Abstract
Objective
The primary objective of this study was to evaluate whether the COVID-19 pandemic altered the racial and ethnic composition of patients receiving cardiac procedural care.
Design
This was a retrospective observational study.
Setting
This study was conducted at a single tertiary-care university hospital.
Participants
A total of 1,704 adult patients undergoing transcatheter aortic valve replacement (TAVR) (n = 413), coronary artery bypass grafting (CABG) (n = 506), or atrial fibrillation (AF) ablation (n = 785) from March 2019 through March 2022 were included in this study.
Interventions
No interventions were performed as this was a retrospective observational study.
Measurements and Main Results
Patients were grouped based on the date of their procedure: pre-COVID (March 2019 to February 2020), COVID Year 1 (March 2020 to February 2021), and COVID Year 2 (March 2021 to March 2022). Population-adjusted procedural incidence rates during each period were examined and stratified based on race and ethnicity. The procedural incidence rate was higher for White patients versus Black, and non-Hispanic patients versus Hispanic patients for every procedure and every period. For TAVR, the difference in procedural rates between White patients versus Black patients decreased between the pre-COVID and COVID Year 1 (12.05-6.34 per 1,000,000 persons). For CABG, the difference in procedural rates between White patients versus Black, and non-Hispanic patients versus Hispanic patients did not change significantly. For AF ablations, the difference in procedural rates between White patients versus Black patients increased over time (13.06 to 21.55 to 29.64 per 1,000,000 persons in the pre-COVID, COVID Year 1, and COVID Year 2, respectively).
Conclusion
Racial and ethnic disparities in access to cardiac procedural care were present throughout all study time periods at the authors’ institution. Their findings reinforce the continuing need for initiatives to reduce racial and ethnic disparities in healthcare. Further studies are needed to fully elucidate the effects of the COVID-19 pandemic on healthcare access and delivery.
Key Words: COVID-19, racial disparities, ethnic disparities, healthcare access, coronary artery bypass grafting, transcatheter aortic valve replacement
RACIAL AND ETHNIC DISPARITIES in healthcare access and delivery in the United States have been reported extensively across various fields.1, 2, 3, 4 Compared to White patients, Black patients are less likely to undergo medical procedures and diagnostic tests, and have a lower life expectancy and worse health outcomes.5 , 6 At the federal, state, and local levels, several institutions, including the United States Department of Health and Human Services Office of Minority Health, the National Institute on Minority Health and Health Disparities, the Centers for Disease Control and Prevention, and others, have implemented several strategies to address health disparities and promote health equity since the 1990s.1 Some of these interventions include diabetes prevention programs in American Indian and Alaska Native communities, the National Hypertension Control Initiative, implementation of cultural competency training for healthcare providers, and pipeline programs to increase underrepresented minority healthcare providers.
Data with regard to racial and ethnic disparities in access to cardiovascular procedures also have been published previously.7, 8, 9 Minority Americans compared to White Americans have worse outcomes and increased mortality for cardiac-related care.10 , 11 Contemporary data with regard to racial and ethnic disparities in cardiac procedural care are limited, especially in the setting of the recent COVID-19 pandemic.
The COVID-19 pandemic has also disproportionately affected people of color and minority Americans in terms of prevalence, mortality, and outcomes.12 , 13 The age-adjusted COVID-19 death rate for Latino and/or Hispanic residents in Los Angeles County was more than 2.5 × the rate for White residents, 452 compared to 176 per 100,000. Furthermore, nationwide surgical case cancellations due to the lack of hospital resources and capacity have exacerbated issues related to access to healthcare.14 The primary objective of this study was to determine whether the COVID-19 pandemic has led to worsening racial and ethnic disparities in access to cardiac procedural care at a single center within Los Angeles County.
Methods
After obtaining Institutional Review Board approval, all adult patients undergoing transcatheter aortic valve replacement (TAVR), coronary artery bypass grafting (CABG), or atrial fibrillation (AF) ablation from March 2019 through March 2022 at the authors’ tertiary-care university hospital were included in this retrospective observational study. Patients undergoing combined surgical procedures, such as CABG along with valve surgery or CABG along with solid organ transplantation, were also included in the study.
Data elements such as patient age, sex, ethnicity, race, insurance provider, preprocedural admission status, ZIP code, procedure type, and procedure year were collected from the electronic medical record and institutional databases. The patient's ZIP code was used to identify Los Angeles County residents. Additionally, the ZIP code data were converted to ZIP Code tabulation areas (ZCTA), which were then used to collect socioeconomic status information, including median income, percent of families living in poverty, and percent unemployment, from the American Community Survey database available through the United States Census Bureau. Patients were separated into the following 3 groups based on the date of their procedure: pre-COVID, indicating March 2019 to February 2020; COVID Year 1, indicating March 2020 to February 2021; and COVID Year 2, indicating March 2021 to March 2022. The procedural incidence rates were adjusted to the Los Angeles County population based on data from the 2020 United States Census Bureau.15 For each study period, these population-adjusted incidence rates were examined and stratified based on race and ethnicity.
Statistical Analysis
The primary objective was to evaluate whether the COVID-19 pandemic led to worsening racial and ethnic disparities in access to TAVR, CABG, or AF ablation for patients at the authors’ institution. All summary data are presented as median and IQRs or as numbers and percentages. The procedural incidence rates are reported as adjusted to the county population as cases per 1,000,000 persons. Statistical analysis with one-way Analysis of Variance, Kruskal-Wallis, or chi-square tests were used to compare the groups. All data were analyzed using STATA statistical software version 14.0 (StataCorp, LLC, College Station, TX), and p < 0.05 was considered statistically significant.
Results
A total of 1,341 patients were identified in the database search. Only 11 patients were excluded (3 undergoing TAVR, 1 undergoing CABG, and 7 undergoing AF ablation) because of incomplete demographic data, such as an unknown address, insurance provider, or admission status. Of the remaining 1,330 patients included in the study, there were 283 patients undergoing TAVR, 455 patients undergoing CABG, and 592 undergoing AF ablation. There were no significant differences in age, sex, race, insurance provider, and preprocedural admission status between the pre-COVID, COVID Year 1, and COVID Year 2 groups for each procedure (Table 1, Table 2, Table 3 ). There was, however, a significant difference in the distribution of Latino and/or Hispanic patients versus non-Latino and/or non-Hispanic patients during COVID Year 1 for CABG procedures.
Table 1.
Demographics for Patients Undergoing AF Ablation
| Pre-COVID (n = 160) | COVID Year 1 (n = 177) | COVID Year 2 (n = 255) | p | |
|---|---|---|---|---|
| Age, n (%), y | 63 (12.3) | 64 (10.7) | 66 (11.5) | 0.111 |
| Female sex, n (%) | 58 (36.25) | 48 (27.11) | 93 (36.47) | 0.092 |
| Ethnicity, n (%) | 0.17 | |||
| Hispanic/Latino | 7 (4.37) | 11 (6.21) | 27 (10.58) | |
| Not Hispanic/Latino | 137 (85.62) | 147 (83.05) | 206 (80.78) | |
| Not reported/not answered | 16 (10.0) | 19 (10.73) | 22 (8.62) | |
| Race, n (%) | 0.371 | |||
| American Indian/Alaska Native | 2 (1.25) | 1 (0.56) | 1 (0.39) | |
| Asian | 12 (7.5) | 11 (6.21) | 14 (5.49) | |
| Black/African American | 7 (4.37) | 3 (1.69) | 4 (1.56) | |
| Native Hawaiian/Pacific Islander | 0 (0.0) | 0 (0.0) | 1 (0.39) | |
| Not reported/not answered | 10 (6.25) | 18 (10.16) | 30 (11.76) | |
| Other | 11 (6.87) | 6 (3.39) | 18 (7.05) | |
| White | 118 (73.75) | 138 (77.96) | 187 (73.33) | |
| Insurance provider, n (%) | 0.61 | |||
| Commercial | 75 (46.87) | 81 (45.76) | 95 (37.25) | |
| Medi-Cal | 2 (1.25) | 1 (0.56) | 4 (1.56) | |
| Medicare | 63 (39.37) | 72 (40.67) | 115 (45.09) | |
| Other | 2 (1.25) | 3 (1.69) | 3 (1.17) | |
| Managed Care | 18 (11.25) | 20 (11.29) | 38 (14.90) | |
| Preprocedure admission status, n (%) | 0.539 | |||
| Same day admit | 157 (98.12) | 176 (99.43) | 252 (98.82) | |
| Inpatient | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| ED admit | 3 (1.87) | 1 (0.56) | 3 (1.17) | |
| Socioeconomic factors (ZCTA-based) | ||||
| Median income, USD | 102,867 (35,027) | 106,026 (37,327) | 101,496 (33,084) | 0.411 |
| Families in poverty, n (%) | 5 (3.4) | 5 (3.9) | 6 (4.1) | 0.422 |
| Unemployed, n (%) | 5 (1.8) | 5 (1.5) | 5 (1.6) | 0.176 |
| Outcomes | ||||
| Hospital length of stay, mean (SD), h | 31 (30.0) | 21 (9.9) | 21 (18.4) | < 0.005 |
| ICU length of stay, mean (SD), h | 1 (12.1) | 0 (4.1) | 0 (9.1) | 0.245 |
Abbreviations: AF, atrial fibrillation; ED, emergency department; ICU, intensive care unit; ZCTA, ZIP code tabulation area.
