Abstract
Background
Glioblastoma multiforme (GBM) is the most common and aggressive primary intracranial tumor. Despite modern therapies, it is still fatal with tremendously poor prognosis with a median survival of 14 months. Even though mean survival and progression-free survival (PFS) are considered as primary response measure, it is important to assess the effects of therapies on disease burden and health-related quality of life (HRQoL). Changes in quality of life (QoL) indicates the impact of cytotoxic therapy and may aid in defining response in the absence of quantifiable endpoints like tumor regression. The objective was to assess 2-year survival and quality of life in GBM patients who underwent primary surgery followed by chemo-radiotherapy and 6-month adjuvant chemotherapy with temozolomide.
Materials and methods
Single-institution retrospective study of 60 patients of GBM from 2015 to 2017. Data regarding patient factors, disease factors, and treatment factors were collected and survival was calculated.
Results
60 patients with GBM were analyzed, male to female ratio was 1.6:1. Patients most commonly presented with headache. Most common tumour site is the frontal lobe. The median overall survival (OS) was 10 months. The 1-year and 2-year survival rates were 30% and 6.7%, respectively. Compared to before surgery patients have showed improved emotional, social and role functioning in Post radiotherapy period. There was a decrease in symptoms like pain, headache and seizures.
Conclusions
OS and QoL in GBM patients remains poor despite constant research and studies. Maximum safe resection followed by adjuvant temozolomide has shown improvement in OS. Post-surgery and adjuvant radiotherapy patients have shown a decrease in symptoms and better QoL.
Keywords: overall survival, quality of life, glioblastoma multiforme, temozolomide
Introduction
Glioblastoma multiforme (GBM) is the most common and malignant primary intracranial tumor, representing as much as 16% of primary brain tumour [1]. It is the most aggressive diffuse glioma of astrocytic lineage and is considered a grade IV glioma based on the World Health Organization (WHO) classification.
According to the 2016 WHO classification of GBM, this tumor has been separated from classical identity and is currently classified into 3 groups: GBM — wild type, GBM — isocitrate dehydrogenase (IDH) mutation (IDH-mutant), and GBM — not otherwise specified (NOS) [2]. These tumours have drawn high attention as most patients with GBMs die of the disease in less than a year and, essentially, none has long-term survival.
Despite the initiation of aggressive treatment along with extensive surgery, concurrent radiation and adjuvant temozolomide, the median survival time of adult patients remains around 10 months and up to 14 months in patients receiving combined treatment with radiotherapy [3].
Only 3% to 5% of patients survive more than three years, and reports of survival exceeding five years are sporadic [4].
A pilot phase 2 trial demonstrated the feasibility of the concomitant administration of temozolomide with fractionated radiotherapy, followed by up to six cycles of adjuvant temozolomide, and this treatment had suggested a promising clinical activity (two-year survival rate, 31%). Phase 3 trial of EORTC 26981 established STUPP REGIMEN as the standard of care in newly diagnosed GBM [5].
In glioma patients mean survival and progression-free survival (PFS) are mainly considered as a primary response measure. But it is also increasingly important to assess the effects of present therapies on disease burden and health-related quality of life (HRQoL) [6]. Quality of life (QoL) measurement scales and outcome concerns have become important to assess the outcomes of research programs in recent years and to assess whether new therapeutic and technological strategies are justified in terms of efficacy, cost and net QoL benefit [7]. Changes in QoL are also an important indicator of the impact of a new cytotoxic therapy, can affect patient’s willingness to continue treatment, and may aid in defining response in the absence of quantifiable endpoints, such as tumor regression [8].
Recently, the European Organization for Research and Treatment of Cancer Core Quality-of-Life Questionnaire (EORTC QLQ-C30), EORTC brain cancer module (EORTC QLQ-BN20) has been widely used to maximize the coverage of QoL issues and to fulfil demands for the reliability, validity, responsiveness and sensitivity of measurements and ascertain health and meaningful life-style in a primary brain tumor population [9].
This retrospective analysis is intended to evaluate the 2-year survival rate, PFS and quality of life in GBM patients who were treated at the Calicut medical college from 2015 to 2017. These data give us a snapshot of outcomes of patients managed as per guidance and evidence-based medicine.
Materials and methods
Study method
Patients with newly diagnosed GBM were eligible in this study. A retrospective audit was carried out of GBM case records of 60 patients registered in the year 2015 to 2017, using the details of Masterfile kept in the department,. Patients who met the inclusion and exclusion criteria was selected as study population. Detailed data were collected, including age, gender, Eastern Cooperative Oncology Group (ECOG) performance status, symptoms, the extent of surgery, radiation dose and volume, status of concurrent and adjuvant temozolomide and follow up.
The patients referred from Neurosurgery Department after primary surgery were evaluated with post-operative magnetic resonance imaging (MRI) within 4 weeks for assessing residual disease. The patients are further classified as follows, based on MRI performed less than 48 hours after surgery:
gross total resection (GTR) — a complete resection of the preoperative fluid-attenuated inversion recovery signal abnormality;
> 50% resection of tumor:
near-total resection (NTR): < 3-mm thin residual fluid-attenuated inversion recovery signal abnormality around the rim of the resection cavity only,
subtotal resection (STR) (residual nodular fluid-attenuated inversion recovery signal abnormality);
biopsy only.
