Abstract
Aim
Periodontal diseases are associated with cardiovascular risk factors/diseases, and whether home oral hygiene practices are inversely related to the same conditions could carry relevant practical implications. We investigated the association of home oral hygiene habits with hypertension.
Materials and Methods
During World Hypertension Day 2020, a nationwide cross‐sectional survey was conducted on volunteers ≥18 years at 733 Italian pharmacies. Participants underwent standardized blood pressure (BP) measurement and answered a questionnaire on cardiovascular risk factors, oral health status, and home oral hygiene habits (toothbrushing daily frequency and manual/electric toothbrush). The association between home oral care habits and BP was assessed using multivariate logistic regression. Interactions between exposures and outcome were formally tested.
Results
Among the 4506 participants (44.8% males, 66.1 ± 37.8 years), 47.6% reported brushing ≥3 times/day and 23.4% declared using the electric toothbrush. Brushing ≥3 versus <3 times/day and use of electric versus manual toothbrush were associated with 19% (odds ratio [OR]: 0.81, 95% confidence interval [CI] 0.70–0.94) and 28% (OR: 0.72, 95% CI 0.61–0.85) lower odds of hypertension, respectively. No significant additive interaction was observed in the association of exposures with the outcome.
Conclusions
Regular daily brushing and electric toothbrushing are associated with a better BP profile in a real‐world context. Future interdisciplinary research is warranted to test these findings.
Keywords: blood pressure, cardiovascular diseases, hypertension, oral hygiene, toothbrushing
Clinical Relevance.
Scientific rationale for study: Home oral hygiene is an accessible, widespread practice for controlling dysbiotic biofilm and local inflammation. Whether it is also associated with blood pressure (BP) remains uninvestigated. We tested its association with BP profiles/control in a real‐world context.
Principal findings: Individuals brushing their teeth at least three times/day and electric toothbrush users had better systolic BP and lower odds of prevalent/uncontrolled hypertension than those reporting less frequent brushing and manual toothbrushing.
Practical implications: We provide a proof‐of‐concept for further research testing the added benefit of home oral hygiene for cardiovascular prevention, with possibly relevant public health implications.
1. INTRODUCTION
Cardiovascular diseases (CVD) are the most common non‐communicable diseases and a leading cause of death worldwide (Virani et al., 2020). This heavy burden of disease, disability, and mortality is driven by several cardiovascular risk factors, including high blood pressure (BP), tobacco smoking, dyslipidaemia, and diabetes, all of which require an integrated multimodal approach combining non‐pharmacological and pharmacological strategies for an effective management.
Growing evidence supports an independent association between periodontal health status and BP (Del Pinto, Landi, et al., 2021a, 2021b). Specifically, gingival bleeding has been related to worse BP profile in individuals with and without chronic periodontitis (Pietropaoli, Del Pinto, et al., 2020; Pietropaoli, Monaco, et al., 2020), and systemic inflammation was shown to mediate this association to a various extent and without threshold effect (Pietropaoli et al., 2018; Pietropaoli, Del Pinto, et al., 2020). Conversely, a healthy periodontium was associated with a better BP profile during antihypertensive therapy and with lower odds of uncontrolled hypertension (Pietropaoli et al., 2018). In parallel, systemic exposure to periodontal microbiota was found to be related to higher mean‐measured BP values, higher odds of high/uncontrolled BP, and with more active periodontal disease (Pietropaoli et al., 2019). Evidence of a common genetic background in terms of polymorphisms in genes entailed in the immune function supports the pathogenic hypothesis of a proinflammatory milieu that favours the development of both hypertension and periodontal diseases and related CVD (Del Pinto, Pietropaoli, et al., 2020; Del Pinto, Landi, et al., 2021a; Landi et al., 2021).
According to meta‐analytic evidence, non‐surgical periodontal therapy might be beneficial for BP lowering and for improving hypertension control (Sharma et al., 2021). In agreement with this, novel evidence indicates that regularly attending the dental office has an independent association with improved BP, with a possible mediating effect of decreased systemic inflammatory burden (Del Pinto, Monaco, et al., 2021). Thus, it would be reasonable to argue that regular tooth brushing has an impact on cardiovascular health. So far, the impact of home oral hygiene practices on hypertension has remained uninvestigated. Herein, we aimed to assess the association between BP and home oral hygiene habits, expressed in terms of frequency and modality of tooth brushing, in a large sample of Italian adults enrolled in a cross‐sectional, real‐world, nationwide survey.
2. MATERIALS AND METHODS
2.1. Study design and population
During World Hypertension Day 2020 and the following week (17–24 October 2020), a nationwide, observational, cross‐sectional, opportunistic survey endorsed by the Italian Society of Hypertension and the national network of pharmacies affiliated with the Italian Federation of Pharmacies (Federfarma) was conducted at 733 Italian pharmacies of the Federfarma network with the aim of increasing awareness of BP and related cardiovascular risk factors. The campaign was promoted nationally through media and the web (bit.ly/3ufPVmH). Eligible participants were recruited at local sites using convenience sampling, in analogy with previous campaigns (Beaney et al., 2019; Del Pinto, Pagliacci, et al., 2020). Specifically, self‐presented volunteer adults aged 18 years or more who had been made aware of the availability of BP screening and wished to take advantage of the campaign and who provided formal consent to participation were enrolled in the survey (Figure S1). Staff at participating pharmacies received specific training on BP measurement and administered a questionnaire on major demographic and clinical features, lifestyle habits, oral health status, and home oral hygiene habits, as specified below. The survey was conducted in conformity with the Helsinki Declaration. Data were anonymized at enrolment, making the identification of participants not possible.
2.2. Exposure, control, and outcome
Herein, we aimed to answer the clinical question whether, in the study population reported above (Italian volunteer adults aged ≥18 years enrolled with convenience sampling at Italian pharmacies), individuals who were exposed to tooth brushing ≥3 times/day (exposed) had a better BP profile (outcome) compared with those who were not (non‐exposed).
2.3. BP measurement
Participants underwent standardized BP measurements by trained pharmacists according to a standard protocol. Specifically, three consecutive BP measurements at 1 min intervals taken with automated, validated sphygmomanometers were collected after a 2 min rest in the sitting position, with back and arm supported and feet flat on floor, and the average of the second and third measurements was recorded.
