Abstract
More meniscus tears are being repaired because this has been shown to delay the onset of osteoarthritis compared with partial meniscectomy. However, there still remains a subset of tears that may be viewed as less amenable to repair due to poorer healing potential. Fibrin clots have been used to augment healing for meniscus tears located in avascular regions due to their potential to promote healing and ability to be easily prepared at a low cost. Placement of fibrin clots within a meniscus repair can be technically challenging. Here, we describe a technique for placing a fibrin clot within a meniscus tear site repaired with an inside-out technique. A passing suture through the tear aids to shuttle the fibrin clot into the tear site and is then secured within the tear by tying down the repair sutures around the clot. This technique is efficient, less technically demanding, and can be accomplished without additional specialized instruments.
Technique Video
The patient is intubated and placed in a supine position on the operating table. A knee examination is performed, including range of motion and ligamentous integrity tests. Medial and lateral arthroscopic parapatellar portal incisions are made and a comprehensive diagnostic arthroscopy is performed. The meniscal tear is identified and probed. A posterolateral incision is made in preparation for passing inside out meniscal sutures. An assistant stirs 20 mL of the patient’s blood using a frosted glass syringe within a small sterile cup to form the clot. Saucerization of the discoid meniscus is performed in this case and is then followed by placement of inside-out sutures along the posterior and mid body portions of the meniscus tear. Outside-in sutures are also placed in the anterior portion of the meniscus tear. One limb of a new meniscus suture is cut from the needle and tied around the well-formed fibrin clot. The remaining meniscus needle is driven through a cannula and through the meniscus tear with the fibrin clot attached on the other end. Once the fibrin clot is correctly positioned, the inside-out and outside-in sutures are tightened around the knot and tied in place. An arthroscopic probe is used to confirm the meniscus is well-stabilized. The tourniquet is then let down and wound closure is performed.
The meniscus plays a critical role in tibiofemoral load distribution and stabilization.1, 2, 3, 4 Damage to the meniscus has been shown to accelerate progression of osteoarthritis in the tibiofemoral joint and may result in significant pain and discomfort.1, 2, 3, 4, 5, 6 In the last decade, a growing push has been made to preserve the meniscus when possible.3, 4, 5,7 Repair of the meniscus has been shown to slow the onset of osteoarthritis and significantly improve patient outcomes when compared with meniscectomy.2,4,6, 7, 8 However, controversy exists regarding which meniscal tear types are amenable for repair. This is particularly true when tears are predominantly located in a relatively avascular region of the meniscus or if patient age or biological characteristics are less favorable.9, 10, 11
Fibrin clots have been used as a form of biologic augmentation to promote healing of the meniscus following repair of complex tears involving avascular areas.8,12, 13, 14, 15, 16, 17 Other nonstructural options exist for augmenting meniscal repairs, including bone marrow aspirate concentrate (BMAC) and platelet-rich plasma (PRP). However, these techniques are expensive and require additional equipment. In addition, BMAC harvest may have associated procedural risks and technical difficulty.11,12,15
Fibrin clots are easy to prepare, may stimulate healing, and are an inexpensive alternative to other healing augmentation techniques.4,8,13,14,16 However, precise placement of the fibrin clot can present a technical challenge due to the need to shuttle it into the joint and deliver it to the tear site following placement of inside-out repair sutures. In this article, we describe a technique for a precise and reproducible method of harvesting and placing a fibrin clot within the prepared meniscus tear site.
Surgical Technique (With Video Illustration)
Patient Positioning
The patient is brought into the operating room and placed in the supine position. The patient is then induced under general anesthesia. An examination under anesthesia, including assessment of knee range of motion and ligamentous stability, is performed before preparation of the extremity. Depending on the surgeon’s preference, a lateral post may be used or a leg holder may be used with the foot of the table removed. The operative lower extremity is then prepped and draped in standard sterile fashion.
Diagnostic Arthroscopy
Medial and lateral arthroscopic parapatellar portals are made. The arthroscopic camera is inserted and the knee is insufflated with normal saline. A comprehensive diagnostic arthroscopy is performed. The arthroscopic findings are correlated with the preoperative magnetic resonance imaging. The meniscal tear is identified and probed (Fig 1). It is important to evaluate the tear for the presence of a hidden horizontal tear component.
