Abstract
Purpose:
To examine characteristics associated with disparities in digital access (i.e., access to high-speed internet via a computer or smartphone) in American rural and urban households given that digital access has a direct impact on access to telemedicine-based services.
Methods:
Using the 2019 American Community Survey, we analyzed the proportions of geographic area, race/ethnicity, and socioeconomic status according to device and high-speed internet access. Maximum likelihood logit estimators estimated how these factors influenced device and high-speed internet access.
Findings:
Of 105,312,959 households, 32.29% were without a desktop or laptop computer with high-speed internet (WDW), 21.51% were without a smartphone with a data plan for wireless internet (WSW), and 14.02% were without any digital access (WDA). Non-metropolitan households were significantly more likely to be WDA than metropolitan households (OR=1.87; 95% CI: 1.83–1.91). Relative to non-Hispanic Whites, non-Hispanic Blacks (OR=1.60; 95% CI: 1.56–1.64), American Indian or Alaska Natives (OR=2.00; 95% CI: 1.82–2.19), or Hispanics (OR=1.70; 95% CI: 1.66–1.74) were significantly more likely to be WDA. When compared to households with private health insurance coverage, households WDA were significantly more likely to have no insurance (OR=2.44; 95% CI: 2.36–2.53) or public insurance coverage (OR=3.78; 95% CI: 3.70–3.86). Households with any digital access reported higher income and more family members living at home. Using the same predictors, similar findings were reported for households WDW or WSW.
Conclusions:
Significant disparities in digital access exist among non-metropolitan households, racial/ethnic minority households, and lower-income households. The lack of digital access has implications for accessibility of health care services via telemedicine and thus could exacerbate health disparities.
Keywords: access to care, health disparities, technology, telemedicine
Brought upon by the ongoing coronavirus (COVID-19) pandemic, health care policy changes temporarily reduced access barriers to telemedicine-based services and stimulated the delivery of health care (e.g., primary care, mental health, and substance use disorder treatment) through this modality across the United States.1,2 Telemedicine-based services require digital access (i.e., availability of high-speed internet and/or an internet-enabled device such as a smartphone or computer). While nationwide digital access has expanded over the past decade, many Americans in rural (non-metropolitan) communities do not have adequate high-speed internet access and/or live in “dead zones,” where high-speed internet or cell phone service is unavailable.3–8 For example, 98.5% of Americans who live in urban (metropolitan) areas have access to high-speed internet, whereas 77.4% in rural areas have access to high-speed internet.3,4 Disparities in smartphone ownership also exist among urban and rural Americans, with rural Americans less likely to own a smartphone (71%) than those living in urban communities (83%).3
The lack of digital access at home also disproportionately affects minorities, low-income populations, those with lower levels of education, and older populations, hindering millions of Americans in receiving telemedicine-based services.3,6,7 When compared to non-Hispanic Whites (80%), non-Hispanic Blacks (71%) and Hispanics (65%) report less often having high-speed internet services at their homes. Households with an annual income less than $30,000 report having high-speed internet services at their home less often (57%) than households with incomes greater than $30,000: $30,000–49,999=74%, $50,000–74,999=87%, and more than $75,000=92%. Additionally, those with a high school education or less (59%) are less likely to have high-speed internet services at home than those with some college education or who are college graduates (80% and 94%, respectively). Individuals 65 years or older report less access to high-speed internet services than 18- to 64-year-olds.9
Given that receiving telemedicine-based services requires an internet-enabled device and high-speed internet access, lack of digital access could have implications for disparities in access to telemedicine-based services. Insufficient research has examined household-level characteristics associated with disparities in digital access. The purpose of this study is to examine digital access (i.e., access to high-speed internet via desktop or laptop computer, smartphone with a data plan, or any digital access) among American rural and urban households using the most recently available national survey data.
