Abstract
Patient: Female, 52-year-old
Final Diagnosis: Calcific tendinitis of gluteus medius
Symptoms: Right lateral hip pain
Medication: —
Clinical Procedure: —
Specialty: Orthopedics and Traumatology
Objective:
Rare disease
Background:
Calcific tendinitis of the hip is rare but most commonly occurs in the gluteus medius. It occurs more frequently in women, usually between the ages of 40 and 70 years. Calcific tendinitis of the gluteus medius is associated with pain and tenderness in the greater trochanter region, can be acute or chronic, and should be distinguished from other differential diagnoses, such as trochanteric bursitis. Calcific tendinitis of the gluteus medius is scarcely reported in the literature, and there is no management guideline for this condition. Although it is usually managed conservatively, there are reports of more invasive techniques, such as needle lavage and surgery.
Case Report:
We report the case of a middle-aged woman who presented with right hip pain of a 1-year duration, mainly on climbing stairs. Plain radiograph and magnetic resonance imaging revealed calcific tendinitis of the right gluteus medius. She underwent a trial of conservative management, which included a triamcinolone injection, but remained symptomatic. She subsequently underwent endoscopic debridement of the calcification and recovered uneventfully after surgery, with complete resolution of her symptoms at the 2-month follow-up.
Conclusions:
This report has shown the importance of imaging in the diagnosis of calcific tendinitis of the gluteus medius and supports endoscopic debridement as an effective modality in the management of this condition.
Keywords: Buttocks; Calcification, Physiologic; Endoscopes; Tendinopathy
Background
Calcific tendinitis is caused by the accumulation of calcium hydroxyapatite crystals [1] in peri-articular musculature attachment sites. It most often occurs in people aged 40 to 70 years [1,2]. Risk factors include an inciting trauma, which could be repetitive, as well as metabolic and autoimmune disorders, such as rheumatoid arthritis [1]. Occurring most often in the shoulder, calcific tendinitis has been less commonly reported in the hip, usually with the gluteus medius being implicated [3].
In calcific tendinitis of the gluteus medius, patients will usually have lateral-sided hip pain, limitation of movement, abductor weakness, and resultant gait abnormalities [4]. Other differential diagnoses of lateral-sided hip pain include noncalcific tendinitis, trochanteric bursitis, infection, lumbar spinal disease, osteoarthritis, and tumor.
There are several useful imaging modalities, starting with first-line plain radiographs, and further evaluation with ultrasound, computer tomography (CT) or magnetic resonance imaging (MRI) [5]. Imaging of the hip characteristically shows edema of the gluteus medius and calcifications lateral or superior to the greater trochanter [4].
Previous case reports have described various ways of treating calcific tendinitis of the gluteus medius, including oral analgesia [6,7], steroid injection [5,8], needle lavage [5,9], and surgery [1,10]. However, due to the paucity of literature on this condition, there is no available guideline for management.
Therefore, this report presents the case of a 57-year-old woman with a 1-year history of right lateral hip pain. A diagnosis of calcific tendinitis of the gluteus medius was made, and the patient’s case was successfully managed by endoscopic debridement.
Case Report
Our patient was a 57-year-old woman who presented with right lateral-sided hip pain for 1 year. This was made worse by walking, climbing stairs, and standing up from a sitting position. There was no history of trauma prior to the start of her symptoms, nor any red flag symptoms, such as recent unplanned loss of weight or appetite and fever. The patient was previously treated with triamcinolone injection to the affected region by a general practitioner, but there was only temporary pain relief. She has a past medical history of colon cancer diagnosed 8 years prior, which was in remission following curative resection with adjuvant chemotherapy.
On physical examination of her right hip, there was no visible deformity and she had full range of motion. She had a positive Trendelenburg test. The flexion-abduction-external rotation (FABER or Patrick’s) test and flexion-adduction-internal rotation (FADIR) test reproduced her pain, which was over the gluteus medius insertion just proximal to the greater trochanter.
Her pelvic radiograph revealed an approximately 4-cm calcification proximal to the superior tip of the greater trochanter (Figure 1). MRI confirmed the presence of the calcification at the myotendinous junction of the gluteus medius (Figure 2).
Figure 1.