2.4. Self‐reported questionnaire data
Participants answered an anonymous questionnaire on major demographic (age and sex) and anthropometric (weight and height) features, cardiovascular risk factors (smoke, obesity, established diagnosis of diabetes mellitus, dyslipidaemia, hypertension, personal history of CVD or chronic kidney disease [CKD], and family history of CVD), lifestyle habits (daily physical activity, use of cooking salt, and fruits/vegetables consumption), oral health status (diagnosed periodontitis, gingival bleeding on brushing [BoB]), and home oral hygiene habits (daily tooth brushing frequency, that is, 0, 1, 2, 3 times or more, and use of manual or electric toothbrush). Anonymous data were then entered by staff at participating sites on online forms that were centralized at the Italian Society of Hypertension coordinating centre for subsequent analyses.
2.5. Definitions
Prevalent hypertension was defined as BP ≥140 and/or 90 mmHg or as taking antihypertensive medications (Williams et al., 2018; Del Pinto, Pagliacci, et al., 2020). According to 2018 European Society of Cardiology/European Society of Hypertension (ESC/ESH) guidelines, individuals who reported taking antihypertensive medications were considered as having measured BP levels within the predefined therapeutic goals if their BP was less than 130/80 mmHg below the age of 65 years, and less than 140/80 mmHg if ≥65 years; otherwise, they were considered as having uncontrolled hypertension (Williams et al., 2018). Sedentary lifestyle was expressed as daily physical activity time less than 30 min (Piepoli et al., 2016). Body mass index (BMI) was derived from self‐reported data as the ratio between body weight (expressed in kilograms) and the square of the body height (expressed in meters), and participants were classified accordingly as being underweight, normal weight, overweight, or obese.
2.6. Statistical analysis
Statistical analyses and data visualization were performed using R (v4.0.2). Unpaired Student's t test and chi‐squared test were used to detect differences in quantitative (mean ± SD) and qualitative (N, %) data, respectively (statistical significance: p < .05).
Daily toothbrushing frequency was expressed as a categorical variable (tooth brushing once, twice, less than three, and three or more times a day). Tooth brushing ≥3 times/day was the exposure. Tooth brushing <3 times/day was the control. Prevalent and uncontrolled hypertension as defined above, globally referred to as BP profile, were the outcome. The association of the exposure with the outcome was investigated in terms of odds ratio (OR; 95% confidence interval [CI]) using logistic regression adjusted for variables of clinical relevance among those collected in the survey, namely sex, age (bivariate model), BMI, current smoking, self‐reported diabetes, self‐reported hypercholesterolaemia, use of electric toothbrush, daily vegetable/fruit consumption, and physical activity (multivariate model). Interactions between the exposure to toothbrush frequency (≥ or <3 daily times) and type of toothbrush device (manual/electric) and the outcome (BP status) were formally tested using relative excess risk due to interaction (RERI) and synergy index (SI). RERI is the proportion of outcome among those with both exposures that is attributable to their interaction (Alli, 2021). SI represents the excess risk from both exposures when interaction is present, relative to the risk from exposure when interaction is absent, and it is the measure of choice in assessing the presence of additive interaction in multivariate models (Skrondal, 2003; de Jager et al., 2011). Estimation of CI for the measures of additive interaction was performed by applying the MOVER method (Zou, 2008).
Multiple comparisons in terms of mean systolic BP values across combinations of type of toothbrush (electric/manual) and brushing frequency were explored using Bonferroni‐corrected Wilcoxon rank sum test with continuity correction.
Data were analysed as recorded, without imputation for missing data. Statistical significance was set at p < .05.
3. RESULTS
3.1. Overall findings
A total of 4506 adult volunteers (39.7% males, 59.9 ± 31.9 years) participated in the survey. Their demographic and clinical features are presented in Table 1. Briefly, the majority were overweight/obese, sedentary individuals who otherwise mostly reported being non‐smokers, regularly consuming fruits and vegetables, and making limited use of cooking salt. Nearly half of the examined population had a history of treated hypertension, and measured BP fell either below the hypertension threshold or within the normal recommended therapeutic goals in 50.6% of participants. More than one third of the sample had a family history of CVD, nearly the same proportion reported having high serum cholesterol levels, while less individuals reported concomitant major cardiovascular risk factors, like smoke and diabetes. Globally, 47.6% of participants reported brushing ≥3 times/day and 23.4% declared using the electric toothbrush. The majority of normotensive participants (55.9%), but only 42.2% of hypertensive individuals, reported brushing ≥3 times/day. In parallel, 32.1% of normotensives and only 17.9% of hypertensives reported using the electric toothbrush. Less than 1 in 10 individuals reported suffering from periodontitis (8.8%), while BoB was reported by nearly one in five responders (18.7%).
TABLE 1.
Clinical and demographic characteristics and lifestyle habits of the examined sample overall and after stratification according to toothbrushing frequency and the use of manual or electric toothbrush (see text for further details)
