, with or without the use of a milled bar with or without additional retentive attachments, on more than three implants is a more predictable solution than the described solution in this paper. However, a more engineered superconstruction on added implants increases the manufacturing price and the patient and possible third‐party stakeholders must always trade‐off between simplicity and costs versus predictability of clinical performance. The positive findings in this clinical study strengthen the notion that for many individuals with an edentulous maxilla, a removable prosthesis retained by three implants fitted with low‐profile stud‐attachment is an optimal technical solution.
AUTHOR CONTRIBUTIONS
AM and CH: Participant recruitment, prosthodontic treatment, clinical data collection and measurements. AJ: Ethics approval, statistical analysis, AM, CH and AJ: Research design, manuscript preparation and final manuscript review.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/joor.13364.
Mo A, Hjortsjö C, Jokstad A. Maxillary overdenture on three implants retained by low‐profile stud attachments – A prospective cohort study. J Oral Rehabil. 2022;49:1069‐1079. doi: 10.1111/joor.13364
DATA AVAILABILITY STATEMENT
The data supporting this study's findings are available from the corresponding author upon reasonable request and following the approval of the local Regional Ethics Committee. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Sharka R, Abed H, Hector M. Oral health‐related quality of life and satisfaction of edentulous patients using conventional complete dentures and implant‐retained overdentures: an umbrella systematic review. Gerodontology. 2019;36:195‐204. doi: 10.1111/ger.12399 [DOI] [PubMed] [Google Scholar]
- 2. Thalji G, McGraw K, Cooper LF. Maxillary complete denture outcomes: a systematic review of patient‐based outcomes. Int J Oral Maxillofac Implants. 2016;31(suppl):s169‐s181. doi: 10.11607/jomi.16suppl.g5.1 [DOI] [PubMed] [Google Scholar]
- 3. McGarry TJ, Nimmo A, Skiba JF, Ahlstrom RH, Smith CR, Koumjian JH. Classification system for complete edentulism. The American College of Prosthodontics. J Prosthodont. 1999;8:27‐39. doi: 10.1111/j.1532-849x.1999.tb00005.x [DOI] [PubMed] [Google Scholar]
- 4. Parel SM. Implants and overdentures: the osseointegrated approach with conventional and compromised applications. Int J Oral Maxillofac Implants. 1986;1:93‐99. [PubMed] [Google Scholar]
- 5. Goodacre C, Goodacre B. Fixed vs removable complete arch implant prostheses: a literature review of prosthodontic outcomes. Eur J Oral Implantol. 2017;10(suppl 1):13‐34. [PubMed] [Google Scholar]
- 6. Saravi BE, Putz M, Patzelt S, Alkalak A, Uelkuemen S, Boeker M. Marginal bone loss around oral implants supporting fixed versus removable prostheses: a systematic review. Int J Implant Dent. 2020;6:20. doi: 10.1186/s40729-020-00217-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Karasan D, Fehmer V, Ligoutsikou M, Srinivasan M, Sailer I. The influence of patient‐related factors and material selection on the clinical outcomes of fixed and removable complete implant prostheses: an overview on systematic reviews. Int J Prosthodont. 2021;34:s46‐s62. doi: 10.11607/ijp.7070 [DOI] [PubMed] [Google Scholar]
- 8. Tsigarida A, Chochlidakis K. A comparison between fixed and removable mandibular implant‐supported full‐arch prostheses: an overview of systematic reviews. Int J Prosthodont. 2021;34:s85‐s92. doi: 10.11607/ijp.6911 [DOI] [PubMed] [Google Scholar]
- 9. Vazouras K, Taylor T. Full‐arch removable vs fixed implant restorations: a literature review of factors to consider regarding treatment choice and decision‐making in elderly patients. Int J Prosthodont. 2021;34:s93‐s101. doi: 10.11607/ijp.7016 [DOI] [PubMed] [Google Scholar]
- 10. Messias A, Nicolau P, Guerra F. Different interventions for rehabilitation of the edentulous maxilla with implant‐supported prostheses: an overview of systematic reviews. Int J Prosthodont. 2021;34:s63‐s84. doi: 10.11607/ijp.7162 [DOI] [PubMed] [Google Scholar]