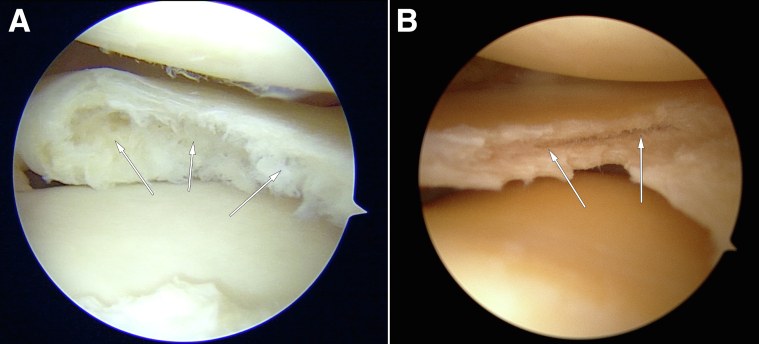
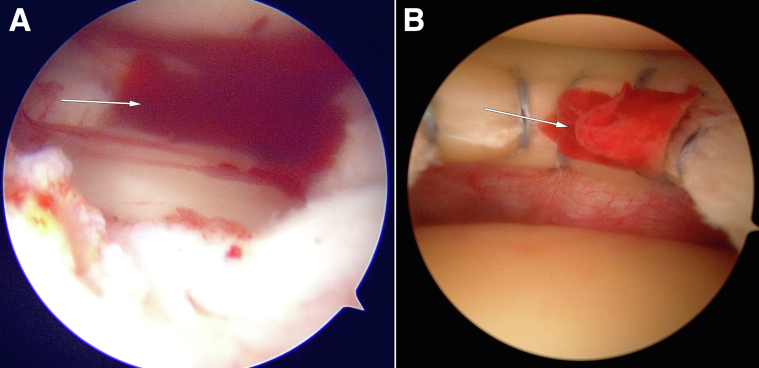
Fig 1.
Arthroscopic visualization of the left knee lateral menisci showing horizontal cleavage tears (white arrows) following saucerization of a discoid lateral meniscus (A-B). An 8- to 9-mm rim should remain following saucerization to preserve the biomechanical function of the meniscus and minimize the onset of osteoarthritis following repair.
Posteromedial and Posterolateral Approach
A posterolateral or posteromedial approach may be used depending on the laterality of the meniscus tear. For a posterolateral approach, the surgeon should identify anatomic landmarks including Gerdy’s tubercle, the superficial layer of the iliotibial band (ITB), lateral aspect of the fibular head, and lateral joint line.6 A transverse oblique incision should be created along the posterior border of the ITB down to Gerdy’s tubercle centered over the lateral joint line. While taking care to avoid injuring the fibular collateral ligament, the superficial layer of the ITB is then incised along the posterior aspect. Care should also be taken to avoid injuring the inferior–lateral genicular artery over the popliteus musculotendinous junction.6 Blunt dissection should be performed above the fibular head and proximal to the long and short heads of the biceps tenson. A Cobb elevator may be used to release any adhesions between the lateral gastrocnemius and the posterolateral joint capsule. A retractor may be placed in this interval to protect the neurovascular bundle.6
In cases in which a posteromedial approach is indicated, the surgeon should first identify the appropriate anatomic landmarks, by palpation of a surgical probe placed inside the knee at the region of the medial meniscus tear, as well as the adductor tubercle, posterior aspect of the tibial plateau, and medial joint line. An oblique vertical incision should be created from the adductor tubercle to the posterior aspect of the medial tibial plateau. Care should be taken to avoid the saphenous nerve which runs posterior to this incision.6 Dissection should then be performed down to the sartorius fascia. The sartorius fascia should be incised as proximally as possible to preserve the pes anserine tendons. An anatomic triangle composed of the posteromedial joint capsule, medial gastrocnemius, and the semimembranosus can be visualized following blunt dissection from the sartorial fascia.6 A Cobb elevator may be used to separate the medial gastrocnemius tendon and muscle from the posterior capsule. A retractor can then be placed in this interval to protect the popliteal vessels.
Meniscal Repair
In the setting of a discoid meniscus tear, saucerization is performed using a basket punch, angled punch, and a straight or curved shaver and an 8- to 9-mm rim is maintained (Fig 2, Table 1). Parameniscal cysts often form in the setting of horizontal meniscus tears and may be decompressed into the joint during probing of the tear. A meniscal rasp and shaver are then used within the substance of the horizontal cleavage tear to abrade the tissue and promote healing. Suction should be off while using the shaver to avoid removing excessive tissue volume from inside the horizontal cleavage tear.
