Abstract
Background:
Heart failure (HF) has been associated with psychosocial distress, but other long-term mental health sequelae are unclear.
Objectives:
To determine risks of major depression and suicide, susceptible time periods, and sex-specific differences after HF diagnosis in a large population-based cohort.
Methods:
A national cohort study was conducted of all 154,572 persons diagnosed with HF at ages 18–75 years during 2002–2017 in Sweden, and 1,545,720 age- and sex-matched population-based controls, followed up for major depression and suicide ascertained from nationwide inpatient, outpatient, and death records through 2018. Poisson regression was used to compute incidence rate ratios (IRRs) while adjusting for sociodemographic factors and comorbidities.
Results:
HF was associated with increased risks of major depression and death by suicide in both men and women, with highest risks in the first 3 months, then declining to modest risks at ≥12 months after HF diagnosis. Within 3 months after HF diagnosis, adjusted IRRs for new-onset major depression were 3.34 (95% CI, 3.04–3.68) in men and 2.78 (2.51–3.09) in women, and for suicide death were 4.47 (2.62–7.62) in men and 2.82 (1.11–7.12) in women. These risks were elevated regardless of age at HF diagnosis. HF was associated with significantly more depression cases in women (P<0.001).
Conclusions:
In this large national cohort, HF was associated with substantially increased risks of depression and suicide in men and women, with highest risks occurring within 3 months after HF diagnosis. Men and women with HF need timely detection and treatment of depression and suicidality.
Keywords: cardiovascular diseases, depression, heart failure, suicide
Condensed abstract:
Heart failure (HF) has been associated with psychosocial distress that may adversely affect clinical outcomes, but risks of major depression and suicide, susceptible time periods, and sex-specific differences are unclear. In a national cohort of 154,572 adults newly diagnosed with HF and 1,545,720 age- and sex-matched controls, HF was associated with 2- to 4-fold risks of major depression and death by suicide in the subsequent 3 months among men and women. These risks were elevated regardless of age at HF diagnosis. Men and women newly diagnosed with HF need timely detection and treatment of depression and suicidality.
INTRODUCTION
Heart failure (HF) is a leading cause of hospitalization, health care expenditures, and premature mortality worldwide (1). Because of its high burden of disease, HF may cause severe psychosocial distress that adversely affects quality of life (2), self-care (3), and survival (4,5). Despite an overall decline in developed countries since 2000 (6,7), HF incidence has increased among younger adults (ages <45–55 years) (7,8), which may translate into larger psychosocial impacts on HF outcomes in the future. A better understanding of long-term psychosocial sequelae is needed to guide timely clinical interventions and improve outcomes in HF patients.
Clinically significant depression has a reported prevalence of 20% to 40% in HF patients (9,10). However, most prior studies have included small samples (<500) of predominantly older adults, lacked a comparison group without HF, and varied widely in depression ascertainment and findings (9,10). To our knowledge, no studies have examined risk of new-onset major depression associated with HF in a large population-based cohort. A few prior studies have reported 1.5- to 1.7-fold risks of suicide death among HF patients compared with healthy controls (11–13). However, sex- and age-specific differences have rarely been examined and may be important because of the known differences in HF (14), depression (15), and suicide (16) incidence between men and women across the life course. Large population-based cohorts are needed to enable well-powered assessments of mental health outcomes, susceptible time periods, and high-risk subgroups among HF patients.
We sought to address these knowledge gaps using nationwide data in Sweden. Our goals were to: (1) determine risks of new-onset major depression and suicide associated with newly diagnosed HF in a large population-based cohort; (2) identify periods of heightened risk after HF diagnosis; and (3) assess for sex- and age-specific differences. We hypothesized that HF is associated with higher risks of major depression and suicide among men and women of all ages, with highest risks occurring shortly after HF diagnosis.
METHODS
Study Population and HF Ascertainment
Using national registries, we identified all 154,572 persons who had a first diagnosis of HF at ages 18 to 75 years during 2002–2017 in Sweden. HF was identified using International Classification of Diseases, Version 10 (ICD-10) codes I50, I11.0, I13.0, and I13.2 assigned at any inpatient or outpatient health care encounter as recorded in the Swedish Hospital and Outpatient Registers or primary care records. Clinical data on HF subtypes were unavailable and could not be used to subclassify HF. The Swedish Hospital Register contains all primary and secondary hospital discharge diagnoses with nationwide coverage since 1987; these diagnoses are currently >99% complete and have been reported to have positive predictive values of 81–95% for HF (17,18). The Swedish Outpatient Register contains all diagnoses from specialty clinics nationwide starting in 2001. Primary care diagnoses previously collected by our group (19) initially covered 20% of the Swedish population starting in 1998, then were expanded to cover 45% starting in 2001 and 90% in 2008 and onward.
Each HF case was matched to 10 controls randomly sampled from the general population who had the same sex, birth year, and were still living in Sweden on the date of HF diagnosis for the respective case (i.e., index date). This study was approved by the Regional Ethical Review Board in Lund, Sweden (No. 2012/795 and later amendments). Participant consent was not required because this study used only pseudonymized registry-based secondary data.