Methods
We conducted secondary analyses using data from the 2019 American Community Survey (ACS) Integrated Public Use Microdata Series (IPUMS USA). The ACS is a cross-sectional survey and is administered yearly to a sample of about 3.5 million households across the United States.10 To represent a household, we used the variable, PERNUM, to include only the record of the first individual who appeared in the census or survey of each household. We used the variable, METRO, to identify the metropolitan status of the household. The METRO variable indicates whether the household is located within a metropolitan area and whether the household resided within or outside a central/principal city (e.g., non-metropolitan). This ACS dataset indicated that in many public-use microdata samples, metropolitan and central/principal-city status are not directly identified. For this reason, METRO codes were derived based on other available geographic information, such as county groups or Public Use Microdata Areas (PUMAs). PUMAs are statistical geographic areas built on census tracts and counties containing at least 100,000 people. If a county group or PUMA was partially within metropolitan areas or central/principal cities, then the status of the METRO variable was identified as indeterminable (mixed). For our analysis, we excluded households whose resident areas were indeterminable. Exemption from the university’s Institutional Review Board was obtained because we used a de-identified and publicly available dataset.
To analyze limitations in device and high-speed internet access, the outcome variables include households without 1) a desktop or laptop computer with high-speed internet, 2) a smartphone with a data plan for wireless internet, or 3) any digital access. For the categorical predictors, we measured the proportion of households for different geographic areas, race/ethnicity groups, health insurance coverage status, poverty level, and the number of family members. Age and education were not included in the analyses because they were not reported at the household level. Due to weighted survey data, all differences were tested using two-sided t-tests. We used maximum likelihood logit estimators to estimate how these factors, when simultaneously considered, influenced the device and high-speed internet access status of each household. All variables were included in the multivariable model. All of the analyses used ACS household weights including the correction of standard errors for the survey design. All data analyses were performed in Stata, version 15.11
Results
The study included data from 1,210,714 survey respondents. After survey data were weighted, this represented 105,312,959 households from metropolitan (n=95,302,321) and non-metropolitan areas (n=10,010,638). A total of 366,568 households were excluded from analysis because of missing data or because counties were identified as “indeterminable” as to their status as metropolitan or non-metropolitan (Figure 1). The proportions of limitations in device and high-speed internet access significantly differed across populations defined by geographic areas, race/ethnicity, health insurance coverage, poverty level, and the number of family members (Table 1). Overall, 32.29% of households reported being without a desktop or laptop computer with high-speed internet (WDH), 21.51% of households reported being without a smartphone with a data plan for wireless internet (WSW), and 14.02% of households reported being without any digital access (WDA). Households in non-metropolitan areas were significantly more likely to have limitations in device and high-speed internet access compared to households in metropolitan areas (WDH: 48.01% vs. 30.64%; WSW: 33.08% vs. 20.29%; WDA: 23.42% vs. 13.03%). The proportion of limitations in device and high-speed internet access (e.g., WDH, WSW, and WDA) was higher among American Indians or Alaska Natives than other racial or ethnic groups. The proportion of limitations in device and high-speed internet access (e.g., WDH, WSW, and WDA) was higher among households with one family member than households with two or more family members. Additionally, households with income under 100% of the poverty threshold reported a higher proportion of limitations in device and high-speed internet access (e.g., WDH, WSW, and WDA) than households whose income was 100% or higher of the poverty threshold. Households without health insurance had the highest proportion of WDH (49.71%), while households with public health insurance coverage had the highest proportion of WSW (36.76%) and WDA (25.46%).