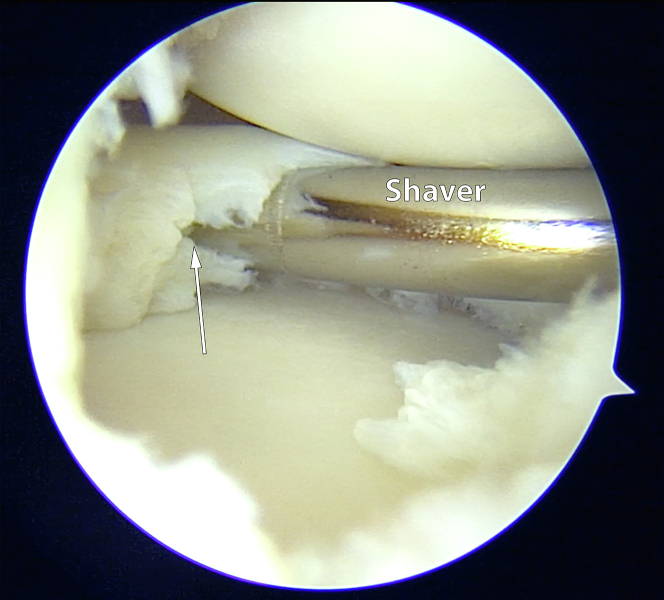
Fig 2.
Arthroscopic visualization of the left knee lateral meniscus showing a straight shaver being used to prepare the meniscus for repair. A shaver is used to abrade the tissue inside of the tear (white arrow) and maximize healing. This should be done to increase healing potential and improve the patient’s recovery process.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| A meniscal rasp and shaver can be used to roughen the meniscus tear edges and promote healing. | If a clot fails to form, thromboxane may be used to accelerate formation of the clot. |
| Mix with a properly frosted glass syringe plunger to effectively form a fibrin clot. | Avoid tightening meniscal sutures before placement of the fibrin clot. |
| Once the clot is sufficiently formed, tie a suture through the clot to provide further substance to allow for efficient clot passage. | Using a fibrin clot without sufficient substance may increase difficulty tying sutures around the clot. |
| A cannula may be used to ease passage of the fibrin clot. |
An arthroscopic probe is then placed inside the joint to localize where the inside-out meniscus repair incision should be made. An incision is then made to facilitate inside-out repair, depending on the meniscus tear site. If a parameniscal cyst is present, it should be carefully excised or decompressed and the capsule must be preserved to support the inside-out suture fixation.
A SharpShooter device (Stryker, Kalamazoo, MI) is used to place multiple inside-out vertical mattress sutures. During repair of a horizontal tear, a typical superior or inferior vertical mattress suture is often not feasible due to tear obliquity, and a cerclage pattern is used, where one limb of the suture is passed superior to the top leaflet and the second is placed inferior to the bottom leaflet (Fig 3). Suture pairs are sequentially tagged after retrieval and secured with an Allis clamp to avoid entanglement outside the knee. For tear patterns that extend anteriorly, the arthroscopic portal incision may be extended and 0-PDS (polydioxanone) absorbable sutures (Ethicon, Raritan, NJ) may be placed with the outside-in technique using a Meniscus Mender (Smith & Nephew, London, UK).18 The stiffness of the absorbable monofilament suture allows for easy passage and retrieval of the device. Adequate suture density for repair of the meniscal tear is confirmed at this point (Fig 4).
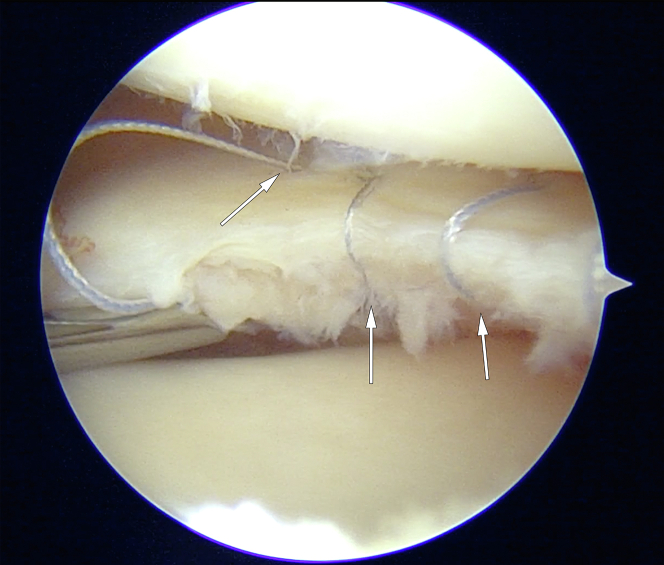
Fig 3.
Arthroscopic visualization of the left knee lateral meniscus showing inside-out meniscal sutures (white arrows) being placed in a cerclage fashion around the horizonal cleavage tear. The sutures should not be tied until after the fibrin clot has been placed and confirmed to be stable. This allows for the fibrin clot to be placed in the optimal position with adjustments if necessary.
