Abstract
As the number of coronavirus disease 2019 (COVID-19) patients increased rapidly, the Korean government decided to pay most of the related medical expenses with finances from the National Health Insurance (NHI). We aimed to document changes in NHI medical expenses during the COVID-19 pandemic period. We also sought to compare how Japan and Taiwan, neighboring countries with NHI systems, responded to COVID-19 and to discuss policy implications.
Keywords: COVID-19, health expenditure, financial implications
The coronavirus disease 2019 (COVID-19) pandemic spurred a global crisis, with many countries adopting restrictive measures to curb its spread.1 Following the first confirmed COVID-19 case in Korea on January 20, 2020, the government implemented policies of social distancing, the wearing of face masks, and a testing–tracing–treatment strategy.2,3 Facing an unprecedented outbreak, the Ministry of Health and Welfare (MOHW) decided to use National Health Insurance (NHI) funding to finance approximately 36 service items,4 including medical treatments, medicines, vaccines, testing costs, and hospital room fees, that would be ordinarily not covered by the public health insurance scheme. These services were delivered nearly free-of-charge in that the NHI covered co-payments and the government covered the remaining out-of-pocket payments.5
Recently, however, with the spread of the Omicron variant, public spending on COVID-19 has risen substantially in Korea. We aimed to look at how Korea, as well as neighboring countries, such as Japan and Taiwan, have responded to COVID-19 in terms of covering health services and costs and to discuss the implications of such decisions.
The total expenditure of the NHI in Korea in 2020, when COVID-19 emerged, was KRW 86.6 trillion: an increase of 0.7% from 2019, which was significantly lower than the 9%–11% annual increase during 2017–2019. This may be attributable to a decline in health service utilization since January 2020. However, the same expenditure rose to KRW 95.5 trillion in 2021, an increase of approximately 10% from 2020, similar to previous growth rates.6
An analysis of the internal database of the Health Insurance Review and Assessment Service revealed that the number of COVID-19 patients increased by 832.1% from 52877 in 2020 to 492848 in 2021. The total medical cost of those patients was KRW 0.22 trillion in 2020, corresponding to 0.3% of the NHI’s total expenditure (KRW 86.6 trillion). In 2021, however, the cost rose to KRW 1.3 trillion, which is approximately 1.1% of the NHI’ total expenditure (KRW 95.5 trillion), an increase of 355.4% over the previous year. In terms of utilization, the number of inpatient days per patient was 16 days in 2020 and 10 days in 2021 (a decrease of 37.5%), and the cost of care per patient decreased by 51.1% from KRW 4.17 million in 2020 to KRW 2.04 million in 2021.7
In 2022, the number of cases surged with the appearance of the Omicron variant. The Korea Disease Control and Prevention Agency (KDCA) announced that, as of November 22, 2022, there were 26654729 cumulative COVID-19 cases and 30111 deaths (crude fatality rate of 0.11%). From 2021 to 2022, the percentage of cumulative COVID-19 cases was 0.2% in 2020, 2.1% in 2021, and 97.6% in 2022. This explosive outbreak of corona patients was reflected in increases in health insurance finances.8
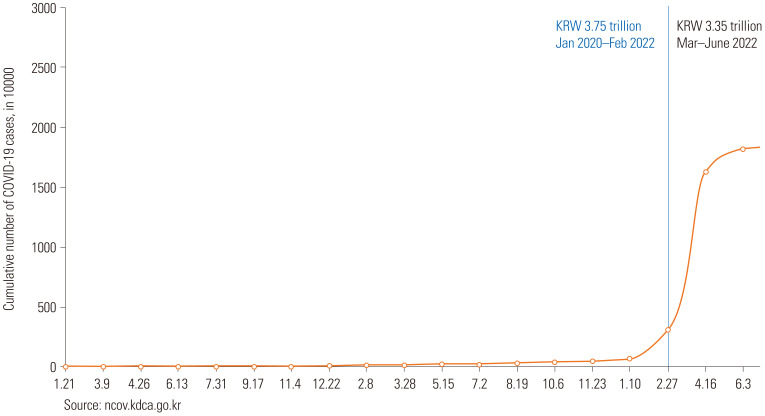
The total expenditure for the newly introduced fees for COVID-19-related services from January 2020 to June 2022 was KRW 7.10 trillion. The total expenditures by year were KRW 3.75 trillion from January 2020 to February 2022 and KRW 3.35 trillion in the 4 months from March to June 2022, which is almost 47% of the total costs over 2.5 years (Fig. 1).9,10
Fig. 1. Cumulative COVID-19 cases and total expenditure of COVID-19 items in Korea.
