Abstract
Objective: To analyze the correlation between self-rated treatment effect and diagnosis and treatment of elderly indigent cataract patients in rural areas of Ganzi Prefecture. Methods: In this retrospective study, senior cataract patients admitted in the Ganzi region from March 2018 to November 2021 were included. 495 indigent patients were classified into the poor group, including 400 cases who received surgical treatment and 95 who did not. The 318 patients that were not indigent were classified as the non-poor group. The basic demographic characteristics, treatment, self-assessed treatment effect, and the cost of surgery, blindness rate, and disability rate were compared between the two groups. The correlation between self-assessed treatment effect and treatment condition of patients in the poor group was analyzed by multi-factor unconditional logistic regression. Results: There were no significant differences in the basic demographic characteristics, self-assessed treatment effect, or postoperative blindness rate between the patients receiving surgery in both groups (P>0.05). The visual acuity of 400 patients after the operation was significantly higher than that before operation (P<0.05). The operation and other costs in the poor group were lower than those of the non-poor group (P<0.05). The elimination rate of disability in the non-poor group was significantly higher than in the poor group (P<0.05). Multivariate regression analysis showed that the level of the hospital, the location of the treatment institution, living alone, education level, and the number of visits were factors affecting the self-rated treatment effect of patients (P<0.05). Conclusion: The self-rated treatment effect of elderly indigent cataract in rural Ganzi Prefecture was closely related to the level of the hospital, the location of treatment institutions, living alone, education level, and the number of visits. Health poverty alleviation programs should be strengthened.
Keywords: Advanced age, countryside, poverty, cataract, self-evaluation of treatment effect, diagnosis and treatment
Introduction
Cataract is the most common blinding eye disease in the world, and the World Health Organization reports that the number of people blinded by cataract is about 20 million worldwide, with a higher incidence in low-income countries and a year-on-year increase. It is expected that the number of blind people may reach 50 million by 2050 [1,2]. In recent years, the burden of cataract disease in China has been growing rapidly, with data from the Chinese Medical Association’s Ophthalmology Branch showing that the prevalence of cataract among those aged 60 to 89 years is about 80%, and that among the population of 90 years old or above is as high as 90%. Cataract is also the number one eye disease causing blindness in China, with 66.9% (about 3.6 million) of the approximately 5.4 million people aged 50 years or older who are blind in China having cataract(s) [3]. The prevalence of and blindness rate caused by cataract in rural lowland areas of China is higher than that in urban areas, especially for cataract patients from poor families who are less able to obtain timely treatment due to financial constraints, increasing the blindness rate and therefore causing poverty and returning to poverty due to the disease, increasing the public health burden and economic pressure on families and society [4]. With the promotion of the Chinese health poverty alleviation project, and the development of the “Brightness Poverty Alleviation Project” and other related projects in the Ganzi region, treatment has been expanded for cataract patients in rural poor areas. Paying attention to the consultation behavior and treatment outcomes of rural elderly poor cataract patients enables their motivation to escape from poverty and prevents returning to poverty due to this disease. It is noted that subjective health self-assessment is considered by several scholars as a validated and robust health assessment with high reliability and validity, that can effectively reflect efficient and comprehensive indicators of individual’s health status, and can be regarded as an indicator to evaluate post-treatment quality of life and prognosis in cataract patients [5,6]. However, there are insufficient data on the self-assessment of treatment outcome in cataract patients and a lack of multi-center large sample related studies. In this study, we focused on this evaluation index of self-assessment of treatment outcome by analyzing regional data to explore the relationship between self-assessment of treatment outcome and treatment of poor elderly cataract patients in the Ganzi region, to provide a reference for future cataract health poverty governance.
Data and methods
Study subjects
A retrospective study was conducted in elderly cataract patients admitted in Ganzi Prefecture from March 2018 to November 2021. 495 rural patients with documented indigent economic condition were classified as the poor group, including 400 who received surgical treatment and 95 who did not. Another 318 non-poor patients were classified as the non-poor group. The poor population was defined as the registered households receiving relief fund (hereinafter referred to as “minimum living security”) in the Civil Affairs Department. The people who do not enjoy the minimum living allowance were regarded as non-poor people. This study was approved by the Ethics Committee of Chengdu Fifth People’s Hospital.
Inclusion criteria for the poor group
(1) Patients met the diagnostic criteria in American Clinical Guidelines for Ophthalmology [7]. (2) Patients with clear consciousness. (3) Patients with complete clinical information. (4) Patients with an age of ≥80 years.
