Abstract
Introduction
An increasing number of elderly patients suffer from hip diseases associated with moderate to severe perioperative pain during the accelerating global ageing process. Optimal analgesia can decrease perioperative complications and facilitate elderly patients’ perioperative recovery. Pericapsular nerve group (PENG) block is a relatively new, analgesia adequate and motor-sparing block technique for perioperative pain management of hip diseases. However, the efficacy of PENG block remains unclear as the limited clinical evidence. Then, we will perform a protocol for a systematic review and meta-analysis to identify the efficacy of PENG block for perioperative pain management.
Methods and analysis
PubMed, Ovid Medline, Cochrane Library, Embase, Web of Science, China National Knowledge Infrastructure, Chinese BioMedical Literature, Wanfang and VIP databases will be searched from inception to August 2022 to identify randomised controlled trials of elderly patients accepting PENG block for hip diseases. The primary outcome will be the pain intensity after pain management. Secondary outcomes will be quadriceps strength, perioperative rescue analgesia information and perioperative complications. Assessment of heterogeneity will be primarily inspected by forest plots. If there is no indication of funnel plot asymmetry, a random-effects meta-analysis will be performed. The Cochrane risk-of-bias tool, Grading of Recommendations Assessment, Development and Evaluation and trial sequential analysis will be conducted to evaluate the evidence quality and control the random errors. Funnel plots and Egger’s regression test will be performed to evaluate publication bias.
Ethics and dissemination
Ethical approval was not required for this systematic review protocol. The results will be disseminated through peer-reviewed publications.
PROSPERO registration number
CRD42022313895
Keywords: Hip, Anaesthesia in orthopaedics, Pain management
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Application of Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols guidelines for a better quality of meta-analytical results.
Control of random errors with trial sequential analysis by calculating the diversity adjusted information size for the outcomes.
Application of Funnel plots and Egger’s regression test for publication bias.
Subgroup analysis based on patients’ age, types of hip disease or surgery, perioperative period, type of anaesthesia and perioperative pain management techniques for heterogeneity assessment.
Introduction
The global population over 60 years old is estimated to increase to 2.1 billion in 2050 (approximately 22% of the global population) and 3.1 billion by 2100.1 With this accelerating ageing process, an increasing number of elderly patients suffer from hip diseases such as hip fractures and hip osteoarthritis.2–4 Hip surgery, including hip arthroplasty, hip fracture internal fixation and hip arthroscopy procedures, is the main treatments for hip diseases.5–8 Hip surgery is often associated with moderate to severe postoperative pain, particularly in hip fracture patients undergoing surgical treatment and severe pain persists throughout the perioperative period.9–11 As a minimally invasive approach, arthroscopic hip surgery is gaining popularity globally.12 Despite being minimally invasive, patients undergoing arthroscopic hip surgery may still experience severe pain after the procedure.13
Perioperative pain, if inadequately controlled, can increase the risk of perioperative complications (including delirium, pulmonary complications and cardiovascular events), delay ambulation, decrease short-term mobility, interfere with rehabilitation, increase hospital length of stay, and even increase the mortality and morbidity, leading to poor functional prognosis.14–19 In elderly patients, the risk of perioperative adverse events is higher due to polypharmacy and multimorbidity.20–22 In contrast, adequate pain management has been shown to facilitate postoperative mobilisation, improve mobility and promote better functional recovery.23–26 Early mobilisation has been associated with reducing postoperative complications, including pneumonia, venous thromboembolism, pressure ulcers and delirium.27–29 Therefore, optimal perioperative analgesia can facilitate elderly patients’ perioperative recovery.13 17 30 31
Traditionally, opioid analgesia is considered the basis of perioperative pain management.32–35 However, opioid-related complications such as delirium, urinary retention, nausea, constipation and respiratory depression may occur and can delay patients’ recovery and discharge.36–41 Considering these adverse events, especially the higher incidence of cognitive deficits in elderly patients suffering a hip fracture, opioid analgesics are often selected hesitantly.42–46 In addition, in light of the current opioid crisis, strategies to minimise opioid use, including the use of multimodal perioperative pain management strategies with opioid-sparing oral and intravenous medications, regional anaesthesia and analgesic techniques have become an increasing clinical focus in hip surgical procedures in elderly patients.47–51
Peripheral nerve blocks (including lumbar plexus block, femoral nerve block, fascia iliac compartment block, three-in-one femoral nerve block, sacral plexus block, obturator block and sciatic nerve block) and some interfascial plane blocks (such as quadratus lumborum block) have also been suggested to decrease postoperative pain and opioid use during hip surgery.52–59 However, peripheral nerve blocks may induce weakness of the quadriceps muscles, delay hospital discharge and even predispose the patient to fall.58 60–62 In some cases, it is difficult to position the patient as the extreme pain, particularly in hip fractures, accompanied by the deep depth of the block target, the lumbar plexus or quadratus lumborum block will become difficult.63–65 In addition, another difficulty of adequate regional analgesia for hip pain is the complex innervation of the hip joint.66 High branches of the femoral and obturator nerves provide innervation to the anterior hip capsule. The accessory obturator nerve was also found to innervate the medial capsule.67 68 In this situation, the coverage of the articular nerve supply to the hip joint is critical for adequate analgesia. Hence, a simple, easy-to-perform, analgesia adequate and motor-sparing regional analgesia technique is the ideal regional analgesia technique for hip surgery.
Pericapsular nerve group (PENG) block is a relatively new peripheral nerve block technique, first described by Giron-Arango in patients with hip fractures, which was based on the complex innervation of the hip joint.69 The target of the PENG block is the musculofascial plane between the psoas tendon anteriorly and the pubic ramus posteriorly. It can be easily performed in the supine position, avoiding the additional pain from positioning the patient for peripheral nerve block.70–73 In theory, PENG block has potential advantages over traditional forms of regional analgesia for pain originating from the hip, as local anaesthetic deposits in this target could provide a broader and more complete block effect on the coverage area of sensory nerves innervating the hip.9 11 74–82 Thus, it has the potential advantage of reducing postoperative pain without motor-blocking.83–86 PENG block has been described as easy to perform in the supine position and as an effective and motor-sparing regional analgesia technique for hip surgery.87–90
The excellent analgesic benefit of PENG block for perioperative analgesia in hip surgery was highlighted in a significant number of publications of case reports, case series, reviews and retrospective studies,9 11 74–78 87–90 but prospective and randomised controlled trials (RCTs) are scarce.79–82 Inadvertent quadriceps weakness was also reported in patients following the PENG block.91–93 Due to limited clinical evidence, the efficacy and safety of the PENG block, particularly the efficacy of motor function preservation and the incidence of block-related adverse events, remain controversial until now.94–98
Therefore, it is necessary to conduct a systematic review and meta-analysis to analyse the clinical efficacy of PENG block on perioperative pain management in elderly patients with hip diseases. The outcomes of this systematic review will provide evidence for better clinical decision-making and possible future directions for further clinical trials.
Objectives
We are performing this protocol of systematic review with meta-analysis and trial sequential analysis (TSA) of randomised clinical trials to evaluate the clinical efficacy and safety of PENG block on perioperative pain management in elderly patients with hip diseases.
