Abstract
Background:
An ambulatory transition of care program, including a pharmacist-provided comprehensive medication review (CMR), was implemented.
Objectives:
The objectives were to: (1) compare 30-day hospital readmission rates between those who received the pharmacist CMR versus eligible patients not scheduled, (2) describe identified problems and recommendations, and (3) quantify recommendation acceptance rates.
Methods:
A retrospective cohort study was conducted between March and October 2016. Inclusion criteria were: LACE score of ≥13, established Michigan Medicine primary care, and discharged from specific inpatient services to home. The primary outcome was 30-day hospital readmission rates. Pharmacist-identified problems, recommendations, and recommendation acceptance rates were examined. χ2 analysis and descriptive statistics were used.
Results:
355 discharges met inclusion criteria and pharmacists provided CMRs for 159 patients. The average age was 60 years (standard deviation [SD]: 14.3), the majority were female (54%), and white/Caucasian (69%). There was no significant difference in 30-day readmission rates in patients who received a CMR (p = .96). A mean of 3.1 problems were identified per visit (SD: 1.8, range: 1–10). 509 recommendations were provided and approximately 50% were provider accepted.
Conclusions:
Reduced readmission rates were not observed; however, pharmacists identified many areas for intervention in highest risk patients during the transition from hospital to home.
Keywords: care transitions, comprehensive medication review, readmissions, ambulatory care pharmacy, LACE risk tool
Introduction
Transitions of care are defined by The Joint Commission (TJC) as the “movement of patients between health-care practitioners, settings and home as their condition and care needs change.”1 Patient movement and transitions between settings of care leads to opportunities for discrepancies to occur. Ineffective care transitions can lead to adverse events, increased health-care costs, and increased readmissions. Forster and colleagues found that approximately 1 in 5 patients experienced an adverse event in Ontario (Canada) within 5 weeks of hospital discharge. Of those, approximately 66% were medication-related and approximately 30% were preventable.2 Readmissions place burden on patients and their families but are also a burden to the health-care system due to the associated increased health-care costs. In the United States in 2011, approximately 3.3 million all-cause adult hospital readmissions accounted for over 40 billion dollars in health-care costs from all payers with over 20 billion from Medicare alone.3 In 2014, the estimated mean cost per inpatient hospitalization was about US$11 000.4
In order to improve transitions of care, the root causes behind why errors occur during transitional periods should be addressed. The 3 core concerns associated with transitions of care are inadequate communication among providers, patients, and caregivers; lack of patient education; and lack of provider accountability for patient care.1 Improving care transitions became a national health-care priority under the Affordable Care Act in 2012. At that time, TJC established a 3-year initiative to improve effectiveness of transitions of care and the Centers for Medicare and Medicaid Services (CMS) started the hospital readmission reduction program. As a result of these initiatives, health-care institutions are held fiscally responsible if they fail to meet the standards outlined by the programs.5 Although these initiatives began over 5 years ago in an effort to reduce readmission rates, providing optimal transitions of care services remain a challenge in health-care today. Analysis of CMS data by Kaiser Health News reveals that for fiscal year 2018 alone, over 2500 hospitals in the United States will be subject to CMS penalties totaling approximately US$528 million as a result of hospital readmissions.6
Health-care systems have incorporated many strategies to improve transitions of care and address high readmission rates. In order to improve readmission rates as an institution, it is crucial to identify patients who may benefit most from dedicated transition of care services. The LACE risk stratification tool is one example of a scoring tool that can be utilized to identify at-risk patients.7 The LACE tool has been derived and validated to prospectively identify patients at risk for readmission or death within 30 days of hospital discharge.7 The LACE score is calculated using 4 criteria related to the patient and the associated hospital encounter. These criteria are: length of stay (L), acuity of hospitalization (A), comorbidities (C), and emergency department (ED) visits within the past 6 months (E). The LACE scoring tool ranges from 1 (lowest) to 19 (highest) risk and scores of 10 and above are associated with high risk of readmission or death within 30 days.7