Pelvic anteroposterior (AP) radiograph showing calcification over the right greater trochanter (red arrow).
Figure 2.
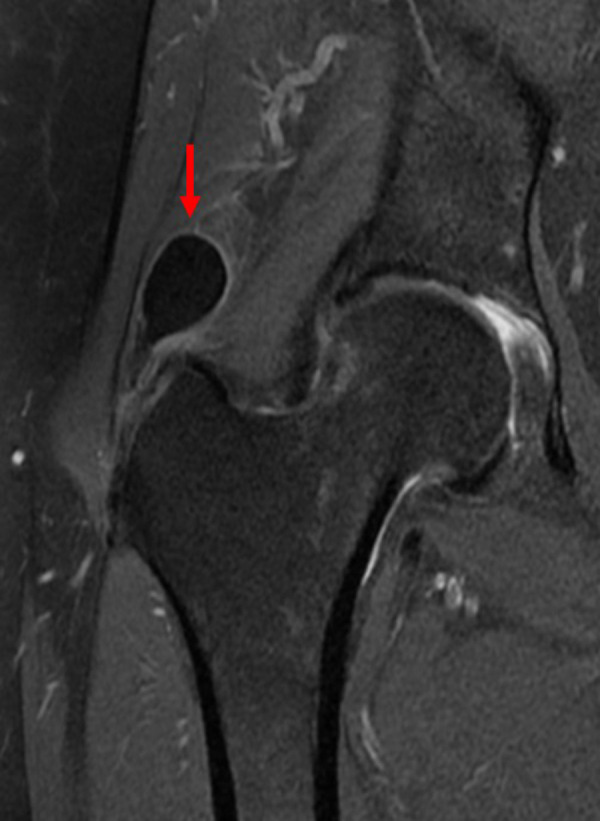
Proton density-weighted coronal image of right hip calcification (red arrow).
The patient was counseled regarding conservative treatment options, which included analgesia, physiotherapy, and ultra-sound-guided barbotage. However, given the protracted duration of her symptoms, she decided for surgical debridement of the calcification.
The patient underwent endoscopic debridement of the right hip gluteus medius calcification. This was done under general anesthesia, with the patient in the left lateral decubitus position. An intraoperative image intensifier was used to confirm the position of the calcification before superolateral and inferolateral portals were created. Endoscopic washout and debridement were performed, with clearance confirmed on the image intensifier (Figures 3, 4). Samples of the calcification and surrounding tissue were taken for histological assessment. Triamcinolone was injected into the affected area under endoscopic visualization before closure. There was no restriction of weight bearing or range of motion as part of her postoperative rehabilitation. She recovered well and was able to ambulate independently in the ward. She was discharged the day after her surgery.
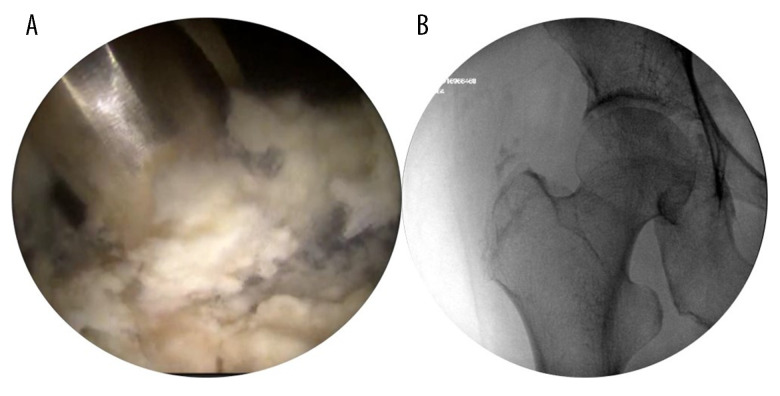
Figure 3.