Methods and analysis
Design and registration of the review
We devised this protocol according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) guidelines registered with PROSPERO 2022 (registration number: CRD42022313895).99 We will perform this systematic review and meta-analysis based on the Cochrane Handbook and report the results following the PRISMA statement.100 101 This study is anticipated to begin searching in August 2022 and will be completed in January 2023.
Inclusion criteria for study selection
Types of studies
Only RCTs involving the clinical efficacy of PENG block on perioperative pain management in elderly patients with hip diseases will be included. There will be no language restrictions.
The exclusion criteria were as follows: (1) studies comparing PENG block versus PENG block combined with other analgesic techniques, or studies comparing PENG block under different guidance techniques (ultrasound guided or traditional landmark technique); (2) studies with data that could not be used for statistical analysis, or studies with incomplete data, or data that could not be extracted after contacting the original authors and (3) studies that were duplicate publications, published as letters or editorials, abstracts from conferences and reviews.
Types of participants
Elderly participants (≥65 years old) with any hip disease (such as hip fracture or hip osteoarthritis) accepting PENG block for perioperative pain management (including preoperative analgesia, intraoperative anaesthesia management and postoperative analgesia) will be included. There will be no limitations on participants’ gender, ethnicity, body mass index or American Society of Anesthesiologists classification.
Types of interventions/controls
The intervention group will be the participants who received any kind of PENG block (including ultrasound-guided, X-ray-guided, CT-guided or traditional landmark-based techniques), alone or in combination with any other kind of analgesia technique for perioperative pain management, while the control group will receive any kind of analgesia technique other than PENG block for perioperative pain management.
Types of outcome measures
Primary outcomes
The primary outcome will be the pain intensity after perioperative pain management by PENG block or other analgesia techniques. Pain intensity, including preoperative and postoperative pain intensity, will be included and assessed by Visual Analogue Scale scores, Numeric Rating Scale scores or other scale scores. Perioperative static and dynamic pain intensity after pain management will also be included if possible.
Secondary outcomes
-
Unexpected perioperative femoral nerve block will be evaluated as follows if possible.
Incidence of quadriceps motor block (defined as paresis or paralysis of knee extension and hip adduction) (Knee extension was graded according to a 3-point scale: 0=normal strength (extension against gravity and resistance)); 1=paresis (extension against gravity but not against resistance); 2=paralysis (no extension possible).102 Hip adduction scores of 0, 1 and 2 points indicated decreases in strength of 0%–20%, 21%–70% and 71%–90% compared with baseline measurement, respectively.103
Mobility of the quadriceps as defined by the Medical Research Council scale.104
Quadriceps strength was assessed by measuring the force produced by voluntary isometric contractions with any type of reliable and valid stationary dynamometer (such as the Chatillon DPPH-250 force gauge, AMETEK, USA or Chatillon; AMETEK, Largo, Florida; Lafayette Instrument, Lafayette, Indiana, USA; and MicroFET, Hoggan Health Industries, West Jordan, Utah, USA).105 106
-
Perioperative rescue analgesia information
Perioperative cumulative analgesic consumption: cumulative analgesic consumption for intraoperative anaesthesia and cumulative rescue analgesics for preoperative/postoperative analgesia will be included if possible. Any kind of analgesics, such as opioid analgesics and non-steroidal analgesics administered by different delivery methods, such as patient-controlled analgesia devices, intravenous, oral or intramuscular will be included if possible.
Time to first analgesic request: time from the end of the preoperative pain management procedure to the first analgesic request or time from the end of surgery to the first analgesic request will be included if possible.
-
Perioperative complications: if possible
Block-related adverse events included vascular puncture, paresthesia, local anaesthetic toxicity, anaphylaxis, permanent nerve injury, bleeding or infection.
Intraoperative adverse effects included hyoxaemia (oxygen saturation less than 90% or oxygen partial arterial pressure ≤60 mm Hg); hypotension (defined as a decrease of >20% from preanaesthetic patient baseline values or a systolic blood pressure less than 90 mm Hg); arrhythmia [including bradycardia (defined as HR <55 beats/min); tachycardia (defined as HR>100 beats/min); any other types of arrhythmias); and blood loss.
Other adverse effects: including postoperative nausea/vomiting, pruritus, urinary retention, respiratory depression, sweating, dizziness, pruritus, urticaria, postoperative arrhythmia and postoperative pulmonary complications, were defined as the composite of any respiratory infection, respiratory failure, pleural effusion, atelectasis or pneumothorax.
Patient recovery: Length of stay, recovery time (defined as the time until recovery room discharge criteria were met after surgery), the quality of postoperative recovery score (such as the Quality of Recovery-40 questionnaire)107 and patients’ ambulation (such as time-to-first ambulation and initial ambulation distance) will be included if possible.
Patient satisfaction:
If possible, patient satisfaction with performing the perioperative pain management techniques or postoperative analgesia will be included. Satisfaction could be measured by a 5-point Likert scale (1=very dissatisfied; 2=dissatisfied; 3=neutral; 4=satisfied; 5=very satisfied), 10-point Likert scale (1=completely unsatisfied; 10=completely satisfied) or a postoperative questionnaire whether the patient would choose the same anaesthetic or analgesia handling by the answer of ‘yes’ or ‘no’.108
Exploratory outcomes
Perioperative sensory block: Sensory block was evaluated using a 3-point scale (0=no block, 1=analgesia (patient can feel touch, not cold), 2=anaesthesia (patient cannot feel touch)), which was assessed in the anterior, lateral and medial aspects of the mid-thigh.102
Block end time: defined as the return of motor (if initially impaired) and/or sensory function, which was acquired from patients’ recall.
Perioperative mortality was defined as all-cause death during the operation procedure, within 30 days after surgery, or death during hospitalisation.
Search strategy
Two reviewers (Z and LD) will independently conduct the search, and any disagreements will be resolved by consulting a third reviewer (WZ) as much as possible. English and Chinese electronic databases will be searched for published literature from inception to August 2022. PubMed, Ovid Medline, Cochrane Library, Embase and Web of Science will be included in the English databases. The Chinese BioMedical Literature (Sino-Med), China National Knowledge Infrastructure, Wanfang database and VIP Database will be included in the Chinese databases. The trial registry database (Clinical Trials.gov and WHO International Clinical Trials Registry Platform) will also be scrutinised to avoid missing ongoing or unpublished clinical trials. In addition, reference lists of each study will also be scanned for missing studies.
The search strategy will use the following search terms: pericapsular nerve group block, PENG block, elderly, hip and RCT. Related search terms will also be translated into Chinese for literature research and study identification in Chinese databases. The search strategies are listed in online supplemental appendix 1. Comprehensive updating of the literature search results will be performed prior to the final publication of systematic reviews to avoid missing published studies during the systematic review preparation.
bmjopen-2022-065304supp001.pdf (137.1KB, pdf)
Data collection and analysis
Selection of studies
At least two review authors (JZ and LD) will be responsible for screening the potentially eligible studies by reading titles and abstracts. All identified and relevant full-text publications will be retrieved by screening the full text thoroughly, and the reasons for excluding the ineligible studies will be recorded. Any disagreement will be resolved through discussion or by consulting a third review author (JZ and GC) as much as possible. A fourth reviewer (WZ) will carefully check out all procedures before the final confirmation of the data extraction. Data extraction will be performed by at least two authors, and a third author will be consulted if there is any disagreement. Duplicate publications and companion papers of the same trial will be assessed by all review authors. The study selection process is displayed in the PRISMA flow diagram (figure 1).