Well-structured multidisciplinary transition of care programs support the provision of comprehensive services for high-risk patients. Pharmacists are equipped to provide comprehensive medication reviews (CMRs), identify and recommend solutions for medication-related problems (MRPs), counsel patients, and assess adherence.8 Many transition of care services utilize telephone consultations to improve access during the transition period. Patient-centered medical home ambulatory care pharmacist involvement in transition of care services has demonstrated a positive impact on patient outcomes.9–12 Stranges and colleagues evaluated a multidisciplinary telephone-based transition of care service within the Michigan Medicine geriatric population, which included the use of a patient-centered medical home ambulatory care pharmacist-provided CMR.11 Patients who received the multidisciplinary transition of care service experienced significantly lower readmission rates versus those who did not receive the entire transition of care service (10.6% and 21.1%; P < .001).11
In order to address 30-day hospital readmissions, Michigan Medicine (a level-1 trauma, academic medical center located in Michigan) launched a system-wide LACE transition of care program in February 2016 to target highest risk patients identified by the LACE risk stratification tool. This initiative included components while patients remained in the hospital and continued after discharge in the ambulatory setting. The LACE transition of care program consisted of a phased implementation, first targeting patients with a LACE score of 13 and above followed by expansion to patients with a LACE score of 10 and above. In the ambulatory setting, the LACE transition of care program included a triad of 3 specific components: a care navigator phone call within 2 business days, a centralized transition of care pharmacist phone CMR visit within 3 to 7 days, and a postdischarge follow-up visit with a provider from the patient’s primary care office within 7 days, as depicted in Figure 1. The pharmacist and primary care provider (PCP) appointments were scheduled via inpatient clinical assistants prior to the patient’s discharge from the hospital. This study evaluated the pilot central transition of care clinical pharmacy program as part of the LACE transition of care initiative. In this program, ambulatory care pharmacists conducted a medication history, performed medication reconciliation, assessed medical stability, completed a CMR, and documented recommendations for providers.
Figure 1.
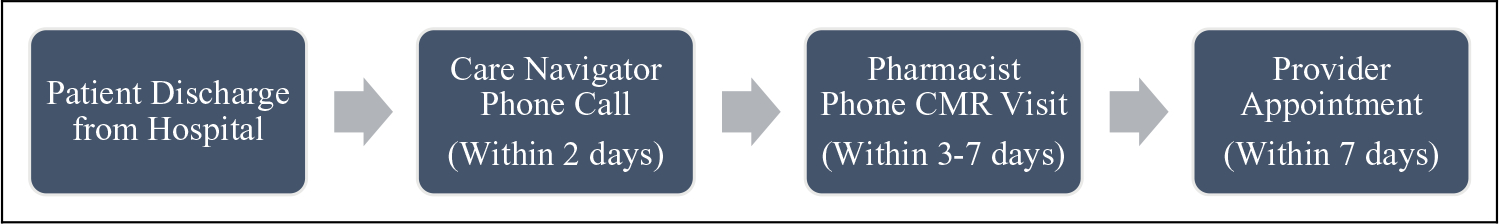
Ambulatory LACE transition of care components. CMR = Comprehensive Medication Review.
The objectives of this evaluation were to (1) compare 30-day hospital readmission rates between those who receive a transition of care CMR with a pharmacist and those not scheduled for a CMR, (2) describe the pharmacist-identified problems during the CMR and their recommendations to resolve these problems identified during the CMR, and (3) quantify the acceptance rate of these recommendations by a PCP and the patient. We hypothesized that patients who received a transition of care CMR with a pharmacist would have lower 30-day readmission rates than those who did not receive this service.
Methods
A retrospective cohort study was conducted using an electronic medical record (EMR) review. The time frame of records reviewed was March to October 2016. Patient inclusion criteria included a LACE score of 13 and greater upon discharge, established primary care within Michigan Medicine patient-centered medical homes, care provided by specific inpatient general or family medicine services, and discharged to home. A list of eligible patients was maintained by the lead transition of care clinical pharmacist.
Data collected included: patient demographics, information from the transition of care program, pharmacist identified health and MRPs, pharmacist recommendations to resolve problems, acceptance of recommendations by providers or patients, health-care utilization and internal readmissions within 30 days. MRPs were based upon validated categories and additional categories were identified through piloting the data collection tool. The tool was revised for clarity after repeated pilot tests.13 The final data collection tool for abstracting MRPs and pharmacist recommendations is included in Online Appendix.
