Abstract
Obstetricians know the statistics: one out of every 10 babies is born premature, preeclampsia affects one in 25 pregnant people, the United States has the highest rate of maternal mortality in the developed world. Yet, physicians and scientists still do not fully understand the biology of normal pregnancy, let alone what causes these complications. Obstetrics and gynecology-trained physician-scientists are uniquely positioned to fill critical knowledge gaps by addressing clinically-relevant problems through fundamental research and interpreting insights from basic and translational studies in the clinical context. Within our specialty, however, physician-scientists are relatively uncommon. Inadequate guidance, lack of support and community, and structural barriers deter fellows and early stage faculty from pursuing the physician-scientist track. One approach to help cultivate the next generation of physician-scientists in obstetrics and gynecology is to demystify the process and address common barriers that contribute to the attrition of early stage investigators. Here, we review major challenges and propose potential pathways forward in the areas of mentorship, obtaining protected research time and resources, and ensuring diversity, equity, and inclusion, from our perspective as early stage investigators in maternal-fetal medicine. We discuss the roles of early stage investigators and leaders at the institutional and national level in the collective effort to retain and grow our physician-scientist workforce. We aim to provide a framework for early stage investigators initiating their research careers and a starting point for discussion with academic stakeholders. We cannot afford to lose the valuable contributions of talented individuals due to modifiable factors or forfeit our voices as advocates for issues that impact pregnant populations.
Keywords: bias; career development; DEI; diversity, equity, inclusion; early stage investigator; ESI; mentee; mentorship; motherhood penalty; NIH; physician-scientist; pipeline; training grants; translational science; underrepresented in medicine; URM
Introduction
Adverse pregnancy-related outcomes are rising in the United States. One in 10 infants is born preterm.1 Hypertensive disorders of pregnancy are diagnosed in ~9% of birthing people, which amounts to >300,000 affected pregnancies per year.2 Disturbingly, the U.S. maternal mortality rate is not improving, and exceeds that of most developed countries.3,4 These concerning trends in reproductive health outcomes affect individuals across all communities and sociodemographic backgrounds, but disproportionately impact Black and Indigenous people, who are 2 to 3 times more likely to die from pregnancy-related causes than white individuals. Despite the urgent need to address these longstanding issues, we have failed to materially improve reproductive health outcomes owing largely to: 1) gaps in our understanding of normal pregnancy biology and disease mechanisms, and 2) underinvestment in women’s health research.5 Failure to prioritize basic and translational research in obstetrics jeopardizes our ability to develop effective preventive, diagnostic, and therapeutic strategies for pregnancy complications and to reverse trends in adverse outcomes.
Physician-scientists trained in obstetrics and gynecology are positioned to understand and address unmet needs in women’s health and reproductive biology. Those who pursue subspecialty training have an opportunity to focus on building their research interests and career beginning in the fellowship years. Subspecialty training coupled with scientific rigor, knowledge of biology, and advanced methods provides the foundation for the clinical translation of bench discoveries. Researchers with advanced training in population health and epidemiology are also needed. Yet, the pathway to recruit and support obstetrics and gynecology-trained physician-scientists remains ill-defined and poorly supported.
The total number of early stage investigators in obstetrics and gynecology is unclear, however, available data suggest a relative dearth of scientists in the field. National Institutes of Health (NIH) data, for example, show that departments of obstetrics and gynecology receive far fewer career development awards than all of the other major specialties (Figure 1, A).6 Furthermore, numbers of obstetrics and gynecology K08 and K23 awardees have remained modest and largely unchanged over the past decade (Figure 1, B). While fast-tracked physician-scientist training programs are well established in internal medicine and pediatrics, similar tracks do not exist in obstetrics and gynecology. This may be one reason that so few U.S. MD-PhD graduates pursue postgraduate training in obstetrics and gynecology compared with other major specialties (Figure 1, C).7,8 The fraction of MD-PhD fellows in obstetrics and gynecology subspecialties is also relatively small. In 2019, for instance, 6% of maternal-fetal medicine (MFM) fellows were MD-PhDs compared with 14% of hematology/oncology fellows.7 These surrogate estimates are limited in that they do not include the other funding mechanisms for early stage investigators, and MD-PhD data do not capture all physician-scientists nor do all MD-PhDs pursue a research career. Still, these data reveal a need to prioritize the development of early stage investigators within obstetrics and gynecology departments, which receive less than 1% of NIH funding overall.9 There has indeed been a renewed call to support the “endangered physician-scientist” at the national level,10 and efforts in our field to expand the perinatal biology physician-scientist workforce.11 Nevertheless, more work is needed to recruit and retain the next generation of researchers.
FIGURE 1: Dearth of early career physician-scientists in obstetrics and gynecology.