Depression and Suicide Ascertainment
The primary outcomes were (1) first-ever diagnosis (i.e., new-onset) of major depression and (2) death by suicide, which were ascertained from the index date (respective case’s HF diagnosis date) through December 31, 2018. Major depression was identified using ICD-10 codes F32-F33 in the Swedish Hospital and Outpatient Registers and primary care records (as described above). Suicide death was identified using nationwide data from the Swedish Cause of Death Register, which includes deaths and ICD codes for cause of death among all persons registered in Sweden with compulsory reporting nationwide. All intentional deaths were identified using ICD-10 codes X60-X84, and deaths of undetermined intent were identified using ICD-10 codes Y10-Y34. Prior studies have indicated that many suicides are misclassified as deaths of undetermined intent (20). In the present study, intentional deaths and deaths of undetermined intent were analyzed together in the primary analysis and separately in a sensitivity analysis.
Covariates
Other characteristics that may be associated with HF and depression or suicide were identified using Swedish national census and health registry data, which were linked using a pseudonymous personal identification number. Covariates included birth year (continuous and categorical by decade), sex (male/female), birth country (Sweden/other), marital status (married/not married), education level (≤9, 10–12, >12 years), income (quartiles), myocardial infarction (yes/no), alcohol use disorder (yes/no), cancer (yes/no), chronic obstructive pulmonary disease (COPD; yes/no), diabetes (yes/no), and Charlson Comorbidity Index score (0–1, 2, ≥3) at the index date. All covariates were 100.0% complete. These comorbidities were included because they are potentially associated with higher risks of HF (21) and depression or suicide (16) independently of other known risk factors.
Statistical Analysis
Conditional Poisson regression was used to compute incidence rate ratios (IRRs) and 95% confidence intervals (CIs) for new-onset major depression or completed suicide associated with HF diagnosis while accounting for matched sets. To examine new-onset depression, all individuals with a depression diagnosis that preceded the index date (11,647 [7.5%] cases and 50,019 [3.8%] controls) were excluded to assess only first-ever diagnoses of depression. In secondary analyses, we also explored (1) associations between HF and any new or recurrent diagnosis of depression in the entire cohort (i.e., including individuals with a prior diagnosis of depression), (2) associations between HF and non-fatal suicidal behavior (defined by diagnoses for intentional injury or injury of undetermined intent), and (3) risks of new-onset major depression or completed suicide after a first hospitalization for HF, as a proxy for higher severity. All analyses were conducted both unadjusted and adjusted for covariates (as defined above). Poisson model goodness-of-fit was assessed using Pearson and deviance tests and was met in each model.
Sex-specific differences were assessed by performing stratified analyses and formally testing for interactions between HF and sex on the additive and multiplicative scale. To assess periods of susceptibility, the outcomes were assessed in specific time intervals after HF diagnosis (<3, 3 to <12, and ≥12 months), which were selected to have sufficient numbers of outcomes in each interval for sex-stratified analyses. Age-specific differences were assessed by stratifying by age at the index date (18–44, 45–54, 55–64, 65–74 years) while adjusting for age as a continuous variable within each stratum, and also testing for additive or multiplicative interaction between HF and age (<55 vs. ≥55 years).
In exploratory analyses, we also assessed interactions between HF and other covariates in relation to major depression or death by suicide, which potentially could reveal other subgroups of HF patients who are more susceptible to these outcomes. All statistical tests were 2-sided and used an α-level of 0.05. All analyses were conducted using Stata version 15.1.
RESULTS
The mean age at HF diagnosis was 64.9 ± 8.7 (range, 18.5 to 75.0) years, and the mean follow-up time was 13.8 ± 4.5 years. A total of 138,002 first diagnoses of major depression and 3,497 deaths by suicide were identified. Across the entire follow-up period, 13.2% of HF cases and 9.7% of controls without prior depression were diagnosed with new-onset major depression, and 0.3% of HF cases and 0.2% of controls died by suicide. The mean age at diagnosis of major depression was 65.1 ± 8.9 years and at suicide death was 68.3 ± 9.4 years.
Table 1 shows characteristics of HF cases, controls, and all persons diagnosed with new-onset major depression or who died by suicide. Nearly 65% of HF cases were male, and nearly 60% were aged 65–74 years. Rates of depression were disproportionately higher in women, whereas suicide death rates were higher in men. Compared with controls, HF cases and individuals diagnosed with major depression or who died by suicide were more likely to be foreign-born, unmarried, and/or to have comorbidities. HF cases and individuals who died by suicide (but not those with depression) were also more likely to have low education level and/or low income.
Table 1.
Characteristics of study participants.
