Abstract
Older patients with hypertension are at a higher risk of cardiovascular events compared to younger adults but are also more vulnerable to the adverse effects of blood pressure (BP) lowering. Frailty is an important predictor of vulnerability to such adverse events, and age alone may not best reflect underlying risk. Therefore, an individualised approach to management of hypertension in the older person is required. Such an approach requires knowledge of frailty, the physiology of hypertension and ageing and a contextual understanding of best evidence. Management needs to be holistic and take account of the older person's care needs, wishes and priorities. This review describes physiological considerations and current guidelines and best practices regarding BP lowering in older people and highlights areas with paucity of evidence. A proposed and testable approach to managing hypertension in the older person (≥70 years) is discussed.
Keywords: ageing, blood pressure, hypertension
Introduction
Hypertension is an important modifiable cardiovascular risk factor in older people. In Australia, the proportion of those ≥75 years who report a diagnosis of hypertension is 42%. 1 Research suggests that hypertension is undertreated in some older patients, but in some who may be more vulnerable to the adverse effects of blood pressure (BP) lowering, treatment is overprescribed. 2
This narrative review summarises evidence regarding the safety and efficacy of BP lowering therapy in older people. This review first describes physiological considerations for BP lowering relevant to the older patient, such as frailty and arterial stiffening, which may not correlate well with chronological age. It then discusses the potential benefits of BP lowering for cardiovascular events and dementia, the adverse effects of BP lowering, and currently recommended BP targets in older people, highlighting where there is a lack of clear evidence. Finally, a proposed and testable approach to managing hypertension in the older patient (defined as ≥70 years) is discussed.
BP and ageing: physiological changes
Systolic blood pressure (SBP) increases from middle age, while diastolic BP decreases. 3 , 4 , 5 This is due to stiffening of the arteries owing to gradual replacement of elastin with collagen, as well as other changes that occur with ageing and in some diseases. 3 In normal physiologic circumstances (such as in a young adult), the large arteries, especially the aorta, create a reservoir effect, expanding and holding blood during cardiac systole and contracting and projecting blood forward during diastole, resulting in even BP throughout the cardiac cycle (normal pulse pressure). 6 However, in older people, when the large arteries are affected by stiffening, the aortic reservoir cannot expand and store as much blood; therefore, a higher pressure is reached during systole, and pressure is lower during diastole due to the lack of blood flow from the reservoir during diastole (widening pulse pressure, see Fig. 1). 6
Figure 1.
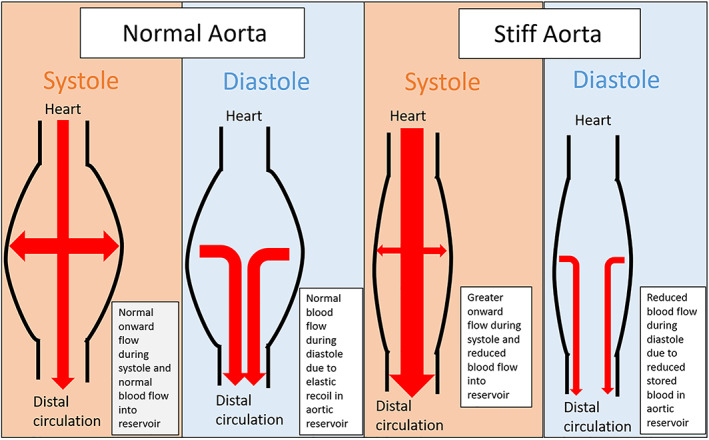
The aortic reservoir.
