Abstract
The valgus deformity in the tibia requires correction because it places increased pressure on the lateral compartment of the knee, intensifying the degenerative process. Correction strategies are diverse and depend on patient profile, age, and soft-tissue conditions as well as the orthopaedic surgeon’s experience with different surgical materials. Deformity size and location are the primary factors contributing to material and shape choice, whether gradual or acute. The only gradual correction approach involves the use of a monolateral or circular external fixator. This is the only indication for correction in cases of excellent deformity, soft-tissue involvement, and a history of bone infection. This study aimed to present a gradual correction technique for tibial valgus deformity using a monolateral external fixator as well as its postoperative follow-up. This technique has the advantages of greater patient acceptance, lighter assembly, and briefer distraction owing to the use of a single piece as well as the ability of the operated limb to bear a load the day after the surgical procedure and dynamic outpatient follow-up.
Technique Video
Here, we present a 3-dimensional animation of a case of left tibial valgus deformity. With the patient in the supine position, the first step is to mark the apex of the deformity, that is, where the local hinge must be created. The hinge is created using a Kirchner wire or drill. Next, we choose a T-clamp, bar clamp, or straight clamp. On the proximal portion of the tibia, the drill is placed 4.8 mm inside the drill guide in contact with the anterolateral cortex of the tibia, the position through which the pin will be inserted parallel to the articular surface of the tibial plateau, about 2 cm below this surface. The pin is then placed using a T-key. The next step is positioning the top of the more distal pin parallel to the surface of the ankle. One pin is placed distally while the other is placed proximally. In each portion, the pin must be parallel, and that on the distal portion will be visible on the coronal plane. On the proximal portion of the tibia, if a T-clamp is used, it will be visible on the axial rather than coronal plane. An osteotomy of the tibia is then performed with a drill 4.8 mm from the anterolateral cortex of the tibia. The medial cortex must remain intact. A complete osteotomy of the fibula is made 10 cm proximal to the lateral malleolus. The L-key is used to perform the distraction by the distractor and the positioned is checked by direct visualization of the focus and under floroscopy.
In a real case of a female patient with post-traumatic valgus, the first step is to mark the apex of the deformity by fluoroscopy. At this moment, we chose clamps. We then proceeded to drill proximally for pin placement. After the first pin, we placed the more distal pin and completed it with one proximal pin and one more distal pin. Under fluoroscopy, the apex of the deformity was marked, and the anterolateral cortex of the tibia is made partially. This was followed by an osteotomy of the fibula.
Alignment of the axis of the lower limbs is important to ensure parallelism between the joint lines; therefore, in an orthostatic position, with a load upon the lower limbs, the axial force exerted by the patient’s weight is distributed uniformly across the joints, thereby optimizing the biomechanics of these limbs.1,2
The articular cartilage degeneration process is associated with different factors, such as age, obesity, mechanical changes, or inflammatory and/or rheumatologic diseases.3 Deformities in the long bones consequently lead to changes to the joints that facilitate locomotion, altering the distribution of forces across the joint compartments and generating arthrosis.3, 4, 5
Panoramic radiography of the lower limbs allows joint angle measurements, which involve crossing of the axes, mechanical or anatomical, with the respective joint orientation lines.6,7 The knee joint is functionally divided into compartments: medial, comprising the medial femoral condyle and medial plateau; lateral, comprising the lateral femoral condyle and lateral plateau; and anterior, formed by the patella in relation to the femoral trochlea. The nonconformity of the distribution of loads by the appropriate joint areas leads to overload and cartilage alteration.1, 2, 3, 4, 5, 6, 7, 8 When varus deviation occurs, overload of the medial compartment of the knee develops, and, in the case of valgus deviation, the lateral compartment. Such axis alterations may have a congenital, post-traumatic, postoperative, tumoral, or idiopathic etiology.,9, 10, 11, 12
Correction of the deformity with consequent restoration of the mechanical axis can be achieved using a plate-and-screw system, external fixator, locked intramedullary nail, hemiepiphysiodesis with a cannulated screw (in pediatric cases), or even primary unicompartmental or total knee arthroplasty; these techniques are limited by the deformity magnitude, surrounding soft tissue, and patients’ social conditions in addition to the surgeon’s experience and need for specificity.11,13
Acute correction has the advantage of being a single surgery, but there is a risk of fracture of the opposite cortex, hypercorrection, infection, or pseudarthrosis of the osteotomy focus.14, 15, 16, 17, 18, 19, 20 When gradual correction is performed using a monolateral external fixator, the advantages include smaller surgical access site, partial osteotomy resulting in less postoperative pain, and the possibility of dynamic correction to avoid hypo- or hypercorrection.21
Assembly using a monolateral external fixator with gradual correction has the advantage of usability when other techniques are contraindicated, in addition to being lighter and easier for the patient to correct compared with the circular fixator.