| Toothbrushing frequency | Toothbrush type | ||||||
|---|---|---|---|---|---|---|---|
| Overall | <3 per day | ≥3 per day | p‐Value | Electric | Manual | p‐Value | |
| n | 4506 | 2361 | 2145 | 1053 | 3453 | ||
| Male | 1788 (39.7) | 1079 (45.7) | 709 (33.1) | <.001 | 377 (35.8) | 1411 (40.9) | .004 |
| Age | 59.95 (31.93) | 62.40 (41.51) | 57.25 (15.21) | <.001 | 53.68 (13.92) | 61.86 (35.44) | <.001 |
| BMI | 26.82 (20.68) | 27.39 (15.67) | 26.20 (25.06) | .053 | 26.13 (18.03) | 27.04 (21.43) | .212 |
| SBP | 133.74 (18.69) | 135.65 (18.59) | 131.63 (18.58) | <.001 | 129.02 (17.14) | 135.17 (18.90) | <.001 |
| DBP | 78.94 (10.94) | 79.45 (11.06) | 78.37 (10.77) | .001 | 78.24 (10.41) | 79.15 (11.09) | .017 |
| HR | 74.46 (24.56) | 74.91 (28.06) | 73.97 (20.01) | .201 | 73.04 (11.20) | 74.90 (27.35) | .031 |
| Treated/untreated HT | 2770 (61.5) | 1598 (67.7) | 1172 (54.6) | <.001 | 496 (47.1) | 2274 (65.9) | <.001 |
| HT status | |||||||
| Above target BP | 1494 (33.2) | 891 (37.7) | 603 (28.1) | <.001 | 233 (22.1) | 1261 (36.5) | <.001 |
| Within target BP | 543 (12.1) | 305 (12.9) | 238 (11.1) | 87 (8.3) | 456 (13.2) | ||
| Normal BP | 1736 (38.5) | 763 (32.3) | 973 (45.4) | 557 (52.9) | 1179 (34.1) | ||
| Untreated HT | 733 (16.3) | 402 (17.0) | 331 (15.4) | 176 (16.7) | 557 (16.1) | ||
| HT history | 2034 (45.1) | 1206 (51.1) | 828 (38.6) | <.001 | 318 (30.2) | 1716 (49.7) | <.001 |
| HT medications | 2037 (45.2) | 1196 (50.7) | 841 (39.2) | <.001 | 320 (30.4) | 1717 (49.7) | <.001 |
| Smoke | 927 (20.6) | 511 (21.6) | 416 (19.4) | .067 | 256 (24.3) | 671 (19.4) | .001 |
| BMI classification | |||||||
| Underweight | 55 (1.2) | 21 (0.9) | 34 (1.6) | <.001 | 18 (1.7) | 37 (1.1) | <.001 |
| Normal | 2076 (46.1) | 930 (39.4) | 1146 (53.4) | 548 (52.0) | 1528 (44.3) | ||
| Overweight | 1625 (36.1) | 927 (39.3) | 698 (32.5) | 356 (33.8) | 1269 (36.8) | ||
| Obese | 750 (16.6) | 483 (20.5) | 267 (12.4) | 131 (12.4) | 619 (17.9) | ||
| Family CVD history | 1679 (37.3) | 863 (36.6) | 816 (38.0) | .316 | 394 (37.4) | 1285 (37.2) | .934 |
| Diabetes | 533 (11.8) | 331 (14.0) | 202 (9.4) | <.001 | 95 (9.0) | 438 (12.7) | .002 |
| Hypercholesterolaemia | 1424 (31.6) | 808 (34.2) | 616 (28.7) | <.001 | 310 (29.4) | 1114 (32.3) | .092 |
| CVD/CKD | 448 (9.9) | 260 (11.0) | 188 (8.8) | .014 | 71 (6.7) | 377 (10.9) | <.001 |
| Physical activity 30′/day | 2026 (45.0) | 967 (41.0) | 1059 (49.4) | <.001 | 547 (51.9) | 1479 (42.8) | <.001 |
| Daily fruits/vegetables use | 3761 (83.5) | 1898 (80.4) | 1863 (86.9) | <.001 | 874 (83.0) | 2887 (83.6) | .677 |
| Unlimited salt use | 1189 (26.4) | 685 (29.0) | 504 (23.5) | <.001 | 249 (23.6) | 940 (27.2) | .024 |
| Daily brushing frequency | |||||||
| 1 | 602 (13.4) | 602 (25.5) | 0 (0.0) | <.001 | 79 (7.5) | 523 (15.1) | <.001 |
| 2 | 1759 (39.0) | 1759 (74.5) | 0 (0.0) | 367 (34.9) | 1392 (40.3) | ||
| ≥3 | 2145 (47.6) | 0 (0.0) | 2145 (100.0) | 607 (57.6) | 1538 (44.5) | ||
| Manual toothbrush | 3453 (76.6) | 1915 (81.1) | 1538 (71.7) | <.001 | 607 (57.6) | 1538 (44.5) | <.001 |
| Bleeding on brushing | 843 (18.7) | 473 (20.0) | 370 (17.2) | .019 | 218 (20.7) | 625 (18.1) | .064 |
| Periodontitis | 396 (8.8) | 230 (9.7) | 166 (7.7) | .02 | 105 (10.0) | 291 (8.4) | .137 |
Note: Data are presented as means ± SDs or numbers (percentages). Unpaired Student's t test and chi‐squared test were used to detect differences in quantitative (mean ± SD) and qualitative (N, %) data, respectively (statistical significance: p < .05).
Abbreviations: BMI, body mass index; BP, blood pressure; CKD, chronic kidney disease; CVD, cardiovascular diseases; DBP, diastolic blood pressure; HR, heart rate; HT, hypertension; SBP, systolic blood pressure.
3.2. Stratification based on home oral hygiene habits
Globally, individuals who brushed their teeth ≥3 times/day and electric toothbrush users were mostly young women with a globally healthy lifestyle and lower BP than their counterparts.
Specifically, individuals who reported brushing their teeth ≥3 times a day (N. 2145; 66.9% women; 57.2 ± 15.2 years) were more physically active, had a healthier eating style, and reported less frequent gum bleeding and periodontitis than their counterparts (Table 1). Their mean systolic and diastolic BP were 131.6 ± 18.6 mmHg (vs. 135.6 ± 18.6 mmHg; p < .001) and 78.4 ± 10.8 mmHg (vs. 79.4 ± 11.1 mmHg; p < .001), respectively. No difference in smoking habits was recorded based on daily toothbrush frequency (p = .67).
In parallel, electric toothbrush users (N. 1053; 53.7 ± 13.9 years; 64.2% women) were more often non‐smoker, physically active, lean individuals reporting a more controlled use of salt compared with non‐users (Table 1). Their mean BP was 129.0 ± 17.1/78.2 ± 10.4 mmHg (vs. 135.2 ± 18.9/79.1 ± 11.1 mmHg; p < .001). On average, 57.4% of electric toothbrush users reported brushing ≥3 times/day, compared with 44.5% of manual toothbrush users (p < .001). No difference in oral health status was reported based on toothbrushing type.
Globally, hypertension, diabetes mellitus, hypercholesterolaemia, and CVD/CKD were more common among those who reported manual toothbrushing or brushing less than three times/day than their counterparts.
A similar trend in clinical and demographic features was confirmed when stratification was made based on brushing frequency once, twice, or three or more times daily, with mean BP values progressively decreasing with the increase in toothbrush frequency (Table 2).
TABLE 2.