It is for this reason that isolated systolic hypertension is common among older patients, while diastolic hypertension is uncommon, and why the range of pulse pressure is wider in older adults on average compared to younger adults. 4 Systolic hypertension is a stronger risk factor for adverse cardiovascular outcomes compared to diastolic hypertension. 4 Postural hypotension is also associated with older age 7 due to these haemodynamic changes but also due to blunted baroreceptor responses that occur with ageing. 8 Such patients may also suffer from supine hypertension, which can make optimising their BP very challenging. 9
Frailty
Frailty is a syndrome of age‐related multi‐organ dysfunction that renders a person more vulnerable to stressor events. 10 , 11 Fried's criteria comprise weight loss, self‐reported exhaustion, grip strength, walking speed and physical activity, 11 whereas Rockwood et al. defined frailty using functional status, such as requiring assistance for daily activities 10 (Table 1). Geriatricians have long been aware of the association between antihypertensive therapy and fall risk in frail older people. 13 However, cardiovascular events are also a highly undesirable outcome for many older people, and quantifying the benefit of antihypertensive therapy compared to the risk is challenging and likely to be modified not only by age but degree of frailty. 14
Table 1.
Rockwood clinical frailty Scale 12
| Category | Summary | Description |
|---|---|---|
| 1 | Very fit | Robust, active, energetic, exercise regularly |
| 2 | Well | No active disease symptoms but less fit than category 1 |
| 3 | Managing well | People whose medical problems are well controlled but who are not regularly active beyond routine walking |
| 4 | Vulnerable | While not dependent on others for daily help, symptoms often limit activities |
| 5 | Mildly frail | More evident slowing, need help in higher order activities of daily living |
| 6 | Moderately frail | Need help with all outside activities and keeping house inside. May need bathing assistance |
| 7 | Severely frail | Completely dependent for personal care |
| 8 | Very severely frail | Completely dependent and approaching the end of life |
| 9 | Terminally ill | Life expectancy <6 months, may be otherwise non‐frail |
Among octogenarians and older, the prevalence of frailty may be as high as 50%, but this is by no means universal. 10 Age‐related changes in BP occur gradually from middle age but are modified by comorbid conditions affecting arterial stiffening like diabetes, obesity and prior cardiovascular disease. 3 , 5 This means that using age alone to study the benefits of BP lowering has significant limitations, given that individuals of the same age may have markedly different cardiovascular risks and susceptibility to adverse effects of BP lowering. In addition, the definition of an older person is changing. The age of retirement is transitioning from 65 to 70 years in many countries, including Australia, reflecting that adults are increasingly able‐bodied through their 60s, thanks to increasing life expectancy and reduced disability. 15 Due to such changes, there is substantial variation in the definition of older age among studies, 16 , 17 which makes understanding the effect of age on BP lowering more difficult. Given that individuals of the same age often vary markedly in their degree of frailty, frailty measures may be more useful for stratifying individuals at higher risk of adverse effects of BP lowering than purely age‐based criteria.
BP lowering for primary prevention in older people
For reasons already discussed, older people are at a higher risk of cardiovascular events than younger adults, 4 , 18 but they may also be at higher risk of adverse outcomes related to BP lowering, 19 , 20 including falls 21 and mortality. 20 There is also evidence that maintaining BP in ranges considered normal in younger adults might be associated with harm in older people. Douros et al. performed a cohort study of an older general population sample with treated hypertension and found that those people ≥80 years who had SBP <140 mmHg had a higher risk of mortality and cardiovascular events, but this was not seen in those 70–79 years. 22 Masoli et al. performed a large prospective observational study in primary care patients ≥85 years with moderate to severe frailty and found that SBP <130 mmHg was associated with higher mortality, which contrasted with findings in younger and non‐frail patients. 17 Finally, Kremer et al. found similarly in their cohort study that frailty was an effect modifier on the association between BP and mortality, such that SBP ≥130 mmHg was associated with lower mortality in frailer patients. 14
These cohort studies can be affected by measured and unmeasured confounders, which can affect the validity of results. Furthermore, low BP might be a marker of outcome events in some of these studies rather than being causally related. There have been some randomised controlled trials (RCTs) of BP lowering for primary prevention in older people, such as the Hypertension in the Very Elderly Trial (HYVET). 23 HYVET showed that BP lowering with indapamide compared to placebo was effective for cardiovascular risk reduction in those ≥80 years, but mean achieved SBP in the treatment group was 146 mmHg compared to 161 mmHg in the placebo arm. 23 This raises the question of whether a more intensive BP target could be beneficial in older people.