Within 6 weeks after presenting to OPD the eligible patients were assigned to receive standard radiotherapy plus concurrent chemotherapy. Radiotherapy (RT) was planned with a dedicated computed tomography (CT) simulator. The patient was positioned and immobilised using a thermoplastic mask to increase setup accuracy. Thin slice CT imaging, preferably with 2.5 mm slice thickness, was taken and transferred to the treatment planning system. Image registration with MRI sequence (T1w, T2w and FLAIR) followed by target volume delineation according to the Radiation Therapy Oncology Group (RTOG) protocol was done in all patients. Conformal radiotherapy (three-dimensional RT or intensity-modulated RT technique) was delivered with linear accelerators with a nominal energy of 6 MV or more to deliver a radical dose of 60 Gy in 30 fractions of 2 Gy, 5 fractions per week.
Concurrent chemotherapy consisted of oral temozolomide in a dose of 75 mg/m2 from day 1 to day 7 for 6 weeks with radiotherapy. Adjuvant chemotherapy consisted of oral temozolomide in a dose of 150–200 mg/m2 from day 1 to day 5, 28 days cycle for 6 cycles. Routine complete blood count, kidney function test, liver function test, and serum electrolytes had been done and chemotherapy had been given only if the mentioned parameters were within normal limits.
Patients were followed up monthly for a period of 2 years. Patients who did not attend the outpatient unit on scheduled follow-up days were contacted by telephone to update disease and patient status.
The quality of life of surviving patients was assessed using EORTC QLQ C30 and BN20. EORTC QLQ-C30 consists of 30 questions divided into 5 domains — physical, role, emotional, social, cognitive and 9 symptoms. EORTC BN-20 consists of questions that specifically assess neurological symptoms and patient’s anxiety and apprehensions. The questionnaire includes 20 items which are organized into 4 scales (future uncertainty, visual disorders, motor dysfunction, and communication deficit) and 7 single items (headache, seizures, drowsiness, hair loss, itchy skin, weakness of legs, and bladder control). These data were collected before surgery and during first follow-up after radiotherapy. For the patients who were not alive, the data were collected from the primary care-taker.
Ethical consideration
Independent ethics committee (IEC) clearance was obtained. Data collection was started only after getting ethics committee approval for study. Confidentiality have been ensured and maintained.
Statistical analysis
All the data collected were coded and entered in a Microsoft Excel sheet which was re-checked and analysed using SPSS statistical software version 22. Quantitative variables were summarised using mean and standard deviation or median and interquartile range depending on the normality of distribution. Categorical variables were represented using frequency and percentage. ANOVA and Kruskal Wallis test were used for comparing continuous variables between groups depending on the normality of distribution. Pearson Chi-square test was used for comparing categorical variables between groups. Wilcoxon signed rank test was used for comparing different dimensions of quality of life before surgery and after radiotherapy. A p value of < 0.05 was considered statistically significant.
Results
The case records of 60 patients with histopathological diagnosis of GBM from 2015 to 2017 was retrospectively analysed. Among the study population, 40% was above 40 years old and 60% below 40 years old, 37 males (61.7%) and 23 females (38.3%), male:female ratio was 1.61:1. Majority of the patients presented complaints of headache (60%) and focal neurological symptoms (36.6%). Vomiting and seizures was also reported 16.6% and 15%, respectively.
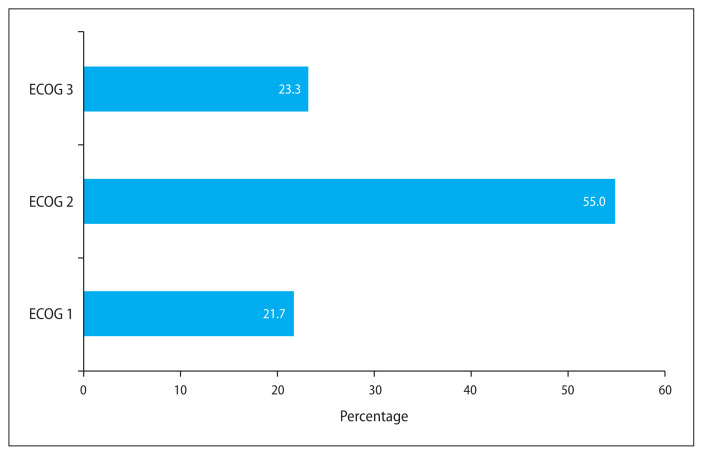
55% of patients presented with ECOG score of 1, 21.7% patients presented with ECOG-0 and 23.3% with ECOG-2 (Tab. 1, Fig. 1). Most of the tumour lesions were seen in a single site (91.7%) while 8.3% of tumours were multiple sites with 58.3% of tumours > 4 cm () and 41.7% < 4 cm in size. The most common site of the tumour was in the frontal region (40%) followed by temporal (33.3%), parietal (11.6%), corpus callosum (13.3%) and thalamus (3.3%).
Table 1.
