Abstract
Background
Head and neck squamous cell carcinomas (HNSCCs) are associated with variable prognosis even with similar clinical characteristics and treatments. Gene polymorphisms have been suggested as prognostic factors for HNSCC which can justified this variable prognosis. So, the aim was to review literatures on gene polymorphisms and prognosis of HNSCCs.
Materials and methods
A systematic search was conducted using PubMed, Web of science, SCOPUS, Google Scholar and Cochrane library databases to find all related articles published up to December 2021 in the field of gene polymorphisms and HNSCC prognosis.
Results
Of 1029 initial searched articles, 71 articles were selected for inclusion in this systematic review. About 93 genes and 204 polymorphisms have been discussed in these articles. Among the most studied polymorphisms, the XRCC1 Arg399Gln and Arg194Trp polymorphisms were not associated with survival in most studies; the ERCC1 C19007T polymorphism had no significant association in any of the studies. Different gene polymorphisms of glutathione s-transferase family, including GSTM1 deletion, GSTT1 deletion and GSTP1 A313G, were not associated with survival in included studies. There are conflicting results regarding the association between polymorphisms such as ERCC2 A35931C, Asp312Asn, ERCC5 rs1047768 and rs17655 with HNSCC prognosis. Less studied polymorphisms, such as hOGG1 rs1052133 or the VEGF rs699947, were generally not associated with HNSCC prognosis.
Conclusion
Reviewed articles reported varied and contradictory results regarding the association of gene polymorphisms and HNSCC prognosis, which necessitates further studies along with meta-analysis on the results of such studies.
Keywords: gene polymorphism, single nucleotide polymorphisms, head and neck squamous cell carcinoma, prognosis, survival
Introduction
Head and neck squamous cell carcinoma (HNSCC) is the sixth most common cancer in the world; HNSCC is associated with severe morbidity and mortality and has a five-year survival rate of approximately 25–60% [1–4].
Overall, survival (OS), disease-specific survival (DSS), progression-free survival (PFS), and disease-free survival (DFS) are among the most important patient’s clinical outcomes. Prognosis of HNSCCs is dependent on multiple clinical factors, including stage, anatomic site, and patient’s overall health status; other prognostic factors include age, gender, race, presence of comorbidities, alcohol drinking and tobacco consumption, tumor differentiation and lymph node metastasis. Human papillomavirus (HPV) infection, tumor markers, and genetic factors have also been correlated with prognosis and clinical outcomes [5, 6].
Studies have shown that HNSCCs are associated with variable prognosis even with similar clinical stages and treatments; at least part of this variable prognosis can be attributed to genetic variations. Genetic variations may cause differential radiosensitivity or chemosensitivity in HNSCC patients. Single nucleotide polymorphisms (SNPs) are among the most common genetic variations and study of SNPs as potential prognostic factors have become increasing in a wide variety of cancers [5–7].
So, the aim was to review literatures on gene polymorphisms and prognosis of HNSCCs.
Materials and methods
Literature search
The research question was defined based on PICO:
P — Population/Patient: HNSCC patients;
I — Intervention: presence of gene polymorphism;
C — comparator: HNSCC patients without gene polymorphism;
O — outcome: prognosis or survival.
A systematic search was conducted using PubMed, Web of science, SCOPUS, Google Scholar and Cochrane library databases to find articles related to the aim of this systematic review.
The search was performed on above databases according to MeSH terms as follows:
(“Single nucleotide polymorphism” OR “genetic variation” OR “genetic polymorphism”) AND (“prognosis” OR “survival” OR “disease-free survival” OR “progression-free survival”) AND (“squamous cell carcinoma of head and neck” OR “head and neck neoplasms”).
All articles were first assessed by title and duplicate articles were also excluded. Afterwards, we selected the articles by reading the abstracts. In the later stage, related articles were selected based on the full text. Two independent researchers made the search and extracted that data. Disagreements were resolved by consensus.
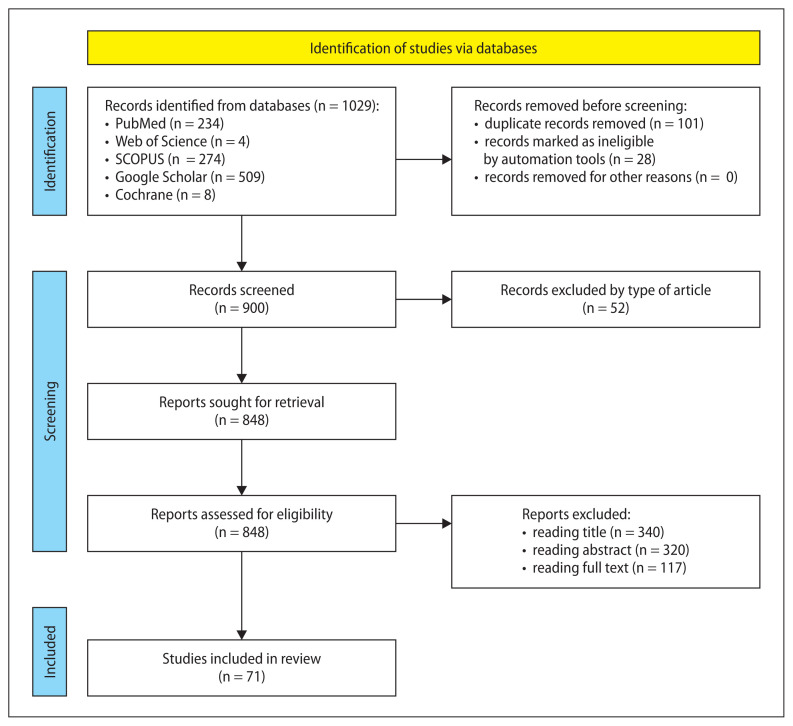
PRISMA flow diagram was used for systematic search of articles and selecting the articles (Fig. 1).
Figure 1.
PRISMA flow diagram representing the process of identification of studies through databases
Inclusion and exclusion criteria
This systematic review included all original English-language research articles published from January 1998 to December 2021 regarding the association of gene polymorphisms with prognosis of HNSCCs. Prognosis in these articles was overall survival (OS), progression-free survival (PFS), disease-free survival (DFS) or disease-specific survival (DSS).
Oral squamous cell carcinoma (OSCC), oropharyngeal SCC (OPSCC), hypopharyngeal SCC (HPSCC), nasopharyngeal SCC (NPSCC) and laryngeal SCC (LSCC) were regarded as HNSCCs.
Exclusion criteria were as follows: studies evaluating neoplasms located in other parts of the body than head and neck area; studies evaluating neoplasms other than squamous cell carcinoma; case report articles, reviews and letters to the editor articles; studies which did not report the association of gene polymorphisms with prognosis; studies which included the association of gene or protein expression with prognosis; studies which reported the association of gene polymorphisms with HNSCC risk, post-treatment toxicity and treatment response; studies which reported the association of gene polymorphisms with prognosis of second primary tumors.
Quality assessment
The Joanna Briggs Institute (JBI) checklist was used for evaluation of the quality of the selected articles. Scoring of final articles based on JBI checklist was done. The acceptable score (based on JBI checklist) was 60% for inclusion of the articles in this systematic review.
Results
Of 1029 initial searched articles, 71 articles were eligible for inclusion in this systematic review. A summary of the characteristics of the included studies are shown in Table 1.
Table 1.