Stratification of participants according to brushing frequency
| Daily toothbrushing frequency | p‐Value | |||
|---|---|---|---|---|
| 1 | 2 | ≥3 | ||
| n | 602 | 1759 | 2145 | |
| Male | 370 (61.5) | 709 (40.3) | 709 (33.1) | <.001 |
| Age | 68.23 (77.67) | 60.40 (15.35) | 57.25 (15.21) | <.001 |
| BMI | 28.61 (16.88) | 26.97 (15.21) | 26.20 (25.06) | .037 |
| SBP | 140.01 (18.17) | 134.16 (18.50) | 131.63 (18.58) | <.001 |
| DBP | 80.49 (10.76) | 79.10 (11.14) | 78.37 (10.77) | <.001 |
| HR | 76.71 (51.49) | 74.29 (12.20) | 73.97 (20.01) | .05 |
| Treated/untreated HT | 457 (75.9) | 1141 (64.9) | 1172 (54.6) | <.001 |
| HT status | ||||
| Above target BP | 273 (45.3) | 618 (35.1) | 603 (28.1) | <.001 |
| Within target BP | 75 (12.5) | 230 (13.1) | 238 (11.1) | |
| Normal BP | 145 (24.1) | 618 (35.1) | 973 (45.4) | |
| Untreated HT | 109 (18.1) | 293 (16.7) | 331 (15.4) | |
| HT history | 355 (59.0) | 851 (48.4) | 828 (38.6) | <.001 |
| HT medications | 348 (57.8) | 848 (48.2) | 841 (39.2) | <.001 |
| Smoke | 133 (22.1) | 378 (21.5) | 416 (19.4) | .167 |
| BMI classification | ||||
| Underweight | 186 (30.9) | 744 (42.3) | 1146 (53.4) | <.001 |
| Normal | 161 (26.7) | 322 (18.3) | 267 (12.4) | |
| Overweight | 2 (0.3) | 19 (1.1) | 34 (1.6) | |
| Obese | 253 (42.0) | 674 (38.3) | 698 (32.5) | |
| Family CVD history | 206 (34.2) | 657 (37.4) | 816 (38.0) | .229 |
| Diabetes | 99 (16.4) | 232 (13.2) | 202 (9.4) | <.001 |
| Hypercholesterolaemia | 225 (37.4) | 583 (33.1) | 616 (28.7) | <.001 |
| CVD/CKD | 90 (15.0) | 170 (9.7) | 188 (8.8) | <.001 |
| Physical activity 30′/day | 224 (37.2) | 743 (42.2) | 1059 (49.4) | <.001 |
| Daily fruits/vegetables use | 472 (78.4) | 1426 (81.1) | 1863 (86.9) | <.001 |
| Unlimited salt use | 167 (27.7) | 518 (29.4) | 504 (23.5) | <.001 |
| Manual toothbrush | 523 (86.9) | 1392 (79.1) | 1538 (71.7) | <.001 |
| Bleeding on brushing | 150 (24.9) | 323 (18.4) | 370 (17.2) | <.001 |
| Periodontitis | 73 (12.1) | 157 (8.9) | 166 (7.7) | .003 |
Note: Nine participants declared no daily brushing (0.19%). Data are presented as means ± SDs or numbers (percentages). Unpaired Student's t test and chi‐squared test were used to detect differences in quantitative (mean ± SD) and qualitative (N, %) data, respectively (statistical significance: p < .05).
Abbreviations: BMI, body mass index; BP, blood pressure; CKD, chronic kidney disease; CVD, cardiovascular diseases; DBP, diastolic blood pressure; HR, heart rate; HT, hypertension; SBP, systolic blood pressure.
3.3. Association of toothbrushing frequency and electric toothbrushing with BP profile
Brushing ≥3 versus <3 times/day was associated with 26%–19% lower odds of prevalent/uncontrolled hypertension, based on the adjustments (bivariate OR: 0.74; 95% CI 0.65–0.86; multivariate OR: 0.81; 95% CI 0.70–0.94). Similarly, the use of the electric versus manual toothbrush was associated with 26% (bivariate OR: 0.74; 95% CI 0.65–0.86) to 28% (multivariate OR: 0.72; 95% CI 0.61–0.85) lower odds of the outcome.
The combined analysis of daily brushing frequency (≥ or <3 times/day) and toothbrush type (electric/manual) showed that mean systolic BP values progressively increased with the reduction of brushing frequency among electric toothbrush users (from 127.5 ± 16.4 mmHg to 131.1 ± 18.0 mmHg), and even more so among manual toothbrush users (from 133.3 ± 19.1 mmHg to 136.7 ± 18.6 mmHg) (Figure 1a). Multiple comparisons showed that electric toothbrush use three or more times on a daily basis was associated with lower mean systolic BP compared with all other home oral hygiene habits, by a magnitude spanning from −3.59 mmHg (vs. electric tooth brushing <3 times/day, p = .007) to −9.21 mmHg (vs. manual tooth brushing <3 times/day, p < .001). Intriguingly, manual brushing at least three times/day was not associated with improved mean systolic BP when compared with electric toothbrushing less than three times/day (p = .349) (Figure 1b). The multivariate model showed that, compared with manual toothbrushing less than three times/day, oral hygiene with the same modality at least three times per day was associated with lower odds of prevalent/uncontrolled hypertension by 17% (OR: 0.83, 95% CI 0.71–0.98, p = .031); electric tooth brushing under the same threshold was associated with 24% lower odds (OR: 0.76, 95% CI 0.60–0.97, p = .027); and electric brushing three times or more was associated with the largest reduction in the same odds, namely −43% (OR: 0.57, 95% CI 0.46–0.71, p < .001) (Figure 1c).
FIGURE 1.
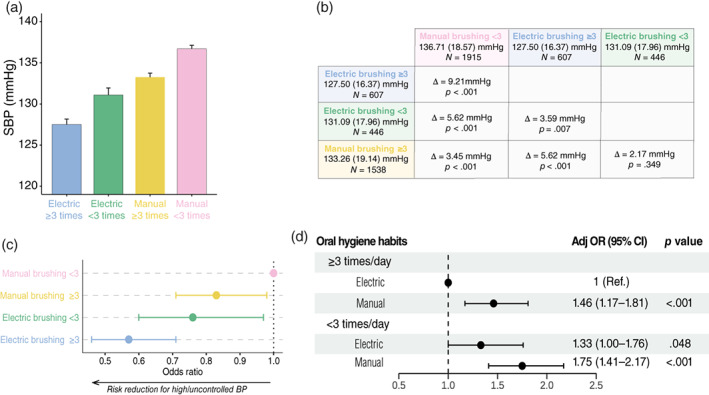
Home oral hygiene habits and blood pressure (BP) profiles. Estimated mean systolic BP (SBP) values based on combinations of brushing frequencies (less or more than three times/day) and modalities (electric or manual toothbrush) (a). Results of multiple pairwise comparisons of mean SBP values across the four strata using Wilcoxon rank test are shown. Bonferroni correction was applied as appropriate (b). Multivariate model (sex, age, BMI, current smoking, diabetes, hypercholesterolaemia, daily vegetable/fruit consumption, and physical activity) indicates that, compared with manual brushing less than three times per day, other combinations of brushing frequency and modality are associated with reduced odds of prevalent/uncontrolled hypertension with various extent (c). Adjusted interaction analysis was performed on the multivariate model using the same process described in Table 3. Forest plot indicates relative adjusted odds ratio (ORs) with 95% confidence interval (CI). Relative excess risk due to interaction: −0.02 (95% CI −0.47 to 0.43); attributable proportion: −0.01 (95% CI −0.25 to 0.23); synergy index: 0.98 (95% CI 0.59–1.61) (d). ***p < .001; **p < .01; *p < .05
When brushing frequency was stratified as once, twice, or three or more daily, mean systolic BP was significantly lower among manual toothbrush users exposed to toothbrushing twice and three times or more per day compared with once per day (Figure S2, Panel A). Among electric toothbrush users, mean systolic BP values were significantly lower among individuals exposed three or more times per day compared with once daily (Figure S2, Panel A). Manual brushing at least three times/day and using an electric toothbrush once or twice daily were associated with similar systolic BP profiles, while brushing three or more times per day with the electric device was associated with nearly 6 mmHg lower systolic BP compared with the same brushing frequency with the manual device (Figure S2, Panel B). Using manual toothbrushing once daily as reference, more frequent manual brushing, and any frequency of electric toothbrushing were associated with better systolic BP in parallel with the progressive increase in brushing frequency (Figure S2, Panel C). Accounting for gingival BoB in the models did not modify the results (data not shown).