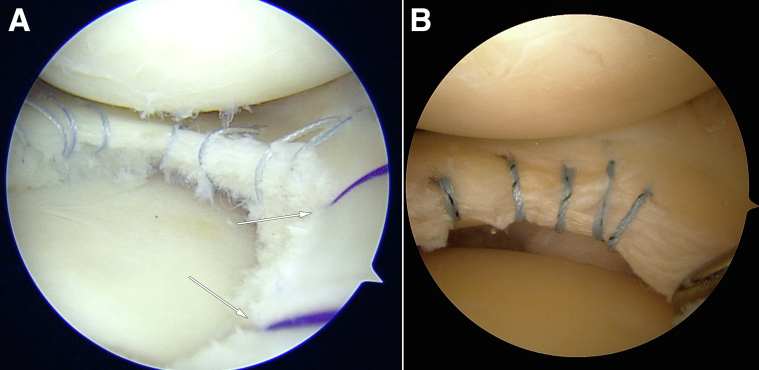
Fig 4.
Arthroscopic images of a left knee lateral menisci illustrating completed passage of the inside-out sutures in a cerclage stitch pattern (A-B). Outside-in 0-PDS meniscal sutures (A, white arrows) may be used for horizontal cleavage tears that extend more anteriorly along the meniscal body. It is recommended to use outside-in sutures for the anterior portion of the tear because this region of the meniscus is not amenable to inside-out sutures due to visualization limitations.
Fibrin Clot Preparation and Delivery
Approximately 20 mL of the patient’s blood is obtained from the antecubital fossa, which can be performed by the anesthesia provider during the examination under anesthesia. The blood is placed in a small sterile specimen cup and then stirred using a frosted glass syringe plunger until a high-quality fibrin clot is formed (Fig 5, Table 2). Of note, stirring may take up to 15 minutes with intermittent pauses to form a high-quality fibrin clot. The fibrin clot is then prepared on the back table, where it is gently washed with normal saline to remove excess blood products that will complicate visualization during shuttling into the knee. A 0-VICRYL (Ethicon) suture is tied around the fibrin clot to provide further substance to the clot (Fig 6).
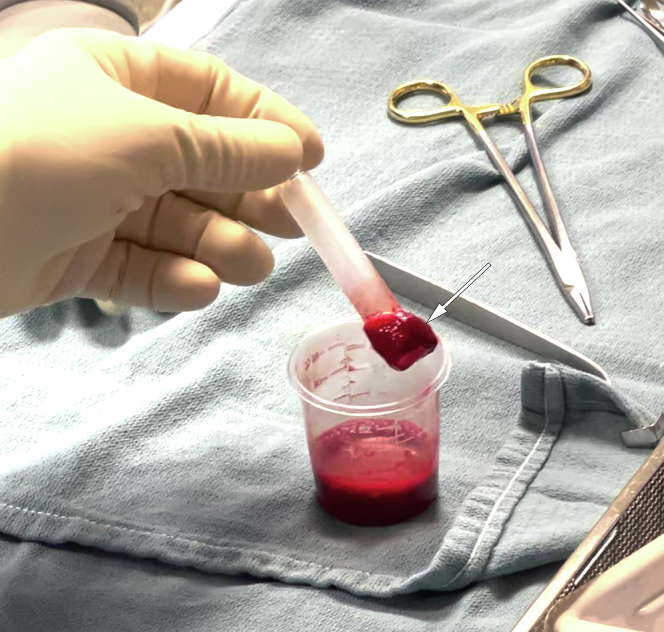
Fig 5.
Intraoperative image illustrating fibrin clot (white arrow) formation on the frosted glass syringe plunger. Approximately 20 mL of the patient’s blood should be stirred in a sterile specimen container until a high-quality clot is formed. The amount of frosting on the glass syringe may affect clot formation time. Intermittent pauses in stirring may also benefit clot formation.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| Fibrin clot placement promotes improved healing of complex meniscus tears | Timing of fibrin clot formation may be inconsistent based on patient blood composition and the amount of frosting on glass syringe. |
| More cost-effective than alternative biologic augmentation options | |
| Shuttling technique allows for precise and replicable placement of the fibrin clot |
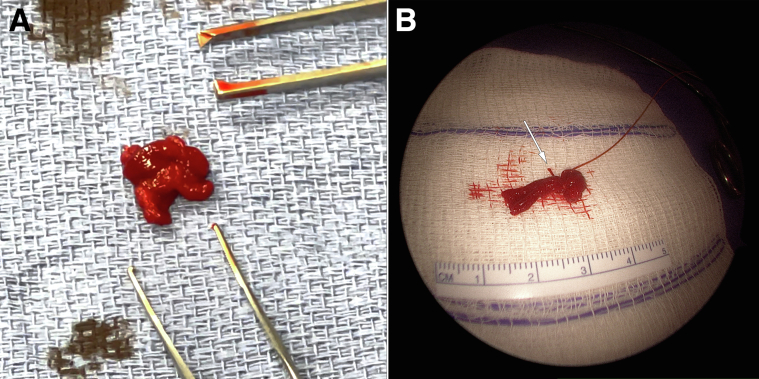
Fig 6.