Here, we describe a surgical technique using a monolateral external fixator that uses gradual correction of post-traumatic valgus tibial deformity with minimally invasive incisions and rapid return to load bearing of the operated limb.
Surgical Technique (With Video Illustration)
Positioning, Preparation, and Evaluation Under Anesthesia
After benig anesthetized, the patient is positioned in a supine position with the operated limb positioned at the distal region of the radiotransparent operating table (Table 1).
Table 1.
Step-by-Step Surgical Procedure
| Step | Description |
|---|---|
| 1 | The patient is anesthetized and positioned supine. |
| 2 | The apex of the deformity is marked using Kirchner wire to indicate the correct point of the hinge of the external fastener. |
| 3 | The distances of this apex are checked so that the appropriate clamps (straight, bar, or T) are chosen. |
| 4 | Under fluoroscopic guidance, the drill is placed 4.8 mm inside the drill guide in contact with the anterolateral cortex of the tibia to create the first channel through which the pin will be inserted parallel to the articular surface of the tibial plateau approximately 2 cm below this surface. A 6.0-mm conical external fixator pin is placed using the T-key until the second cortex is ironed. |
| 5 | Distally, the lower pin is placed, thus delimiting the size of the device in relation to the tibia and the point of the fixator hinge being exactly at the apex of the deformity. |
| 6 | One or two more pins are placed proximally and distally. |
| 7 | With the aid of fluoroscopy, the center of the tibia deformity is marked, with anterior access of approximately 5 cm being performed. With the visualization of the tibia, a partial osteotomy is performed of the tibia, leaving the area intact from the crest of the tibia to the medial cortex will function as a hinge. |
| 8 | Access to the fibula is performed 10 cm from the lateral maleollus and an osteotomy of the fibula is performed to prevent an impediment in the distraction of the tibia. |
| 9 | The self-centering switch is added to the self-centering body, which is responsible for the distraction of the external fastener. The L-key is used to perform the distraction by the distractor, and its results are checked by direct visualization of the focus and fluoroscopy. |
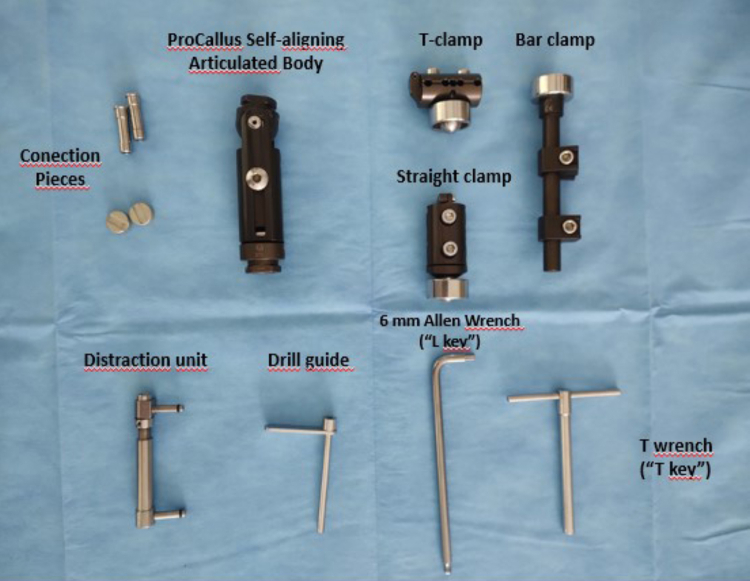
Asepsis, antisepsis, and surgical field placement are performed (Video 1). All individual parts of the ProCallus Fixator (Orthofix Medical, Verona, Italy) necessary to create the correct assembly must be separated (Fig 1).
Fig 1.
ProCallus Fixator Orthofix pieces (Orthofix, Verona, Italy).