- 11. Jokstad A, Sanz M, Ogawa T, et al. A systematic review of the role of implant design in the rehabilitation of the edentulous maxilla. Int J Oral Maxillofac Implants. 2016;31:s43‐s99. doi: 10.11607/jomi.16suppl.g2 [DOI] [PubMed] [Google Scholar]
- 12. Raghoebar GM, Meijer HJ, Slot W, Slater JJ, Vissink A. A systematic review of implant‐supported overdentures in the edentulous maxilla, compared to the mandible: how many implants? Eur J Oral Implantol. 2014;7(Suppl 2):s191‐s201. [PubMed] [Google Scholar]
- 13. Di Francesco F, De Marco G, Gironi Carnevale UA, Lanza M, Lanza A. The number of implants required to support a maxillary overdenture: a systematic review and meta‐analysis. J Prosthodont Res. 2019;63:15‐24. doi: 10.1016/j.jpor.2018.08.006 [DOI] [PubMed] [Google Scholar]
- 14. Payne AG, Alsabeeha NH, Atieh MA, Esposito M, Ma S, Anas E‐WM. Interventions for replacing missing teeth: attachment systems for implant overdentures in edentulous jaws. Cochrane Database Syst Rev. 2018;10:CD008001. doi: 10.1002/14651858.CD008001.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ghiasi P, Ahlgren C, Larsson C, Chrcanovic BR. Implant and prosthesis failure rates with implant‐supported maxillary overdentures: a systematic review. Int J Prosthodont. 2021;34:482‐491. doi: 10.11607/ijp.6905 [DOI] [PubMed] [Google Scholar]
- 16. Van de Winkel T, Heijens L, Listl S, Meijer G. What is the evidence on the added value of implant‐supported overdentures? A review. Clin Implant Dent Relat Res. 2021;23:644‐656. doi: 10.1111/cid.13027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sendi P, Ramadani A, Zitzmann NU, Bornstein MM. A systematic review of WTA‐WTP disparity for dental interventions and implications for cost‐effectiveness analysis. Healthcare. 2020;8:301. doi: 10.3390/healthcare8030301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mo A, Hjortsjö C, Olsen‐Bergem H, Jokstad A. Maxillary 3‐implant removable prostheses without palatal coverage on Locator abutments ‐ a case series. Clin Oral Implants Res. 2016;27:1193‐1199. doi: 10.1111/clr.12724 [DOI] [PubMed] [Google Scholar]
- 19. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344‐349. doi: 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 20. Allen PF, McMillan AS, Walshaw D. A patient‐based assessment of implant‐stabilized and conventional complete dentures. J Prosthet Dent. 2001;85:141‐147. doi: 10.1067/mpr.2001.113214 [DOI] [PubMed] [Google Scholar]
- 21. Allen F, Locker D. A modified short version of the oral health impact profile for assessing health‐related quality of life in edentulous adults. Int J Prosthodont. 2002;15:446‐450. [PubMed] [Google Scholar]
- 22. Mombelli A, van Oosten MAC, Schürch E Jr, Lang NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987;2:145‐151. doi: 10.1111/j.1399-302x.1987.tb00298.x [DOI] [PubMed] [Google Scholar]
- 23. Buser D, Weber HP, Lang NP. Tissue integration of non‐submerged implants. 1‐year results of a prospective study with 100 ITI hollow‐cylinder and hollow‐screw implants. Clin Oral Implants Res. 1990;1:33‐40. doi: 10.1034/j.1600-0501.1990.010105.x [DOI] [PubMed] [Google Scholar]
- 24. Szentpétery V, Lautenschläger C, Setz JM. Frictional telescopic crowns in severely reduced dentitions: a 5‐year clinical outcome study. Int J Prosthodont. 2012;25:217‐220. [PubMed] [Google Scholar]
- 25. Hinz S, Schweyen R, Hey J, Setz J, Arnold C. Clinical performance of non‐precious metal double crowns with friction pins in severely reduced dentitions. Clin Oral Investig. 2020;24:3567‐3575. doi: 10.1007/s00784-020-03228-1 [DOI] [PubMed] [Google Scholar]
- 26. Steffel VL. Planning removable partial dentures. J Prosthet Dent. 1962;12:524‐535. [Google Scholar]
- 27. Hug S, Mantokoudis D, Mericske‐Stern R. Clinical evaluation of 3 overdenture concepts with tooth roots and implants: 2‐year results. Int J Prosthodont. 2006;19:236‐243. [PubMed] [Google Scholar]
- 28. Kaufmann R, Friedli M, Hug S, Mericske‐Stern R. Removable dentures with implant support in strategic positions followed for up to 8 years. Int J Prosthodont. 2009;22:233‐241. [PubMed] [Google Scholar]