Table 2.
Demographics for Patients Undergoing CABG
| Pre-COVID (n = 167) | COVID Year 1 (n = 130) | COVID Year 2 (n = 158) | p | |
|---|---|---|---|---|
| Age, n (%), y | 65 (9.4) | 64 (10.5) | 65 (11.6) | 0.88 |
| Female sex, n (%) | 32 (19.16) | 28 (21.53) | 21 (13.29) | 0.161 |
| Ethnicity, n (%) | 0.025 | |||
| Hispanic/Latino | 27 (16.16) | 35 (26.92) | 29 (18.35) | |
| Not Hispanic/Latino | 132 (79.04) | 86 (66.15) | 111 (70.25) | |
| Not reported/not answered | 8 (4.79) | 9 (6.92) | 18 (11.39) | |
| Race, n (%) | 0.062 | |||
| American Indian/Alaska Native | 3 (1.796) | 0 (0.0) | 0 (0.0) | |
| Asian | 19 (11.37) | 20 (15.38) | 19 (12.02) | |
| Black/African American | 11 (6.58) | 5 (3.84) | 7 (4.43) | |
| Native Hawaiian/Pacific Islander | 1 (0.59) | 2 (1.53) | 1 (0.63) | |
| Not reported/not answered | 6 (3.59) | 8 (6.15) | 19 (12.02) | |
| Other | 27 (16.168) | 30 (23.07) | 32 (20.25) | |
| White | 100 (59.88) | 65 (50.0) | 80 (50.63) | |
| Insurance provider, n (%) | 0.492 | |||
| Commercial | 44 (26.34) | 47 (36.15) | 42 (26.58) | |
| Medi-Cal | 16 (9.58) | 11 (8.46) | 18 (11.39) | |
| Medicare | 81 (48.50) | 59 (45.38) | 76 (48.10) | |
| Other | 6 (3.59) | 2 (1.53) | 2 (1.26) | |
| Managed care | 20 (11.97) | 11 (8.46) | 20 (12.65) | |
| Preprocedure admission status, n (%) | 0.447 | |||
| Same day admit | 72 (43.11) | 65 (50.0) | 81 (51.26) | |
| Inpatient | 37 (22.15) | 31 (23.84) | 33 (20.88) | |
| ED admit | 58 (34.73) | 34 (26.15) | 44 (27.84) | |
| Socioeconomic factors (ZCTA-based) | ||||
| Median income deciles, mean (SD), USD | 88,047 (32,622) | 86,038 (32,948) | 92318 (36657) | 0.274 |
| Families in poverty, n (%) | 8 (5.9) | 8 (5.7) | 7 (5.6) | 0.67 |
| Unemployed, n (%) | 6 (1.8) | 6 (1.9) | 6 (1.7) | 0.523 |
| Outcomes | ||||
| Hospital length of stay, mean (SD), h | 359 (329.7) | 420 (1,105.5) | 310 (233.7) | 0.348 |
| ICU length of stay, mean (SD), h | 217 (320.7) | 587 (4841.6) | 117 (90.2) | 0.283 |
Abbreviations: CABG, coronary artery bypass graft; ED, emergency department; ICU, intensive care unit; ZCTA, ZIP code tabulation area.
Table 3.
Demographics for Patients Undergoing TAVR
| Pre-COVID (n = 85) | COVID Year 1 (n = 87) | COVID Year 2 (n = 111) | p | |
|---|---|---|---|---|
| Age, n (%), y | 80 (7.9) | 77 (10.4) | 78 (8.2) | 0.102 |
| Female sex, n (%) | 38 (44.706) | 38 (43.678) | 46 (41.441) | 0.893 |
| Ethnicity, n (%) | 0.404 | |||
| Hispanic/Latino | 6 (7.05) | 9 (10.34) | 17 (15.31) | |
| Not Hispanic/Latino | 74 (87.05) | 72 (82.75) | 85 (76.57) | |
| Not reported/not answered | 5 (5.88) | 6 (6.89) | 9 (8.10) | |
| Race, n (%) | 0.28 | |||
| American Indian/Alaska Native | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Asian | 6 (7.05) | 6 (6.89) | 4 (3.60) | |
| Black/African American | 1 (1.17) | 6 (6.89) | 7 (6.30) | |
| Native Hawaiian/Pacific Islander | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Not reported/not answered | 6 (7.05) | 5 (5.74) | 13 (11.71) | |
| Other | 11 (12.94) | 12 (13.79) | 8 (7.20) | |
| White | 61 (71.76) | 58 (66.66) | 79 (71.17) | |
| Insurance provider, n (%) | 0.098 | |||
| Commercial | 5 (5.88) | 2 (2.29) | 6 (5.40) | |
| Medi-Cal | 0 (0.0) | 4 (4.59) | 2 (1.80) | |
| Medicare | 63 (74.11) | 62 (71.26) | 92 (82.88) | |
| Other | 1 (1.17) | 0 (0.0) | 1 (0.90) | |
| Managed Care | 16 (18.82) | 19 (21.83) | 10 (9.01) | |
| Preprocedure admission status, n (%) | 0.229 | |||
| Same day admit | 60 (70.58) | 63 (72.41) | 91 (81.98) | |
| Inpatient | 11 (12.94) | 13 (14.94) | 7 (6.30) | |
| ED admit | 14 (16.47) | 11 (12.64) | 13 (11.71) | |
| Socioeconomic factors (ZCTA-based) | ||||
| Median income deciles, mean (SD), USD | 97405 (35651) | 96320 (35537) | 100204 (37199) | 0.736 |
| Families in poverty, n (%) | 6 (4.6) | 7 (5.6) | 6 (5.8) | 0.205 |
| Unemployed, n (%) | 5 (1.8) | 5 (1.6) | 5 (1.9) | 0.684 |
| Outcomes | ||||
| Hospital length of stay, mean (SD), h | 123 (125.6) | 146 (182.8) | 125 (285.5) | 0.722 |
| ICU length of stay, mean (SD), h | 21 (65.8) | 57 (215.7) | 27 (106.7) | 0.192 |
NOTE. Data are presented as mean (SD) or count (%) where appropriate.
Abbreviations: ED, emergency department; ICU, intensive care unit; TAVR, transcatheter aortic valve replacement; ZCTA, ZIP code tabulation area.
