Abstract
Aims
Racial and ethnic disparities exist in gestational diabetes prevalence and risk of subsequent type 2 diabetes mellitus (T2DM). Postpartum engagement in healthy behaviours is recommended for prevention and early detection of T2DM, yet uptake is low among women from diverse cultural backgrounds. Greater understanding of factors impacting postpartum health behaviours is needed. Applying the Theoretical Domains Framework (TDF) and Capability, Opportunity, Motivation‐Behaviour (COM‐B) model, our aim was to synthesise barriers to and enablers of postpartum health behaviours among women from diverse cultural backgrounds with prior GDM and identify relevant intervention components.
Methods
Databases, reference lists and grey literature were searched from September 2017 to April 2021. Two reviewers screened articles independently against inclusion criteria and extracted data. Using an inductive–deductive model, themes were mapped to the TDF and COM‐B model.
Results
After screening 5148 citations and 139 full texts, we included 35 studies (N = 787 participants). The main ethnicities included Asian (43%), Indigenous (15%) and African (11%). Barriers and enablers focused on Capability (e.g. knowledge), Opportunity (e.g. competing demands, social support from family, friends and healthcare professionals, culturally appropriate education and resources) and Motivation (e.g. negative emotions, perceived consequences and necessity of health behaviours, social/cultural identity). Five relevant intervention functions are identified to link the barriers and enablers to evidence‐based recommendations for communications to support behaviour change.
Conclusions
We provide a conceptual model to inform recommendations regarding the development of messaging and interventions to support women from diverse cultural backgrounds in engaging in healthy behaviours to reduce risk of T2DM.
Keywords: behaviour change; diabetes mellitus, type 2; diabetes, gestational; interventions; lifestyle behaviours; novelty statement; review; screening
What is already known?
Following gestational diabetes, women find it challenging to engage in healthy behaviours.
Some population groups, such as Asian/Pacific Islander, Hispanic/Latina and Indigenous Peoples (1 are at high risk of type 2 diabetes warranting targeted intervention.
Previous recommendations have not specifically addressed these priority populations.
What this study has found?
Culturally specific barriers included lack of culturally appropriate education, cultural beliefs, lack of social support, cultural identity, negative emotions, placing needs above family and unsafe environments.
Enablers included social support, family history of diabetes, beliefs about positive influences of health behaviours, proactive behaviours and role modelling.
What are the implications of the study?
Guided by a behaviour change framework, we suggest a conceptual model to inform culturally appropriate messaging which should be incorporated into continuing professional development.
1. INTRODUCTION
Gestational diabetes mellitus (GDM), defined as glucose intolerance that is first diagnosed in pregnancy 1 , 2 affects about one in six live births worldwide. 3 Often perceived as a short‐term condition, evidence indicates long‐term consequences for women and their children. 2 The most significant risk is progression to type 2 diabetes mellitus (T2DM). Women with a history of GDM are 8–10 times more likely to develop T2DM than women without GDM with relative risk highest during the first 3–6 years postpartum, 4 , 5 highlighting the need for effective postpartum intervention. 3
Some ethnic groups have greater risk. Women from Asian/Pacific Islands, Hispanic/Latina backgrounds and Indigenous peoples have been identified as having higher rates of GDM 6 , 7 , 8 , 9 with a social gradient particularly apparent among older women. 10 There is also increased progression to T2DM. A meta‐analysis of women globally shows future risk for T2DM of 1.49 for those of non‐white ethnicity. 11 Indigenous women in Canada and Australia had substantially more subsequent T2DM than non‐Indigenous women, partially due to socio‐economic and environmental barriers. 12 , 13 Australian population data showed higher prevalence odds of T2DM in nearly all migrant groups (male and female) compared with the Australian‐born population with those experiencing the most disadvantage having the highest prevalence. 14 These socio‐cultural disparities have implications for preventive efforts when targeting those most at risk.
Many risk factors are potentially modifiable and the onset of T2DM can be significantly delayed or prevented. 15 , 16 In women with prior GDM, postpartum weight retention (PPWR) is an independent risk factor for future diabetes. 17 , 18 Weight loss of ≥2 kg during the postpartum period is associated with significant improvement in glucose metabolism at the 1‐year postpartum period. 18 Importantly, studies have associated South Asian, Middle Eastern and African ethnicity with PPWR. 19 In the Diabetes Prevention Program Outcomes Study, intensive lifestyle interventions to reinforce weight loss and physical activity goals reduced progression to T2DM over 10 years in women (mixed ethnicities) with prior GDM by 35%. 20 However, there is a lack of evidence for effective interventions in the more immediate postpartum stage where challenges may be different and for culturally diverse relevant interventions. 21 International guidelines 22 , 23 recommend T2DM screening, breastfeeding and healthy postpartum behaviours, such as weight management, healthy eating and physical activity. However, uptake of T2DM screening remains low across multiple countries, 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 particularly for immigrant groups, 29 and few women undertake sufficient lifestyle behaviours to decrease future risks. 32 , 33 , 34
Recent reviews have identified barriers to and enablers of postpartum healthy behaviours 35 and T2DM screening 36 , 37 in women with prior GDM in general populations. Modifiable person‐level factors included prioritising children, social support and knowledge regarding health behaviours. Modifiable practice‐level factors included clinicians' information provision and accurate risk communication. Policy‐level factors included screening type and requirements and reminder systems. 35 , 36 , 37 While recommendations from these reviews recognise the need for culturally relevant information, no specific guidelines have been made.
A person's beliefs, attitudes and behaviour may become attuned to, and supportive of, the demands in the cultural system. 38 While migrant women may have similar access to health services as other women, in practice, access can be challenging and their needs may be different due to factors such as adapting to a new culture, insufficient support, discrimination, racism, cultural and social beliefs, mental health issues and lack of culturally specific information. 35 , 39 , 40 Understanding personal‐level factors in women from diverse backgrounds is important and under‐recognised with overrepresentation of WEIRD (White, Educated, Industrialised, Rich, Democratic) populations in prior studies. 41
Progressing from identifying barriers and enablers to interventions aimed at increasing engagement with postpartum health behaviours requires grounding in behaviour change theory to ensure effectiveness. 42 The Theoretical Domains Framework (TDF) comprises 14 domains synthesised from 33 behaviour change theories. 43 , 44 The domains are an expansion of the three core components: Capability, Opportunity and Motivation in the Capability, Opportunity, Motivation and Behaviour (COM‐B) model. 44 , 45 Both TDF and COM‐B form the hub of the Behaviour Change Wheel (Figure 1), a comprehensive tool to guide intervention development. 45 Mapping barriers and enablers onto the TDF and COM‐B model enables systematic identification of intervention functions that can inform development of theoretically grounded recommendations.
FIGURE 1.
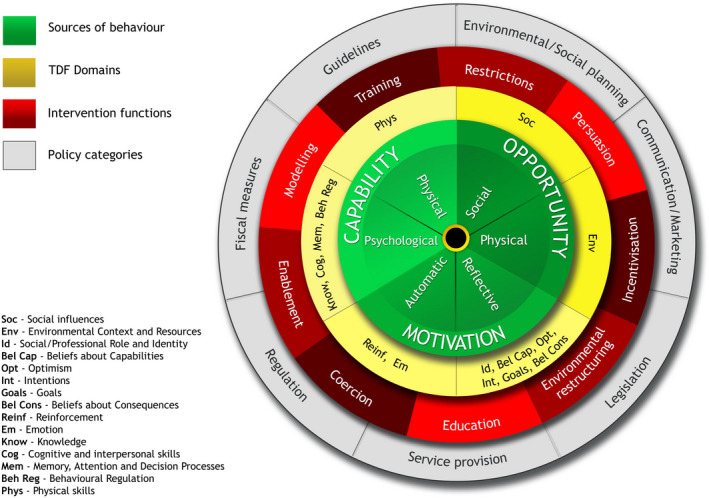
COM‐B model (reproduced with permission).
Our team recently published a review of personal‐level factors impacting T2DM screening among women with prior GDM. 46 To date, no attempt has been made to synthesise literature on the perspectives of women from diverse cultural backgrounds. The current review extends Dennison's systematic reviews 35 , 36 of postpartum healthy behaviours and recommendation to ensure that intervention material is culturally appropriate. Thus, our primary aim was to identify personal‐level factors impacting postpartum health behaviours and engagement in T2DM screening among women from diverse cultural backgrounds with prior GDM. Using contemporary behaviour change frameworks, our secondary aim was to develop a conceptual model to inform the design and implementation of personal‐level messaging tailored to this priority population.
2. METHODS
Our protocol was registered on PROSPERO (CRD42020164855). 47 One research question outlined in the protocol has been addressed in a previous systematic review. 46 The current review is reported according to ENTREQ and PRISMA statements (S1).
2.1. Search strategy
The search strategy by Dennison et al 35 , 36 was duplicated to identify studies from September 2017 (end date of Dennison's search) to April 2021. We searched MEDLINE, CINAHL, Embase, PsycINFO, the Cochrane Library electronic databases, grey literature databases (OpenGrey, PsychEXTRA), published abstracts from leading diabetes conferences (2018–2021), and conducted a Google advanced search (S2). Bibliographies were also screened. The 31 studies reviewed by Dennison et al., 35 , 36 were considered for inclusion.
2.2. Study selection
We included qualitative studies or qualitative data from mixed method studies reporting on factors impacting engagement with postpartum health behaviours among women from diverse cultural backgrounds with prior GDM. We excluded studies with a White sample only or with a mixed sample without ethnicity details to ensure data extracted were specific to women from diverse cultural backgrounds. There were no restrictions on language, country or date. Non‐primary studies (e.g. systematic reviews), studies reporting on effectiveness of interventions, women's experience with interventions and experiences of healthcare professionals were excluded.
Using Endnote, two reviewers (AN and AL) independently screened eligible studies against the eligibility criteria. Queries were resolved in consultation with co‐authors.