Intraoperative images of the prepared fibrin clots (A-B). Once the clot is washed of any excess unclotted blood, a 0 VICRYL suture (B, white arrow) is passed through the clot to improve the substance of the clot. It is recommended to verify that the clot is of sufficient substance prior to passing the suture. This is to ensure that the clot will not break apart as a result of tying the suture around it.
The SharpShooter device is used to pass one limb of a 2-0 FiberWire Meniscus Repair Needle (Arthrex) into the main portion of the horizontal cleavage tear where the fibrin clot will be placed and the needle of the second limb is cut. Alternatively, in the setting of a horizontal tear in the meniscal body or anterior horn, a 0 PDS suture may be placed through an 18-gauge spinal needle and retrieved through an arthroscopic portal and used for shuttling (Fig 7). The arthroscopic portal is dilated or a cannula is used to facilitate delivery of the fibrin clot.
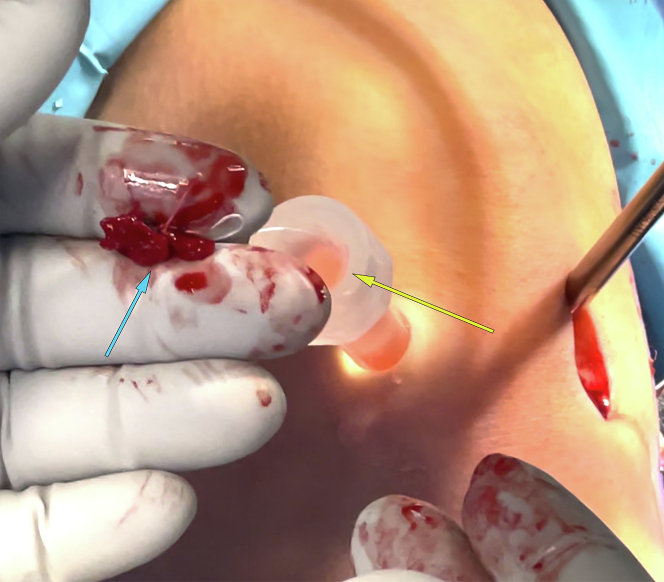
Fig 7.
Intraoperative image of the left knee of the fibrin clot (blue arrow) being shuttled through a canula (yellow arrow) and through the anteromedial arthroscopy portal. One end of the meniscal needle is placed through the horizontal cleavage tear, and the second needle is cut off. The remaining suture is tied around the previously placed intra-clot suture and used to guide the clot into the tear.
The VICRYL suture from the fibrin clot is tied to the end of the shuttling suture. The repair sutures are loosened to allow delivery of the fibrin clot into the horizontal tear. The shuttling suture is then gently pulled to deliver the fibrin clot directly into the horizontal cleavage tear (Fig 8). The repair sutures are then manipulated with the arthroscopic probe over the fibrin clot and light tension is applied by pulling the extra-articular suture limbs. The meniscal repair sutures are then tied and the fibrin clot is secured within the tear (Fig 9). An arthroscopic probe is used to confirm the meniscus is well stabilized.
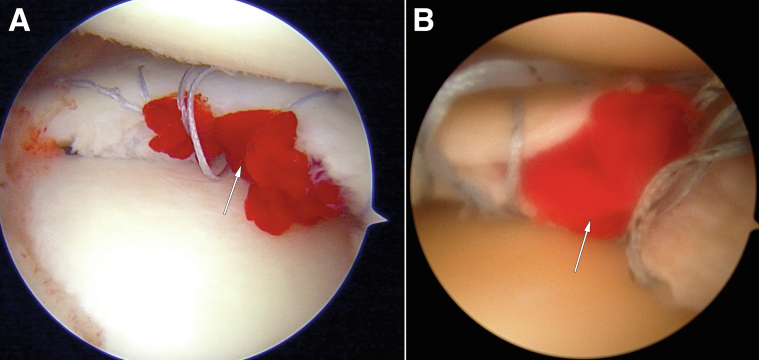
Fig 8.
Arthroscopic visualization left knee lateral menisci showing correct placement of the fibrin clot (A-B, white arrows) following shuttling. The previously placed sutures are manipulated with a probe to fit around the clot and lightly secure it in place. This method of shuttling allows for precise and reproducible placement of the clot within the horizontal cleavage tear.