Figure 1.
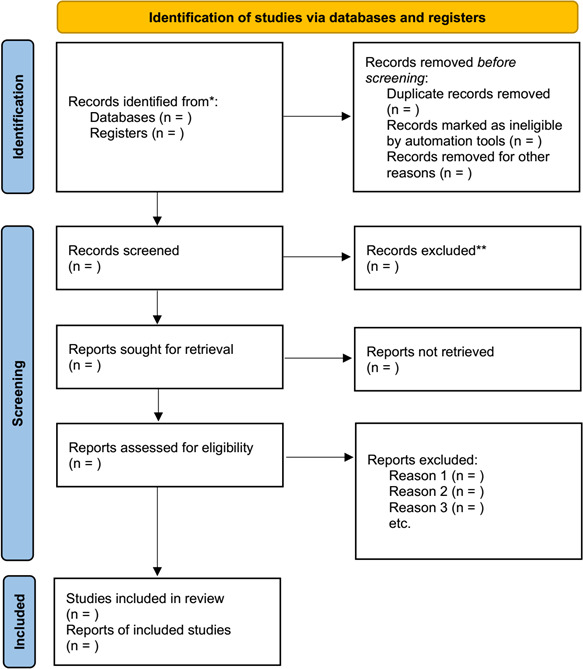
The PRISMA flow diagram. *Consider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers). **If automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Data extraction
Two review authors (JZ andLZ) will use a standardised data collection form (Excel version 2013, Microsoft, Washington DC, USA) for data extraction from each included study. The data extraction form included participants’ demographic data, type of hip disease or hip surgery, type of anaesthesia: local, spinal or general anaesthesia, period of perioperative pain management (preoperative analgesia, intraoperative anaesthesia and postoperative analgesia), inclusion and exclusion criteria, detailed information of analgesia techniques (type of perioperative analgesia techniques: PENG block or other analgesia techniques; type, concentration, dose, volume and adjuvant of local anaesthetics), and any outcomes including primary, secondary and exploratory outcomes. Study design characteristics including randomisation method, allocation concealment, blinding (patients, treatment providers, outcome investigators), incomplete outcome data collection and statistical analysis and outcome reporting) will be recorded simultaneously. Continuous and dichotomous data will be recorded as the mean±SD and the percentages or the proportion. If necessary, a third review author (XD) will cross-check the data to ensure precision. When the necessary information or data for analysis is missing or incomplete, we will contact the corresponding author of the research via email for the original data as much as possible. Necessary numerical data in the graphs will be extracted by Adobe Photoshop if necessary.109 Extracted information and data are presented in table 1.
Table 1.
Information and data extraction schedule
| Subject | Content |
| Publication information | Title; author; publish year; country of origin; corporate sponsorship; contact email. |
| Participant | Sample size; age; sex; height and weight or BMI; ASA physical status classification levels; type of hip disease or hip surgery; inclusion and exclusion criteria if necessary. |
| Intervention | Detail information of PENG block techniques (guidance techniques; target area of block; block needle; needle tracking techniques: in-plane and out-of-plane) detail information of local anaesthetics (type, concentration, dose, volume and adjuvant of local anaesthetics). |
| Control | Detail information of block analgesia techniques (including guidance techniques; target area of block; block needle; needle tracking techniques: in-plane and out-of-plane; detail information of local anaesthetics including type, concentration, dose, volume and adjuvant of local anaesthetics) and non-block analgesia techniques (including type, dose and administration method of analgesics). |
| Outcome | Primary outcome (pain intensity after perioperative pain management); secondary outcome measurements (perioperative quadriceps strength; perioperative rescue analgesia information: perioperative cumulative analgesic consumption; time to first analgesic request; patients’ recovery; perioperative complications; patients’ satisfaction); Exploratory outcomes (perioperative sensory block; block-ended time; perioperative mortality). |
| Study design | Randomisation method; blinding; allocation concealment; statistical analysis; sample size calculation; outcome reporting. |
| Other information | Type of anaesthesia: local, spinal or general anaesthesia; period of perioperative pain management (preoperative analgesia, intraoperative anaesthesia and postoperative analgesia); anaesthesia time; operation time; assessment method or equipment of outcomes. |
ASA, American Society of Anesthesiologists; BMI, body mass index; PENG, pericapsular nerve group.
Quality assessment
The risk of bias in each included study will be assessed independently by two review authors (LD and LZ) under the guidance of the Cochrane risk of bias tool.110 Methodology (including random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, other risks of bias and overall risk of bias) will be evaluated. Each included study will be assessed by the risk of bias assessment tool from the Cochrane Handbook for Systematic Reviews of Interventions and then categorised into three levels (low risk of bias, unclear of bias and high risk of bias).100 111 112 Any discrepancies will be settled through discussions by all review authors or arbitration of a third reviewer (WZ). Assessment of risk of bias is listed in online supplemental appendix 2.
bmjopen-2022-065304supp002.pdf (82.2KB, pdf)
Measures of treatment effect
Mean differences (MDs) with 95% CIs will be used for continuous outcome data reported by the same scale, and standardised MDs with 95% CIs will be used for continuous outcome data reported by different scales. The relative risks (RRs) with 95% CIs will be used for dichotomous outcome data.
Assessment of heterogeneity
The application of a fixed-effects model or random-effects model based on statistical heterogeneity is not recommended by the Cochrane guidelines.100 Assessment of heterogeneity will be primarily inspected by forest plots. If there is no indication of funnel plot asymmetry, a random-effects meta-analysis will be performed.100 If there is an indication of funnel plot asymmetry, then both a fixed-effect and a random-effect meta-analysis are problematic. In this situation, a sensitivity analysis will be performed by excluding small studies or meta-regression will be addressed directly. A p<0.05 was assumed to be statistically significant.
Trial sequential analysis
The required information size (RIS) will be calculated to correct the risks of random errors by TSA using the TSA program V.0.9.5.10 Beta (Copenhagen Trial Unit, Copenhagen, Denmark).113–115 TSA programme version is available at http://www.ctu.dk/tsa.116 Each outcome will be detected by RIS, the cumulative Z-curve and the TSA monitoring boundaries.117 118
For continuous outcomes, the observed SD, an MD of the observed SD/2 (clinically meaningful value), an alpha (type I error) of 2.5%, and a beta (type II error) of 10% will be used in the TSA.119 For dichotomous outcomes, the proportion or percentage from the control group, an RR variation of 20% (clinically meaningful value), an alpha (type I error) of 2.5%, and a beta (type II error) of 10% will be used in the TSA.120
Subgroup analysis
The results will be comprehensively interpreted through an analysis of subgroups or subsets as much as possible. If sufficient trials are available, data from different participants’ ages, different types of hip disease or different kinds of surgical techniques of hip surgery, pain management during different perioperative periods, different pain management techniques in the control group, different types of anaesthesia and different types, concentrations, doses, volumes and adjuvants of local anaesthetics for PENG block will be analysed independently.
Different participants’ ages (PENG block for perioperative analgesia in elderly patients with different ages as follows: 65 years≤patients<75 years; 75 years≤patients<80 years; patients≥80 years).
