Abstract
In-office needle arthroscopy (IONA) has been available in various iterations for decades. Studies have described it as comparable if not superior to magnetic resonance imaging for identifying intra-articular pathology with associated cost savings per patient. A new IONA system has been brought to market with a modernized user interface and disposable handpieces offering the opportunity to address intra-articular pathology. This article outlines the use of this IONA system for the postoperative evaluation of an osteochondral allograft transplant.
Technique Video
In-office needle arthroscopy for postoperative evaluation of osteochondral allograft transplant. The patient had undergone trochlear transplantation of an allograft from a cadaver. Typically, the postoperative protocol for this procedure is 2 months of non-weight bearing with the use of a continuous passive motion machine. Often, a magnetic resonance imaging scan will be obtained afterward to evaluate healing of the osteochondral autograft transfer system (OATS) transplant. In this case, at the 2-month mark, the patient opted to undergo in-office needle arthroscopy so that the lesion could be visualized. The NanoScope is a tiny, chip-on-tip camera with a console. With the patient in the office, local anesthetic is applied at the locations of the arthroscopic portals. The sharp trocar is placed into the notch of the knee, followed by the NanoScope, in the office by use of the console. The surgeon can see inside the knee. A syringe is attached to the NanoScope and insufflates the knee with saline solution. The scope is in the notch and is then withdrawn; it is subsequently advanced into the suprapatellar pouch with the knee in extension. The NanoScope is again inserted, and insufflation with fluid is performed. One can see the edge of the trochlea; one can also see where the edge of the OATS plug has been placed. It looks as though it has incorporated nicely. The OATS plug itself is well maintained. The trochlear groove edge is observed. Often, fat can interfere with the NanoScope, and therefore, one must perform insufflation with fluid. One can observe what appears to be a well-incorporated edge of the OATS plug, and the cartilage looks well maintained. The surgeon now looks at the inferior and medial border. As can be observed, the medial and superior border is satisfactory. One can see the transition between the plug and native cartilage. The contour is also satisfactory. After the needle arthroscopy, the surgeon suctions out all the fluid from the knee. Then, the incision is simply bandaged and wrapped with gauze and an elastic bandage wrap. The in-office procedure has many benefits because it requires only local anesthetic and therefore the patient can remain awake to see the images in real time. Here the patient and surgeon are reviewing the OATS plug and the contour. As shown, the medial border of the plug has healed and has been well incorporated, which is a favorable result. In addition, minimal to no step-off is present, so there is a smooth transitional border. Being able to perform the evaluation using the NanoScope allows the surgeon to tell the patient that the plug is healed and the weight-bearing and recovery period can begin. The patient is given crutches and is guided out of the office.
Arthroscopy is a minimally invasive procedure that uses a fiberoptic video camera through a small incision to visualize the inside of a joint. It has been a significant advancement in orthopaedics by providing reduced morbidity, quicker recovery times, and diagnostic value.1,2
Humans have an extensive history of using scopes to examine the cavities of the human body. In 1912, Severin Nordentoft of Denmark was accredited with the first intra-articular application of an endoscope to the knee.3 Kenji Takagi, one of the pioneers of arthroscope technology, performed his first arthroscopy in 1918 using a cystoscope to examine the knees of cadavers to visualize the intra-articular effects of tuberculosis.4 Over the next 2 decades, he refined this technology by creating a 3.5-mm arthroscope and using saline solution to distend and better visualize the knee joint.4 Swiss surgeon Eugen Bircher used a Jacobaeus endoscope to confirm preoperative diagnoses before open procedures.5 In 1921, he published the first reports of knee arthroscopy in live patients.5
Further advances in arthroscopy continued after World War II. Masaki Watanabe, whose work was a successor to Takagi’s work, developed arthroscopic models ready for clinical use.6 Previous arthroscopes required the surgeon to view directly through the scope.4 Earlier models also used incandescent bulbs for lighting, which often broke or caused an electrical short circuit.4 Watanabe was the first surgeon to implement a fiberoptic light and cable, reducing the possibility of electrical malfunction.7 He also developed the concept of “triangulation”—the use of secondary portals for instrumentation.7 With these advances, Watanabe performed the first arthroscopic meniscectomy in 1962.7
In subsequent decades, arthroscopy techniques have been refined and scope and implant technologies have advanced, leading to widespread adoption of arthroscopic procedures. In-office needle arthroscopy (IONA) has been available in various iterations for decades.8, 9, 10, 11 Studies have described it as comparable if not superior to magnetic resonance imaging (MRI) for identifying intra-articular pathology; however, it has not yet been adopted as the diagnostic modality of choice.12,13 This article outlines the use of IONA for the postoperative evaluation of an osteochondral allograft transplant (Video 1).