Exclusion criteria for the poor group
(1) Those with organic disease and abnormal coagulation function. (2) Contraindications to surgery. (3) Ophthalmic diseases other than cataract that cause vision loss. (4) History of previous eye surgery. (5) Abnormal cognitive function, mental illness, inability to express their feelings clearly.
Inclusion criteria for the non-poor group
(1) Patients meeting the diagnostic criteria for cataract disease in the Clinical Guidelines in Ophthalmology - 3rd Edition (American Academy of Ophthalmology) [7] with indications for surgery. (2) The patient was conscious and could communicate normally. (3) Patients with complete clinical profile. (4) Patients with an age ≥80 years.
Exclusion criteria for the non-poor group
(1) Those with organic disease and coagulation abnormalities. (2) Ophthalmic diseases other than cataract causing vision loss. (3) Those with a history of previous ocular surgery. (4) Those with traumatic eye disease, long-term eye medication, or macular and retinal pathology. (5) Those with abnormal cognitive function, mental illness or inability to express their feelings clearly.
Basic patient information
Based on the information in the visit records, basic demographic characteristics including patient’s gender, age, education level, residence status, and whether they had comorbid diseases were collected. Basic medical visit information were obtained including whether surgical treatment was performed, the level of the hospital visited, the location of the treatment institution, and the number of visits from March 2018 to November 2021.
Self-assessment of treatment outcome
Self-assessment of treatment effect was collected and archived before the patient’s discharge or at the end of treatment. Patients were asked to rate themselves according to their health and treatment statuses, with the corresponding options being “cured”, “improved”, “long-term rehabilitation”, “in treatment”, “death” (excluded in subsequent analyses). The above-mentioned indicators were self-ratings and changes that reflected the individual’s judgement and prediction of the severity of the disease and recovery, which cannot be evaluated by medical means. The aim of this study was to examine whether the condition had improved after the treatment, so the self-assessment results were classified into three variables and codes, including 0 for “cured”, 1 for “improved” and 3 for “long-term rehabilitation” and “in treatment”.
Effectiveness of surgical treatment
The preoperative and 1-week postoperative visual acuity of the surgically treated patients in the poor group was examined using the international common visual acuity scale; the elimination rate of blindness and the elimination rate of disability in the non-poor group were compared to those in the poor group. Surgical cost, including: total cost, medication cost, surgery cost, consumables, and examination fee, was recorded. Blindness elimination: postoperative visual acuity ≥0.5; disability elimination: postoperative visual acuity ≥0.3.
Control of confounding factors
Previous studies have reported age, gender, literacy, and occupation as factors affecting cataract treatment outcome [8,9], while age and literacy are closely related to cataract development [10], thus, the above factors were controlled for as confounding factors in this study. In the subjective self-assessment of treatment outcome, objective health status was also controlled to reduce bias in the results, as different objective health conditions have a significant effect on the degree of fundus lesions, which is not conducive to recovery of vision after treatment.
Statistical analysis
GraphPad Prism 9.0 was used for figure rendering, and SPSS 26 software was used for statistical analysis. The measured data conforming to normal distribution were expressed by mean ± SEM, independent sample t-test was used for comparison of measurement data between groups, and paired t-test was used for comparison within groups. Counted data were expressed using the number of cases/percentage (n/%), and were compared by χ2/Z test, and the continuity-corrected χ2 test was used when the theoretical frequency in the chi-square test was less than 5. Descriptive analyses of the basic demographic characteristics of the sample, treatment, and self-rated treatment effects were performed, and the χ2 test was used for univariate analysis of ordered variables. Multifactor logistic regression analysis model was used to adjust for confounding factors, and ordered multifactor unconditional logistic regression analysis was performed, with α = 0.05 as the test level.
Results
Basic demographic characteristics, treatment and self-assessed treatment effects of the poor group
The self-assessed cure and improvement rate of 495 patients in the poor group was 78.79%, of which 58.18% were seen in secondary hospitals, 80.61% were seen in the county, 400 (80.81%) had received cataract surgery and 81.41% had one visit from March 2018 to November 2021, the results are shown in Table 1.
Table 1.