Figure 1:
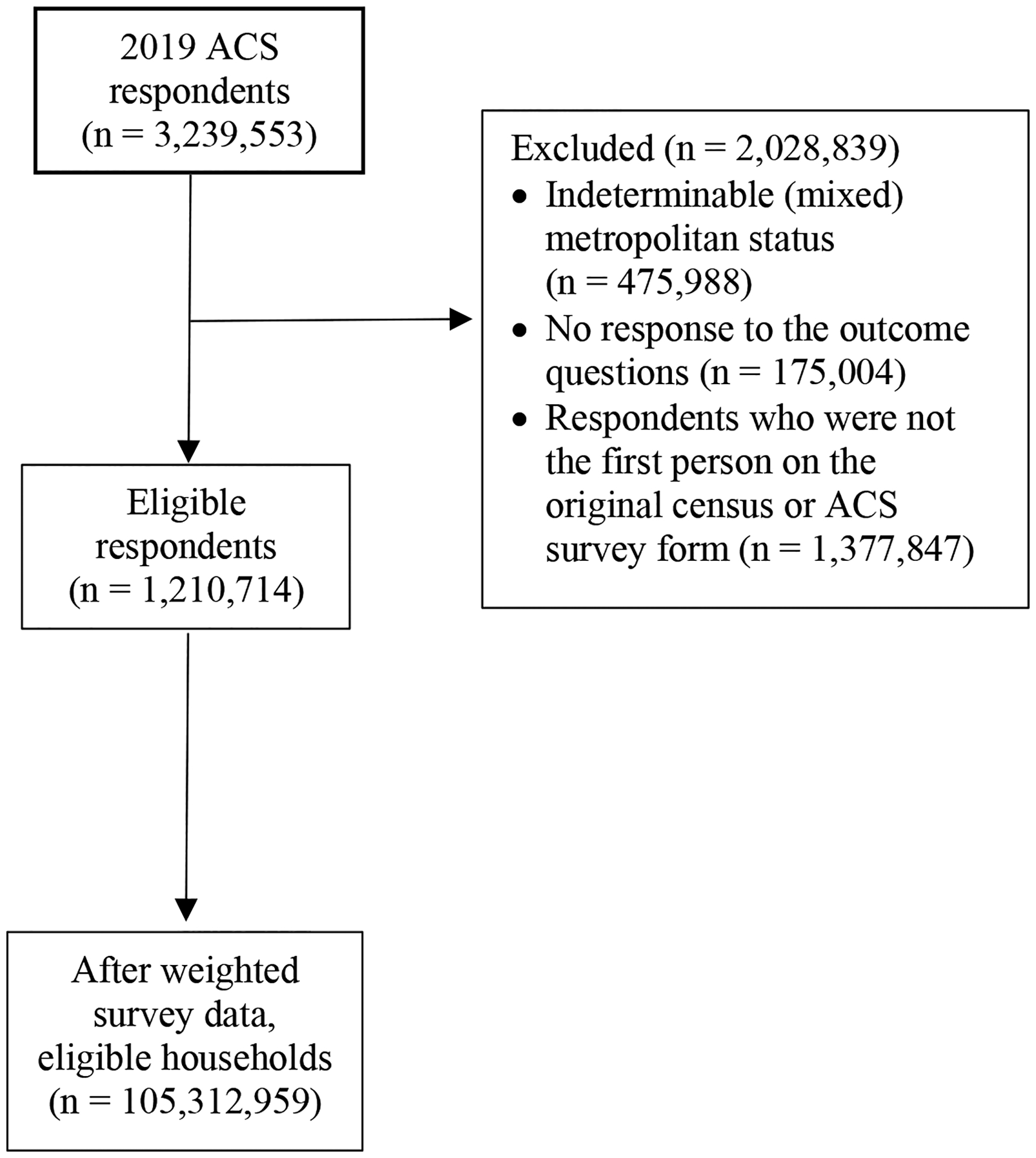
2019 American Community Survey Population Flow Chart
Table 1:
Limitations in Device and High-Speed Internet Access of Households in 2019a
| Characteristic | Without desktop or laptop computer with high-speed internet | Without smartphone with a data plan for wireless internet | Without any digital access | |||
|---|---|---|---|---|---|---|
| Proportion (95% CI), % | P value | Proportion (95% CI), % | P value | Proportion (95% CI), % | P value | |
| Among the whole population | 32.29 (32.17, 32.41) |
NA | 21.51 (21.40, 21,61) |
NA | 14.02 (13.93, 14.11) |
NA |
| Geographic area | ||||||
| Non-metro | 48.01 (47.64, 48.39) |
< .001 | 33.08 (32.73, 33.44) |
< .001 | 23.42 (23.10, 23.74) |
< .001 |
| Metro | 30.64 (30.51, 30.76) |
20.29 (20.18, 20.40) |
13.03 (12.94, 13.13) |
|||
| Race/Ethnicity | ||||||
| Non-Hispanic White | 28.36 (28.23, 28.49) |
< .001 | 20.87 (20.75, 20.98) |
< .001 | 12.55 (12.45, 12.65) |
< .001 |
| Non-Hispanic Black | 45.70 (45.39, 46.11) |
27.97 (27.61, 28.33) |
21.17 (20.84, 21.50) |
|||
| Hispanic | 42.17 (41.82, 42.53) |
22.46 (22.15, 22.76) |
16.86 (16.59, 17.14) |
|||
| American Indian or Alaska Native | 53.58 (51.77, 55.39) |
34.24 (32.57, 35.90) |
27.50 (25.95, 29.05) |
|||
| Asian or Pacific Islander | 20.73 (20.29, 21.17) |
12.57 (12.20, 12.94) |
7.44 (7.14, 7.74) |
|||
| Other race | 36.29 (33.18, 39.41) |
20.25 (17.73, 22.78) |
13.74 (11.57, 15.91) |
|||
| Two or more major races | 28.26 (27.34, 29.19) |
15.47 (14.71, 16.23) |
10.15 (9.52, 10.78) |
|||
| Health insurance coverage | ||||||
| Private coverageb | 20.77 (20.62, 20.91) |
< .001 | 10.36 (10.25, 10.47) |
< .001 | 5.26 (5.18, 5.35) |
< .001 |
| Uninsured | 49.71 (49.20, 50.21) |
24.86 (24.42, 25.31) |
19.30 (18.89, 19.71) |
|||