Eastern Cooperative Oncology Group (ECOG) performance status — Majority of patients presented with ECOG score of 1 (55%). 21.7% patients presented with ECOG-0 and 23.3% — ECOG-2
| ECOG performance status | N (%) |
|---|---|
| ECOG 0 | 13 (21.7) |
| ECOG 1 | 33 (55) |
| ECOG 2 | 14 (23.3) |
Figure 1.
Eastern Cooperative Oncology Group (ECOG) performance score
Patients who underwent surgical procedure (46.7%) could only undergo near or STR while 31.7% underwent GTR and in 21.7% only biopsy was done. Postoperative MRI showed residual disease in 68.3% while 31.7% had no residual disease.
IDH status was unknown for majority of patients (88.3%), 10% showed IDH wild type and 1 (7%) — IDH-mutant. Out of 60 patients, 59 started RT within 6 weeks while 1 patient RT was delayed beyond 6 weeks due to a personal reason. 83.3% patients completed full course of radiotherapy treatment, whereas 10 (16.7%) patients could not complete RT. Adjuvant temozolomide was completed by 37 (61.7%) of patients while 38.3% patients could not complete the 6-month course. Temozolomide induced neutropenia was seen in 6 out of 60 patients. Temozolomide was given if absolute neutrophil count (ANC) was >1500 and platelet was > 100,000. Temozolomide induced hepatotoxicity was seen in 1 out of 60 patients with elevated bilirubin and treatment was stopped and supportive care continued. Among 37 patients who completed adjuvant temozolomide 24 patients had recurrence (64%) where in 50% the site of recurrence was infield of radiotherapy and in 50%, outfield of radiotherapy. Among 24 patients who had recurrence with ECOG 0–1 were treated with lomustine therapy and 2 patients were treated with bevacizumab, others were treated with supportive care.
Pneumocystis Carini prophylaxis is recommended in high grade glioma treatment with chemo radiation; however, in our institution, it is not a common practice. A study conducted by Neuwelt et al. in 240 patients showed only < 1% with Pneumocystis jiroveci pneumonia (PCP) infection without prophylaxis [10]. While Green et al. reported 15.2% of adverse reactions and 3.1% of severe adverse reactions (mainly leukopenia) in non-HIV adults who were administered a prophylactic trimethoprim-sulfamethoxazole drug [11], caution was taken while treating immunocompromised patients.
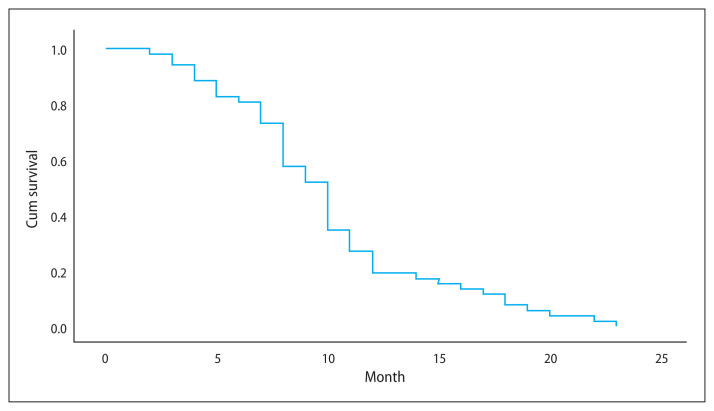
Majority of patients had disease-free survival of below 6 months (78.3%) and 15% patients survived 6 months to 1 year and 6.7% patients had disease free survival of > 1 year. Median overall survival (OS) time was 10 months. 1-year OS was 30% [14] and 2-year OS was 6.7% [4] (Tab. 2).
Table 2.
Association between various factors and overall survival (OS)
| Factors | OS | p-value | |||
|---|---|---|---|---|---|
| < 6 months (n = 14) | 6 months–1 year (n = 28) | 1 year–2 years (n = 14) | > 2 years (n = 4) | ||
| Age | |||||
| < 39 years | 8 (22.2) | 19 (52.8) | 6 (16.7) | 3 (8.3) | 0.414 |
| > 40 years | 6 (25) | 9 (37.5) | 8 (33.3) | 1 (4.2) | |
| Gender | |||||
| Male | 9 (24.3) | 15 (40.5) | 11 (29.7) | 2 (5.4) | 0.434 |
| Female | 5 (21.7) | 13 (56.5) | 3 (13) | 2 (8.7) | |
| Duration of symptoms | |||||