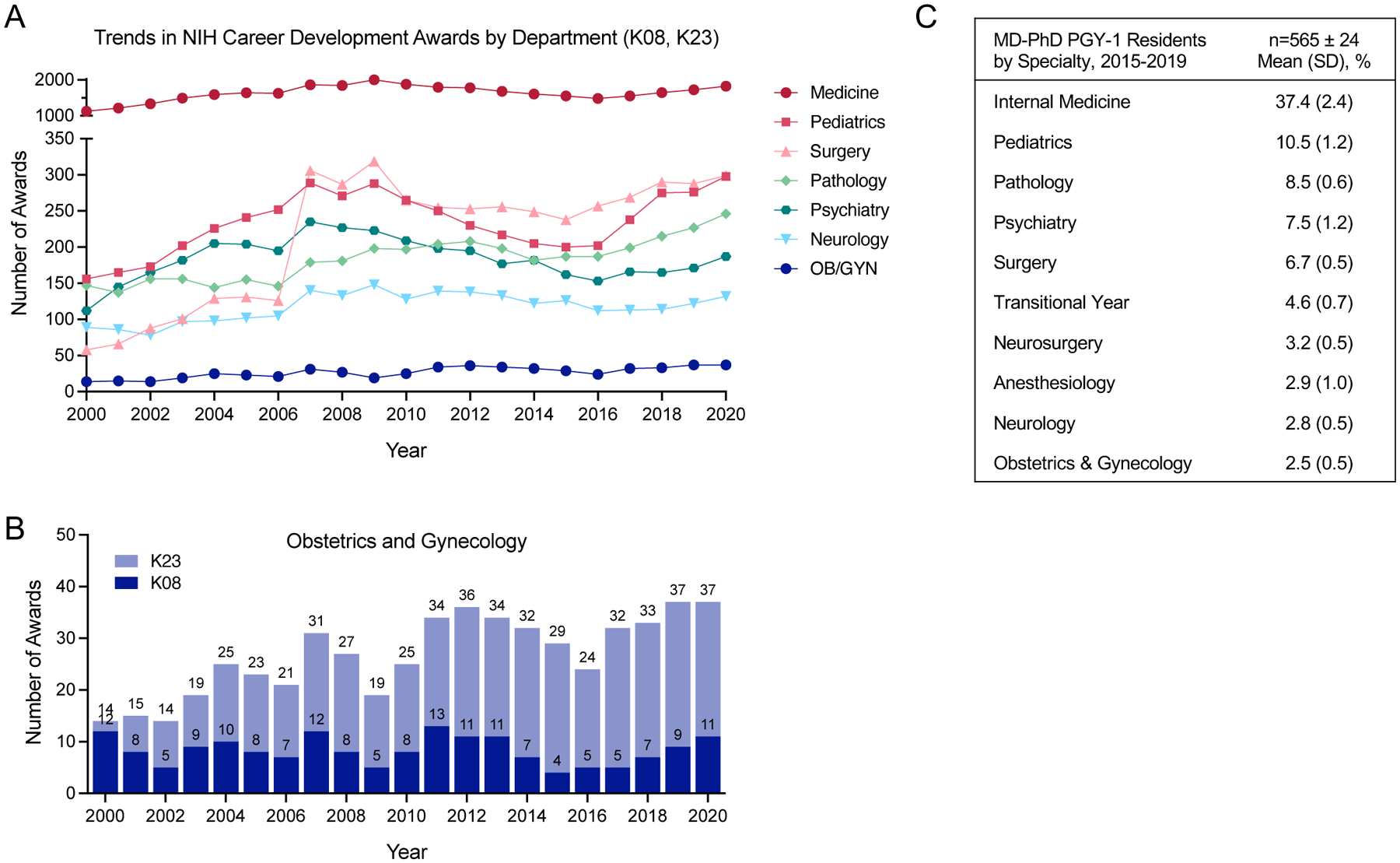
A, Trend in number of NIH career development grants (K08, K23) awarded to departments from 2000 to 2020. Source: NIH RePORTER.6 B, Number of K08 and K23 grants awarded to obstetrics and gynecology departments. C, Top 10 residencies entered by MD-PhD graduates. Transitional year includes a mix of specialties. Data from the Association of American Medical Colleges.7
NIH, National Institutes of Health; OB/GYN, Obstetrics and Gynecology; PGY, postgraduate year.
Here, we describe the challenges facing early stage investigators from our perspective as maternal-fetal medicine physician-scientists. We identify major areas for early stage investigators and obstetrics and gynecology leaders to consider and address when investing in a research career: mentorship; protected research time and resources; and diversity, equity, and inclusion (DEI; Figure 2). Our objectives are to voice the perspectives of early stage investigators and to optimize the academic environment to enable their success, given that the future of our field depends on a robust physician-scientist workforce. We anticipate that many of the themes presented will resonate broadly, but acknowledge that this commentary cannot fully address the experiences and specific issues germane to other subspecialties, in particular the heavily surgical subspecialties, gynecologic oncology, female pelvic medicine and reconstructive surgery, and minimally-invasive gynecologic surgery, which have their own set of unique concerns.12 Although we focus on the needs of lab-based researchers here, supporting early stage investigators on the clinical research track is an equally important goal, and much of the discussion will apply to them as well.
Figure 2: Foundations for growing and sustaining early stage investigators.
Artist: Vipanchi Mungara.
For MFM fellows and junior faculty interested in a research-focused career, figuring out how to get started is the first hurdle. Early stage investigators rely on support and guidance from others, but are ultimately responsible for navigating their own careers. In Table 1, we provide a reference for early stage investigators – the checklist we wish we had. Ideas for how department leaders, institutions, professional organizations, and the NIH can support early stage investigators are presented in Table 2.
Table 1:
Early Stage Investigator Guide
| Fellowship and Transition to Faculty |
|---|
|
| Early Faculty (Years 1–2) |
|
AAOGF, American Association for Obstetrics and Gynecology Foundation; ABOG, American Board of Obstetrics and Gynecology; ADA, American Diabetes Association; AHA, American Heart Association; BIRCWH, Building Interdisciplinary Research Careers in Women’s Health; BWF, Burroughs Wellcome Fund; CTSA, Clinical and Translational Science Awards; CTSI, Clinical and Translational Science Institute; ESI, early stage investigator; MOD, March of Dimes; NIH, National Institutes of Health; SMFM, Society for Maternal-Fetal Medicine; WRHR, Women’s Reproductive Health Research.
Table 2:
Ways That Leaders and Organizations Can Support ESIs
| Mentorship | Protected Time and Resources | Diversity, Equity and Inclusion | |
|---|---|---|---|
| Department Leaders and Institutions |
|
|
|
| Professional Organizations |
|
|
|
| NIH |
|
|
|
DEI, diversity, equity and inclusion; NIH, National Institutes of Health; SRI, Society for Reproductive Investigation; URM, underrepresented in medicine.