Surgical Technique
Patient Positioning
The patient is positioned supine on an examination bed in a patient room with his or her knees at the edge of the bed and legs hanging freely over the edge (Fig 1). Patient comfort can be achieved with pillows and/or bumps as desired.
Fig 1.
The patient is lying on an in-office examination table and is positioned supine with the legs bilaterally suspended off the edge of the table. The NanoScope and associated tools are prepared sterilely on a Mayo stand a Mayo stand to the patient's left. The display to the patient's right will provide the physician with a live picture of the intra-articular space in the right knee when the NanoScope is inserted.
Preparation
The portal sites and surrounding area are sterilized with a chlorhexidine sponge. Local anesthetic is infiltrated into and posterior to the site for the anterolateral portal to anesthetize the capsule and surrounding area. The procedure is paused for 10 minutes to allow for the local anesthetic to take effect. Further local anesthetic is injected into the joint in preparation for needle arthroscopy.
Establishment of Viewing Portal
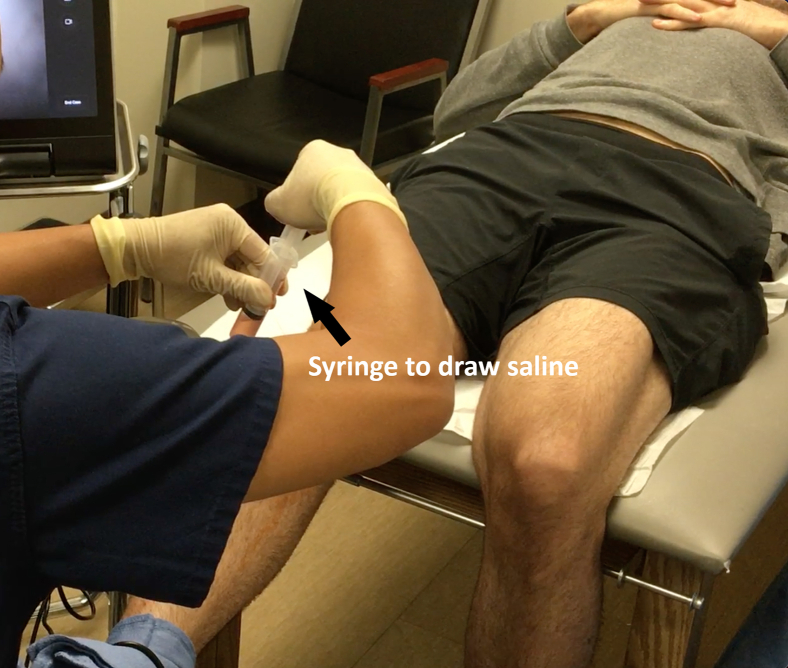
Landmarks including the inferior pole of the patella, patellar tendon, tibial tubercle, and joint lines may be marked on the skin prior to proceeding. The anterolateral portal is established in the standard fashion, lateral to the patellar tendon and above the tibial plateau joint line. A NanoCannula (Arthrex, Naples, FL) and trocar are introduced into the knee joint through the site for the anterolateral portal. The cannula and trocar are aimed toward the intercondylar notch for insertion. The trocar is then removed. Sterile saline solution in a 30-mL syringe is injected into the joint via the cannula (Fig 2) to expand the joint.
Fig 2.
The patient is positioned supine on an in-office examination table with both legs suspended off the table. With the knee supported in extension, the NanoScope is inserted through the anterolateral portal, and saline solution is injected through the cannula of the scope, expanding the joint. As seen through the display, saline solution in the joint allows the physician to properly survey and evaluate the joint surface.
Needle Arthroscopy
A NanoScope (Arthrex) is introduced into the joint through the anterolateral portal with the knee in full extension, and a diagnostic arthroscopy is performed in the standard fashion. The suprapatellar pouch is inspected for loose bodies. The scope is withdrawn slowly to examine the undersurface of the patella and trochlear groove cartilage for degenerative changes and focal chondral defects (Fig 3). The scope is moved laterally and the hand is elevated to visualize the lateral gutter for loose bodies and osteophyte formation. This is repeated with movement of the scope medially to evaluate the medial gutter. At this time, the osteochondral autograft transfer system (OATS) plug, which had been placed in the trochlea of the medial femoral condyle, is visualized and evaluated (Figs 4 and 5). The scope is then brought back into the patellofemoral joint, and the knee is carefully flexed to bring the scope into the intercondylar notch. The lateral compartment is examined for degenerative changes and focal chondral defects. The lateral meniscus is evaluated for tears. The scope is returned to the intercondylar notch. The anterior and posterior cruciate ligaments are visualized and evaluated for pathology. The medial compartment is examined for degenerative changes and focal chondral defects. The medial meniscus is evaluated for tears.