| < 6 months | 13 (23.2) | 26 (46.4) | 13 (23.2) | 4 (7.1) | 0.959 |
| > 6 months | 1 (25) | 2 (50) | 1 (25) | 0 (0) | |
| ECOG performance status | |||||
| ECOG 1 | 2 (15.4) | 6 (46.2) | 5 (38.5) | 0 | 0.671 |
| ECOG 2 | 9 (27.3) | 14 (42.4) | 7 (21.2) | 3 (9.1) | |
| ECOG 3 | 3 (21.4) | 8 (57.1) | 2 (14.3) | 1 (7.1) | |
| Lesion | |||||
| Single | 14 (25.5) | 23 (41.8) | 14 (25.5) | 4 (7.3) | 0.101 |
| Multiple | 0 (0) | 5 (100) | 0 (0) | 0 (0) | |
| Tumour size | |||||
| < 4 cm | 6 (24) | 9 (36) | 6 (24) | 4 (16) | 0.084 |
| > 4 cm | 8 (22.9) | 19 (54.3) | 8 (22.9) | 0 (0) | |
| Per op | |||||
| Gross total resection | 2 (10.5) | 12 (63.2) | 2 (10.5) | 3 (15.8) | 0.030* |
| > 50% removal | 6 (21.4) | 12 (42.9) | 10 (35.7) | 0 (0) | |
| Only biopsy taken | 6 (46.2) | 4 (30.8) | 2 (15.4) | 1 (7.7) | |
| Post-op MRI | |||||
| No residual | 1 (5.3) | 10 (52.6) | 6 (31.6) | 2 (10.5) | 0.137 |
| Residual | 13 (31.7) | 18 (43.9) | 8 (19.5) | 2 (4.9) | |
| IDH | |||||
| Mutant | 0 (0) | 1 (100) | 0 (0) | 0 (0) | 0.915 |
| Wild | 1 (16.7) | 3 (50) | 2 (33.3) | 0 (0) | |
| Not known | 13 (24.5) | 24 (45.3) | 12 (22.6) | 4 (7.5) | |
| Radiotherapy started | |||||
| < 6 weeks | 14 (23.7) | 27 (45.8) | 14 (23.7) | 4 (6.8) | 0.762 |
| > 6 weeks | 0 (0) | 1 (100) | 0 (0) | 0 (0) | |
| Completed radiotherapy | |||||
| Yes | 10 (20) | 23 (46) | 14 (28) | 3 (6) | 0.216 |
| No | 4 (40) | 5 (50) | 0 (0) | 1 (10) | |
| Adjuvant temozolomide for 6 months | |||||
| Yes | 3 (8.1) | 20 (54.1) | 10 (27) | 4 (10.8) | 0.003* |
| No | 11 (47.8) | 8 (34.8) | 4 (17.4) | 0 (0) | |
| Brain volume | |||||
| Mean | 1333 ± 143.92 | 1297.82 ± 132.92 | 1346.57 ± 123.73 | 1278.75 ± 34.06 | 0.600 |
| PTV volume | |||||
| Mean | 305.71 ± 99.41 | 344.39 ± 274.19 | 354.29 ± 137.91 | 309.25 ± 111.93 | 0.508 |
| Treated % brain volume (%) | |||||
| Mean | 23.19 ± 7.89 | 26.65 ± 22.08 | 27.05 ± 12.35 | 24.12 ± 8.36 | 0.634 |
| Recurrent site | |||||
| Yes | 1 (4.2) | 10 (41.7) | 9 (37.5) | 4 (16.7) | 0.001* |
| No | 13 (36.1) | 18 (50) | 5 (13.9) | 0 (0) | |
| Site | |||||
| In field | 1 (8.3) | 3 (25) | 5 (41.7) | 3 (25) | 0.294 |
| Out Field | 0 (0) | 7 (58.3) | 4 (33.3) | 1 (8.3) | |
| Disease-free survival | |||||
| < 6 months | 14 (29.8) | 26 (55.3) | 7 (14.9) | 0 (0) | < 0.001* |
| 6 months–1 year | 0 (0) | 2 (22.2) | 7 (77.8) | 0 (0) | |
| > 1 year | 0 (0) | 0 (0) | 0 (0) | 4 (100) | |
ECOG — Eastern Cooperative Oncology Group; MRI — magnetic resonance imaging; IDH — isocitrate dehydrogenase; PTV — planning target volume
The table shows the factors which effects the OS. The study shows adjuvant temozolomide (p = 0.003*) and gross total resection (p = 0.030*) are statistically significant for OS
Figure 2.
Overall survival (OS)
Overall survival
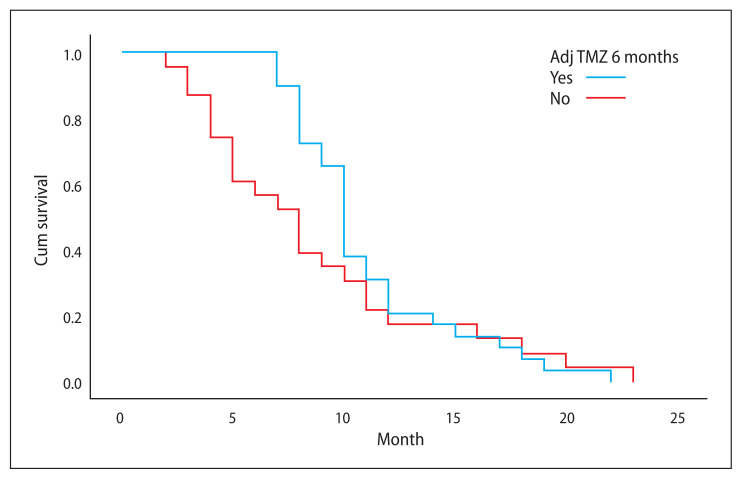
Median OS time was 10 months and 8 months for those patients who completed full course adjuvant temozolomide and those who did not, respectively (Tab. 2).
Survival analysis with adjuvant temozolomide vs. no adjuvant temozolomide
The study shows adjuvant temozolomide (p = 0.003*) and GTR (p = 0.030*) are statistically significant for OS.