Characteristics of the studies included in this systematic review
| First author, year | Studied Genes (polymorphisms) | Primary outcome |
|---|---|---|
| Matthias, 1998 [8] | CCND1 (A870G) | DFS |
| Holley, 2001 [9] | CCND1 (A870G, G1722C) | DFS |
| Sullivan, 2004 [10] | p53 (Arg72Pro) | OS, PFS |
| Wang, 2004 [11] | DNMT3B6 (C-149T) | OS |
| Streit, 2004 [12] | FGFR4 (Gly388Arg) | OS |
| Monteiro, 2004 [13] | CCND1 (A870G) | OS, DFS |
| Geisler, 2005 [14] | GSTT1 (deletion), GSTM1 (deletion), GSTP1 (Ile105Val), XRCC1 (Arg399Gln, Arg194Trp) | OS, DSS |
| Etienne-Grimaldi, 2005 [15] | EGFR (rs11568315) | DSS |
| Gal, 2005 [16] | XRCC1 (Arg399Gln), XRCC3 (Thr241Met), XPD (Lys751Gln), MGMT (Leu84Phe), MGMT (Val143Ile) | OS, DSS |
| Kondo, 2005 [17] | MMP1 (1G 1607 2G) | OS |
| Wong, 2006 [18] | CTLA-4 (A49G) | OS |
| Carles, 2006 [19] | XPA (rs1800975), XPC (Lys939Gln), XPD (Lys751Gln), ERCC1 (Lys259Thr), ERCC5 (His1104Asp, C581T), XRCC5 (rs1051677, rs1051685), XRCC1 (Arg399Gln) | OS |
| Matthias, 2006 [20] | CCND1 (A870G), TNFa (TNFBID5) | DFS |
| Quintela-Fandino, 2006 [21] | ERCC1 (C8092A), XPD (Asp312Asn, Lys751Gln), XRCC1 (Arg399Gln) | OS |
| da Costa Andrade, 2007 [22] | FGFR4 (Gly388Arg) | OS |
| Lehnerdt, 2009 [23] | BCL2 (−938C>A) | DFS, OS |
| Lundberg, 2009 [24] | TGFβ1 (rs1982073) | DFS, OS |
| Klinghammer, 2010 [25] | EGFR (R521K, CA-SSR) | PFS, OS |
| Lundberg, 2010 [26] | TGFβ1 (rs1982073) | DFS, OS |
| Tanuma, 2010 [27] | FGFR4 (Gly388Arg), TP53 (Mutant) | OS |
| Corrêa, 2011 [28] | TNF-α (−308) | OS |
| Bergmann, 2011 [29] | TLR4 (Asp299Gly, Thr399Ile) | DFS, OS |
| De Castro, 2011 [30] | ERCC1 (T19007C) | OS |
| Hama, 2011 [31] | VDR (rs11568820), FokI (rs10735810), BsmI (rs1544410), ApaI (rs7976091), TaqI (rs731236) | PFS |
| Zhong, 2011 [32] | ERCC2 (rs13181), CCND1 (rs9344) | OS, DSS, PFS, DFS |
| Wang, 2012 [33] | KRAS (rs1137282, rs712) | OS |
| Azad, 2012 [34] | CCND1 (A870G), TP53 (Arg72Pro), DNMT3B (C149T), ERCC1 (C8092A, Lys259Thr), ERCC4 (T2505C), ERCC5 (C581T, His1104Asp), MSH2 (C211þ9G), ERCC2 (Asp312Asn, Lys751Gln), XRCC1 (Arg399Gln), XRCC3 (Thr241Met), FGFR4 (Gly388Arg), CTLA4 (A49G), MMP3 (−1612insA), GSTM1 (Deletion), GSTT1 (Deletion), CYP2D6 (*3, *4, *5) | OS, DFS |
| Lima, 2012 [35] | ERCC1 (G19007A) | OS |
| Lundberg, 2012 [36] | TGFβ1 (rs1800470) | OS, DFS |
| Stoehlmacher-Williams, 2012 [37] | EGFR (−216 G/T, −191 C/A, R497K G → A), EGF (61 A/G) | OS |
| Supic, 2012 [38] | VEGF-A (−2578C/A, −1154A/G, −634G/C, +936C/T) | OS |
| Liu, 2013 [39] | FGFR4 (rs351855), VEGF (rs2010963, rs833061, rs3025039), ERCC1 (rs3212986), ERCC2 (rs1799793, rs13181 ), XRCC1 (rs25487), hOGG1 (rs1052133), APEX1 (rs1130409), ADPRT (rs1136410), MTHFR (rs1801131, rs1801133), ABCB1 (rs1045642, rs2032582), MPO (rs2243828), MDM2 (rs2279744) | OS, PFS |
| Guan, 2013 [40] | Pre-microRNA (rs2910164, rs2292832, rs11614913, rs3746444) | OS, DSS, DFS |
| Jin, 2013 [41] | IL-10 (rs1800871, rs1800872, rs1800896) | OS, DSS, DFS |
| Liu, 2013 [42] | miR-196a2 (rs11614913) | DFS |
| Zhang, 2014 [43] | TNF-α (rs1800629, rs1799724, rs1800630, rs1799964) | DFS |
| Chung, 2014 [44] | KRAS (rs61764370) | OS, PFS |
| Lin, 2014 [45] | hMLH1 (rs1800734, rs1540354) | OS, DFS |
| Su, 2014 [46] | EGF (A61G A>G), EGFR (R521K G>A, G-216T) | OS, PFS |
| Zhang, 2014 [47] | TNF-α (rs1800629, rs1799724, rs1800630, rs1799964) | DFS |
| Farnebo, 2015 [48] | XPC (A499V), XPD (K751Q), XRCC1 (R399Q), XRCC3 (T241M) | OS |
| Pfisterer, 2015 [49] | AKT1 (rs2494738, rs2498804, rs3803304), AKT2 (rs892119, rs8100018), FRAP1 (rs11121704, rs2295080), PIK3CA (rs2699887, rs7640662), PTEN (rs12569998, rs2299939) | OS, PFS |
| Reuter, 2015 [50] | PXR (rs3814055, rs1523127, rs2472677, rs6785049, rs2276707, rs1054190, rs1054191) | OS |
| Stur, 2015 [51] | XRCC1 (Arg194Trp, Arg399Gln), XRCC3 (Thr241Met), XPC (Lys939Gln), ERCC1 (Asn118Asn), RAD51 (−98G>C) | DSS, DFS |
| Costa, 2016 [52] | OGG1 (rs1052133), APEX1 (rs1130409), XRCC1 (rs3213245, rs1799782, rs25489, rs25487) | PFS, OS |
| Wang, 2016 [53] | Pre-microRNA (rs2910164, rs11614913, rs2292832, rs3746444) | OS, DSS, DFS |
| Agostini, 2017 [54] | ATM (5557G>A, IVS62 + 60G>A), TP53 (215G>C), BCL2 (−938C>A), TGFβ (−509C>T, 29C>T) | DFS, DSS |
| Braig, 2017 [55] | EGFR (EGFR-K521) | PFS |
| Chen, 2017 [6] | FADS1 (rs174549) | PFS, OS |
| Lopes-Aguiar, 2017 [56] | XPC (c.2815A>C), XPD (c.934G>A, c.2251A>C), XPF (c.2505T>C), ERCC1 (c.354C>T) | PFS, OS |
| Zhu, 2017 [57] | ATM (rs227091), BRCA1 (rs12516, rs8176318), PARP1 (rs8679), LIG3 (rs4796030), NBS1 (rs2735383, rs1063054, rs1063053), RAD51 (rs7180135) | DFS |
| Magnes, 2018 [58] | FCGR2A (rs1801274), FCGR3A (rs396991) | PFS, OS |
| Nanda, 2018 [7] | XRCC1 (Arg194Trp) | DFS, OS |
| Senghore, 2019 [59] | MSH2 (rs3732183), MSH3 (rs12515548, rs26279), EXO1 (rs1047840), MLH1 (rs1800734) | DFS, OS |
| Senghore, 2019 [60] | ERCC5 (rs2094258, rs1047768, rs17655, rs873601), ERCC2 (rs13181, rs1799793), ERCC1 (rs735482, rs3212986, rs11615), XPC (rs2228001, rs2228000), XPA (rs1800975, rs10817938) | OS, DFS |
| Hirakawa, 2020 [4] | ERCC1 (C8092A), XRCC1 (Arg399Gln) | OS |
| Butkiewicz, 2020 [61] | VEGF (rs2010963, rs699947, rs3025039), VEGFR1 (rs9582036, rs7996030), VEGFR2 (rs2071559, rs1870377), ANGPT1 (rs2507800, rs1954727), ANGPT2 (rs3739391, rs3020221), TEK (rs639225) | OS, DFS |
| Dutta, 2020 [62] | XRCC1 (Arg399Gln) | OS, PFS |
| Maniglia, 2020 [63] | GSTT1 (Deletion), GSTM1 (Deletion), GSTP1 (A313G, C341T) | OS |
| Senghore, 2020 [64] | XRCC1 (rs25487, rs25489, rs1799782), OGG1 (rs1052133), APEX1 (rs1760944), MUTYH (rs3219489) | OS, DFS |
| Yadav, 2021 [65] | CYP2A6 (*4B, *4C, *9) | OS |