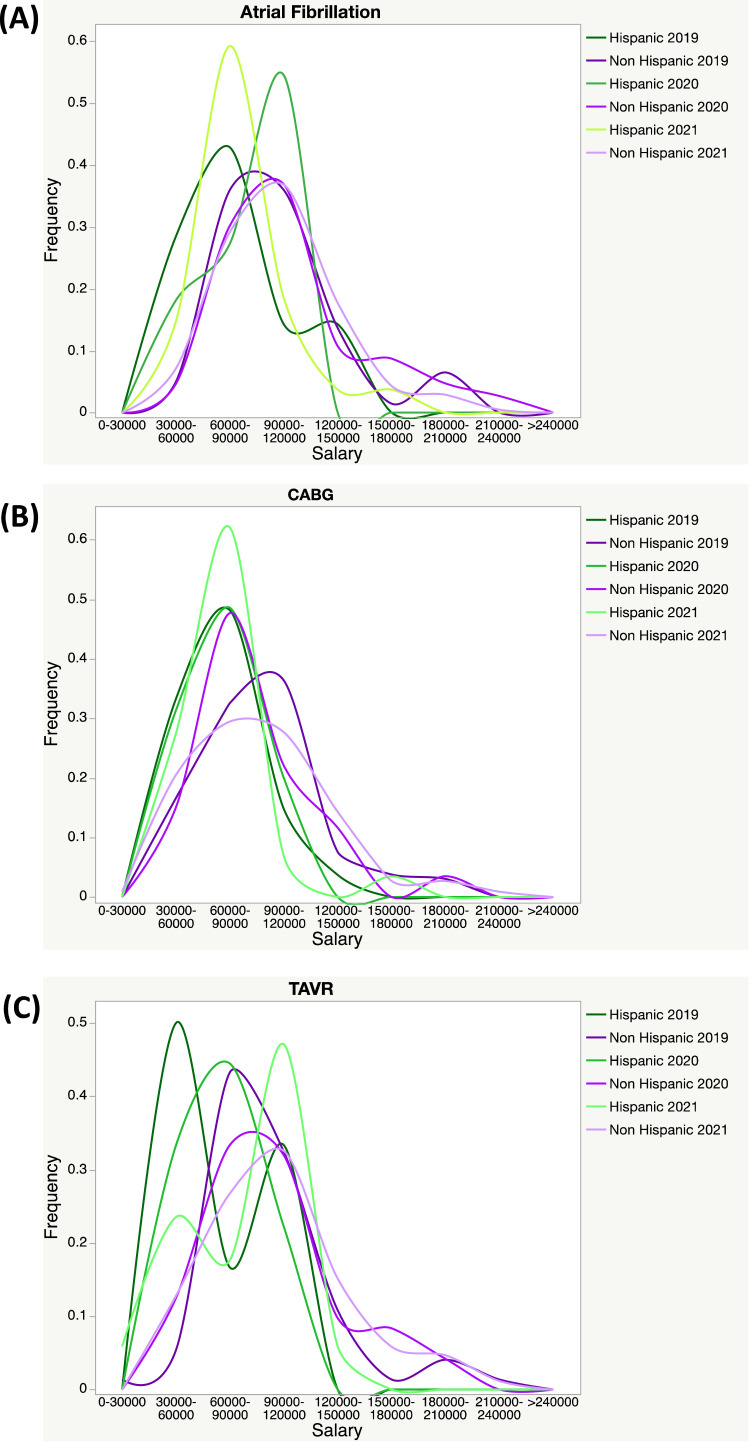
When Latino and/or Hispanic patients were compared to non-Latino and/or non-Hispanic patients according to period and procedure, several additional differences were notable (Table 4 ). Within COVID Year 2, Latino and/or Hispanic patients undergoing AF ablation and CABG were statistically younger than their non-Latino and/or non-Hispanic counterparts (Table 4, Table 5, Table 6 ). For AF ablation and TAVR in COVID Year 1 and Year 2, as well as CABG in all years, Latino and/or Hispanic patients resided in ZIP codes with lower median incomes and higher percentages of families in poverty. The distribution of the median incomes throughout all 3 time periods remained consistent within each ethnic group (Fig 1 ). Additionally, in the pre-COVID period for AF ablation and COVID Year 2 for TAVR, the distribution of insurance providers was different among ethnic groups.
Table 4.
AF Ablation in Latino/Hispanic Versus Non-Latino/Hispanic Patients Across COVID Years
| Pre-COVID |
COVID Year 1 |
COVID Year 2 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Latino or Hispanic (n = 7) | Non-Latino or Hispanic (n = 137) | p | Latino or Hispanic (n = 11) | Non-Latino or Hispanic (n = 147) | p | Latino or Hispanic (n = 27) | Non-Latino or Hispanic (n = 206) | p | |
| Age, y | 54.86 (19.18) | 64.05 (12.32) | 0.063 | 60.64 (13.48) | 64.35 (10.85) | 0.283 | 59.26 (15.9) | 67.19 (10.55) | < 0.005 |
| Female sex | 4 (57.14) | 48 (35.03) | 0.433 | 4 (36.36) | 41 (27.89) | 0.799 | 10 (37.03) | 79 (38.35) | 1 |
| Insurance provider | 0.041 | 0.811 | 0.174 | ||||||
| Commercial | 4 (57.14) | 66 (48.17) | 7 (63.63) | 66 (44.89) | 10 (37.03) | 73 (35.43) | |||
| Medi-Cal | 1 (14.28) | 1 (0.73) | 0 (0.0) | 1 (0.68) | 1 (3.70) | 3 (1.45) | |||
| Medicare | 2 (28.57) | 54 (39.41) | 3 (27.27) | 58 (39.45) | 8 (29.63) | 100 (48.54) | |||
| Other | 0 (0.0) | 2 (1.46) | 0 (0.0) | 3 (2.04) | 1 (3.70) | 2 (0.97) | |||
| Managed care | 0 (0.0) | 14 (10.21) | 1 (9.09) | 19 (12.92) | 7 (25.92) | 28 (13.59) | |||
| Preprocedure admission status | |||||||||
| Same day admit | 7 (100.0) | 134 (97.81) | 1 | 11 (100.0) | 146 (99.32) | 1 | 27 (100.0) | 203 (98.54) | 1 |
| Inpatient | 0 (0.0) | 0 (0.0) | 1 | 0 (0.0) | 0 (0.0) | 1 | 0 (0.0) | 0 (0.0) | 1 |
| ED admit | 0 (0.0) | 3 (2.19) | 1 | 0 (0.0) | 1 (0.68) | 1 | 0 (0.0) | 3 (1.456) | 1 |
| Socioeconomic factors, ZCTA-based | |||||||||
| Median income deciles, USD | 82,741 (26,085) | 101,720 (34,979) | 0.16 | 84,635 (23,169) | 108,841 (38,388) | 0.041 | 78,832 (24,683) | 102,564 (32,590) | < 0.005 |
| Families in poverty, n (%) | 8.2 (4.03) | 5.68 (3.44) | 0.063 | 8.25 (6.08) | 5.37 (3.28) | 0.01 | 9.09 (5.03) | 5.88 (3.87) | < 0.005 |
| Unemployed, n (%) | 5.9 (1.12) | 5.97 (1.89) | 0.919 | 6.09 (1.22) | 5.39 (1.46) | 0.125 | 6.09 (1.35) | 5.63 (1.63) | 0.155 |
| Outcomes | |||||||||
| Hospital length of stay, h | 28.57 (3.6) | 32.23 (32.33) | 0.766 | 20.18 (6.1) | 21.19 (10.41) | 0.752 | 20.26 (7.17) | 22.46 (20.14) | 0.575 |
| ICU length of stay, h | 0.0 (0.0) | 2.25 (13.01) | 0.65 | 0.0 (0.0) | 0.49 (4.49) | 0.72 | 0.0 (0.0) | 0.81 (10.15) | 0.679 |
NOTE. Data is present as mean (SD) or count (%) where appropriate.
Abbreviations: AF, atrial fibrillation; CABG, coronary artery bypass graft; ED, emergency department; ICU, intensive care unit; TAVR, transcatheter aortic valve replacement; ZCTA, ZIP code tabulation area.
Table 5.
CABG in Latino/Hispanic vs Non-Latino/Hispanic Patients Across COVID Years
| Pre-COVID |
COVID Year 1 |
COVID Year 2 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Latino or Hispanic (n = 27) | Non-Latino or Hispanic (n = 132) | p | Latino or Hispanic (n = 35) | Non-Latino or Hispanic (n = 86) | p | Latino or Hispanic (n = 29) | Non-Latino or Hispanic (n = 111) | p | |
| Age, y | 64.15 (9.49) | 65.54 (9.53) | 0.491 | 62.71 (12.22) | 65.59 (9.79) | 0.176 | 58.76 (13.49) | 66.71 (10.61) | < 0.005 |
| Female sex | 7 (25.92) | 22 (16.66) | 0.389 | 12 (34.28) | 16 (18.60) | 0.106 | 6 (20.69) | 14 (12.613) | 0.419 |
| Insurance provider | 0.2 | 0.025 | 0.236 | ||||||
| Commercial | 5 (18.51) | 37 (28.03) | 7 (20.0) | 37 (43.02) | 6 (20.69) | 30 (27.02) | |||
| Medi-Cal | 6 (22.22) | 10 (7.576) | 7 (20.0) | 4 (4.65) | 6 (20.69) | 12 (10.81) | |||
| Medicare | 13 (48.14) | 64 (48.48) | 16 (45.71) | 38 (44.18) | 15 (51.72) | 52 (46.84) | |||
| Other | 1 (3.70) | 5 (3.78) | 1 (2.85) | 1 (1.16) | 1 (3.44) | 1 (0.90) | |||
| Managed care | 2 (7.40) | 16 (12.12) | 4 (11.42) | 6 (6.97) | 1 (3.44) | 16 (14.41) | |||
| Preprocedure admission status | 0.816 | 0.721 | 0.073 | ||||||
| Same day admit | 12 (44.444) | 56 (42.42) | 18 (51.42) | 39 (45.34) | 9 (31.03) | 58 (52.25) | |||
| Inpatient | 7 (25.92) | 29 (21.97) | 7 (20.0) | 23 (26.74) | 10 (34.48) | 20 (18.01) | |||
| ED admit | 8 (29.63) | 47 (35.60) | 10 (28.57) | 24 (27.90) | 10 (34.48) | 33 (29.73) | |||
| Socioeconomic factors, ZCTA-based | |||||||||
| Median income deciles, USD | 70,948 (20,581) | 91,615 (338,68) | < 0.005 | 71,079 (21,390) | 88,846 (32,101) | < 0.005 | 73,061 (23,558) | 93,175 (36,990) | 0.006 |
| Families in poverty, n (%) | 11.02 (6.17) | 7.83 (5.86) | 0.012 | 11.14 (6.44) | 7.8 (5.21) | < 0.005 | 10.28 (5.21) | 7.8 (5.72) | 0.036 |
| Unemployed, n (%) | 6.57 (1.9) | 5.91 (1.77) | 0.086 | 7.03 (1.91) | 6.03 (1.8) | 0.007 | 6.32 (1.73) | 6.03 (1.71) | 0.418 |
| Outcomes | |||||||||
| Hospital length of stay, h | 442.3 (406.24) | 348.32 (320.4) | 0.188 | 662.09 (2049.01) | 345.55 (373.79) | 0.169 | 369.86 (307.53) | 309.12 (222.36) | 0.231 |
| ICU length of stay, h | 243.44 (318.5) | 212.32 (331.1) | 0.655 | 1694.02 (9314.77) | 188.43 (422.15) | 0.135 | 125.8 (83.48) | 121.14 (96.66) | 0.813 |
NOTE. Data is present as mean (SD) or count (%) where appropriate.