| HF cases N=154,572 (100.0%) | Controls N=1,545,720 (100.0%) | New-onset major depression N=138,002 (8.1%) | Died by suicide N=3,497 (0.2%) | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| Age at index date (years) | ||||
| 18–44 | 5,496 (3.6) | 54,960 (3.6) | 6,858 (5.0) | 140 (4.0) |
| 45–54 | 14,578 (9.4) | 145,780 (9.4) | 14,693 (10.6) | 423 (12.1) |
| 55–64 | 42,405 (27.4) | 424,050 (27.4) | 34,150 (24.8) | 1,079 (30.9) |
| 65–74 | 92,093 (59.6) | 920,930 (59.6) | 82,301 (59.6) | 1,855 (53.0) |
| Sex | ||||
| Male | 99,977 (64.6) | 999,770 (64.6) | 70,577 (51.1) | 2,798 (80.0) |
| Female | 54,595 (35.3) | 545,950 (35.3) | 67,425 (48.9) | 699 (20.0) |
| Birth country | ||||
| Sweden | 131,268 (84.9) | 1,365,031 (88.3) | 119,838 (86.8) | 3,045 (87.1) |
| Other | 23,304 (15.1) | 180,689 (11.7) | 18,164 (13.2) | 452 (12.9) |
| Marital status | ||||
| Married | 84,296 (54.5) | 979,598 (63.4) | 84,139 (61.0) | 1,581 (45.2) |
| Not married | 70,276 (45.5) | 566,122 (36.6) | 53,863 (39.0) | 1,916 (54.8) |
| Education (years) | ||||
| ≤9 | 61,803 (40.0) | 496,638 (32.1) | 46,371 (33.6) | 1,406 (40.2) |
| 10–12 | 65,924 (42.6) | 647,791 (41.9) | 58,162 (42.1) | 1,448 (41.4) |
| >12 | 26,845 (17.4) | 401,291 (26.0) | 33,469 (24.3) | 643 (18.4) |
| Income (quartile) | ||||
| 1st (highest) | 28,176 (18.2) | 387,063 (25.0) | 41,703 (30.2) | 601 (17.2) |
| 2nd | 34,487 (22.3) | 385,834 (25.0) | 40,443 (29.3) | 748 (21.4) |
| 3rd | 43,283 (28.0) | 387,664 (25.1) | 32,533 (23.6) | 1,050 (30.0) |
| 4th (lowest) | 48,626 (31.5) | 385,159 (24.9) | 23,323 (16.9) | 1,098 (31.4) |
| Myocardial infarction | 44,371 (28.1) | 65,715 (4.3) | 8,968 (6.5) | 211 (6.0) |
| Alcohol use disorder | 3,239 (2.1) | 10,906 (0.7) | 1,539 (1.1) | 209 (6.0) |
| Cancer | 27,830 (18.0) | 230,023 (14.9) | 20,545 (14.9) | 377 (10.8) |
| Chronic obstructive pulmonary disease | 25,591 (16.6) | 65,940 (4.3) | 9,565 (6.9) | 224 (6.4) |
| Diabetes | 41,853 (27.1) | 159,579 (10.3) | 17,245 (12.5) | 405 (11.6) |
| Charlson Comorbidity Index | ||||
| 0–1 | 142,447 (92.2) | 1,531,171 (99.1) | 135,185 (98.0) | 3,424 (97.9) |
| 2 | 8,631 (5.6) | 12,899 (0.8) | 2,262 (1.6) | 52 (1.5) |
| ≥3 | 3,494 (2.3) | 1,650 (0.1) | 555 (0.4) | 21 (0.6) |
HF and New-Onset Depression
HF was associated with substantially increased risks of new-onset major depression in both men and women (Table 2). These risks were highest in the first 3 months after HF diagnosis, then declined to only modestly or no increased risks at ≥12 months after HF diagnosis. Adjusted IRRs for new-onset major depression within 3 months after HF diagnosis were 3.34 (95% CI, 3.04–3.68) in men and 2.78 (2.51–3.09) in women. Among HF cases and controls, respectively, the cumulative incidences of new-onset major depression were 11.7% and 8.7% in men and 18.5% and 15.8% in women.
Table 2.
Sex-stratified associations between HF diagnosis (2002–2017) and risk of new-onset major depression through 2018, Sweden.
| Time after HF diagnosis | HF cases | Controls | Unadjusted | Adjusteda | |
|---|---|---|---|---|---|
| Major depression, n (% of HF cases) | Major depression, n (% of controls) | IRR (95% CI) | IRR (95% CI) | P | |
| Men | |||||
| <3 months | 746 (0.8) | 1,922 (0.2) | 4.01 (3.69, 4.36) | 3.34 (3.04, 3.68) | <0.001 |
| 3 to <12 months | 1,056 (1.1) | 4,399 (0.5) | 2.48 (2.32, 2.65) | 2.06 (1.91, 2.22) | <0.001 |
| ≥12 months | 5,257 (5.6) | 43,154 (4.5) | 1.25 (1.22, 1.29) | 1.18 (1.15, 1.22) | <0.001 |
| Women | |||||
| <3 months | 644 (1.3) | 2,051 (0.4) | 3.34 (3.06, 3.65) | 2.78 (2.51, 3.09) | <0.001 |
| 3 to <12 months | 830 (1.7) | 4,593 (0.9) | 1.92 (1.79, 2.07) | 1.53 (1.41, 1.67) | <0.001 |
| ≥12 months | 4,097 (8.3) | 42,686 (8.2) | 1.01 (0.98, 1.04) | 0.97 (0.94, 1.01) | 0.06 |
Adjusted for age, birth country, marital status, education, income, myocardial infarction, alcohol use disorder, cancer, chronic obstructive pulmonary disease, diabetes, and Charlson Comorbidity Index.
CI = confidence interval, IRR = incidence rate ratio
Among HF cases, the risk of new-onset major depression within 3 months of the index date was nearly 1.7-fold higher in women than men (Online Table 1). HF and female sex had a positive additive but negative multiplicative interaction (i.e., the combined effects of HF and female sex on risk of depression within 3 months after HF diagnosis exceeded the sum but was less than the product of their separate effects) (P<0.001 for each; Online Table 1). The positive additive interaction indicates that HF accounted for significantly more depression cases within 3 months after HF diagnosis in women than men.
In both men and women, HF diagnosis was associated with elevated risks of new-onset major depression regardless of age (Central Illustration; Online Table 2). HF and older age at diagnosis (≥55 years) had a positive interaction on the additive and multiplicative scale (P<0.001 for each; Online Table 3). The positive additive interaction suggests that HF accounted for significantly more depression cases within 3 months after HF diagnosis in older compared with younger adults.