The more recent Systolic Blood Pressure Intervention Trial (SPRINT) provided some evidence in primary prevention that intensive BP lowering (achieved SBP <120 mmHg) may be safe and beneficial in older people (mean 79.9 years). 24 In this study, intensive BP lowering reduced cardiovascular events (relative risk (RR): 0.66, 95% confidence interval (CI): 0.51–0.85) over 3 years but did not appear to cause a higher rate of serious adverse events, injurious falls or hypotension in people aged ≥75 years. 24 However, although the authors performed an adjusted analysis using frailty scoring, the degree of frailty in the study sample was low, 25 , 26 which means the findings may not be generalisable to those with greater degrees of frailty. Furthermore, those with previous stroke, dementia and heart failure were excluded from the study, as were those with standing SBP <110 mmHg, further limiting generalisability to many older patients. 24 , 27 Finally, the specific method of BP assessment in SPRINT was likely to have underestimated BP compared to other trials. 24 , 27
Age‐based subgroup analyses of other RCTs have also been conducted to investigate the efficacy and safety of BP lowering in older participants, but these studies have limitations, such as not measuring important outcomes like falls, 28 separating subgroups into broad age groups such as below and above 65 years, which limits their generalisability to older patients, 16 or having low numbers of older people, 29 which limits our ability to draw conclusions regarding such older subgroups.
BP lowering for secondary prevention in older people
RCT evidence for BP lowering in secondary prevention in older people is also lacking, given many with pre‐existing cardiovascular disease have been excluded from studies such as SPRINT. 24 We recently performed a meta‐analysis of trials of BP lowering in patients with previous stroke and found that those ≥80 years old did have a higher risk of hypotensive symptoms (RR: 2.17, 95% CI: 1.22–3.86) but not falls or serious adverse events. 30 However, the mean extent of BP lowering was small (SBP 5.6 mmHg), and frailty data were not available. The International Verapamil SR Trandolapril Study (INVEST) trial authors examined a sample of patients over 50 years of age with hypertension and known coronary disease, 31 randomised to either verapamil‐ or atenolol‐based therapy. The authors performed an age‐based subgroup analysis and found that for the primary outcome (mortality and/or cardiovascular events), achieved SBP plotted against this outcome showed a ‘J’ shaped curve for those aged ≥70 years, but not for younger patients. Those ≥70 years had a nadir of benefit of around 140 mmHg, with increasing risk of the primary outcome with BP lower than this. 31 Given that those older people with pre‐existing cardiovascular disease may be more vulnerable to the adverse effects of BP lowering, and that such disease is common in this group, more evidence for BP lowering in secondary prevention in older people is needed.
Guidelines for BP lowering in older people
Guidelines, including the 2016 Australian National Heart Foundation (NHF) guidelines, provide differing and often conflicting advice regarding BP lowering in older people. 27 , 32 In 2021, Bogaerts et al. reviewed 34 guidelines, including American Heart Association (AHA) and National Institute of Health and Care Excellence (NICE) guidelines, for the management of hypertension in older people and found that many of these offered distinct advice for older people and for those who may be frail, 33 illustrating a lack of clear evidence for BP targets.
The 2019 NICE guidelines recommend targeting BP <150/90 mmHg in those over 80, individualised decision‐making for those with frailty or multimorbidity, 34 and measuring standing as well as seated BP in individuals ≥80 years and treating hypertension based on standing BP, due to concern regarding postural hypotension in older individuals. 34 In the 2017 AHA guidelines, a cautious approach to BP lowering in frail older adults is recommended, 35 and in the European Society of Hypertension (ESH) guidelines, individualised BP targets based on physical function rather than age alone are recommended in frail patients ≥80, but if well tolerated, a target SBP <140 mmHg but not less than 130 mmHg. 36 Within Australia, the NHF guidelines also suggest a target of <140/90 mmHg for all patients regardless of age. However, the authors of NHF and ESH guidelines cite the SPRINT study as evidence of the safety of BP lowering in older people, 32 , 36 but as stated, there are some significant limitations regarding the generalisability of this study to frail older people or those with some comorbidities, and therefore the differences between these guidelines may be due to reliance on interpreting the results of this single study.