Abbreviations: AF, atrial fibrillation; CABG, coronary artery bypass graft; ED, emergency department; ICU, intensive care unit; TAVR, transcatheter aortic valve replacement; ZCTA, ZIP code tabulation area.
Table 6.
TAVR in Latino/Hispanic vs Non-Latino/Hispanic Patients Across COVID Years
| Pre-COVID |
COVID Year 1 |
COVID Year 2 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Latino or Hispanic (n = 6) | Non-Latino or Hispanic (n = 74) | p | Latino or Hispanic (n = 9) | Non-Latino or Hispanic (n = 72) | p | Latino or Hispanic (n = 17) | Non-Latino or Hispanic (n = 85) | p | |
| Age, y | 84.83 (5.31) | 79.84 (7.9) | 0.133 | 72.56 (9.3) | 78.35 (10.09) | 0.106 | 76.29 (7.42) | 79.38 (8.44) | 0.164 |
| Female sex | 3 (50.0) | 32 (43.24) | 1 | 2 (22.22) | 33 (45.83) | 0.322 | 9 (52.94) | 34 (40.0) | 0.473 |
| Insurance provider | 0.225 | 0.669 | 0.029 | ||||||
| Commercial | 0 (0.0) | 5 (6.75) | 0 (0.0) | 2 (2.77) | 0 (0.0) | 6 (7.05) | |||
| Medi-Cal | 0 (0.0) | 0 (0.0) | 1 (11.11) | 3 (4.16) | 0 (0.0) | 2 (2.35) | |||
| Medicare | 3 (50.0) | 56 (75.67) | 7 (77.77) | 51 (70.83) | 12 (70.58) | 71 (83.52) | |||
| Other | 0 (0.0) | 1 (1.35) | 0 (0.0) | 0 (0.0) | 1 (5.88) | 0 (0.0) | |||
| Managed care | 3 (50.0) | 12 (16.21) | 1 (11.11) | 16 (22.22) | 4 (23.52) | 6 (7.05) | |||
| Preprocedure admission status | 0.503 | 0.034 | 0.478 | ||||||
| Same day admit | 5 (83.33) | 50 (67.56) | 5 (55.55) | 52 (72.22) | 14 (82.35) | 68 (80.0) | |||
| Inpatient | 1 (16.66) | 10 (13.51) | 4 (44.44) | 9 (12.5) | 2 (11.76) | 5 (5.88) | |||
| ED admit | 0 (0.0) | 14 (18.91) | 0 (0.0) | 11 (15.27) | 1 (5.88) | 12 (14.11) | |||
| Socioeconomic factors, ZCTA-based | |||||||||
| Median income deciles, USD | 67,273.0 (29,740.45) | 98,236.39 (354,69.38) | 0.041 | 68,733.56 (20,183.8) | 97,353.89 (34,778.94) | 0.018 | 86,004.82 (27,623.69) | 103,873.36 (38,868.92) | 0.074 |
| Families in poverty, n (%) | 14.23 (9.87) | 5.74 (3.45) | < 0.005 | 10.9 (7.7) | 7.44 (5.34) | 0.085 | 8.82 (9.53) | 5.88 (4.54) | 0.053 |
| Unemployed, n (%) | 6.35 (1.31) | 5.89 (1.82) | 0.546 | 6.8 (1.57) | 5.67 (1.61) | 0.051 | 6.08 (2.21) | 5.91 (1.89) | 0.745 |
| Outcomes | |||||||||
| Hospital length of stay, h | 107.5 (81.61) | 120.81 (114.94) | 0.782 | 192.67 (152.77) | 148.67 (191.76) | 0.51 | 94.47 (102.85) | 139.16 (321.95) | 0.574 |
| ICU length of stay, h | 2.97 (7.27) | 15.86 (26.73) | 0.245 | 46.21 (82.1) | 63.91 (235.12) | 0.824 | 16.04 (39.44) | 32.0 (120.44) | 0.591 |
NOTE. Data is present as mean (SD) or count (%) where appropriate.
Abbreviations: AF, atrial fibrillation; CABG, coronary artery bypass graft; ED, emergency department; ICU, intensive care unit; TAVR, transcatheter aortic valve replacement; ZCTA, ZIP code tabulation area.
Fig 1.
ZIP code tabulation area–median income data for pre-COVID, COVID year 1 and COVID year 2 in Latino/Hispanic versus non-Latino/Hispanic Patients in (A) atrial fibrillation ablation, (B) coronary artery bypass graft, and (C) transcatheter aortic valve replacement. The median income was divided into deciles (10 bins) and charted as a smooth histogram as a frequency of the total population for each ethnic group and period.
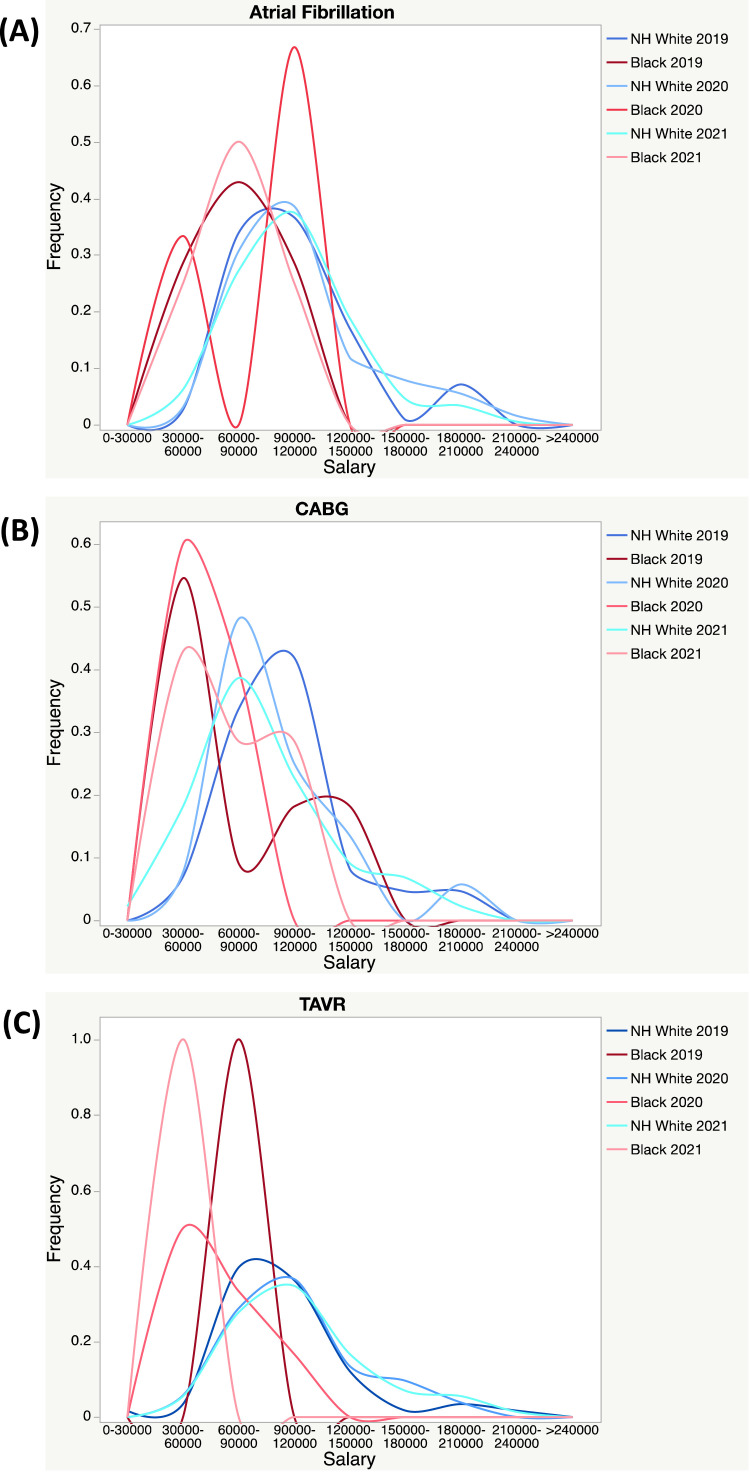
Similar to Latino and/or Hispanic patients, Black and/or African American patients were statistically younger than their non-Hispanic White peers when undergoing CABG (Table 7, Table 8, Table 9 ). For all procedures, the addresses of Black and/or African American patients were in ZIP codes with lower median income, a higher percentage of families in poverty, and an increased percentage of unemployment. The smoothed histogram of the median income deciles revealed that non-Hispanic White patients tended to have a right-skewed distribution, with a higher median income mode compared to Black and/or African Americans (Fig 2 ). There were no differences in the total hospital and intensive care unit lengths of stay between these 2 racial groups.