3.4. Interaction between brushing frequency and toothbrush type
The joint effect of manual tooth brushing modality and less than three times/day brushing frequency on the odds of prevalent/uncontrolled hypertension is reported in Table 3 (crude results) and Figure 1 (adjusted results). No evidence of a significant joint effect of manual tooth brushing modality and less than three times/day brushing frequency on the outcome was observed.
TABLE 3.
Crude results of interaction analysis between daily toothbrushing (≥ or <3 times/day) and toothbrush type (manual/electric)
| Oral hygiene habits | Outcome | At risk | Crude prevalence rate (95% CI) | OR (95% CI) | p Value |
|---|---|---|---|---|---|
| ≥3 times/day | |||||
| Electric | 256 | 607 | 42.2 (38.2–46.2) | 1 (Ref.) | |
| Manual | 916 | 1538 | 59.6 (57.1–62.0) | 2.02 (1.67–2.44) | <.001 |
| <3 times/day | |||||
| Electric | 240 | 446 | 53.8 (49.1–58.5) | 1.60 (1.25–2.04) | <.001 |
| Manual | 1358 | 1915 | 70.9 (68.8–72.9) | 3.34 (2.77–4.04) | <.001 |
Note: The number of individuals with prevalent/uncontrolled hypertension (outcome) across strata and the crude prevalence rate are reported. The combination of the exposures associated with the lowest prevalence rate of the outcome (i.e., brushing teeth ≥3 times/day × electric toothbrush) was set as the reference. Relative excess risk due to interaction (RERI), proportion of disease among those with both exposures that is attributable to their interaction (AP), and the synergy index (SI) were calculated. RERI: 0.73 (95% CI 0.2–1.22); AP: 0.22 (95% CI 0.06–0.35); SI: 1.45 (95% CI 1.08–1.95). See Figure 1, Panel D for adjusted results.
Abbreviations: CI, confidence interval; OR, odds ratio.
4. DISCUSSION
The results of this nationwide, real‐world, opportunistic survey indicate that home oral hygiene habits, in terms of tooth brushing frequency and modality, are inversely associated with BP profile independent of some confounders, namely sex, age, BMI, smoking and diet habits, physical activity, and history of diabetes and hypercholesterolaemia. Specifically, brushing at least three times/day and electric toothbrushing were associated with lower odds of having prevalent/uncontrolled hypertension by at least 19% and 28%, respectively, compared with less frequent brushing and with manual toothbrushing. The combination associated with the best BP profile was that of electric toothbrushing at least three times on a daily basis. Interestingly, we found that manual brushing at least three times/day and using an electric toothbrush less than the same threshold were associated with similar systolic BP profiles.
These findings provide the first evidence of the association between home oral hygiene habits and BP, and expand previous observational evidence on the association between periodontal health status and BP profile (Pietropaoli et al., 2018; Pietropaoli, Del Pinto, et al., 2020), while also adding to recent evidence linking oral health habits with cardiovascular health (Park et al., 2019; Del Pinto, Monaco, et al., 2021; Hwang et al., 2022). In fact, cross‐sectional evidence from the Korea National Health and Nutrition Examination Survey (KNHANES) 2008–2010 showed that the adjusted prevalence of hypertension decreased as the frequency of toothbrushing increased, but the impact of toothbrushing modality was only assessed in combination with the use of other oral products (Choi et al., 2015). In addition, an analysis of 247,696 healthy adults (≥40 years) without history of major cardiovascular events undergoing an oral health screening programme (median follow‐up: 9.5 years) showed that each unit increase in daily tooth brushing frequency was associated with a 9% reduction in the risk of cardiovascular events (myocardial infarction, stroke, heart failure, and cardiovascular death) (Park et al., 2019). This benefit was further amplified in combination with regular professional dental hygiene interventions. However, home oral hygiene modalities were not explored. More recently, a study has assessed the association of tooth brushing frequency with incident hypertension in middle‐aged and older Korean adults, reporting a 15% reduced risk of the outcome among individuals who brushed their teeth at least three times/day, but the modality of brushing (electric/manual) was not assessed (Hwang et al., 2022). In parallel, an analysis of 2350 propensity‐matched, highly educated, high‐income adults from the National Health and Nutrition Examination Survey (NHANES) found that regular access to dental care impacts on BP profiles independent of socio‐economic confounders, with reduced risk of high/uncontrolled BP in association with attendance ≤6 months compared with attendance >6 months (Del Pinto, Monaco, et al., 2021). From a biological standpoint, nearly 7% of the effect of accessing dental care on BP was mediated by low‐grade systemic inflammation.
With an estimated 36 h/year devoted to home oral care, against the estimated 2 h/year spent in professional oral hygiene, the contribution of home oral hygiene habits to local and global health might be proportionally relevant (Del Pinto, Monaco, et al., 2021). The possible mechanisms behind the systemic benefit of home oral care practices include their modulating effects on the local microbiota and the immune system, two emerging factors in CVD pathogenesis (Del Pinto, Pietropaoli, et al., 2020; Pietropaoli, Del Pinto, et al., 2020; Del Pinto, Landi, et al., 2021b). In fact, periodontal bacteria appear to elicit a hypertension‐specific immune host response (Pietropaoli et al., 2019), and periodontal treatment was found to have a significant modulatory effect on adaptive immunity (Czesnikiewicz‐Guzik et al., 2019) and BP (Sharma et al., 2021). In parallel, those bacteria that are considered causative of periodontal disease were found to be positively associated with both BP and prevalent hypertension in the Oral Infections and Vascular Disease Epidemiology Study (INVEST) (Desvarieux et al., 2010). Thus, regular home oral care might represent an additional, non‐pharmacological strategy for cardiovascular prevention, possibly through dysbiosis reversal and consequent systemic anti‐inflammatory effects.