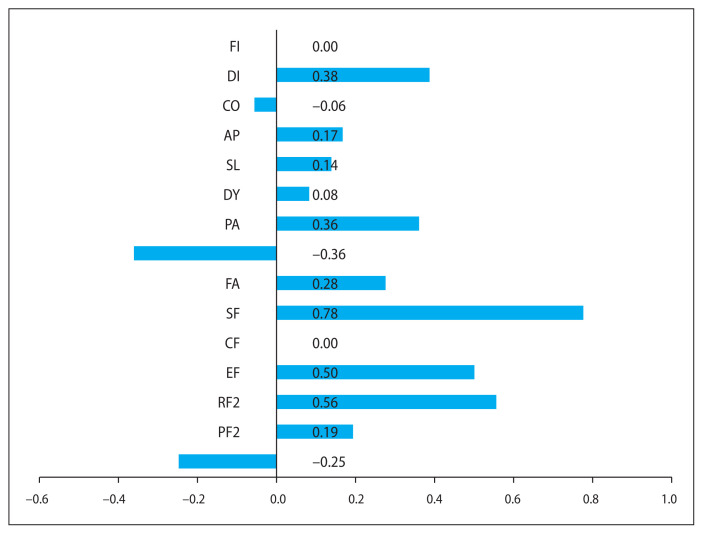
In general, quality of life assessment showed significant improvement in emotional, social and role functioning along with overall global health status in the post-radiation period and a decrease in symptoms like fatigue and pain. The symptoms like nausea and vomiting showed an increased incidence.
Post radiation patients have decreased incidence of symptoms like headache and seizures. There is an improvement in motor functioning, weakness of leg and communication deficit. Patients are also concerned about post-radiation hair fall.
Figure 3.
Survival analysis with adjuvant temozolomide (TMZ) vs. no adjuvant temozolomide
Discussion
This is a retrospective study conducted in a tertiary cancer care center in north Kerala, with 60 histopathologically diagnosed GBM patients. The study was conducted for a period of 2 years. The majority of the patients presented to the OPD from the Neurosurgery department post-surgery status.
In GBM, various patient-related, tumor-related, and treatment-related factors affect the outcome. It is, therefore, important to analyze the impact of the factors like age, performance status, the extent of surgery, concurrent and adjuvant chemotherapy on the result.
Among the study population of 60 subjects, 37 (61.7%) were males and 23% were females with a male to female ratio of 1.6:1. The study conducted by Bello et al. established the impact of sex on the prevalence and progression of glioblastomas. Estradiol and progesterone can exert promoter or protective effects while the role of testosterone has always been associated with glioblastomas progression [12].
The majority (14 out of 36) were in the age group of below 40 years which is about 60% and the duration between onset of symptoms and diagnosis was about 6 months in 93.3% of patients (56 in 60 patients). 52.8% of patients above 40 years survived up to one year and 8.3%, up to 2 years. Compared to age > 40, 1-year survival was 37.5% and 2-year was 4.2%, but the difference is less significant (p = 0.414). Most of the patients were younger than 40 years in contrast to the Stupp study [5] where the median age was 56 years. The reason for our patients being younger than the western population is not known. One reason could be the shorter life span of people living in developing countries than those living in developed countries [13].
In the Stupps study, 83% of patients underwent major tumor debulking with 40% having a complete excision. The median OS for patients who underwent resection was 15.8 while for those who were treated with biopsy it was only 9.4 months. In our study, patients who underwent GTR had a median OS of 10 months in those who had biopsy alone survival was 8 months only. In our study, 31.7% of patients had a complete excision and 46.7% had subtotal excision (debulking, decompression) while 21.7% had biopsy only. A study by Brown et al., a systemic review and metanalysis showed decreased mortality for GTR compared to STR [14]. It showed GTR substantially improves OS and PFS compared to STR, but the quality of the study was low. In our study GTR in patients has shown improved OS with those who have survived > 6 months (p = 0.030). This correlation strongly supports the importance of GTR in terms of survival in GBM patients.
A study conducted by Song Tao et al. reported adjuvant concurrent chemotherapy with TMZ was associated with improved survival on both univariate and multivariate analyses [15]. In our study, out of 60 patients, 37 (61.7%) have completed adjuvant temozolomide, while 23 patients did not complete a 6-month course duration due to a poor performance status, personal or logistic issues, and one patient reported temozolomide induced hepatic toxicity. Among 37 patients who completed adjuvant temozolomide, 20 patients (54.1%) survived 1 year, 10 patients (27%) survived 1 to 2 years and 4 patients (10.8%) survived more than 2 years (p = 0.003), while patients who did not complete adjuvant temozolomide survived less: 34.8% survived 1 year, 17.4%, 1 to 2 years and no patients survived more than 2 years (p = 0.003).
Out of 60 patients, 59 started RT within 6 weeks while 1 patient had a delayed RT start due to personal reasons. 83.3% of patients could complete RT while 16.7% of patients could not complete RT due to a poor performance status and toxicity.
Studies have shown that a median OS is 31 months for secondary GBM patients with IDH mutations compared to 15 months for those without the mutations [15]. In our study among 60 patients 53 patients’ IDH status was not known. 6 (10%) were wild IDH status and 1 patient IDH-mutant (1.7%) (p = 0.915). But not enough data to correlate with survival due to the unavailability of testing in the study period in our centre.