Different types of hip disease or different kinds of surgical techniques of hip surgery (hip disease, such as hip fracture and hip osteoarthritis; hip surgery, such as different kinds of surgical techniques of hip arthroplasty, hip fracture fixation and hip arthroscopy procedures).
Pain management of different perioperative periods (PENG block for preoperative analgesia, intraoperative anaesthesia and postoperative analgesia).
Different pain management techniques in the control group (such as block analgesia techniques, including lumbar plexus block, femoral nerve block, fascia-iliac compartment block, three-in-one femoral nerve block, sacral plexus block, obturator and sciatic nerve block, and quadratus lumborum block. Non-block analgesia techniques such as opioid and no-opioid analgesics).
Different types of anaesthesia (such as local anaesthesia, spinal anaesthesia or general anaesthesia).
Different volumes, concentrations, doses and adjuvants of local anaesthetics for PENG block.
The interaction p value will be considered to test the statistically significant subgroup difference; if testing for interaction p<0.05 (a significant difference between subgroups exists), the results for individual subgroups will be reported separately.100
Sensitivity analysis
Sensitivity analysis will be applied after the analysis of subgroups or subsets to evaluate the stability of the combined results, which could be affected by uncertain assumptions of data and usage. Significant changes in the pooled results may indicate significant heterogeneity in the included studies. Low-quality studies, defined as high-risk bias studies according to the Cochrane risk of bias tool assessment, will be excluded. Then, the included studies will be reanalysed to detect obvious differences between the combined effects. The stability of the pooled estimations will be detected by removing each included study if necessary.
Assessment of publication biases
Egger’s regression test and funnel plot analysis will be performed to estimate the potential publication bias, while more than 10 original studies involved an outcome.121 122 The symmetric pattern of the funnel plot by trim-and-fill analysis will also be used to confirm the potential publication bias. The effect sizes of each included study will normally be symmetrically distributed around the centre of a funnel plot in the absence of publication bias.123 Publication biases will be detected by Stata/MP V.16.0 (StataCorp).
Grading the quality of evidence
The quality of evidence for each outcome will be assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria.124 The quality of effect estimates will be classified as high, moderate, low or very low depending on the risk of bias, consistency, directness, precision and publication bias.124 Data from RCTs are classified as high-quality evidence according to GRADE. However, it can be degraded according to the risk of bias, imprecision, inconsistency, indirectness or publication bias.
Patient and public involvement statement
Patients or the public were not involved in the design, conduct, reporting or dissemination plans of our research.
Discussion
More and more elderly patients suffer from hip diseases in the global accelerating ageing process. As the main therapy for hip diseases, hip surgery is often associated with moderate to severe perioperative pain. Optimal perioperative analgesia can decrease the risk of perioperative complications and facilitate elderly patient perioperative recovery. Opioid analgesics are often selected hesitantly as opioid-related complications, which can delay patient recovery and discharge. Regional anaesthesia and analgesic techniques for perioperative pain management have gradually become the clinical focus in elderly patients with hip diseases to facilitate patient recovery. A simple, easy-to-perform, adequate analgesia and motor-sparing regional analgesia technique is ideal for perioperative pain management of hip diseases.
The PENG block is a relatively new, easy-to-perform, analgesia adequate and motor-sparing peripheral nerve block technique. The benefit of PENG block for perioperative analgesia in hip surgery was based on many publications of case reports, case series, reviews and retrospective studies. However, prospective and RCTs are rare. Due to the limited clinical evidence, the efficacy and safety of the PENG block remain unclear.
This systematic review will provide an overview of the current state of evidence on the clinical efficacy and safety of the PENG block for perioperative analgesia in elderly patients with hip disease. We will examine the perioperative analgesia efficacy, the advantage of motor function preservation and the incidence of block-related adverse events of PENG block. The results of this systematic review will facilitate clinical decision-making on better perioperative pain management of elderly patients with hip disease.
This systematic review protocol was rigorously performed according to the PRISMA-P guidelines. The strengths of our systematic review are as follows: First, a comprehensive literature search of English and Chinese databases will be performed. Second, we will perform multivariable analysis (including subgroup analysis, TSA for random errors, sensitivity analysis, study quality assessment, funnel plots and Egger’s regression test for publication bias) to improve the quality of the evidence. Third, literature retrieval, data extraction and study quality assessment will be performed independently according to the guidelines by at least two review authors. Any disagreement will be resolved through discussion or by consulting another review author as much as possible.
Limitations are as follows: First, studies with different perioperative periods, hip diseases or hip surgeries will be included, leading to potential heterogeneity. Second, PENG block is a relatively new peripheral nerve block technique, so the sample size of each included study may be limited, and the number of studies with available data for subgroup analyses may be small. Third, studies with high-level evidence such as well-designed RCTs with double-blind designs may be limited, as it is difficult to perform blinding for different block techniques in different puncture positions. Fourth, PENG block is a relatively new peripheral nerve block technique. It is difficult to define a significant clinical plausible value of MD and RR increase/decrease during literature research or clinical experience. Therefore, a significant clinical plausible value will be defined according to TSA guidelines.
Supplementary Material
Footnotes
Contributors: JZ and LD conceived the idea for this systematic review. All authors (JZ, LD, GC, LZ, XD and WZ) developed the methodology for the systematic review. The manuscript was drafted by JZ and LD, and revised by all authors. GC and WZ will screen potential studies, and perform duplicate independent data abstraction. JZ and LZ will undertake a risk of bias assessment and assess the evidence quality. JZ and LD will conduct the data synthesis. All authors contributed to the research and agreed to be responsible for all aspects of the work.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.World Health Organization . Ageing and health, 2020. Available: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health [Accessed 28 May 2022].
- 2.Centers for Disease Control and Prevention . Injury prevention & control: hip fractures among older adults. Available: https://www.cdc.gov/falls/hip-fractures.html [Accessed 28 May 2022].