Central Illustration.
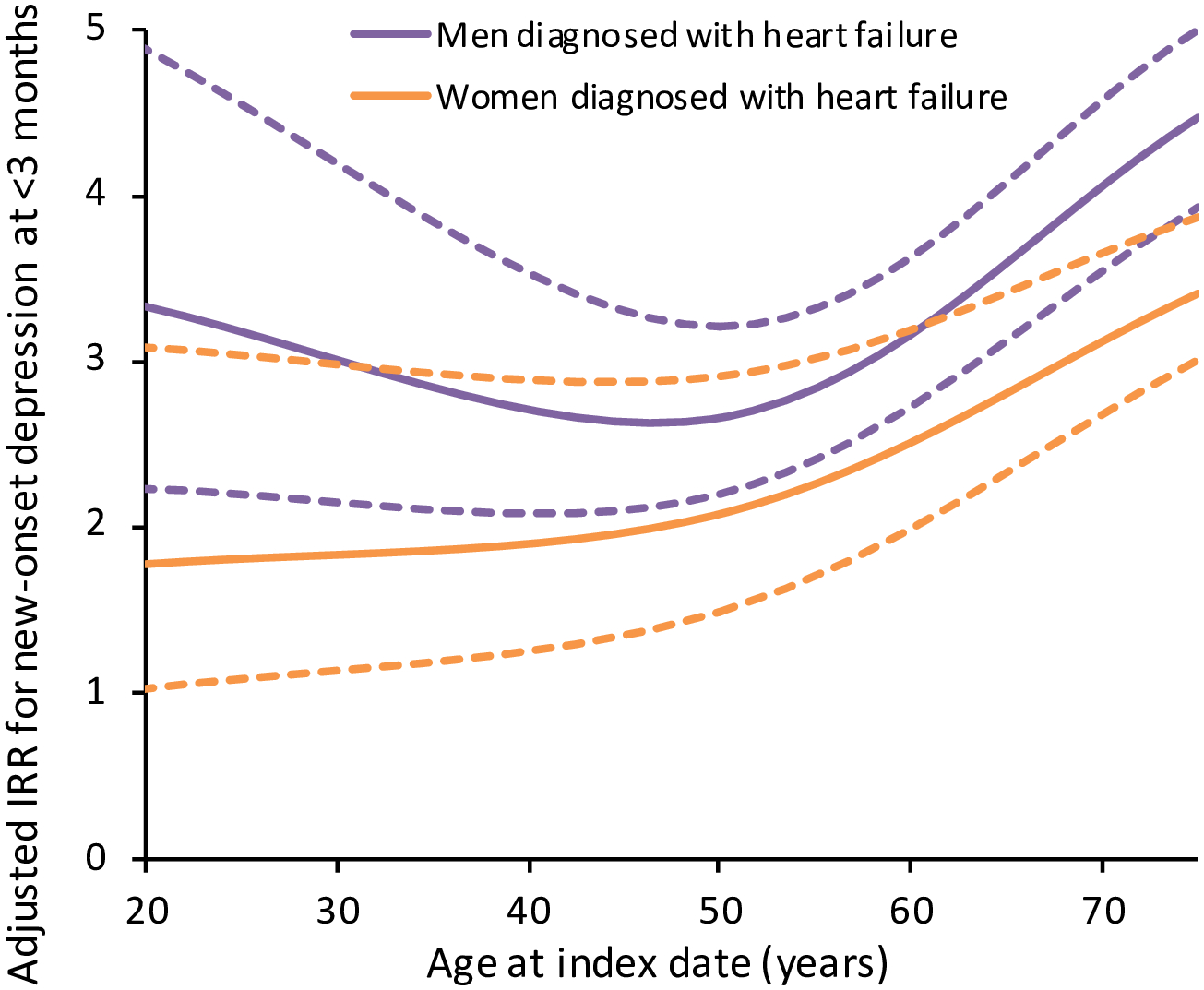
Sex-stratified associations between heart failure diagnosis and risk of new-onset major depression within 3 months after index date. The incidence rate ratios (IRRs) were adjusted for age, birth country, marital status, education, income, myocardial infarction, alcohol use disorder, cancer, chronic obstructive pulmonary disease, diabetes, and Charlson Comorbidity Index (dashed lines indicate 95% CIs).
Adjusted IRRs are shown for risk of new-onset major depression within 3 months after HF diagnosis compared with age- and sex-matched controls from the general population. In men and women of all ages, diagnosis with HF was associated with substantially elevated risks of new-onset major depression in the subsequent 3 months. CI = confidence interval, IRR = incidence rate ratio, HF = heart failure.
In a secondary analysis, we examined associations between HF and any new or recurrent diagnosis of major depression in the entire cohort (i.e., including individuals with a depression diagnosis before the index date), rather than only first-ever diagnoses. All risk estimates were attenuated compared with the main analyses but remained significantly elevated within 3 months after HF diagnosis (adjusted IRR, men: 1.52; 95% CI, 1.43–1.60; women: 1.76; 1.66–1.87).
HF and Suicide Death
HF was associated with >4- and 2.8-fold risks of suicide death among men and women, respectively, in the first 3 months after HF diagnosis (adjusted IRR, men: 4.47; 95% CI, 2.62–7.62; women: 2.82; 1.11–7.12) (Table 3). These risks declined but remained significantly elevated in women (but not men) at ≥1 year after HF diagnosis (adjusted IRR, 1.63; 95% CI, 1.21–2.18) (Table 3). Among HF cases and controls, respectively, the cumulative incidences of suicide death were 0.3% and 0.2% in men and 0.2% and 0.1% in women.