- 29. Krennmair G, Krainhöfner M, Waldenberger O, Piehslinger E. Dental implants as strategic supplementary abutments for implant‐tooth‐supported telescopic crown‐retained maxillary dentures: a retrospective follow‐up study for up to 9 years. Int J Prosthodont. 2007;20:617‐622. [PubMed] [Google Scholar]
- 30. Bernhart G, Koob A, Schmitter M, Gabbert O, Stober T, Rammelsberg P. Clinical success of implant‐supported and tooth‐implant‐supported double crown‐retained dentures. Clin Oral Investig. 2012;16:1031‐1037. doi: 10.1007/s00784-011-0592-1 [DOI] [PubMed] [Google Scholar]
- 31. Joda T. Combined tooth‐implant‐supported telescopic prostheses in a midterm follow‐up of >2 years. Int J Prosthodont. 2013;26:536‐540. doi: 10.11607/ijp.3289 [DOI] [PubMed] [Google Scholar]
- 32. Rinke S, Ziebolz D, Ratka‐Krüger P, Frisch E. Clinical outcome of double crown‐retained mandibular removable dentures supported by a combination of residual teeth and strategic implants. J Prosthodont. 2015;24:358‐365. doi: 10.1111/jopr.12214 [DOI] [PubMed] [Google Scholar]
- 33. Kappel S, Klotz AL, Eberhard L, Lorenzo Bermejo J, Rammelsberg P, Giannakopoulos NN. Maxillary implant overdentures on two or four implants. A prospective randomized cross‐over clinical trial of implant and denture success and survival. Clin Oral Implants Res. 2021;32:1061‐1071. doi: 10.1111/clr.13800 [DOI] [PubMed] [Google Scholar]
- 34. Bouhy A, Rompen E, Lamy M, Legros C, Lecloux G, Lambert F. Maxillary implant overdenture retained by four unsplinted attachments and opposed by a natural or fixed dentition: one‐year clinical outcomes. Clin Oral Implants Res. 2020;31:747‐767. doi: 10.1111/clr.13623 [DOI] [PubMed] [Google Scholar]
- 35. Manes Ferrer JF, Fernandez‐Estevan L, Selva‐Otaolaurruchi E, Labaig‐Rueda C, Sola‐Ruiz MF, Agustin‐Panadero R. Maxillary implant‐supported overdentures: mechanical behavior comparing individual axial and bar retention systems. A cohort study of edentulous patients. Medicina (Kaunas). 2020;56:139. doi: 10.3390/medicina56030139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Boven GC, Speksnijder CM, Meijer HJA, Vissink A, Raghoebar GM. Masticatory ability improves after maxillary implant overdenture treatment: a randomized controlled trial with 1‐year follow‐up. Clin Implant Dent Relat Res. 2019;21:369‐376. doi: 10.1111/cid.12721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Anadioti E, Gates WD 3rd, Elpers J, De Kok IJ, Cooper LF. Retrospective cohort analysis of maxillary overdentures retained by unsplinted implants. J Prosthet Dent. 2019;122(3):301‐308.e1. doi: 10.1016/j.prosdent.2018.10.014 [DOI] [PubMed] [Google Scholar]
- 38. Lian M, Zhao K, Wang F, Huang W, Zhang X, Wu Y. Stud‐vs‐bar attachments for maxillary four‐implant‐supported overdentures: 3‐ to 9‐year results from a retrospective study. Int J Oral Maxillofac Implants. 2019;34:936‐946. doi: 10.11607/jomi.7224 [DOI] [PubMed] [Google Scholar]
- 39. Offord D, Mathieson G, Kingsford N, Matthys C, Glibert M, De Bruyn H. Peri‐implant health, clinical outcome and patient‐centred outcomes of implant‐supported overdentures in the mandible and the maxilla. BDJ Open. 2017;3:17017. doi: 10.1038/bdjopen.2017.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Strong SM. Success of unsplinted implant‐retained removable mandibular and maxillary overdentures: a retrospective study of consecutive cases. Int J Periodontics Restorative Dent. 2015;35:533‐539. doi: 10.11607/prd.2233 [DOI] [PubMed] [Google Scholar]
- 41. Wang F, Monje A, Huang W, Zhang Z, Wang G, Wu Y. Maxillary four implant‐retained overdentures via Locator® attachment: intermediate‐term results from a retrospective study. Clin Implant Dent Relat Res. 2016;18:571‐579. doi: 10.1111/cid.12335 [DOI] [PubMed] [Google Scholar]
- 42. Ebinger A, Katsoulis J, Hakimi M, Mazzi D, Mericske‐Stern R. Mucosal manifestations in the edentulous maxilla with implant‐supported prostheses: clinical results from a well‐maintained patient cohort. Clin Implant Dent Relat Res. 2016;18:639‐648. doi: 10.1111/cid.12345 [DOI] [PubMed] [Google Scholar]