Emerging evidence: hypertension and dementia
The prevalence of dementia is increasing due to population ageing, and dementia‐related healthcare costs are predicted to double by 2056. 37 Potentially developing dementia is also an important health concern for many older people. 38 Hypertension has been associated with the risk of dementia in observational studies, 39 , 40 identifying it as a potential target for dementia risk reduction. The SPRINT‐MIND study examined participants in the SPRINT study and did not find that intensive BP lowering reduced the incidence of dementia, 41 although it was associated with less hippocampal atrophy. 42
Peters et al. examined SPRINT‐MIND and seven RCTs of BP lowering in a meta‐analysis and did not find a statistically significant association between BP reduction and a lower risk of dementia (RR: 0.93, 95% CI: 0.86–1.00, P = 0.07). 43 However, trials in which BP was lowered to a greater extent had a lower point estimate, which indicated that benefit might only be seen with higher degrees of BP lowering (≥10 mmHg). Hughes et al. also recently examined 12 trials (92 135 participants) including SPRINT‐MIND and the recent Heart Outcomes Prevention Evaluation (HOPE‐3) study 44 and found that BP lowering was associated with a reduced risk of dementia, in a sample of mean age 69 years, followed up for a mean of 49 months (OR: 0.93, 95% CI, 0.88–0.98). 45 However, in many of these trials, the extent of BP lowering was low or the achieved BP control in the comparison group was poor. More recently, Dallaire‐Theroux et al. performed a meta‐analysis of RCTs for primary prevention and found that intensive BP lowering in older adults (17 396 adults, mean age 65 years) was not associated with a reduced risk of dementia or cognitive impairment but was associated with a lower risk of cerebrovascular events. 46
Overall, BP lowering may have a role in dementia risk reduction, but BP targets are unclear. Furthermore, brain changes associated with dementia have been shown to start occurring in middle age. 47 Given the substantial variation in mean age within these trials, 45 it is still unclear as to when in life BP lowering might be effective for dementia risk reduction.
Approach to therapy in older people
In those older people who have a degree of frailty or polypharmacy which is impacting on their quality of life, the OPtimising Treatment for MIld Systolic hypertension in the Elderly (OPTiMISE) trial provides some evidence that reducing antihypertensive burden may have little effect on BP control. 48 The authors examined a sample of older people with a moderate degree of frailty, with SBP <150 mmHg on two or more agents. They found that over 12 weeks, the SBP in the experimental group was 134 mmHg on average compared to 131 mmHg in the control group, suggesting that such a reduction might be safe. However, evidence for long‐term effect of this on cardiovascular risk is unclear. 49 Therefore, in those older people with polypharmacy, reducing or ceasing antihypertensive with subsequent regular monitoring of BP may be safe, but potential risks of doing so should be discussed with the patient or medical decision maker.
With regard to choice of medical therapy, the ESH guidelines recommend first‐line treatment with angiotensin‐converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) and suggest not commencing dual agents in frail older people. 36 However, these may not be optimal for all older people as some may have comorbidities that inform choice of therapy. For example, an older person with atrial fibrillation might warrant a beta blocker as first line for hypertension, whereas in certain patients with chronic kidney disease, ACE/ARB might be best avoided.