Table 7.
AF Ablation in Non-Hispanic White and Black and/or African American Patients Across COVID Years
| Pre-COVID |
COVID Year 1 |
COVID Year 2 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-Hispanic White (n = 110) | Black and/or African American (n = 7) | p | Non-Hispanic White (n = 126) | Black and/or African American (n = 3) | p | Non-Hispanic White (n = 173) | Black and/or African American (n = 4) | p | |
| Age, y | 64.76 (11.14) | 68.57 (11.63) | 0.581 | 64.49 (10.76) | 63.0 (14.73) | 0.581 | 67.66 (10.28) | 57.75 (10.31) | 0.581 |
| Female sex | 41 (37.27) | 2 (28.57) | 0.953 | 37 (29.36) | 1 (33.3) | 1 | 68 (39.30) | 1 (25.0) | 0.951 |
| Insurance provider | 0.367 | 0.861 | < 0.005 | ||||||
| Commercial | 56 (50.90) | 2 (28.57) | 57 (45.23) | 1 (33.33) | 64 (36.99) | 1 (25.0) | |||
| Medi-Cal | 1 (0.90) | 0 (0.0) | 1 (0.79) | 0 (0.0) | 1 (0.57) | 1 (25.0) | |||
| Medicare | 44 (40.0) | 3 (42.85) | 50 (39.68) | 1 (33.33) | 83 (47.97) | 1 (25.0) | |||
| Other | 1 (0.90) | 0 (0.0) | 3 (2.38) | 0 (0.0) | 1 (0.57) | 0 (0.0) | |||
| Managed care | 8 (7.27) | 2 (28.57) | 15 (11.90) | 1 (33.33) | 24 (13.87) | 1 (25.0) | |||
| Preprocedure admission status | 1 | 1 | 1 | ||||||
| Same day admit | 108 (98.18) | 7 (100.0) | 125 (99.20) | 3 (100.0) | 170 (98.26) | 4 (100.0) | |||
| Inpatient | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| ED admit | 2 (1.81) | 0 (0.0) | 1 (0.79) | 0 (0.0) | 3 (1.73) | 0 (0.0) | |||
| Socioeconomic factors (ZCTA-based) | |||||||||
| Median income deciles, USD | 105,192 (355,44) | 77,871 (15,909) | 0.005 | 108,987 (36,450) | 84,636 (28,757) | 0.005 | 104,752 (33,560) | 80,059 (19,672) | 0.005 |
| Families in poverty, n (%) | 5.29 (3.31) | 7.0 (3.47) | 0.021 | 5.19 (3.08) | 7.83 (4.59) | 0.021 | 5.73 (3.73) | 8.5 (3.49) | 0.021 |
| Unemployed, n (%) | 5.93 (1.84) | 6.53 (1.79) | 0.075 | 5.38 (1.48) | 5.4 (2.42) | 0.075 | 5.61 (1.66) | 7.05 (1.4) | 0.075 |
| Outcomes | |||||||||
| Hospital length of stay, h | 32.79 (34.1) | 26.0 (9.38) | 0.737 | 21.06 (10.64) | 22.33 (9.81) | 0.737 | 21.4 (16.88) | 16.0 (5.72) | 0.737 |
| ICU length of stay, h | 2.8 (14.48) | 0.0 (0.0) | 0.665 | 0.4 (4.47) | 0.0 (0.0) | 0.665 | 0.13 (1.76) | 0.0 (0.0) | 0.665 |
NOTE. Data is present as mean (SD) or count (%) where appropriate.
Abbreviations: AF, atrial fibrillation; CABG, coronary artery bypass graft; ED, emergency department; ICU, intensive care unit; TAVR, transcatheter aortic valve replacement; ZCTA, ZIP code tabulation area.
Table 8.
CABG in Non-Hispanic White and Black and/or African American Patients Across COVID Years
| Pre-COVID |
COVID Year 1 |
COVID Year 2 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-Hispanic White (n = 86) | Black and/or African American (n = 11) | p | Non-Hispanic White (n = 52) | Black and/or African American (n = 5) | p | Non-Hispanic White (n = 71) | Black and/or African American (n = 7) | p | |
| Age, y | 67.14 (9.03) | 61.27 (12.17) | 0.003 | 67.08 (7.82) | 62.6 (14.83) | 0.003 | 66.38 (9.84) | 58.43 (11.15) | 0.003 |
| Female sex | 14 (16.27) | 1 (9.091) | 0.859 | 9 (17.30) | 2 (40.0) | 0.526 | 11 (15.49) | 0 (0.0) | 0.579 |
| Insurance provider | 0.121 | 0.048 | 0.996 | ||||||
| Commercial | 24 (27.90) | 4 (36.36) | 23 (44.23) | 0 (0.0) | 21 (29.57) | 2 (28.57) | |||
| Medi-Cal | 2 (2.32) | 2 (18.18) | 1 (1.92) | 1 (20.0) | 8 (11.26) | 1 (14.28) | |||
| Medicare | 45 (52.32) | 4 (36.36) | 25 (48.07) | 3 (60.0) | 31 (43.66) | 3 (42.85) | |||
| Other | 4 (4.65) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| Managed care | 11 (12.79) | 1 (9.09) | 3 (5.76) | 1 (20.0) | 11 (15.49) | 1 (14.28) | |||
| Pre-procedure admission status | 0.885 | 0.152 | 0.994 | ||||||
| Same day admit | 38 (44.18) | 4 (36.36) | 25 (48.07) | 1 (20.0) | 42 (59.15) | 4 (57.14) | |||
| Inpatient | 21 (24.41) | 3 (27.27) | 11 (21.15) | 3 (60.0) | 10 (14.08) | 1 (14.28) | |||
| ED admit | 27 (31.39) | 4 (36.36) | 16 (30.76) | 1 (20.0) | 19 (26.76) | 2 (28.57) | |||
| Socioeconomic factors, ZCTA-based | |||||||||
| Median income deciles, USD | 99,316 (33,917.72) | 76,893 (32,659.55) | < 0.005 | 96,741 (34,341.0) | 57,120 (5,354.97) | < 0.005 | 99,547 (38,651.74) | 69,212 (20,583.61) | < 0.005 |
| Families in poverty, n (%) | 6.31 (3.89) | 11.03 (6.39) | < 0.005 | 6.51 (4.59) | 15.96 (4.36) | < 0.005 | 6.88 (5.18) | 10.89 (6.86) | < 0.005 |
| Unemployed, n (%) | 5.92 (1.82) | 6.76 (1.74) | < 0.005 | 5.78 (1.58) | 9.1 (0.53) | < 0.005 | 5.91 (1.75) | 6.19 (1.69) | < 0.005 |
| Outcomes | |||||||||
| Hospital length of stay, h | 364.78 (333.79) | 267.82 (120.95) | 0.536 | 343.73 (412.72) | 328.6 (83.39) | 0.536 | 293.32 (245.7) | 304.71 (183.32) | 0.536 |
| ICU length of stay, h | 233.07 (368.95) | 109.41 (47.39) | 0.54 | 223.89 (538.03) | 180.7 (109.09) | 0.54 | 114.48 (99.35) | 170.76 (163.81) | 0.54 |
NOTE. Data is present as mean (SD) or count (%) where appropriate.