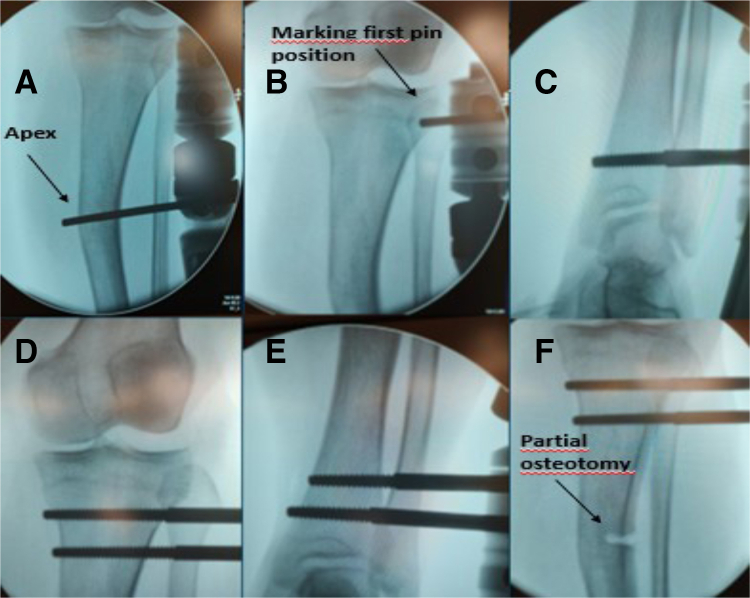
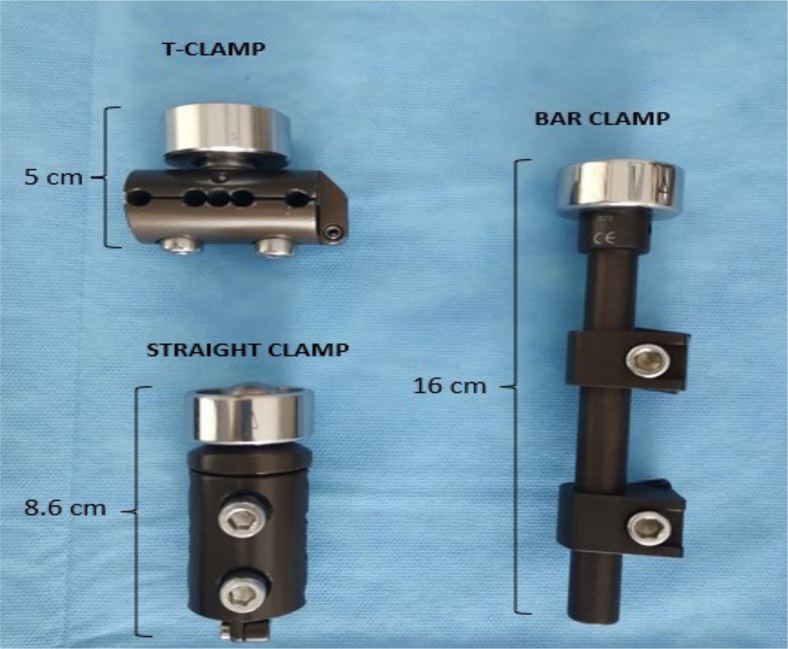
Using fluoroscopic guidance, the apex of the deformity is marked with a Kirchner wire to indicate the correct point of the hinge of the external fastener (Fig 2A). The distances of this apex to the tibial plateau and ankle articular line are compared with the clamp sizes to determine the best choice (straight, bar, or T) (Fig 3).
Fig 2.
Fluoroscopy. (A) Marking the apex of the deformity. (B) Marking of the pin entry point in the proximal tibia. (C) More distal pin in the tibia. (D) Positioning of the proximal pins. (E) Positioning of the distal pins. (F) Partial osteotomy at the apex of the deformity.
Fig 3.
ProCallus Orthofix clamps.
Surgical Intervention
The surgical area is accessed using a scalpel of approximately 1 cm in the anterolateral space of the proximal portion of the tibia. Thus, divulsionation of the muscular and subcutaneous planes is performed with Metzenbaum scissors. Under intraoperative fluoroscopic guidance, the drill is placed 4.8 mm inside the drill guide in contact with the anterolateral cortex of the tibia and performs the first pertuite, through which the pin is inserted parallel to the articular surface of the tibial plateaus approximately 2 cm below this surface (Fig 2B); a 6.0-mm conical external fixator pin is placed using the T-key until the second cortex is ironed.