| Public coveragec | 45.14 (44.95, 45.34) |
36.76 (36.57, 36.94) |
25.46 (25.28, 25.63) |
|||
| Poverty Level (as a percentage of the poverty thresholds)d | ||||||
| <100 | 58.22 (57.83, 58.60) |
< .001 | 38.52 (38.14, 38.90) |
< .001 | 31.36 (30.99, 31.73) |
< .001 |
| 100–200 | 50.07 (49.74, 50.40) |
34.15 (33.84, 34.46) |
25.50 (25.21, 25.79) |
|||
| 200–300 | 38.53 (38.20, 38.86) |
25.54 (25.25, 25.83) |
16.62 (16.37, 16.87) |
|||
| 300–400 | 29.97 (29.66, 30.29) |
19.76 (19.49, 20.03) |
11.23 (11.01, 11.45) |
|||
| ≥400 | 17.89 (17.75, 18.03) |
11.81 (11.69, 11.92) |
5.43 (5.35, 5.52) |
|||
| Number of family members | ||||||
| 1 | 46.30 (46.07, 46.53) |
< .001 | 35.28 (35.06, 35.49) |
< .001 | 25.89 (25.69, 26.09) |
< .001 |
| 2 | 28.43 (28.24, 28.62) |
19.76 (19.60, 19.93) |
11.23 (11.09, 11.36) |
|||
| 3 | 24.61 (24.31, 24.91) |
12.29 (12.06, 12.52) |
6.96 (6.78, 7.14) |
|||
| 4 | 21.32 (21.00, 21.64) |
9.58 (9.34, 9.81) |
5.21 (5.03, 5.39) |
|||
| ≥5 | 25.56 (25.17, 25.95) |
11.77 (11.46, 12.07) |
6.88 (6.64, 7.12) |
|||
Analysis based on 1,210,714 observations in the 2019 American Community Survey, among them 135,748 are non-metro and 925,711 are metro, after weighting, representing 10,010,638 and 95,302,321 households respectively.
Poverty level expresses each family’s total income for the previous year as a percentage of the poverty thresholds established by the Social Security Administration, adjusted for inflation.
Private coverage is classified by the Census Bureau to include employer- or union-provided insurance, plans purchases by individuals from private insurance companies and military health care.
Public coverage is classified by the Census Bureau to include the federal insurance programs Medicare, Medicaid, and the Department of Veterans Affairs insurance.