The total costs from January 2020 to June 2022 can be divided into the following five major service areas (Table 1): 1) KRW 2.97 trillion (41.8%) for treatment, 2) KRW 2.34 trillion (33.0%) for diagnostic tests, 3) KRW 1.10 trillion for vaccines and other expenses (15.5%), 4) KRW 0.42 trillion for non-COVID-19 care (5.9%), and 5) KRW 0.26 trillion for prevention (3.7%).
Table 1. Expenditures for COVID-19 Coverage Areas and Items by the National Health Insurance of Korea10,12.
| Support area | Support item | Health cost (%) | |||
|---|---|---|---|---|---|
| 1) 2020.1–2022.2 (37473 100 Million KRW) | 2) 2022.3–2022.6 (33555 100 Million KRW) | 1)+2) 2020.1–2022.6 (71028 100 Million KRW) | |||
| 1. Prevention | 2036 (5.4) | 599 (1.8) | 2635 (3.7) | ||
| 1) Infection prevention management related to COVID-19 | 59 (0.2) | 29 (0.1) | 88 (0.1) | ||
| 2) Infection prevention management at nursing facilities | 1651 (4.4) | 494 (1.5) | 2145 (3.0) | ||
| 3) Infection prevention management at psychiatric hospitals | 326 (0.9) | 76 (0.2) | 402 (0.6) | ||
| 2. Diagnostic testing | 11119 (29.7) | 12307 (36.7) | 23426 (33.0) | ||
| 1) COVID-19 PCR test–Single sample test | 9340 (24.9) | 4341 (12.9) | 13681 (19.3) | ||
| 2) COVID-19 PCR test–Pooled sample test | 709 (1.9) | 443 (1.3) | 1152 (1.6) | ||
| 3) Rapid PCR COVID-19 screening for emergency patients | 344 (0.9) | 135 (0.4) | 479 (0.7) | ||
| 4) Integrated diagnostic PCR test for COVID-19 and influenza | 35 (0.10) | 6 (0.0) | 41 (0.1) | ||
| 5) COVID-19 rapid antigen test | 691 (1.80) | 7382 (22.0) | 8073 (11.4) | ||
| 3. Treatment | 10428 (27.80) | 19292 (57.5) | 29720 (41.8) | ||
| 1) Treatment of severe COVID-19 patients | |||||
| (1) Isolation room admission | 5411 (14.40) | 2926 (8.7) | 8337 (11.7) | ||
| (2) Admission to intensive care units and management of negative pressure rooms in wards dedicated to treating severe patients | 1650 (4.40) | 1190 (3.5) | 2840 (4.0) | ||
| (3) Isolation room management or admission for new/transfer inpatients at nursing facilities/psychiatric hospitals | 153 (0.4) | 94 (0.3) | 247 (0.3) | ||
| (4) Integrated Isolation/shared room management | - | 1424 (4.2) | 1424 (2.0) | ||
| 2) Treatment of mild COVID-19 patients | |||||
| (1) Patient management at community treatment centers | 1255 (3.3) | 243 (0.7) | 1498 (2.1) | ||