- 3.Katz JN, Arant KR, Loeser RF. Diagnosis and treatment of hip and knee osteoarthritis. JAMA 2021;325:568–78. 10.1001/jama.2020.22171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fu M, Zhou H, Li Y, et al. Global, regional, and national burdens of hip osteoarthritis from 1990 to 2019: estimates from the 2019 global burden of disease study. Arthritis Res Ther 2022;24:8. 10.1186/s13075-021-02705-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hasan K, Shankar S, Sharma A, et al. HIP surgery and its evidence base: progress over a decade? J Orthopaed Traumatol 2016;17:291–5. 10.1007/s10195-016-0421-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Antoniou J, Silotch C, Epure LL, et al. Elective total hip arthroplasties in nonagenarians-age does matter: a national surgical quality improvement program study. J Arthroplasty 2022;37:S524–9. 10.1016/j.arth.2022.01.067 [DOI] [PubMed] [Google Scholar]
- 7.Cui L, Zhao S, Tian H, et al. Curative efficacy of surgical procedures for older patients with femoral neck fracture: a network meta-analysis and systematic review. J Orthop Surg Res 2022;17:127. 10.1186/s13018-022-02914-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cross GWV, Sobti AS, Khan T. HIP arthroscopy in osteoarthritis: is it an option? J Clin Orthop Trauma 2021;22:101617. 10.1016/j.jcot.2021.101617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morrison C, Brown B, Lin D-Y, et al. Analgesia and anesthesia using the pericapsular nerve group block in hip surgery and hip fracture: a scoping review. Reg Anesth Pain Med 2021;46:169–75. 10.1136/rapm-2020-101826 [DOI] [PubMed] [Google Scholar]
- 10.Abou-Setta AM, Beaupre LA, Rashiq S, et al. Comparative effectiveness of pain management interventions for hip fracture: a systematic review. Ann Intern Med 2011;155:234–45. 10.7326/0003-4819-155-4-201108160-00346 [DOI] [PubMed] [Google Scholar]
- 11.Orozco S, Muñoz D, Jaramillo S, et al. Pericapsular nerve group (PENG) block for perioperative pain control in hip arthroscopy. J Clin Anesth 2020;59:3–4. 10.1016/j.jclinane.2019.04.037 [DOI] [PubMed] [Google Scholar]
- 12.Bozic KJ, Chan V, Valone FH, et al. Trends in HIP arthroscopy utilization in the United States. J Arthroplasty 2013;28:140–3. 10.1016/j.arth.2013.02.039 [DOI] [PubMed] [Google Scholar]
- 13.Bech NH, Hulst AH, Spuijbroek JA, et al. Perioperative pain management in HIP arthroscopy; what options are there? J Hip Preserv Surg 2016;3:181–9. 10.1093/jhps/hnw015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 2017;10:2287–98. 10.2147/JPR.S144066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pozek J-PJ, De Ruyter M, Khan TW. Comprehensive acute pain management in the perioperative surgical home. Anesthesiol Clin 2018;36:295–307. 10.1016/j.anclin.2018.01.007 [DOI] [PubMed] [Google Scholar]
- 16.Tsinaslanidis G, Tsinaslanidis P, Mahajan RH. Perioperative pain management in patients undergoing total hip arthroplasty: where do we currently stand? Cureus 2020;32:e9049. 10.7759/cureus.9049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pepper AM, Mercuri JJ, Behery OA, et al. Total HIP and knee arthroplasty perioperative pain management: what should be in the cocktail. JBJS Rev 2018;6:e5. 10.2106/JBJS.RVW.18.00023 [DOI] [PubMed] [Google Scholar]
- 18.Pyati S, Gan TJ. Perioperative pain management. CNS Drugs 2007;21:185–211. 10.2165/00023210-200721030-00002 [DOI] [PubMed] [Google Scholar]
- 19.Morrison RS, Magaziner J, Gilbert M, et al. Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J Gerontol A Biol Sci Med Sci 2003;58:M76–81. 10.1093/gerona/58.1.M76 [DOI] [PubMed] [Google Scholar]
- 20.Feldt KS, Oh HL. Pain and HIP fracture outcomes for older adults. Orthopaedic Nursing 2000;19:35–44. 10.1097/00006416-200019060-00008 [DOI] [PubMed] [Google Scholar]
- 21.Roche JJW, Wenn RT, Sahota O, et al. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 2005;331:1374. 10.1136/bmj.38643.663843.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shellito AD, Dworsky JQ, Kirkland PJ, et al. Perioperative pain management issues unique to older adults undergoing surgery. Ann Surg Open 2021;2:e072. 10.1097/AS9.0000000000000072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tan M, Law LS-C, Gan TJ. Optimizing pain management to facilitate enhanced recovery after surgery pathways. Can J Anesth/J Can Anesth 2015;62:203–18. 10.1007/s12630-014-0275-x [DOI] [PubMed] [Google Scholar]
- 24.Ranawat AS, Ranawat CS. Pain management and accelerated rehabilitation for total HIP and total knee arthroplasty. J Arthroplasty 2007;22:12–15. 10.1016/j.arth.2007.05.040 [DOI] [PubMed] [Google Scholar]
- 25.Wan H-yang, Li S-yi, Ji W, et al. Fascia Iliaca compartment block for perioperative pain management of geriatric patients with hip fractures: a systematic review of randomized controlled trials. Pain Res Manag 2020;2020:1–12. 10.1155/2020/8503963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang S, Zhang T, Wang P, et al. The impact of perioperative multimodal pain management on postoperative outcomes in patients (aged 75 and older) undergoing short-segment lumbar fusion surgery. Pain Res Manag 2022;2022:1–8. 10.1155/2022/9052246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baer M, Neuhaus V, Pape HC, et al. Influence of mobilization and weight bearing on in-hospital outcome in geriatric patients with HIP fractures. Sicot J 2019;5:4. 10.1051/sicotj/2019005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guerra ML, Singh PJ, Taylor NF. Early mobilization of patients who have had a HIP or knee joint replacement reduces length of stay in hospital: a systematic review. Clin Rehabil 2015;29:844–54. 10.1177/0269215514558641 [DOI] [PubMed] [Google Scholar]
- 29.Okamoto T, Ridley RJ, Edmondston SJ, et al. Day-of-surgery mobilization reduces the length of stay after elective hip arthroplasty. J Arthroplasty 2016;31:2227–30. 10.1016/j.arth.2016.03.066 [DOI] [PubMed] [Google Scholar]
- 30.Ruel M, Boussat B, Boudissa M, et al. Management of preoperative pain in elderly patients with moderate to severe cognitive deficits and hip fracture: a retrospective, monocentric study in an orthogeriatric unit. BMC Geriatr 2021;21:575. 10.1186/s12877-021-02500-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karam JA, Schwenk ES, Parvizi J. An update on multimodal pain management after total joint arthroplasty. J Bone Joint Surg Am 2021;103:1652–62. 10.2106/JBJS.19.01423 [DOI] [PubMed] [Google Scholar]
- 32.Baker DW. History of the joint commission's pain standards: lessons for today's prescription opioid epidemic. JAMA 2017;317:1117–8. 10.1001/jama.2017.0935 [DOI] [PubMed] [Google Scholar]
- 33.El Moheb M, Mokhtari A, Han K, et al. Pain or no pain, we will give you opioids: relationship between number of opioid pills prescribed and severity of pain after operation in US vs non-US patients. J Am Coll Surg 2020;231:639–48. 10.1016/j.jamcollsurg.2020.08.771 [DOI] [PubMed] [Google Scholar]