Abbreviations: AF, atrial fibrillation; CABG, coronary artery bypass graft; ED, emergency department; ICU, intensive care unit; TAVR, transcatheter aortic valve replacement; USD, United States dollars; ZCTA, ZIP code tabulation area.
Table 9.
TAVR in Non-Hispanic White and Black and/or African American Patients Across COVID Years
| Pre-COVID |
COVID Year 1 |
COVID Year 2 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-Hispanic White (n = 58) | Black and/or African American (n = 1) | p | Non-Hispanic White (n = 51) | Black and/or African American (n = 6) | p | Non-Hispanic White (n = 71) | Black and/or African American (n = 7) | p | |
| Age, y | 79.34 (8.12) | 81.0 (NA) | 0.295 | 79.96 (8.86) | 72.67 (7.09) | 0.295 | 78.97 (8.15) | 80.0 (10.63) | 0.295 |
| Female sex | 23 (39.65) | 0 (0.0) | 1 | 21 (41.17) | 3 (50.0) | 1 | 29 (40.84) | 3 (42.85) | 1 |
| Insurance provider | 0.854 | 0.336 | 0.738 | ||||||
| Commercial | 5 (8.62) | 0 (0.0) | 1 (1.96) | 0 (0.0) | 5 (7.04) | 0 (0.0) | |||
| Medi-Cal | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (2.81) | 0 (0.0) | |||
| Medicare | 44 (75.86) | 1 (100.0) | 37 (72.54) | 6 (100.0) | 60 (84.50) | 7 (100.0) | |||
| Other | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| Managed care | 9 (15.51) | 0 (0.0) | 13 (25.4) | 0 (0.0) | 4 (5.63) | 0 (0.0) | |||
| Pre-procedure admission status | 0.109 | 0.021 | 0.668 | ||||||
| Same day admit | 40 (68.96) | 0 (0.0) | 40 (78.43) | 2 (33.33) | 57 (80.28) | 5 (71.42) | |||
| Inpatient | 8 (13.79) | 0 (0.0) | 6 (11.76) | 1 (16.66) | 4 (5.63) | 1 (14.28) | |||
| ED admit | 10 (17.24) | 1 (100.0) | 5 (9.80) | 3 (50.0) | 10 (14.08) | 1 (14.28) | |||
| Socioeconomic factors, ZCTA-based | |||||||||
| Median income deciles, USD | 100,244 (35,357.25) | 84,505.0 (NA) | < 0.005 | 104,471 (31,567.08) | 64,990 (21,515.43) | < 0.005 | 109,082 (38,331.42) | 49,679 (6,508.79) | < 0.005 |
| Families in poverty, n (%) | 5.48 (3.57) | 5.4 (NA) | < 0.005 | 5.93 (3.71) | 13.85 (7.52) | < 0.005 | 5.07 (3.35) | 17.36 (6.51) | < 0.005 |
| Unemployed, n (%) | 5.97 (1.87) | 5.5 (NA) | < 0.005 | 5.44 (1.57) | 6.8 (1.89) | < 0.005 | 5.69 (1.74) | 9.3 (0.79) | < 0.005 |
| Outcomes | |||||||||
| Hospital length of stay, h | 123.69 (121.92) | 191.0 (NA) | 0.706 | 121.75 (155.78) | 229.83 (123.04) | 0.706 | 147.49 (349.69) | 90.71 (109.9) | 0.706 |
| ICU length of stay, h | 16.98 (26.78) | 0.0 (NA) | 0.659 | 54.96 (229.05) | 40.43 (99.04) | 0.659 | 35.19 (130.43) | 0.0 (0.0) | 0.659 |
NOTE. Data is present as mean (SD) or count (%) where appropriate.
Abbreviations: AF, atrial fibrillation; CABG, coronary artery bypass graft; ED, emergency department; ICU, intensive care unit; TAVR, transcatheter aortic valve replacement; ZCTA, ZIP code tabulation area.
Fig 2.
ZIP code tabulation area–median income data for pre-COVID, COVID Year 1 and COVID Year 2 in Black and/or African American versus non-Hispanic White patients in (A) atrial fibrillation ablation, (B) coronary artery bypass graft, and (C) transcatheter aortic valve replacement. The median income was divided into deciles (10 bins) and charted as a smooth histogram as a frequency of the total population for each ethnic group and period. CABG, coronary artery bypass graft; TAVR, transcatheter aortic valve replacement.
The population-adjusted procedural incidence rate was higher for White patients compared to Black patients, and for non-Hispanic patients compared to Hispanic patients at every time point in the study period (Table 10-11 ). For AF ablation, the difference in procedural incidence rates between non-Hispanic White patients and Black and/or African American patients increased from 3.63-to-4.72 to 6.51 per 100,000 persons in the pre-COVID, COVID Year 1, and COVID Year 2 groups, respectively. A similar trend was seen when comparing non-Latino and/or non-Hispanic patients to Latino and/or Hispanic patients, as the difference in procedural incidence rates increased from 2.57-to-2.7 to 3.54 per 100,000 persons in the pre-COVID, COVID Year 1, and COVID Year 2 groups, respectively. The largest differences in population-adjusted procedural incidence rates between White patients and Black patients and between non-Hispanic patients and Hispanic patients were seen with AF ablation rates in all 3 study time periods (Table 10-11).
Table 10.
Comparison of population-adjusted incidence rates of cardiac procedures per 100,000 persons in Los Angeles County by Race
| Pre-COVID |
COVID Year 1 |
COVID Year 2 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Non-Hispanic White | Black/Afr. American | Difference | Non-Hispanic White | Black/Afr. AfricanAmerican | Difference | Non-Hispanic White | Black/Afr. AfricanAmerican | Difference | |
| AF ablation | 4.42 | 0.79 | 3.63 | 5.06 | 0.34 | 4.72 | 6.96 | 0.45 | 6.51 |
| CABG | 3.46 | 1.24 | 2.22 | 2.09 | 0.57 | 1.52 | 2.85 | 0.79 | 2.06 |
| TAVR | 2.33 | 0.11 | 2.22 | 2.05 | 0.68 | 1.37 | 2.85 | 0.79 | 2.06 |
NOTE. Data are presented as mean (SD) or count (%) where appropriate.
Abbreviations: AF, atrial fibrillation; CABG, coronary artery bypass graft; TAVR, transcatheter aortic valve replacement.
Table 11.
Comparison of population-adjusted incidence rates of cardiac procedures per 100,000 persons in Los Angeles County by ethnicity
| Pre-COVID |
COVID Year 1 |
COVID Year 2 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Latino or Hispanic | Non-Latino or Hispanic | Difference | Latino or Hispanic | Non-Latino or Hispanic | Difference | Latino or Hispanic | Non-Latino or Hispanic | Difference | |
| AF ablation | 0.15 | 2.72 | 2.57 | 0.22 | 2.92 | 2.7 | 0.56 | 4.10 | 3.54 |
| CABG | 0.56 | 2.59 | 2.03 | 0.72 | 1.69 | 0.97 | 0.6 | 2.20 | 1.6 |
| TAVR | 0.12 | 1.45 | 1.33 | 0.19 | 1.43 | 1.24 | 0.35 | 1.68 | 1.33 |
NOTE. Data are presented as mean (SD) or count (%) where appropriate.
Abbreviations: AF, atrial fibrillation; CABG, coronary artery bypass graft; TAVR, transcatheter aortic valve replacement.
For TAVR, the difference in procedural incidence rates between White patients and Black patients decreased from 2.22 per 100,000 persons in the pre-COVID group to 1.37 per 100,00 persons in COVID Year 1 prior to returning to a similar difference in COVID Year 2 (2.06 per 100,000). The procedural incidence rates between non-Latino and/or non-Hispanic patients to Latino and/or Hispanic patients undergoing TAVR remained relatively stable throughout all 3 time periods, 1.33-to-1.43 to 1.33 per 100,000 persons.