2.3. Terminology
Here, ‘women from diverse cultural backgrounds’ refers to women of colour/non‐white women, women born in non‐English speaking countries and/or who do not speak the National language of their country of residence at home, migrants and Indigenous peoples. Culturally responsive care refers to ‘the capacity of clinicians to provide care that is respectful of, and relevant to, the health beliefs, health practices, cultural and linguistic needs of diverse patient populations and communities. It describes the capacity to respond to the healthcare issues of different communities’. 48 Culturally competent care is often used in the context of providing healthcare to Indigenous peoples. It is ‘… a set of congruent behaviours, attitudes, and policies that come together in a system, agency, or amongst professionals and enables that system, agency, or those professionals to work effectively in cross‐cultural situations’. 49 Cultural safety, more broadly, recognises the systemic issues that contribute to ‘the barriers to clinical effectiveness arising from the inherent power imbalance between provider and patient’. 50 Cultural humility is defined as ‘the life‐long process of self‐exploration and self‐critique with a willingness to learn from others. It promotes interpersonal sensitivity and openness, addresses power imbalances, and develops an appreciation of intracultural variation and individuality to avoid stereotyping and have a more other‐oriented perspective’. 51
2.4. Quality assessment and confidence in synthesis findings
Studies were assessed using the Critical Appraisal Skills Programme (CASP) Qualitative Checklist. 52 This study tool consists of 10 questions aiming to critique internal validity, results and relevance of healthcare evidence. We developed additional criteria for checklist items that were more stringent than the original prompts, which if fulfilled were assessed as a ‘Yes’ response option. The ‘No’ response option was assigned where the criteria were not fulfilled, and ‘Unclear’ where reporting was inadequate. A pragmatic approach was used to determine overall study quality with consideration of elements deemed important in the context of this review. 53 For example, rigour of data analysis was weighted highly. Three reviewers (A.N., A.L. and A.W.) piloted assessment, independently assessing 10% of papers. Three reviewers (A.L., A.W. and A.M.) subsequently assessed the remaining studies independently, reaching agreement about study strengths and limitations by consensus. Two reviewers (A.N. and A.W.) used the Grades of Recommendation, Assessment, Development and Evaluation‐Confidence in the Evidence from Qualitative Reviews (GRADE‐CERQual) approach 54 to assess confidence in synthesised qualitative findings. It assesses four components: (1) methodological limitations, (2) coherence, (3) adequacy of data and (4) relevance (S3). 54
2.5. Qualitative synthesis
2.5.1. Data extraction
Using excel, we extracted author, year, country, sample size, ethnicity, study objectives, recruitment and data collection method (S4) and data containing first‐order (participant quotations) and second‐order (author interpretations and themes) constructs relating to postpartum health behaviours. 55 Data were extracted by two reviewers (H.N. and A.W.) after three reviewers (A.L., A.W. and H.N.) independently piloted data extraction from 10% of papers. Authors were contacted for more detail about ethnicity of participants where required. Using Excel, the units were categorised as first‐order qualitative constructs (participant quotations) and second‐order interpretations (author interpretations and themes).
2.5.2. Development of coding manual
We used an iterative inductive–deductive coding approach to avoid rigid operationalisation of TDF constructs. 56 Inductive coding was undertaken by three reviewers (A.N., A.L. and A.W.) who generated themes and subthemes for similar response clusters. We developed theme definitions in consultation with co‐authors. For the deductive element, we developed a TDF‐based coding manual with statements about how to categorise the inductively generated themes into the TDF (S5). Exercising reflexivity, we updated the manual and guidelines when needed. 43
2.5.3. Theoretical domains framework data coding and synthesis
Using an established framework synthesis approach 43 , 57 , 58 each data unit was coded as a TDF subtheme, and as a barrier or enabler. Ten per cent of studies were coded independently by three reviewers (A.N., A.L. and A.W.) using the TDF coding manual and discrepancies resolved by consensus. Two reviewers (H.N. and A.W.) coded the remaining data. Three reviewers (A.N., A.L. and A.W.) cross‐validated every extracted data item and disagreements were discussed until consensus was reached.
2.5.4. Data analysis
Key TDF domains were identified using two ‘importance’ criteria 58 : (i) frequency (number of studies identifying a domain) and (ii) elaboration (number of inductively generated themes within each domain). In contrast to the protocol, 47 we did not use statements from the authors emphasising importance because conclusions based on samples including White women were not always generalisable to women from diverse cultural backgrounds. The domains identified as ‘high’ importance are those where intervention is considered necessary to achieve personal‐level change. 45
3. RESULTS
3.1. Study characteristics
From 5148 unique records, we screened 139 full‐text articles. We excluded 16 studies from Dennison's reviews because they did not meet inclusion criteria (i.e. no participants from diverse cultures or insufficient data on participants' ethnicity). Exclusions are detailed in S6. We included 38 papers reporting 35 studies (Figure 2). Of these, 23 papers were new, including 17 papers published since Dennison's review. Thirty‐three (94%) were peer‐reviewed articles. In three cases, results of a single study were reported in two or more papers. We nominated the study as the unit of interest, 59 the earliest publication 60 , 61 , 62 as the primary source and retained the secondary papers. 63 , 64 , 65
FIGURE 2.
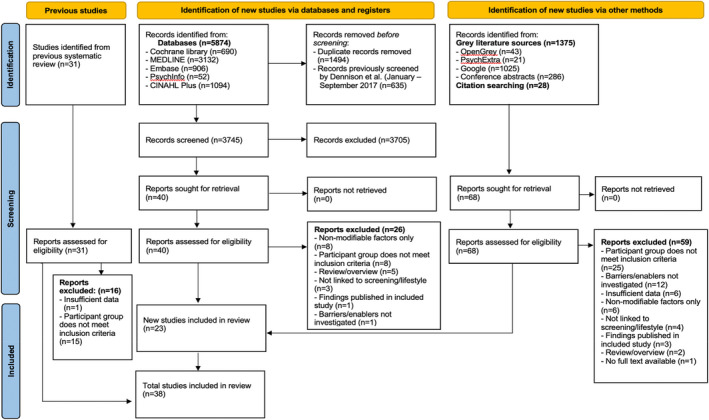
PRISMA flow diagram.
Study characteristics are summarised in Table 1 and detailed in S4. All studies were published between 2010 and 2021. The main data collection method was interviews (63%). Most (54%) reported sample sizes of N ≥ 16. Main study locations were North America, Europe and Australia (34%, 20% and 17% respectively). About two thirds of participants were living in their country of birth and one third were migrants. The ethnicity of most participants was Asian, Indigenous and African (43%, 15% and 11% respectively, Table 2).
TABLE 1.
Characteristics of 35 included studies
| Characteristic | N | % |
|---|---|---|
| Year of publication | ||
| ≤2011 | 6 | 17 |
| 2012–2016 | 12 | 34 |
| ≥2017 | 17 | 49 |
| Publication type | ||
| Peer reviewed | 33 | 94 |
| Grey literature | 2 | 6 |
| Study location | ||
| North America | 12 | 34 |
| Europe/UK | 7 | 20 |
| Australia | 6 | 17 |
| Asia | 7 | 20 |
| Middle East | 1 | 3 |
| Africa | 2 | 6 |
| Study sample size | ||
| ≤15 | 16 | 46 |
| 16–30 | 14 | 40 |
| ≥31 | 5 | 14 |
| Language | ||
| English | 35 | 100 |
| Interviews | 22 | 63 |
| Focus groups | 3 | 8 |
| Survey with open‐ended questions | 2 | 6 |
| Mixed | 8 | 23 |
| Quality rating (CASP) | ||
| Low | 4 | 11 |
| Medium | 14 | 40 |
| High | 17 | 49 |
Abbreviation: CASP, Critical Appraisal Skills Program assessment. 52
TABLE 2.
Ethnicity of participants in included studies (N = 787)
| Ethnicity | Country of origin (n) | Immigrants (n) | Total (N) | Total (%) |
|---|---|---|---|---|
| Asian a | 227 | 111 | 338 | 43 |
| Indigenous b | 118 | N/A | 118 | 15 |
| African c | 35 | 49 | 84 | 11 |
| Hispanic d | 0 | 70 | 70 | 9 |
| African American | 61 | NA | 61 | 8 |
| Middle Eastern e | 22 | 37 | 59 | 7 |
| Appalachian | 43 | 0 | 43 | 5 |
| Polynesian f | 11 | N/A | 11 | 1.4 |
| Mixed Ancestry g | 0 | 3 | 3 | 0.3 |
| Total | 517 | 270 | 787 |
South Asian (India, Sri Lanka [or speak Sinhala], Bangladesh, Pakistan, Nepal, Immigrant South Asian women who speak Hindi, Bengali or English), South‐eastern Asian (Malaysian, Malay, Thailand, Filipino, Indonesia), China/Chinese or Chinese speaking, Asian (no further specification).
Aboriginal and Torres Strait Islander (Australian Indigenous), Algonquin (First Nations Eastern Canada), Aboriginal Canadian, Cree (Indigenous women in Northern Quebec), American Indian/Alaska Native.
Haitian Creole speaking, Black African (UK), African and ‘mixed ancestry women in South Africa (English speaking, Xhosa speaking, Afrikaans speaking, Shona speaking, French speaking), African (UK, Sweden, France), South African (Australia).
Hispanic (US), Spanish speaking (US) Peruvian (Australia).
Arab (UK), Middle Eastern (Sweden), Iranian, Arabic (Australia).
Tongan.
Mixed Ancestry (UK).
3.2. Quality assessment
CASP rating was high (49%), medium (40%) or low (11%) (S7). Generally, aims were clear, with appropriate study methodology and design, recruitment strategies and data collection. A key area of strength was discussion of contribution of findings (Q10), with most studies providing implications and recommendations relevant to current policy and practice. Data analysis was typically well described and adequately rigorous, although some studies lacked adequate detail of analysis methods and evidence of cross‐validation. The main source of bias was a lack of critical examination of the role of the researcher in the formulation of research questions and data collection, and consideration of their relationship with participants. Furthermore, credibility of findings was not always discussed adequately. Lastly, some studies lacked detailed reporting of how ethical standards were maintained beyond obtaining ethical approval
3.3. Importance of theoretical domains framework domains
In total, 529 data units were extracted, with almost twice as many identified as barriers than as enablers (337 vs. 192, Table 3). Thirteen domains and five COM‐B constructs were identified. The (physical) dimension of Capability was not represented, nor was the TDF domain ‘Skills’. In general, frequency and elaboration were in good convergence for identifying the importance of eight domains, suggesting these domains are likely to impact postpartum health behaviours. This finding was supported by the proportion of data units coded into each domain (89%) and high proportion of themes and subthemes (78% and 87% respectively) (Table 4).
TABLE 3.
COM‐B construct and TDF domains by importance criteria
| COM‐B | TDF domain, definition (component constructs) | Relevance at the personal level | Importance criteria | Importance assessment | |
|---|---|---|---|---|---|
| Freq a | Elab b | ||||
| Capability (Psychological) | Knowledge |
(Lack of) knowledge of link between postpartum health behaviours and future type 2 diabetes risk (Lack of) knowledge of specific health behaviour recommendations to prevent future type 2 diabetes risk |
20 (57) | 2 | High |
| Memory, attention and decision processes |
Forgetting health behaviour recommendations Deciding not to take up postpartum health behaviour recommendations |
9 (26) | 4 | Low | |
| Behavioural regulation |
Planning and engaging with postpartum health behaviour recommendations Sustaining lifestyle changes made during pregnancy |
18 (51) | 2 | High | |
| Capability (Physical) | Skills | Not relevant (although postpartum health behaviours could be acquired through practice, e.g. learning to cook a healthy meal, this was not reported in the included studies) | 0 (0) | 0 | N/A |
| Opportunity (Physical) | Environmental context and resources (EC&R) | Environmental barriers (competing demands, lack of cultural‐specific resources, environment of facilities [e.g. not feeling safe], accessibility, socio‐economic) | 22 (63) | 8 | High |
| Opportunity (social) | Social influences |
Finding value in the health advice of healthcare professionals Social/emotional, pragmatic and peer support from family and friends to enable healthy behaviours Respecting the social norms of women's cultural group |
32 (91) | 5 | High |
| Motivation (Automatic) | Reinforcement | Previous experience of OGTT and GDM management during pregnancy | 7 (20) | 2 | Low |
| Emotion |
Fear and anxiety of being diagnosed with future type 2 diabetes as a motivator of healthy behaviours Impact of early parenthood and migrant experience on emotions including postpartum abandonment |
15 (43) | 3 | High | |
| Motivation (Reflective) | Beliefs about consequences |
Beliefs about the consequences of (not) following healthy behaviours on women's lives Beliefs about the importance of healthy behaviours for reducing future type 2 diabetes risk Cultural beliefs, norms or myths about healthy eating and exercise in the postpartum period |
24 (69) | 6 | High |
| Social/Professional Role and Identity | Placing one's healthcare needs secondary to those of the newborn, and secondary to family and cultural norms and needs | 17 (49) | 2 | High | |
| Beliefs about capabilities |
Perceived (in)ability to manage type 2 diabetes risk; perceived inevitability of type 2 diabetes Lack of confidence in capability to adhere to follow postpartum health behaviours |
16 (46) | 4 | High | |
| Optimism | Low perceived personal susceptibility to type 2 diabetes | 9 (26) | 1 | Low | |
| Goals | Setting goals relevant to postpartum health behaviours (e.g. being healthy for children, reduce weight) | 11 (31) | 1 | Low | |
| Intentions | Intentions to engage in/maintain healthy behaviour recommendations | 1 (3) | 1 | Low | |
Number of studies identified (%).