Among 37 patients who completed adjuvant temozolomide, 24 patients had recurrence of whom 12 patients had an in-field recurrence and 12 had an out-field recurrence. The volume of brain irradiated was less in patients who had survived 2 years (24.12 + 8) compared to 1 year (27.05 + 12) but not statistically significant.
The median survival, 1-year OS, and 2-year OS for the entire cohort were 10 months, 30%, and 6.7%, respectively. The OS is significantly associated with the extent of resection and adjuvant temozolomide, whereas age, ECOG performance status, treated brain volume has not significantly affected survival in our study.
Quality of life in glioma patients was assessed in pre-surgery and post-radiotherapy periods in our study (Tab. 3, 4, Fig. 4, 5). This showed a significant decrease in symptoms like pain, headache, seizures post-surgery, and adjuvant radiotherapy. There was also a significant improvement in their role and social functioning (p < 0.001) which can be correlated with decreased symptoms. Patients have had better emotional functioning (p < 0.008) in the post radio-therapy period, which may be due to this sense of well-being.
Table 3.
Quality of life before surgery and after radiotherapy — European Organization for Research and Treatment of Cancer Core Quality-of-Life Questionnaire (EORTC QLQ-C30) (n = 36)
| Variable | Mean ± SD | Median (IQR) | p-value |
|---|---|---|---|
| Global health status (GH) | |||
| Before surgery | 9.06 ± 2.16 | 10 (9–10) | 0.106 |
| After radiotherapy | 9.31 ± 2.61 | 10 (9–11) | |
| Physical functioning (PF) | |||
| Before surgery | 10.17 ± 3.06 | 10 (8–12) | 0.282 |
| After radiotherapy | 9.94 ± 3.05 | 10 (7–11) | |
| Role functioning (RF) | |||
| Before surgery | 4.36 ± 1.33 | 4 (4–5) | < 0.001* |
| After radiotherapy | 3.81 ± 1.45 | 3 (3–4.75) | |
| Emotional functioning (EF) | |||
| Before surgery | 8.06 ± 2.46 | 7 (6–11) | 0.008* |
| After radiotherapy | 7.53 ± 2.36 | 6 (6–10) | |
| Cognitive functioning (CF) | |||
| Before surgery | 4.22 ± 0.95 | 4 (4–5) | 0.847 |
| After radiotherapy | 4.25 ± 1.18 | 4 (3–5) | |
| Social functioning (SF) | |||
| Before surgery | 5.47 ± 1.13 | 5 (4.25–6.75) | < 0.001* |
| After radiotherapy | 4.69 ± 1.21 | 4 (4–5.75) | |
| Fatigue (FA) | |||
| Before surgery | 6.39 ± 1.71 | 6 (5–8.50) | 0.247 |
| After radiotherapy | 6.11 ± 1.65 | 6 (4–7) | |
| Nausea and vomiting (NV) | |||
| Before surgery | 2.92 ± 1.29 | 2.5 (2–4) | 0.012* |
| After radiotherapy | 3.31 ± 1.61 | 3.5 (2–4) | |
| Pain (PA) | |||
| Before surgery | 4.03 ± 1.27 | 4 (3–4) | 0.037* |
| After radiotherapy | 3.69 ± 1.03 | 3 (3–4) | |
| Dyspnea (DY) | |||
| Before surgery | 1.25 ± 0.43 | 1 (1–1.75) | 0.102 |
| After radiotherapy | 1.14 ± 0.35 | 1 (1–1) | |
| Insomnia (SL) | |||
| Before surgery | 1.89 ± 0.62 | 2 (1.25–2) | 0.346 |
| After radiotherapy | 1.78 ± 0.89 | 1 (1–3) | |
| Appetite loss (AP) | |||
| Before surgery | 2.14 ± 0.35 | 2 (2–2) | 0.014* |
| After radiotherapy | 1.97 ± 0.56 | 2 (2–2) | |
| Constipation (CO) | |||
| Before surgery | 1 ± 0 | 1 (1–1) | 0.157 |
| After radiotherapy | 1.06 ± 0.23 | 1 (1–1) | |
| Diarrhea (DI) | |||
| Before surgery | 1.67 ± 0.47 | 2 (1–2) | 0.003* |
| After radiotherapy | 1.31 ± 0.46 | 1 (1–2) | |
| Financial difficulties (FI) | |||
| Before surgery | 3.11 ± 0.31 | 3 (3–3) | 1.000 |
| After radiotherapy | 3.11 ± 0.57 | 3 (3–3) | |
statistically significant;
SD — standard deviation
Table 4.