Next, a monolateral external fastener with a telescopic self-aligning body and previously defined clamps is assembled. The chosen clamp is placed on the proximal pin and the screws are temporarily tightened. Distally, the lower pin is placed, thus delimiting the device size in relation to the tibia and the point of the fixator hinge being exactly at the apex of the deformity (Fig 2C). One more pin is placed proximally and distally (Fig 2 D and E).
Osteotomies
Under fluoroscopic guidance, the center of the tibial deformity is marked with an anterior access of approximately 5 cm. The subcutaneous and muscular planes are divulsionated and separated using 2 Hohmann-type retractors. Under visualization of the tibia, a partial osteotomy is performed, leaving it intact from the crest of the tibia to the medial cortex, which functions as a hinge (Fig 2G).
Access to the fibula is made 10 cm from the lateral maleollus while an osteotomy of the fibula is performed with a 4.8-mm drill to prevent an impediment in the distraction of the tibia.
Opening the Osteotomies
A self-centering switch is added to the self-centring body, which is responsible for the distraction of the external fastener. An L-key is used to perform the distraction by approximately 1 cm, which is then checked by direct visualization of the focus and under fluoroscopy. Hemostasis is reviewed and both surgical sites are closed using nylon 2.0 wire. At the end of the procedure, postoperative control radiography is performed (Fig 4 A-C).
Fig 4.
(A) Panoramic radiograph demonstrating the valgus deformity of the tibia. (B) Preoperative radiograph of the anteroposterior aspect of the tibia. (C) Postoperative radiograph of the anteroposterior aspect of the tibia.
Postoperative Orientation and Rehabilitation
On the first postoperative day, each patient is encouraged to walk with the aid of crutches, and placing a load upon the operated limb is necessary to stimulate bone consolidation and enable the return to daily activities. The total length of hospital stay is usually 3 days.
Each participant returns at 14 days postoperatively to receive an L key of the same model used during surgery and is taught how to distract the device (a quarter turn every 6 hours). Distraction begins at 1 mm/day (0.25 mm each quarter of the distractor’s turn every 6 hours using the Ilizarov concept) and can be changed according to outpatient follow-up; if new bone is seen on the tibial osteotomy on new radiographs, distraction is maintained at 0.25 mm/day; if not, the rate is slowed to a quarter turn every 8 hours.
The patient should return weekly for updated radiography of the leg, and a full load should be placed on the operated limb without the aid of crutches. The weekly evaluation considers ectoscopy of the limbs, the radiologic pattern of correction, and bone formation at the osteotomy site as well as the skin conditions and hygiene of the device and reinforcement of the correct way to perform the distraction.
If satisfactory clinical correction is achieved and radiologically confirmed by the correction of proximal and distal joint angles on leg radiography at anteroposterior incidence, the distraction is paused. The consolidation phase of the regenerated material is initiated. In contrast, if hypercorrection occurred, leading to varus deformity of the tibia, it is possible to compress the distractor to the correction position of the angle on new radiographs.
Discussion
Use of the monolateral external fixator with the technique presented here features minimally invasive surgical access, minor assembly (less physical effort for the patient to walk, easier cleaning, and fewer transfixing structures), and partial osteotomy, leading to better patient acceptance, less postoperative pain, encouragement to return to daily activities, and fewer postoperative complications.22
Depending on the deviation of the mechanical axis in the frontal plane, overload of the medial or lateral compartment can occur that requires surgical correction, even at the same surgical time in conjunction with ligament or meniscal correction.23 The lateral opening osteotomy in the proximal tibia using a plate and screw presents some points of technical difficulty. Collins et al.24 reported 24 osteotomies (23 patients) as a safe and effective method. However, 38% of patients required a surgical procedure after lateral opening osteotomy in the proximal region of the tibia due to complications of the synthesis material, postoperative stiffness, or other complications, and 10% were considered cases of early failure requiring total knee arthroplasty.