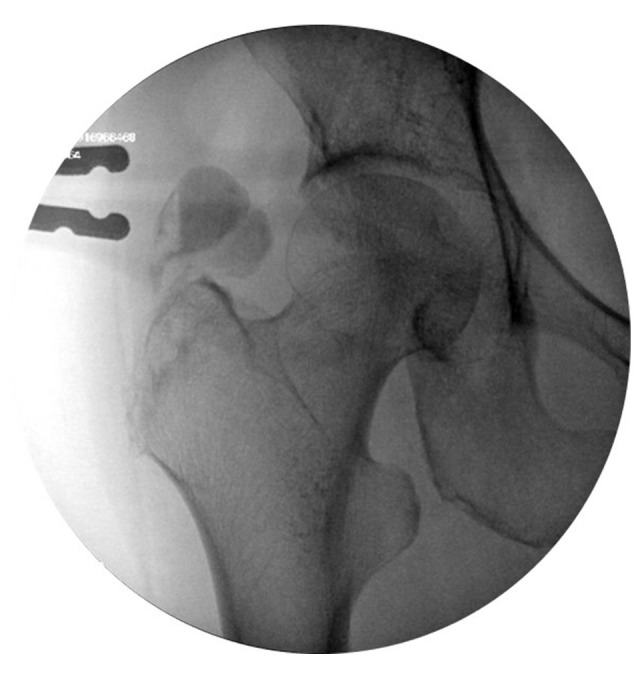
Intraoperative imaging showing air-fluid level within the lesion (patient in left lateral position).
Figure 4.
Endoscopic image showing debridement of the calcification (A), and intraoperative imaging after debridement showing clearance of the lesion (B).
The patient was seen in the clinic 2 weeks after the surgery. She reported complete resolution of her right hip pain. The surgical wounds had healed and the stitches were removed. Histological analysis of the tissue samples was reported as infarcted cartilage, muscle, and fat, with no evidence of malignancy. At 2 months after surgery, the patient remained asymptomatic and had resumed her normal daily activities.
Discussion
There are 2 key points that can be gleaned from this case. The first would be coming to the diagnosis of calcific tendinitis of the gluteus medius, and the second is its management.
Calcium hydroxyapatite crystal deposition can occur in various parts of the body. While it rarely occurs in the hip, the gluteus medius is one of the more commonly involved tendons [2,3] in such cases. Calcific tendinitis of the gluteus medius can present as either acute or chronic [7,11]. Patients who present acutely tend to experience significantly more pain, and the size of the calcifications on plain radiographs tend to be smaller [11].
In this case, the patient presented with mechanical lateral hip pain, which is similar to previous case reports [1,6,7,10]. However, it can occasionally present with groin or anterior thigh pain and buttock or posterolateral thigh pain [4]. The absence of preceding trauma is commonly reported, which may help to differentiate from myositis ossificans, which is often associated with trauma. Red flag symptoms such as fever, chills, and loss of appetite and weight, suggestive of infection or malignancy, are usually absent in calcific tendinitis of the gluteus medius, although a patient in one case was reported to have fever [7].
Tenderness over the greater trochanter, antalgic gait, and a positive Trendelenburg test are common signs present in calcific tendinitis of the gluteus medius [1,4–7,10]. The pain can be significant enough to cause restriction in range of motion. All these signs, along with a normal neurological examination, are suggestive of disease around the hip joint rather than the lumbar spine.
Once the pathology has been narrowed down to the hip, the necessary imaging investigations can be performed. In the present case, a plain radiograph of the affected hip was sufficient to demonstrate the presence of calcification over the greater trochanter and to rule out hip osteoarthritis as a source of pain. However, an MRI scan of the right hip was performed to localize the inflammation to the gluteus medius and rule out other differential diagnoses or concurrent hip pathology. Advanced imaging was commonly used in previous case reports as well [4–7,10] in the form of CT or MRI scans, which often show edema of the gluteus medius and surrounding hip muscles. Advanced imaging is useful to look for other pathologies, such as labral tears, infection, and malignancy.
While generally a self-limiting pathology [3,4,7], calcific tendinitis of the gluteus medius is known to persist for months in some cases [1,7]. Management of calcific tendinitis ranges from conservative to surgical options. Conservative treatment includes rest, analgesia, and physiotherapy [1,9], with a case series reporting a success rate of 80% [3]. There have been reports of treatment using minimally invasive techniques when conservative management has failed, such as ultrasound-guided needle lavage [5,8] or needle tenotomy with platelet-rich plasma injection [12], with good symptom relief.