| Dimitrakopoulos, 2021 [66] | VEGFA (rs699947, rs12664104, rs34376996, rs144854329, rs35864111, rs833061, rs149983590, rs833062, rs1570360, rs28357093, rs13207351, rs79469752, rs59260042, rs3025039, rs149179279, rs112005313, rs187429037, rs111933757), EDNRA (rs5333, rs5334, rs10305924, rs17856670, rs112710542), FAS (rs1800682, rs34995925, rs2234768, rs150130637), NBS1 (rs1805794, rs192240705, rs780661058, rs151070415, rs61754966, rs182756889) | OS |
| Guberina, 2021 [67] | ERCC2 (rs1799793, rs13181, rs50871), XRCC6 (rs2267437), ERCC1 (rs11615), ATM (rs4988023), ERCC5 (rs17655), XRCC1 (rs25487) | OS, DFS |
| Duran, 2021 [68] | ABCB1 (rs1045642, rs2032582), ABCC1 (rs246221, rs45511401), ABCC2 (rs717620), ABCG2 (rs2231142), ATP6V1C1 (rs2248718), ATP7B (rs1061472, rs1801244, rs2147363), CDA (rs2072671), ND3 (rs2853826), RRM1 (rs12806698), SLC28A1 (rs2242047), COX-2 (rs689466), IL3 (rs1800925), TGFB1 (rs1800469), FGFR4 (rs351855), GSTP1 (rs1695), NQO1 (rs1800566), MMP-2 (rs12934241), SOD2 (rs4880), RAD51 (rs1801320), XRCC6 (rs2267437), ERCC1 (rs11615, rs3212986), ERCC4 (rs1799801), XPC (rs2228001), ERCC2 (rs13181, rs1799793, rs238406), ERCC5 (rs17655), XRCC1 (rs25487), XRCC2 (rs6464268), XRCC3 (rs861539), RPA34 (rs735482) | OS, DFS |
| Jović, 2021 [69] | CCND1 (rs9344), p21 (rs1801270, rs1059234) | OS, DFS |
| Lubiński, 2021 [70] | SOD2 (rs4880), CAT (rs1001179), GPX1 (rs1050450) | OS |
| Novais, 2021 [71] | XRCC1 (rs25487), HOGG1 (rs1052133), CYP1A1 (rs1048943), GSTM1 (rs4025935), GSTT1 (rs71748309), GSTP1 (rs1695), NAT2 (*4) | OS, DFS |
| Pasvenskaite, 2021 [72] | IL-10 (rs1800871, rs1800872, rs1800896) | OS |
| Pasvenskaite, 2021 [73] | IL-9 (rs1859430, rs2069870, rs11741137, rs2069885, rs2069884) | OS |
| Wei, 2021 [74] | ERCC2 (rs13181) | OS, DFS |
| Zhu, 2021 [75] | UCA1 (rs7255437) | DSS |
OS — overall survival; PFS — progression-free survival; DFS — disease-free survival; DSS — disease-specific survival
Carcinogen-metabolizing enzymes
In general, different gene polymorphisms of glutathione-S-transferases (GSTs), including GSTM1 deletion, GSTT1 deletion, GSTP1 rs1695 and GSTP1 rs749174, were not associated with survival in HNSCCs [14, 34, 63, 68, 71]. In one study, the non-null variant of GSTT1 deletion polymorphism was significantly associated with poor OS and DSS [14]. In cytochrome P-450 (CYP) family, the CYP2A6 *4B, *4C and *9 polymorphisms were associated with poor OS compared to common alleles [65].
DNA repair
In HNSCCs, in most studies, the XRCC1 rs25487 polymorphism was not associated with survival [4, 14, 19, 39, 48, 51, 52, 62, 64, 67, 68, 71], although, in a few studies, this polymorphism was significantly associated with OS [16, 21, 34]; the results on the favorable variant in these studies were inconsistent so that the GG genotype was associated with worse OS compared to GA + AA genotypes in two studies [16, 21] and the GA + AA variant was associated with worse OS in one study [34]. In the same way, in most studies, the XRCC1 rs1799782 polymorphism was not significantly associated with survival [7, 14, 51, 52]; in one study, CT + TT variant was significantly associated with OS, but not DFS, compared to CC genotype in OSCC patients [64]. The ERCC1 rs11615 polymorphism was not significantly associated with survival [30, 35, 51, 56, 60, 67, 68]. In most studies, the ERCC1 rs3212986 polymorphism was not associated with survival [21, 34, 60, 68]; in studies with a significant association, there is no agreement on the favorable variant so that in one study, the CC genotype was associated with poor PFS compared to CA + AA variant in NPC [39] while in another study, CA + AA variant was associated with worse OS compared to CC genotype in pharyngolaryngeal SCC (PLSCC) patients [4]. In two studies, the ERCC1 rs735482 polymorphism was significantly associated with survival [19, 60]; the CC genotype was significantly associated with poor DFS, but not OS, compared to AC + AA genotypes in OSCC [60]. There are conflicting results regarding the association between ERCC2/XPD rs13181 and rs1799793, ERCC5/XPG rs1047768 and rs17655, XRCC3 rs861539, RAD51 rs1801320 polymorphisms with HNSCC prognosis; the ERCC2 rs13181 polymorphism was significantly associated with survival in some studies [21, 32, 48, 67, 74]; the AA genotype was associated with poor OS compared to AC + CC genotypes [21]; the AA genotype was associated with worse OS in stage III–IV HNSCCs treated with radiation compared to AC + CC genotypes but it was associated with better survival in stage III–IV HNSCC patients who were not treated with radiation; also, this polymorphism was not associated with OS in stage I–II HNSCC patients [32]. In contrast, the AA genotype was associated with a significantly better OS and/ or DFS compared to AC + CC genotypes [48, 74]; the CC genotype was associated with worse OS and DFS compared to AC + AA genotypes [67]. In a few studies, the ERCC2 rs1799793 polymorphism was significantly associated with survival [21, 67]; the GG genotype was the unfavorable variant in one study [21] and the favorable variant in another study [67]. In one study, the ERCC5 rs1047768 polymorphism was significantly associated with OS [19]. In some studies, the ERCC5 rs17655 polymorphism was significantly associated with survival [60, 67]; the CC genotype was significantly associated with worse DFS, but not OS, compared to GC + GG genotype in OSCC [60]; in another study, the GG genotype was significantly associated with better DFS compared to CG + CC genotypes [67]. In one study, the Thr allele of XRCC3 rs861539 polymorphism had significantly better DFS and DSS compared to the Met allele in irradiated LSCC [51]. The RAD51 rs1801320 polymorphism was significantly associated with DFS in non-irradiated OSCC and OPSCC so that the G allele had a better DFS compared to C allele [51]. Each of the hOGG1 rs1052133, XPC rs2228001, MSH2 rs3732183, hMLH1 rs1800734, RAD51 rs7180135, BRCA1 rs12516 and MUTYH rs3219489 polymorphisms was significantly associated with survival in HNSCCs in one study [45, 51, 52, 57, 59, 64].