- 43. Cordaro L, Torsello F, Mirisola di Torresanto V, Baricevic M. Rehabilitation of an edentulous atrophic maxilla with four unsplinted narrow diameter titanium‐zirconium implants supporting an overdenture. Quintessence Int. 2013;44:37‐43. doi: 10.3290/j.qi.a28745 [DOI] [PubMed] [Google Scholar]
- 44. Zou D, Wu Y, Huang W, et al. A 3‐year prospective clinical study of telescopic crown, bar, and locator attachments for removable four implant‐supported maxillary overdentures. Int J Prosthodont. 2013;26:566‐573. doi: 10.11607/ijp.3485 [DOI] [PubMed] [Google Scholar]
- 45. Troeltzsch M, Troeltzsch V, Brodine AH, Frankenberger R, Messlinger K, Troeltzsch M. Clinical performance and peri‐implant parameters of 132 implants supporting locator‐retained overdentures: a case series of 33 patients. Int J Oral Maxillofac Implants. 2013;28:1132‐1139. doi: 10.11607/jomi.3009 [DOI] [PubMed] [Google Scholar]
- 46. Gibreel MF, Khalifa A, Said MM, et al. Biomechanical aspects of reinforced implant overdentures: a systematic review. J Mech Behav Biomed Mater. 2019;91:202‐211. doi: 10.1016/j.jmbbm.2018.12.006 [DOI] [PubMed] [Google Scholar]
- 47. Takahashi T, Gonda T, Maeda Y. Can reinforcement of maxillary implant overdentures decrease stress on underlying implants? Int J Oral Maxillofac Implants. 2017;32:63‐69. doi: 10.11607/jomi.4921 [DOI] [PubMed] [Google Scholar]
- 48. Sanz M, Herrera D, Kebschull M, et al. Treatment of stage I‐III periodontitis‐The EFP S3 level clinical practice guideline. J Clin Periodontol. 2020;47(suppl 22):4‐60. doi: 10.1111/jcpe.13290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Berglundh T, Armitage G, Araujo MG, et al. Peri‐implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Diseases and Conditions. J Periodontol. 2018;89(suppl 1):S313‐S318. doi: 10.1002/JPER.17-0739 [DOI] [PubMed] [Google Scholar]
- 50. Schimmel M, Müller F, Suter V, Buser D. Implants for elderly patients. Periodontol 2000. 2017;73:228‐240. doi: 10.1111/prd.12166 [DOI] [PubMed] [Google Scholar]
- 51. Guedat C, Nagy U, Schimmel M, Müller F, Srinivasan M. Clinical performance of LOCATOR® attachments: a retrospective study with 1‐8 years of follow‐up. Clin Exp Dent Res. 2018;4:132‐140. doi: 10.1002/cre2.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Walton TR. Making sense of complication reporting associated with fixed dental prostheses. Int J Prosthodont. 2014;27:114‐118. doi: 10.11607/ijp.2014.2.ic [DOI] [PubMed] [Google Scholar]
- 53. Payne AG, Walton TR, Walton JN, Solomons YF. The outcome of implant overdentures from a prosthodontic perspective: proposal for a classification protocol. Int J Prosthodont. 2001;14:27‐32. [PubMed] [Google Scholar]
- 54. Leles CR, Dias DR, Nogueira TE, McKenna G, Schimmel M, Jordão LMR. Impact of patient characteristics on edentulous subjects' preferences for prosthodontic rehabilitation with implants. Clin Oral Implants Res. 2019;30:285‐292. doi: 10.1111/clr.13414 [DOI] [PubMed] [Google Scholar]
- 55. Elfadil S, Johnston B, Normand C, Allen F, O'Connell B. An investigation of the characteristics of edentulous patients who choose or refuse implant treatment. Int J Prosthodont. 2021;34:147‐153. doi: 10.11607/ijp.6222 [DOI] [PubMed] [Google Scholar]
- 56. Pommer B, Mailath‐Pokorny G, Haas R, Busenlechner D, Fürhauser R, Watzek G. Patients' preferences towards minimally invasive treatment alternatives for implant rehabilitation of edentulous jaws. Eur J Oral Implantol. 2014;7(suppl 2):S91‐S109. [PubMed] [Google Scholar]
- 57. Yao CJ, Cao C, Bornstein MM, Mattheos N. Patient‐reported outcome measures of edentulous patients restored with implant‐supported removable and fixed prostheses: a systematic review. Clin Oral Implants Res. 2018;29(suppl 16):s241‐s254. doi: 10.1111/clr.13286 [DOI] [PubMed] [Google Scholar]
- 58. Zhang Q, Jin X, Yu M, et al. Economic evaluation of implant‐supported overdentures in edentulous patients: a systematic review. Int J Prosthodont. 2017;30:321‐326. doi: 10.11607/ijp.5023 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting this study's findings are available from the corresponding author upon reasonable request and following the approval of the local Regional Ethics Committee. The data are not publicly available due to privacy or ethical restrictions.