Table 3.
Sex-stratified associations between HF diagnosis (2002–2017) and risk of suicide death through 2018, Sweden.
| Time after HF diagnosis | HF cases | Controls | Unadjusted | Adjusteda | |
|---|---|---|---|---|---|
| Suicide deaths, n (% of HF cases) | Suicide deaths, n (% of controls) | IRR (95% CI) | IRR (95% CI) | P | |
| Men | |||||
| <3 months | 31 (<0.1) | 63 (<0.1) | 5.17 (3.33, 8.04) | 4.47 (2.62, 7.62) | <0.001 |
| 3 to <12 months | 33 (<0.1) | 169 (<0.1) | 2.00 (1.37, 2.92) | 1.88 (1.25, 2.84) | 0.003 |
| ≥1 year | 230 (0.2) | 2,278 (0.2) | 1.19 (1.02, 1.40) | 1.12 (0.95, 1.32) | 0.19 |
| Women | |||||
| <3 months | 7 (<0.1) | 20 (<0.1) | 3.33 (1.32, 8.40) | 2.82 (1.11, 7.12) | 0.03 |
| 3 to <12 months | 15 (<0.1) | 51 (<0.1) | 3.06 (1.72, 5.46) | 2.07 (1.12, 3.80) | 0.02 |
| ≥1 year | 79 (0.1) | 527 (0.1) | 1.78 (1.37, 2.32) | 1.63 (1.21, 2.18) | 0.001 |
Adjusted for age, birth country, marital status, education, income, myocardial infarction, alcohol use disorder, cancer, chronic obstructive pulmonary disease, diabetes, and Charlson Comorbidity Index.
CI = confidence interval, IRR = incidence rate ratio
In the entire cohort, 42.8% (1,496/3,497) of suicide decedents had a prior diagnosis of major depression, and 31.5% (471/1,496) of such persons were first diagnosed within 1 year before the suicide. Among HF cases, 51.9% (205/395) of suicide decedents had a prior diagnosis of major depression, and 26.8% (55/205) of such persons were first diagnosed within 1 year before the suicide.
Figure 1 shows the risks of suicide death within 1 year after HF diagnosis by age at the index date. HF was associated with elevated risks of suicide death across all ages in both men and women, although risks declined with increasing age among women (Figure 1; Online Table 4). There were no significant interactions between HF and sex or age in relation to suicide death (Online Tables 5 and 6).
Figure 1.
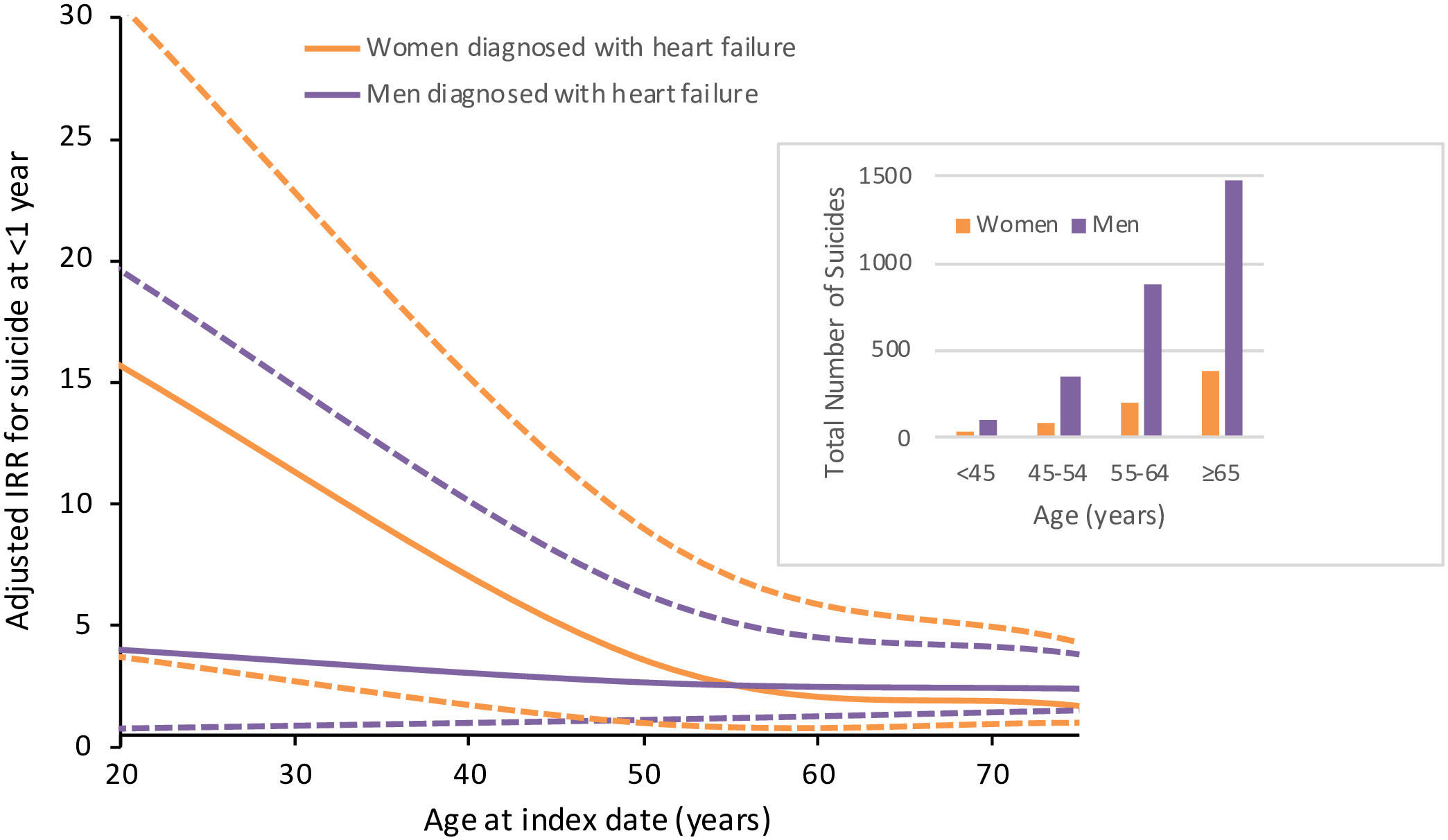
Sex-stratified associations between heart failure diagnosis and risk of suicide death within 1 year after index date. The incidence rate ratios (IRRs) were adjusted for age, birth country, marital status, education, income, myocardial infarction, alcohol use disorder, cancer, chronic obstructive pulmonary disease, diabetes, and Charlson Comorbidity Index (dashed lines indicate 95% CIs).