I. Mentorship
Mentors are essential for navigating an individualized route to success and setting expectations. Effective mentors provide constructive feedback and insight, accelerate professional growth, and help the mentee build a quality research portfolio that complements their clinical interests.13,14 Mentorship teams (also known as “launch” teams) oversee career development, meet regularly with the mentee to ensure that career milestones are met (typically 2–4 times per year), identify opportunities for professional advancement, and serve as advocates when barriers are encountered. Each mentor plays a distinct role in an early stage investigator’s development into a confident and productive physician-scientist. Research mentors provide intellectual input, constructive feedback, practical guidance, and resources. Career mentors help early stage investigators strategize, define career goals, and prioritize opportunities. Peer mentors are incredibly important sources of support and advice; having a peer group at a similar career and life stage is invaluable at every career stage. The roles of different mentors often overlap, and any given individual’s team will look different.
Finding mentors at your institution
Assembling a mentor team may be challenging if the department lacks senior mentors or if the early stage investigator is moving to a new institution. Access to experienced mentors is extremely important.13,15 When interviewing for a position at a new institution, it is imperative that early stage investigators identify potential mentors in advance, especially research mentors who often serve as the primary mentor on the mentorship team. Prospective mentors can be identified through online investigation, publications, referrals from faculty and department leaders, and formal mentorship programs. Meeting multiple people is worth the effort, as finding the right mentors is critical. Poor mentors can exhibit dysfunctional or passive-aggressive behaviors that put a mentee’s academic career at risk (this has been referred to as “mentorship malpractice”).16 Department leaders, institutions, professional organizations, and the NIH can help foster productive mentor/mentee relationships and support good mentors (Table 2).
Obstetrics and gynecology department leaders play an important role in connecting early stage investigators with established mentors and assembling a diverse team to meet the needs of the early stage investigator. Mentors should have commensurate experience, a track record of NIH or NIH-equivalent funding, and be willing to mentor and sponsor. Distinct from the advisory role of a mentor, a sponsor uses their connections and status to create opportunities for early stage investigators that they otherwise would not have access to on their own.17 Early stage investigators need both. Chairs can consider working with established physician-scientist training programs in other fields to identify training opportunities, as these programs often provide an outstanding peer and research mentor network and frequently host seminars on useful topics, such as university resources (e.g. statistical support, core facilities, grant units, etc.), academic promotions, and work-life balance. Encouraging and supporting early stage investigators to attend grant writing seminars can provide peer support and exposure to mentors who can provide feedback on grant proposals.
Institution and society leaders – with support from the NIH when applicable – can incentivize mentorship by: 1) providing time and salary support for mentorship activities; 2) encouraging and supporting formal mentorship training; and 3) rewarding outstanding mentors for their contributions. Recognition of mentors who are identified by their mentees as outstanding and those who have successfully mentored early stage investigators to independence is an important mechanism for identifying good mentors. Additional ideas for supporting mentorship are summarized in Table 2.
Due to the relative dearth of physician-scientists in obstetrics and gynecology, effective mentors may reside in other departments. Assigning mentors solely based on their position within the obstetrics and gynecology department or on objective successes (e.g. grants and publications) may be a disservice to the early stage investigator if the mentor is a poor fit scientifically or personally. For research mentorship, we all found mentors outside of our departments. Hybrid mentorship with one co-mentor in obstetrics and gynecology and the other outside of the department can also work well. This broad approach can be encouraged by department and institution leaders to increase collaboration and innovation, expand skill sets, improve the science, and accelerate discovery.
Expanding your network
Mentorship need not occur within the confines of an organization or practice. As we have learned during the COVID-19 pandemic, videoconferencing technology removes geographic barriers and fosters connections beyond traditional boundaries, including across disciplines and continents. Connections with mentors and peers at other institutions are often facilitated by career development program retreats, national meetings, mutual colleagues, and social media networks (e.g. Twitter). An external mentor and peer support group can provide a valuable outsider’s perspective, particularly when institutional problems arise or when trying to assess whether one is on track to accomplish their career goals.
The role of the mentee
Building positive and productive mentorship relationships starts with the mentee. Mentees must take responsibility for their role in the collaborative alliance and guide the mentor’s efforts to promote a mutually beneficial working relationship.15,18 An upfront discussion about the role and commitment of the mentor can help ensure that expectations and goals are clear and agreed upon from the start, while recognizing that a mentor’s role might evolve over time.15 Additionally, mentees should take the lead by setting up regular meetings with clear agendas and plans for follow up. Early stage investigators who approach mentorship proactively and positively are more likely to develop durable and satisfying relationships with mentors.18 Commitment, adaptability, honest and open lines of communication, and drive are paramount to a successful mentor-mentee relationship. With this foundation, mentees can move forward confidently, knowing their mentors will be there to celebrate their successes and provide honest constructive guidance through disappointments.
II. Protected Research Time and Resources
In the early career phase, protected research time is essential. Many career development awards require at least 75% protected research time, although some NIH institute policies have recently changed and are allowing for a reduction in research time to 50% for the specific purpose of maintaining specialty clinical competency skills in specific surgical subspecialties.19 While this is likely less of an issue in MFM, the flexibility in research effort may be beneficial for researchers in heavily surgical subspecialties, such as gynecologic oncology and female pelvic medicine and reconstructive surgery. Regardless, early stage investigators require a substantial amount of protected research time to actively engage in their research and career development. The notion that early stage investigators can generate data and obtain funding without significant protected research time fails to recognize the time investment required for research training, data collection and analysis, writing, and the development of new ideas.