- 34.Loh FE, Herzig SJ. Pain in the United States: time for a culture shift in expectations, messaging, and management. J Hosp Med 2019;14:787–8. 10.12788/jhm.3277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hyland SJ, Brockhaus KK, Vincent WR, et al. Perioperative pain management and opioid stewardship: a practical guide. Health Care 2021;9:333. 10.3390/healthcare9030333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oderda GM, Senagore AJ, Morland K, et al. Opioid-related respiratory and gastrointestinal adverse events in patients with acute postoperative pain: prevalence, predictors, and burden. J Pain Palliat Care Pharmacother 2019;33:82–97. 10.1080/15360288.2019.1668902 [DOI] [PubMed] [Google Scholar]
- 37.Kane-Gill SL, Rubin EC, Smithburger PL, et al. The cost of opioid-related adverse drug events. J Pain Palliat Care Pharmacother 2014;28:282–93. 10.3109/15360288.2014.938889 [DOI] [PubMed] [Google Scholar]
- 38.Oderda GM, Said Q, Evans RS, et al. Opioid-related adverse drug events in surgical hospitalizations: impact on costs and length of stay. Ann Pharmacother 2007;41:400–7. 10.1345/aph.1H386 [DOI] [PubMed] [Google Scholar]
- 39.Brat GA, Agniel D, Beam A, et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ 2018;360:j5790. 10.1136/bmj.j5790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg 2017;152:e170504. 10.1001/jamasurg.2017.0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chau D, et al. Opiates and elderly: use and side effects. Clin Interv Aging 2008;3:273–8. 10.2147/CIA.S1847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gazelka HM, Leal JC, Lapid MI, et al. Opioids in older adults: indications, prescribing, complications, and alternative therapies for primary care. Mayo Clinic Proceedings 2020;95:793–800. 10.1016/j.mayocp.2020.02.002 [DOI] [PubMed] [Google Scholar]
- 43.Bitsch M, Foss N, Kristensen B, et al. Pathogenesis of and management strategies for postoperative delirium after hip fracture: a review. Acta Orthop Scand 2004;75:378–89. 10.1080/00016470410001123 [DOI] [PubMed] [Google Scholar]
- 44.Amador LF, Goodwin JS. Postoperative delirium in the older patient. J Am Coll Surg 2005;200:767–73. 10.1016/j.jamcollsurg.2004.08.031 [DOI] [PubMed] [Google Scholar]
- 45.Bicket MC, Brat GA, Hutfless S, et al. Optimizing opioid prescribing and pain treatment for surgery: review and conceptual framework. Am J Health Syst Pharm 2019;76:1403–12. 10.1093/ajhp/zxz146 [DOI] [PubMed] [Google Scholar]
- 46.Pasero CL, McCaffery M. Reluctance to order opioids in elders. Am J Nurs 1997;97:20–3. 10.1097/00000446-199709000-00018 [DOI] [PubMed] [Google Scholar]
- 47.Chia PA, Cannesson M, Bui CCM. Opioid free anesthesia: feasible? Curr Opin Anaesthesiol 2020;33:512–7. 10.1097/ACO.0000000000000878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kharasch ED, Avram MJ, Clark JD. Rational perioperative opioid management in the era of the opioid crisis. Anesthesiology 2020;132:603–5. 10.1097/ALN.0000000000003166 [DOI] [PubMed] [Google Scholar]
- 49.Larach DB, Hah JM, Brummett CM. The opioid crisis, and the anesthesiologist. Anesthesiology 2022;136:594–608. 10.1097/ALN.0000000000004109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Everson M, McLain N, Collins MJ, et al. Perioperative pain management strategies in the age of an opioid epidemic. J Perianesth Nurs 2020;35:347–52. 10.1016/j.jopan.2020.01.001 [DOI] [PubMed] [Google Scholar]
- 51.Bugada D, Bellini V, Lorini LF, et al. Update on selective regional analgesia for hip surgery patients. Anesthesiol Clin 2018;36:403–15. 10.1016/j.anclin.2018.04.001 [DOI] [PubMed] [Google Scholar]
- 52.Hogan MV, Grant RE, Lee L. Analgesia for total HIP and knee arthroplasty: a review of lumbar plexus, femoral, and sciatic nerve blocks. Am J Orthop 2009;38:E129–33. [PubMed] [Google Scholar]
- 53.Foss NB, Kristensen BB, Bundgaard M, et al. Fascia iliaca compartment blockade for acute pain control in hip fracture patients: a randomized, placebo-controlled trial. Anesthesiology 2007;106:773–8. 10.1097/01.anes.0000264764.56544.d2 [DOI] [PubMed] [Google Scholar]
- 54.Haines L, Dickman E, Ayvazyan S, et al. Ultrasound-guided fascia iliaca compartment block for hip fractures in the emergency department. J Emerg Med 2012;43:692–7. 10.1016/j.jemermed.2012.01.050 [DOI] [PubMed] [Google Scholar]
- 55.Unneby A, Svensson O, Gustafson Y, et al. Femoral nerve block in a representative sample of elderly people with hip fracture: a randomised controlled trial. Injury 2017;48:1542–9. 10.1016/j.injury.2017.04.043 [DOI] [PubMed] [Google Scholar]
- 56.Beaudoin FL, Haran JP, Liebmann O. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: a randomized controlled trial. Acad Emerg Med 2013;20:584–91. 10.1111/acem.12154 [DOI] [PubMed] [Google Scholar]
- 57.Desmet M, Vermeylen K, Van Herreweghe I, et al. A longitudinal supra-inguinal fascia Iliaca compartment block reduces morphine consumption after total hip arthroplasty. Reg Anesth Pain Med 2017;42:327–33. 10.1097/AAP.0000000000000543 [DOI] [PubMed] [Google Scholar]
- 58.Gasanova I, Alexander JC, Estrera K, et al. Ultrasound-guided suprainguinal fascia iliaca compartment block versus periarticular infiltration for pain management after total hip arthroplasty: a randomized controlled trial. Reg Anesth Pain Med 2019;44:206–11. 10.1136/rapm-2018-000016 [DOI] [PubMed] [Google Scholar]
- 59.Kuchálik J, Magnuson A, Lundin A, et al. Local infiltration analgesia or femoral nerve block for postoperative pain management in patients undergoing total hip arthroplasty. A randomized, double-blind study. Scand J Pain 2017;16:223–30. 10.1016/j.sjpain.2017.05.002 [DOI] [PubMed] [Google Scholar]
- 60.Behrends M, Yap EN, Zhang AL, et al. Preoperative fascia Iliaca block does not improve analgesia after arthroscopic hip surgery, but causes quadriceps muscles weakness. Anesthesiology 2018;129:536–43. 10.1097/ALN.0000000000002321 [DOI] [PubMed] [Google Scholar]
- 61.Johnson RL, Kopp SL, Hebl JR, et al. Falls and major orthopaedic surgery with peripheral nerve blockade: a systematic review and meta-analysis. Br J Anaesth 2013;110:518–28. 10.1093/bja/aet013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gadsden JC, Lindenmuth DM, Hadzic A, et al. Lumbar plexus block using high-pressure injection leads to contralateral and epidural spread. Anesthesiology 2008;109:683–8. 10.1097/ALN.0b013e31818631a7 [DOI] [PubMed] [Google Scholar]
- 63.Brixel SM, Biboulet P, Swisser F, et al. Posterior quadratus lumborum block in total hip arthroplasty: a randomized controlled trial. Anesthesiology 2021;134:722–33. 10.1097/ALN.0000000000003745 [DOI] [PubMed] [Google Scholar]
- 64.Kukreja P, MacBeth L, Sturdivant A, et al. Anterior quadratus lumborum block analgesia for total hip arthroplasty: a randomized, controlled study. Reg Anesth Pain Med 2019;44. 10.1136/rapm-2019-100804. [Epub ahead of print: 25 Oct 2019]. [DOI] [PubMed] [Google Scholar]