Other Secondary Analyses
HF also was associated with increased risks of non-fatal suicidal behavior (defined as intentional injury or injury of undetermined intent). For example, adjusted IRRs within 3 months after HF diagnosis were 3.42 (95% CI, 2.14–5.48) in men and 2.40 (1.27–4.53) in women (Online Table 7). When restricting the outcome to confirmed intentional injury, most risk estimates were moderately higher but had wider confidence intervals due to fewer events (Online Table 8).
Risks of major depression and completed suicide also were examined after a first hospitalization for HF, as a proxy for higher severity. Most risk estimates were only slightly higher than those in the main analyses (Online Tables 9–10), related in part to the high proportion (77.6%) of first HF diagnoses that occurred during a hospitalization.
Exploratory analyses to assess interactions between HF and other covariates revealed only negative multiplicative (and no additive) interactions between HF and being foreign-born, unmarried, or having alcohol use disorder in relation to major depression (i.e., the combined effects of HF and each of these factors on risk of major depression within 3 months after HF diagnosis was less than the product of their separate effects; P<0.001 for each).
In a sensitivity analysis that assessed confirmed suicides (n=2,770) and deaths of undetermined intent (n=727) separately, HF was significantly associated with both outcomes with similar risk magnitudes. For example, within 3 months after HF diagnosis, the IRR was 3.51 (95% CI, 2.09–5.91; P<0.001) for confirmed suicide and 3.80 (1.69–8.56; P=0.001) for death of undetermined intent, adjusting for sex and other covariates.
DISCUSSION
In this large national cohort, men and women newly diagnosed with HF had substantially increased risks of new-onset major depression and death by suicide. Risks were highest in the first 3 months after HF diagnosis, when men and women respectively had more than 3.3- and 2.7-fold risks of major depression and 4.4- and 2.8-fold risks of suicide death, adjusting for sociodemographic differences and comorbidities. These risks were elevated regardless of age at HF diagnosis. All risks declined to only modestly or no increased risks at ≥1 year after HF diagnosis.
To our knowledge, this is the first study to examine risks of major depression after HF diagnosis in a large population-based cohort, and one of the first to examine suicide risks, periods of susceptibility, and sex-specific differences. Previous smaller studies have assessed depression prevalence in selected clinical samples of HF patients. A meta-analysis of 27 such studies with a total of 6,202 HF patients (average sample size 230) reported an overall 21.5% prevalence of clinically significant depression, with a higher prevalence in women (32.7% in 16 studies that reported sex-specific results) (9). A more recent meta-analysis of 149 studies with 305,407 HF patients (average sample size 2,050) reported that the prevalence of any severity or moderate to severe depression (variably defined) was 41.9% and 28.1%, respectively, with a higher prevalence in women (45.5% for depression of any severity) (10). However, these studies had high heterogeneity of findings because of different ascertainment methods and populations, and did not include a comparison group without HF.
A few prior studies also have assessed suicide risks in HF patients. A case-control study of 52,749 adult patients who died by suicide in Taiwan (including 1,624 with HF) and 210,996 matched controls (4,053 with HF) reported an adjusted odds ratio (OR) of 1.68 (95% CI, 1.59–1.79) for suicide death associated with HF, with highest risk in the first 6 months after HF diagnosis (7.04; 5.37–9.22) (11). A case-control study of 1,354 Canadian adults aged ≥66 years who died by suicide and 4:1 matched healthy controls reported an unadjusted OR of 1.73 (95% CI, 1.33–2.24) for suicide death associated with HF, and OR of 1.36 (1.00–1.85) after adjusting for comorbidities (12). A Danish cohort study of >7 million persons reported a nearly 1.5-fold risk of suicide death associated with HF diagnosis (adjusted IRR, 1.48; 95% CI, 1.38–1.58), with highest risk in the first 6 months (2.38; 2.04–2.79) (13).