For protected research time to be truly protected, department leaders must clearly specify their expectations for clinical coverage (Table 2). Contracts that define the number of clinical days and outline the schedule are useful given that percentage-based contracts are inherently nebulous – flexibility in the denominator means that “75% protected research time” will look different for different people. Leaders can recognize the various forms of clinical work (clinic, inpatient service, in-house and home call) and count all of it towards clinical time. It is important to avoid “clinical creep,” additional clinical time that encroaches on protected research time. The assumption that researchers are “available” on research days is incorrect.
Departments and institutions must be committed to research and have the financial resources to hire and properly support early stage investigators. A major challenge encountered when transitioning from fellowship to the first faculty position is identifying institutions with the infrastructure, finances, and desire to invest in nascent research careers. Starting the search for potential opportunities early is advisable. Investigating programs with institutional K awards is a good start (Table 1). Note that these positions are limited and have specific application cycles, thus timing may dictate which opportunities are available. Additionally, personal factors, such as proximity to family and a partner’s job, may further limit the scope of a job search. Coming to terms with these realities will help early stage investigators strategize and decide what is most important to them and what they are willing to sacrifice to pursue a research career.
Understanding the cost of research and science
Research is expensive and it is critical for early stage investigators and department chairs to understand the cost of doing science. Consumables alone, for instance, might cost $20,000 to 30,000 per person per year, and a mouse colony of 200 can cost $55,000 per year.20 While career development awards may provide some funds for direct research costs, these alone are not sufficient as they typically do not cover equipment purchases, personnel or other technical help, or finance discovery biology.
Between 1995 and 2005, the median start-up package for physician-scientists was $710,000.21 Current start-up packages to support early stage investigators in medicine subspecialties are likely more in the range of $750,000 to $1,000,000 for the first 3 years (personal communication). The source of start-up funds will vary at different institutions. For example, the department may support a portion of a start-up package with the remainder financed by the medical school. This type of arrangement requires advanced planning and collaborative negotiation. While department chairs may not have unilateral authority to allocate start-up funds, chairs who want to prioritize the development of early stage investigators can learn how physician-scientists are developed in other fields and know the typical value of start-up packages and ways to finance them (Table 2). Support from department and institution leaders is key. We cannot expect early stage investigators in obstetrics and gynecology to succeed with fewer resources than those in other fields. This investment is especially important in the context of an unfavorable funding environment; the success rate for NIH grant applications decreased from 33% in 2000 to 22% in 2020.22 National societies can also help by developing workshops and educational resources for chairs and trainees.
Maximizing fellowship time to develop a research niche and apply for funding
Motivated early stage investigators can be encouraged to collect preliminary data during fellowship to be strongly positioned for career development awards. Trainees with an early interest in research should seek fellowships with research time structured in blocks of protected research time or tailored to the needs of the fellow and their project. Ask specifically about the support of protected research time and schedule flexibility during fellowship interviews. For those pursuing basic science projects, a protected year of research to generate preliminary data is extremely helpful compared with staggered short blocks which impede research momentum. Similar support may be needed for fellows pursuing clinical research. In addition to thoughtful scheduling, statistical support and other resources help to ensure feasibility and accurate interpretation as fellows build their research skills.
Several obstetrics and gynecology-specific programs support budding physician-scientists (Table 1). Early stage investigators can consider applying for career development grants prior to starting a faculty position, for example during the second year of fellowship. This may be in the form of an award to the individual (which is often transferrable between institutions), or by seeking institutions with openings in their institutional K programs during the job search as noted above (e.g. KL2/Clinical and Translational Science Award program, Women’s Reproductive Health Research [WRHR], and Building Interdisciplinary Research Careers in Women’s Health [BIRCWH]). Foundation grants and other seed funding opportunities should also be investigated. Examples include the American Heart Association, Thrasher Research Fund, Doris Duke Charitable Foundation, American College of Obstetricians and Gynecologists (ACOG), and Preeclampsia Foundation (Table 1). Websites for organizations such as ACOG and the Foundation for SMFM (Society for Maternal-Fetal Medicine) are good resources.23,24 Even if not funded, the experience of writing a grant and going through the review process supports growth, hones research ideas, and demonstrates commitment. If an early stage investigator is transitioning to a new institution, they should strongly consider investigating transfer options for funding or applying for institutional K awards, determine whether the new institution will be able to support their current work, and try to identify mentors at the new location prior to arrival through the help of the chair and others.
While career development awards have served an important role in the development of early stage investigators in obstetrics and gynecology, the number of awards is limited and it is unrealistic to expect all early stage investigators to have secured funding prior to starting their first faculty position. Furthermore, as previously mentioned, career development awards do not sufficiently cover research expenses and typically cannot be used for indirect costs or salary support for mentors. Therefore, department chairs and institutions must be willing to make an investment up front. This may include finding ways to provide protected research time to support an early stage investigator’s application for a career development award, recognizing that 3 years is a typical time frame needed to obtain K funding (i.e. 1 year of protected research time is insufficient).
Equitable pay for physician-scientists
As a result of decreased clinical activity, physician-scientist faculty often accept pay inequity despite assuming many roles crucial to the academic mission of the department and institution. Unlike other fields that produce more physician-scientists, such as internal medicine and pediatrics, the pay differential between research-focused and clinical obstetrics and gynecology faculty can be substantial depending on compensation structure and productivity metrics, which vary by institution. This difference in earning potential can be a significant disincentive for obstetrics and gynecology early stage investigators. While they cannot expect to have the same earning potential as full-time clinical faculty, compensation for early stage investigators can be commensurate with the value they bring to the department. Besides securing grant dollars, physician-scientists enrich the intellectual environment, contribute to the academic productivity of the department, lead and initiate innovative collaborations, provide content expertise, perform administrative and committee work, mentor trainees and peers, and serve as role models for other obstetrician and gynecologists pursuing research careers.