Basic demographic characteristics, treatment, and self-assessed treatment effects of the poor group (n = 495)
| Variable | Number of cases (cases) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 232 | 46.87 |
| Female | 263 | 53.13 |
| Age (years) | ||
| 80-85 | 213 | 43.03 |
| 86-90 | 238 | 48.08 |
| 91-95 | 32 | 6.47 |
| ≥95 | 12 | 2.42 |
| Literacy | ||
| Illiterate or semi-literate | 187 | 37.77 |
| Elementary school | 221 | 44.65 |
| Junior high school and above | 87 | 17.58 |
| Living alone or not | ||
| Yes | 81 | 16.36 |
| No | 414 | 83.67 |
| Are you suffering from other diseases | ||
| Yes | 108 | 21.82 |
| No | 387 | 78.18 |
| Surgical treatment | ||
| Yes | 400 | 80.81 |
| No | 95 | 19.19 |
| Hospital level | ||
| Tertiary hospital | 86 | 17.37 |
| Level 2 hospital | 288 | 58.18 |
| Level 1 Hospital | 74 | 14.95 |
| Primary health institution | 47 | 9.50 |
| Place of treatment | ||
| Within the county | 399 | 80.61 |
| Outside the county | 96 | 19.39 |
| Number of visits from March 2018-November 2021 | ||
| 1 visit | 403 | 81.41 |
| 2 times | 83 | 16.77 |
| ≥3 times | 9 | 1.82 |
| Self-assessed treatment effect | ||
| Cured | 257 | 51.92 |
| Condition improved | 133 | 26.87 |
| Treatment required | 105 | 21.21 |
Comparison of the results of cataract surgery and treatment for patients in the poor group
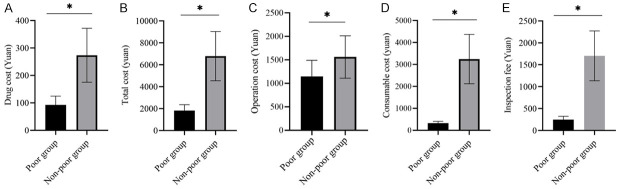
All 400 surgically treated patients in the poor group had significantly higher visual acuity 1 week after surgery than before surgery (all P<0.05), see Table 2 and Figure 1.
Table 2.
Comparison of the results of cataract surgery and treatment in the poor group (n = 400)
| Time | Visual acuity <0.05 | 0.05≤ Visual acuity <0.3 | 0.3≤ Visual acuity <0.5 | Visual acuity ≥0.05 |
|---|---|---|---|---|
| Pre-operative | 238 (59.50) | 133 (33.25) | 20 (5.00) | 9 (2.25) |
| 1 week after surgery | 14 (3.50) | 57 (14.25) | 34 (8.50) | 295 (73.75) |
| Z | 502.206 | |||
| P | <0.001 | |||
Figure 1.
Comparison of cataract surgical treatment outcome in the poor group (*P<0.05).
Comparison of basic demographic characteristics, treatment and self-assessed treatment effects between two groups
There was no significant difference in general data between the poor group (only surgical patients) and the non-poor group (P>0.05), as shown in Table 3.
Table 3.
Comparison of basic demographic characteristics, treatment and self-assessed treatment effects between the two groups
| General data | Poor group (n = 400) | Non-poor group (n = 318) | χ2 | P |
|---|---|---|---|---|
| Gender | ||||
| Male (n, %) | 186 (46.50) | 134 (42.14) | 1.364 | 0.243 |
| Female (n, %) | 214 (53.50) | 184 (57.86) | ||
| Age (years old) | 85.96±3.99 | 85.56±3.71 | 1.376 | 0.169 |
| Degree of education | ||||
| Illiterate or semi-illiterate | 150 (37.50) | 94 (29.56) | 5.572 | 5.572 |
| Primary school | 181 (45.25) | 155 (48.74) | ||
| Junior high school and above | 69 (17.25) | 69 (21.70) | ||
| Other disease | ||||
| Hypertension | 25 (6.25) | 20 (6.29) | 0.018 | 0.894 |
| Diabetes | 18 (4.50) | 14 (4.40) | 0.004 | 0.950 |
| Hyperlipidemia | 21 (5.25) | 15 (4.72) | 0.274 | 0.600 |
| Coronary heart disease | 16 (4.00) | 19 (5.97) | 1.490 | 0.222 |
| Rheumatoid arthritis | 1 (0.25) | 2 (0.63) | 0.611 | 0.434 |
| Serious mental disorder | 1 (0.25) | 0 (0.00) | 0.796 | 0.372 |