Tumor suppressor genes/oncogenes
Given the key role of TP53 in the carcinogenesis process, it is not surprising that TP53 mutations can reduce the survival rate of HNSCC patients [27]. In two studies, the TP53 Arg72Pro (rs1042522) polymorphism was significantly associated with survival [10, 34]; HNSCC patients with a wild-type p53 allele had better OS and PFS compared to patients without wild-type allele; the OS and PFS were significantly different among patients with a wild-type 72R (Arg) allele, with a wild-type 72P (Pro) allele and with both wild-type alleles so that 72R allele had the best OS and PFS [10]; this polymorphism was associated with DFS in patients with stage I and II radiation-treated HNSCC so that the DFS was worse for each Pro allele when compared with the reference (Arg/Arg) [34]. The GT/GG variant of MDM2 rs2279744 polymorphism was significantly associated with poor PFS compared to TT genotype in NPC patients [39].
Anti- or pro-apoptotic regulators
The CC genotype of BCL-2-938C>A polymorphism was significantly associated with worse survival compared to the AA + CA genotypes [23, 54].
Cell cycle control
Results on the association between CCND1 rs603965 polymorphism and HNSCC prognosis were contradictory; in most studies, the GG genotype of this polymorphism was significantly associated with poor DFS compared to AA genotype in HNSCC patients [8, 9, 13, 20]; the AA genotype was significantly associated with better DFS and OS in LSCC compared to AG + GG genotypes [13]. In contrast, the GG genotype was associated with better OS in stage III–IV HNSCC patients who were not treated with radiation [32]. With regard to CCND1 rs678653 polymorphism, the CC genotype was significantly associated with poor DFS compared to GG genotype in one study [9]. The VDR FokI (rs10735810) [31], AKT2 rs8100018, AKT1 rs3803304 and PTEN rs12569998 [49] polymorphisms were significantly associated with survival. The TT genotype of VDR rs10735810 polymorphism was associated with poor PFS [31]. The GG genotype of AKT2 rs8100018 polymorphism was associated with a significantly worse OS and PFS compared to CC genotype. The CG+GG genotypes of AKT1 rs3803304 polymorphism had significantly better OS compared to CC genotype [49].
Antioxidant gene
The SOD2 rs4880, CAT rs1001179 and GPX1 rs1050450 polymorphisms were not associated with survival [68, 70].
Inflammatory mediators
Results on the association between TNF-α polymorphisms and HNSCC prognosis were contradictory; in one study, the GG genotype of −308G>A polymorphism was associated with a significantly worse DFS compared to corresponding variant genotypes [47]; also, in one study, the TNF-α −857 and −1031 polymorphisms were significantly associated with DFS so that the −857 CC and −1031 TT genotypes had significantly worse DFS compared to corresponding variant genotypes [43]. The TNF-α −863 polymorphism was significantly associated with DFS so that the CC genotype was associated with a significantly worse DFS compared to corresponding variant genotypes [43, 47]. The BID5+ variant of TNFα TNFBID5 polymorphism was significantly associated with poor DFS [20]. The IL-9 rs1859430 polymorphism was significantly associated with OS so that the AA genotype was associated with poor OS compared to AG + GG genotypes [73]. Results on the association between IL-10 polymorphisms and HNSCC prognosis were contradictory; in one study, the CC genotype of IL-10 rs1800871 polymorphism (compared to CT + TT genotypes) and the CC genotype of IL-10 rs1800872 polymorphism (compared to CA + AA genotypes) were associated with a significantly better survival in HPV16+ OPSCC patients [41]. In HNSCC patients who received chemoradiotherapy without surgical treatment, the CC + CT genotypes of TGFβ1 rs1982073 polymorphism were significantly associated with a better DFS and OS in comparison with TT genotype [24, 26]. The TGFβ1 rs1800470 polymorphism was significantly associated with survival [36, 54]; the TT + CT genotypes were associated with a better OS compared to the CC variant [36]; in irradiated LSCCs, the TC+TT genotypes had a better DFS compared to the CC genotype [54]. The TGFβ1 rs1800469 polymorphism was significantly associated with DSS in irradiated OSCC/OPSCC patients so that the CC genotype had better DSS compared to TC+TT genotypes [54].
Angiogenesis
The CC genotype of VEGF rs2010963 polymorphism was significantly associated with poor OS and metastasis-free survival (MFS) compared to CG/GG genotypes [61]. The AA genotype of VEGF rs699947 polymorphism was significantly associated with poor local recurrence-free survival (LRFS), but not OS, compared to AC/CC genotypes [61]. The GG genotype of VEGF-A rs1570360 polymorphism was significantly associated with decreased OS in OSCCs [38]. The AA genotype of VEGFA rs13207351 polymorphism was significantly associated with poor OS compared to GG genotype in LSCC patients [66]. The TT genotype of VEGFR2 rs1870377 polymorphisms was significantly associated with poor DFS, but not OS, compared to TA+AA genotypes [61]. The GA/AA genotypes of ANGPT2 rs3739391 polymorphism and the CC genotype of ANGPT2 rs3020221 polymorphism were significantly associated with poor OS, but not DFS, compared to corresponding variants [61].
Growth control
In some studies, the FGFR4 rs351855 polymorphism was significantly associated with OS in HN-SCC patients (12, 22, 27); the Gly/Arg + Arg/Arg genotypes (Arg388 allele) were associated with poor OS compared to Gly/Gly genotype [12, 22, 27]. The TG/GG genotypes of KRAS rs61764370 polymorphism were significantly associated with poor PFS compared to the TT genotype in HNSCC patients who were treated with cisplatin + placebo or cetuximab [44]. In one study, the G/G genotype of EGF A61G polymorphism was significantly associated with poor OS and PFS compared to G/A or A/A genotypes in PLSCC but this association did not exist for OSCC [46]. There are conflicting results regarding EGFR R521K polymorphism; in some studies, the K-allele carriers had shorter OS/PFS compared to HNSCC patients with RR genotype [37, 55]; in one study, the RR/RK genotypes were significantly associated with poor PFS compared to KK genotype in PLSCC but this association did not exist for OSCC [46].
Non-coding RNA
Results on the association between miRNAs polymorphisms and HNSCC prognosis are contradictory; in one study, the hsa-mir-146a rs2910164 polymorphism was significantly associated with DSS and DFS in OPSCC so that the GG genotype had better DSS and DFS compared to the CG + CC variant [40]; also, in one study, the hsa-mir-149 rs2292832 polymorphism was significantly associated with survival so that the CC genotype had better OS, DSS and DFS compared to the CT/TT genotypes in non-OPSCCs [53]. The hsa-mir-196a2 rs11614913 polymorphism was significantly associated with survival in OPSCC so that the CT + TT variant had better OS, DSS and DFS compared to the CC genotype [40]; the TT genotype of this polymorphism was associated with poor DFS in OSCC patients compared to the CT + CC genotypes [42]. In one study, the hsa-mir-499 rs3746444 polymorphism was significantly associated with survival so that the TT genotype had better OS, DSS and DFS compared to the CT/CC genotypes in non-OPSCCs [53]. The NEAT1 rs3741384 and UCA1 rs7255437 polymorphisms were significantly associated with DSS in OSCC patients so that the GG genotype of NEAT1 rs3741384 polymorphism and TC + TT genotypes of UCA1 rs7255437 were associated with poor DSS [75].
Invasion and metastasis
The 1G/1G genotype of MMP-1–1607 1G/2G polymorphism was significantly associated with better OS compared to 1G/2G+2G/2G genotype in NPSCC [17]. The MMP-2 rs12934241 polymorphism was significantly associated with OS and DFS; the CT+TT genotypes were associated with poor OS and DFS compared to CC genotype [68].