The present study extends prior evidence by examining risks of both major depression and suicide, periods of heightened risk, and sex-specific differences associated with HF in a large population-based cohort. Our findings showed substantially increased risks of major depression in both men and women newly diagnosed with HF. Although HF was more common in men, it was associated with more depression diagnoses in women. This finding could partly be explained by underdiagnosis of depression in men, which has previously been reported (22). Our suicide risk estimates were higher than those in some (12,13) but not all (11) prior studies, possibly because the time window shortly after HF diagnosis has the highest risks but has seldom been examined. Nearly half of HF patients who died by suicide had no prior diagnosis of depression, further suggesting underdiagnosis and the importance of clinical assessment for depression and suicidality in these patients. Importantly, we found significantly elevated risks of both major depression and suicide among young adults with HF (ages <45; Central Illustration and Figure 1). Given the rising incidence of HF in this age group (7,8), these findings may translate into larger public health impacts in the future. Adults of all ages with HF may need assessment for depression and among those at high risk, assessment for suicidality, beginning at the time of HF diagnosis.
The large burden of disease associated with HF may potentially cause psychosocial distress that worsens suffering, quality of life, and long-term health outcomes (1). Prior evidence has shown that HF patients with psychosocial distress are more likely to struggle with HF self-care, resulting in higher hospitalization rates (3). Depression in HF patients has been associated with worse clinical outcomes, including 1.4- to 1.7-fold risks of all-cause hospitalization, cardiovascular mortality, and all-cause mortality compared to HF patients without depression (4). Moreover, severity of depression in HF patients has been identified as a stronger predictor of health-related quality of life than HF severity (23). The American Heart Association previously recommended routine screening for depression in all patients with coronary heart disease, but did not specifically address HF (24). More recently, the U.S. Preventive Services Task Force recommended routine screening for depression in the general adult population, while emphasizing that patients with cardiovascular disease are at higher risk (25). Unfortunately, such screening is not consistently implemented and remains underutilized (26). Our findings underscore the importance of screening for depression and suicidality in patients with HF. Patients with positive screens need prompt psychiatric treatment, followed by close monitoring for adherence with treatment for both their mental and cardiovascular health (3,24).
Strengths and Limitations
A key strength of the present study was its large national cohort design, which provided high statistical power needed to examine narrowly defined periods of susceptibility and sex-specific differences. Clinical diagnoses from inpatient, specialty outpatient, and primary care settings allowed more complete ascertainment of both HF and major depression, thus enabling more valid risk estimates for a national population. We were able to assess risks of both major depression and suicide while controlling for multiple potential confounders. Previously reported incidences of depression and suicide are comparable between Sweden and the US (19,27,28).
This study also had several limitations. Clinical data on HF subtypes or severity were unavailable and could not be used to subclassify HF. Future studies with access to this information will be needed to further improve risk stratification and target clinical interventions in these patients. Major depression was identified using nationwide ICD codes, and more detailed clinical data were unavailable to validate these diagnoses. However, their validity has previously been supported by their prevalence, sex ratio, sibling and twin correlations, and associations with well-documented psychosocial risk factors (19,29). Depression is often undiagnosed, and such cases could not be identified in this study. However, the inclusion of diagnoses from primary care settings where most depression is diagnosed and treated (19) enabled more complete capture than in prior studies. As in other large population-based studies, the reporting of suicides also involves some misclassification. However, available data on intentional deaths and deaths of undetermined intent enabled separate analyses of these outcomes in a sensitivity analysis, which showed little difference in risk estimates. Fortunately, despite higher risks of depression and suicide, a large majority of HF patients did not experience these outcomes. Additional research will be needed to identify modifiable protective factors that can be targeted in interventions to promote mental health in HF patients.
CONCLUSIONS
In this large national cohort, newly diagnosed HF was associated with increased relative risks of new-onset major depression and suicide in men and women of all ages, with highest risks occurring in the first 3 months after HF diagnosis. HF was associated with more depression cases among women than men. Men and women with HF need timely detection and treatment of depression and suicidality.
Supplementary Material
Tweet:
In a large national cohort, newly diagnosed heart failure was associated with 2- to 4-fold risks of major depression and suicide within the first 3 months. Men and women with heart failure need timely detection and treatment of depression and suicidality.
PERSPECTIVES.
Competency in Medical Knowledge:
Heart failure (HF) was associated with substantially increased risks of major depression and death by suicide in men and women, with highest risks occurring in the first 3 months after HF diagnosis.
Competency in Patient Care:
Men and women newly diagnosed with HF need timely detection and treatment of depression and suicidality.
Competency in Interpersonal & Communication Skills:
These findings underscore the importance of screening for depression and suicidality in all patients with HF.
Translational Outlook:
Additional investigations will be needed to elucidate risks for mental health sequelae associated with different HF subtypes and severity.
Funding:
This work was supported by the National Institute on Alcohol Abuse and Alcoholism [R01 AA027522 to A.E. and K.S.] at the National Institutes of Health; the Swedish Research Council; the Swedish Heart-Lung foundation; and ALF project grant, Region Skåne/Lund University, Sweden. The funding agencies had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Abbreviations:
- CI
confidence interval
- HF
heart failure
- ICD
International Classification of Diseases
- IRR
incidence rate ratio
- OR
odds ratio
Footnotes
Disclosures: There are no conflicts of interest.