- 65.Jadon A, Kedia S, Dixit S, et al. Comparative evaluation of femoral nerve block and intravenous fentanyl for positioning during spinal anaesthesia in surgery of femur fracture. Indian J Anaesth 2014;58:705–8. 10.4103/0019-5049.147146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Birnbaum K, Prescher A, Heßler S, et al. The sensory innervation of the hip joint - an anatomical study. Surg Radiol Anat 1997;19:371–5. 10.1007/BF01628504 [DOI] [PubMed] [Google Scholar]
- 67.Short AJ, Barnett JJG, Gofeld M, et al. Anatomic study of innervation of the anterior hip capsule: implication for image-guided intervention. Reg Anesth Pain Med 2018;43:186–92. 10.1097/AAP.0000000000000701 [DOI] [PubMed] [Google Scholar]
- 68.Gerhardt M, Johnson K, Atkinson R, et al. Characterisation and classification of the neural anatomy in the human hip joint. HIP International 2012;22:75–81. 10.5301/HIP.2012.9042 [DOI] [PubMed] [Google Scholar]
- 69.Girón-Arango L, Peng PWH, Chin KJ, et al. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med 2018;43:1–63. 10.1097/AAP.0000000000000847 [DOI] [PubMed] [Google Scholar]
- 70.Acharya U, Lamsal R. Pericapsular nerve group block: an excellent option for analgesia for positional pain in hip fractures. Case Rep Anesthesiol 2020;2020:1–3. 10.1155/2020/1830136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jadon A, Mohsin K, Sahoo R, et al. Comparison of supra-inguinal fascia iliaca versus pericapsular nerve block for ease of positioningduring spinal anaesthesia: a randomised double-blinded trial. Indian J Anaesth 2021;65:572–8. 10.4103/ija.IJA_417_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sahoo R, Jadon A, Sharma S, et al. Peri-capsular nerve group block provides excellent analgesia in hip fractures and positioning for spinal anaesthesia: a prospective cohort study. Indian J Anaesth 2020;64:898–900. 10.4103/ija.IJA_450_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mistry T, Sonawane K, Raghuvanshi A, et al. Preemptive pericapsular nerve group block to facilitate sitting position for neuraxial anesthesia in patients with acetabular fractures: a case series. Saudi J Anaesth 2022;16:221–5. 10.4103/sja.sja_614_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kukreja P, Avila A, Northern T, et al. A retrospective case series of pericapsular nerve group (PENG) block for primary versus revision total hip arthroplasty analgesia. Cureus 2020;12:e8200. 10.7759/cureus.8200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mysore K, Sancheti SA, Howells SR, et al. Postoperative analgesia with pericapsular nerve group (PENG) block for primary total hip arthroplasty: a retrospective study. Can J Anesth/J Can Anesth 2020;67:1673–4. 10.1007/s12630-020-01751-z [DOI] [PubMed] [Google Scholar]
- 76.Kinjo S, Zhang AL. Rescue pericapsular nerve group block for hip arthroscopy: a report of 3 cases. A A Pract 2022;16:e01553. 10.1213/XAA.0000000000001553 [DOI] [PubMed] [Google Scholar]
- 77.Jacob Tannehill I, Jacob Tannehill I, Tucker CJ, et al. The pericapsular nerve group block for perioperative pain management for hip arthroscopy. Arthrosc Tech 2021;10:e1799–803. 10.1016/j.eats.2021.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rocha‐Romero A, Arias‐Mejia K, Salas‐Ruiz A, et al. Pericapsular nerve group (PENG) block for hip fracture in the emergency department: a case series. Anaesth Rep 2021;9:97–100. 10.1002/anr3.12118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Natrajan P, Bhat RR, Remadevi R, et al. Comparative study to evaluate the effect of ultrasound-guided pericapsular nerve group block versus fascia Iliaca compartment block on the postoperative analgesic effect in patients undergoing surgeries for hip fracture under spinal anesthesia. Anesth Essays Res 2021;15:285–9. 10.4103/aer.aer_122_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mosaffa F, Taheri M, Manafi Rasi A, et al. Comparison of pericapsular nerve group (PENG) block with fascia iliaca compartment block (FICB) for pain control in hip fractures: a double-blind prospective randomized controlled clinical trial. Orthop & Surg Res 2022;108:103135. 10.1016/j.otsr.2021.103135 [DOI] [PubMed] [Google Scholar]
- 81.Aliste J, Layera S, Bravo D, et al. Randomized comparison between pericapsular nerve group (PENG) block and suprainguinal fascia iliaca block for total hip arthroplasty. Reg Anesth Pain Med 2021;46:874–8. 10.1136/rapm-2021-102997 [DOI] [PubMed] [Google Scholar]
- 82.Zheng J, Pan D, Zheng B, et al. Preoperative pericapsular nerve group (PENG) block for total hip arthroplasty: a randomized, placebo-controlled trial. Reg Anesth Pain Med 2022;47:155–60. 10.1136/rapm-2021-103228 [DOI] [PubMed] [Google Scholar]
- 83.Hua H, Xu Y, Jiang M, et al. Evaluation of pericapsular nerve group (PENG) block for analgesic effect in elderly patients with femoral neck fracture undergoing hip arthroplasty. J Healthc Eng 2022;2022:1–7. 10.1155/2022/7452716 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 84.Pascarella G, Costa F, Del Buono R, et al. Impact of the pericapsular nerve group (PENG) block on postoperative analgesia and functional recovery following total hip arthroplasty: a randomised, observer‐masked, controlled trial. Anaesthesia 2021;76:1492–8. 10.1111/anae.15536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lin D-Y, Brown B, Morrison C, et al. Pericapsular nerve group block results in a longer analgesic effect and shorter time to discharge than femoral nerve block in patients after hip fracture surgery: a single-center double-blinded randomized trial. J Int Med Res 2022;50:030006052210850. 10.1177/03000605221085073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Choi YS, Park KK, Lee B, et al. Pericapsular nerve group (PENG) block versus supra-inguinal fascia Iliaca compartment block for total hip arthroplasty: a randomized clinical trial. J Pers Med 2022;12:408. 10.3390/jpm12030408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sahoo R, Jadon A, Sharma S, et al. Pericapsular nerve group (PENG) block for hip fractures: another weapon in the armamentarium of anesthesiologists. J Anaesthesiol Clin Pharmacol 2021;37:295–6. 10.4103/joacp.JOACP_295_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Black ND, Chin KJ. Pericapsular nerve group (PENG) block: comments and practical considerations. J Clin Anesth 2019;56:143–4. 10.1016/j.jclinane.2019.02.010 [DOI] [PubMed] [Google Scholar]
- 89.Del Buono R, Padua E, Pascarella G, et al. Pericapsular nerve group block: an overview. Minerva Anestesiol 2021;87:458–66. 10.23736/S0375-9393.20.14798-9 [DOI] [PubMed] [Google Scholar]
- 90.Bilal B, Öksüz G, Boran Ömer Faruk, et al. High volume pericapsular nerve group (PENG) block for acetabular fracture surgery: a new horizon for novel block. J Clin Anesth 2020;62:109702. 10.1016/j.jclinane.2020.109702 [DOI] [PubMed] [Google Scholar]
- 91.Endersby RVW, Moser JJ, Ho ECY, et al. Motor blockade after iliopsoas plane (IPB) and pericapsular nerve group (PENG) blocks: a little may go a long way. Acta Anaesthesiol Scand 2021;65:135–6. 10.1111/aas.13707 [DOI] [PubMed] [Google Scholar]