Training for data collection was conducted to ensure consistency and accuracy in the data collection process. Recommendations and MRPs coded as “Other” were reviewed by 2 study team members and recategorized when possible. Consensus around new categories created and recoding of the “Other” responses was reached with 5 study team members. All study data were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at the University of Michigan.14 REDCap is a secure, web-based application designed to support data capture for research studies, providing (1) an intuitive interface for validated data entry, (2) audit trails for tracking data manipulation and export procedures, (3) automated export procedures for seamless data downloads to common statistical packages, and (4) procedures for importing data from external sources.
Data Analysis
Descriptive statistics were used. χ2 analysis was used to compare internal 30-day readmission rates between patients who received the pharmacist CMR and eligible patients not scheduled. Medication and health-related problems identified, pharmacist recommendations, and acceptance of pharmacist recommendations by patients and providers were described. All analyses were conducted at the visit level. This study was approved by the institutional review board of University of Michigan (HUM00120101). SAS version 9.4 (SAS Institute Inc, Cary, North Carolina) was used for data analysis.
Results
A total of 355 hospital discharges met inclusion criteria. Of these, 216 discharges had an appointment scheduled with a central transition of care pharmacist, and 159 CMR calls (73.6%) were completed. Reasons for noncompletion of scheduled CMR calls include: unable to reach patient after 3 attempts (n = 26), patient canceled appointment (n = 6), patient refused (n = 5), phone disconnected (n = 2), and other (n = 18). The comparison group consisted of a total of 139 hospital discharges that were never scheduled for a transition of care call with a pharmacist either throughout or after their hospital stay due to procedural error. The study flow chart is provided in Figure 2. The overall mean age was 59.7 years (standard deviation [SD]: 14.3), the majority were female, white/Caucasian, and non-Hispanic ethnicity. There were no statistically significant differences, including LACE scores, between groups. Demographics and number of discharge medications of the eligible discharges are described in Table 1.
Figure 2.
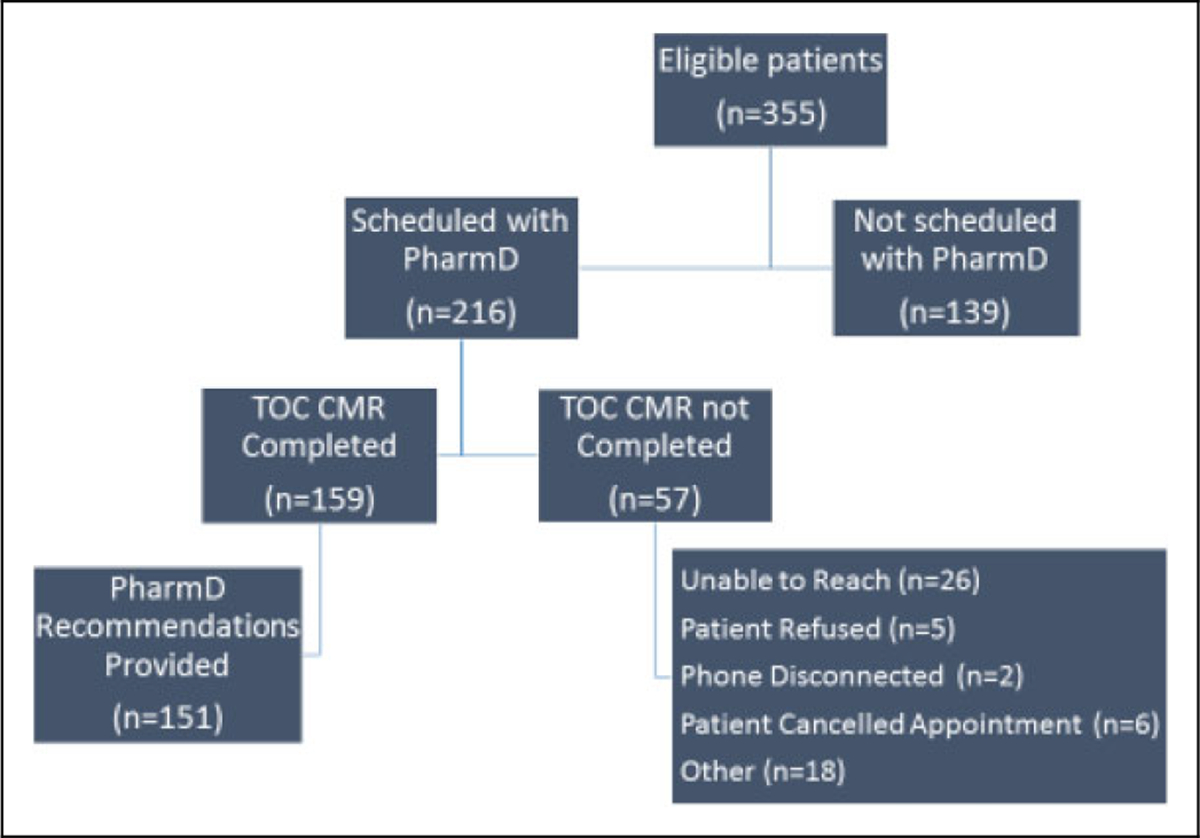
Study flow chart. TOC = Transition of Care, CMR = Comprehensive Medication Review.