One approach is the adoption of base pay equity upon hiring of faculty at the Assistant Professor level regardless of their focus or track, with incentive pay based on productivity. Instead of revenue value units (RVUs), productivity metrics for physician-scientists might include publications, service (e.g. leadership roles and mentorship), and research funding. Another potential strategy is paying researchers a blended salary based on research effort at the NIH cap and clinical effort at the clinical rate. Regardless of the approach, transparency is critical for ensuring that colleagues perceive fair treatment and feel they are valued for their individual contributions. Chairs can be clear and consistent about the different roles and responsibilities of faculty on different tracks and how work is compensated. Structured compensation plans can also reduce salary gaps related to gender and race/ethnicity.25–27
III. Diversity, Equity, and Inclusion (DEI)
Greater attention has been given to DEI efforts as evidence of pervasive biases, harassment, and structural oppression of people of color that has become a focal point of societal discourse.28,29 In academic medicine, these behaviors and systemic inequities are particularly detrimental to the careers and morale of underrepresented racial/ethnic and gender groups,30 and threaten the recruitment and retention of a diverse and representative workforce, including early stage investigators.31 Such a workforce is essential for the provision of culturally competent care, reducing disparate health outcomes, ensuring equitable and safe learning and working environments, and for scientific novelty and innovation.32–37 This is particularly important in the field of obstetrics and gynecology where persistent inequities in representation, compensation, academic advancement, and health outcomes exist.12,38,39
In this section, we focus on a few salient DEI issues that impact the development and retention of early stage investigators in obstetrics and gynecology. We use “underrepresented in medicine” to refer broadly to groups and people with intersectional identities who are impacted by systemic racism, bias, and discrimination, including underrepresented racial/ethnic groups, people who identify as women or transgender, members of the LGBTQ+ community, people with disabilities, and others. Although women are not underrepresented in obstetrics and gynecology as a whole, they remain disadvantaged and occupy a minority of leadership positions.12
Establishing a peer support network
Finding peers who know the specific challenges facing early stage investigators who are underrepresented in medicine is worth the effort. Peer support is incredibly important for validating experiences and understanding the systems issues that stem from a lack of representation and contribute to the devaluation of underrepresented faculty (Table 1).37,40 Early stage investigators who experience discrimination commonly suffer from isolation, imposter syndrome, and self-blame.30 Listening to and believing their experiences is an important first step to move beyond recognition of the problem to developing a path forward, and peer networks can be a safe and invaluable source of authentic and non-judgmental support.
Early stage investigators can ask other researchers who identify as underrepresented in medicine about their experiences and strategies for overcoming barriers. Leaders and other faculty can facilitate connections with peers and mentors within or outside of the institution. Many institutions also have an Office of Diversity, Equity, and Inclusion, which may be a good starting point. While conferences have traditionally been a good venue for networking, the popularity of social media groups and virtual networking during the COVID-19 pandemic have expanded the possibilities; if the desired peer group does not yet exist, it can be created. Social media has emerged as an important and effective mechanism for professional networking.41,42
Ensuring equitable compensation and opportunity
Inequities in compensation and opportunity for underrepresented in medicine faculty are well documented. Data show that women and faculty belonging to underrepresented racial/ethnic groups are systematically underpaid12,43–46 and less likely to be promoted.46,47 These differences in opportunity and support are present starting from the early career stage. For example, Black, Indigenous, and Latinx medical graduates are less likely to receive a K award, due in part to differences in research-related opportunities.48 In a recent survey study of K awardees, women were more likely than men to report concerns about access to resources, clinical work load, and unfair treatment.49 Women were also less likely to be sponsored, and even among sponsored early stage investigators, were less successful than their male counterparts.17 For researchers with intersectional identities, these disadvantages are likely magnified. Attention to structural changes to promote equitable allocation of resources and opportunities and a commitment to an inclusive culture are needed.
One way early stage investigators are derailed from achieving their research and career goals is through the guise of academic opportunity. Uncompensated work-related duties that contribute to the organization but are less likely to contribute to career advancement (known as “citizenship tasks”) are shouldered primarily by women in academic medicine, and women of color are more likely to feel obligated to volunteer for such tasks.50 Underrepresented faculty also carry the burden of extra responsibilities placed on them because of their racial/ethnic or gender identity, including mentoring of underrepresented trainees and diversity efforts.46 Framing the work as “voluntary” centers the problem on the person doing the work, when in reality, many external and internal factors create an environment in which faculty feel they cannot say “no” due to their identity. Appointing a Black woman faculty member to an uncompensated DEI task force position is one example of this.30,51 Mentors can help early stage investigators select opportunities that advance their primary research and career goals (strategic yes). In certain situations, mentors may also help by declining opportunities on their mentee’s behalf if the mentee feels undue pressure to take on a new commitment that does not align with their mission and career strategy.