- 92.Yu HC, Moser JJ, Chu AY, et al. Inadvertent quadriceps weakness following the pericapsular nerve group (PENG) block. Reg Anesth Pain Med 2019;44:611–3. 10.1136/rapm-2018-100354 [DOI] [PubMed] [Google Scholar]
- 93.Ciftci B, Ahiskalioglu A, Altintas HM, et al. A possible mechanism of motor blockade of high volume pericapsular nerve group (PENG) block: a cadaveric study. J Clin Anesth 2021;74:110407. 10.1016/j.jclinane.2021.110407 [DOI] [PubMed] [Google Scholar]
- 94.Mistry T, Sonawane KB. Gray zone of pericapsular nerve group (PENG) block. J Clin Anesth 2019;58:123–4. 10.1016/j.jclinane.2019.07.006 [DOI] [PubMed] [Google Scholar]
- 95.Allard C, Pardo E, de la Jonquière C, et al. Comparison between femoral block and PENG block in femoral neck fractures: a cohort study. PLoS One 2021;16:e0252716. 10.1371/journal.pone.0252716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Valoriani J, Conti D, Gianesello L, et al. Combined pericapsular nerve group and lateral femoral cutaneous nerve blocks for hip fracture in a polytraumatized patient-A case report. Saudi J Anaesth 2022;16:211–3. 10.4103/sja.sja_625_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gong W-Y, Li N, Chen Y-Y, et al. Combination of pericapsular nerve group (PENG) and sacral plexus blocks for minimally invasive percutaneous internal fixation in outpatient with femoral neck pathologic fracture. Pain Med 2022;23:427–8. 10.1093/pm/pnab307 [DOI] [PubMed] [Google Scholar]
- 98.Luo W, Liang J, Wu J, et al. Effects of pericapsular nerve group (PENG) block on postoperative recovery in elderly patients with hip fracture: study protocol for a randomised, parallel controlled, double-blind trial. BMJ Open 2022;12:e051321. 10.1136/bmjopen-2021-051321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 100.Higgins JPT, Thomas J, Chandler J. Cochrane Handbook for systematic reviews of interventions version 6.2. Cochrane, 2021. www.training.cochrane.org/handbook [Google Scholar]
- 101.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bravo D, Layera S, Aliste J, et al. Lumbar plexus block versus suprainguinal fascia iliaca block for total hip arthroplasty: a single-blinded, randomized trial. J Clin Anesth 2020;66:109907. 10.1016/j.jclinane.2020.109907 [DOI] [PubMed] [Google Scholar]
- 103.Arnuntasupakul V, Chalachewa T, Leurcharusmee P, et al. Ultrasound with neurostimulation compared with ultrasound guidance alone for lumbar plexus block: a randomised single blinded equivalence trial. Eur J Anaesthesiol 2018;35:224–30. 10.1097/EJA.0000000000000736 [DOI] [PubMed] [Google Scholar]
- 104.McGillivray MK, Haldane C, Doherty C. Evaluation of muscle strength following peripheral nerve surgery: a scoping review. PM&R 2022;14:383–94. 10.1002/pmrj.12586 [DOI] [PubMed] [Google Scholar]
- 105.Behrends M, Yap EN, Zhang AL, et al. Preoperative fascia Iliaca block does not improve analgesia after arthroscopic hip surgery, but causes quadriceps muscles weakness: a randomized, double-blind trial. Anesthesiology 2018;129:536–43. 10.1097/ALN.0000000000002321 [DOI] [PubMed] [Google Scholar]
- 106.Maffiuletti NA. Assessment of hip and knee muscle function in orthopaedic practice and research. J Bone Joint Surg Am 2010;92:220–9. 10.2106/JBJS.I.00305 [DOI] [PubMed] [Google Scholar]
- 107.Wessels E, Perrie H, Scribante J, et al. Quality of recovery in the perioperative setting: a narrative review. J Clin Anesth 2022;78:110685. 10.1016/j.jclinane.2022.110685 [DOI] [PubMed] [Google Scholar]
- 108.Soares RW, Ruzbarsky JJ, Arner JW, et al. Midterm outcomes after hip Labral augmentation in revision hip arthroscopy. Am J Sports Med 2022;50:1299–305. 10.1177/03635465221080162 [DOI] [PubMed] [Google Scholar]
- 109.Gheibi S, Mahmoodzadeh A, Kashfi K, et al. Data extraction from graphs using adobe photoshop: applications for meta-analyses. Int J Endocrinol Metab 2019;17:e95216. 10.5812/ijem.95216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Higgins JPT, Altman DG, Gøtzsche PC, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Higgins JPT, Savović J, Page MJ. Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, et al., eds. Cochrane Handbook for systematic reviews of interventions version 6.2. 2021. Cochrane, 2021. www.training.cochrane.org/handbook [Google Scholar]
- 112.Savović J, Turner RM, Mawdsley D, et al. Association between risk-of-bias assessments and results of randomized trials in cochrane reviews: the ROBES meta-epidemiologic study. Am J Epidemiol 2018;187:1113–22. 10.1093/aje/kwx344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wetterslev J, Thorlund K, Brok J, et al. Estimating required information size by quantifying diversity in random-effects model meta-analyses. BMC Med Res Methodol 2009;9:86. 10.1186/1471-2288-9-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wetterslev J, Jakobsen JC, Gluud C. Trial sequential analysis in systematic reviews with meta-analysis. BMC Med Res Methodol 2017;17:39. 10.1186/s12874-017-0315-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wetterslev J, Thorlund K, Brok J, et al. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol 2008;61:64–75. 10.1016/j.jclinepi.2007.03.013 [DOI] [PubMed] [Google Scholar]
- 116.Thorlund K, Engstrøm J, Wetterslev J. User manual for trial sequential analysis (TSA) Copenhagen trial unit, centre for clinical intervention research. Denmark, 2021. http://www.ctu.dk/tsa [Google Scholar]
- 117.Imberger G, Thorlund K, Gluud C, et al. False-positive findings in cochrane meta-analyses with and without application of trial sequential analysis: an empirical review. BMJ Open 2016;6:e011890. 10.1136/bmjopen-2016-011890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Brok J, Thorlund K, Gluud C, et al. Trial sequential analysis reveals insufficient information size and potentially false positive results in many meta-analyses. J Clin Epidemiol 2008;61:763–9. 10.1016/j.jclinepi.2007.10.007 [DOI] [PubMed] [Google Scholar]
- 119.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 2003;41:582–92. 10.1097/01.MLR.0000062554.74615.4C [DOI] [PubMed] [Google Scholar]
- 120.Castellini G, Nielsen EE, Gluud C. Comment on: "cell therapy for heart disease: trial sequential analyses of two cochrane reviews". Clin Pharmacol Ther 2017;102:21–4. 10.1002/cpt.536 [DOI] [PubMed] [Google Scholar]
- 121.Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol 2000;53:1119–29. 10.1016/s0895-4356(00)00242-0 [DOI] [PubMed] [Google Scholar]
- 123.Mavridis D, Salanti G. How to assess publication bias: funnel plot, trim-and-fill method and selection models. Evid Based Ment Health 2014;17:30. 10.1136/eb-2013-101699 [DOI] [PubMed] [Google Scholar]
- 124.Guyatt G, Oxman AD, Akl EA, et al. Grade guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383–94. 10.1016/j.jclinepi.2010.04.026 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-065304supp001.pdf (137.1KB, pdf)
bmjopen-2022-065304supp002.pdf (82.2KB, pdf)