Number of themes.
TABLE 4.
Number of barriers and enablers coded to each TDF domain
| TDF domain | Barrier | Enabler | Combined |
|---|---|---|---|
| Environmental context and resources | 106 (31.5) | 17 (8.9) | 123 (23.2) |
| Social influences | 54 (16.0) | 50 (26.0) | 104 (19.7) |
| Beliefs about consequences | 41 (12.2) | 28 (14.6) | 69 (13.0) |
| Knowledge | 22 (6.5) | 25 (13.0) | 47 (8.9) |
| Social professional role and identity | 27 (8.0) | 9 (4.7) | 36 (6.8) |
| Beliefs about capabilities | 31 (9.2) | 2 (1.0) | 33 (6.2) |
| Behavioural regulation | 9 (2.7) | 23 (12.0) | 32 (6.0) |
| Emotion | 18 (5.3) | 7 (3.6) | 25 (4.7) |
| Goals | 2 (5.9) | 21 (10.9) | 23 (4.3) |
| Memory, attention and decision processes | 13 (3.9) | 3 (1.6) | 16 (3.0) |
| Optimism | 8 (2.4) | 4 (2.1) | 12 (2.3) |
| Reinforcement | 6 (1.8) | 2 (2.2) | 8 (1.5) |
| Intentions | 0 (0) | 1 (0.5) | 1 (0.2) |
| Skills | 0 (0) | 0 (0) | 0 (0) |
| Total | 337 | 192 | 529 |
Note: Values are n (% of barrier, enabler or combined data units).
3.4. High importance domains that likely influence postpartum health behaviours
Domains identified as high importance are described below and summarised in Tables 3 and S8. Details of domains and themes/subthemes that were considered less important are provided in S9.
3.4.1. COM‐B capability
Knowledge (20 studies; 18 barriers, 18 enablers)
Knowledge of future diabetes risk or healthy behaviours was an important enabler, the lack thereof was a barrier.
Knowledge and awareness of health behaviours (17 studies) and Knowledge and awareness of condition (6 studies). Awareness of postpartum health behaviours and future T2D risk were enablers: ‘Mothers recognised that healthier eating and being more active were ways of reducing their risk of T2DM’. 66 Women listed examples including restricting carbohydrates, sugar and fat, 66 , 67 , 68 , 69 , 70 , 71 eating more vegetables, wholegrains, proteins and an appropriate amount of fruit, 66 , 67 , 68 , 72 being physically active 66 , 67 , 68 , 70 , 71 , 72 and screening for T2DM. 73 , 74 For example, a migrant Middle Eastern women describes ‘Vegetables … Fat content should be low, for example in cheese, milk … brown bread … That I should not eat more than two fruits … ’. 67 Indigenous women noted that traditional diets could be adapted: ‘we could choose game meats that have less fat than others’ 66 , 75 or review ‘current recipes and change ingredients’. 69
Lack of awareness was a barrier. Some women believed GDM was ‘confined to pregnancy’ and were unaware of future risks. 60 , 62 , 63 , 65 , 77 For them, risk beyond the immediate postpartum period was not a concern. 60 , 63 , 77 Thus, ‘many reverted to previous diet habits … and did not engage in … prevention activities’. 60 , 63 Some indicated insufficient knowledge of diet recommendations and glycaemic impact 69 , 71 , 73 , 78 : ‘I thought me just eating fruit was good, but it actually was… how much you eat, you know?’. 71
Behavioural regulation (18 studies; 8 barriers, 19 enablers).
While some found engaging in healthy behaviours challenging, many women were motivated and proactive in maintaining healthy habits after birth.
Proactive behaviour (16 studies) and Sustaining behaviour change and/or habits (6 studies). Many women felt motivated to overcome difficulties related to sustaining healthy behaviours after birth: ‘It was a big lifestyle change that I had to do. I would eat the food like any normal African eats…Now …when I make chicken, I remove the skin’. 61 , 64 Some women were proactive by initiating T2DM screening with their HCPs. 62 , 65 , 74 Mi'kmaq (First Nations people of North‐eastern Canada) were raising ‘awareness about their health and the health of their children and communities’. 69 Others found sustaining behaviours initiated during pregnancy challenging 68 , 70 , 73 , 79 , 80 , 81 , 82 : ‘We have a beautiful new trail … I know it's there, but I don't go’. 66 Many were ‘eating as usual’ 78 and ‘exercise habits … were abandoned following childbirth’. 68 COM‐B Opportunity.
Environmental context and resources (22 studies; 91 barriers, 16 enablers)
A range of environmental factors, such as competing demands, lack of (culturally appropriate) resources and inaccessible or unsafe environments were barriers to healthy behaviours. Conversely, appropriate education and resources were enablers.
Competing demands (16 studies). Adjusting to life with a newborn while also being overwhelmed with other responsibilities constrained women's time and/or ability to prioritise their own health: ‘Once you have your baby it's all about caring for them… I don't have any memory of ‘Did I eat right or did I exercise?’. 72 Consequently, some women ‘eat anything available at home’, 83 postpone exercising ‘until my baby becomes a little bit bigger’ 68 and found ‘no time in a day to go to the lab for screening’. 84
Education and resources (15 studies). Education on health behaviours was an enabler, and the lack thereof was a barrier, particularly resources adapted to women's culture and way of life. 75 , 85 Predominantly, women mentioned that information on how to modify their diet while continuing to cook traditional meals was notably absent 66 , 73 , 75 and largely catered to a western audience: ‘It's all according to Australian things like steak, meat pie… we don't eat those things’. 86
Environment of facilities and resources (15 studies), accessibility of facilities and resources (10 studies) and Screening requirements (3 studies). An important barrier to using services (health services, programs promoting physical activity, healthy foods, library) was inaccessibility, regarding both transport and physical distance. An African American woman cited ‘lack of transportation as a barrier for poorer women, as they need to travel to providers' offices or the library to do research on GDM, and suggested home visits from providers as a solution’. 81 Due to a lack of grocery stores nearby, Mi'kmaq women suggested a local food bank would enable better access ‘until transportation became available to get to the supermarket’. 69 , 81
Unsafe or unfriendly (e.g. cultural, gender or physical) environments were barriers, especially in Indigenous communities. 66 , 69 , 71 , 79 , 87 Women were hindered by intimidating or unwelcoming environments ‘without Aboriginal or Torres Strait Islander staff’ 79 and ‘dogmatic attitudes’. 71 Some were deterred by the presence of ‘strong built people’ 66 in exercise facilities, preferring a ‘private place to exercise away from men’. 69 Other barriers included issues with appointment scheduling, 68 , 76 , 81 , 88 lack of childcare and breastfeeding facilities, 61 , 64 , 84 limited or inflexible opening hours, 71 , 79 , 88 long waiting times 62 , 65 , 84 , 87 , 88 , 89 and test duration. 62 , 65 , 68 , 89
Social Influences (32 studies; 47 barriers, 38 enablers)
Information regarding future risks or healthy behaviour recommendations provided by HCPs were important enablers, as were pragmatic or emotional support from family and friends. The lack thereof was identified as barriers.
Communication with Healthcare professionals (HCPs) (23 studies). Women perceived (family) doctors as important sources of advice and support 74 , 78 , 90 and ‘used information provided by clinicians to interpret the seriousness of GDM and to decide what value they should personally place on postnatal follow‐up’. 74 This enabled prioritisation of follow‐up when HCPs stressed their future T2D risk and the importance of healthy behaviours. 61 , 62 , 63 , 64 , 65 , 73 , 74 , 75 , 78 , 79 , 86 , 87 , 88 , 89 Lack of information provision was a barrier. Many women reported that HCPs did not inform them about their risk of T2DM 62 , 65 , 68 , 74 , 84 , 89 :or strategies to support T2DM prevention 67 , 71 , 81 , 91 : ‘The breastfeeding helps control blood sugar …? I was never told that’. 71 They also noted a lack of specific or accurate recommendations 62 , 65 , 68 , 70 , 77 , 78 , 81 , 86 , 87 , 88 , 89 , 92 : ‘Health workers said … they could eat and drink in the same manner as a women who had a normal pregnancy’. 68
Social support (19 studies). The presence of social support (both pragmatic and social/emotional) was an enabler. Spouses, parents and siblings, some of whom also lived with diabetes, helped with childcare, 71 , 89 encouragement, 68 , 71 , 75 , 81 , 85 , 87 , 89 role modelling 66 , 75 , 77 , 89 and joining them in healthy behaviours. 68 , 69 , 72 , 73 , 75 Algonquin (First Nations Eastern Canada) women mentioned that health centres held community meals with traditional foods adapted for a special diet, for example ‘banik (traditional bread) prepared with whole‐wheat flour’ and ‘distributed the recipes’. 75 The communities also supported physical activities by ‘painting these in a positive light’. 75
Conversely, some women reported little pragmatic support 62 , 65 , 73 , 76 , 84 , 85 , 88 , 89 or encouragement 68 , 72 , 75 , 77 , 85 , 86 , 88 : ‘They have their own ways of doing things, and it kind of gets handed down to us, and it's hard to change’. 93 Migrant women, customarily supported by female relatives in the postpartum period in their home country, reported that their engagement in healthy behaviours was impaired by lack of support at home, and feelings of isolation and loneliness. 73 , 85 They expressed a desire for ‘someone to help me … to lighten my burden’. 85
3.4.2. COM‐B motivation
Beliefs about consequences (24 studies; 31 barriers, 25 enablers)
Perceived negative consequences of healthy behaviours or cultural beliefs were important barriers, and perceived positive consequences were enablers. While the perception of continuing healthy behaviours as unnecessary was a barrier, visible consequences of diabetes in families or anticipated regret were important enablers.