| (2) Reimbursement for treatment/management at home (community treatment center) | 1325 (3.5) | 12307 (36.7) | 13632 (19.2) | ||
| (3) Reimbursement for outpatient (outpatient, nursing, facilities, pharmacy | 2 (0.0) | 816 (2.4) | 818 (1.2) | ||
| 3) Treatment of emergency patients | |||||
| (1) Emergency treatment management at screening centers | 159 (0.4) | 150 (0.4) | 309 (0.4) | ||
| (2) Treatment management at emergency treatment centers for severely ill patient | 464 (1.2) | 108 (0.3) | 572 (0.8) | ||
| (3) Reserve bed for emergency patient/cohort isolated area/portable isolated bed | 9 (0.0) | 34 (0.1) | 43 (0.1) | ||
| 4. Other patient treatments except COVID-19 | 3275 (8.7) | 946 (2.8) | 4221 (5.9) | ||
| 1) Medical fee for telemedicine | 744 (2.0) | 283 (0.8) | 1027 (1.4) | ||
| 2) National Safety Hospitals | 1223 (3.3) | 138 (0.4) | 1361 (1.9) | ||
| 3) Respiratory clinics | 1285 (3.40) | 390 (1.2) | 1675 (2.4) | ||
| 4) Isolated area management for operating/delivery room | 1 (0.0) | 24 (0.1) | 25 (0.0) | ||
| 5) Dialysis patients | 22 (0.1) | 111 (0.3) | 133 (0.2) | ||
| 5. Other support for effective COVID-19 responses | 10615.35 (28.3) | 411 (1.2) | 11026.4 (15.5) | ||
| 1) Nighttime nursing care | 268 (0.7) | 171 (0.5) | 439 (0.6) | ||
| 2) Infection management for COVID19 medical personnel | 1399 (3.7) | 2 (0.0) | 1401 (2.0) | ||
| 3) COVID19 vaccination(temporary) | 8588 (22.9) | 0 (0.0) | 8588 (12.1) | ||
| 4) Health certificate(temporary) | 360 (1.0) | 238 (0.7) | 598 (0.8) | ||
| 5) COVID-19-related depression | 0.35 (0.0) | 0.05 (0.0) | 0.4 (0.0) | ||
PCR, polymerase chain reaction.
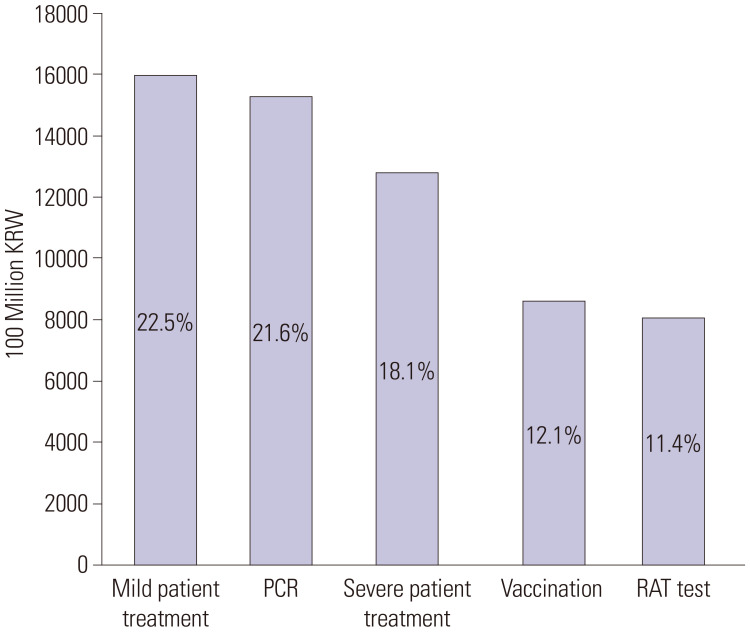
The service items in descending order of their proportions and total costs are as follows (Fig. 2): 1) mild patient treatment (residential treatment centers and home treatment), 22.5% (KRW 1.59 trillion); 2) COVID-19 polymerase chain reaction (PCR) testing, 21.6% (KRW 1.54 trillion); 3) inpatient care (e.g., critically ill patients), 18.1% (KRW 1.28 trillion); 4) vaccination, 12.1% (KRW 0.85 trillion); and 5) rapid antigen testing, 11.4% (KRW 0.81 trillion).9,10,11,12
Fig. 2. Expenditure of COVID-19 coverage items in NHI.10,12 PCR, polymerase chain reaction; RAT, rapid antigen testing; NHI, National Health Insurance.