Fig 9.
Arthroscopic visualization of left knee lateral menisci showing the stable fibrin clot (A-B, white arrows) following suture fixation. The fibrin clot is confirmed to lie stabile within the correct area of the horizontal meniscal repair. It is critical not to tie any sutures before placement of the fibrin clot to prevent incorrect placement of the fibrin clot.
A marrow venting procedure is performed using a microfracture awl to place perforations in the lateral aspect of the intercondylar notch.19 This procedure grants access to the marrow cavity and serves as an additional biologic augment for this complex tear type (Fig 10, Video 1). The tourniquet is then let down and blood can be observed from the perforations.
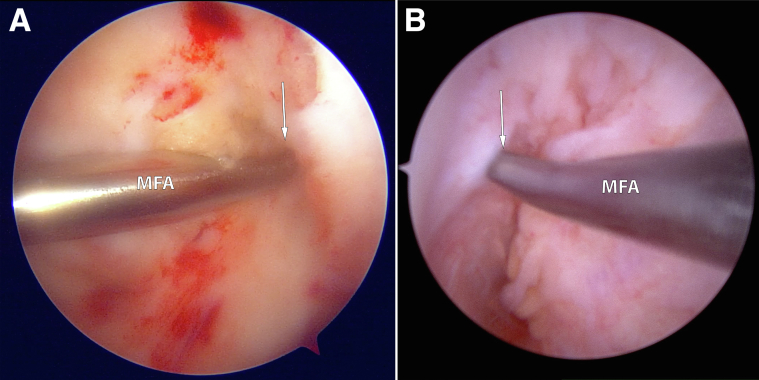
Fig 10.
Arthroscopic visualization of the left knee lateral intercondylar notch (A) and right knee lateral intercondylar notch (B) showing a marrow venting procedure that is performed following the repair of the horizontal cleavage tear. A marrow venting procedure is performed along the lateral aspect of the intercondylar notch (white arrows). This procedure allows for additional augmentation of meniscal healing secondary to increased healing factors released from the bone marrow. (MFA, microfracture awl.)
Postoperative Rehabilitation
A knowledgeable and effective physical therapy team is essential to optimize meniscus healing and knee functional recovery. The patient is initially non–weight-bearing on the surgical extremity for 6 weeks’ postoperatively. Flexion of the knee is limited to 90° for the first 2 weeks, after which range of motion may be gradually increased as tolerated. Physical therapy begins on postoperative day 1, focusing on quadriceps activation, edema control, and knee motion. Prophylaxis for deep-vein thrombosis is performed based on patient risk factors and is maintained until weight-bearing is initiated. Gradual progression of strengthening is performed and a jogging progression is considered at 12 weeks postoperatively if the patient has adequate muscle strength and no knee effusion. Return to pivoting and impact sports is considered at 6 months’ postoperatively if the patient meets appropriate return to sport testing.
Discussion
The relatively limited vascular supply of the meniscus has historically presented challenges in treating complex meniscal tears.20,21 For older patients, or in the case of degenerative meniscus tears, the biological healing environment is also of concern. Patient outcomes following meniscus repairs can be limited by the healing capacity of the meniscus. The use of biologic augmentation has been explored in recent years as the incidence of meniscus repair procedures has increased. While early studies examining biologics have been promising, there is a need for more long-term outcomes. Fibrin clot augmentation has many benefits over alternatives such as BMAC or PRP. BMAC and PRP are associated with significantly greater costs for disposable and capital equipment required for preparation. Fibrin clots provide an accessible and effective treatment at a lower cost.