Considering the aforementioned evidence, a proposed and testable framework for managing hypertension in the older person (defined here as ≥70 years) with hypertension is shown in Figure 2. This framework is proposed here with the intention that its potential utility be examined in future studies. This approach includes a clinical assessment of frailty, using the Rockwood Frailty Scale 12 (Table 1) to determine extent of frailty. An older patient with no significant frailty may benefit from more aggressive BP lowering for cardiovascular risk reduction. In the SPRINT study, frail patients were included, but such people only had a mild degree of frailty. 25 However, such patients appeared to tolerate and benefit from intensive BP lowering. 24 Therefore, for more robust older people, an approach similar to the NHF guidelines is recommended in Figure 2, with a suggestion that more intensive BP control could be sought in some patients. In such non‐frail patients, lifestyle changes may also be beneficial. 50 Current guidelines recommend limiting alcohol intake to <14 units per week, reducing salt intake to <5 g per day, smoking cessation, weight loss to avoid obesity and moderate aerobic exercise of ≥30 min per day. 34 , 36
Figure 2.
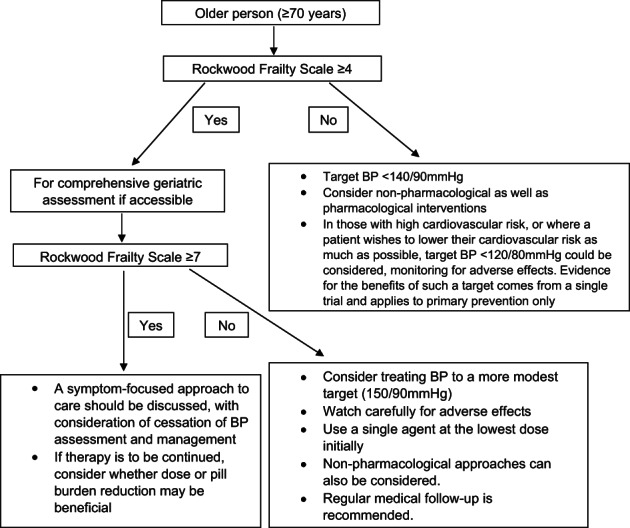
An approach to the management of hypertension in older people based on frailty. 12
In those who have a degree of frailty (Rockwood Frailty Scale ≥ 4), it may be beneficial to undergo geriatric assessment, if accessible, which has been shown to improve mortality and function. 51 Comprehensive geriatric assessment involves a thorough assessment, and considers all the patient's medical problems together, in an individualised approach, although it has not been specifically studied with regard to hypertension management. This approach often involves deprescribing some medications, while commencing others. 51 When prescribing medication for frail older people, we must consider that frailty increases mortality risk and therefore reduces life expectancy. 10 Therefore, in treating a person with greater frailty, absolute risk must be considered rather than only relative risk, 52 as the adverse outcomes that are to be averted usually have a low absolute risk over one year, but absolute risk is rarely reported in studies. 53 Given that the benefit of antihypertensive therapy in such people may be unclear, management should include discussing their priorities and values and adopting shared decision‐making. Frail older people often prefer not to receive treatment aimed purely at prolonging life expectancy. 54 They may be concerned about issues such as high pill burden, and, if offered, they and their families may choose to prioritise those medications aimed at symptom control, such as analgesia, rather than those aimed at reducing cardiovascular risk.
If hypertension is to be treated, patients may warrant regular check‐ups with their general practitioner to monitor BP and for adverse effects such as falls and electrolyte abnormalities. Discussions should be had as to whether such monitoring is feasible or desirable given limited mobility and access to services for some older people. The approach outlined in Figure 2 suggests that, in those with a degree of frailty, the least frail may benefit from BP lowering therapy to a more modest target (150/90 mmHg), watching carefully for adverse effects. A single agent should be used initially, at close to the lowest dose available. 36 For those with a greater degree of frailty (Rockwood Frailty Scale ≥ 7), aforementioned discussions should occur with consideration for avoidance of antihypertensive therapy, given the lack of evidence for the benefit of BP lowering therapy in this group.
Conclusion
Hypertension in the older person should be managed using an individualised approach. Considered alone, age is not a good indicator of the risk of adverse effects of BP lowering, given heterogeneity with regard to the extent of frailty. Evidence is lacking with respect to appropriate BP targets in older people, and geriatric assessment is recommended for frail older people in whom antihypertensive treatment is being considered.