Since the first case in 2020, the MOHW announced reimbursement for about 36 medical service items related to COVID-19. In 2022, the surge in confirmed cases due to the Omicron variant was reflected in an increase in health insurance expenditures. According to government audit data on October 13, 2022,13 the cost for COVID-19-related services were KRWs 0.35 trillion in 2020 and 3.03 trillion in 2021, which corresponds to 0.4% and 3.2% of the total NHI expenditure, respectively. In the first half of 2022, the COVID-19-related costs rose to KRW 4.22 trillion, about 8.4% of the NHI’s total expenditure (KRW 50.0 trillion14). If the cost in the first half is doubled, it is expected to reach 8.44 trillion won in 2022, a 178% increase from the previous year.
The cost burden for vaccines (12.1% of the total cost from January 2020 to June 2022), tests (21.6%), and mildly infected patients (22.5%) has been rapidly increasing, compared to that for the treatment of severely infected patients (18.1%).10 To this end, the MOHW discussed ways to efficiently utilize limited health insurance resources, such as adjusting service items and co-payment rates.9 In the prolonged COVID-19 pandemic, medical insurance benefits should be adjusted flexibly by predicting their financial impact and expected effects. In addition, expansion of financial resources is required through various means of raising funds. Ultimately, a sound and sustainable NHI system must be maintained.
Similar to Korea, Japan and Taiwan have universal NHI systems, and their health authorities expanded medical benefits for COVID-19-related medical procedures.15 The Japanese Parliament decided to release a supplementary budget for COVID-19 outbreak in 2020.16 This included financial support for health resource capacity for PCR testing, medical personnel, medical infrastructure with masks and ventilators, and research and development of vaccines.
To respond to the COVID-19 outbreak, Korea has implemented various strategies and policies to manage and mitigate the impact of the crisis on the healthcare system and society in general. A framework for evaluating the OECD’s COVID-19 responses was developed to identify government policy responses. The three policy responses correspond to the phases of the risk management cycle: pandemic preparedness, crisis management, and response and recovery.17 Reflecting this, we will examine Korea’s policy response, focusing on the medical system and comparing it with Japan and Taiwan.
Pandemic preparedness refers to a government’s ability to anticipate a pandemic by developing necessary knowledge and capacity.17 The designated COVID-19 control tower and the Infectious Disease Act were revised to fight the pandemic in Korea. Having experienced Middle East respiratory syndrome in 2015, the government recognized the importance of infectious disease management. Through the preparatory process, it strengthened its capacity for infectious disease management and laid its administrative foundations. With the outbreak of COVID-19 in 2020, the KDCA, promoted from the Korea Centers for Disease Control and Prevention in 2020) has been monitoring the pandemic situation and preparing related strategies, such as testing, tracing, and treating potential and confirmed cases.18 Also, Taiwan’s experience with SARS strengthened its epidemic prevention system, redefined its infectious disease control laws, and led to stronger governance during COVID-19 period.19 Japan does not have an independent administrative agency for disease control and prevention. The National Institute of Infectious Disease is responsible for research and administrative support with lack of decision-making autonomy.20
On February 23, 2020, the Central Disaster and Safety Countermeasures Headquarters in Korea was established to control and manage the COVID19 crisis with the highest official authority.18 The Novel Coronavirus Response Headquarters in Japan was officially established when a related law was passed on March 26, 2020.20 The Taiwan Centers for Disease Control officially activated the Central Epidemics Command Center as a central commending center on January 20, 2020.19,21 In these countries, control towers, headed by the prime ministers, played critical roles in collaboration with local governments and communication across different ministries and agencies.