Beyond the main scope of this study, we also observed a low rate of self‐reported periodontitis in the examined population (8.8%). Since national epidemiological estimates set at about 40% the prevalence of moderate/severe periodontitis (Aimetti et al., 2015), it could be argued that participants in this survey possibly had low awareness of their periodontal health status. At the same time, it is interesting to note that gingival BoB was indeed quite often reported (18.7%), suggesting greater awareness with reference to this sign and supporting its use as an indicator of self‐reported periodontal health status at the population level, as recently proposed (Tonetti et al., 2020; Deng et al., 2021).
This study has limitations and strengths. As an analysis of observational, cross‐sectional data, any causal inference is prevented. A certain degree of selection bias, as well as the use of self‐reported data, need consideration when interpreting the relative results and might limit their generalizability. In parallel, the use of dental floss, mouthwash, and inter‐dental brush, as well as dental office attendance habits, were not assessed in the survey. Similarly, clinical information on pocket depth, attachment loss, number of teeth, and oral hygiene level was not collected. The survey was not designed to detect conditions like white‐coat hypertension and masked hypertension. Information on antihypertensive medications type and doses, compliance with treatment, and on concomitant conditions with possible impact on BP control (Del Pinto et al., 2018; Del Pinto, Wright, et al., 2020) was not available. Similarly, indicators of socio‐economic status were not collected in the survey and could therefore not be accounted for their potential confounding role; it must be noted, however, that recent evidence indicates that the association of periodontal health status with BP is preserved among high‐income, highly educated individuals (Del Pinto, Monaco, et al., 2021). Considering the above, the odds ratios reported in this study are an overestimation of the true association between toothbrushing and hypertension. On the other hand, to the best of the authors' knowledge, this study is the first to examine the association of home oral care habits in terms of both frequency and modality of toothbrushing with hypertension. The survey was conducted nationwide on a large sample of non‐institutionalized Italian adults. BP was measured with a standardized protocol based on the use of automated devices. Data were tested with multiple adjustments accounting for major possible confounders in the examined association.
5. CONCLUSIONS
This nationwide, real‐world survey on a large sample of the non‐institutionalized Italian population shows an association between home oral care habits and hypertension, providing the first evidence that electric toothbrushing and frequent daily brushing are associated with a better BP profile, even more so when such modalities are combined. Future interdisciplinary research is warranted to test whether home oral hygiene may represent a cost‐effective, complementary approach to the management of hypertension.
AUTHOR CONTRIBUTIONS
Rita Del Pinto conceived the study. Federfarma, here represented by Marco Cossolo and Alfredo Procaccini, collected the data. Rita Del Pinto and Davide Pietropaoli analysed the data, interpreted the results, and wrote the first draft. Rita Del Pinto edited the manuscript. Claudio Ferri, Guido Grassi, Maria Lorenza Muiesan, and Annalisa Monaco provided critical guidance throughout the manuscript drafting. All the authors have read and approved the final version of the manuscript.
FUNDING INFORMATION
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: the authors acknowledge the 2020 grant to RDP by Federfarma and the Italian Society of Hypertension.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
ETHICS STATEMENT
The present study was approved by local IRB (protocol No. 36/2020). The survey was conducted in conformity with the Helsinki Declaration. The study followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.
Supporting information
Table S1. Stratification of participants according to brushing frequency. Nine participants declared no daily brushing (0.19%).
Figure S1. With 17,980 affiliate pharmacies in the Federfarma network in 2020, the campaign acceptance rate was 4.1%. Geographical distribution of recruitment sites and numbers of attending volunteers for each pharmacy are presented in panel A. Based on 2020 population data, the median attendance rate across Italian regions was 5.45 per 100,000 inhabitants (range: 1.8–25.5 per 100,000). No difference in attendance rate was observed across Italian regions (panel B).
Figure S2. Threshold effect for brushing frequency. Mean systolic BP according to daily brushing frequency stratified for electric and manual devices (A). Results of multiple pairwise comparisons (Wilcoxon rank test) of mean systolic BP values across strata are shown (A). Bonferroni correction was applied as appropriate (B). Estimates of the full adjusted generalized linear model sbp ~ OralHabitsTimes + Age + Gender + Diabetes + Smoke + Hypercholesterolemia + BMI + Veg_Fruits_Every_Day + PhysicalActivity30min (C).
ACKNOWLEDGEMENTS
The authors acknowledge the work of all the pharmacists who collected the data during the campaign, and the contribution of Corman®, Omron®, and Cittadinanzattiva. The authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation. RDP is a Young Investigator of the Italian Society of Hypertension. GG is President of the Italian Society of Hypertension. MLM is Vice‐President of the Italian Society of Hypertension. CF is Past‐President of the Italian Society of Hypertension. MC is President of Federfarma. Open Access Funding provided by Universita degli Studi dell'Aquila within the CRUI‐CARE Agreement. [Correction added on 23 November 2022, after first online publication: CRUI funding statement has been added.]
APPENDIX A.
Members of the Italian Society of Hypertension Board: Prof. Guido Grassi, Prof. Claudio Ferri, Prof. Maria Lorenza Muiesan, Prof. Massimo Salvetti, Prof. Leonardo Sechi, Prof. Arrigo FG Cicero, Prof. Guido Iaccarino, Prof. Pietro Minuz, Prof. Paolo Mulatero, Prof. Giuseppe Mulè, Dr. Giacomo Pucci, Prof. Carmine Savoia, Prof. Claudio Borghi, and Prof. Massimo Volpe.
Del Pinto, R. , Pietropaoli, D. , Grassi, G. , Muiesan, M. L. , Monaco, A. , Cossolo, M. , Procaccini, A. , & Ferri, C. (2022). Home oral hygiene is associated with blood pressure profiles: Results of a nationwide survey in Italian pharmacies. Journal of Clinical Periodontology, 49(12), 1234–1243. 10.1111/jcpe.13720
Members of the Italian Society of Hypertension Board are provided in Appendix.