Consequences of health behaviours (17 studies) including T2DM screening (4 studies). Some perceived following a healthy diet to be restrictive. 71 , 80 , 87 A South African woman explains: ‘it required eating separately from the rest of the family … impractical when having to also cater for the rest of the family’. Others were ‘enjoying healthy foods’ 80 or reported a ‘sense of well‐being with healthier diets’. 77 Some women mentioned breastfeeding as a reason to eat more (potentially unhealthy) food. 83 , 94 Breastfeeding motivated others ‘because they perceived their own nutrition was important for the baby’. 81 Some beliefs were culture specific. In Sri Lanka, women believe that certain traditional foods can reduce blood glucose: ‘kola kanda [a drink made with green leaves and coconut milk] has a sugar‐lowering effect’. 68 In some South Asian communities, women customarily eat or restrict certain foods to promote breastfeeding and recovery 77 , 83 , 86 and reduce physical activity levels in the first month after delivery: ‘one month definitely not going outside’. 86 Women perceived exercise positively as it relieved stress, 75 made them feel and eat healthier 91 because ‘when you train a lot, diet follows’. 75
Perceived necessity of healthy behaviours (12 studies), Salience of consequences (5 studies) and Anticipated outcome (6 studies). Some women felt that sustaining healthy behaviours was no longer a priority because ‘my baby is no longer in my womb’ 83 and could not be hurt by their behaviours. 61 , 64 , 93 Some ‘swiftly reverted to their pre‐GDM lifestyles after the first postnatal normal blood glucose level’, 86 because they experienced no symptoms. 68 Some perceived they were already engaging in sufficient physical activity: ‘I do exercise at home: I clean (laughs)’. 71 , 77 , 94 Others were aware of the necessity of healthy behaviours because consequences of diabetes in their family or friends were visible to them including complications and death. 60 , 62 , 65 , 73 , 86 , 91 For example, ‘I can't allow myself to have complications like that’, and anticipated that they were ‘going to regret it’ if they did not change. 62 , 65 , 72 , 82 , 89
Beliefs about capabilities (16 studies; 24 barriers, 2 enablers)
Fatalistic attitudes relating to T2DM risk and perceived inability to follow healthy lifestyles were common barriers to healthy behaviours.
Perceived (in)ability to control T2DM risk (seven studies). Belief in the inevitability of developing T2DM was a key barrier to engaging in healthy behaviours. 60 , 63 , 72 , 73 , 80 , 85 Fatalistic attitudes 73 were illustrated by expressions such as ‘matter of fate or luck’, 85 ‘God decides’ 70 and ‘its in my blood’. 60 , 63 Therefore, recommended changes were considered futile: ‘there was nothing they could do but accept it and get on with their life’. 85
Perceived (in)ability to follow healthy lifestyles (six studies), Physical capability (six studies) Despite their efforts many women found the prospect of lifelong behavioural management challenging. 78 , 80 , 84 , 94 They expressed how difficult it is ‘to plan healthy meals and learn how to cook differently’. 80 Sometimes this related to physical capabilities, such as lacking energy, 73 , 79 , 94 exhaustion, 72 feeling weak 94 or unwell. 84 Others did not think they could initiate healthy behaviours on their own. 68
Social–professional role and identity (17 studies; 22 barriers, 5 enablers)
Here, social role and identity refers to a women's role as a mother, wife, family member and member of a cultural group. Honouring these roles was a common barrier. Role modelling children was an enabler.
Often, role expectations were embedded in a context of cultural notions and identity. Women's motivation to engage in healthy behaviours was hindered by their prioritisation of the needs of their children, husband and household tasks. 68 , 72 , 79 , 83 , 84 , 85 , 88 , 89 Most women believed that putting themselves last to be a part of their role as a mother 68 , 84 , 89 : ‘That is the beauty of being a mother’. 84 Cultural expectations regarding their responsibilities made them feel bound to honour their roles 83 , 85 and reluctant to rely on family. 82 , 85 , 89 Ultimately, their own needs would come last: ‘I put my stuff on the back burner’. 72
Cultural expectations around food and social gatherings was a barrier to healthy dietary practices: ‘everything revolves around food’. 80 Women felt that healthy eating went against the norm of family meals: ‘sitting down and eating the same thing at the dinner table’, 95 causing disruptions and tensions and reduced enjoyment of mealtimes. 87 , 95 Consequently, they felt bound to eat whatever was offered to them 85 : ‘because in our cooking you cannot just say … chicken curry on its own without rice or chapatti…’. 73
Conversely, for some, the opportunity to act as a role model for their children was an enabler: ‘If I'm eating right, then they see me eating right … they're getting the idea it's important to exercise … So hopefully to kind of break the cycle’. 72
Emotion (15 studies; 15 barriers, 6 enablers)
Fear of T2D acted either as a barrier or enabler for healthy behaviours. Emotions such as stress or depression were barriers.
Fear/anxiety (nine studies). The fear of T2DM and its potential consequences was a motivating factor for healthy behaviours for some, 62 , 65 , 68 , 78 , 91 , 93 and a barrier to attend T2DM screening for others, 60 , 63 , 68 , 79 , 89 as they were ‘not ready to accept a life‐threatening diagnosis’. 68
Emotion (other) (six studies). For several women, psychological distress after delivery, including stress, shame and depression stood in the way of continuing health behaviours. 61 , 64 , 67 , 79 Some described a ‘sense of abandonment’ when in contrast to pregnancy, care was ceased abruptly after delivery 61 , 64 , 86 , 92 : ‘Once you've had your baby it's on your way mate… They don't bother…’. 92 For migrant Arabic women in Australia, mental health could not be separated from migrant experiences: ‘I don't interact with anyone. And even this country affects one's psychological health as well. Psychological condition can affect everything’. 85
3.5. Development of conceptual model and linkages between TDF domains
Guided by the Behaviour Change Wheel (Figure 1), and underpinned by 25 established behaviour change techniques, we developed a conceptual model (Figure 3). The model structures the synthesised data (focused on the TDF domains of highest importance) according to Capability, Opportunity and Motivation (COM‐B model components) and link this to evidence‐based communication recommendations via intervention functions of the Behaviour Change Wheel. Full detail and example communication points are in S11.
FIGURE 3.
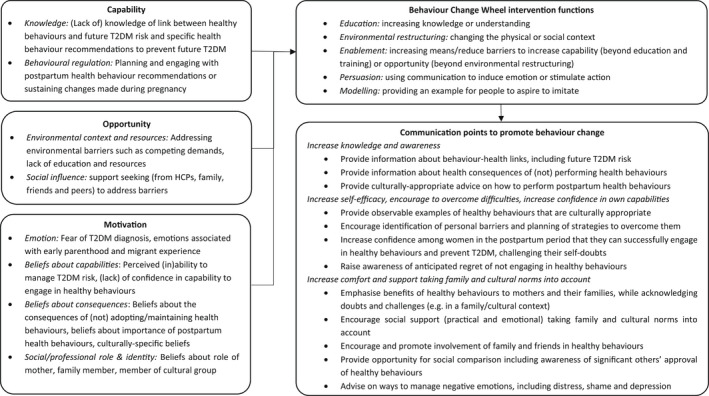
Evidence‐based recommendations to promote postpartum uptake of healthy behaviours among women from diverse cultural backgrounds with previous gestational diabetes.
3.6. Confidence in synthesis findings
Confidence in findings and explanation are summarised in Table 5 (full detail and GRADE‐CERQual qualitative evidence profile in S10). The degree of confidence for all findings within important TDF domains was judged to be moderate to high.
TABLE 5.
Confidence in synthesised qualitative findings for ‘high’ importance TDF domains
| COM‐B | TDF domain, definition (component constructs) | Finding | Number of studies (N) (participants) | Confidence and explanation |
|---|---|---|---|---|
| Capability (Psychological) | Knowledge |
(Lack of) knowledge of specific health behaviour recommendations to prevent future T2DM risk (Lack of) knowledge of link between GDM and future T2DM risk |
19 (444) Bandyopadhyay 2015; Gaudreau; Hjelm 2007; Hjelm 2012; Hjelm 2018; Ingol; Jones 2015; Kilgour; Mohd Suan; Nielsen 2015; Oza Frank; Pace; Pinidiyapathirage; Rafii; Razee; Stotz; Sunny; Tang; Whitty Rogers 6 (149) Bernstein & Gunn; Krompa; Mohd Suan; Pace; Rafii; Pace |
High confidence: Finding is supported by 19 studies with moderate methodological concerns, and no or very minor coherence, adequacy and relevance concerns High confidence: Finding is supported by six studies with minor methodological concerns and no or very minor coherence, adequacy and relevance concerns |
| Behavioural regulation |
Planning and engaging with postpartum health behaviour recommendations Sustaining lifestyle changes made during pregnancy |
16 (354) Bandyopadhyay 2015; Campbell; Gaudreau; Hjelm Hjelm 2012; 2018; Jones 2012; Kilgour; Krompa; Muhwava; Oza Frank; Pace; Pinidiyapathirage; Rafii; Razee; Tang; Whitty Rogers 2016 6(93) Bandyopadhyay 2011; Hjelm 2007; Hjelm 2012; Hjelm 2018; Pinidiyapatharige; Whitty Rogers |
Moderate confidence: Finding is supported by 16 studies with moderate methodological concerns, no or minor coherence concerns, minor adequacy concerns and no or very minor relevance concerns High confidence: Finding is supported by six studies with minor methodological concerns and no or very minor coherence, adequacy and relevance concerns |
|
| Opportunity (Physical) | Environmental Context and Resources |
Competing demands Education and resources Environment and accessibility of facilities |
16 (529) Bandyopadhyay 2015; Bernstein & Gunn; Campbell; Ingol; Jones 2015; Mathew; Mohd Suan 2015; Oza Frank; Pace; Pinidiyapathirage; Rafii; Razee; Sunny; Tang; Tewari 14(319) Bandyopadhyay 2011; Bandyopadhyay 2015; Campbell; Doran; Gaudreau; Ingol; Jones 2015; Krompa; Nielsen 2015; Pace; Pinidiyapathirage; Razee; Tewari; Zulfiqar 15(473) Bernstein & Gunn; Campbell; Ingol; Jones 2015; Mathew; Mohd Suan; Muhwava; Oza Frank; Pace; Pinidiyapathirage; Rafii; Sakeena; Sunny; Tewari; Whitty Rogers |
High confidence: Finding is supported by 16 studies with moderate methodological concerns, no or very minor coherence, adequacy and relevance concerns High confidence: Finding is supported by 14 studies with minor methodological concerns, no or very minor coherence, adequacy and relevance concerns Moderate confidence: Finding is supported by 15 studies with moderate methodological concerns, no or very minor coherence and adequacy concerns and minor relevance concerns |
| Opportunity (Social) | Social Influences |
Finding value in the health advice of HCPs Seeking social/emotional, pragmatic and peer support from family and friends to enable postpartum health behaviours Respecting social norms of a women's cultural group |
23(518) Campbell 2017; Bandyopadhyay 2015; Bernstein & Gunn; Doran; Gaudreau; Hjelm 2007; Hjelm 2012; Hjelm 2018; Ingol; Kandasamy; Kilgour; Krompa; Mathew; Muhwava; Nielsen 2015; Oza Frank; Parsons; Pinidiyapathirage; Rafii; Sakeena; Sunny; Tewari; Zulfiqar 19 (543) Campbell; Bandyopadhyay 2011; Bandyopadhyay 2015; Gaudreau; Ingol; Jones 2015; Krompa; Mathew; Mohd Suan; Oza Frank; Pace; Pinidiyapathirage; Rafii; Razee; Sakeena; Sunny; Tewari; Whitty Rogers; Zulfiqar 5(160) Ingol; Jones; Neufeld; Pinidiyapathirage; Zulfiqar |
High confidence: Finding is supported by 23 studies with minor methodological concerns, no or very minor coherence, adequacy and relevance concerns High confidence: Finding is supported by 19 studies with minor methodological concerns, no or very minor coherence, adequacy and relevance concerns High confidence: Finding is supported by five studies with minor methodological concerns, no or very minor coherence, adequacy and relevance concerns |
| Motivation (Automatic) | Emotion |
Fear screening procedure or T2DM diagnosis, or that T2DM management will be the same as GDM management Impact of early parenthood and migrant experience on emotions including postpartum abandonment |
9(162) Bernstein&Gunn; Campbell; Doran; Hjelm 2007; Neufeld; Pinidiyapathirage; Rafii; Sakeena; Sunny 6(148) Campbell; Hjelm 2012; Muhwava; Parsons; Razee; Zulfiqar |
High confidence: Finding is supported by nine studies with minor methodological concerns, no or very minor coherence, adequacy and relevance concerns Moderate confidence: Finding is supported by six studies with moderate methodological concerns, no or very minor coherence and adequacy concerns and minor relevance concerns |