Deployed government policies must respond in an appropriate, timely, and coordinated manner.17 Crisis management also requires clear communication to the public and transparent decision-making. Since the COVID-19 crisis, governments have implemented strategies and policies affecting all of society, such as social distancing, face mask use, quarantine, and border blockades (in Japan and Taiwan).3,18,19,20
The pandemic has placed pressure on medical resource capacity, and countries have responded with various measures to control resource shortages. In Korea, the MOHW secured beds by cooperating with private hospital and implementing administer orders.22 The level of cooperation with private hospitals has differed among countries: requested at the recommended level in Japan23 and legally obligated in Taiwan.24
Also, to solve patient acceptance at medical institutions, patients with mild symptoms in the triage system have been treated at residential treatment centers and home treatment in Korea,18 similar in Japan23 and Taiwan.24 All confirmed COVID-19 patients were initially hospitalized in infectious disease isolation rooms. However, as the number of patients increased, patients with mild symptoms were treated at residential treatment centers and at home. As more than 90% of hospital beds in Korea are in private medical institutions,25 the MOHW had to secure the beds by working with private hospitals and implementing administrative orders. Medical resources were procured through the fast-track approval system for diagnostic reagents, and vaccination began in February 2021, reaching a vaccination rate of 88% in 2022.8
An effective pandemic response requires having control systems in place to prevent transmission and mitigate health impacts. As the outbreak continues, countries have implemented a range of policies and appropriate initial response measures to manage the crisis. An integrated approach to managing healthcare resources and healthcare expenditures can increase resilience and better prepare for future crises.
In order to effectively respond to the epidemic of COVID-19, an unprecedented infectious disease, Korea has used health insurance finances to support medical expenses and costs related with tests and vaccination. It has also proactively responded by strengthening various laws and governance and adjusting health insurance policies. However, in order to prepare for the post-COVID-19 era, it is necessary to assess the effectiveness and efficiency of these policies.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Yoon Jung Choi and Tae Hyun Kim.
- Data curation: Yoon Jung Choi.
- Formal analysis: Yoon Jung Choi.
- Methodology: Yoon Jung Choi.
- Project administration: all authors.
- Resources: Yoon Jung Choi and Tae Hyun Kim.
- Supervision: Tae Hyun Kim.
- Validation: Jungwoo Sohn and Tae Hyun Kim.
- Writing—original draft: Yoon Jung Choi and Tae Hyun Kim.
- Writing—review & editing: all authors.
- Approval of final manuscript: all authors.
References
- 1.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Korea Disease Control and Prevention Agency. COVID-19 social distancing 2020. [accessed on 2022 August 22]. Available at: https://ncov.kdca.go.kr/tcmBoardView.do?brdId=&brdGubun=&dataGubun=&ncvContSeq=353917&contSeq=353917&board_id=&gubun=ALL .
- 3.Korea Disease Control and Prevention Agency. Government Business Report 2021. [accessed on 2022 August 25]. Available at: https://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015&act=view&list_no=711912.
- 4.Ministry of Health and Welfare. Current status of the national health insurance medical fee introduced by the Korean government in response to COVID-19. [accessed on 2022 September 10]. Available at: https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020002000100&brdScnBltNo=4&brdBltNo=9378&pageIndex=1 .
- 5.Korea Legislation Research Institute. Infectious disease control and prevention act. [accessed on 2022 August 16]. Available at: https://elaw.klri.re.kr/kor_service/lawView.do?hseq=53530&lang=ENG .
- 6.Health Insurance Review and Assessment. National Health Accounts, 2020. [accessed on 2022 July 25]. Available at: https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020045030000.
- 7.Health Insurance Review and Assessment. Analysis of health care utilization and effect related to COVID-19 in health insurance system. Wonju: HIRA; 2021. [Google Scholar]
- 8.CoronaBoard. Covid-19 dashboard [Internet] [accessed on 2021 August 22]. Available at: https://coronaboard.kr/
- 9.Ministry of Health and Welfare. The 16th health insurance policy review committee in 2022 [Internet] [accessed on 2022 July 20]. Available at: http://www.mohw.go.kr/react/jb/sjb0703vw.jsp?PAR_MENU_ID=04&MENU_ID=0425&CONT_SEQ=372246 .