Regulation of immune response
In HNSCCs, the Asp/Gly variant of TLR4 Asp299Gly polymorphism was significantly associated with reduced DFS and OS. The Thr/Ile variant of TLR4 Thr399Ile polymorphism was significantly associated with reduced DFS [29]. The AA genotype of CTLA4 A49G polymorphism was significantly associated with poorer OS [18]. In another study, the GG+AG genotypes of this polymorphism had poorer OS compared with the AA genotype [34]. HNSCC patients with 131H/H genotype of FCGR2A H131R polymorphism and/or 157V/V genotype of FCGR3A V157F polymorphism had significantly better PFS compared to patients carrying 131R and 157F alleles [58].
Multidrug resistance
The AT/AA variant of ABCB1 rs2032582 polymorphism was significantly associated with poor PFS compared to other variants in NPC patients [39]. The ABCC2 rs717620 polymorphism was significantly associated with OS and DFS so that the GA+AA variant was associated with poor OS and DFS compared to the GG genotype [68]. The SLC28A1/CNT1 rs2242047 polymorphism was significantly associated with OS and DFS so that the GA+AA variant was associated with better OS and DFS compared to the GG genotype [68].
Discussion
Various factors have been attributed to prognosis of HNSCCs including staging, grading, tumor site, health status, age, gender, race, comorbidities, alcohol drinking and tobacco consumption, lymph node metastasis and HPV positivity [5, 6]. Even with relatively similar clinical features and treatments, the prognosis of HNSCCs may vary widely. In recent years, gene polymorphisms have been suggested as at least parts of the source of this variable prognosis. In a polygenic mechanism, these polymorphisms with their corresponding alleles can contribute to varied prognosis; in fact, these alleles are low-penetrance alleles (each with a small risk) that combine together to cause varied cancer prognosis. Some believe that since the frequency of these polymorphic alleles is relatively high, the role of them in cancer prognosis can be quite high, even if their penetrance is low. Also, the importance of gene polymorphisms in cancer prognosis may become more pronounced when these polymorphisms are analyzed in specific subgroups of the population. The gene polymorphisms may cause variable prognosis through the differential response of tumors to treatment or through involvement in various carcinogenesis pathways [5–7]. For example, it has been reported that carriers of C allele of TGFβ1 rs1982073 polymorphism have elevated serum concentrations of TGFβ1 in comparison with TT genotype; the better survival of the C allele carriers after chemoradiotherapy can be justified by the fact that the elevated serum concentration of TGF-β1 may sensitize cancer cells to chemoradiotherapy [24, 26, 36]. Arginine to lysine substitution in R521K EGFR polymorphism leads to an EGFR variant that shows less affinity to its related ligand and less mitogenic activity. So, it has been hypothesized that EGFR gene polymorphisms may affect sensitivity to anti-EGFR treatment and prognosis [25, 37]. Sometimes, a dual function has been described for gene polymorphisms; for example, the ERCC1 gene and associated protein (as a part of DNA repair pathway) regulates cell sensitivity to cisplatin (cisplatin causes cytotoxicity through formation of DNA adducts which blocks nucleotide replication and transcription) which has been correlated with chemo-radiation-resistance. Lower ERCC1 expression (as a result of functional gene polymorphism in ERCC1 gene) has been reported to correlate with better prognosis in some cancers; at the same time it may be associated with the accumulation of DNA damage and results in a more aggressive behavior of tumor which implicates a dual effect in terms of prognosis [4, 30, 35, 60]. Invasion and metastasis affect clinical outcome of HNSCC. Invasion and metastasis are dependent on angiogenesis. VEGF/VEGFR genes and ANGPT/TEK genes play key roles in angiogenesis and are over-expressed in different human cancers including HNSCC. Functional SNPs in these genes are associated with high or low expression level of their related proteins. For example, the −2578C, −1154A or −634G variant alleles have been linked with the low VEGF expression. Consequently, it can affect the angiogenesis process and may result in variations of tumor progression and clinical outcomes [38, 61, 66]. Function of some growth control genes like FGFR4 also involves up-regulation of proteolytic enzymes required for cell migration; overexpression of these genes has been suggested as a possible mechanism in cancer progression. Some variant alleles (like the Arg388 allele of FGFR4 Gly388Arg polymorphism) increase the gene expression (e.g. FGFR4) and may increase the aggressive behavior of cancer cells and, consequently, may affect HNSCC prognosis [27]. Polymorphisms in the promoter region of the genes related to inflammatory mediators (like TNF-α gene) are implicated in the regulation of expression level of its related cytokine. Such a polymorphism has been proposed to be linked with the prognosis in cancers (such as gastric and colorectal cancers) [28, 43, 47]. GSTs are a group of phase II detoxification enzymes. Genetic polymorphisms of GSTs have probably some impact on HNSCC risk by regulating the efficacy of detoxification of carcinogens derived from cigarette smoking. Based on these evidences, it has been hypothesized that polymorphism of these genes may also be involved in HNSCC prognosis [14, 34]. Expression of anti-apoptotic proteins (like BCL-2) has been associated with better local control and survival in HNSCCs. A regulatory polymorphism (like BCL2 −938C>A) in gene promoter produces different promoter function and activity which may be associated with outcome in HNSCC patients [23]. Variants of cell cycle regulatory genes like CCND1 may promote alternative splicing of transcript which produces truncated proteins that lack regulatory motifs. This results in protein degradation and nuclear export which may have some impact on cancer survival [32]. The importance of the epigenetic changes in tumors including HNSCCs is apparent. DNA methylation (as an epigenetic change) is regulated by a family of enzymes called DNA methyltransferases (DNMTs). The DNMT gene polymorphism may be associated with aberrant DNA methylation in HNSCCs and, consequently, affects survival as reported in a study by Supic et al. [77]. Research has suggested miRNAs (miR), such as miR-149, suppress tumor cell mobility. The pre-miR gene polymorphism may affect the processing of miR (for example, T variant of pri-mir-149 polymorphism shows a low processing efficacy) which results in a lower frequency of the mature form of miRNA, which consequently regulates tumor progression and HNSCC survival [78].
Conclusion
HNSCC prognosis may be affected by deregulations of different pathways and several studies have assessed the gene polymorphisms involved in these pathways which have been associated with different and sometimes contradictory results. In order to analyze the association between gene polymorphisms and HNSCC prognosis and to overcome these contradictory results, further studies along with conducting meta-analyses are necessary.
Footnotes
Declaration
All authors have viewed and agreed to the submission.
Conflict of interest
None declared.
Funding
None declared.