| Motivation (Reflective) | Beliefs about Consequences |
Beliefs about the impact of postpartum health behaviours on women's daily lives Beliefs about importance of postpartum health behaviours and future T2DM risk Cultural beliefs, norms and myths about diet and exercise in the postpartum period |
20(509) Bandyopadhyay 2011; Bandyopadhyay 2015; Campbell; Doran; Gaudreau; Hjelm 2018; Ingol; Jones 2012; Jones 2015; Krompa; Muhwava; Neufeld; Oza Frank; Pinidiyapathirage; Razee; Sakeena; Sundarapperuma; Sunny; Tewari; Zulfiqar 17 (300) Bandyopadhyay 2011; Bandyopadhyay 2015; Bernstein&Gunn; Doran; Ingol; Jones 2015; Krompa; Mathew; Muhwava; Neufeld; Pinidiyapathirage; Rafii; Sakeena; Sundarapperuma; Sunny; Tang; Zulfiqar 4(82) Krompa; Pinidiyapathirage; Sundarapperuma; Zulfiqar |
High confidence: Finding is supported by 20 studies with moderate methodological concerns, no or very minor coherence, adequacy and relevance concerns Moderate confidence: Findings is supported by 17 studies with moderate methodological concerns, no or very minor coherence, adequacy and relevance concerns Moderate confidence: Finding is supported by four studies with moderate methodological concerns, no or very minor coherence and concerns, minor adequacy concerns and moderate relevance concerns |
| Social/Professional Role and Identity | Placing one's healthcare needs secondary to those of the newborn and secondary to family and cultural norms and needs | 19(376) Bandyopadhyay 2011; Bandyopadhyay 2015; Boyd; Campbell; Jones 2012; Jones 2015; Mathew; Muhwava; Pinidiyapathirage; Razee; Sakeena; Sundarapperuma; Sunny; Tang; Tewari; Zulfiqar |
High confidence: Finding is supported by 19 studies with moderate methodological concerns, no or very minor coherence, adequacy and relevance concerns |
|
| Beliefs about Capabilities |
Perceived (in)ability to manage T2DM risk, perceived inevitability of T2DM Lack of confidence in capability to adhere to postpartum health behaviour recommendations |
7(151) Bandyopadhyay 2015; Bernstein&Gunn; Campbell; Hjelm 2018; Jones 2012; Jones 2015; Razee; 6(103) Bandyopadhyay 2011; Doran; Hjelm 2007; Jones 2012; Pinidiyapathirage; Whitty Rogers |
High confidence: Finding is supported by seven studies with minor methodological concerns, no or very minor coherence and adequacy concerns and minor relevance concerns Moderate confidence: Finding is supported by six studies with minor methodological concerns, minor coherence concerns, moderate adequacy concerns and no or very minor relevance concerns |
4. DISCUSSION
To our knowledge, this is the first comprehensive qualitative synthesis to apply behaviour change frameworks to enable systematic analysis of the views of women from diverse cultural backgrounds with prior GDM regarding their uptake of healthy lifestyle and screening behaviours in the postpartum period. These findings highlight that psychological Capability, physical and social Opportunity, and reflective and automatic Motivation are barriers and enablers to recommended postpartum health behaviours. While our work complements findings from previous reviews and finds some barriers and enablers common to those of general populations, it provides deeper understanding and cultural context to the perspectives of women from diverse cultural backgrounds. We identified multiple modifiable personal‐level factors impacting postpartum health behaviours across eight domains that are unique to these groups, such as social/cultural identity. Furthermore, we demonstrated linkages between domains to provide context and understanding. We developed a conceptual model to address these factors. This is likely to support optimised health behaviours in women from diverse cultures.
The combination of knowledge, information provision, (cultural) beliefs about consequences and importance of healthy behaviours, (culturally specific) education, fatalism and fear of a diabetes diagnosis impacted engagement in postpartum health behaviours. While reinforcing the findings of earlier reviews regarding the need to increase knowledge, 5 , 36 , 37 , 46 our work adds insight into cultural beliefs and customs that need to be addressed. Recent work among postpartum women in Singapore expands on cultural practices such as confinement, drinking red date tea (high sugar content) and excessive consumption of refined carbohydrates impacting healthy lifestyles. 96 Working with the broader community when developing messaging explaining that T2DM can be prevented (e.g. for American Indian women in Oklahoma who often perceive future T2DM as inevitable given most people they know are affected 97 ) and how to adapt traditional diets to eat healthier is warranted.
As part of their role as a mother, wife or member of a family and/or cultural group, women were often influenced by social norms or cultural expectations, competing demands and negative emotions that impacted their ability to prioritise their own health, especially in the absence of social support. Reviews in general populations highlighted the importance of the woman's role as a mother but for women from diverse backgrounds role expectations were additionally embedded in a context of family and/or cultural notions and identity. Social support 35 , 36 , 46 was important as for general populations but in contrast emotional support appeared particularly important compared to pragmatic support. 46 This complements previous reviews in populations with and without prior GDM, 21 , 35 to consider a family‐focused approach. Our work strengthens this by demonstrating that messaging content needs to be aimed at mothers, their families and communities, addressing family and cultural attitudes towards healthy behaviours. Importantly, engagement of (Indigenous) communities in the design of interventions is crucial and have reported to have positive effects on health behaviours, self‐efficacy, health consequences and perceived social support across various health conditions. 98 , 99 , 100 We underline that mental health and feelings of isolation, particularly related to migrant experiences is an important factor and HCPs need to be aware, identify and support women to access relevant social and professional support.
This review also identified themes related to self‐efficacy. Despite being aware of the need for postpartum health behaviours and trying to be proactive, feeling unable or unmotivated to overcome difficulties hindered women to engage in postpartum health behaviours. This finding has not been extensively explored in previous reviews regarding postpartum screening 35 , 36 , 37 , 46 potentially because they relate particularly to lifestyle behaviours that require sustained change. We encourage providing culturally appropriate advice and persuasive messaging, designed to address self‐doubts and fatalistic attitudes, and to persuade women that they can plan new approaches to overcome these barriers, successfully integrate healthy behaviours and prevent T2DM. Recent design of evidence‐based smartphone apps enables them to provide practical strategies and information at end user convenience. 101 , 102 , 103 , 104 This may offer opportunities for women to improve motivation without many of the barriers commonly experienced in the postpartum period. This may be particularly useful in under‐resourced rural environments. 105 It is important that design and usability of these e‐health interventions is relevant to women from diverse cultural backgrounds.
While this paper focuses on factors influencing individual‐level behaviour change, several important systemic barriers were identified, including accessibility, flexibility and safety. This requires broader policy and health service factors beyond individual messaging. For example, the prevalence of GDM and T2DM among migrants is higher than among the populations in their countries of origin. 106 , 107 Given the global rise in migration, currently affecting 135 million women internationally, the majority of reproductive age, this is of great public health importance. 108 Factors contributing to this increased risk are multifaceted (e.g. [epi]genetics, early life factors, lifestyle changes and migration‐related contextual factors) 106 , 107 and many challenges impacting healthy behaviours relate to immigration and broader socio‐economic issues rather than their cultural backgrounds per se. 40 Examples include issues related to communication with HCPs, a lack of culturally responsive healthcare services, preoccupation with needs such as finding appropriate living conditions, poverty, history of trauma and confusion about cultural customs. 109 , 110 Additionally, social determinants of health and impacts of detrimental colonial policies such as individual and systemic discrimination are recognised as contributors to poorer health outcomes and the epidemic of T2DM in Indigenous women across Australia and Canada. 12 , 98 , 99 , 111 , 112 To address this complex interplay of factors, directing attention to the root causes of disparities in GDM and T2DM and offering comprehensive, cultural competent (e.g. the presence of Indigenous healthcare staff) care catering for the needs of young families and women in remote areas that addresses history and context is needed. Increasing social support by peers, community centres and cultural workers in the community is also warranted.
4.1. Strengths and limitations
This review has several strengths. We included published and grey literature, qualitative and mixed method studies and focused solely on the perspectives of women from diverse cultural backgrounds, making our findings and recommendations culturally appropriate. Screening, coding, analysis and interpretation were cross‐validated by multiple authors in a multidisciplinary team. A hybrid thematic synthesis approach identified a broad range of behavioural determinants, avoiding risk of ‘rigid operationalisation’. 56 Using validated behaviour change frameworks to analyse and interpret our findings enabled theory‐driven, evidence‐based recommendations for clinical practice and future research.
This review also has limitations. A lack of adequate description hampered our ability to differentiate between perspectives relating to the pregnancy or postpartum period, between the perspectives of women from White or diverse cultural backgrounds or migrant compared with other women. Although we contacted authors for more details about participants' ethnicity, responses were not always forthcoming. Furthermore, while CASP assessments of study quality were generally high, the main limitation across all studies was lack of reflexivity. Finally, most participants came from Asian or Indigenous populations, thus factors salient to other cultural groups may be under‐represented in these findings. For example, data relating to cultural beliefs, norms and myths came mainly from South Asian women.
4.2. Implications for practice and research
Using the TDF framework, a conceptual model developed in this review informs on the most important domains and relevant intervention components to consider when developing messaging content for women from diverse cultural backgrounds with prior GDM. The current work includes a broad group of women. Most themes identified in this review applied across cultural groups with significant overlap compared to general populations. 21 , 35 , 36 , 46 Similarly, recent work among South Asian and Nordic women in Norway reported that determinants of suboptimal follow‐up after GDM were comparable across the two groups. 113 While we do not necessarily recommend designing different interventions for every ethnic group, there are specific needs such as tailoring information to address cultural food needs, translation of resources into relevant languages and broadening engagement to include family and community in knowledge and support. Policy makers need to take those into account when considering intervention components relevant to their target populations and tailor messaging content accordingly.