Marti et al.25 reported on 34 patients in whom the complication rate was low compared with the long-term benefit, with 9% experiencing transient fibular nerve palsy, one developing superficial infection of the surgical site, and one developing thrombophlebitis. Mirouse et al.26 reported follow-up of at least 1 year in 19 patients, detailing that the rate of early failure requiring total knee arthroplasty of 50% of cases when the deformity was less than 10°. Rozbruch et al.27 demonstrated correcting tibial deformities using blocked intramedullary nails with or without stretching; however, correction in the proximal third was limited because of proximity to the blockade and geometry of the tibial medullary canal. Fragomen et al.28 showed that the tibia has the potential for slower consolidation and regeneration than the femur when associated with deformity correction with stretching in addition to neurolysis of the prophylactic fibular nerve in cases of valgus deformity.
A circular external fixator also can be used to correct tibial deformity. Rozbruch et al.27 published the results of 102 patients with at least 10° deformities of the tibia using a Taylor spatial frame. This type of fixator requires specific software, and the patient must rotate 6 rods for correction and manage pins and wires that are fixed to the skin. Complications included cellulitis requiring venous antibiotic therapy, peroneal nerve palsy, pseudarthrosis of the osteotomy site, and undercorrection; moreover, most patients developed a pin tract infection that resolved with oral antibiotic therapy.29 Horn et al.30 presented similar results of correction of the distal third of the tibia with the same model of fixator in 54 patients, reporting a pin path infection in 27 patients, cellulitis requiring venous antibiotic therapy in 4 patients, pseudarthrosis of the osteotomy focus in 1 patient, and the need for analgesics in 3 patients. Another 3 patients progressed to ankle arthrodesis because of persistent pain.30
Total knee arthroplasty is part of the deformity correction arsenal; however, compared with other methods, it involves more significant limitations due to patient profile and age as well as deformity magnitude and location.31 Thus, surgeons must carefully perform soft-tissue balancing because valgus deformity leads to increased ligament laxity in the lateral compartment.21
The technique presented here has limitations inherent to the use of the external fixator, such as discomfort and nonacceptance of its use by some patients, the frequent occurrence of infection in the pin path, and the need for 2 surgical procedures, including removal of the external fixator assembly.
This technique’s advantages are also encouraging. Table 2 lists the advantages, disadvantages, risks, and tips. This technique introduces the possibility of dynamic and gradual deformity correction. In cases of hypercorrection in the outpatient clinic, it is possible to compress the distractor to return it to the ideal position. Another advantage is the lighter assembly and easier mobilization by patients to enable local hygiene. Moreover, postoperative pain may be lower due to the partial osteotomy.
Table 2.
Technical Advantages, Disadvantages, Risks, and Tips
| Advantages | Disadvantages | Risks | Tips |
|---|---|---|---|
| Lighter assembly than circular fastener | Need for patient commitment to distraction | Inaccurate distraction can lead to consolidation or a lack of regeneration | If the osteotomy is consolidated, perform a new osteotomy. Compress the osteotomy and restart the distraction if the tissue does not regenerate due to distraction error. |
| Significant deformities can be corrected. | Need for care with pin dressing | Peroneal nerve neuropraxia | If neuropraxia occurs, start neuropathic pain medication. |
| Apply load on day 1 postoperative. | Fracture of the medial cortex of the osteotomy | If medial cortex fracture occurs, replace the self-centering apparatus and acutely reduce the residual deformity | |
| A unique distractor facilitates patient understanding. | |||
| If overcorrection occurs, compress the osteotomy to the optimal point. |
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Here, we present a 3-dimensional animation of a case of left tibial valgus deformity. With the patient in the supine position, the first step is to mark the apex of the deformity, that is, where the local hinge must be created. The hinge is created using a Kirchner wire or drill. Next, we choose a T-clamp, bar clamp, or straight clamp. On the proximal portion of the tibia, the drill is placed 4.8 mm inside the drill guide in contact with the anterolateral cortex of the tibia, the position through which the pin will be inserted parallel to the articular surface of the tibial plateau, about 2 cm below this surface. The pin is then placed using a T-key. The next step is positioning the top of the more distal pin parallel to the surface of the ankle. One pin is placed distally while the other is placed proximally. In each portion, the pin must be parallel, and that on the distal portion will be visible on the coronal plane. On the proximal portion of the tibia, if a T-clamp is used, it will be visible on the axial rather than coronal plane. An osteotomy of the tibia is then performed with a drill 4.8 mm from the anterolateral cortex of the tibia. The medial cortex must remain intact. A complete osteotomy of the fibula is made 10 cm proximal to the lateral malleolus. The L-key is used to perform the distraction by the distractor and the positioned is checked by direct visualization of the focus and under floroscopy.