References
- 1.Liu Z, Li G, Wei S, et al. Genetic variants in selected pre-microRNA genes and the risk of squamous cell carcinoma of the head and neck. Cancer. 2010;116(20):4753–4760. doi: 10.1002/cncr.25323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fernández-Mateos J, Seijas-Tamayo R, Klain JC, et al. Analysis of autophagy gene polymorphisms in Spanish patients with head and neck squamous cell carcinoma. Sci Rep. 2017;7(1):6887. doi: 10.1038/s41598-017-07270-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Faghih Z, Abtahi S, Khademi B, et al. Association of OX40 gene polymorphisms (rs17568G/A and rs229811A/C) with head and neck squamous cell carcinoma. Mol Biol Rep. 2019;46(3):2609–2616. doi: 10.1007/s11033-019-04602-3. [DOI] [PubMed] [Google Scholar]
- 4.Hirakawa H, Ikegami T, Azechi S, et al. ERCC1 C8092A polymorphism predicts fair survival outcome in Japanese patients with pharyngo-laryngeal squamous cell carcinoma. Eur Arch Otorhinolaryngol. 2020;277(2):601–610. doi: 10.1007/s00405-019-05731-y. [DOI] [PubMed] [Google Scholar]
- 5.Hopkins J, Cescon DW, Tse D, et al. Genetic polymorphisms and head and neck cancer outcomes: a review. Cancer Epidemiol Biomarkers Prev. 2008;17(3):490–499. doi: 10.1158/1055-9965.EPI-07-2714. [DOI] [PubMed] [Google Scholar]
- 6.Chen Fa, He B, Yan L, et al. FADS1 rs174549 Polymorphism May Predict a Favorable Response to Chemoradiotherapy in Oral Cancer Patients. J Oral Maxillofac Surg. 2017;75(1):214–220. doi: 10.1016/j.joms.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Nanda SS, Gandhi AK, Rastogi M, et al. Evaluation of XRCC1 Gene Polymorphism as a Biomarker in Head and Neck Cancer Patients Undergoing Chemoradiation Therapy. Int J Radiat Oncol Biol Phys. 2018;101(3):593–601. doi: 10.1016/j.ijrobp.2018.03.039. [DOI] [PubMed] [Google Scholar]
- 8.Matthias C, Branigan K, Jahnke V, et al. Polymorphism within the cyclin D1 gene is associated with prognosis in patients with squamous cell carcinoma of the head and neck. Clinic Cancer Res. 1998;4(10):2411–8. [PubMed] [Google Scholar]
- 9.Holley SL, Parkes G, Matthias C, et al. Cyclin D1 polymorphism and expression in patients with squamous cell carcinoma of the head and neck. Am J Pathol. 2001;159(5):1917–1924. doi: 10.1016/S0002-9440(10)63038-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sullivan A, Syed N, Gasco M, et al. Polymorphism in wild-type p53 modulates response to chemotherapy in vitro and in vivo. Oncogene. 2004;23(19):3328–3337. doi: 10.1038/sj.onc.1207428. [DOI] [PubMed] [Google Scholar]
- 11.Wang L, Rodriguez M, Kim ES, et al. A novel C/T polymorphism in the core promoter of human de novo cytosine DNA methyltransferase 3B6 is associated with prognosis in head and neck cancer. Int J Oncol. 2004;25(4):993–1002. [PubMed] [Google Scholar]
- 12.Streit S, Bange J, Fichtner A, et al. Involvement of the FGFR4 Arg388 allele in head and neck squamous cell carcinoma. Int J Cancer. 2004;111(2):213–217. doi: 10.1002/ijc.20204. [DOI] [PubMed] [Google Scholar]
- 13.Monteiro E, Varzim G, Pires AM, et al. Cyclin D1 A870G polymorphism and amplification in laryngeal squamous cell carcinoma: implications of tumor localization and tobacco exposure. Cancer Detect Prev. 2004;28(4):237–243. doi: 10.1016/j.cdp.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Geisler SA, Olshan AF, Cai J, et al. Glutathione S-transferase polymorphisms and survival from head and neck cancer. Head Neck. 2005;27(3):232–242. doi: 10.1002/hed.20141. [DOI] [PubMed] [Google Scholar]
- 15.Etienne-Grimaldi MC, Pereira S, Magné N, et al. Analysis of the dinucleotide repeat polymorphism in the epidermal growth factor receptor (EGFR) gene in head and neck cancer patients. Ann Oncol. 2005;16(6):934–941. doi: 10.1093/annonc/mdi189. [DOI] [PubMed] [Google Scholar]
- 16.Gal TJ, Huang WY, Chen C, et al. DNA repair gene polymorphisms and risk of second primary neoplasms and mortality in oral cancer patients. Laryngoscope. 2005;115(12):2221–2231. doi: 10.1097/01.mlg.0000183736.96004.f7. [DOI] [PubMed] [Google Scholar]
- 17.Kondo S, Wakisaka N, Schell MJ, et al. Epstein-Barr virus latent membrane protein 1 induces the matrix metalloproteinase-1 promoter via an Ets binding site formed by a single nucleotide polymorphism: enhanced susceptibility to nasopharyngeal carcinoma. Int J Cancer. 2005;115(3):368–376. doi: 10.1002/ijc.20849. [DOI] [PubMed] [Google Scholar]
- 18.Wong YK, Chang KW, Cheng CY, et al. Association of CTLA-4 gene polymorphism with oral squamous cell carcinoma. J Oral Pathol Med. 2006;35(1):51–54. doi: 10.1111/j.1600-0714.2005.00377.x. [DOI] [PubMed] [Google Scholar]
- 19.Carles J, Monzo M, Amat M, et al. Single-nucleotide polymorphisms in base excision repair, nucleotide excision repair, and double strand break genes as markers for response to radiotherapy in patients with Stage I to II head- and-neck cancer. Int J Radiat Oncol Biol Phys. 2006;66(4):1022–1030. doi: 10.1016/j.ijrobp.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 20.Matthias C, Harréus U, Strange R. Influential factors on tumor recurrence in head and neck cancer patients. Eur Arch Otorhinolaryngol. 2006;263(1):37–42. doi: 10.1007/s00405-005-0947-9. [DOI] [PubMed] [Google Scholar]
- 21.Quintela-Fandino M, Hitt R, Medina PP, et al. DNA-repair gene polymorphisms predict favorable clinical outcome among patients with advanced squamous cell carcinoma of the head and neck treated with cisplatin-based induction chemotherapy. J Clin Oncol. 2006;24(26):4333–4339. doi: 10.1200/JCO.2006.05.8768. [DOI] [PubMed] [Google Scholar]
- 22.da Costa Andrade VC, Parise O, Hors CP, et al. The fibroblast growth factor receptor 4 (FGFR4) Arg388 allele correlates with survival in head and neck squamous cell carcinoma. Exp Mol Pathol. 2007;82(1):53–57. doi: 10.1016/j.yexmp.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 23.Lehnerdt GF, Franz P, Bankfalvi A, et al. The regulatory BCL2 promoter polymorphism (−938C>A) is associated with relapse and survival of patients with oropharyngeal squamous cell carcinoma. Ann Oncol. 2009;20(6):1094–1099. doi: 10.1093/annonc/mdn763. [DOI] [PubMed] [Google Scholar]
- 24.Lundberg M, Pajusto M, Koskinen WJ, et al. Association between transforming growth factor beta1 genetic polymorphism and response to chemoradiotherapy in head and neck squamous cell cancer. Head Neck. 2009;31(5):664–672. doi: 10.1002/hed.21014. [DOI] [PubMed] [Google Scholar]
- 25.Klinghammer K, Knödler M, Schmittel A, et al. Association of epidermal growth factor receptor polymorphism, skin toxicity, and outcome in patients with squamous cell carcinoma of the head and neck receiving cetuximab-docetaxel treatment. Clin Cancer Res. 2010;16(1):304–310. doi: 10.1158/1078-0432.CCR-09-1928. [DOI] [PubMed] [Google Scholar]
- 26.Lundberg M, Saarilahti K, Mäkitie AA, et al. TGFbeta1 genetic polymorphism is associated with survival in head and neck squamous cell carcinoma independent of the severity of chemoradiotherapy induced mucositis. Oral Oncol. 2010;46(5):369–372. doi: 10.1016/j.oraloncology.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 27.Tanuma JI, Izumo T, Hirano M, et al. FGFR4 polymorphism, TP53 mutation, and their combinations are prognostic factors for oral squamous cell carcinoma Oncol Rep 2010233739–744.. [PubMed] [Google Scholar]