| Residence | ||||
| Live with family | 335 (83.75) | 276 (86.79) | 1.293 | 0.255 |
| Live alone | 65 (16.25) | 42 (13.21) | ||
| Hospital level | ||||
| First-level | 61 (15.25) | 39 (12.26) | 6.434 | 0.092 |
| Second-level | 234 (58.50) | 215 (67.61) | ||
| Third-level | 66 (16.50) | 42 (13.21) | ||
| Primary health centers | 39 (9.75) | 22 (6.92) | ||
| Territory of treatment institution | ||||
| Within the county | 322 (80.50) | 241 (75.79) | 2.326 | 0.127 |
| County extraterritorial | 78 (19.50) | 77 (24.21) | ||
| Number of visits from March 2018 to November 2021 | ||||
| Once | 326 (81.50) | 256 (80.50) | 10.793 | 0.05 |
| Twice | 69 (17.25) | 45 (14.15) | ||
| More than twice | 5 (1.25) | 17 (5.35) | ||
| Self-assessment of therapeutic effect | ||||
| Cure | 207 (51.75) | 187 (58.80) | 4.550 | 0.103 |
| Be better | 110 (27.50) | 82 (25.79) | ||
| Need treatment | 83 (20.75) | 49 (15.41) |
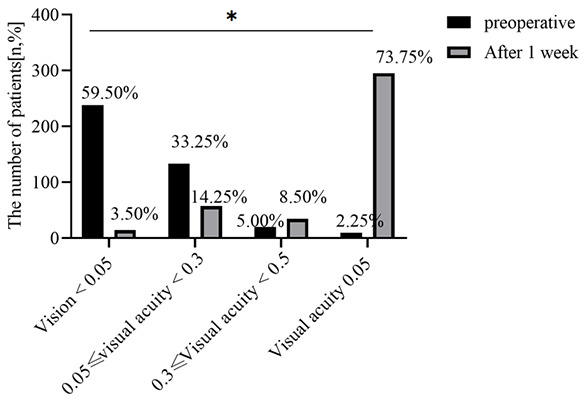
Analysis of the cost of cataract surgery in the two groups
The cost of surgery and other costs were lower in the poor group than in the non-poor group (all P<0.05), as shown in Table 4 and Figure 2.
Table 4.
Analysis of cataract surgery costs for patients in the two groups (Yuan)
| Group | Number of cases | Total Costs | Drugs | Surgical Fees | Consumables | Examination Fees |
|---|---|---|---|---|---|---|
| Poor group | 400 | 1804.6±508.1 | 93.8±32.4 | 1150.2±342.5 | 320.8±86.3 | 249.7±75.8 |
| Non-poor group | 318 | 6484.4±3641.3 | 288.8±140.2 | 1503.1±479.9 | 3090.0±1972.9 | 1752.1±1067.1 |
| t | 25.399 | 26.931 | 11.482 | 28.043 | 28.216 | |
| P | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Figure 2.
Analysis of cataract surgery cost between the two groups (*P<0.05). A. The comparison of drug cost; B. The comparison of Total cost; C. The comparison of Operation cost; D. The comparison of Consumable cost; E. The comparison of Inspection fee.
Comparison of the elimination rate of blindness and elimination rate of disability between the two groups
There was no statistical difference in the elimination rate of blindness between the poor group and the non-poor group (P>0.05); the elimination rate of disability in the non-poor group was significantly higher than that of the poor group (P<0.05), as shown in Table 5.
Table 5.
Comparison of elimination rate of blindness and elimination rate of disability between the two groups [n (%)]
| Group | Number of cases | Elimination rate of blindness | Elimination rate of disability |
|---|---|---|---|
| Poor group | 400 | 295 (73.75) | 386 (86.50) |
| Non-poor group | 318 | 251 (78.93) | 296 (93.08) |
| χ2 | - | 2.610 | 7.268 |
| P | - | 0.106 | 0.007 |
Univariate analysis of factors affecting self-rated treatment outcomes in patients of poor group
The univariate analysis showed that differences in education level, whether they lived alone, whether they suffered from other diseases, the level of the hospital visited, the territory of the treatment institution, and the number of visits from March 2018 to November 2021 were significant among the patients who were cured, improved, or needed treatment in the self-assessed treatment effect (all P<0.05); while the differences in other variables were not significant among the patients with different self-assessed outcomes (all P>0.05), see Table 6.
Table 6.