Table 1.
Demographics and Number of Medications at Discharge.
| Demographics | Overall (N = 355) | Scheduled, Completed Pharmacist TOC call (n = 159) | Not Scheduled (n = 139) | P Valuea |
|---|---|---|---|---|
|
| ||||
| Gender | N (%) | N (%) | N (%) | .50 |
| Female | 193 (54.4) | 82 (51.6) | 77 (55.4) | |
| Male | 162 (45.6) | 77 (48.4) | 62 (44.6) | |
| Raceb | N (%) | N (%) | N (%) | .77 |
| White/Caucasian | 246 (69.5) | 115 (72.3) | 96 (69.6) | |
| Black/African-American | 92 (26.0) | 36 (22.6) | 36 (26.1) | |
| Other | 16 (4.5) | 8 (5.0) | 6 (4.4) | |
| Mean age (years) at discharge (SD), range | 59.7 (14.3), 24–100 | 60.0 (14.4), 24–97 | 60.4 (13.3), 24–94 | .79 |
| Mean number of prescription medications on discharge list (SD), range | 12.7 (5.2), 1–27 | 13.1 (5.2), 1–25 | 12.1 (5.3), 2–27 | .12 |
| Mean number of OTC medications on discharge list (SD), range | 4.9 (2.8), 0–15 | 4.9 (2.8), 0–14 | 5.0 (2.8), 0–15 | .82 |
Abbreviations: OTC, over-the-counter; SD, standard deviation; TOC, transition of care.
P value for test between scheduled, completed call group, and not scheduled group.
Due to small sample size, other race includes: Asian (n = 9), American Indian or Alaska Native (n = 2), and other (n = 5). Patient refused (n = 1) not included. 98% were non-Hispanic.
Completion of all 3 LACE transition of care components occurred in approximately 23% of eligible discharges. The majority of PCP follow-up appointments were completed, if scheduled (70.7%). There were more care navigator calls completed in the group that also received a pharmacist transition of care call (63.5% vs 35.3%; P < .001).
Impact on 30-day Readmission Rates and Health-Care Utilization After Discharge
In hospital discharges that met the criteria for inclusion in this study, there were a total of 59 (37.1%) readmissions in the group that received the transition of care pharmacist CMR and 52 (37.4%) readmissions in the group never scheduled for a CMR. There was no significant difference in the number of readmissions in those who received a transition of care pharmacist CMR versus those who were not scheduled for a CMR (P = .96). The average number of days between hospital discharge and readmission was 12. Approximately 15% of those eligible for the transition of care service visited the ED within 7 days of discharge and 38% visited the ED within 8 to 30 days of discharge. There were no significant differences between PCP visit completion and ED visits within 30 days of discharge between the 2 groups. Table 2 summarizes 30-day health-care utilization variables after discharge.
Table 2.
Thirty-Day Postdischarge Health-Care Utilization.