Acknowledgements
Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
Conflict of interest: None.
References
- 1. Australian Bureau of Statistics . Hypertension and Measured High Blood Pressure (Online). Available from URL: https://www.abs.gov.au/methodologies/national-health-survey-first-results-methodology/2017-18
- 2. Hanlon JT, Schmader KE, Ruby CM, Weinberger M. Suboptimal prescribing in older inpatients and outpatients. J Am Geriatr Soc 2001; 49: 200–9. [DOI] [PubMed] [Google Scholar]
- 3. Laurent S, Cockroft J. Central Aortic Blood Pressure. Neuilly‐sur‐Seine Cedex, France: Servier; 2008. [Google Scholar]
- 4. Chobanian AV. Isolated systolic hypertension in the elderly. New Engl J Med 2007; 357: 789–96. [DOI] [PubMed] [Google Scholar]
- 5. Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M et al. Prevalence of hypertension in the US adult population. Results from the third National Health and nutrition examination survey, 1988‐1991. Hypertension 1995; 25: 305–13. [DOI] [PubMed] [Google Scholar]
- 6. Davies JE, Hadjiloizou N, Leibovich D, Malaweera A, Alastruey‐Arimon J, Whinnett ZI et al. Importance of the aortic reservoir in determining the shape of the arterial pressure waveform–the forgotten lessons of frank. Artery Res 2007; 1: 40–5. [Google Scholar]
- 7. Ooi WL, Hossain M, Lipsitz LA. The association between orthostatic hypotension and recurrent falls in nursing home residents. Am J Med 2000; 108: 106–11. [DOI] [PubMed] [Google Scholar]
- 8. Fisher JP, Kim A, Young CN, Ogoh S, Raven PB, Secher NH et al. Influence of ageing on carotid baroreflex peak response latency in humans. J Physiol 2009; 587: 5427–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gibbons CH, Schmidt P, Biaggioni I, Frazier‐Mills C, Freeman R, Isaacson S et al. The recommendations of a consensus panel for the screening, diagnosis, and treatment of neurogenic orthostatic hypotension and associated supine hypertension. J Neurol 2017; 264: 1567–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. The lancet 2013; 381: 752–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56: M146–57. [DOI] [PubMed] [Google Scholar]
- 12. Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I et al. A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J 2005; 173: 489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM et al. Meta‐analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 2009; 169: 1952–60. [DOI] [PubMed] [Google Scholar]
- 14. Kremer K‐M, Braisch U, Rothenbacher D, Denkinger M, Dallmeier D, ActiFE Study Group . Systolic blood pressure and mortality in community‐dwelling older adults: frailty as an effect modifier. Hypertension 2022; 79: 24–32. [DOI] [PubMed] [Google Scholar]
- 15. Wheaton F, Crimmins EM. The Demography of Aging and Retirement. Oxford, UK: Oxford University Press; 2012. [Google Scholar]
- 16. Rodgers A, Chapman N, Woodward M, Liu LS, Colman S, Lee A et al. Perindopril‐based blood pressure lowering in individuals with cerebrovascular disease: consistency of benefits by age, sex and region. J Hypertens 2004; 22: 653–9. [DOI] [PubMed] [Google Scholar]
- 17. Masoli JA, Delgado J, Pilling L, Strain D, Melzer D. Blood pressure in frail older adults: associations with cardiovascular outcomes and all‐cause mortality. Age Ageing 2020; 49: 807–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lloyd‐Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA 2005; 294: 466–72. [DOI] [PubMed] [Google Scholar]
- 19. Kim J, Gall SL, Nelson MR, Sharman JE, Thrift AG. Lower systolic blood pressure is associated with poorer survival in long‐term survivors of stroke. J Hypertens 2014; 32: 904–11. [DOI] [PubMed] [Google Scholar]