- 28.Corrêa GT, Bandeira GA, Cavalcanti BG, et al. Association of −308 TNF-α promoter polymorphism with clinical aggressiveness in patients with head and neck squamous cell carcinoma. Oral Oncol. 2011;47(9):888–894. doi: 10.1016/j.oraloncology.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 29.Bergmann C, Bachmann HS, Bankfalvi A, et al. Toll-like receptor 4 single-nucleotide polymorphisms Asp299Gly and Thr399Ile in head and neck squamous cell carcinomas. J Transl Med. 2011;9:139. doi: 10.1186/1479-5876-9-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Castro G, Pasini FS, Siqueira SA, et al. ERCC1 protein, mRNA expression and T19007C polymorphism as prognostic markers in head and neck squamous cell carcinoma patients treated with surgery and adjuvant cisplatin-based chemoradiation. Oncol Rep. 2011;25(3):693–699. doi: 10.3892/or.2011.1133. [DOI] [PubMed] [Google Scholar]
- 31.Hama T, Norizoe C, Suga H, et al. Prognostic significance of vitamin D receptor polymorphisms in head and neck squamous cell carcinoma. PLoS One. 2011;6(12):e29634. doi: 10.1371/journal.pone.0029634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhong S, Nukui T, Buch S, et al. Effects of ERCC2 Lys751Gln (A35931C) and CCND1 (G870A) polymorphism on outcome of advanced-stage squamous cell carcinoma of the head and neck are treatment dependent. Cancer Epidemiol Biomarkers Prev. 2011;20(11):2429–2437. doi: 10.1158/1055-9965.EPI-11-0520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang WY, Chien YC, Wong YK, et al. Effects of KRAS mutation and polymorphism on the risk and prognosis of oral squamous cell carcinoma. Head Neck. 2012;34(5):663–666. doi: 10.1002/hed.21792. [DOI] [PubMed] [Google Scholar]
- 34.Azad AK, Bairati I, Samson E, et al. Validation of genetic sequence variants as prognostic factors in early-stage head and neck squamous cell cancer survival. Clin Cancer Res. 2012;18(1):196–206. doi: 10.1158/1078-0432.CCR-11-1759. [DOI] [PubMed] [Google Scholar]
- 35.Lima LM, de Souza LR, da Silva TF, et al. DNA repair gene excision repair cross complementing-group 1 (ERCC1) in head and neck squamous cell carcinoma: analysis of methylation and polymorphism (G19007A), protein expression and association with epidemiological and clinicopathological factors. Histopathology. 2012;60(3):489–496. doi: 10.1111/j.1365-2559.2011.04062.x. [DOI] [PubMed] [Google Scholar]
- 36.Lundberg M, Leivo I, Saarilahti K, et al. Transforming growth factor beta 1 genotype and p16 as prognostic factors in head and neck squamous cell carcinoma. Acta Otolaryngol. 2012;132(9):1006–1012. doi: 10.3109/00016489.2012.678944. [DOI] [PubMed] [Google Scholar]
- 37.Stoehlmacher-Williams J, Obermann L, Ehninger G, et al. Polymorphisms of the epidermal growth factor receptor (EGFR) and survival in patients with advanced cancer of the head and neck (HNSCC) Anticancer Res 2012322421–425.. [PubMed] [Google Scholar]
- 38.Supic G, Jovic N, Zeljic K, et al. Association of VEGF-A genetic polymorphisms with cancer risk and survival in advanced-stage oral squamous cell carcinoma patients. Oral Oncol. 2012;48(11):1171–1177. doi: 10.1016/j.oraloncology.2012.05.023. [DOI] [PubMed] [Google Scholar]
- 39.Liu H, Qi B, Guo X, et al. Genetic variations in radiation and chemotherapy drug action pathways and survival in locoregionally advanced nasopharyngeal carcinoma treated with chemoradiotherapy. PLoS One. 2013;8(12):e82750. doi: 10.1371/journal.pone.0082750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guan X, Sturgis EM, Song X, et al. Pre-microRNA variants predict HPV16-positive tumors and survival in patients with squamous cell carcinoma of the oropharynx. Cancer Lett. 2013;330(2):233–240. doi: 10.1016/j.canlet.2012.11.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jin L, Sturgis EM, Cao X, et al. Interleukin-10 promoter variants predict HPV-positive tumors and survival of squamous cell carcinoma of the oropharynx. FASEB J. 2013;27(6):2496–2503. doi: 10.1096/fj.12-226803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu CJ, Tsai MM, Tu HF, et al. miR-196a overexpression and miR-196a2 gene polymorphism are prognostic predictors of oral carcinomas. Ann Surg Oncol. 2013;20(Suppl 3):S406–S414. doi: 10.1245/s10434-012-2618-6. [DOI] [PubMed] [Google Scholar]
- 43.Zhang C, Sturgis EM, Zheng H, et al. TNF-α promoter polymorphisms and risk of recurrence in patients with squamous cell carcinomas of the nonoropharynx. Int J Cancer. 2014;135(7):1615–1624. doi: 10.1002/ijc.28793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chung CH, Lee JW, Slebos RJ, et al. A 3′-UTR KRAS-variant is associated with cisplatin resistance in patients with recurrent and/or metastatic head and neck squamous cell carcinoma. Ann Oncol. 2014;25(11):2230–2236. doi: 10.1093/annonc/mdu367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lin LH, Lin MW, Mar K, et al. The hMLH1-93G>A promoter polymorphism is associates with outcomes in oral squamous cell carcinoma patients. Ann Surg Oncol. 2014;21(13):4270–4277. doi: 10.1245/s10434-014-3897-x. [DOI] [PubMed] [Google Scholar]
- 46.Su NW, Leu YS, Lee JC, et al. EGF and EGFR genetic polymorphisms predict prognosis in locally advanced pharyngolaryngeal squamous cell carcinoma patients receiving postoperative concurrent chemoradiotherapy. Onco Targets Ther. 2014;7:2197–2204. doi: 10.2147/OTT.S70188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang C, Sturgis EM, Zheng H, et al. Genetic variants in TNF-α promoter are predictors of recurrence in patients with squamous cell carcinoma of oropharynx after definitive radiotherapy. Int J Cancer. 2014;134(8):1907–1915. doi: 10.1002/ijc.28512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Farnebo L, Stjernström A, Fredrikson M, et al. DNA repair genes XPC, XPD, XRCC1, and XRCC3 are associated with risk and survival of squamous cell carcinoma of the head and neck. DNA Repair (Amst) 2015;31:64–72. doi: 10.1016/j.dnarep.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 49.Pfisterer K, Fusi A, Klinghammer K, et al. PI3K/PTEN/ AKT/mTOR polymorphisms: association with clinical outcome in patients with head and neck squamous cell carcinoma receiving cetuximab-docetaxel. Head Neck. 2015;37(4):471–478. doi: 10.1002/hed.23604. [DOI] [PubMed] [Google Scholar]
- 50.Reuter T, Warta R, Theile D, et al. Role of NR1I2 (pregnane X receptor) polymorphisms in head and neck squamous cell carcinoma. Naunyn Schmiedebergs Arch Pharmacol. 2015;388(11):1141–1150. doi: 10.1007/s00210-015-1150-1. [DOI] [PubMed] [Google Scholar]
- 51.Stur E, Agostini LP, Garcia FM, et al. Prognostic significance of head and neck squamous cell carcinoma repair gene polymorphism. Genet Mol Res. 2015;14(4):12446–12454. doi: 10.4238/2015.October.16.11. [DOI] [PubMed] [Google Scholar]
- 52.Costa EF, Santos ES, Liutti VT, et al. Association between polymorphisms in genes related to DNA base-excision repair with risk and prognosis of oropharyngeal squamous cell carcinoma. J Cancer Res Clin Oncol. 2016;142(9):1917–1926. doi: 10.1007/s00432-016-2202-8. [DOI] [PubMed] [Google Scholar]