Fig 3.
The patient is positioned supine on the in-office examination table with the right knee supported in extension. With the NanoScope inserted through the anterolateral portal, the suprapatellar pouch is observed (not shown). As the NanoScope is drawn out of the pouch, the patellofemoral joint is evaluated for any chondral defects.
Fig 4.

The patient is positioned supine on the in-office examination table with the right knee supported in extension. With the NanoScope inserted through the anterolateral portal, the medial aspect of the trochlea of the medial femoral condyle is observed. The allograft osteochondral autograft transfer system (OATS) plug is well maintained with no evidence of chondral defects or step-off.
Fig 5.
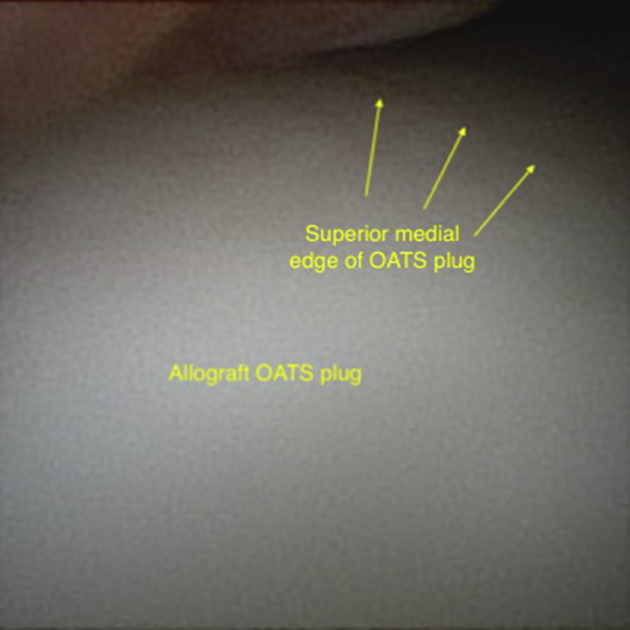
The patient is positioned supine on the in-office examination table with the right knee supported in extension. Through the anterolateral portal, the NanoScope is positioned laterally on the medial femoral condyle to observe the entirety of the allograft osteochondral autograft transfer system (OATS) plug. The OATS plug is well maintained with no evidence of chondral defects.
Accessory Portals and Pathology
If desired, an anteromedial working portal and/or other accessory portals may be created with the use of a Percutaneous Insertion Kit (Arthrex). The site of the working portal and the surrounding area are infiltrated with local anesthetic, and the working portal is sited under needle localization with an 18-gauge spinal needle. This needle is marked with depth lines to estimate the required cannula depth. The stylet from the needle is removed as the needle is kept in place and a nitinol wire is advanced through the needle into the joint. The needle is then removed while the nitinol wire is kept in place. A small incision is made in the skin at the site of the nitinol wire. A NanoCannula is then advanced over the wire with an obturator and secured in place with an adhesive. Small instrumentation can be introduced into the joint through this cannula to address intra-articular pathology.
Post-procedure Protocol
An empty 30-mL syringe is attached to the inflow port of the scope, and the saline solution that was injected into the joint at the start of the procedure is aspirated (Fig 6). This is done to limit post-procedural pain. The scope is then withdrawn from the joint, and the portal or portals are dressed and bandaged. The patient may immediately use the knee as tolerated.
Fig 6.
The patient is positioned supine on an in-office examination table with the legs bilaterally suspended off the table. At this point, the procedure is completed. With the knee supported in extension, the NanoScope is held by an assistant while the physician draws the saline solution through the cannula of the NanoScope.
Discussion
This article details the use of IONA for postoperative evaluation of an osteochondral allograft in the knee. However, the described technique can be applied to the evaluation of other suspected intra-articular pathologies.