- 20. Lin MP, Ovbiagele B, Markovic D, Towfighi A. Systolic blood pressure and mortality after stroke: too low, no go? Stroke 2015; 46: 1307–13. [DOI] [PubMed] [Google Scholar]
- 21. Klein D, Nagel G, Kleiner A, Ulmer H, Rehberger B, Concin H et al. Blood pressure and falls in community‐dwelling people aged 60 years and older in the VHM&PP cohort. BMC Geriatr 2013; 13: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Douros A, Toelle M, Ebert N, Gaedeke J, Huscher D, Kreutz R et al. Control of blood pressure and risk of mortality in a cohort of older adults: the Berlin initiative study. Eur Heart J 2019; 40: 2021–8. [DOI] [PubMed] [Google Scholar]
- 23. Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008; 358: 1887–98. [DOI] [PubMed] [Google Scholar]
- 24. Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged≥ 75 years: a randomized clinical trial. JAMA 2016; 315: 2673–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Russo G, Liguori I, Aran L, Bulli G, Curcio F, Galizia G et al. Impact of SPRINT results on hypertension guidelines: implications for “frail” elderly patients. J Hum Hypertens 2018; 32: 633–8. [DOI] [PubMed] [Google Scholar]
- 26. Karayiannis C, Phan TG, Srikanth V. Intensive vs standard blood pressure control for older adults. JAMA 2016; 316: 1920–1. [DOI] [PubMed] [Google Scholar]
- 27. Harrap SB, Lung T, Chalmers J. New blood pressure guidelines pose difficult choices for Australian physicians. Circ Res 2019; 124: 975–7. [DOI] [PubMed] [Google Scholar]
- 28. White CL, Szychowski JM, Pergola PE, Field TS, Talbert R, Lau H et al. Can blood pressure be lowered safely in older adults with lacunar stroke? The secondary prevention of small subcortical strokes study experience. J Am Geriatr Soc 2015; 63: 722–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rahimi K, Bidel Z, Nazarzadeh M, Copland E, Canoy D, Wamil M et al. Age‐stratified and blood‐pressure‐stratified effects of blood‐pressure‐lowering pharmacotherapy for the prevention of cardiovascular disease and death: an individual participant‐level data meta‐analysis. Lancet 2021; 398: 1053–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tharmaratnam D, Karayiannis CC, Collyer TA, Arima H, McClure LA, Chalmers J et al. Is blood pressure lowering in the very elderly with previous stroke associated with a higher risk of adverse events? J Am Heart Assoc 2021; 10: e022240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Denardo SJ, Gong Y, Nichols WW, Messerli FH, Bavry AA, Cooper‐DeHoff RM et al. Blood pressure and outcomes in very old hypertensive coronary artery disease patients: an INVEST substudy. Am J Med 2010; 123: 719–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gabb GM, Mangoni AA, Anderson CS, Cowley D, Dowden JS, Golledge J et al. Guideline for the diagnosis and management of hypertension in adults—2016. Med J Australia 2016; 205: 85–9. [DOI] [PubMed] [Google Scholar]
- 33. Bogaerts JM, von Ballmoos LM, Achterberg WP, Gussekloo J, Streit S, van der Ploeg MA et al. Do we AGREE on the targets of antihypertensive drug treatment in older adults: a systematic review of guidelines on primary prevention of cardiovascular diseases. Age Ageing 2022; 51: afab192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. National Institute of Health and Care Excellence (NICE) . Hypertension in Adults: Diagnosis and Management (Online). Available from URL: https://www.nice.org.uk/guidance/ng136 [PubMed]
- 35. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and Management of High Blood Pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol 2018; 71: 1269–324. [Google Scholar]
- 36. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J 2018; 39: 3021–104. [DOI] [PubMed] [Google Scholar]
- 37. Brown L, Hansnata E, La HA. Economic cost of dementia in Australia. Alzheimer's Australia, Canberra; 2017.