For CABG, the difference in procedural incidence rates between White patients and Black patients decreased between pre-COVID and COVID Year 1 prior to returning to pre-COVID rates in COVID Year 2, 2.22-to-1.52 to 2.06 per 100,000 persons, respectively. From pre-COVID to COVID Year 1, the difference in procedural incidence rates for Hispanic and/or Latino versus non-Hispanic and/or non-Latino decreased, 2.03-to-0.97 per 100,000 persons. Between COVID Year 1 and Year 2, the difference increased from 0.97 to 1.6 per 100,000 persons, though it did not return to the pre-COVID rate.
Discussion
In this study, the authors reported data on discrepancies in procedural incidence rates between non-Hispanic White and Black and/or African American patients, and between non-Latino and/or non-Hispanic and Latino and/or Hispanic patients, and how these differences changed over time at the authors’ institution. The COVID-19 pandemic was associated with an increase in disparities between White and Black patients and between non-Hispanic and Hispanic patients with AF undergoing catheter ablations. Surprisingly, the disparities between non-Hispanic White and Black and/or African American patients, and between non-Latino Hispanic and Latino and/or Hispanic patients undergoing CABG and TAVR decreased with the onset of the COVID-19 pandemic prior to returning to near prepandemic rates. The disparities between non-Hispanic and Hispanic patients undergoing TAVR did not change significantly over time.
Racial and ethnic disparities in access to healthcare have been previously reported in various fields. One broad-ranging study published by the American Public Health Association reported that White patients were more likely to receive higher-cost care and have access to higher-technology health services compared to Black patients, and that the disparity could not be explained by differences in the disease prevalence, patients’ clinical characteristics, or financial barriers.5 Racial and ethnic disparities in the use of surgical procedures have been well-described across a variety of surgical subspecialties.2, 3, 4, 5 Despite numerous national and local initiatives to reduce racial differences in access to healthcare, Jha et al. found no meaningful change in disparities between White and Black Medicare enrollees.1 Although healthcare-focused interventions are important, they are insufficient to fully address health disparities if social determinants of health, such as economic stability and opportunity, access to quality education, safe and affordable housing, food security, and community support and/or engagement access, are not also addressed.
The discrepancy in procedural and surgical rates is also evident in cardiovascular care. With regard to coronary artery disease, previous studies have published data showing lower rates of myocardial revascularization by percutaneous interventions or CABG in Black patients compared to White patients.7, 8, 9 , 16 , 17 There also have been previous reports of discrepancies in the use of catheter ablation in patients with AF18, 19, 20 and, more recently, in access to TAVR procedures in patients with aortic stenosis.21, 22, 23 The disparities are not limited to just access to cardiac procedures and surgeries, but also include worse outcomes and increased mortality for minorities who undergo such procedures.5 , 6 In the authors’ present study, they similarly found that the procedural incidence rates were higher for White and non-Latino and/or Hispanic patients undergoing CABG, AF ablation, and TAVR at every time point throughout the study period. This was consistent with data that have been reported previously in the literature.
The COVID-19 pandemic has also disproportionately affected minority Americans more so than White Americans. Minorities are more likely to be of lower socioeconomic status, suffer from chronic medical conditions that are poorly controlled, have lower healthcare literacy and access to healthcare, and experience living and working conditions that predispose them to worse outcomes.24 Though the most pervasive disparities have been reported among Black and Hispanic patients, there are data to suggest that these disparities exist for other minorities such as American Indian and/or Alaskan Native and Native Hawaiian and/or Pacific Islander populations as well.12 Other studies have reported higher incidences of COVID-19 and COVID-19-related hospitalizations and deaths in racial and ethnic minority groups compared to White Americans.13 , 25 , 26
Nevertheless, there is a paucity of data analyzing the effects of the COVID-19 pandemic on access to cardiac procedural care. The authors initially hypothesized that the disparities in cardiac procedure rates would be exacerbated by the pandemic considering the previously published data. Interestingly, they found that discrepancies in procedural rates for Black and Hispanic patients requiring CABG and TAVR decreased at the onset of the pandemic. As COVID disproportionately affected minority populations, an unintended consequence of this disparity may have been that more minority patients interacted with the healthcare system during COVID, and more underlying cardiac conditions were diagnosed and treated. This increased minority patient-healthcare interaction may have led to better access at a higher-level center for cardiac procedural care that was more urgent or emergent, such as severe aortic stenosis and acute coronary syndromes. In this study, the authors also found that discrepancies in the procedural rates for Black and Hispanic patients undergoing AF ablation increased significantly during the pandemic, which they posit may be a disappointing trend toward worsening disparities in access to more elective, nonurgent procedures for minorities. Given the observational nature of this study and the multitude of potential confounding factors, the authors cannot conclude definitively that the COVID-19 pandemic was responsible for these trends. However, their data did confirm that disparities in access to cardiac procedural care are still prevalent at their institution.
The causes of disparities in healthcare access and delivery are multifactorial, and, as such, strategies to reduce these disparities must be multifaceted. One approach has been a push to improve the diversification and cultural competency of the healthcare workforce, as there is evidence to suggest this may help address racial and ethnic disparities.27 , 28 In the last 5 years, there have been exponential increases in publications and discussions regarding the effective implementation of diversity, equity, and inclusion programs in all aspects of medicine, nursing, and science.29, 30, 31, 32, 33, 34, 35 Although some progress has been made, there is ample evidence that racial and ethnic disparities still remain prevalent.34 , 36 , 37 The authors’ institution participates in several diversity, equity, and inclusion programs to introduce underrepresented minority students at all training levels to medicine, and engages with the community to promote education and build support networks to ensure they can be a trusted resource for at-risk populations. As COVID has shown, the populace needs to know that healthcare remains a ‘helping’ profession that can be trusted to care for individuals in moments of vulnerability.
Despite efforts within the healthcare system, perhaps the largest contributing causes to these disparities are related to social determinants of health that are external to healthcare systems.27 In this study, Black and/or African American and Latino and/or Hispanic patients were more likely to reside within areas with indicators of lower socioeconomic status, such as lower median income and a higher percentage of families living in poverty or dealing with unemployment. Therefore, interventions focused on the healthcare sector are most likely to be insufficient to address these population-level health disparities. Thornton et al. reviewed the evidence and presented recommendations for a multipronged approach to reducing health disparities, including interventions surrounding early childhood education, parental support programs, urban planning and community development, housing quality and neighborhood safety, income enhancements and supplements, and specific employment interventions.38 There are, of course, financial and logistical challenges to the implementation of these strategies that need to be addressed in order to make any progress in reducing healthcare disparities. Governmental advocacy at the local, state, and federal levels is important to inform lawmakers and policymakers of the extent of the problem, and there is a political will to address these problems with novel, evidence-based solutions that are multidisciplinary in nature. Local and national nongovernmental organizations and most medical societies are involved in these activities and can serve as a good resource for those who want further information.
This study had a few inherent limitations that should be acknowledged. The data collected and analyzed in this study were dependent on the accuracy and completeness of records stored in the authors’ institutional databases and the reliability of their automated electronic data extraction tools. Because this was a retrospective analysis, the authors were unable to verify the accuracy of each patient's reported race and ethnicity, and it is possible that patients who declined to report their race or ethnicity or reported “Other” may have been misclassified. It is also possible that other clinical practice changes during the COVID-19 pandemic may have occurred over the study period, resulting in unknown confounders that may have influenced the outcomes of this study. Particularly during the first year of the pandemic, resource allocation was constantly shifted in order to manage the increased hospitalizations due to COVID and its associated sequelae. The authors chose to study AF ablation, CABG, and TAVR, as they are associated with cardiovascular pathophysiology that requires prompt intervention. Though they did see a decline in these cases in the first year of the pandemic, the authors’ institution made every effort to limit cancellations for urgent cardiac procedures and perform these procedures within a narrow frame of time after the initial cancellation to ensure timely patient care. Lastly, the authors report data from a single tertiary-care academic institution with a diverse patient population, and the results may not be generalizable to other clinical settings or institutions.
Conclusion
In conclusion, racial and ethnic disparities in access to cardiac procedural care were present throughout all study time periods at the authors’ institution. The COVID-19 pandemic was associated with an increase in disparities for patients undergoing AF ablation, a decrease in disparities for patients undergoing TAVR, and no change in disparities for patients undergoing CABG. The findings of this study reinforce the continuing need for initiatives to reduce racial and ethnic disparities in medicine and to achieve equal access to healthcare.
Conflict of Interest
None.
Footnotes
This material was presented at Society of Cardiovascular Anesthesiologist's 44th Annual Meeting in May 2022 as a poster.