The accuracy of MRI compared with the gold standard of arthroscopy for the evaluation of intra-articular pathology has been reported extensively in the literature.14, 15, 16, 17, 18 However, MRI has been found to be less sensitive in evaluating chondral lesions and lateral meniscal injuries.19, 20, 21, 22, 23 Furthermore, MRI may be less effective for postoperative evaluation. Hong et al.24 reported that 93% of surveyed board-certified orthopaedic surgeons believe that there is a problem with the accuracy of MRI in the setting of prior surgery and/or implanted hardware. Studies have shown that higher field strength can improve MRI diagnostic accuracy; however, machines with higher field strength are not widely available, such machines are associated with increased costs, and higher field strength can cause increased artifacts from implanted hardware.25, 26, 27
IONA has significant potential for in-office diagnosis and postoperative evaluation. It has several advantages when compared with conventional arthroscopy. First, it does not require large machines and complex pumps. It can be performed in nontraditional settings such as the office or clinic and in remote areas. The console is battery powered and the instruments are disposable, eliminating the need for postoperative instrument processing. These qualities make the IONA system an ideal candidate for use in remote areas that do not have the infrastructure and/or resources to operate an MRI machine. Additionally, unlike MRI, simpler encountered pathologies such as meniscal tears may be addressed at the time of IONA via use of an accessory portal. However, IONA is limited in scope to intra-articular pathology. Furthermore, IONA in deeper joints such as the shoulder and hip may be challenging. The benefits and drawbacks of IONA are listed in Table 1.
Table 1.
Benefits and Drawbacks of In-Office Needle Arthroscopy Using NanoScope System
| Benefits |
| Immediate evaluation of joint |
| Interactive involvement with patient |
| Smaller portals |
| Avoidance of general anesthesia |
| Immediate postoperative mobilization |
| Decreased pain and edema |
| Avoidance of multiple office visits |
| Ability to navigate smaller spaces |
| Avoidance of excessive use of saline solution |
| Avoidance of expensive OR time |
| Elimination of need for post-procedure processing owing to disposable instruments |
| Drawbacks |
| Inability to evaluate extra-articular and periarticular soft tissue |
| Environmental concerns of disposable components |
| Lacking variability in scope |
| Inability to alter intraoperative blood pressure |
| Limited joint manipulation |
| Inability to alter degree of joint distension |
| Adequate visualization can be more technically challenging |
| Cost not significantly different from MRI |
MRI, magnetic resonance imaging; OR, operating room.
Several studies have compared the effectiveness of IONA versus MRI. In their 2018 clinical trial of 110 patients with knee pain, Gill et al.12 reported that the accuracy, sensitivity, and specificity of IONA were equivalent to those of surgical diagnostic arthroscopy and that IONA was more accurate than MRI with no associated complications. One limitation of their study was that the needle arthroscopy was performed in the operating room immediately preceding a standard diagnostic arthroscopy, thereby not simulating an in-office setup.
A 2019 systematic review examining IONA conducted by Zhang et al.13 assessed 404 patients across 11 publications. IONA was found to have superior sensitivity and specificity to MRI in the evaluation of knee osteoarthritis, ligament insufficiency, and meniscal tears. IONA was comparable or inferior to MRI in diagnosing osteochondral lesions and rotator cuff tears; however, the authors noted the paucity of data on IONA in joints other than the knee.
Several studies performing cost-effectiveness analyses on IONA versus MRI have been published. Using 2013 Medicare reimbursement data, Voigt et al.28 calculated cost savings between $115 million and $177 million per year when replacing MRI with IONA. McMillan et al.29 performed a retrospective review of 200 patients and calculated minimum savings of $418 and $554 per non-contrast knee scan and shoulder scan, respectively, increasing to $961 and $1,097, respectively, in hospital facilities. In a 2019 cost-effectiveness analysis of IONA versus MRI in the diagnosis and treatment of meniscal tears, Amin et al.30 observed significant cost savings with no difference in patient outcomes as measured by the global Knee Injury and Osteoarthritis Outcome Score (KOOS). Most recently, a 2021 cost-effective analysis of IONA versus MRI showed that IONA was more cost-effective, saving between $7,852 and $11,227 per operative patient.31 Whereas these studies have broadly examined the cost-effectiveness of IONA compared with MRI, the current NanoScope system console costs $24,999 and each disposable handpiece costs $659. Further studies are required to determine the true cost savings per patient. It is possible that widespread adoption of this technology will bring costs below those of MRI as production increases.
From an international health perspective, as life spans continue to extend in the developing world, there has been an epidemiologic shift toward chronic and degenerative diseases. Musculoskeletal disorders are included among the primary drivers of the global increase in years lived with disability.32 MRI is often the diagnostic test of choice in the developed world. The global estimated median number of MRI machines per population is 0.12 per 100,000.33 The concentration is greatest in the Western Pacific region, with Japan offering 5.52 units per 100,000—the most in the world.33,34 The United States is second, with 3.91 units per 100,000, followed closely by Italy, Germany, and the Republic of Korea.34 By region, the Western Pacific region shows the highest MRI unit density, at 2.03 per 100,000, followed by the European region (0.67), region of the Americas (0.24), and African region (0.01).35 The figure for the region of the Americas is artificially deflated because US data are not included. This illustrated disparity in MRI availability between high- and low-income countries or regions could be addressed by IONA. IONA could potentially be offered as a portable, low-cost alternative to MRI to patients in austere environments or those with equivocal MRI findings who prefer to avoid general anesthesia to evaluate intra-articular pathology.