| Health-Care Use | Overall (N = 355) N (%) |
Scheduled, Completed Pharmacist TOC Call (n = 159) N (%) |
Not Scheduled (n = 139) N (%) |
P Valuea |
|---|---|---|---|---|
|
| ||||
| Unplanned 30-day internal hospital readmission | ||||
| No | 211 (59.44) | 100 (62.89) | 87 (62.59) | .96 |
| Yes | 144 (40.56)b | 59 (37.11) | 52 (37.41) | |
| ED visit within 7 days | ||||
| No | 300 (84.51) | 139 (87.42) | 121 (87.05) | .92 |
| Yes | 55 (15.49) | 20 (12.58) | 18 (12.95) | |
| ED visit within 8–30 days | ||||
| No | 221 (62.25) | 96 (60.38) | 92 (66.19) | .30 |
| Yes | 134 (37.75) | 63 (39.62) | 47 (33.81) | |
| Nonroutine PCP visits within 30 days of discharge (not including TOC provider follow-up visit) | ||||
| No | 326 (91.83) | 144 (90.57) | 130 (93.53) | .34 |
| Yes | 29 (8.17) | 15 (9.43) | 9 (6.47) | |
| Mean number of days until hospital readmission (SD), rangeb | 12.2 (7.32), 0–30 | 13.0 (6.69), 2–28 | 12.0 (6.87), 0–30 | .44 |
Abbreviations: ED, emergency department; PCP, primary care provider; SD, standard deviation; TOC, transition of care.
P value for test between scheduled, completed call group, and not scheduled group.
n = 144 for number of hospital readmissions.
Problems Identified in a CMR by a Centralized Transition of Care Pharmacist
Transition of care pharmacists identified health-related problems or MRPs in 151 (94.9%) of the 159 completed CMRs. There were a total of 478 problems identified and the mean number of problems identified in a pharmacist transition of care call was 3.1 (SD: 1.8, range: 1–10). Need for assessment or monitoring (n = 99, 20.7%), drug interaction (n = 47, 9.8%), and lab or diagnostic test indicated, not ordered, or inadequate refills between scheduled visits (both n = 43, 9.0%) were the most common problems identified. Cardiology, gastroenterology, and endocrinology were the most common indications for the problems identified. A summary of the problems identified by the pharmacist is provided in Table 3.
Table 3.
Number and Type of Problem Identified During the Pharmacist-Provided Comprehensive Medication Review.a
| Problem Identified | n (%)b |
|---|---|
|
| |
| Need for assessment or monitoring | 99 (20.7) |
| Drug interaction | 47 (9.8) |
| Lab or diagnostic test indicated, not ordered | 43 (9.0) |
| Inadequate refills between scheduled visits | 43 (9.0) |
| Medication underuse | 38 (7.9) |
| Subtherapeutic dosage | 29 (6.1) |
| Improper drug selection | 29 (6.1) |
| Not cost-effective drug choice | 20 (4.2) |
| Need for information | 19 (4.0) |
| Untreated indication | 15 (3.1) |
| Incomplete/improper instructions | 15 (3.1) |
| Overdosage | 12 (2.5) |
| Failure to receive medication | 12 (2.5) |
| Patient medication overuse | 11 (2.3) |
| No follow-up appointment with provider | 8 (1.7) |
| Adverse drug reaction | 6 (1.3) |
| Pill burden | 6 (1.3) |
| Medication use without indication | 5 (1.0) |
| Medication duplication | 5 (1.0) |
| Dosage form not reasonable for patient | 5 (1.0) |
n = 478.
Other problems identified: polypharmacy (n = 4, 0.8%), other (n = 3, 0.6%), abnormal lab result not addressed (n = 2, 0.4%), and inadequate patient lifestyle self-management (n = 2, 0.4%).
Recommendations for Identified Problems and Acceptance Rates
There were a total of 509 recommendations provided by transition of care pharmacists for the problems identified in the CMRs. The mean number of recommendations per pharmacist transition of care call was 3.4 (SD: 2.0, range: 1–11). The most common recommendations were provider review request (n = 180, 35.4%), coordination of care (n = 97, 19.1%), lab monitoring (n = 65, 12.8%), and patient education provided (n = 46, 9.0%). Communicating information to the provider and coordinating refill requests were the most prevalent care coordination activities performed. Over half of the recommendations for identified MRPs were related to the hospitalization rather than other chronic medical conditions (51%). Transition of care pharmacist recommendations are provided in Table 4. Approximately 50% of the pharmacists’ recommendations were accepted by a provider and approximately 96% of pharmacists’ recommendations were accepted by the patient.
Table 4.