Finally, surgical excision and debridement of the calcification can be considered if other modalities of treatment are unsuccessful. Endoscopic debridement of gluteus medius calcification has been rarely reported in the literature [1,3,10], while open surgery for this condition has not been reported, to the best of our knowledge. One advantage of endoscopic debridement is that it is less invasive, although it may be more technically demanding. Surgery is typically advocated for those with chronic symptoms and where the lesions are large and well-defined [3,11] and appears to result in good clinical outcomes [1,3,10].
Conclusions
Calcific tendinitis of the gluteus medius is an uncommon pathology that can mimic other conditions. A proper history, physical examination, and targeted imaging investigations are paramount in coming to the right diagnosis. Overall, owing to the small number of cases of gluteus medius calcific tendinitis in the literature, there are no definitive guidelines with regards to its treatment. However, some risk factors for failure of conservative management have been identified, in which endoscopic debridement can be considered in such cases. This report has shown the importance of imaging in the diagnosis of calcific tendinitis of the gluteus medius and supports endoscopic debridement as an effective modality in the management of this condition.
Footnotes
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Kandemir U, Bharam S, Philippon MJ, Fu FH. Endoscopic treatment of calcific tendinitis of gluteus medius and minimus. Arthroscopy. 2003;19(1):E4. doi: 10.1053/jars.2003.50021. [DOI] [PubMed] [Google Scholar]
- 2.Ellatif M, Razi F, Hogarth M, et al. Bilateral gluteus medius and minimus calcific tendonitis in a patient with previous bilateral calcific tendonitis of the shoulder: A case report. Radiol Case Rep. 2021;16(11):3222–25. doi: 10.1016/j.radcr.2021.07.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park SM, Baek JH, Ko YB, et al. Management of acute calcific tendinitis around the hip joint. Am J Sports Med. 2014;42(11):2659–65. doi: 10.1177/0363546514545857. [DOI] [PubMed] [Google Scholar]
- 4.Paik NC. Acute calcific tendinitis of the gluteus medius: An uncommon source for back, buttock, and thigh pain. Semin Arthritis Rheum. 2014;43(6):824–29. doi: 10.1016/j.semarthrit.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 5.Vereecke E, Mermuys K, Casselman J. A Case of bilateral acute calcific tendinitis of the gluteus medius, treated by ultrasound-guided needle lavage and corticosteroid injection. J Belg Soc Radiol. 2015;99(2):16–19. doi: 10.5334/jbr-btr.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sakai T, Shimaoka Y, Sugimoto M, Koizumi T. Acute calcific tendinitis of the gluteus medius: A case report with serial magnetic resonance imaging findings. J Orthop Sci. 2004;9(4):404–7. doi: 10.1007/s00776-004-0799-y. [DOI] [PubMed] [Google Scholar]
- 7.Almedghio S, Garneti N. The acute and chronic presentation of gluteus medius calcific tendinitis – a case report of two. J Orthop Case Rep. 2014;4(4):48–50. doi: 10.13107/jocr.2250-0685.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang I, Hayes CW, Biermann JS. Calcific tendinitis of the gluteus medius tendon with bone marrow edema mimicking metastatic disease. Skeletal Radiol. 2002;31(6):359–61. doi: 10.1007/s00256-002-0516-x. [DOI] [PubMed] [Google Scholar]
- 9.Koen SM, Pecha F, Nilsson K. Ultrasound-guided needle lavage for calcific tendonitis of the gluteus medius tendon. Athletic Training & Sports Health Care. 2017;9(5):238–40. [Google Scholar]
- 10.Jian C, Dan W, Gangliang W. Endoscopic treatment for calcific tendinitis of the gluteus medius: A case report and review. Front Surg. 2022;9:917027. doi: 10.3389/fsurg.2022.917027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yi SR, Lee MH, Yang BK, et al. Characterizing the progression of varying types of calcific tendinitis around hip. Hip Pelvis. 2015;27(4):265–72. doi: 10.5371/hp.2015.27.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hung CY, Chang KV. Ultrasound-guided percutaneous needle tenotomy with platelet-rich plasma injection for an uncommon case of proximal gluteus medius tendinopathy. J Med Ultrasound. 2019;27(2):111–12. doi: 10.4103/JMU.JMU_86_18. [DOI] [PMC free article] [PubMed] [Google Scholar]