Most recently, the literature has explored new potential uses of IONA. A recent study by Peters et al.36 showed favorable results using IONA for elbow arthroscopy. In another recent study, Dankert et al.37 detailed the use of IONA for removal of loose bodies in the ankle joint that were not identifiable by MRI. IONA has also been used for in-office biceps tenotomy, as detailed in a recent study by Gauci et al.38 In a prospective study of patients undergoing IONA for the treatment of anterior ankle impingement, Colasanti et al.39 reported significant pain reduction, low complication rates, excellent patient-reported outcomes, and high patient satisfaction with the procedure. Patients reported a willingness to undergo the same procedure and believed that seeing the procedure in real time helped with their understanding of the underlying pathology. These recent studies have demonstrated the potential for using IONA in more complicated arthroscopic procedures, and this should continue to be explored. There is a need for larger-scale studies to be performed to evaluate the efficacy and safety of IONA and to reveal the most appropriate diagnoses and patient populations for its use.40
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.L.C. receives personal fees from Arthrex for lectures and educational material, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
In-office needle arthroscopy for postoperative evaluation of osteochondral allograft transplant. The patient had undergone trochlear transplantation of an allograft from a cadaver. Typically, the postoperative protocol for this procedure is 2 months of non-weight bearing with the use of a continuous passive motion machine. Often, a magnetic resonance imaging scan will be obtained afterward to evaluate healing of the osteochondral autograft transfer system (OATS) transplant. In this case, at the 2-month mark, the patient opted to undergo in-office needle arthroscopy so that the lesion could be visualized. The NanoScope is a tiny, chip-on-tip camera with a console. With the patient in the office, local anesthetic is applied at the locations of the arthroscopic portals. The sharp trocar is placed into the notch of the knee, followed by the NanoScope, in the office by use of the console. The surgeon can see inside the knee. A syringe is attached to the NanoScope and insufflates the knee with saline solution. The scope is in the notch and is then withdrawn; it is subsequently advanced into the suprapatellar pouch with the knee in extension. The NanoScope is again inserted, and insufflation with fluid is performed. One can see the edge of the trochlea; one can also see where the edge of the OATS plug has been placed. It looks as though it has incorporated nicely. The OATS plug itself is well maintained. The trochlear groove edge is observed. Often, fat can interfere with the NanoScope, and therefore, one must perform insufflation with fluid. One can observe what appears to be a well-incorporated edge of the OATS plug, and the cartilage looks well maintained. The surgeon now looks at the inferior and medial border. As can be observed, the medial and superior border is satisfactory. One can see the transition between the plug and native cartilage. The contour is also satisfactory. After the needle arthroscopy, the surgeon suctions out all the fluid from the knee. Then, the incision is simply bandaged and wrapped with gauze and an elastic bandage wrap. The in-office procedure has many benefits because it requires only local anesthetic and therefore the patient can remain awake to see the images in real time. Here the patient and surgeon are reviewing the OATS plug and the contour. As shown, the medial border of the plug has healed and has been well incorporated, which is a favorable result. In addition, minimal to no step-off is present, so there is a smooth transitional border. Being able to perform the evaluation using the NanoScope allows the surgeon to tell the patient that the plug is healed and the weight-bearing and recovery period can begin. The patient is given crutches and is guided out of the office.