Number and Type of Pharmacist Recommendations.a
| Recommendation Type | n (%) |
|---|---|
|
| |
| Provider review request | 180 (35.4) |
| Coordination of care | 97 (19.1) |
| Lab monitoring | 65 (12.8) |
| Patient education provided | 46 (9.0) |
| Drug interaction review/information provided | 45 (8.8) |
| Adjust medication dose | 25 (4.9) |
| Change medication | 24 (4.7) |
| Start medication | 9 (1.8) |
| Stop medication | 7 (1.4) |
| Adverse drug reaction review/information provided | 4 (0.8) |
| Other | 4 (0.8) |
| Adjust medication interval | 3 (0.6) |
n = 509.
Discussion
Our findings described the potential impact of a multidisciplinary transition of care intervention implemented in an institution with several transition of care programs in place. Although significant reductions in readmission rates were not identified, this study adds to the transition of care and patient-centered medical home literature through the novel use of the LACE scoring tool to identify highest risk patients for readmission at hospital discharge. This program provided services across the continuum from inpatient to ambulatory care. Additionally, the results of this pilot study indicated that the transition of care pharmacists identified several medication-related or health-related problems associated with a variety of medications and health conditions once the patient returned home. Although some of the problems identified were related to challenges faced in the ambulatory setting transition of care, such as difficulty with medication access, many of the problems could have been resolved with a CMR before discharge (eg, drug interaction, subtherapeutic dosage).
Various studies have described different approaches to improve transitions of care in an effort to reduce hospital readmissions. Trang and colleagues described the impact of the ambulatory care pharmacist in the Pharmacist Advancement of Transitions of Care to Home (PATCH) service in Florida.15 In the PATCH study, high-risk patients were identified as having one of the disease states outlined by the CMS Readmissions Reduction Program or disease states that have multiple medications, including high-risk medications. Patients identified upon discharge received a postdischarge pharmacist phone call followed by a face-to-face appointment with the pharmacist and the patient’s PCP. Patients who received the PATCH service had significantly lower ED visits and readmissions within 30 days compared to patients who received standard care (23% vs 41.4%, respectively; P = .013). In those patients who completed the PATCH service, a total of 49 MRPs, or approximately 2 MRPs were identified per patient, as compared to the average of approximately 3 MRPs identified per patient with this pilot study.
A study by Hitch et al described a team-based, transition of care model in Western North Carolina, and assessed the impact of the service on 30-day readmission rates at a large academic family medicine practice.16 Eligible moderate high-risk patients received a series of interventions which included contact with a nurse care manager, medication reconciliation (completed by a clinical pharmacist, care manager, or physician), and follow-up with a physician based on the patients’ risk level. Patients eligible for the transition of care interventions were compared to the usual care provided prior to implementation of this triad of team-based transition of care services. In patients who received the transition of care services, readmission rates decreased to 5.3% compared to 14.2% in the usual care group (P = .011). Of the 188 discharges, the majority of patients completed all 3 components (n = 166) and over half of the patients (n = 110) completed medication reconciliation with a clinical pharmacist specifically.
The transition of care services described by Stranges and colleagues implemented at Michigan Medicine (Michigan) in 2009 showed that a multidisciplinary transition of care service reduced readmissions in adults 60 years and older.11 Based on the results of Stranges et al, this study’s transition of care service components were modeled closely to address high readmission rates. The readmission rates in this study (37%) were higher than those identified in the study by Stranges et al (11%–21%) over 7 years ago. These differences may be reflecting the more selective patient enrollment criteria of a LACE score of 13 and above and potential differences in numbers of overall effective care transitions. Patients with a LACE score of 13 and above likely have more severe conditions, lower rates of preventable hospitalizations, and lower rates of preventable readmissions. The transition of care service described by Stranges et al also utilized social workers to address patients’ social needs, which may have influenced patient outcomes by addressing socioeconomic risk factors not captured in the current study. Additionally, they focused transition of care interventions for patients with an average age of 80 years (±8) and the current study population included adult patients with an average age of 60 years (±14). Many of these factors may have impacted the results seen in this study.
In this pilot study, the most common MRPs identified included major drug interactions between various medications, suboptimal dosing of medications such as blood pressure medications, inappropriate use of medications, and the need for additional laboratory or objective monitoring for appropriate medication use. Accordingly, implementation of this service led to recommendations to improve or minimize medication and health-related problems and concerns. Many of the MRPs identified required ongoing symptom or objective monitoring and these specific recommendations were made available to the PCP evaluating the patient. For example, when patients were on interacting medications that may increase the risk of bleeding, pharmacists recommended ongoing assessment for signs and symptoms of bleeding.