For HCPs, our review may provide guidance in practicing cultural competence by increasing awareness for specific needs to better connect and communicate with women from diverse cultural backgrounds. These findings need to be included in clinical guidelines and continuing professional development programs. Acknowledgement of women's health beliefs, and enabling them to feel included and respected as equal partners, will strengthen relationships with women, increasing their confidence that the HCP understands and supports them. 114 For example, clinicians could assess and acknowledge social context such as potential food insecurity, traditional diets or cultural beliefs regarding food and breastfeeding, and then integrate this into culturally appropriate dietary advice, as opposed to recommending a one‐size‐fits‐all approach. Moreover, including family and ensuring they are informed about and supportive of healthy behaviours will help increase women's engagement. Equally, or even more, important when understanding and appreciating experiences of women from diverse cultural backgrounds, is practicing cultural humility, because when building competence of the ‘other’, ‘cultural’ competence can inadvertently become synonymous with a static vision of race or ethnicity, thereby unintentionally implying that barriers are due to ‘cultural’ differences. 115 By critically self‐reflecting on one's own systematic biases, values and cultural assumptions, HCPs and systems that provide culturally safe care can relinquish the role of competent ‘expert’ and rather humbly acknowledge themselves as learners and supporters. 115
Primary papers included in this review did not always consistently or adequately describe ethnicity and findings from migrant women were underrepresented. Research needs to support better health equity in GDM for all women by including and identifying women from diverse cultures in order to recognise and be responsive to specific needs. 116 , 117 However, measurements of ethnicity are complex and numerous definitions are used in health research. Examples include self‐identified race/ethnicity, country of birth, language(s) spoken, ancestry, country of origin, immigrant status and years spent in country. 116 Inconsistent or inadequate use of definitions can undermine comparability and generalisability of research findings and could fail to identify groups at risk, such as second generation South Asian women. 116 While this work provides cultural context to the perspectives of women from diverse cultural backgrounds, we highlight that future studies using consistent and adequate definitions are needed across groups less studied and migrant groups across countries to explore (culturally) specific needs in more depths. Recent work offers recommendations for ethnicity definitions and reporting on migrant‐specific demographics. 117 , 118 , 119 Exploration of experiences from both women, their families and communities is warranted given many women come from collectivist cultures, in which decisions are shared and involve both family and community.
5. CONCLUSION
This review provides evidence on eight important theoretical domains mediating postpartum health behaviours unique to women from diverse cultural backgrounds with previous GDM. Thematic synthesis identified subthemes that are especially important in these groups in comparison to general populations (e.g. culturally appropriate education and resources, unsafe environments, social support, social norms, social/cultural identity, negative emotions, cultural beliefs, norms and myths and placing own needs above family and cultural norms). Hence, this review provides guidance on relevant intervention functions that will be more effective if they target these domains. Interventions informed by this work need to be trialled to evaluate effectiveness among priority cultural and migrant groups. 106 Future research using consistent and adequate definitions of cultural groups is needed to enrich data reporting on experiences from these women and to distinguish between needs for migrant and other women.
FUNDING INFORMATION
This project is funded by the Australian Government Department of Health (Health/18/1904983). CH and JS are supported by the core funding to the Australian Centre for Behavioural Research in Diabetes provided by the collaboration between Diabetes Victoria and Deakin University. HT is supported by a National Health and Medical Research Council Fellowship.
CONFLICT OF INTEREST
Nothing to declare.
Supporting information
Appendix S1
ACKNOWLEDGEMENTS
We thank Dr Becky Dennison for providing the search strings from her review. We thank Dr Marie Misso, Evidence Program, Monash University for systematic search guidance. We thank Angela Melder, Monash University for her assistance. Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
Neven ACH, Lake AJ, Williams A, et al. Barriers to and enablers of postpartum health behaviours among women from diverse cultural backgrounds with prior gestational diabetes: A systematic review and qualitative synthesis applying the theoretical domains framework. Diabet Med. 2022;39:e14945. doi: 10.1111/dme.14945
Footnotes
The term ‘Indigenous’ is used respectfully throughout this paper when referring to mixed groups of Indigenous, First Nations or Tribal people of Australia, Canada and the United States, in line with the ‘United Nations Declaration on the Rights of Indigenous peoples’.1 We recognise that it is a generic term that excludes any description of language group or Country and that it is not the preferred term among all Indigenous peoples. Elsewhere in the manuscript, we have adopted the terms used by the authors of the relevant empirical studies.)
REFERENCES
- 1. Classification and diagnosis of diabetes: standards of medical care in diabetes‐2020. Diabetes Care. 2020;43(Suppl 1):S14‐s31. [DOI] [PubMed] [Google Scholar]
- 2. Saravanan P. Gestational diabetes: opportunities for improving maternal and child health. Lancet Diabetes Endocrinol. 2020;8(9):793‐800. [DOI] [PubMed] [Google Scholar]
- 3. International Diabetes Federation . IDF diabetes atlas teB, Belgium, 2021. https://www.diabetesatlas.org.
- 4. Vounzoulaki E, Khunti K, Abner SC, Tan BK, Davies MJ, Gillies CL. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta‐analysis. BMJ. 2020;369:m1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dennison RA, Chen ES, Green ME, et al. The absolute and relative risk of type 2 diabetes after gestational diabetes: a systematic review and meta‐analysis of 129 studies. Diabetes Res Clin Pract. 2021;171:108625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. United Nations general assembly United Nations declaration on the rights of indigenous peoples. UN Wash. 2007;12:1–18. [Google Scholar]
- 7. Voaklander B, Rowe S, Sanni O, Campbell S, Eurich D, Ospina MB. Prevalence of diabetes in pregnancy among indigenous women in Australia, Canada, New Zealand, and the USA: a systematic review and meta‐analysis. Lancet Glob Health. 2020;8(5):e681‐e698. [DOI] [PubMed] [Google Scholar]
- 8. Shah NS, Wang MC, Freaney PM, et al. Trends in gestational diabetes at first live birth by race and ethnicity in the US, 2011‐2019. JAMA. 2021;326(7):660‐669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ahmed MA, Bailey HD, Pereira G, White SW, Wong K, Shepherd CCJ. Trends and burden of diabetes in pregnancy among aboriginal and non‐aboriginal mothers in Western Australia, 1998–2015. BMC Public Health. 2022;22(1):263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Abouzeid M, Versace VL, Janus ED, et al. Socio‐cultural disparities in GDM burden differ by maternal age at first delivery. PLoS ONE. 2015;10(2):e0117085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rayanagoudar G, Hashi AA, Zamora J, Khan KS, Hitman GA, Thangaratinam S. Quantification of the type 2 diabetes risk in women with gestational diabetes: a systematic review and meta‐analysis of 95,750 women. Diabetologia. 2016;59(7):1403‐1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shen GX, Shafer LA, Martens PJ, et al. Does first nations ancestry modify the association between gestational diabetes and subsequent diabetes: a historical prospective cohort study among women in Manitoba, Canada. Diabet Med. 2016;33(9):1245‐1252. [DOI] [PubMed] [Google Scholar]
- 13. Chamberlain CR, Oldenburg B, Wilson AN, et al. Type 2 diabetes after gestational diabetes: greater than fourfold risk among indigenous compared with non‐indigenous Australian women. Diabetes Metab Res Rev. 2016;32(2):217‐227. [DOI] [PubMed] [Google Scholar]
- 14. Abouzeid M, Philpot B, Janus E, Coates M, Dunbar J. Type 2 diabetes prevalence varies by socio‐economic status within and between migrant groups: analysis and implications for Australia. BMC Public Health. 2013;13:252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Xin Y, Davies A, McCombie L, et al. Within‐trial cost and 1‐year cost‐effectiveness of the DiRECT/counterweight‐plus weight‐management programme to achieve remission of type 2 diabetes. Lancet Diabetes Endocrinol. 2019;7(3):169‐172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lean ME, Leslie WS, Barnes AC, et al. Primary care‐led weight management for remission of type 2 diabetes (DiRECT): an open‐label, cluster‐randomised trial. Lancet. 2018;391(10120):541‐551. [DOI] [PubMed] [Google Scholar]
- 17. Bao W, Yeung E, Tobias DK, et al. Long‐term risk of type 2 diabetes mellitus in relation to BMI and weight change among women with a history of gestational diabetes mellitus: a prospective cohort study. Diabetologia. 2015;58(6):1212‐1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ehrlich SF, Hedderson MM, Quesenberry CP Jr, et al. Post‐partum weight loss and glucose metabolism in women with gestational diabetes: the DEBI study. Diabet Med. 2014;31(7):862‐867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Waage C, Falk R, Sommer C, et al. Ethnic differences in postpartum weight retention: a Norwegian cohort study. BJOG. 2016;123(5):699‐708. [DOI] [PubMed] [Google Scholar]
- 20. Aroda VR, Christophi CA, Edelstein SL, et al. The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the diabetes prevention program outcomes study 10‐year follow‐up. J Clin Endocrinol Metab. 2015;100(4):1646‐1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Makama M, Awoke MA, Skouteris H, Moran LJ, Lim S. Barriers and facilitators to a healthy lifestyle in postpartum women: a systematic review of qualitative and quantitative studies in postpartum women and healthcare providers. Obes Rev. 2021;22(4):e13167. [DOI] [PubMed] [Google Scholar]
- 22. National Institute for Health and Care Excellence . (2015). Diabetes in pregnancy: management from preconception to the postnatal period. NICE Guideline [NG3]. https://www.nice.org.uk/guidance/ng3. Accessed 11 December 2021. [PubMed]
- 23. Management of diabetes in pregnancy: standards of medical care in diabetes‐2020. Diabetes Care. 2020;43(Suppl 1):S183‐s192. [DOI] [PubMed] [Google Scholar]
- 24. Tovar A, Chasan‐Taber L, Eggleston E, Oken E. Postpartum screening for diabetes among women with a history of gestational diabetes mellitus. Prev Chronic Dis. 2011;8(6):A124. [PMC free article] [PubMed] [Google Scholar]
- 25. Nouhjah S, Shahbazian H, Amoori N, et al. Postpartum screening practices, progression to abnormal glucose tolerance and its related risk factors in Asian women with a known history of gestational diabetes: a systematic review and meta‐analysis. Diabetes Metab Syndr. 2017;11(Suppl 2):S703‐s712. [DOI] [PubMed] [Google Scholar]
- 26. Boyle DIR, Versace VL, Dunbar JA, et al. Results of the first recorded evaluation of a national gestational diabetes mellitus register: challenges in screening, registration, and follow‐up for diabetes risk. PLoS ONE. 2018;13(8):e0200832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vounzoulaki E, Khunti K, Tan B, Davies M, Gillies C. Gestational diabetes: screening uptake, current challenges and the future – a focused review. Brit J Diabetes. 2020;20:9‐14. [Google Scholar]
- 28. Butalia S, Donovan L, Savu A, Johnson J, Edwards A, Kaul P. Postpartum diabetes testing rates after gestational diabetes mellitus in Canadian women: a population‐based study. Can J Diabetes. 2017;41(6):613‐620. [DOI] [PubMed] [Google Scholar]
- 29. Dalfrà MG, Burlina S, Del Vescovo GG, Anti F, Lapolla A. Adherence to a follow‐up program after gestational diabetes. Acta Diabetol. 2020;57(12):1473‐1480. [DOI] [PubMed] [Google Scholar]
- 30. Goueslard K, Cottenet J, Mariet AS, Sagot P, Petit JM, Quantin C. Early screening for type 2 diabetes following gestational diabetes mellitus in France: hardly any impact of the 2010 guidelines. Acta Diabetol. 2017;54(7):645‐651. [DOI] [PubMed] [Google Scholar]