Univariate analysis of self-rated treatment outcomes of cataract patients in the poor group
| Variable | Cured (n = 257) | Condition improved (n = 133) | Treatment required (n = 105) | χ2 | P |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 121 (24.44) | 62 (12.53) | 49 (9.89) | 0.009 | 0.995 |
| Female | 136 (27.47) | 71 (14.34) | 56 (11.31) | ||
| Age (years) | |||||
| 80-85 | 116 (23.43) | 53 (10.71) | 44 (8.89) | 11.875 | 0.064 |
| 86-90 | 128 (25.86) | 64 (12.93) | 46 (9.29) | ||
| 91-95 | 10 (2.02) | 12 (2.42) | 10 (2.02) | ||
| ≥95 | 3 (1.02) | 4 (0.81) | 5 (1.01) | ||
| Literacy | |||||
| Illiterate or semi-literate | 56 (11.31) | 33 (6.67) | 98 (19.79) | 183.946 | <0.001 |
| Elementary school | 154 (31.11) | 62 (12.53) | 5 (1.01) | ||
| Junior high school and above | 47 (9.49) | 38 (7.68) | 2 (0.40) | ||
| Living alone or not | |||||
| Yes | 19 (3.39) | 15 (11.29) | 47 (44.76) | 79.497 | <0.001 |
| No | 238 (4.08) | 118 (23.84) | 58 (11.72) | ||
| Are you suffering from other diseases | |||||
| Yes | 43 (8.69) | 19 (3.84) | 46 (9.29) | 38.091 | <0.001 |
| No | 214 (43.23) | 114 (23.03) | 59 (11.92) | ||
| Is surgical treatment | |||||
| Yes | 207 (41.82) | 110 (22.22) | 83 (16.77) | 0.530 | 0.767 |
| No | 50 (10.10) | 23 (4.65) | 22 (4.44) | ||
| Hospital level | |||||
| Tertiary hospital | 26 (5.25) | 32 (6.46) | 28 (5.66) | 62.846 | <0.001 |
| Level 2 hospital | 189 (38.18) | 60 (12.12) | 39 (7.88) | ||
| Level 1 Hospital | 32 (6.46) | 25 (5.05) | 17 (3.43) | ||
| Primary health institution | 10 (2.02) | 16 (3.23) | 21 (4.24) | ||
| Place of treatment | |||||
| Within the county | 208 (42.02) | 94 (18.99) | 97 (19.60) | 17.718 | <0.001 |
| Outside the county | 49 (9.90) | 39 (7.88) | 8 (1.62) | ||
| Number of visits from March 2018-November 2021 | |||||
| 1 visit | 239 (48.28) | 122 (24.65) | 42 (8.48) | 151.695 | <0.001 |
| 2 times | 17 (3.43) | 9 (1.82) | 57 (11.52) | ||
| ≥3 times | 1 (0.20) | 2 (0.40) | 6 (1.21) |
Multi-factor unconditional logistic regression analysis of factors affecting self-rated treatment outcomes of cataract patients in the poor group
Using the self-rated treatment effect as the dependent variable (need to continue treatment = 0, improved = 1, cured = 2), the multi-factor regression analysis showed that the level of the hospital visited, the location of the treatment facility, whether the patient lived alone, the level of education, and the number of visits were important factors affecting the patients’ self-rated treatment outcomes (all P<0.05), as shown in Table 7.
Table 7.
Multi-factor unconditional logistic regression analysis of self-rated treatment outcomes of cataract patients in the poor group (n = 495)
| Variable | Estimated Value | Standard error | Wald chi-square | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| Educational level | ||||||
| Illiterate or semi-literate | 1.00 | |||||
| Primary school | 0.983 | 0.283 | 12.065 | 0.001 | 2.672 | 1.535-4.654 |
| Junior high school and above | 1.023 | 0.358 | 8.166 | 0.004 | 2.782 | 1.379-5.611 |
| Live alone | ||||||
| Yes | 0.923 | 0.213 | 18.778 | 0.000 | 2.517 | 1.658-3.821 |
| no | 1.00 | |||||
| Have other diseases | ||||||
| Yes | 0.234 | 0.316 | 0.548 | 0.459 | 1.264 | 0.680-2.348 |
| no | 1.00 | |||||
| Hospital level | ||||||
| Tertiary hospital | 1.00 | |||||
| Secondary hospital | 1.092 | 0.183 | 35.608 | 0.000 | 2.980 | 2.082-4.266 |
| First class hospital | 0.984 | 0.219 | 20.188 | 0.000 | 2.675 | 1.742-4.109 |
| Primary health institutions | 0.832 | 0.217 | 14.700 | 0.000 | 2.298 | 1.502-3.516 |
| Territory of treatment facility | ||||||
| within the county | 1.00 | |||||
| Outside the county | 0.983 | 0.183 | 28.854 | 0.000 | 2.672 | 1.867-3.825 |
| Number of visits from March 2018 to November 2021 | ||||||
| 1 time | 1.00 | |||||
| 2 times | 1.293 | 0.472 | 7.504 | 0.006 | 3.644 | 1.445-9.190 |
| ≥3 times | 1.182 | 0.231 | 26.182 | 0.000 | 3.261 | 2.074-5.128 |
Discussion
Cataract is the most common blindness-causing eye disease in China, and most of the patients from poor families cannot be treated in time due to economic constraints. Recently, with the implementation of the “Brightness Poverty Alleviation Project” in China, a large number of cataract patients are being treated in the Ganzi area every year. Authoritative data on their treatment effect, visual acuity change, and complications are uncertain. The subjective perception and evaluation of cataract patients on the treatment and rehabilitation effects are crucial, and the current relevant studies in this area focus on national or characteristic diseases and lack regional representative studies, so this study investigated the self-assessed treatment effects of rural senior cataract patients in the Ganzi area.