The specific recommendations associated with recent changes throughout the hospitalization (51%) may have required more urgent follow-up or monitoring. The recent hospitalization was the focus of the provider follow-up visit, and the pharmacist’s recommendations were available in the EMR for the provider’s review. Pharmacists also reviewed each patient’s history, health conditions, and identified other potential MRPs associated with chronic disease state management. About 49% of the problems identified were related to other medical problems aside from those specific conditions or medication therapy changes during the hospitalization.
Program Evaluation and Practical Applications
Before hospital discharge, appointments for the transition of care pharmacist and PCP were scheduled. A large number (n = 139) of hospital discharges were never scheduled for a transition of care call with a pharmacist, which was a major barrier to effective implementation of the service. Charts of patients discharged between June 2016 through August 2016 were reviewed and indicated that about 60% of eligible patients were being scheduled for a pharmacist phone appointment prior to discharge. Process improvements using Plan, Do, Study, Act cycles were used to improve scheduling rates with some improvement, up to about 70%, in the scheduling process. This remains an ongoing challenge that continues to be a focus for improvement.
As a result of this study, additional opportunities for improvement have been identified. Currently, the provider acceptance rate of pharmacist recommendations is about 50% within the first 30 days following hospital discharge. The current study’s provider acceptance rate is comparable to a community pharmacist-provided medication therapy management service in patients with a hospital discharge for pneumonia, congestive heart failure, and chronic obstructive pulmonary disease (acceptance rate 46%).17 However, our pharmacist notes were routed to providers via the EMR and the study by Luder et al. faxed their communication to the provider.17 We did not have confirmation that the providers opened and read the notes versus not accepting our recommendations. We are now implementing a process within the EMR to detect this difference in a future study. It appears that the pharmacists embedded within each clinic may be more successful in leading to provider acceptance of recommendations, as the embedded patient-centered medical home pharmacists have an established relationship with the clinic PCPs. There may be barriers to interprofessional communication, including the lack of a face-to-face discussion, that may limit providers’ receipt and understanding of the transition of care pharmacists’ assessments and recommendations.
This transition of care service has been expanded to eligible patients discharged with a LACE score of 10 or higher. We are in the process of evaluating whether this expanded criteria identifies a patient population where we can impact 30-day readmission rates. It is feasible that patients with lower LACE scores may have higher rates of preventable readmissions versus sicker patients identified at highest risk for readmission. Additionally, an alternative identification tool for medication-related issues may better identify patients who would benefit from pharmacist transition of care services than the LACE score at discharge which warrants further research.
Limitations
The small sample size, enrollment of only those patients with the highest LACE scores, and short duration of this pilot study were limitations, but this study provided valuable initial data to refine the central transition of care service. We did not randomize patients to receive the transition of care pharmacist call in this study; however, a group of eligible patients who were not scheduled for the pharmacist call were used as a comparison group. We assumed that there was no bias in who was scheduled and that each eligible patient had equal opportunity for a scheduled appointment. Additionally, this study was only able to capture internal readmission data from Michigan Medicine, thus readmissions may be underreported. Socioeconomic factors that may impact readmission rates, such as income level, educational level, caregiver support, and access to care, were not assessed.18 In using EMR data, we were limited by the amount and accuracy of information documented. However, it is assumed that information documented in the medical record would be similar for all eligible hospital discharges.
Conclusions
Although 30-day internal readmission rates were not lower in patients who received a pharmacist-provided CMR, pharmacists identified many MRPs and areas for intervention in highest risk patients during the transition from hospital to home. Pharmacist’s utility may be demonstrated through appropriateness of medication use and provider satisfaction. Continued evaluation of this multidisciplinary transition of care program is warranted to examine the impact on hospital readmission rates and identification and resolution of MRPs in a larger group of high-risk patients.
Supplementary Material
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The use of REDCap for this project was supported by National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR000433/UL1TR002240. Research reported in this publication was supported by National Center for Advancing Translational Sciences of the National Institutes of Health under award number KL2TR002241 to Dr Antoinette B. Coe. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
Authors’ Note
This study was approved by the institutional review board of University of Michigan (HUM00120101).