Funding information Italian Society of Hypertension; Federfarma
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Aimetti, M. , Perotto, S. , Castiglione, A. , Mariani, G. M. , Ferrarotti, F. , & Romano, F. (2015). Prevalence of periodontitis in an adult population from an urban area in north Italy: Findings from a cross‐sectional population‐based epidemiological survey. Journal of Clinical Periodontology, 42(7), 622–631. [DOI] [PubMed] [Google Scholar]
- Alli, B. Y. (2021). InteractionR: An R package for full reporting of effect modification and interaction. Software Impacts, 10, 100147. [Google Scholar]
- Beaney, T. , Burrell, L. M. , Castillo, R. R. , Charchar, F. J. , Cro, S. , Damasceno, A. , Kruger, R. , Nilsson, P. M. , Prabhakaran, D. , Ramirez, A. J. , Schlaich, M. P. , Schutte, A. E. , Tomaszewski, M. , Touyz, R. , Wang, J.‐G. , Weber, M. A. , Poulter, N. R. , & MMM Investigators . (2019). May measurement month 2018: A pragmatic global screening campaign to raise awareness of blood pressure by the International Society of Hypertension. European Heart Journal, 40(25), 2006–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, H. M. , Han, K. , Park, Y.‐G. , & Park, J.‐B. (2015). Associations among oral hygiene behavior and hypertension prevalence and control: The 2008 to 2010 Korea National Health and Nutrition Examination Survey. Journal of Periodontology, 86(7), 866–873. [DOI] [PubMed] [Google Scholar]
- Czesnikiewicz‐Guzik, M. , Osmenda, G. , Siedlinski, M. , Nosalski, R. , Pelka, P. , Nowakowski, D. , Wilk, G. , Mikolajczyk, T. P. , Schramm‐Luc, A. , Furtak, A. , Matusik, P. , Koziol, J. , Drozdz, M. , Munoz‐Aguilera, E. , Tomaszewski, M. , Evangelou, E. , Caulfield, M. , Grodzicki, T. , D'Aiuto, F. , & Guzik, T. J. (2019). Causal association between periodontitis and hypertension: Evidence from Mendelian randomization and a randomized controlled trial of non‐surgical periodontal therapy. European Heart Journal, 40(42), 3459–3470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jager, D. J. , de Mutsert, R. , Jager, K. J. , Zoccali, C. , & Dekker, F. W. (2011). Reporting of interaction. Nephron. Clinical Practice, 119(2), c158–c161. [DOI] [PubMed] [Google Scholar]
- Del Pinto, R. , Landi, L. , Grassi, G. , Sforza, N. M. , Cairo, F. , Citterio, F. , Paolantoni, G. , D'Aiuto, F. , Ferri, C. , Monaco, A. , Pietropaoli, D. , & Italian working group on Hypertension, Periodontitis (Hy‐Per Group) . (2021a). Hypertension and periodontitis: A joint report by the Italian Society of Hypertension (SIIA) and the Italian Society of Periodontology and Implantology (SIdP). Oral Diseases. 10.1111/odi.14009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Pinto, R. , Landi, L. , Grassi, G. , Sforza, N. M. , Cairo, F. , Citterio, F. , Paolantoni, G. , D'Aiuto, F. , Ferri, C. , Monaco, A. , Pietropaoli, D. , & Italian working group on Hypertension, Periodontitis (Hy‐Per Group) . (2021b). Hypertension and periodontitis: A joint report by the Italian Society of Hypertension (SIIA) and the Italian Society of Periodontology and Implantology (SIdP). High Blood Pressure & Cardiovascular Prevention: The Official Journal of the Italian Society of Hypertension, 28(5), 427–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Pinto, R. , Monaco, A. , Ortu, E. , Czesnikiewicz‐Guzik, M. , Aguilera, E. M. , Giannoni, M. , D'Aiuto, F. , Guzik, T. J. , Ferri, C. , & Pietropaoli, D. (2021). Access to dental care and blood pressure profiles in adults with high socioeconomic status. Journal of Periodontology, 93(7), 1060–1071. 10.1002/JPER.21-0439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Pinto, R. , Pagliacci, S. , De Feo, M. , Grassi, D. , Ferri, C. , & Italian Society of Hypertension and Federfarma . (2020). Prevalence of hypertension and associated cardiovascular risk factors among pharmacies customers: An Italian Nationwide Epidemiological Survey. European Journal of Preventive Cardiology, 27(11), 1228–1230. [DOI] [PubMed] [Google Scholar]
- Del Pinto, R. , Pietropaoli, D. , & Ferri, C. (2018). Diastolic blood pressure and risk profile in renal and cardiovascular diseases. Results from the SPRINT trial. Journal of the American Society of Hypertension, 12(7), 513–23.e3. [DOI] [PubMed] [Google Scholar]
- Del Pinto, R. , Pietropaoli, D. , Munoz‐Aguilera, E. , D'Aiuto, F. , Czesnikiewicz‐Guzik, M. , Monaco, A. , Guzik, T. J. , & Ferri, C. (2020). Periodontitis and hypertension: Is the association causal? High Blood Pressure & Cardiovascular Prevention: The Official Journal of the Italian Society of Hypertension, 27(4), 281–289. [DOI] [PubMed] [Google Scholar]
- Del Pinto, R. , Wright, J. T. , Monaco, A. , Pietropaoli, D. , & Ferri, C. (2020). Vitamin D and blood pressure control among hypertensive adults: Results from NHANES 2001–2014. Journal of Hypertension, 38(1), 150–158. [DOI] [PubMed] [Google Scholar]
- Deng, K. , Pelekos, G. , Jin, L. , & Tonetti, M. S. (2021). Gingival bleeding on brushing as a sentinel sign of gingival inflammation: A diagnostic accuracy trial for the discrimination of periodontal health and disease. Journal of Clinical Periodontology, 48(12), 1537–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desvarieux, M. , Demmer, R. T. , Jacobs, D. R., Jr. , Rundek, T. , Boden‐Albala, B. , Sacco, R. L. , & Papapanou, P. N. (2010). Periodontal bacteria and hypertension: The oral infections and vascular disease epidemiology study (INVEST). Journal of Hypertension, 28(7), 1413–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang, S.‐Y. , Oh, H. , Rhee, M.‐Y. , Kang, S. , & Kim, H.‐Y. (2022). Association of periodontitis, missing teeth, and oral hygiene behaviors with the incidence of hypertension in middle‐aged and older adults in Korea: A 10‐year follow‐up study. Journal of Periodontology. 10.1002/JPER.21-0706 [DOI] [PubMed] [Google Scholar]