References
- 1.Faour M., Sultan A.A., George J., et al. Arthroscopic irrigation and debridement is associated with favourable short-term outcomes vs. open management: An ACS-NSQIP database analysis. Knee Surg Sports Traumatol Arthrosc. 2019;27:3304–3310. doi: 10.1007/s00167-018-5328-1. [DOI] [PubMed] [Google Scholar]
- 2.Day M., Westermann R., Duchman K., et al. Comparison of short-term complications after rotator cuff repair: Open versus arthroscopic. Arthroscopy. 2018;24:1130–1136. doi: 10.1016/j.arthro.2017.10.027. [DOI] [PubMed] [Google Scholar]
- 3.Kieser C.W., Jackson R.W. Severin Nordentoft: The first arthroscopist. Arthroscopy. 2001;17:532–535. doi: 10.1053/jars.2001.24058. [DOI] [PubMed] [Google Scholar]
- 4.Watanabe M., Bechtol R.C., Nottage W.M. In: O’Connor’s textbook of arthroscopic surgery. Shahriaree H., editor. JB Lippincott; Philadelphia: 1992. History of arthroscopic surgery; pp. 1–6. [Google Scholar]
- 5.Bircher E. Die Arthroendoskopie. Zentralbl Chir. 1921;48:1460. [in German] [Google Scholar]
- 6.Watanabe M., Takeda S., Hiroshi I. Atlas of arthroscopy. Ed 3. Igaku-Shoin; Tokyo: 1979. History of arthroscopy; pp. 1–11. [Google Scholar]
- 7.DeMaio M. Giants of orthopaedic surgery: Masaki Watanabe. Clin Orthop Relat Res. 2013;471:2443–2448. doi: 10.1007/s11999-013-3052-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wallace D.A., Carr A.J., Loach A.B., et al. Day case arthroscopy under local anaesthesia. Ann R Coll Surg Engl. 1994;76:330–331. [PMC free article] [PubMed] [Google Scholar]
- 9.Fairclough J.A., Graham G.P., Pemberton D. Local or general anaesthetic in day case arthroscopy? Ann R Coll Surg Engl. 1990;72:104–107. [PMC free article] [PubMed] [Google Scholar]
- 10.Halbrecht J.L., Jackson D.W. Office arthroscopy: A diagnostic alternative. Arthroscopy. 1992;8:320–326. doi: 10.1016/0749-8063(92)90062-g. [DOI] [PubMed] [Google Scholar]
- 11.Cooper D.E. Editorial Commentary: The desire to take a look: Surgeons and patients must weigh the benefits and costs of in-office needle arthroscopy versus magnetic resonance imaging. Arthroscopy. 2018;34:2436–2437. doi: 10.1016/j.arthro.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Gill T.J., Safran M., Mandelbaum B., et al. A prospective, blinded, multicenter clinical trial to compare the efficacy, accuracy, and safety of in-office diagnostic arthroscopy with magnetic resonance imaging and surgical diagnostic arthroscopy. Arthroscopy. 2018;34:2429–2435. doi: 10.1016/j.arthro.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Zhang K., Crum R.J., Samuelsson K., et al. In-office needle arthroscopy: A systematic review of indications and clinical utility. Arthroscopy. 2019;35:2709–2721. doi: 10.1016/j.arthro.2019.03.045. [DOI] [PubMed] [Google Scholar]
- 14.Li K., Du J., Huang L.X., et al. The diagnostic accuracy of magnetic resonance imaging for anterior cruciate ligament injury in comparison to arthroscopy: A meta-analysis. Sci Rep. 2017;7:7583. doi: 10.1038/s41598-017-08133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Phelan N., Rowland P., Galvin R., O’Byrne J.M. A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee Surg Sports Traumatol Arthrosc. 2016;24:1525–1539. doi: 10.1007/s00167-015-3861-8. [DOI] [PubMed] [Google Scholar]
- 16.Wuennemann F., Kintzelé L., Zeifang F., et al. Diagnostic performance of 3D-multi-Echo-data-image-combination (MEDIC) for evaluating SLAP lesions of the shoulder. BMC Musculoskelet Disord. 2019;20:598. doi: 10.1186/s12891-019-2986-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madell J.C., Rhodes J.A., Shah N., et al. Routine clinical knee MR reports: Comparison of diagnostic performance at 1.5 T and 3.0 T for assessment of the articular cartilage. Skeletal Radiol. 2017;46:1487–1498. doi: 10.1007/s00256-017-2714-6. [DOI] [PubMed] [Google Scholar]
- 18.Marinetti A., Tessarolo F., Ventura L., et al. Morphological MRI of knee cartilage: Repeatability and reproducibility of damage evaluation and correlation with gross pathology examination. Eur Radiol. 2020;30:3226–3235. doi: 10.1007/s00330-019-06627-5. [DOI] [PubMed] [Google Scholar]
- 19.Lee G.Y., Kim S., Baek S.H., et al. Accuracy of magnetic resonance imaging and computed tomography in diagnosing acetabular labral tears and chondral lesions. Clin Orthop Surg. 2019;11:21–27. doi: 10.4055/cios.2019.11.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Orlando Júnior N., de Souza Leão M.G., de Oliveira N.H.C. Diagnosis of knee injuries: Comparison of the physical examination and magnetic resonance imaging with the findings from arthroscopy. Rev Bras Ortop. 2015;50:712–719. doi: 10.1016/j.rboe.2015.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Danieli M.V., Guerreiro J.P., Ad Q., et al. Diagnosis and classification of chondral knee injuries: Comparison between imaging and arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2016;24:1627–1633. doi: 10.1007/s00167-015-3622-8. [DOI] [PubMed] [Google Scholar]