- 53.Wang C, Sturgis EM, Chen X, et al. Pre-miRNA variants as predictors of clinical outcome in patients with squamous cell carcinomas of the nonoropharynx. Oncotarget. 2016;7(18):26444–26453. doi: 10.18632/oncotarget.8512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Agostini LP, Stur E, Garcia FM, et al. ATM, BCL2, and TGFβ Gene Polymorphisms as Radiotherapy Outcome Biomarkers in Head and Neck Squamous Cell Carcinoma Patients. Genet Test Mol Biomarkers. 2017;21(12):727–735. doi: 10.1089/gtmb.2017.0180. [DOI] [PubMed] [Google Scholar]
- 55.Braig F, Kriegs M, Voigtlaender M, et al. Cetuximab Resistance in Head and Neck Cancer Is Mediated by EGFR-K Polymorphism. Cancer Res. 2017;77(5):1188–1199. doi: 10.1158/0008-5472.CAN-16-0754. [DOI] [PubMed] [Google Scholar]
- 56.Lopes-Aguiar L, Costa EF, Nogueira GA, et al. XPD c.934G>A polymorphism of nucleotide excision repair pathway in outcome of head and neck squamous cell carcinoma patients treated with cisplatin chemoradiation. Oncotarget. 2017;8(10):16190–16201. doi: 10.18632/oncotarget.7668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhu L, Sturgis EM, Zhang H, et al. Genetic variants in microRNA-binding sites of DNA repair genes as predictors of recurrence in patients with squamous cell carcinoma of the oropharynx. Int J Cancer. 2017;141(7):1355–1364. doi: 10.1002/ijc.30849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Magnes T, Melchardt T, Hufnagl C, et al. The influence of FCGR2A and FCGR3A polymorphisms on the survival of patients with recurrent or metastatic squamous cell head and neck cancer treated with cetuximab. Pharmacogenomics J. 2018;18(3):474–479. doi: 10.1038/tpj.2017.37. [DOI] [PubMed] [Google Scholar]
- 59.Senghore T, Wang WC, Chien HT, et al. Polymorphisms of Mismatch Repair Pathway Genes Predict Clinical Outcomes in Oral Squamous Cell Carcinoma Patients Receiving Adjuvant Concurrent Chemoradiotherapy. Cancers (Basel) 2019;11(5) doi: 10.3390/cancers11050598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Senghore T, Chien HT, Wang WC, et al. Polymorphisms in rs17655 and rs735482 Genes Associated with the Survival of Male Patients with Postoperative Oral Squamous Cell Carcinoma Treated with Adjuvant Concurrent Chemoradiotherapy. J Clin Med. 2019;8(1) doi: 10.3390/jcm8010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Butkiewicz D, Gdowicz-Kłosok A, Krześniak M, et al. Association of Genetic Variants in ANGPT/TEK and VEGF/VEGFR with Progression and Survival in Head and Neck Squamous Cell Carcinoma Treated with Radiotherapy or Radiochemotherapy. Cancers (Basel) 2020;12(6) doi: 10.3390/cancers12061506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dutta D, Abarna R, Shubham M, et al. Effect of Arg399Gln single-nucleotide polymorphism in gene on survival rate of Indian squamous cell head-and-neck cancer patients. J Cancer Res Ther. 2020;16(3):551–558. doi: 10.4103/jcrt.JCRT_476_18. [DOI] [PubMed] [Google Scholar]
- 63.Maniglia MP, Russo A, Biselli-Chicote PM, et al. Glutathione S-transferase Polymorphisms in Head and Neck Squamous Cell Carcinoma Treated with Chemotherapy and/or Radiotherapy. Asian Pac J Cancer Prev. 2020;21(6):1637–1644. doi: 10.31557/APJCP.2020.21.6.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Senghore T, Chien HT, Wang WC, et al. Predictive value of genetic variants XRCC1 rs1799782, APEX1 rs1760944, and MUTYH rs3219489 for adjuvant concurrent chemoradiotherapy outcomes in oral squamous cell carcinoma patients. Pharmacogenomics J. 2020;20(6):813–822. doi: 10.1038/s41397-020-0170-5. [DOI] [PubMed] [Google Scholar]
- 65.Yadav VK, Katiyar T, Ruwali M, et al. Polymorphism in cytochrome P4502A6 reduces the risk to head and neck cancer and modifies the treatment outcome. Environ Mol Mutagen. 2021;62(9):502–511. doi: 10.1002/em.22466. [DOI] [PubMed] [Google Scholar]
- 66.Dimitrakopoulos FI, Koliou GA, Kotoula V, et al. Genetic Variation in the ) Gene at rs13207351 Is Associated with Overall Survival of Patients with Head and Neck Cancer. Cancers (Basel) 2021;13(5) doi: 10.3390/cancers13051163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Guberina M, Sak A, Pöttgen C, et al. ERCC2 gene single-nucleotide polymorphism as a prognostic factor for locally advanced head and neck carcinomas after definitive cisplatin-based radiochemotherapy. Pharmacogenomics J. 2021;21(1):37–46. doi: 10.1038/s41397-020-0174-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Duran G, Cruz R, Aguín S, et al. Predictive value of ERCC2, ABCC2 and MMP2 of response and long-term survival in locally advanced head and neck cancer patients treated with chemoradiotherapy. Cancer Chemother Pharmacol. 2021;88(5):813–823. doi: 10.1007/s00280-021-04330-1. [DOI] [PubMed] [Google Scholar]
- 69.Jovic S, Zeljic K, Ivkovic N, et al. Cyclin D1 and p21 gene variants and oral squamous cell carcinoma risk and prognosis Arch Biol Sci 2021734437–445. 10.2298/abs210813037j. [DOI] [Google Scholar]
- 70.Lubiński J, Jaworowska E, Derkacz R, et al. Survival of Laryngeal Cancer Patients Depending on Zinc Serum Level and Oxidative Stress Genotypes. Biomolecules. 2021;11(6) doi: 10.3390/biom11060865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Novais O, Bezerra D, Barbosa A, et al. Polymorphisms in biotransformation and DNA repair genes, and survival on head and neck squamous cell carcinoma. Braz J Oncol. 2020 doi: 10.5935/2526-8732.20200048.. [DOI] [Google Scholar]
- 72.Pasvenskaite A, Liutkeviciene R, Gedvilaite G, et al. Impact of Promoter Polymorphisms and IL-10 Serum Levels on Advanced Laryngeal Squamous Cell Carcinoma and Survival Rate. Cancer Genomics Proteomics. 2021;18(1):53–65. doi: 10.21873/cgp.20241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pasvenskaite A, Liutkeviciene R, Gedvilaite G, et al. The Role of Polymorphisms and Serum IL-9 Levels in Carcinogenesis and Survival Rate for Laryngeal Squamous Cell Carcinoma. Cells. 2021;10(3) doi: 10.3390/cells10030601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wei Z, Yao M, Ning S, et al. The Association of Single-Nucleotide Polymorphism rs13181 in ERCC2 with Risk and Prognosis of Nasopharyngeal Carcinoma in an Endemic Chinese Population. Pharmgenomics Pers Med. 2021;14:359–367. doi: 10.2147/PGPM.S296215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhu L, He Y, Feng G, et al. Genetic variants in long non-coding RNAs UCA1 and NEAT1 were associated with the prognosis of oral squamous cell carcinoma. Int J Oral Maxillofac Surg. 2021;50(9):1131–1137. doi: 10.1016/j.ijom.2020.11.024. [DOI] [PubMed] [Google Scholar]
- 76.Fernández-Mateos J, Seijas-Tamayo R, Adansa Klain JC, et al. Genetic Susceptibility in Head and Neck Squamous Cell Carcinoma in a Spanish Population. Cancers (Basel) 2019;11(4) doi: 10.3390/cancers11040493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Supic G, Kozomara R, Zeljic K, et al. Prognostic value of the DNMTs mRNA expression and genetic polymorphisms on the clinical outcome in oral cancer patients. Clin Oral Investig. 2017;21(1):173–182. doi: 10.1007/s00784-016-1772-9. [DOI] [PubMed] [Google Scholar]
- 78.Tu HF, Liu CJ, Chang CL, et al. The association between genetic polymorphism and the processing efficiency of miR-149 affects the prognosis of patients with head and neck squamous cell carcinoma. PLoS One. 2012;7(12):e51606. doi: 10.1371/journal.pone.0051606. [DOI] [PMC free article] [PubMed] [Google Scholar]