In this study, the consultation rate in secondary hospitals was 58.18%, and the consultation rate in the county was 80.61%. 400 cases (80.81%) had received cataract surgery, and the number of consultations of 1 from March 2018 to November 2021 accounted for 81.41%. Rural elderly cataract patients who were indigent were mainly in secondary hospitals and basically completed the consultation and treatment in the county. The reasons for this are mainly due to the lack of financial support, transportation, and disease awareness among those population, which affects their choice of medical treatment when facing major diseases, as described by Hashemi and Belda et al. [11,12]. At the same time, the aforementioned access is also closely related to the preferential policies for access to health care in the Ganzi region under the health poverty alleviation project. Surgery is currently recognized as the preferred treatment option for cataract, and surgical treatment for patients who meet the surgical indications can save vision and reduce the blindness rate. Atik et al. showed that more frequent treatment visits in a certain time period correlated with a more difficult treatment and slower recovery [13]. In the present study, all 400 surgically treated patients had significantly higher visual acuity 1 week after surgery than before surgery (all P<0.05), and there was no statistical difference in the elimination rate of blindness between the poor and non-poor groups (P>0.05). The elimination rate of disability in the non-poor group (93.08%) was significantly higher than that of the poor group (86.50%) (P<0.05), which was slightly lower than that of cataract patients in previous studies who received surgery. However, the study also reflected that the effect of the “Brightness and Poverty Alleviation Project” on the treatment of elderly cataract patients in rural areas was improved, which verified the above analysis that patients with surgical treatment had better postoperative recovery. The decrease in the postoperative detachment rate may be related to the cost of medical care, and the high cost of medical care reflects the high quality of medical services provided to patients [14,15]. In this study, surgical and other costs were lower in the poor group than in the non-poor group (all P<0.05), suggesting that higher medical costs in non-poor cataract surgery patients resulted in greater marginal health gains.
Individual subjective health self-assessment is a robust health measure, that can be used as a predictor of a patient’s prognosis and quality of life [16]. In this study, we found that the self-assessed cure and improvement rate of 495 patients was 78.79%, which was lower than the self-assessed cure and improvement rate of 90.0% reported by Cui et al. [17] in rural poor cataract patients aged ≥60 years. The reasons may be related to the age of the patients in this study being advanced (≥80 years old) and the Ganzi region being a high-altitude area, where cataract occurs 5-10 years earlier compared to inland areas due to the effects of hypoxia and strong radiation [18]. Cataract patients have declining organ function with age, decreasing corneal endothelial number, cellular status and function, and increasing sensitivity to therapeutic damage, thus affecting patients’ self-assessed treatment outcome [19].