The variables associated with higher odds of WDH, WSW, or WDA were similar for all models (Table 2). After controlling for socioeconomic and demographic variables, households residing in non-metropolitan areas were nearly twice as likely to be WDH (OR=2.07, 95% CI: 2.03–2.11), WSW (OR=1.72, 95% CI: 1.69–1.76), and WDA (OR=1.87, 95% CI: 1.83–1.91) than households residing in metropolitan areas. Relative to non-Hispanic Whites, non-Hispanic Blacks (OR=1.60; 95% CI: 1.56–1.64), American Indian or Alaska Natives (OR=2.00; 95% CI: 1.82–2.19), or Hispanics (OR=1.70; 95% CI: 1.66–1.74) were nearly twice as likely to be WDA. Racial and ethnic minorities (relative to non-Hispanic Whites) were also associated with higher odds of WDH or WSW. When compared to households with private health insurance coverage, households WDA were significantly more likely to have no health insurance (OR=2.44; 95% CI: 2.36–2.53) or public health insurance coverage (OR=3.78; 95% CI: 3.70–3.86). Having no health insurance or public health insurance coverage (relative to private health insurance) in a household was associated with higher odds of WDH or WSW. Income in a higher percentage of the poverty thresholds and having two or more family members in a household were associated with lower odds of WDH, WSW, or WDA.
Table 2:
Logistic regression resultsa
| Characteristics | (1) Without desktop or laptop computer with high-speed internet |
(2) Without smartphone with a data plan for wireless internet |
(3) Without any digital access |
|---|---|---|---|
| Non-Metro (Ref: Metro) | 2.07*** (2.03, 2.11) |
1.72*** (1.69, 1.76) |
1.87*** (1.83, 1.91) |
| Race/Ethnicity (Ref: Non-Hispanic White) | |||
| Non-Hispanic Black | 1.83*** (1.79, 1.86) |
1.28*** (1.25, 1.31) |
1.60*** (1.56, 1.64) |
| Hispanic | 1.89*** (1.85, 1.92) |
1.30*** (1.27, 1.32) |
1.70*** (1.66, 1.74) |
| American Indian or Alaska Native | 2.13*** (1.96, 2.31) |
1.54*** (1.41, 1.68) |
2.00*** (1.82, 2.19) |
| Asian or Pacific Islander | 0.87*** (0.84, 0.90) |
0.79*** (0.76, 0.82) |
0.86*** (0.82, 0.90) |
| Other race | 1.48*** (1.27, 1.73) |
1.09 (0.92, 1.30) |
1.25* (1.02, 1.53) |
| Two or more major races | 0.97 (0.92, 1.01) |
0.71*** (0.66, 0.76) |
0.80*** (0.74, 0.86) |
| Health insurance coverage (Ref: Private coverage) | |||
| Uninsured | 2.13*** (2.08, 2.18) |
1.91*** (1.86, 1.97) |
2.44*** (2.36, 2.53) |
| Public coverage | 2.06*** (2.03, 2.09) |
3.44*** (3.39, 3.49) |
3.78*** (3.70, 3.86) |
| Poverty Level (as a percentage of the poverty thresholds) (Ref: <100) | |||
| 100–200 | 0.85*** (0.83, 0.87) |
1.01 (0.99, 1.04) |
0.93*** (0.91, 0.95) |
| 200–300 | 0.63** (0.62, 0.625 |
0.83*** (0.81, 0.85) |
0.69*** (0.67, 0.71) |
| 300–400 | 0.48*** (0.46, 0.49) |
0.67*** (0.65, 0.69) |
0.50*** (0.49, 0.52) |
| ≥400 | 0.28*** (0.28, 0.29) |
0.41*** (0.41, 0.42) |
0.28*** (0.27, 0.28) |
| Number of family members (Ref: 1) | |||
| 2 | 0.58*** (0.57, 0.59) |
0.54*** (0.53, 0.55) |
0.46*** (0.46, 0.47) |
| 3 | 0.46*** (0.45, 0.47) |
0.34*** (0.39, 0.35) |
0.28*** (0.27, 0.29) |
| 4 | 0.37*** (0.37, 0.38) |
0.27*** (0.26, 0.27) |
0.21*** (0.20, 0.22) |
| ≥5 | 0.34*** (0.34, 0.35) |
0.26*** (0.25, 0.26) |
0.20*** (0.19, 0.21) |
| Observation | 1,061,469 | 1,061,469 | 1,061,469 |
Table presents odds ratios; 95% confidence intervals in brackets
P < .05,
P < .01,
P < .001
Analysis based on 1,210,714 observations in the 2019 American Community Survey, after weighting, representing 105,312,959 households.