How to support early stage investigators with caregiving responsibilities
The impact of familial responsibilities, especially on women, during the critical early faculty years cannot be overstated. The COVID-19 pandemic has shined a light on these challenges.52 The factor that most influenced research productivity during the pandemic was having a dependent aged 5 or younger, while being a woman and having work that involves bench science also negatively affected productivity.53
The early career phase inevitably overlaps with birthing and raising young children. Thus, many early stage investigators will experience maternal discrimination (also known as the “motherhood penalty”). Physician mothers have reported: 1) gendered performance expectations (either higher standards to prove their commitment and competence, or lower standards with colleagues assuming that mothers were not interested or able to assume new tasks or leadership roles); 2) limited opportunities for advancement (e.g. being excluded from decision making, being passed over for leadership positions, or having contracts grossly modified in response to pregnancy or after returning from maternity leave); 3) financial inequalities (e.g. receiving a lower salary than colleagues with comparable or less experience, taking on uncompensated work, and being required to “make up” leave time); 4) lack of support during pregnancy and postpartum (e.g. being asked to forego leave to which they were entitled); and 5) challenging work-life balance.54 Structural changes to eliminate maternal discrimination include unequivocal support and protection during maternity leave, expanding childcare options, and increasing flexibility in work hours (Table 2).55
Institutions can support faculty with caregiving responsibilities by improving paid parental and family medical leave.56 Institutions can also offer and encourage use of parental leave for partners, a change that is not only practical but also may help shift gender norms around caregiving. Promotion and tenure committees can recognize and expect that major life events will have a substantial impact on research and career momentum.57 Appropriately, the NIH extends early stage investigator status to account for childbearing.58 Although we have focused the discussion on parental leave, other circumstances, including caring for an ill parent or grieving (such as the loss of a loved one or a pregnancy), in our opinion deserve the same accommodation without penalty. We cannot afford to lose more early stage investigators who would have succeeded if provided the right support and environment.5
A call to action: Addressing systemic racism, sexism, and bias
While many have expressed their commitment to workforce diversification and programs to eliminate racism, sexism, and bias, this intention must coincide with action. Department leaders must address specific challenges affecting underrepresented in medicine faculty, which include and extend beyond the challenges noted above. This begins with acknowledging the pervasiveness of discrimination and inequity of opportunity in academic medicine. Institutions and chairs need to act with the awareness that structural changes – rather than individual adaptation to the current system – will enable more early stage investigators to meet academic benchmarks required for tenure and promotion.57,59 Institutions, professional organizations, and the NIH must prioritize DEI efforts and implement bold action plans to address systemic racism, sexism, and bias through research and policy reform.60–62 Sponsors, including the NIH, also need to address funding disparities.63,64 The depth of this problem was exemplified in a recent study that found that underrepresented in medicine scientists were more likely to submit grants with terms such as “health disparities, disease prevention and intervention, and socioeconomic factors,” resulting in a 21% reduction in funding success.65
IV: Investing in physician-scientists in obstetrics and gynecology
There is a need for an obstetrics and gynecology physician-scientist workforce that will diversify ideas, break down silos, and bridge gaps between clinical and basic science researchers. While the training grant mechanisms specific to reproductive health research have been critical to the success of many early stage investigators, additional support and reform are needed. Intentional sponsorship of early stage investigators through strong mentorship teams, protected research time, start-up resources, and support to overcome unique challenges related to an early stage investigator’s identity or major life events will encourage a new generation of physician-scientists in our field. Efforts to diversify the physician-scientist workforce and address disparities in recruitment and retention of early stage investigators who are underrepresented in medicine are critical for long term research excellence in our field. We anticipate that by building a critical mass of up-and-coming researchers poised to tackle longstanding clinical questions in our specialty, we can have a significant impact on the health, wellbeing and lifespan of our patients.
Acknowledgments:
We are grateful for support from the Womxn’s Health Collaborative. Special thanks to Drs. Michal Elovitz and Geeta Swamy for critical reading of the manuscript. We wish to acknowledge the Foundation for the Society for Maternal-Fetal Medicine, American Association of Obstetricians and Gynecologists Foundation, Reproductive Scientist Development Program, Eunice Kennedy Shriver National Institute of Child Health and Human Development, and American College of Obstetricians and Gynecologists for their funding and support. We would also like to thank the artist, Vipanchi Mungara, an incoming Biological Sciences major at UC Irvine, for her work in Figure 2.
Funding:
Drs. Parchem and Townsel are recipients of the Foundation for the Society for Maternal-Fetal Medicine/American Association of Obstetricians and Gynecologists Foundation Scholar Award. Drs. Afshar and Wernimont are supported by the Reproductive Scientist Development Program (RSDP) by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K12 HD000849) and the American College of Obstetricians and Gynecologists, as part of the RSDP.
Footnotes
Disclosures: The authors report no conflict of interest.
References
- 1.Martin JA, Hamilton BE, Osterman MJK. Births in the United States, 2019. NCHS Data Brief 2020;(387):1–8. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention: Data on Selected Pregnancy Complications in the United States. Available at: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-complications-data.htm#hyper. Accessed April 29, 2021.
- 3.Centers for Disease Control and Prevention: Pregnancy Mortality Surveillance System. Available at: https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm. Accessed May 6, 2021.
- 4.Gravitz L. The United States is failing its mothers. Nature 2017;550(7674):S20–S23.. [DOI] [PubMed] [Google Scholar]
- 5.Spong CY. Addressing inequalities in women’s health research. Contemporary OB/GYN 2020. Available at: https://www.contemporaryobgyn.net/view/addressing-inequalities-in-women-s-health-research. Accessed August 16, 2020.
- 6.NIH RePORTER. Available at: https://reporter.nih.gov/. Accessed September 3, 2021.
- 7.AAMC Report on Residents. Available at: https://www.aamc.org/data-reports/students-residents/report/report-residents. Accessed September 3, 2021.