Age, gender, literacy, and occupation were found to be risk factors affecting the treatment outcome of cataract patients [20]. In the present study, multi-factor regression analysis showed that the level of the hospital visited, the place of origin of the treatment facility, whether the patient lived alone or not, the level of education, and the number of visits were significant factors influencing the self-rated treatment outcome of patients (all P<0.05). Age and gender were not related to the self-rated treatment outcome of elderly poor cataract patients in rural Ganzi area. This might be becauseolder age did not have a significant effect on self-perception. In terms of consultation, hospital level, and structural affiliation influenced patients’ self-rated treatment outcome, which may be related to the better care rendered by by high-level hospitals. It was found that patients with out-of-county medical visits tended to have better self-rated treatment outcomes due to the spatial feasibility and economic conditions of their health service utilization [21]. However, the vast majority of rural elderly cataract patients with poor financial condition stay in county for treatment, as cataract patients in poor rural areas have lower demand for medical care and less medical awareness. Patients who live alone have poor self-rated treatment outcomes, while non-solitary patients can enjoy family care after treatment, receive family support, and improve their treatment-cooperative behavior to promote recovery. The education level is closely related to the self-assessed treatment effect, and the self-assessed treatment effect decreases in those with higher level of education, probably due to the differences in the perceived ability of this group of elderly people because they have more correct knowledge of the disease and have higher requirements for recovery [22]. In terms of the number of treatments, the difficulty of treatment and the increase in the number of visits during treatment, as analyzed in the previous paper, were not conducive to the evaluation of the self-assessed treatment effect of patients.
Conclusion
The surgical treatment of cataract better restored vision. The cost of surgery and other costs decreased significantly after state support. The rate of disability removal increased, and the self-assessed treatment outcome of rural elderly indigent cataract patients in Ganzi was closely related to the level of the hospital visited, the location of the treatment institution, whether they lived alone, their education level, the number of visits, and other treatment conditions. This study is important for promoting the “Brightness and Poverty Alleviation Project” and providing health care protection in poor rural areas of Ganzi. However, there are some shortcomings in this study: first, there are many poor areas in Ganzi, and senior cataract patients are generally not well educated, so the outcome variable of patients’ competent treatment may have some bias. Second, the data of patients’ socio-economic variables were not collected at the time of consultation, so there may be confounding factors missed in this study. These shortcomings remain to be further studied in the future.
Disclosure of conflict of interest
None.
References
- 1.Delbarre M, Froussart-Maille F. Signs, symptoms, and clinical forms of cataract in adults. J Fr Ophtalmol. 2020;43:653–659. doi: 10.1016/j.jfo.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 2.Thevi T, Abas AL. Cataract surgery incidence trends in a tertiary public hospital in Malaysia. Kathmandu Univ Med J (KUMJ) 2019;17:101–106. [PubMed] [Google Scholar]
- 3.Hashemi H, Asharlous A, Yekta A, Aghamirsalim M, Nabovati P, Sadoughi MM, Khabazkhoob M. Astigmatism profile in the elderly population: Tehran Geriatric Eye Study. Jpn J Ophthalmol. 2022;66:461–473. doi: 10.1007/s10384-022-00936-x. [DOI] [PubMed] [Google Scholar]
- 4.Clausen T, Romøren TI, Ferreira M, Kristensen P, Ingstad B, Holmboe-Ottesen G. Chronic diseases and health inequalities in older persons in Botswana (southern Africa): a national survey. J Nutr Health Aging. 2005;9:455–461. [PubMed] [Google Scholar]