REFERENCES
- 1.Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail 2020;22:1342–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Faller H, Stork S, Schuler M et al. Depression and disease severity as predictors of health-related quality of life in patients with chronic heart failure--a structural equation modeling approach. J Card Fail 2009;15:286–292 e2. [DOI] [PubMed] [Google Scholar]
- 3.Freedland KE, Skala JA, Steinmeyer BC, Carney RM, Rich MW. Effects of Depression on Heart Failure Self-Care. J Card Fail 2021;27:522–532. [DOI] [PubMed] [Google Scholar]
- 4.Chouairi F, Fuery MA, Mullan CW et al. The Impact of Depression on Outcomes in Patients With Heart Failure and Reduced Ejection Fraction Treated in the GUIDE-IT Trial. J Card Fail 2021;27:1359–1366. [DOI] [PubMed] [Google Scholar]
- 5.Sokoreli I, de Vries JJG, Pauws SC, Steyerberg EW. Depression and anxiety as predictors of mortality among heart failure patients: systematic review and meta-analysis. Heart Fail Rev 2016;21:49–63. [DOI] [PubMed] [Google Scholar]
- 6.Zarrinkoub R, Wettermark B, Wandell P et al. The epidemiology of heart failure, based on data for 2.1 million inhabitants in Sweden. Eur J Heart Fail 2013;15:995–1002. [DOI] [PubMed] [Google Scholar]
- 7.Conrad N, Judge A, Tran J et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet 2018;391:572–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barasa A, Schaufelberger M, Lappas G, Swedberg K, Dellborg M, Rosengren A. Heart failure in young adults: 20-year trends in hospitalization, aetiology, and case fatality in Sweden. Eur Heart J 2014;35:25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol 2006;48:1527–37. [DOI] [PubMed] [Google Scholar]
- 10.Moradi M, Doostkami M, Behnamfar N, Rafiemanesh H, Behzadmehr R. Global Prevalence of Depression among Heart Failure Patients: A Systematic Review and Meta-Analysis. Curr Probl Cardiol 2021:100848. [DOI] [PubMed] [Google Scholar]
- 11.Liu CH, Wang JH, Weng SC et al. Is Heart Failure Associated With Risk of Suicide? J Card Fail 2018;24:795–800. [DOI] [PubMed] [Google Scholar]
- 12.Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA. Medical illness and the risk of suicide in the elderly. Arch Intern Med 2004;164:1179–84. [DOI] [PubMed] [Google Scholar]
- 13.Petersen BD, Stenager E, Mogensen CB, Erlangsen A. The association between heart diseases and suicide: a nationwide cohort study. J Intern Med 2020;287:558–568. [DOI] [PubMed] [Google Scholar]
- 14.Virani SS, Alonso A, Benjamin EJ et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation 2020;141:e139–e596. [DOI] [PubMed] [Google Scholar]
- 15.Van de Velde S, Bracke P, Levecque K. Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Soc Sci Med 2010;71:305–313. [DOI] [PubMed] [Google Scholar]
- 16.Crump C, Sundquist K, Sundquist J, Winkleby MA. Sociodemographic, psychiatric and somatic risk factors for suicide: a Swedish national cohort study. Psychological medicine 2014;44:279–89. [DOI] [PubMed] [Google Scholar]
- 17.Nilsson AC, Spetz CL, Carsjo K, Nightingale R, Smedby B. [Reliability of the hospital registry. The diagnostic data are better than their reputation]. Lakartidningen 1994;91:598, 603–5. [PubMed] [Google Scholar]
- 18.Ingelsson E, Arnlov J, Sundstrom J, Lind L. The validity of a diagnosis of heart failure in a hospital discharge register. Eur J Heart Fail 2005;7:787–91. [DOI] [PubMed] [Google Scholar]
- 19.Sundquist J, Ohlsson H, Sundquist K, Kendler KS. Common adult psychiatric disorders in Swedish primary care where most mental health patients are treated. BMC Psychiatry 2017;17:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bjorkenstam C, Johansson LA, Nordstrom P et al. Suicide or undetermined intent? A register-based study of signs of misclassification. Popul Health Metr 2014;12:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khatibzadeh S, Farzadfar F, Oliver J, Ezzati M, Moran A. Worldwide risk factors for heart failure: a systematic review and pooled analysis. Int J Cardiol 2013;168:1186–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krumm S, Checchia C, Koesters M, Kilian R, Becker T. Men’s Views on Depression: A Systematic Review and Metasynthesis of Qualitative Research. Psychopathology 2017;50:107–124. [DOI] [PubMed] [Google Scholar]
- 23.Muller-Tasch T, Peters-Klimm F, Schellberg D et al. Depression is a major determinant of quality of life in patients with chronic systolic heart failure in general practice. J Card Fail 2007;13:818–24. [DOI] [PubMed] [Google Scholar]
- 24.Lichtman JH, Bigger JT Jr., Blumenthal JA et al. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation 2008;118:1768–75. [DOI] [PubMed] [Google Scholar]
- 25.Siu AL, Force USPST, Bibbins-Domingo K et al. Screening for Depression in Adults: US Preventive Services Task Force Recommendation Statement. JAMA 2016;315:380–7. [DOI] [PubMed] [Google Scholar]
- 26.Jha MK, Qamar A, Vaduganathan M, Charney DS, Murrough JW. Screening and Management of Depression in Patients With Cardiovascular Disease: JACC State-of-the-Art Review. J Am Coll Cardiol 2019;73:1827–1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annu Rev Public Health 2008;29:115–29. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. Global Health Observatory data repository: Suicide rate estimates, age-standardized. 2021.
- 29.Kendler KS, Ohlsson H, Lichtenstein P, Sundquist J, Sundquist K. The Genetic Epidemiology of Treated Major Depression in Sweden. Am J Psychiatry 2018;175:1137–1144. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