- 31. McGovern A, Butler L, Jones S, et al. Diabetes screening after gestational diabetes in England: a quantitative retrospective cohort study. Br J Gen Pract. 2014;64(618):e17‐e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kieffer EC, Sinco B, Kim C. Health behaviors among women of reproductive age with and without a history of gestational diabetes mellitus. Diabetes Care. 2006;29(8):1788‐1793. [DOI] [PubMed] [Google Scholar]
- 33. Persson M, Winkvist A, Mogren I. Lifestyle and health status in a sample of Swedish women four years after pregnancy: a comparison of women with a history of normal pregnancy and women with a history of gestational diabetes mellitus. BMC Pregnancy Childbirth. 2015;15:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Stage E, Ronneby H, Damm P. Lifestyle change after gestational diabetes. Diabetes Res Clin Pract. 2004;63(1):67‐72. [DOI] [PubMed] [Google Scholar]
- 35. Dennison RA, Ward RJ, Griffin SJ, Usher‐Smith JA. Women's views on lifestyle changes to reduce the risk of developing type 2 diabetes after gestational diabetes: a systematic review, qualitative synthesis and recommendations for practice. Diabet Med. 2019;36(6):702‐717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dennison RA, Fox RA, Ward RJ, Griffin SJ, Usher‐Smith JA. Women's views on screening for type 2 diabetes after gestational diabetes: a systematic review, qualitative synthesis and recommendations for increasing uptake. Diabet Med. 2020;37(1):29‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sanderson H, Loveman E, Colquitt J, Royle P, Waugh N, Tan BK. Improving uptake of postnatal checking of blood glucose in women who had gestational diabetes mellitus in universal healthcare settings: a systematic review. J Clin Med. 2018;8(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gelfand MJ, Raver JL, Nishii L, et al. Differences between tight and loose cultures: a 33‐nation study. Science. 2011;332(6033):1100‐1104. [DOI] [PubMed] [Google Scholar]
- 39. Rogers HJ, Hogan L, Coates D, Homer CSE, Henry A. Responding to the health needs of women from migrant and refugee backgrounds—models of maternity and postpartum care in high‐income countries: a systematic scoping review. Health Soc Care Commun. 2020;28(5):1343‐1365. [DOI] [PubMed] [Google Scholar]
- 40. Bagger S, Maindal HT, Nielsen KK, Vrå AG, Aagaard‐Hansen J. Perceptions of risk and motivation for healthy living among immigrants from non‐western countries with prior gestational diabetes mellitus living in Denmark. Health Psychol Behav Med. 2021;9(1):761‐777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Henrich J, Heine SJ, Norenzayan A. The weirdest people in the world? Behav Brain Sci. 2010;33(2–3):61‐83. [DOI] [PubMed] [Google Scholar]
- 42. Bartholomew LK, Mullen PD. Five roles for using theory and evidence in the design and testing of behavior change interventions. J Public Health Dent. 2011;71(Suppl 1):S20‐S33. [DOI] [PubMed] [Google Scholar]
- 43. Atkins L, Francis J, Islam R, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lake AJ, Neven ACH, Williams A, et al. Barriers to and enablers of type 2 diabetes screening among women with prior gestational diabetes: a systematic review update and qualitative synthesis applying the theoretical domains framework. Diabet Med. 2021;39:e14772. [DOI] [PubMed] [Google Scholar]
- 47. H Neven, J Boyle, Teede H, et al. Barriers and enablers to postpartum diabetes screening and healthy lifestyle after gestational diabetes: a systematic review and qualitative synthesis (CRD42020164855). https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020164855. Accessed 19 December 2021.
- 48. Working Group of the Migrant and Refugee Women's Health Partnership . Culturally responsive clinical practice: working with people from migrant and refugee backgrounds: competency standards framework for clinicians January 2019. Migrant and Refugee Women's Health Partnership; 2019:44 p. https://www.midwives.org.au/sites/default/files/uploaded‐content/website‐content/culturally_responsive_clinical_practice_‐_working_with_people_from_migrant_and_refugee_backgrounds_jan2019.pdf. Accessed 8 July 2022. [Google Scholar]
- 49. Bainbridge R, McCalman J, Clifford A, Tsey K. Cultural competency in the delivery of health services for indigenous people. Closing the Gap Clearinghouse. Canberra, Australia: James Cook University; 2015. [Google Scholar]
- 50. Laverty M, McDermott DR, Calma T. Embedding cultural safety in Australia's main health care standards. Med J Aust. 2017;207(1):15‐16. [DOI] [PubMed] [Google Scholar]
- 51. Stubbe DE. Practicing cultural competence and cultural humility in the care of diverse patients. Focus (Am Psychiatr Publ). 2020;18(1):49‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Critical Appraisal Programme . CASP qualitative checklist. https://casp‐uknet/wp‐content/uploads/2018/01/CASP‐Qualitative‐Checklist‐2018pdf
- 53. Long HA, French DP, Brooks JM. Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res Meth Med Health Sci. 2020;1(1):31‐42. [Google Scholar]
- 54. Lewin S, Booth A, Glenton C, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci. 2018;13(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Noyes J, Booth A, Flemming K, et al. Cochrane qualitative and implementation methods group guidance series‐paper 3: methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. J Clin Epidemiol. 2018;97:49‐58. [DOI] [PubMed] [Google Scholar]
- 56. McGowan LJ, Powell R, French DP. How can use of the theoretical domains framework be optimized in qualitative research? A rapid systematic review. Br J Health Psychol. 2020;25(3):677‐694. [DOI] [PubMed] [Google Scholar]
- 57. Shaw RL, Holland C, Pattison HM, Cooke R. Patients' perceptions and experiences of cardiovascular disease and diabetes prevention programmes: a systematic review and framework synthesis using the theoretical domains framework. Soc Sci Med. 2016;156:192‐203. [DOI] [PubMed] [Google Scholar]
- 58. Graham‐Rowe E, Lorencatto F, Lawrenson JG, et al. Barriers to and enablers of diabetic retinopathy screening attendance: a systematic review of published and grey literature. Diabet Med. 2018;35(10):1308‐1319. [DOI] [PubMed] [Google Scholar]
- 59. Lefebvre C, Glanville J, Briscoe S, et al. Chapter 4: Searching for and selecting studies. In: Higgins JPT, Thomas J, Chandler J, et al., eds. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane; 2022. www.training.cochrane.org/handbook. Accessed 8 July 2022. [Google Scholar]
- 60. Bernstein JA, McCloskey L, Gebel CM, Iverson RE, Lee‐Parritz A. Lost opportunities to prevent early onset type 2 diabetes mellitus after a pregnancy complicated by gestational diabetes. BMJ Open Diabetes Res Care. 2016;4(1):e000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Muhwava LS, Murphy K, Zarowsky C, Levitt N. Experiences of lifestyle change among women with gestational diabetes mellitus (GDM): a behavioural diagnosis using the COM‐B model in a low‐income setting. PLoS ONE. 2019;14(11):e0225431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Rafii F, Rahimparvar SFV, Mehrdad N, Keramat A. Barriers to postpartum screening for type 2 diabetes: a qualitative study of women with previous gestational diabetes. Pan Afr Med J. 2017;26:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Gunn C, Bernstein J, Bokhour B, McCloskey L. Narratives of gestational diabetes provide a lens to tailor postpartum prevention and monitoring counseling. J Midwifery Womens Health. 2020;65(5):681‐687. [DOI] [PubMed] [Google Scholar]
- 64. Muhwava LS, Murphy K, Zarowsky C, Levitt N. Perspectives on the psychological and emotional burden of having gestational diabetes amongst low‐income women in Cape Town, South Africa. BMC Womens Health. 2020;20(1):231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Rafii F, Vasegh Rahimparvar SF, Keramat A, Mehrdad N. Procrastination as a key factor in postpartum screening for diabetes: a qualitative study of Iranian women with recent gestational diabetes. Iran Red Crescent Med J. 2017;19(5). doi: 10.5812/ircm.44833 [DOI] [Google Scholar]
- 66. Pace R, Loon O, Chan D, et al. Preventing diabetes after pregnancy with gestational diabetes in a Cree community: an inductive thematic analysis. BMJ Open Diabetes Res Care. 2020;8(1):e001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Hjelm K, Bard K, Apelqvist J. Gestational diabetes: prospective interview‐study of the developing beliefs about health, illness and health care in migrant women. J Clin Nurs. 2012;21(21–22):3244‐3256. [DOI] [PubMed] [Google Scholar]
- 68. Pinidiyapathirage MJ. Sociocognitive Determinants of Lifestyle Behaviours of Sri Lankan Women with a Recent History of Gestational Diabetes Mellitus. University of New South Wales; 2015. [Google Scholar]
- 69. Whitty‐Rogers J, Caine V, Cameron B. Aboriginal Women's experiences with gestational diabetes mellitus: a participatory study with Mi'kmaq women in Canada. ANS Adv Nurs Sci. 2016;39(2):181‐198. [DOI] [PubMed] [Google Scholar]
- 70. Hjelm K, Bard K, Apelqvist J. A qualitative study of developing beliefs about health, illness and healthcare in migrant African women with gestational diabetes living in Sweden. BMC Womens Health. 2018;18(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Ingol TT, Kue J, Conrey EJ, Oza‐Frank R, Weber MB, Bower JK. Perceived barriers to type 2 diabetes prevention for low‐income women with a history of gestational diabetes: a qualitative secondary data analysis. Diabetes Educ. 2020;46(3):271‐278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Jones EJ, Peercy M, Woods JC, et al. Identifying postpartum intervention approaches to reduce cardiometabolic risk among American Indian women with prior gestational diabetes, Oklahoma, 2012‐2013. Prev Chronic Dis. 2015;12:E45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Bandyopadhyay M. Attendance for postpartum glucose tolerance testing following gestational diabetes among south Asian women in Australia: a qualitative study. J Women's Health, Issues Care. 2015;4(1). doi: 10.4172/2325-9795.1000178 [DOI] [Google Scholar]
- 74. Kilgour C, Bogossian FE, Callaway L, Gallois C. Postnatal gestational diabetes mellitus follow‐up: Australian women's experiences. Women Birth. 2015;28(4):285‐292. [DOI] [PubMed] [Google Scholar]
- 75. Gaudreau S, Michaud C. Cultural factors related to the maintenance of health behaviours in Algonquin women with a history of gestational diabetes. Chronic Dis Inj Can. 2012;32(3):140‐148. [PubMed] [Google Scholar]
- 76. Mohd Suan MA. Return for postpartum Oral glucose tolerance test following gestational diabetes mellitus. Asia Pac J Public Health. 2015;27(6):601‐609. [DOI] [PubMed] [Google Scholar]
- 77. Krompa K, Sebbah S, Baudry C, Cosson E, Bihan H. Postpartum lifestyle modifications for women with gestational diabetes: a qualitative study. Eur J Obstet Gynecol Reprod Biol. 2020;252:105‐111. [DOI] [PubMed] [Google Scholar]
- 78. Hjelm K, Bard K, Berntorp K, Apelqvist J. Beliefs about health and illness postpartum in women born in Sweden and the Middle East. Midwifery. 2009;25(5):564‐575. [DOI] [PubMed] [Google Scholar]
- 79. Campbell S, Roux N, Preece C, et al. Paths to improving care of Australian aboriginal and Torres Strait islander women following gestational diabetes. Prim Health Care Res Dev. 2017;18(6):549‐562. [DOI] [PubMed] [Google Scholar]
- 80. Jones EJ, Appel SJ, Eaves YD, Moneyham L, Oster RA, Ovalle F. Cardiometabolic risk, knowledge, risk perception, and self‐efficacy among American Indian women with previous gestational diabetes. J Obstet Gynecol Neonatal Nurs. 2012;41(2):246‐257. [DOI] [PubMed] [Google Scholar]
- 81. Oza‐Frank R, Conrey E, Bouchard J, Shellhaas C, Weber MB. Healthcare experiences of low‐income women with Prior gestational diabetes. Matern Child Health J. 2018;22(7):1059‐1066. [DOI] [PubMed] [Google Scholar]
- 82. Tang JW, Foster KE, Pumarino J, Ackermann RT, Peaceman AM, Cameron KA. Perspectives on prevention of type 2 diabetes after gestational diabetes: a qualitative study of Hispanic, African‐American and White women. Matern Child Health J. 2015;19(7):1526‐1534. [DOI] [PubMed] [Google Scholar]
- 83. Sundarapperuma TD, Wijesinghe CJ, Hettiarachchi P, Wasalathanthri S. Perceptions on diet and dietary modifications during postpartum period aiming at attenuating progression of GDM to DM: a qualitative study of mothers and health care workers. J Diabetes Res. 2018;2018:6459364‐6459366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Sakeena K, Ravindran TS. Perceived barriers to timely postpartum screening of women with gestational diabetes (GDM): a qualitative study http://www.esocialsciences.org/essh/Repository/4N_Perceived%20Barriers%20to%20Timely_K%20Sakeena.pdf. Accessed 16 February 2020.