- 8.Brass LF, Akabas MH. The national MD-PhD program outcomes study: Relationships between medical specialty, training duration, research effort, and career paths. JCI Insight 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rice LW, Cedars MI, Sadovsky Y, Siddiqui NY, Teal SB, Wright JD, et al. Increasing NIH funding for academic departments of obstetrics and gynecology: a call to action. Am J Obstet Gynecol 2020;223(1):79.e1–79.e8. [DOI] [PubMed] [Google Scholar]
- 10.Jain MK, Cheung VG, Utz PJ, Kobilka BK, Yamada T, Lefkowitz R. Saving the Endangered Physician-Scientist - A Plan for Accelerating Medical Breakthroughs. N Engl J Med 2019;381(5):399–402. [DOI] [PubMed] [Google Scholar]
- 11.Society for Maternal-Fetal Medicine, Sadovsky Y, Caughey AB, DiVito M, D’Alton ME, Murtha AP, et al. Research to knowledge: promoting the training of physician-scientists in the biology of pregnancy. Am J Obstet Gynecol 2018;218(1):B9–B13. [DOI] [PubMed] [Google Scholar]
- 12.Heisler CA, Mark K, Ton J, Miller P, Temkin SM. Has a critical mass of women resulted in gender equity in gynecologic surgery? Am J Obstet Gynecol 2020;223(5):665–673. [DOI] [PubMed] [Google Scholar]
- 13.Liénard JF, Achakulvisut T, Acuna DE, David SV. Intellectual synthesis in mentorship determines success in academic careers. Nat Commun 2018;9(1):4840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salata RA, Geraci MW, Rockey DC, Blanchard M, Brown NJ, Cardinal LJ, et al. U.S. Physician-Scientist Workforce in the 21st Century: Recommendations to Attract and Sustain the Pipeline. Acad. Med 2018;93(4):565–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sarabipour S, Hainer SJ, Arslan FN, de Winde CM, Furlong E, Bielczyk N, et al. Building and sustaining mentor interactions as a mentee. FEBS J 2021. doi: 10.1111/febs.15823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chopra V, Edelson DP, Saint S. Mentorship Malpractice. JAMA 2016;315(14):1453–1454. [DOI] [PubMed] [Google Scholar]
- 17.Patton EW, Griffith KA, Jones RD, Stewart A, Ubel PA, Jagsi R. Differences in Mentor-Mentee Sponsorship in Male vs Female Recipients of National Institutes of Health Grants. JAMA Intern Med 2017;177(4):580–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zerzan JT, Hess R, Schur E, Phillips RS, Rigotti N. Making the most of mentors: a guide for mentees. Acad Med 2009;84(1):140–144. [DOI] [PubMed] [Google Scholar]
- 19.NOT-HL-21–003: Updated NHLBI Guidance Concerning Mentored Career Development (K08 and K23) Awards: Percent Effort. Available at: https://grants.nih.gov/grants/guide/notice-files/NOT-HL-21-003.html. Accessed July 17, 2021.
- 20.What does it cost to run an academic lab? Available at: https://www.biolegend.com/en-us/blog/what-does-it-cost-to-run-an-academic-lab. Accessed May 6, 2021.
- 21.Academic Tenure-Track Offer Letters | Burroughs Wellcome Fund. Available at: https://www.bwfund.org/career-tools/academic-tenure-track-offer-letters. Accessed October 14, 2020.
- 22.NIH Data Book - Research Grants. Available at: https://report.nih.gov/nihdatabook/category/6. Accessed October 15, 2020.
- 23.Non-Federal Sources for Research Funding | ACOG. Available at: https://www.acog.org/education-and-events/creog/curriculum-resources/non-federal-sources-for-research-funding. Accessed July 17, 2021.
- 24.Foundation for SMFM Programs. Available at: https://foundationforsmfm.org/programs. Accessed July 17, 2021.
- 25.Mello JA. Why the Equal Pay Act and Laws Which Prohibit Salary Inquiries of Job Applicants Can Not Adequately Address Gender-Based Pay Inequity. Sage Open 2019;9(3):215824401986910. [Google Scholar]
- 26.Hayes SN, Noseworthy JH, Farrugia G. A Structured Compensation Plan Results in Equitable Physician Compensation: A Single-Center Analysis. Mayo Clin Proc 2020;95(1):35–43. [DOI] [PubMed] [Google Scholar]
- 27.Does Pay Transparency Close the Gender Wage Gap? PayScale. Available at: https://www.payscale.com/data/pay-transparency. Accessed October 21, 2020.
- 28.Grubbs V. Diversity, equity, and inclusion that matter. N Engl J Med 2020;383(4):e25. [DOI] [PubMed] [Google Scholar]
- 29.Morse M, Loscalzo J. Creating Real Change at Academic Medical Centers - How Social Movements Can Be Timely Catalysts. N Engl J Med 2020;383(3):199–201. [DOI] [PubMed] [Google Scholar]
- 30.Doll KM, Thomas CR. Structural Solutions for the Rarest of the Rare - Underrepresented-Minority Faculty in Medical Subspecialties. N Engl J Med 2020;383(3):283–285. [DOI] [PubMed] [Google Scholar]
- 31.Lett LA, Orji WU, Sebro R. Declining racial and ethnic representation in clinical academic medicine: A longitudinal study of 16 US medical specialties. PLoS One 2018;13(11):e0207274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ruzycki SM, Franceschet S, Brown A. Making medical leadership more diverse. BMJ 2021;373:n945. [DOI] [PubMed] [Google Scholar]
- 33.Marrast L, Zallman L, Woolhandler S, Bor DH, McCormick D. Minority Physicians’ Role in the Care of Underserved Patients: Diversifying the Physician Workforce May Be Key in Addressing Health Disparities. JAMA Intern Med 2014;174(2):289–291. [DOI] [PubMed] [Google Scholar]
- 34.Greenwood BN, Hardeman RR, Huang L, Sojourner A. Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc Natl Acad Sci 2020;117(35):21194–21200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Greenwood BN, Carnahan S, Huang L. Patient-physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci 2018;115(34):8569–8574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Committee on Health Care for Underserved Women. ACOG committee opinion no. 649: racial and ethnic disparities in obstetrics and gynecology. Obstet Gynecol 2015;126(6):e130–4. [DOI] [PubMed] [Google Scholar]