In a real case of a female patient with post-traumatic valgus, the first step is to mark the apex of the deformity by fluoroscopy. At this moment, we chose clamps. We then proceeded to drill proximally for pin placement. After the first pin, we placed the more distal pin and completed it with one proximal pin and one more distal pin. Under fluoroscopy, the apex of the deformity was marked, and the anterolateral cortex of the tibia is made partially. This was followed by an osteotomy of the fibula.
References
- 1.Goes R.A., Cruz R.S., Pavão D.M., et al. Posterior-medial meniscal root repair through lateral tibial tunnel combined with medial opening osteotomy and homologous graft. Arthrosc Tech. 2022;11:e1321–e1333. doi: 10.1016/j.eats.2022.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ozeki N., Seil R., Krych A.J., Koga H. Surgical treatment of complex meniscus tear and disease: state of the art. J ISAKOS. 2021;6:35–45. doi: 10.1136/jisakos-2019-000380. [DOI] [PubMed] [Google Scholar]
- 3.Huang Y., Deng Q., Yang L., et al. Efficacy and safety of ultrasound-guided radiofrequency treatment for chronic pain in patients with knee osteoarthritis: A systematic review and meta-analysis. Pain Res Manag. 2020;2020 doi: 10.1155/2020/2537075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kamenaga T., Nakano N., Takayama K., et al. Comparison of plantar pressure distribution during walking and lower limb alignment between modified kinematically and mechanically aligned total knee arthroplasty. J Biomech. 2021 7;120 doi: 10.1016/j.jbiomech.2021.110379. [DOI] [PubMed] [Google Scholar]
- 5.Springer B., Bechler U., Waldstein W., Rueckl K., Boettner C.S., Boettner F. The influence of femoral and tibial bony anatomy on valgus OA of the knee. Knee Surg Sports Traumatol Arthrosc. 2020;28:2998–3006. doi: 10.1007/s00167-019-05734-6. [DOI] [PubMed] [Google Scholar]
- 6.Paley D., Tetsworth K. Mechanical axis deviation of the lower limbs: Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop Rel Res. 1992;280:65–71. [PubMed] [Google Scholar]
- 7.Marques Luís N., Varatojo R. Radiological assessment of lower limb alignment. EFORT Open Rev. 2021;6:487–494. doi: 10.1302/2058-5241.6.210015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooke D., Scudamore A., Li J., Wyss U., Bryant T., Costigan P. Axial lower-limb alignment: Comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage. 1997;5:39–47. doi: 10.1016/s1063-4584(97)80030-1. [DOI] [PubMed] [Google Scholar]
- 9.Ballhause T.M., Stiel N., Breyer S., Stucker R., Spiro A.S. Does eight-plate epiphysiodesis of the proximal tibia in treating angular deformity create intra-articular deformity? Bone Joint J. 2020;102-B:1412–1418. doi: 10.1302/0301-620X.102B10.BJJ-2020-0473.R1. [DOI] [PubMed] [Google Scholar]
- 10.Reif T.J., Matthias J., Fragomen A.T., Rozbruch S.R. Limb length discrepancy and angular deformity due to benign bone tumors and tumor-like lesions. JAAOS Global Res Rev. 2021;5 doi: 10.5435/JAAOSGlobal-D-20-00214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Socc A.R., Horn D., Fornari E.D., Lakra A., Schulz J.F., Sharkey M.S. What’s new in pediatric limb lengthening and deformity correction? J Pediatr Orthop. 2020;40 doi: 10.1097/BPO.0000000000001456. e598–e602. [DOI] [PubMed] [Google Scholar]
- 12.Vrettakos N.A., Evaggelidis D.C., Krykos M.J., Tsatsos A.V., Nenopoulos A., Beslikas T. Lower limb deformity following proximal tibia physeal injury: Long-term follow-up. J Orthopaed Traumatol. 2012;13:7–11. doi: 10.1007/s10195-012-0179-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greenberg A., Kandel L., Liebergall M., Mattan Y., Rivkin G. Total knee arthroplasty for valgus deformity via a lateral approach: Clinical results, comparison to medial approach, and review of recent literature. J Arthroplasty. 2020;35:2076–2083. doi: 10.1016/j.arth.2020.03.037. [DOI] [PubMed] [Google Scholar]