- 22.Krych A.J., Wu I.T., Desai V.S., et al. High rate of missed lateral meniscus posterior root tears on preoperative magnetic resonance imaging. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118765722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Massimiliano L., Giuseppe G., Michela B., et al. Role of low field MRI in detecting knee lesions. Acta Biomed. 2019;90(suppl 1):116–122. doi: 10.23750/abm.v90i1-S.7977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hong A., Liu J.N., Gowd A.K., et al. Reliability and accuracy of MRI in orthopedics: A survey of its use and perceived limitations. Clin Med Insights Arthritis Musculoskelet Disord. 2019;12 doi: 10.1177/1179544119872972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheng Q., Zhao F.C. Comparison of 1.5- and 3.0-T magnetic resonance imaging for evaluating lesions of the knee. Medicine (Baltimore) 2018;97 doi: 10.1097/MD.0000000000012401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nouri N., Bouaziz M.C., Riahi H., et al. Traumatic meniscus and cruciate ligament tears in young patients: A comparison of 3T versus 1.5T MRI. J Belg Soc Radiol. 2017;101:14. doi: 10.5334/jbr-btr.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Juras V., Mlynarik V., Szomolanyi P., et al. Magnetic resonance imaging of the musculoskeletal system at 7T. Top Magn Reson Imaging. 2019;28:125–135. doi: 10.1097/RMR.0000000000000205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Voigt J.D., Mosier M., Huber B. Diagnostic needle arthroscopy and the economics of improved diagnostic accuracy: A cost analysis. Appl Health Econ Health Policy. 2014;12:523–535. doi: 10.1007/s40258-014-0109-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McMillan S., Schwartz M., Jennings B., et al. In-office diagnostic needle arthroscopy: Understanding the potential value for the US healthcare system. Am J Orthop. 2017;46:252–256. [PubMed] [Google Scholar]
- 30.Amin N., McIntyre L., Carter T., et al. Cost-effectiveness analysis of needle arthroscopy versus magnetic resonance imaging in the diagnosis and treatment of meniscal tears of the knee. Arthroscopy. 2019;35:554–562. doi: 10.1016/j.arthro.2018.09.030. e13. [DOI] [PubMed] [Google Scholar]
- 31.Liu J., Farr J., Ramos O., Voigt J., Amin N. Workers’ societal costs after knee and shoulder injuries and diagnosis with in-office arthroscopy or delayed MRI: A cost-minimization analysis. JB JS Open Access. 2021;6 doi: 10.2106/JBJS.OA.20.00151. e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vos T., Barber R.M., Bell B., et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: A systemic analysis for the global burden of disease study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization and Multiple Sclerosis International Federation . World Health Organization; Geneva: 2008. Atlas: Multiple sclerosis resources in the world 2008. [Google Scholar]
- 34.Organisation for Economic Cooperation and Development. Magnetic resonance imaging (MRI) units. 10.1787/1a72e7d1-en. Published 2020. Accessed March 18, 2020. [DOI]
- 35.World Health Organization . World Health Organization; Geneva: 2017. Global atlas of medical devices—WHO medical devices technical series. [Google Scholar]
- 36.Peters M., Gilmer B., Kassam H.F. Diagnostic and therapeutic elbow arthroscopy using small-bore needle arthroscopy. Arthrosc Tech. 2020;9:e1703–e1708. doi: 10.1016/j.eats.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dankert J.F., Shimozono Y., Williamson E.R.C., Kennedy J.G. Application of nano arthroscopy in the office setting for the removal of an intra-articular loose osseous body not identified by magnetic resonance imaging: A case report. Foot Ankle Surg Tech Rep Cases. 2021;1 [Google Scholar]
- 38.Gauci M.O., Monin B., Rudel A., Blasco L., Bige B., Boileau P. In-office biceps tenotomy with needle arthroscopy: A feasibility study. Arthrosc Tech. 2021;10:e1263–e1268. doi: 10.1016/j.eats.2021.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Colasanti C.A., Mercer N.P., Garcia J.V., Kerkhoffs G.M.M.J., Kennedy J.G. In-office needle arthroscopy for the treatment of anterior ankle impingement yields high patient satisfaction with high rates of return to work and sport. Arthroscopy. 2022;38:1302–1311. doi: 10.1016/j.arthro.2021.09.016. [DOI] [PubMed] [Google Scholar]
- 40.Lavender C. Editorial Commentary: Indications for needle arthroscopy as an alternative to magnetic resonance imaging: More to the picture than meets the eye. Arthroscopy. 2021;37:2099–2101. doi: 10.1016/j.arthro.2021.04.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