Private coverage is classified by the Census Bureau to include employer- or union-provided insurance, plans purchases by individuals from private insurance companies and military health care.
Public coverage is classified by the Census Bureau to include the federal insurance programs Medicare, Medicaid, and the Department of Veterans Affairs insurance.
Poverty level expresses each family’s total income for the previous year as a percentage of the poverty thresholds established by the Social Security Administration, adjusted for inflation.
Discussion
Using 2019 ACS household-weighted data, we found significant disparities in digital access. Households that resided in a non-metropolitan area or had no health insurance or public health insurance were nearly two to three times more likely not to have access to devices required to receive telemedicine-based services. We also found a difference among racial and ethnic minorities, with non-Hispanic Blacks, Hispanics, and American Indians or Alaska Natives reporting less access to a computer or laptop with high-speed internet, smartphone with a data plan, or any digital access in comparison to non-Hispanic Whites. Lastly, households that were above the 100% poverty threshold or had two or more family members were more likely to have access to high-speed internet-enabled technology.
Our findings align with previous research that reported disparities in digital access among ethnic and racial minorities and rural communities.5,6,8 Our study contributes to the literature by utilizing the most recent digital access data and identifying household-level disparities. Most of the existing literature examines these disparities separately; however, this study assessed them simultaneously in a multivariable model, which confirms their unique contribution to digital access disparities. Now, more than ever, disparities in digital access may lead to increased health disparities among vulnerable groups (e.g., rural communities, minorities, low income, and uninsured or public insurance). Our study results suggest that disparity in digital access persists among these vulnerable groups who could benefit from receiving telemedicine-based services. Such disparities may even worsen during the COVID-19 pandemic, and future studies should replicate our findings when more recent data become available as the current study is based on data prior to COVID.
Federal policy changes hastened by COVID-19 have expanded access to telemedicine-based services by temporarily increasing reimbursement rates for providers,12 but these changes have not addressed the problem of patients’ lack of digital access required to make use of telemedicine. Over the past five years, the federal government has attempted to improve digital access, similar to the expansion of electricity in the early 20th century.13,14 The federal government has allocated billions to internet service providers to improve digital access in rural America and subsidize the cost of building new network infrastructure or network upgrades to high-need areas (i.e., Connect America Fund Phase II).13 Federal efforts created a new data collection method to properly map high-speed internet services and accurately report data speeds and coverage (i.e., Digital Opportunity Data Collection).14 The COVID-19 pandemic accelerated the paradigm shift in which Americans rely on high-speed internet for health care services, exacerbating the immediate need for devices and internet access. While federal initiatives aim to decrease the digital divide for rural America, limitations still inhibit delivery of high-speed internet (e.g., 100 mbps), including the reluctance of internet service providers to improve infrastructure and services in high-cost development areas (e.g., mountainous and extreme cold regions).
Limitations
Our study has several limitations. The first limitation is the lack of data available in the ACS database on the ability to use technology. The second limitation is the exclusion of households in a PUMA region that lies partially within metropolitan areas. This decision was made to clearly define our groups and reduce ambiguity. The third limitation is the reliance on household-level data, which precluded the examination of factors such as age and education. This decision was made because of the insufficient research that examined household-level characteristics associated with disparities in digital access. The fourth limitation was not examining differences between the record of the first individual who appeared in the census or survey of each household and the other individuals in the household. The fifth limitation is that the data were collected in 2019 and digital access could have changed since then. For instance, the COVID-19 pandemic highlighted the need for improved digital access and advanced federal initiatives that aim to reduce the digital divide and increase digital access to telemedicine-based services.