- 37.Hofstra B, Kulkarni VV, Munoz-Najar Galvez S, He B, Jurafsky D, McFarland DA. The Diversity-Innovation Paradox in Science. Proc Natl Acad Sci 2020;117(17):9284–9291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Esters D, Xierali IM, Nivet MA, Rayburn WF. The rise of nontenured faculty in obstetrics and gynecology by sex and underrepresented in medicine status. Obstet Gynecol 2019;134 Suppl 1:34S–39S. [DOI] [PubMed] [Google Scholar]
- 39.Sutton MY, Anachebe NF, Lee R, Skanes H. Racial and ethnic disparities in reproductive health services and outcomes. Obstet Gynecol 2021;137(2):225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Laland KN. Racism in academia, and why the “little things” matter. Nature 2020;584(7822):653–654. [DOI] [PubMed] [Google Scholar]
- 41.Shillcutt SK, Silver JK. Social media and advancement of women physicians. N Engl J Med 2018;378(24):2342–2345. [DOI] [PubMed] [Google Scholar]
- 42.Britton B, Jackson C, Wade J. The reward and risk of social media for academics. Nat Rev Chem 2019;3:459–461. [Google Scholar]
- 43.Jagsi R, Griffith KA, Stewart A, Sambuco D, DeCastro R, Ubel PA. Gender differences in the salaries of physician researchers. JAMA 2012;307(22):2410–2417. [DOI] [PubMed] [Google Scholar]
- 44.Jena AB, Olenski AR, Blumenthal DM. Sex differences in physician salary in US public medical schools. JAMA Intern Med 2016;176(9):1294–1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mensah M, Beeler W, Rotenstein L, Jagsi R, Spetz J, Linos E, Mangurian C. Sex differences in salaries of department chairs at public medical schools. JAMA Intern Med 2020;180(5):789–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rodríguez JE, Campbell KM, Pololi LH. Addressing disparities in academic medicine: what of the minority tax? BMC Med Educ 2015;15(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Richter KP, Clark L, Wick JA, Cruvinel E, Durham D, Shaw P, et al. Women physicians and promotion in academic medicine. N Engl J Med 2020;383(22):2148–2157. [DOI] [PubMed] [Google Scholar]
- 48.Andriole DA, Yan Y, Jeffe DB. Mediators of racial/ethnic disparities in mentored K award receipt among U.S. medical school graduates. Acad. Med 2017;92(10):1440–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Holliday E, Griffith KA, De Castro R, Stewart A, Ubel P, Jagsi R. Gender differences in resources and negotiation among highly motivated physician-scientists. J Gen Intern Med 2015;30(4):401–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Armijo PR, Silver JK, Larson AR, Asante P, Shillcutt S. Citizenship tasks and women physicians: additional woman tax in academic medicine? J Womens Health 2020. Ahead of print: doi: 10.1089/jwh.2020.8482. [DOI] [PubMed] [Google Scholar]
- 51.Carr RM. Reflections of a Black woman physician-scientist. J Clin Invest 2020;130(11):5624–5625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gibson EM, Bennett FC, Gillespie SM, Güler AD, Gutmann DH, Halpern CH, et al. How Support of Early Career Researchers Can Reset Science in the Post-COVID19 World. Cell 2020;181(7):1445–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Myers KR, Tham WY, Yin Y, Cohodes N, Thursby JG, Thursby MC, et al. Unequal effects of the COVID-19 pandemic on scientists. Nat Hum Behav 2020;4(9):880–883. [DOI] [PubMed] [Google Scholar]
- 54.Halley MC, Rustagi AS, Torres JS, Linos E, Plaut V, Mangurian C, et al. Physician mothers’ experience of workplace discrimination: a qualitative analysis. BMJ 2018;363:k4926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Reese TA, Harris-Tryon TA, Gill JG, Banaszynski LA. Supporting women in academia during and after a global pandemic. Sci Adv 2021;7(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lu DJ, King B, Sandler HM, Tarbell NJ, Kamrava M, Atkins KM. Paid Parental Leave Policies Among U.S. News & World Report 2020–2021 Best Hospitals and Best Hospitals for Cancer. JAMA Netw Open 2021;4(5):e218518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Marcotte LM, Arora VM, Ganguli I. Toward gender equity in academic promotions. JAMA Intern Med 2021. doi: 10.1001/jamainternmed.2021.3471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Early Stage Investigator Policies | grants.nih.gov. Available at: https://grants.nih.gov/policy/early-investigators/index.htm#background. Accessed May 7, 2021.
- 59.Xierali IM, Nivet MA, Syed ZA, Shakil A, Schneider FD. Recent trends in faculty promotion in U.S. medical schools: implications for recruitment, retention, and diversity and inclusion. Acad Med 2021. doi: 10.1097/ACM.0000000000004188. [DOI] [PubMed] [Google Scholar]
- 60.Fenner DE. Equality, equity, and justice. Am J Obstet Gynecol 2020;223(5):619–620. [DOI] [PubMed] [Google Scholar]
- 61.Choo E. Seven things organisations should be doing to combat racism. Lancet 2020;396(10245):157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Olayiwola JN, Choo E. Seven more things organisations should be doing to combat racism. Lancet 2020;396(10251):593. [DOI] [PubMed] [Google Scholar]
- 63.Ginther DK, Schaffer WT, Schnell J, Masimore B, Liu F, Haak LL, et al. Race, ethnicity, and NIH research awards. Science 2011;333(6045):1015–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Oliveira DFM, Ma Y, Woodruff TK, Uzzi B. Comparison of National Institutes of Health Grant Amounts to First-Time Male and Female Principal Investigators. JAMA 2019;321(9):898–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hoppe TA, Litovitz A, Willis KA, Meseroll RA, Perkins MJ, Hutchins BI, et al. Topic choice contributes to the lower rate of NIH awards to African-American/black scientists. Sci Adv 2019;5(10):eaaw7238. [DOI] [PMC free article] [PubMed] [Google Scholar]