Quality of life before surgery and after radiotherapy — European Organization for Research and Treatment of Cancer Core Quality-of-Life Questionnaire brain cancer module (EORTC QLQ-BN20)
| Variable | Mean ± SD | Median (IQR) | p-value |
|---|---|---|---|
| Future uncertainty (FU) | |||
| Before surgery | 9.03 ± 1.4 | 9 (8–10) | 0.252 |
| After radiotherapy | 9.25 ± 1.55 | 9 (8.25–10) | |
| Headaches (H) | |||
| Before surgery | 2.56 ± 0.77 | 3 (2–3) | < 0.001* |
| After radiotherapy | 1.72 ± 0.84 | 2 (1–2) | |
| Visual disorder (VD) | |||
| Before surgery | 3.22 ± 0.59 | 3 (3–3) | 0.083 |
| After radiotherapy | 3.14 ± 0.42 | 3 (3–3) | |
| Seizures (S) | |||
| Before surgery | 1.31 ± 0.71 | 1 (1–1) | 0.024* |
| After radiotherapy | 1.06 ± 0.23 | 1 (1–1) | |
| Motor dysfunction (MD) | |||
| Before surgery | 6.08 ± 2.68 | 5 (4–9) | < 0.001* |
| After radiotherapy | 5.44 ± 2.51 | 4 (3.25–7.75) | |
| Communication deficit (CD) | |||
| Before surgery | 6 ± 2.66 | 5 (4–8.75) | < 0.001* |
| After radiotherapy | 5.42 ± 2.54 | 4 (3.25–7.75) | |
| Drowsiness (Dr) | |||
| Before surgery | 1.33 ± 0.58 | 1 (1–2) | 0.102 |
| After radiotherapy | 1.44 ± 0.69 | 1 (1–2) | |
| Hair loss (HL) | |||
| Before surgery | 1 ± 0 | 1 (1–1) | < 0.001* |
| After radiotherapy | 2.53 ± 0.6 | 3 (2–3) | |
| Itchy skin (IS) | |||
| Before surgery | 1 ± 0 | 1 (1–1) | 0.317 |
| After radiotherapy | 1.03 ± 0.16 | 1 (1–1) | |
| Weakness of legs (WL) | |||
| Before surgery | 1.58 ± 0.84 | 1 (1–2) | 0.046* |
| After radiotherapy | 1.47 ± 0.73 | 1 (1–2) | |
| Bladder control (BC) | |||
| Before surgery | 1.19 ± 0.46 | 1 (1–1) | 0.317 |
| After radiotherapy | 1.17 ± 0.44 | 1 (1–1) | |
statistically significant;
SD — standard deviation; IQR — interquartile range
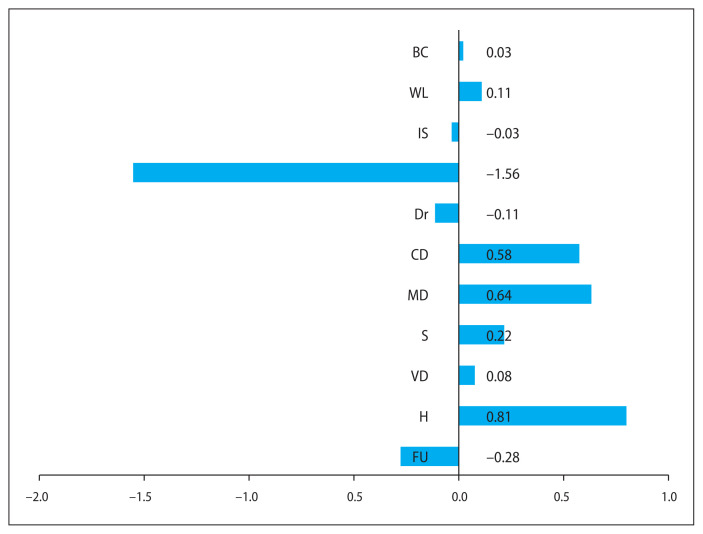
Figure 4.
Improvement in dimensions of quality of life — European Organization for Research and Treatment of Cancer Core Quality-of-Life Questionnaire (EORTC QLQ-C30). In general quality of life assessment showed significant improvement in emotional, social and role functioning along with overall global health status in the post-radiation period and a decrease in symptoms like fatigue and pain. The symptoms like nausea and vomiting showed an increased incidence
Figure 5.
Improvement in dimensions of quality of life—European Organization for Research and Treatment of Cancer Core Quality-of-Life Questionnaire brain cancer module (EORTC QLQ-BN20). Post radiation patients have decreased incidence of symptoms like headache and seizures. There is an improvement in motor functioning, weakness of leg and communication deficit. Patients are also concerned about post-radiation hair fall
Two randomized controlled trials in newly diagnosed HGG patients with a good performance status evaluated the effect of two treatment strategies—radiotherapy in combination with chemotherapy (concomitant and/or adjuvant) versus radiotherapy alone — on survival and HRQoL [16, 17]. Although baseline HRQoL scores were already substantially diminished, no negative effects of radiotherapy on glioblastoma patients were observed. HRQoL even improved slightly over time, which may be partially explained by response to the treatment. Patients also reported to have increased nausea and vomiting, which may be related to factors like chemotherapy, residual tumour, radiotherapy induced brain edema and steroid and stress-induced gastritis. Post radiotherapy period patients were also concerned about post-radiation hair loss.
Overall, there was an increase in global health status in our cohort after treatment. Patients were also concerned about the future uncertainties and financial difficulties but these were not statistically significant.