Conclusion
The lack of digital access among vulnerable populations inhibits the abilty of many people, including from rural populations, to obtain health care services via telemedicine. Insufficient access to the ever-growing delivery of health care via telemedicine could exacerbate health disparities in our society, especially for communities that are disproportionately affected, such as rural, minority, and low-income communities. As a result, there is a pressing need to target these communities and provide the required economic resources to increase their access to internet-enabled devices and to internet services at an adequate speed (e.g., 100 mbps). Collaboration at the federal, state, and local policy levels needs to effectively expand digital access and narrow the digital divide in those that are disproportionately affected.
Funding:
The efforts of the authors were supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number UG1DA049435. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures:
Larissa J. Mooney, MD, has previously received travel support and consultant fees from Alkermes, Inc. All other authors report no financial or possible conflicts of interest.
References
- 1.Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 Pandemic, lessons for the future. Telemed J E Health. 2020.571–573. 10.1089/tmj.2020.29040.rbexternalicon [DOI] [PubMed] [Google Scholar]
- 2.Czeisler MÉ , Lane RI, Petrosky E, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perrin A Digital gap between rural and nonrural America persists. Pew Research Center, Washington, D.C. May 31, 2019. Accessed September 19, 2020. https://www.pewresearch.org/fact-tank/2019/05/31/digital-gap-between-rural-and-nonrural-america-persists/ [Google Scholar]
- 4.Federal Communications Commission, 2020 Broadband Deployment Report. April 24, 2020. Accessed September 20, 2020. https://docs.fcc.gov/public/attachments/FCC-20-50A1.pdf
- 5.Busby B, Tanberk J. FCC Reports Broadband Unavailable to 21.3 Million Americans, Broadband Now Study Indicates 42 Million Do Not Have Access. Broadband Now Research website. February 3, 2020. Accessed September 22, 2020. https://broadbandnow.com/research/fcc-underestimates-unserved-by-50-percent [Google Scholar]
- 6.Lorence DP, Park H, Fox S. Racial disparities in health information access: Resilience of the digital divide. J Med Syst. 2006;30(4):241–249. doi: 10.1007/s10916-005-9003-y [DOI] [PubMed] [Google Scholar]
- 7.Mitchell UA, Chebli PG, Ruggiero L, Muramatsu N. The digital divide in health-related technology use: The significance of race/ethnicity. Gerontologist. 2019;59(1):6–14. doi: 10.1093/geront/gny138 [DOI] [PubMed] [Google Scholar]
- 8.Greenberg AJ, Haney D, Blake KD, Moser RP, Hesse BW. Differences in access to and use of electronic personal health information between rural and urban. J Rural Health. 2018;34(Suppl 1):s30–s38. doi: 10.1111/jrh.12228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pew Research Center. Internet/Broadband Fact Sheet. Pew Research website. April 7, 2021. Access April 14, 2021. https://www.pewresearch.org/internet/fact-sheet/internet-broadband/?menuItem=3109350c-8dba-4b7f-ad52-a3e976ab8c8f [Google Scholar]
- 10.Ruggles S, Flood S, Goeken R, et al. IPUMS USA: Version 10.0 [dataset]. IPUMS; 2020. doi: 10.18128/D010.V10.0 [DOI] [Google Scholar]
- 11.StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC. [Google Scholar]
- 12.Centers for Medicare and Medicaid Services. Medicare and Medicaid programs; policy and regulatory revisions in response to the COVID-19 public health emergency. Federal Regist. 2020;85(66):19230–19292. [Google Scholar]
- 13.Wireline Competition, Wireless Telecommunications. Connect America auction to expand broadband to 713,176 rural locations. 2018. https://www.fcc.gov/document/connect-america-auction-expand-broadband-713176-rural-locations. Accessed April 14,2021 [Google Scholar]
- 14.Federal Communications Commission. Establishing the digital opportunity data collection; modernizing the FCC form 477 data program. FedRegist. 2021;86:18124–18163. [Google Scholar]