- 85. Razee H, van der Ploeg HP, Blignault I, et al. Beliefs, barriers, social support, and environmental influences related to diabetes risk behaviours among women with a history of gestational diabetes. Health Promot J Austr. 2010;21(2):130‐137. [DOI] [PubMed] [Google Scholar]
- 86. Zulfiqar T, Lithander FE, Banwell C, et al. Barriers to a healthy lifestyle post gestational‐diabetes: an Australian qualitative study. Women Birth. 2017;30(4):319‐324. [DOI] [PubMed] [Google Scholar]
- 87. Tewari A, Praveen D, Madhira P, et al. Feasibility of a lifestyle intervention program for prevention of diabetes among women with Prior gestational diabetes mellitus (LIVING study) in South Asia: a formative research study. Front Global Womens Health. 2020;1(21):1‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Mathew NP, Rao AP, Narayanan P. Barriers to postpartum follow‐up of mothers with gestational diabetes mellitus and its implications: a mixed method study. Int J Diabetes Dev Ctries. 2021;41(1):127‐135. [Google Scholar]
- 89. Sunny SH, Malhotra R, Ang SB, et al. Facilitators and barriers to post‐partum diabetes screening among mothers with a history of gestational diabetes mellitus‐a qualitative study from Singapore. Front Endocrinol (Lausanne). 2020;11:602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Kandasamy S, Nguyen L, Desai D, Anand SS, Sherifali D, de Souza RJ. Barriers to, and facilitators of, lifestyle changes to prevent gestational diabetes: an interpretive description of south Asian women and health‐care providers living and working in southern Ontario, Canada. Can J Diabetes. 2021;45(2):144‐154. [DOI] [PubMed] [Google Scholar]
- 91. Doran F, Davis K. Gestational diabetes mellitus in Tonga: insights from healthcare professionals and women who experienced gestational diabetes mellitus. N Z Med J. 2010;123(1326):59‐67. [PubMed] [Google Scholar]
- 92. Parsons J, Sparrow K, Ismail K, Hunt K, Rogers H, Forbes A. Experiences of gestational diabetes and gestational diabetes care: a focus group and interview study. BMC Pregnancy Childbirth. 2018;18(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Neufeld HT. Food perceptions and concerns of aboriginal women coping with gestational diabetes in Winnipeg, Manitoba. J Nutr Educ Behav. 2011;43(6):482‐491. [DOI] [PubMed] [Google Scholar]
- 94. Bandyopadhyay M, Small R, Davey MA, Oats JJ, Forster DA, Aylward A. Lived experience of gestational diabetes mellitus among immigrant south Asian women in Australia. Aust N Z J Obstet Gynaecol. 2011;51(4):360‐364. [DOI] [PubMed] [Google Scholar]
- 95. Boyd J, McMillan B, Easton K, Delaney B, Mitchell C. Utility of the COM‐B model in identifying facilitators and barriers to maintaining a healthy postnatal lifestyle following a diagnosis of gestational diabetes: a qualitative study. BMJ Open. 2020;10(8):e037318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Teh K, Quek IP, Tang WE. Postpartum dietary and physical activity‐related beliefs and behaviors among women with recent gestational diabetes mellitus: a qualitative study from Singapore. BMC Pregnancy Childbirth. 2021;21(1):612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Taylor C, Keim KS, Sparrer A, Van Delinder J, Parker S. Social and cultural barriers to diabetes prevention in Oklahoma American Indian women. Prev Chronic Dis. 2004;1(2):A06. [PMC free article] [PubMed] [Google Scholar]
- 98. Titmuss A, Davis EA, Brown A, Maple‐Brown LJ. Emerging diabetes and metabolic conditions among aboriginal and Torres Strait islander young people. Med J Aust. 2019;210(3):111‐113.e111. [DOI] [PubMed] [Google Scholar]
- 99. Maple‐Brown LJ, Graham S, McKee J, Wicklow B. Walking the path together: incorporating indigenous knowledge in diabetes research. Lancet Diabetes Endocrinol. 2020;8(7):559‐560. [DOI] [PubMed] [Google Scholar]
- 100. O'Mara‐Eves A, Brunton G, McDaid D, et al. Public Health Research. In: Community engagement to reduce inequalities in health: a systematic review, meta‐analysis and economic analysis. NIHR Journals Library. Copyright © Queen's Printer and Controller of HMSO 2013; 2013. [PubMed] [Google Scholar]
- 101. Cawley C, Buckenmeyer H, Jellison T, Rinaldi JB, Vartanian KB. Effect of a health system‐sponsored Mobile app on perinatal health behaviors: retrospective cohort study. JMIR Mhealth Uhealth. 2020;8(7):e17183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. O'Reilly SL, Laws R. Health‐e mums: evaluating a smartphone app design for diabetes prevention in women with previous gestational diabetes. Nutr Diet. 2019;76(5):507‐514. [DOI] [PubMed] [Google Scholar]
- 103. Potzel AL, Gar C, Banning F, et al. A novel smartphone app to change risk behaviors of women after gestational diabetes: a randomized controlled trial. PLoS ONE. 2022;17(4):e0267258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Ekezie W, Dallosso H, Saravanan P, Khunti K, Hadjiconstantinou M. Experiences of using a digital type 2 diabetes prevention application designed to support women with previous gestational diabetes. BMC Health Serv Res. 2021;21(1):772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Tinius R, Duchette C, Beasley S, Blankenship M, Schoenberg N. Obstetric patients and healthcare providers perspectives to inform Mobile app Design for Physical Activity and Weight Control during Pregnancy and postpartum in a rural setting. Int J Womens Health. 2021;13:405‐432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Agyemang C, van der Linden EL, Bennet L. Type 2 diabetes burden among migrants in Europe: unravelling the causal pathways. Diabetologia. 2021;64(12):2665‐2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Gagnon AJ, McDermott S, Rigol‐Chachamovich J, Bandyopadhyay M, Stray‐Pedersen B, Stewart D. International migration and gestational diabetes mellitus: a systematic review of the literature and meta‐analysis. Paediatr Perinat Epidemiol. 2011;25(6):575‐592. [DOI] [PubMed] [Google Scholar]
- 108. United Nations . International migrant stock. https://www.un.org/development/desa/pd/content/international‐migrant‐stock. Accessed 21 March 2022.
- 109. Watson H, Harrop D, Walton E, Young A, Soltani H. A systematic review of ethnic minority women's experiences of perinatal mental health conditions and services in Europe. PLoS ONE. 2019;14(1):e0210587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Fair F, Raben L, Watson H, Vivilaki V, van den Muijsenbergh M, Soltani H. Migrant women's experiences of pregnancy, childbirth and maternity care in European countries: a systematic review. PLoS ONE. 2020;15(2):e0228378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Gracey M, King M. Indigenous health part 1: determinants and disease patterns. Lancet. 2009;374(9683):65‐75. [DOI] [PubMed] [Google Scholar]
- 112. Browne AJ, Varcoe C, Lavoie J, et al. Enhancing health care equity with indigenous populations: evidence‐based strategies from an ethnographic study. BMC Health Serv Res. 2016;16(1):544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Sharma A, Birkeland KI, Nermoen I, et al. Understanding mechanisms behind unwanted health behaviours in Nordic and south Asian women and how they affect their gestational diabetes follow‐ups: a qualitative study. Diabet Med. 2021;38(10):e14651. [DOI] [PubMed] [Google Scholar]
- 114. Dragomanovich HM, Shubrook JH. Improving cultural humility and competency in diabetes care for primary care providers. Clin Diabet. 2021;39(2):220‐224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. MacKenzie L, Hatala A. Addressing culture within healthcare settings: the limits of cultural competence and the power of humility. Can Med Educ J. 2019;10(1):e124‐e127. [PMC free article] [PubMed] [Google Scholar]
- 116. Abouzeid M, Bhopal RS, Dunbar JA, Janus ED. The potential for measuring ethnicity and health in a multicultural milieu‐‐the case of type 2 diabetes in Australia. Ethn Health. 2014;19(4):424‐439. [DOI] [PubMed] [Google Scholar]
- 117. Pham TTL, Berecki‐Gisolf J, Clapperton A, O'Brien KS, Liu S, Gibson K. Definitions of culturally and linguistically diverse (CALD): a literature review of epidemiological research in Australia. Int J Environ Res Public Health. 2021;18(2):737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Balaam M‐C, Haith‐Cooper M, Pařízková A, et al. A concept analysis of the term migrant women in the context of pregnancy. Int J Nurs Pract. 2017;23(6):e12600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Australian Bureau of Statistics (ABS) standards for statistics on cultural and language diversity. 1999. https://www.abs.gov.au/ausstats/abs@.nsf/0/79fab04272992d54ca25697e0018febd/$FILE/ATT41EIH/DIMA%20Guide_Final.pdf. Accessed 21 March 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1