In-office needle arthroscopy for postoperative evaluation of osteochondral allograft transplant. The patient had undergone trochlear transplantation of an allograft from a cadaver. Typically, the postoperative protocol for this procedure is 2 months of non-weight bearing with the use of a continuous passive motion machine. Often, a magnetic resonance imaging scan will be obtained afterward to evaluate healing of the osteochondral autograft transfer system (OATS) transplant. In this case, at the 2-month mark, the patient opted to undergo in-office needle arthroscopy so that the lesion could be visualized. The NanoScope is a tiny, chip-on-tip camera with a console. With the patient in the office, local anesthetic is applied at the locations of the arthroscopic portals. The sharp trocar is placed into the notch of the knee, followed by the NanoScope, in the office by use of the console. The surgeon can see inside the knee. A syringe is attached to the NanoScope and insufflates the knee with saline solution. The scope is in the notch and is then withdrawn; it is subsequently advanced into the suprapatellar pouch with the knee in extension. The NanoScope is again inserted, and insufflation with fluid is performed. One can see the edge of the trochlea; one can also see where the edge of the OATS plug has been placed. It looks as though it has incorporated nicely. The OATS plug itself is well maintained. The trochlear groove edge is observed. Often, fat can interfere with the NanoScope, and therefore, one must perform insufflation with fluid. One can observe what appears to be a well-incorporated edge of the OATS plug, and the cartilage looks well maintained. The surgeon now looks at the inferior and medial border. As can be observed, the medial and superior border is satisfactory. One can see the transition between the plug and native cartilage. The contour is also satisfactory. After the needle arthroscopy, the surgeon suctions out all the fluid from the knee. Then, the incision is simply bandaged and wrapped with gauze and an elastic bandage wrap. The in-office procedure has many benefits because it requires only local anesthetic and therefore the patient can remain awake to see the images in real time. Here the patient and surgeon are reviewing the OATS plug and the contour. As shown, the medial border of the plug has healed and has been well incorporated, which is a favorable result. In addition, minimal to no step-off is present, so there is a smooth transitional border. Being able to perform the evaluation using the NanoScope allows the surgeon to tell the patient that the plug is healed and the weight-bearing and recovery period can begin. The patient is given crutches and is guided out of the office.
In-office needle arthroscopy for postoperative evaluation of osteochondral allograft transplant. The patient had undergone trochlear transplantation of an allograft from a cadaver. Typically, the postoperative protocol for this procedure is 2 months of non-weight bearing with the use of a continuous passive motion machine. Often, a magnetic resonance imaging scan will be obtained afterward to evaluate healing of the osteochondral autograft transfer system (OATS) transplant. In this case, at the 2-month mark, the patient opted to undergo in-office needle arthroscopy so that the lesion could be visualized. The NanoScope is a tiny, chip-on-tip camera with a console. With the patient in the office, local anesthetic is applied at the locations of the arthroscopic portals. The sharp trocar is placed into the notch of the knee, followed by the NanoScope, in the office by use of the console. The surgeon can see inside the knee. A syringe is attached to the NanoScope and insufflates the knee with saline solution. The scope is in the notch and is then withdrawn; it is subsequently advanced into the suprapatellar pouch with the knee in extension. The NanoScope is again inserted, and insufflation with fluid is performed. One can see the edge of the trochlea; one can also see where the edge of the OATS plug has been placed. It looks as though it has incorporated nicely. The OATS plug itself is well maintained. The trochlear groove edge is observed. Often, fat can interfere with the NanoScope, and therefore, one must perform insufflation with fluid. One can observe what appears to be a well-incorporated edge of the OATS plug, and the cartilage looks well maintained. The surgeon now looks at the inferior and medial border. As can be observed, the medial and superior border is satisfactory. One can see the transition between the plug and native cartilage. The contour is also satisfactory. After the needle arthroscopy, the surgeon suctions out all the fluid from the knee. Then, the incision is simply bandaged and wrapped with gauze and an elastic bandage wrap. The in-office procedure has many benefits because it requires only local anesthetic and therefore the patient can remain awake to see the images in real time. Here the patient and surgeon are reviewing the OATS plug and the contour. As shown, the medial border of the plug has healed and has been well incorporated, which is a favorable result. In addition, minimal to no step-off is present, so there is a smooth transitional border. Being able to perform the evaluation using the NanoScope allows the surgeon to tell the patient that the plug is healed and the weight-bearing and recovery period can begin. The patient is given crutches and is guided out of the office.