Fibrin clots have proven effective in the treatment of meniscal tears.6,11,22 The mechanism through which fibrin clots augment healing of the meniscus has been described by Arnoczky and Warren.9 The fibrin clot placed within the meniscus tear stimulates proliferation of the fibrous connective tissue so that the clot is eventually replaced with fibrocartilaginous tissue.9 While fibrin clot augmentation has shown consistently good outcomes, the procedure can be technically difficult. Optimal healing is dependent on accurate placement of the fibrin clot. This technique illustrates a reproducible, efficient, and less technically challenging method that allows the surgeon to anchor the fibrin clot into the meniscus tear. This technique is particularly useful for complex and horizontal cleavage tears of the meniscus. More studies are needed comparing the outcomes of fibrin clot–augmented repairs with other biologics.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.G.G. reports editorial board, Arthroscopy; editor, Infographics; paid consultant for Smith & Nephew; and paid presenter or speaker for Ossur. R.F.L. reports personal fees from Arthrex; grants and personal fees from Ossur and Smith & Nephew; and personal fees from Linvatec, outside the submitted work; editorials boards of American Orthopaedic Society for Sports Medicine (AOSSM), Journal of Experimental Orthopaedics, and Knee Surgery, Sports Traumatology, Arthroscopy; and committees for AOSSM, AANA, and International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is intubated and placed in a supine position on the operating table. A knee examination is performed, including range of motion and ligamentous integrity tests. Medial and lateral arthroscopic parapatellar portal incisions are made and a comprehensive diagnostic arthroscopy is performed. The meniscal tear is identified and probed. A posterolateral incision is made in preparation for passing inside out meniscal sutures. An assistant stirs 20 mL of the patient’s blood using a frosted glass syringe within a small sterile cup to form the clot. Saucerization of the discoid meniscus is performed in this case and is then followed by placement of inside-out sutures along the posterior and mid body portions of the meniscus tear. Outside-in sutures are also placed in the anterior portion of the meniscus tear. One limb of a new meniscus suture is cut from the needle and tied around the well-formed fibrin clot. The remaining meniscus needle is driven through a cannula and through the meniscus tear with the fibrin clot attached on the other end. Once the fibrin clot is correctly positioned, the inside-out and outside-in sutures are tightened around the knot and tied in place. An arthroscopic probe is used to confirm the meniscus is well-stabilized. The tourniquet is then let down and wound closure is performed.
References
- 1.Beamer B.S., Walley K.C., Okajima S., et al. Changes in contact area in meniscus horizontal cleavage tears subjected to repair and resection. Arthroscopy. 2017;33:617–624. doi: 10.1016/j.arthro.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 2.Krause W.R., Pope M.H., Johnson R.J., Wilder D.G. Mechanical changes in the knee after meniscectomy. J Bone Joint Surg Am. 1976;58:599–604. [PubMed] [Google Scholar]
- 3.Kurzweil P.R., Lynch N.M., Coleman S., Kearney B. Repair of horizontal meniscus tears: A systematic review. Arthroscopy. 2014;30:1513–1519. doi: 10.1016/j.arthro.2014.05.038. [DOI] [PubMed] [Google Scholar]
- 4.Ozeki N., Seil R., Krych A.J., Koga H. Surgical treatment of complex meniscus tear and disease: State of the art. J ISAKOS. 2021;6:35–45. doi: 10.1136/jisakos-2019-000380. [DOI] [PubMed] [Google Scholar]
- 5.Aman Z.S., Dickens J.F., Dekker T.J. Meniscal repair techniques for middle- and posterior-third tears. Arthroscopy. 2021;37:792–794. doi: 10.1016/j.arthro.2021.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Chahla J., Serra Cruz R., Cram T.R., Dean C.S., LaPrade R.F. Inside-out meniscal repair: Medial and lateral approach. Arthrosc Tech. 2016;5:e163–e168. doi: 10.1016/j.eats.2015.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krych A.J., Reardon P., Sousa P., Levy B.A., Dahm D.L., Stuart M.J. Clinical outcomes after revision meniscus repair. Arthroscopy. 2016;32:1831–1837. doi: 10.1016/j.arthro.2016.01.070. [DOI] [PubMed] [Google Scholar]
- 8.Chahla J., Kennedy N.I., Geeslin A.G., et al. Meniscal repair with fibrin clot augmentation. Arthrosc Tech. 2017;6:e2065–e2069. doi: 10.1016/j.eats.2017.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arnoczky S.P., Warren R.F. The microvasculature of the meniscus and its response to injury. An experimental study in the dog. Am J Sports Med. 1983;11:131–141. doi: 10.1177/036354658301100305. [DOI] [PubMed] [Google Scholar]
- 10.Barber-Westin S.D., Noyes F.R. Clinical healing rates of meniscus repairs of tears in the central-third (red-white) zone. Arthroscopy. 2014;30:134–146. doi: 10.1016/j.arthro.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Chahla J., Cinque M.E., Godin J.A., Geeslin A.G., Moatshe G., LaPrade R.F. Review of Arnoczky and Warren on the microvasculature of the human meniscus. J ISAKOS. 2017;2:229–232. [Google Scholar]