References
- 1.The Joint Commission, Joint Commission Center for Transforming Healthcare, Joint Commission Resources . Transitions of care: the need for a more effective approach to continuing patient care; 2002. https://www.jointcommission.org/assets/1/18/Hot_Topics_Transitions_of_Care.pdf. Accessed October 7, 2018.
- 2.Forster AJ, Murff HJ, Peterson JF, et al. Adverse drug events occurring following hospital discharge. J Gen Intern Med. 2005;20(4):317–323. doi: 10.1111/j.1525-1497.2005.30390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hines AL, Barrett ML, Jiang HJ, et al. Conditions With the Largest Number of Adult Hospital Readmissions by Payer, 2011. HCUP Statistical Brief #172. April 2014. Rockville, MD: Agency for Healthcare Research and Quality. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb172-Conditions-Readmissions-Payer.pdf. Accessed October 7, 2018. [PubMed] [Google Scholar]
- 4.McDermott KW, Elixhauser A, Sun R. Trends in Hospital Inpatient Stays in the United States, 2005–2014. HCUP Statistical Brief #225 2017. Rockville, MD: Agency for Healthcare Research and Quality. www.hcup-us.ahrq.gov/reports/statbriefs/sb225-Inpatient-US-Stays-Trends.pdf. Accessed October 7, 2018. [Google Scholar]
- 5.Centers for Medicare and Medicaid Services. Hospital Readmission Reduction Program. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/HRRP/Hospital-Readmission-Reduction-Program.html. Accessed October 7, 2018.
- 6.Kaiser Health News. Under Trump, Hospitals Face Same Penalties Embraced by Obama; 2017. https://khn.org/news/. Accessed October 7, 2018.
- 7.Van Walraven C, Dhalla IA, Bell C, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. Can Med Assoc J. 2010;182(6):551–557. doi: 10.1503/cmaj.091117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schnipper JL, Kirwin JL, Cotugno MC, et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch Intern Med. 2006;166(5):565. doi: 10.1001/archinte.166.5.565. [DOI] [PubMed] [Google Scholar]
- 9.Hawes EM, Maxwell WD, White SF, et al. Impact of an outpatient pharmacist intervention on medication discrepancies and health care resource utilization in posthospitalization care transitions. J Prim Care Community Health. 2014;5(1):14–18. doi: 10.1177/2150131913502489. [DOI] [PubMed] [Google Scholar]
- 10.Phatak A, Prusi R, Ward B, et al. Impact of pharmacist involvement in the transitional care of high-risk patients through medication reconciliation, medication education, and postdischarge call-backs (IPITCH Study). J Hosp Med. 2016;11(1):39–44. doi: 10.1002/jhm.2493. [DOI] [PubMed] [Google Scholar]
- 11.Stranges PM, Marshall VD, Walker PC, et al. A multidisciplinary intervention for reducing readmissions among older adults in a patient-centered medical home. Am J Manag Care. 2015;21(2):106–113. [PubMed] [Google Scholar]
- 12.Walker PC, Bernstein SJ, Tucker Jones JN, et al. Impact of a pharmacist-facilitated hospital discharge program. Arch Intern Med. 2009;169(21):2003. doi: 10.1001/archinternmed.2009.398. [DOI] [PubMed] [Google Scholar]
- 13.Strand LM, Morley PC, Cipolle RJ, et al. Drug-related problems: their structure and function. Ann Pharmacother. 1990;24:1093–1097. [DOI] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trang J, Martinez A, Aslam S, et al. Pharmacist Advancement of Transitions of Care to Home (PATCH) service. Hosp Pharm. 2015;50(11):994–1002. doi: 10.1310/hpj5011-994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hitch B, Parlier AB, Reed L, et al. Evaluation of a team-based, transition-of-care management service on 30-day readmission rates. N C Med J. 2016;77(2):87–92. doi: 10.18043/ncm.77.2.87. [DOI] [PubMed] [Google Scholar]
- 17.Luder HR, Frede SM, Kirby JA, et al. TransitionRX: impact of community pharmacy postdischarge medication therapy management on hospital readmission rate. J Am Pharm Assoc. 2015;55:246–254. [DOI] [PubMed] [Google Scholar]
- 18.Nagasako EM, Reidhead M, Waterman B, et al. Adding socioeconomic data to hospital readmissions calculations may produce more useful results. Health Aff. 2014;33(5):786–791. doi: 10.1377/hlthaff.2013.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