- 10.Medical Times. During the corona pandemic, 1.46 trillion won was invested in non-face-to-face treatment alone [Internet] [accessed on 2022 July 2]. Available at: https://m.medicaltimes.com/News/NewsView.html?ID=1148517 .
- 11.Ministry of Health and Welfare. The 5th health insurance policy review committee in 2022. [accessed on 2022 February 25]. Available at: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=370391 .
- 12.News the Voice for Healthcare. Corona 19 input health insurance finance 3.74 trillion won..30% is diagnostic and test cost [Internet] [accessed on 2022 March 23]. Available at: https://www.newsthevoice.com/news/articleView.html?idxno=26004 .
- 13.Medigate News. Injecting 5.6 trillion won in health insurance finance to respond to corona 19 “we have to fill it up again with state treasury support [Internet] [accessed on 2022 October 23]. Available at: https://medigatenews.com/news/2914684676 .
- 14.National Health Insurance Service. Health long-term care insurance major statistics for the first half of 2022. [accessed on 2022 October 23]. Available at: https://www.nhis.or.kr/nhis/together/wbhaec07100m01.do?mode=view&articleNo=10828799&article.offset=0&articleLimit=10 .
- 15.Yeh MJ, Cheng Y. Policies tackling the COVID-19 pandemic: a sociopolitical perspective from Taiwan. Health Secur. 2020;18:427–434. doi: 10.1089/hs.2020.0095. [DOI] [PubMed] [Google Scholar]
- 16.Tokumoto A, Akaba H, Oshitani H, Jindai K, Wada K, Imamura T COVID-19 health system response monitor: Japan. [accessed on 2022 October 23]. Available at: https://apps.who.int/iris/handle/10665/338399 .
- 17.OECD. First lessons from government evaluations of COVID-19 responses: a synthesis [Internet] [accessed on 2022 October 23]. Available at: https://www.oecd.org/coronavirus/policy-responses/first-lessons-from-government-evaluations-of-covid-19-responses-a-synthesis-483507d6/
- 18.Kim W, Jung TY, Roth S, Um W, Kim C. Management of the COVID-19 pandemic in the Republic of Korea from the perspective of governance and public-private partnership. Yonsei Med J. 2021;62:777–791. doi: 10.3349/ymj.2021.62.9.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang CJ, Ng CY, Brook RH. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020;323:1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 20.Moon MJ, Suzuki K, Park TI, Sakuwa K. A comparative study of COVID-19 responses in South Korea and Japan: political nexus triad and policy responses. Int Rev Adm Sci. 2021;87:651–671. [Google Scholar]
- 21.Huang IY. Fighting COVID-19 through government initiatives and collaborative governance: the Taiwan experience. Public Adm Rev. 2020;80:665–670. doi: 10.1111/puar.13239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ministry of Health and Welfare. Additional hospital bed expansion and operation plan to overcome daily recovery crisis. [accessed on 2022 August 11]. Available at: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=5&CONT_SEQ=369031 .
- 23.Yamamoto T, Ozaki M, Kasugai D, Burnham G. Assessment of critical care surge capacity during the COVID-19 pandemic in Japan. Health Secur. 2021;19:479–487. doi: 10.1089/hs.2020.0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Laws and Regulations Database. Special act for prevention, relief and revitalization measures for severe pneumonia with novel pathogens [Internet] [accessed on 2022 August 11]. Available at: https://law.moj.gov.tw/LawClass/LawAll.aspx?pcode=L0050039 .
- 25.Organization for Economic Cooperation and Development. OECD Health Statistics 2022. [cited 2022 Octerver 24]. Available at: https://www.oecd.org/health/health-data.htm .