- 12.Blough CL, Bobba CM, DiBartola AC, et al. Biologic augmentation during meniscal repair [published online November 15, 2021]. J Knee Surg. https://doi.org/10.1055/s-0041-1739198. [DOI] [PubMed]
- 13.Desai T., Babu S.S., Lal J.V., Kaushik Y.S., Lukose A.M., Sandesh G.M., et al. Fibrin clot augmented repair of longitudinal tear of medial meniscus. Arthrosc Tech. 2021;10:e2449–e2455. doi: 10.1016/j.eats.2021.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamimura T., Kimura M. Repair of a chronic large meniscal defect with implantation of autogenous meniscal fragments using a tubular-shaped fibrin clot. Arthrosc Tech. 2018;7:e257–e263. doi: 10.1016/j.eats.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Longo U.G., Campi S., Romeo G., Spiezia F., Maffulli N., Denaro V. Biological strategies to enhance healing of the avascular area of the meniscus. Stem Cells Int. 2012;2012 doi: 10.1155/2012/528359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Port J., Simon T.M., Jackson D.W. Preparation of an exogenous fibrin clot. Arthroscopy. 1995;11:332–337. doi: 10.1016/0749-8063(95)90013-6. [DOI] [PubMed] [Google Scholar]
- 17.Yamanashi Y., Kato T., Akao M., Takata T., Kobayakawa K., Deie M. Meniscal repair using fibrin clots made from bone marrow blood wrapped in a polyglycolic acid sheet. Arthrosc Tech. 2021;10:e2541–e2546. doi: 10.1016/j.eats.2021.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Menge T.J., Dean C.S., Chahla J., Mitchell J.J., LaPrade R.F. Anterior horn meniscal repair using an outside-in suture technique. Arthrosc Tech. 2016;5:e1111–e1116. doi: 10.1016/j.eats.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dean C.S., Chahla J., Matheny L.M., Mitchell J.J., LaPrade R.F. Outcomes after biologically augmented isolated meniscal repair with marrow venting are comparable with those after meniscal repair with concomitant anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:1341–1348. doi: 10.1177/0363546516686968. [DOI] [PubMed] [Google Scholar]
- 20.Arnoczky S.P., Warren R.F. Microvasculature of the human meniscus. Am J Sports Med. 1982;10:90–95. doi: 10.1177/036354658201000205. [DOI] [PubMed] [Google Scholar]
- 21.Crawford M.D., Hellwinkel J.E., Aman Z., et al. Microvascular anatomy and intrinsic gene expression of menisci from young adults. Am J Sports Med. 2020;48:3147–3153. doi: 10.1177/0363546520961555. [DOI] [PubMed] [Google Scholar]
- 22.Ra H.J., Ha J.K., Jang S.H., Lee D.W., Kim J.G. Arthroscopic inside-out repair of complete radial tears of the meniscus with a fibrin clot. Knee Surg Sports Traumatol Arthrosc. 2013;21:2126–2130. doi: 10.1007/s00167-012-2191-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is intubated and placed in a supine position on the operating table. A knee examination is performed, including range of motion and ligamentous integrity tests. Medial and lateral arthroscopic parapatellar portal incisions are made and a comprehensive diagnostic arthroscopy is performed. The meniscal tear is identified and probed. A posterolateral incision is made in preparation for passing inside out meniscal sutures. An assistant stirs 20 mL of the patient’s blood using a frosted glass syringe within a small sterile cup to form the clot. Saucerization of the discoid meniscus is performed in this case and is then followed by placement of inside-out sutures along the posterior and mid body portions of the meniscus tear. Outside-in sutures are also placed in the anterior portion of the meniscus tear. One limb of a new meniscus suture is cut from the needle and tied around the well-formed fibrin clot. The remaining meniscus needle is driven through a cannula and through the meniscus tear with the fibrin clot attached on the other end. Once the fibrin clot is correctly positioned, the inside-out and outside-in sutures are tightened around the knot and tied in place. An arthroscopic probe is used to confirm the meniscus is well-stabilized. The tourniquet is then let down and wound closure is performed.
The patient is intubated and placed in a supine position on the operating table. A knee examination is performed, including range of motion and ligamentous integrity tests. Medial and lateral arthroscopic parapatellar portal incisions are made and a comprehensive diagnostic arthroscopy is performed. The meniscal tear is identified and probed. A posterolateral incision is made in preparation for passing inside out meniscal sutures. An assistant stirs 20 mL of the patient’s blood using a frosted glass syringe within a small sterile cup to form the clot. Saucerization of the discoid meniscus is performed in this case and is then followed by placement of inside-out sutures along the posterior and mid body portions of the meniscus tear. Outside-in sutures are also placed in the anterior portion of the meniscus tear. One limb of a new meniscus suture is cut from the needle and tied around the well-formed fibrin clot. The remaining meniscus needle is driven through a cannula and through the meniscus tear with the fibrin clot attached on the other end. Once the fibrin clot is correctly positioned, the inside-out and outside-in sutures are tightened around the knot and tied in place. An arthroscopic probe is used to confirm the meniscus is well-stabilized. The tourniquet is then let down and wound closure is performed.