- 14.de Andrade M.A.P., Gomes D.C.F.F., Portugal A.L., de Abreu e Silva G.M. Osteotomia femoral distal de varização para osteoartrose no joelho valgo: Seguimento em longo prazo. Rev Bras Ortop. 2009;44:346–350. doi: 10.1016/S2255-4971(15)30165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Navarro R.D., Cortelazo M.J., Filho A.A.A. As complicações nas osteotomias valgizantes e varizantes do joelho. Rev Bras Ortop. 1997;32:5. [Google Scholar]
- 16.Severino N.R., Camargo O.P.A., Aihara T., et al. Osteotomia supracondiliana femoral no tratamento da deformidade em valgo do joelho. Rev Bras Ortop. 1998;33(4) [Google Scholar]
- 17.Peng H., Ou A., Huang X., et al. Osteotomy around the knee: The surgical treatment of osteoarthritis. Orthop Surg. 2021;13:1465–1473. doi: 10.1111/os.13021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uboldi F.M., Travi M., Tradati D., Maione A., Manunta A.F., Berruto M. Medial closure supracondylar femoral osteotomy: An effective solution for long-term treatment of arthritic valgus knee? J Orthop Traumatol. 2021;22:35. doi: 10.1186/s10195-021-00600-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Lieshout W.A.M., Van Ginneken B.J.T., Kerkhoffs G.M.M., Van Heerwaarden R.J. Medial closing wedge high tibial osteotomy for valgus tibial deformities: Good clinical results and survival with a mean 4.5 years of follow-up in 113 patients. Knee Surg Sports Traumatol Arthrosc. 2020;28:2798–2807. doi: 10.1007/s00167-019-05480-9. [DOI] [PubMed] [Google Scholar]
- 20.Wang X., Shi L., Zhang R., et al. Salvage of severe knee osteoarthritis: Efficacy of tibial condylar valgus osteotomy versus open wedge high tibial osteotomy. J Orthop Surg Res. 2021;16:451. doi: 10.1186/s13018-021-02597-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roessler P.P., Getgood A. The role of osteotomy in chronic valgus instability and hyperextension valgus thrust (medial closing wedge distal femoral varus osteotomy and lateral opening wedge high tibial osteotomy) Clin Sports Med. 2019;38:435–449. doi: 10.1016/j.csm.2019.02.012. [DOI] [PubMed] [Google Scholar]
- 22.Cerqueira F.D.S., Motta G.A.T.A., Rocha de Faria J.L., et al. Controlled double gradual opening osteotomy for the treatment of severe varus of the knee—Blount’s disease. Arthrosc Tech. 2021;10:e2199–e2206. doi: 10.1016/j.eats.2021.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rocha de Faria J.L., Pavão D.M., Moreirão M.C., et al. Posterior root repair of medial meniscus combined with valgus opening wedge tibial osteotomy. Arthrosc Tech. 2021;10:e1373–e1382. doi: 10.1016/j.eats.2021.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Collins B., Getgood A., Alomar A.Z., et al. A case series of lateral opening wedge high tibial osteotomy for valgus malalignment. Knee Surg Sports Traumatol Arthrosc. 2013;21:152–160. doi: 10.1007/s00167-012-2070-y. [DOI] [PubMed] [Google Scholar]
- 25.Marti R.K., Verhagen R.A., Kerkhoffs G.M., Moojen T.M. Proximal tibial varus osteotomy. Indications, technique, and five to twenty-one-year results. J Bone Joint Surg Am. 2001;83:164–170. [PubMed] [Google Scholar]
- 26.Mirouse G., Dubory A., Roubineau F., et al. Failure of high tibial varus osteotomy for lateral tibio-femoral osteoarthritis with<10° of valgus: Outcomes in 19 patients. Orthop Traumatol Surg Res. 2017;103:953–958. doi: 10.1016/j.otsr.2017.03.020. [DOI] [PubMed] [Google Scholar]
- 27.Rozbruch S.R., Birch J.G., Dahl M.T., Herzenberg J.E. Motorized intramedullary nail for management of limb-length discrepancy and deformity. J Am Acad Orthop Surg. 2014;22:403–409. doi: 10.5435/JAAOS-22-07-403. [DOI] [PubMed] [Google Scholar]
- 28.Fragomen A.T., Rozbruch S.R. Lengthening and deformity correction about the knee using a magnetic internal lengthening nail. SICOT J. 2017;3:25. doi: 10.1051/sicotj/2017014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rozbruch S.R., Segal K., Ilizarov S., Fragomen A.T., Ilizarov G. Does the Taylor Spatial Frame accurately correct tibial deformities? Clin Orthop Rel Res. 2010;468:1352–1361. doi: 10.1007/s11999-009-1161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Horn D.M., Fragomen A.T., Rozbrich S.R. Supramalleolar osteotomy using circular external fixation with six-axis deformity correction of the distal tibia. Foot Ankle Int. 2011;32:986–993. doi: 10.3113/FAI.2011.0986. [DOI] [PubMed] [Google Scholar]