- 38. Corner L, Bond J. Being at risk of dementia: fears and anxieties of older adults. J Aging Stud 2004; 18: 143–55. [Google Scholar]
- 39. Launer LJ, Ross GW, Petrovitch H, Masaki K, Foley D, White LR et al. Midlife blood pressure and dementia: the Honolulu‐Asia aging study. Neurobiol Aging 2000; 21: 49–55. [DOI] [PubMed] [Google Scholar]
- 40. Whitmer RA, Sidney S, Selby J, Johnston SC, Yaffe K. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology 2005; 64: 277–81. [DOI] [PubMed] [Google Scholar]
- 41. Williamson JD. A randomized trial of intensive versus standard blood pressure control and the risk of mild cognitive impairment and dementia: results from SPRINT MIND. Alzheimers Dement 2018; 14: 1665–6. [Google Scholar]
- 42. Nasrallah IM, Gaussoin SA, Pomponio R, Dolui S, Erus G, Wright CB et al. Association of intensive vs standard blood pressure control with magnetic resonance imaging biomarkers of Alzheimer disease: secondary analysis of the SPRINT MIND randomized trial. JAMA Neurol 2021; 78: 568–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Peters R, Warwick J, Anstey KJ, Anderson CS. Blood pressure and dementia: what the SPRINT‐MIND trial adds and what we still need to know. Neurology 2019; 92: 1017–18. [DOI] [PubMed] [Google Scholar]
- 44. Bosch J, O'Donnell M, Swaminathan B, Lonn EM, Sharma M, Dagenais G et al. Effects of blood pressure and lipid lowering on cognition: results from the HOPE‐3 study. Neurology 2019; 92: e1435–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hughes D, Judge C, Murphy R, Loughlin E, Costello M, Whiteley W et al. Association of blood pressure lowering with incident dementia or cognitive impairment: a systematic review and meta‐analysis. JAMA 2020; 323: 1934–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dallaire‐Théroux C, Quesnel‐Olivo M‐H, Brochu K, Bergeron F, O'Connor S, Turgeon AF et al. Evaluation of intensive vs standard blood pressure reduction and association with cognitive decline and dementia: a systematic review and meta‐analysis. JAMA Netw Open 2021; 4: e2134553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Raz N, Rodrigue KM, Acker JD. Hypertension and the brain: vulnerability of the prefrontal regions and executive functions. Behav Neurosci 2003; 117: 1169–80. [DOI] [PubMed] [Google Scholar]
- 48. Sheppard JP, Burt J, Lown M, Temple E, Lowe R, Fraser R et al. Effect of antihypertensive medication reduction vs usual care on short‐term blood pressure control in patients with hypertension aged 80 years and older: the OPTIMISE randomized clinical trial. JAMA 2020; 323: 2039–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Applegate WB, Williamson JD, Berlowitz D. Deprescribing antihypertensive medication in elderly adults. JAMA 2020; 324: 1682–2, 1683. [DOI] [PubMed] [Google Scholar]
- 50. Burke V, Beilin L, German R, Grosskopf S, Ritchie J, Puddey I et al. Association of lifestyle and personality characteristics with blood pressure and hypertension: a cross‐sectional study in the elderly. J Clin Epidemiol 1992; 45: 1061–70. [DOI] [PubMed] [Google Scholar]
- 51. Welsh TJ, Gordon AL, Gladman J. Comprehensive geriatric assessment—a guide for the non‐specialist. Int J Clin Pract 2014; 68: 290–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Noordzij M, van Diepen M, Caskey FC, Jager KJ. Relative risk versus absolute risk: one cannot be interpreted without the other. Nephrol Dial Transplant 2017; 32: ii13–18. [DOI] [PubMed] [Google Scholar]
- 53. Nuovo J, Melnikow J, Chang D. Reporting number needed to treat and absolute risk reduction in randomized controlled trials. JAMA 2002; 287: 2813–14. [DOI] [PubMed] [Google Scholar]
- 54. Nahm E‐S, Resnick B. End‐of‐life treatment preferences among older adults. Nurs Ethics 2001; 8: 533–43. [DOI] [PubMed] [Google Scholar]