- 5.Ruiz-Algueró M, Hernando V, Marcos H, Gutiérrez G, Pérez-Elías MJ, López-Bernaldo de Quirós JC, Pulido F, Górgolas M, Sanz J, Suarez-García I, Fernandez MT, Losa JE, Pérez JL, Ladrero MO, Prieto MA, González G, Izquierdo A, Viloria LJ, López I, Martínez E, Castrillejo D, Aranguren R, Belmonte MA, Aranda-García IV, Arraiza A, Diaz A Hospital Survey Study Group. Self-rated health among people living with HIV in Spain in 2019: a cross-sectional study. BMC Infect Dis. 2021;21:129. doi: 10.1186/s12879-021-05815-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Willadsen TG, Siersma V, Nielsen ABS, Køster-Rasmussen R, Guassora AD, Jarbøl DE, Eusebi P, Malterud K, Reventlow S, de Fine Olivarius N. The effect of structured personal care on diabetes symptoms and self-rated health over 14 years after diabetes diagnosis. Prim Care Diabetes. 2018;12:354–363. doi: 10.1016/j.pcd.2018.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Miller KM, Oetting TA, Tweeten JP, Carter K, Lee BS, Lin S, Nanji AA, Shorstein NH, Musch DC American Academy of Ophthalmology Preferred Practice Pattern Cataract/Anterior Segment Panel. Cataract in the adult eye preferred practice pattern. Ophthalmology. 2022;129:P1–P126. doi: 10.1016/j.ophtha.2021.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Ang MJ, Afshari NA. Cataract and systemic disease: a review. Clin Exp Ophthalmol. 2021;49:118–127. doi: 10.1111/ceo.13892. [DOI] [PubMed] [Google Scholar]
- 9.Hugosson M, Ekström C. Prevalence and risk factors for age-related cataract in Sweden. Ups J Med Sci. 2020;125:311–315. doi: 10.1080/03009734.2020.1802375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olusanya BA, Ugalahi MO, Adeyemo AO, Baiyeroju AM. Age at detection and age at presentation of childhood cataract at a tertiary facility in Ibadan, Southwest Nigeria. BMC Ophthalmol. 2020;20:38. doi: 10.1186/s12886-020-1323-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hashemi H, Pakzad R, Khabazkhoob M. Decomposition of economic inequality in cataract surgery using Oaxaca blinder decomposition: Tehran Geriatric Eye Study (TGES) Ophthalmic Epidemiol. 2022;29:401–410. doi: 10.1080/09286586.2021.1946827. [DOI] [PubMed] [Google Scholar]
- 12.Belda JI, Placeres J, Elvira JC, Puig X, Pérez-Vives C, Zou M, Sun S, Yu J, O’Boyle D. Costs and healthcare resource utilization associated with posterior capsule opacification after cataract surgery with five different intraocular lenses: an economic analysis for Spain. Clin Ophthalmol. 2022;16:993–1001. doi: 10.2147/OPTH.S349003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atik A, Rhodes LA, Samuels BC, Mennemeyer ST, Girkin CA. Cost utility of Schlemm’s canal microstent injection with cataract surgery for open-angle glaucoma in the US medicare system. J Glaucoma. 2022;31:413–422. doi: 10.1097/IJG.0000000000001993. [DOI] [PubMed] [Google Scholar]
- 14.Do VQ, McCluskey P, Palagyi A, White A, Stapleton FJ, Carnt N, Keay L. Patient perspectives of cataract surgery: protocol and baseline findings of a cohort study. Clin Exp Optom. 2018;101:732–739. doi: 10.1111/cxo.12686. [DOI] [PubMed] [Google Scholar]
- 15.Fang Z, Chen XY, Lou LX, Yao K. Socio-economic disparity in visual impairment from cataract. Int J Ophthalmol. 2021;14:1310–1314. doi: 10.18240/ijo.2021.09.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu Q, Jin Y, Wang Y, Feng J, Qiao X, Ji L, Si H, Bian Y, Wang W, Yu J, Wang C. Association between self-efficacy and self-management behaviours among individuals at high risk for stroke: social support acting as a mediator. J Clin Nurs. 2023;32:71–82. doi: 10.1111/jocn.16191. [DOI] [PubMed] [Google Scholar]
- 17.Cui NN, Zhang YL, Chen JP, Zhang L. Correlation between hospital visit and self-rated treatment effect among rural poor elderly cataract patients. Chinese Journal of Public Health. 2022;38:385–389. [Google Scholar]
- 18.Garrigan H, Ifantides C, Prashanthi GS, Das AV. Biogeographical and altitudinal distribution of cataract: a nine-year experience using electronic medical record-driven big data analytics in India. Ophthalmic Epidemiol. 2021;28:392–399. doi: 10.1080/09286586.2020.1849741. [DOI] [PubMed] [Google Scholar]
- 19.Pahor D, Gracner T. Cataract surgery in very old patients. Klin Monbl Augenheilkd. 2020;237:938–942. doi: 10.1055/a-0917-6966. [DOI] [PubMed] [Google Scholar]
- 20.Chen X, Zhou DY, Shen J, Wu YB, Sun QZ, Dong JM, Yu JC. Prevalence and risk factors on age-related cataract and surgery in adults over 50 years old in Binhu District, Wuxi, China. Int J Ophthalmol. 2020;13:445–451. doi: 10.18240/ijo.2020.03.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Z, Liu C, Chen Z. Prevalence and age-related changes of corneal astigmatism in patients undergoing cataract surgery in northern China. J Ophthalmol. 2020;2020:6385098. doi: 10.1155/2020/6385098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marmamula S, Boopalan D, Khanna RC, Hassija N, Keeffe J. Awareness of cataract and glaucoma in two rural districts of Telangana, India. Indian J Ophthalmol. 2022;70:982–987. doi: 10.4103/ijo.IJO_977_21. [DOI] [PMC free article] [PubMed] [Google Scholar]