- Landi, L. , Grassi, G. , Sforza, N. M. , Ferri, C. , & Italian working group on Hypertension and Periodontitis (Hy‐Per Group) . (2021). Hypertension and periodontitis: An upcoming joint report by the Italian Society of Hypertension (SIIA) and the Italian Society of Periodontology and Implantology (SIdP). High Blood Pressure & Cardiovascular Prevention: The Official Journal of the Italian Society of Hypertension, 28(1), 1–3. [DOI] [PubMed] [Google Scholar]
- Park, S.‐Y. , Kim, S.‐H. , Kang, S.‐H. , Yoon, C.‐H. , Lee, H.‐J. , Yun, P.‐Y. , Youn, T.‐J. , & Chae, I.‐H. (2019). Improved oral hygiene care attenuates the cardiovascular risk of oral health disease: A population‐based study from Korea. European Heart Journal, 40(14), 1138–1145. [DOI] [PubMed] [Google Scholar]
- Piepoli, M. F. , Hoes, A. W. , Agewall, S. , Albus, C. , Brotons, C. , Catapano, A. L. , Cooney, M.‐T. , Corrà, U. , Cosyns, B. , Deaton, C. , Graham, I. , Hall, M. S. , Hobbs, F. D. R. , Løchen, M.‐L. , Löllgen, H. , Marques‐Vidal, P. , Perk, J. , Prescott, E. , Redon, J. , … ESC Scientific Document Group . (2016). 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by Representatives of 10 Societies and by Invited experts)Developed with the Special Contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). European Heart Journal, 37(29), 2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietropaoli, D. , Del Pinto, R. , Ferri, C. , Marzo, G. , Giannoni, M. , Ortu, E. , & Monaco, A. (2020). Association between periodontal inflammation and hypertension using periodontal inflamed surface area and bleeding on probing. Journal of Clinical Periodontology, 47(2), 160–172. [DOI] [PubMed] [Google Scholar]
- Pietropaoli, D. , Del Pinto, R. , Ferri, C. , Ortu, E. , & Monaco, A. (2019). Definition of hypertension‐associated oral pathogens in NHANES. Journal of Periodontology, 90(8), 866–876. [DOI] [PubMed] [Google Scholar]
- Pietropaoli, D. , Del Pinto, R. , Ferri, C. , Wright, J. T., Jr. , Giannoni, M. , Ortu, E. , & Monaco, A. (2018). Poor oral health and blood pressure control among US hypertensive adults. Hypertension, 72(6), 1365–1373. [DOI] [PubMed] [Google Scholar]
- Pietropaoli, D. , Monaco, A. , D'Aiuto, F. , Aguilera, E. M. , Ortu, E. , Giannoni, M. , Czesnikiewicz‐Guzik, M. , Guzik, T. J. , Ferri, C. , & Del Pinto, R. (2020). Active gingival inflammation is linked to hypertension. Journal of Hypertension, 38(10), 2018–2027. 10.1097/HJH.0000000000002514 [DOI] [PubMed] [Google Scholar]
- Sharma, S. , Sridhar, S. , McIntosh, A. , Messow, C.‐M. , Aguilera, E. M. , Del Pinto, R. , Pietropaoli, D. , Gorska, R. , Siedlinski, M. , Maffia, P. , Tomaszewski, M. , Guzik, T. J. , D'Aiuto, F. , & Czesnikiewicz‐Guzik, M. (2021). Periodontal therapy and treatment of hypertension‐alternative to the pharmacological approach. A systematic review and meta‐analysis. Pharmacological Research, 166, 105511. [DOI] [PubMed] [Google Scholar]
- Skrondal, A. (2003). Interaction as departure from additivity in case‐control studies: A cautionary note. American Journal of Epidemiology, 158(3), 251–258. [DOI] [PubMed] [Google Scholar]
- Tonetti, M. S. , Deng, K. , Christiansen, A. , Bogetti, K. , Nicora, C. , Thurnay, S. , & Cortellini, P. (2020). Self‐reported bleeding on brushing as a predictor of bleeding on probing: Early observations from the deployment of an internet of things network of intelligent power‐driven toothbrushes in a supportive periodontal care population. Journal of Clinical Periodontology, 47(10), 1219–1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virani, S. S. , Alonso, A. , Benjamin, E. J. , Bittencourt, M. S. , Callaway, C. W. , Carson, A. P. , Chamberlain, A. M. , Chang, A. R. , Cheng, S. , Delling, F. N. , Djousse, L. , Elkind, M. S. V. , Ferguson, J. F. , Fornage, M. , Khan, S. S. , Kissela, B. M. , Knutson, K. L. , Kwan, T. W. , Lackland, D. T. , … American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . (2020). Heart disease and stroke statistics‐2020 update: A report From the American Heart Association. Circulation, 141(9), e139–e596. [DOI] [PubMed] [Google Scholar]
- Williams, B. , Mancia, G. , Spiering, W. , Rosei, E. A. , Azizi, M. , Burnier, M. , Clement, D. L. , Coca, A. , de Simone, G. , Dominiczak, A. , Kahan, T. , Mahfoud, F. , Redon, J. , Ruilope, L. , Zanchetti, A. , Kerins, M. , Kjeldsen, S. E. , Kreutz, R. , Laurent, S. , … ESC Scientific Document Group . (2018). 2018 ESC/ESH guidelines for the management of arterial hypertension. European Heart Journal, 39(33), 3021–3104. [DOI] [PubMed] [Google Scholar]
- Zou, G. Y. (2008). On the estimation of additive interaction by use of the four‐by‐two table and beyond. American Journal of Epidemiology, 168(2), 212–224. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Stratification of participants according to brushing frequency. Nine participants declared no daily brushing (0.19%).
Figure S1. With 17,980 affiliate pharmacies in the Federfarma network in 2020, the campaign acceptance rate was 4.1%. Geographical distribution of recruitment sites and numbers of attending volunteers for each pharmacy are presented in panel A. Based on 2020 population data, the median attendance rate across Italian regions was 5.45 per 100,000 inhabitants (range: 1.8–25.5 per 100,000). No difference in attendance rate was observed across Italian regions (panel B).
Figure S2. Threshold effect for brushing frequency. Mean systolic BP according to daily brushing frequency stratified for electric and manual devices (A). Results of multiple pairwise comparisons (Wilcoxon rank test) of mean systolic BP values across strata are shown (A). Bonferroni correction was applied as appropriate (B). Estimates of the full adjusted generalized linear model sbp ~ OralHabitsTimes + Age + Gender + Diabetes + Smoke + Hypercholesterolemia + BMI + Veg_Fruits_Every_Day + PhysicalActivity30min (C).
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