Conclusion
In the present study, the patients with GBM, 1-year OS was 30% and 2-year OS was 6.7% for those who have completed maximum safe resection followed by chemoradiotherapy and adjuvant temozolomide for 6 months, Factors like age, ECOG, adjuvant temozolomide and extent of resection had an impact on OS.
Following surgery, post radiotherapy patients have reported better quality of life in some aspects with a decrease in symptoms and betterment in emotional and role functioning. But social functioning and financial instability have been worrisome in most of the patients.
Limitation
Factors such as IDH mutation correlation could not be assessed due to the unavailability of the test in that study period. Majority of the patients were not alive for assessment of the quality of life; therefore, reliability issues were present.
References
- 1.Ostrom QT, Bauchet L, Davis FG, et al. The epidemiology of glioma in adults: a “state of the science” review. Neuro Oncol. 2014;16(7):896–913. doi: 10.1093/neuonc/nou087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang YH, Li Z, Zeng T, et al. Distinguishing Glioblastoma Subtypes by Methylation Signatures. Front Genet. 2020;11:604336. doi: 10.3389/fgene.2020.604336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dubrow R, Darefsky AS. Demographic variation in incidence of adult glioma by subtype, United States, 1992–2007. BMC Cancer. 2011;11:325. doi: 10.1186/1471-2407-11-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krex D, Klink B, Hartmann C, et al. German Glioma Network. Long-term survival with glioblastoma multiforme. Brain. 2007;130(Pt 10):2596–2606. doi: 10.1093/brain/awm204. [DOI] [PubMed] [Google Scholar]
- 5.Stupp R, Mason WP, van den Bent MJ, et al. European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups, National Cancer Institute of Canada Clinical Trials Group. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 6.Henriksson R, Asklund T, Poulsen HS. Impact of therapy on quality of life, neurocognitive function and their correlates in glioblastoma multiforme: a review. J Neurooncol. 2011;104(3):639–646. doi: 10.1007/s11060-011-0565-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kalkanis SN, Quiñones-Hinojosa A, Buzney E, et al. Quality of life following surgery for intracranial meningiomas at Brigham and Women’s Hospital: a study of 164 patients using a modification of the functional assessment of cancer therapy-brain questionnaire. J Neurooncol. 2000;48(3):233–241. doi: 10.1023/a:1006476604338. [DOI] [PubMed] [Google Scholar]
- 8.Cella D, Chang CH, Lai JS, et al. Advances in quality of life measurements in oncology patients. Semin Oncol. 2002;29(3 Suppl 8):60–68. doi: 10.1053/sonc.2002.33535. [DOI] [PubMed] [Google Scholar]
- 9.Mahalakshmi P, Vanisree AJ. Quality of life measures in glioma patients with different grades: A preliminary study. Indian J Cancer. 2015;52(4):580–585. doi: 10.4103/0019-509X.178395. [DOI] [PubMed] [Google Scholar]
- 10.Neuwelt AJ, Nguyen TM, Fu R, et al. Incidence of Pneumocystis jirovecii pneumonia after temozolomide for CNS malignancies without prophylaxis. CNS Oncol. 2014;3(4):267–273. doi: 10.2217/cns.14.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Green H, Paul M, Vidal L, et al. Prophylaxis of Pneumocystis pneumonia in immunocompromised non-HIV-infected patients: systematic review and meta-analysis of randomized controlled trials. Mayo Clin Proc. 2007;82(9):1052–1059. doi: 10.4065/82.9.1052. [DOI] [PubMed] [Google Scholar]
- 12.Bello-Alvarez C, Camacho-Arroyo I. Impact of sex in the prevalence and progression of glioblastomas: the role of gonadal steroid hormones. Biol Sex Differ. 2021;12(1):28. doi: 10.1186/s13293-021-00372-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Munshi A, Jalali R. Therapy for glioma: Indian perspective. Indian J Cancer. 2009;46(2):127–131. doi: 10.4103/0019-509x.49150. [DOI] [PubMed] [Google Scholar]
- 14.Brown TJ, Brennan MC, Li M, et al. Association of the Extent of Resection With Survival in Glioblastoma: A Systematic Review and Meta-analysis. JAMA Oncol. 2016;2(11):1460–1469. doi: 10.1001/jamaoncol.2016.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.SongTao Qi, Yu Lei, Si G, et al. IDH mutations predict longer survival and response to temozolomide in secondary glioblastoma. Cancer Sci. 2012;103(2):269–273. doi: 10.1111/j.1349-7006.2011.02134.x. [DOI] [PubMed] [Google Scholar]
- 16.Taphoorn M, Stupp R, Coens C, et al. Health-related quality of life in patients with glioblastoma: a randomised controlled trial. Lancet Oncol. 2005;6(12):937–944. doi: 10.1016/s1470-2045(05)70432-0. [DOI] [PubMed] [Google Scholar]
- 17.Taphoorn MJB, van den Bent MJ, Mauer MEL, et al. European Organisation for Research and Treatment of Cancer. Health-related quality of life in patients treated for anaplastic oligodendroglioma with adjuvant chemotherapy: results of a European Organisation for Research and Treatment of Cancer randomized clinical trial. J Clin Oncol. 2007;25(36):5723–5730. doi: 10.1200/JCO.2007.12.7514. [DOI] [PubMed] [Google Scholar]