- 31.Loures F.B., Correia W., Reis J.H., et al. Outcomes after knee arthroplasty in extra-articular deformity. Int Orthop. 2019;43:2065–2070. doi: 10.1007/s00264-018-4147-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Here, we present a 3-dimensional animation of a case of left tibial valgus deformity. With the patient in the supine position, the first step is to mark the apex of the deformity, that is, where the local hinge must be created. The hinge is created using a Kirchner wire or drill. Next, we choose a T-clamp, bar clamp, or straight clamp. On the proximal portion of the tibia, the drill is placed 4.8 mm inside the drill guide in contact with the anterolateral cortex of the tibia, the position through which the pin will be inserted parallel to the articular surface of the tibial plateau, about 2 cm below this surface. The pin is then placed using a T-key. The next step is positioning the top of the more distal pin parallel to the surface of the ankle. One pin is placed distally while the other is placed proximally. In each portion, the pin must be parallel, and that on the distal portion will be visible on the coronal plane. On the proximal portion of the tibia, if a T-clamp is used, it will be visible on the axial rather than coronal plane. An osteotomy of the tibia is then performed with a drill 4.8 mm from the anterolateral cortex of the tibia. The medial cortex must remain intact. A complete osteotomy of the fibula is made 10 cm proximal to the lateral malleolus. The L-key is used to perform the distraction by the distractor and the positioned is checked by direct visualization of the focus and under floroscopy.
In a real case of a female patient with post-traumatic valgus, the first step is to mark the apex of the deformity by fluoroscopy. At this moment, we chose clamps. We then proceeded to drill proximally for pin placement. After the first pin, we placed the more distal pin and completed it with one proximal pin and one more distal pin. Under fluoroscopy, the apex of the deformity was marked, and the anterolateral cortex of the tibia is made partially. This was followed by an osteotomy of the fibula.
Here, we present a 3-dimensional animation of a case of left tibial valgus deformity. With the patient in the supine position, the first step is to mark the apex of the deformity, that is, where the local hinge must be created. The hinge is created using a Kirchner wire or drill. Next, we choose a T-clamp, bar clamp, or straight clamp. On the proximal portion of the tibia, the drill is placed 4.8 mm inside the drill guide in contact with the anterolateral cortex of the tibia, the position through which the pin will be inserted parallel to the articular surface of the tibial plateau, about 2 cm below this surface. The pin is then placed using a T-key. The next step is positioning the top of the more distal pin parallel to the surface of the ankle. One pin is placed distally while the other is placed proximally. In each portion, the pin must be parallel, and that on the distal portion will be visible on the coronal plane. On the proximal portion of the tibia, if a T-clamp is used, it will be visible on the axial rather than coronal plane. An osteotomy of the tibia is then performed with a drill 4.8 mm from the anterolateral cortex of the tibia. The medial cortex must remain intact. A complete osteotomy of the fibula is made 10 cm proximal to the lateral malleolus. The L-key is used to perform the distraction by the distractor and the positioned is checked by direct visualization of the focus and under floroscopy.
In a real case of a female patient with post-traumatic valgus, the first step is to mark the apex of the deformity by fluoroscopy. At this moment, we chose clamps. We then proceeded to drill proximally for pin placement. After the first pin, we placed the more distal pin and completed it with one proximal pin and one more distal pin. Under fluoroscopy, the apex of the deformity was marked, and the anterolateral cortex of the tibia is made partially. This was followed by an osteotomy of the fibula.