References
- 1.Jha AK, Fisher ES, Li Z, et al. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353:683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 2.Best MJ, McFarland EG, Thakkar SC, et al. Racial disparities in the use of surgical procedures in the US. JAMA Surg. 2021;156:274. doi: 10.1001/jamasurg.2020.6257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goodman SM, Parks ML, McHugh K, et al. Disparities in outcomes for African Americans and Whites undergoing total knee arthroplasty: A systematic literature review. J Rheumatol. 2016;43:765–770. doi: 10.3899/jrheum.150950. [DOI] [PubMed] [Google Scholar]
- 4.Schoenfeld AJ, Sturgeon DJ, Dimick JB, et al. Disparities in rates of surgical intervention among racial and ethnic minorities in medicare accountable care organizations. Ann Surg. 2019;269:459–464. doi: 10.1097/SLA.0000000000002695. [DOI] [PubMed] [Google Scholar]
- 5.Escarce JJ, Epstein KR, Colby DC, et al. Racial differences in the elderly's use of medical procedures and diagnostic tests. Am J Public Health. 1993;83:948–954. doi: 10.2105/ajph.83.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schoenbaum M, Waidmann T. Race, socioeconomic status, and health: Accounting for race differences in health. J Gerontol B Psychol Sci Soc Sci. 1997;52(Spec No):61–73. doi: 10.1093/geronb/52b.special_issue.61. [DOI] [PubMed] [Google Scholar]
- 7.Gaglia MA, Shavelle DM, Tun H, et al. African-American patients are less likely to receive drug-eluting stents during percutaneous coronary intervention. Cardiovasc Revascularization Med Mol Interv. 2014;15:214–218. doi: 10.1016/j.carrev.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Albert MA, Ayanian JZ, Silbaugh TS, et al. Early results of Massachusetts healthcare reform on racial, ethnic, and socioeconomic disparities in cardiovascular care. Circulation. 2014;129:2528–2538. doi: 10.1161/CIRCULATIONAHA.113.005231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kressin NR, Petersen LA. Racial differences in the use of invasive cardiovascular procedures: Review of the literature and prescription for future research. Ann Intern Med. 2001;135:352–366. doi: 10.7326/0003-4819-135-5-200109040-00012. [DOI] [PubMed] [Google Scholar]
- 10.Lillie-Blanton M, Maddox TM, Rushing O, et al. Disparities in cardiac care: Rising to the challenge of healthy people 2010. J Am Coll Cardiol. 2004;44:503–508. doi: 10.1016/j.jacc.2004.04.043. [DOI] [PubMed] [Google Scholar]
- 11.Trivedi AN, Sequist TD, Ayanian JZ. Impact of hospital volume on racial disparities in cardiovascular procedure mortality. J Am Coll Cardiol. 2006;47:417–424. doi: 10.1016/j.jacc.2005.08.068. [DOI] [PubMed] [Google Scholar]
- 12.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323:2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joynt Maddox KE, Reidhead M, Grotzinger J, et al. Understanding contributors to racial and ethnic inequities in COVID-19 incidence and mortality rates. PloS One. 2022;17 doi: 10.1371/journal.pone.0260262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.United States Census Bureau Quick Facts Los Angeles County, California. Available at: https://www.census.gov/quickfacts/losangelescountycalifornia. Accessed June 22, 2022.
- 16.Canto JG, Allison JJ, Kiefe CI, et al. Relation of race and sex to the use of reperfusion therapy in Medicare beneficiaries with acute myocardial infarction. N Engl J Med. 2000;342:1094–1100. doi: 10.1056/NEJM200004133421505. [DOI] [PubMed] [Google Scholar]
- 17.Schneider EC, Leape LL, Weissman JS, et al. Racial differences in cardiac revascularization rates: Does “overuse” explain higher rates among white patients? Ann Intern Med. 2001;135:328–337. doi: 10.7326/0003-4819-135-5-200109040-00009. [DOI] [PubMed] [Google Scholar]
- 18.Tamariz L, Rodriguez A, Palacio A, et al. Racial disparities in the use of catheter ablation for atrial fibrillation and flutter. Clin Cardiol. 2014;37:733–737. doi: 10.1002/clc.22330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naderi S, Rodriguez F, Wang Y, Foody JM. Racial disparities in hospitalizations, procedural treatments and mortality of patients hospitalized with atrial fibrillation. Ethn Dis. 2014;24:144–149. [PubMed] [Google Scholar]
- 20.Eberly LA, Garg L, Yang L, et al. Racial/ethnic and socioeconomic disparities in management of incident paroxysmal atrial fibrillation. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.0247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hernandez-Suarez DF, Ranka S, Villablanca P, et al. Racial/ethnic disparities in patients undergoing transcatheter aortic valve replacement: Insights from the healthcare cost and utilization project's national inpatient sample. Cardiovasc Revascularization Med Mol Interv. 2019;20:546–552. doi: 10.1016/j.carrev.2019.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ali A, Mather JF, McMahon S, et al. Racial and ethnic disparities in the use of transcatheter aortic valve replacement in the state of Connecticut. Cardiovasc Revascularization Med Mol Interv. 2022;37:7–12. doi: 10.1016/j.carrev.2021.06.120. [DOI] [PubMed] [Google Scholar]
- 23.Nathan AS, Yang L, Yang N, et al. Racial, ethnic, and socioeconomic disparities in access to transcatheter aortic valve replacement within major metropolitan areas. JAMA Cardiol. 2022;7:150–157. doi: 10.1001/jamacardio.2021.4641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tai DBG, Shah A, Doubeni CA, et al. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis Off Publ Infect Dis Soc Am. 2021;72:703–706. doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mackey K, Ayers CK, Kondo KK, et al. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: A systematic review. Ann Intern Med. 2021;174:362–373. doi: 10.7326/M20-6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khanijahani A, Iezadi S, Gholipour K, et al. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. Int J Equity Health. 2021;20:248. doi: 10.1186/s12939-021-01582-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Betancourt JR, Green AR, Carrillo JE. Ananeh-Firempong O. Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118:293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000;57(Suppl 1):181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gill GK, McNally MJ, Berman V. Effective diversity, equity, and inclusion practices. Healthc Manage Forum. 2018;31:196–199. doi: 10.1177/0840470418773785. [DOI] [PubMed] [Google Scholar]
- 30.Morrison V, Hauch RR, Perez E, et al. M. Diversity, Equity, and Inclusion in Nursing: The Pathway to Excellence Framework Alignment. Nurs Adm Q. 2021;45:311–323. doi: 10.1097/NAQ.0000000000000494. [DOI] [PubMed] [Google Scholar]
- 31.Capers Q, Johnson A, Berlacher K, et al. The urgent and ongoing need for diversity, inclusion, and equity in the cardiology workforce in the United States. J Am Heart Assoc. 2021;10 doi: 10.1161/JAHA.120.018893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moreno FA. Diversity, equity, and inclusion in psychiatry. Focus Am Psychiatr Publ. 2020;18:1. doi: 10.1176/appi.focus.18101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Estime SR, Lee HH, Jimenez N, et al. Diversity, equity, and inclusion in anesthesiology. Int Anesthesiol Clin. 2021;59:81–85. doi: 10.1097/AIA.0000000000000337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhu K, Das P, Karimuddin A, et al. Equity, diversity, and inclusion in academic American surgery faculty: An elusive dream. J Surg Res. 2021;258:179–186. doi: 10.1016/j.jss.2020.08.069. [DOI] [PubMed] [Google Scholar]
- 35.Russell RS. Equity, diversity, and inclusion in Science. Viral Immunol. 2020;33:535. doi: 10.1089/vim.2020.0249. [DOI] [PubMed] [Google Scholar]
- 36.Sanchez AN, Martinez CI, Stampas A, et al. Ethnic and racial diversity in academic physical medicine and rehabilitation compared with all other medical specialties. Am J Phys Med Rehabil. 2021;100:S12–S16. doi: 10.1097/PHM.0000000000001486. [DOI] [PubMed] [Google Scholar]
- 37.Chaudhary AMD, Naveed S, Siddiqi J, et al. US psychiatry faculty: Academic rank, gender and racial profile. Acad Psychiatry J Am Assoc Dir Psychiatr Resid Train Assoc Acad Psychiatry. 2020;44:260–266. doi: 10.1007/s40596-020-01192-2. [DOI] [PubMed] [Google Scholar]
- 38.Thornton RLJ, Glover CM, Cené CW, et al. Evaluating strategies for reducing health disparities by addressing the social determinants of health. Health Aff (Millwood) 2016;35:1416–1423. doi: 10.1377/hlthaff.2015.1357. [DOI] [PMC free article] [PubMed] [Google Scholar]