Patient 1 was a 4‐month‐old boy who was admitted to our hospital due to a history of left cheek fistula and left ear mass since birth. Intermittent watery fluid discharge was observed from the cheek fistula, however, no redness, swelling, fever, pain or other discomfort was present. A tip‐sized fistula and left preauricular appendage were observed (Fig. 1a) without mandibular dysplasia. B‐ultrasound examination showed that the fistula extended to the adipose layer. Ectopic accessory parotid system was therefore diagnosed on the medical history and physical examination.
Fig. 1.
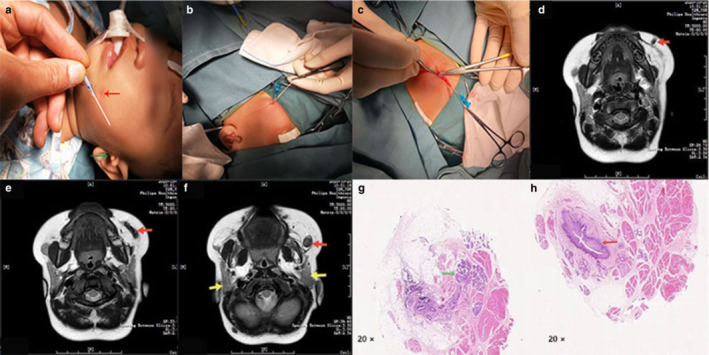
(a) Clinical manifestations consisted of a fistula located in the oral joint (red arrow) and an ipsilateral preauricular appendage (green arrow). (b,c) The cheek hole was injected with methylene blue using a catheter to assist in the dissection of the fistula. Traction sutures were placed on the fistula and the tissues around it, then traction was applied with the sutures to dissect the fistulous duct. (d–f) The fistula (red arrow) and normal parotid (yellow arrows) as observed on magnetic resonance imaging (MRI). (g,h) H & E staining: histopathology of the excised specimens showing salivary glands (green arrow) and the fistulous tracts (red arrow), which were enclosed in squamous epithelium. Note: Panels a, b, c, g and h refers to patient 1; Panels d, e and f refers to patient 2.
Patient 2 was a 10‐month‐old boy who also presented with a congenital punctate skin opening on his left cheek that discharged pellucid fluid, especially while eating. Bilateral preauricular appendages with no other abnormalities were observed in the head–neck region and elsewhere in the body. The diagnosis was made on magnetic resonance imaging (MRI). Normal bi‐parotids were observed on MRI, however, an approximately 3‐mm‐diameter fistula was observed along the lateral aspect of the left masseter muscle (Fig. 1d,e,f).
Under general anesthesia in patient 1, the cheek hole was injected with methylene blue using a catheter to assist in the dissection of the fistula. The duct was dissected by approximately 2.0 cm using the methylene staining as a guide for complete removal (Fig. 1b,c). The skin defect was closed with interrupted absorbable stitches and the preauricular appendage was excised. Histopathology of the excised specimens consisted of salivary glands and fistulous tracts. The fistulous duct was enclosed with squamous epithelium (Fig. 1g,h). In patient 2, the same opetation was done. No recurrence or complications were observed in both patients during the 2 years and 1 year follow‐up periods, respectively.
Ectopic accessory parotid system with congenital cheek fistula (EAPS) and parotid gland malformations are rare. The clinical manifestations consist of fistula located in the oral joint, ipsilateral preauricular appendage and mandibular dysplasia. Patients with EAPS have an independent salivary gland excretion system that includes a functional accessory parotid gland and an ectopic duct that does not communicate with the Stenson's duct. 1
B‐ultrasonography is rarely used to diagnose EAPS because it has a limited ability to visualize the ectopic duct and small ectopic parotid tissue. However, Kulkarni et al. 2 believed that B‐ultrasonography was worth further consideration in diagnosing EAPS because of the low cost and repeatability. In the present cases the accessory parotid gland and ectopic duct were difficult to see on B‐ultrasonography. MRI and computed tomography (CT) have several advantages and disadvantages for the diagnosis of EAPS. Using MRI, the parotid gland, masseter muscle, parotid duct, ectopic accessory parotid gland and fistula can be observed, 1 , 3 while CT can show bone abnormalities, such as dysplasia of the jaw. 2 Because CT carries a radiation hazard, MRI is the preferred diagnostic tool for pediatric patients.
Surgical excision is the primary method to treat EAPS. The procedure entails a cheek skin and intraoral incision to remove the fistula and parotid gland or to perform fistula diversion. Some surgeons believe that intraoral incision is aesthetic, while others believe that external skin resection is simple and easy to perform. However, if it is an oral incision or cheek skin resection, part of the skin would still have to be removed. 4 Regardless of the surgical procedure, the prognosis after fistula resection is good. When fistulectomy is performed, a few surgeons opt not to remove the accessory ear and the anterior auricular depression. 3 In addition to surgical treatment, fistula injection with trichloroacetic acid and botulinum has also been reported, 5 however, long‐term follow‐up and/or prognosis data are lacking, therefore it is not possible to make a comparison between the treatment strategies.
In the case of clinical symptoms of cheek fistula it is necessary to perform preoperative CT or MRI to confirm the presence of the duct, ectopic accessory parotid gland and dysplasia of the mandible for suspected EAPS. Because of the favorable prognosis of surgery, we suggest that excision of the ectopic duct should be the preferred treatment strategy. Removal of the accessory appendage and anterior auricular depression could be performed simultaneously.
Disclosure
The authors declare no conflicts of interest.
Author contributions
LZ wrote the paper. YW diagnosed the disease and supervised the paper. LZ, YW and ZL carried out the surgery. All authors read and approved the final manuscript.
Ethics statement
Informed consent was obtained from the patients’ parents.
References
- 1. Dutta M. The ectopic accessory parotid system with congenital cheek fistula: an overview and current update. Laryngoscope 2017; 127: 1351–60. [DOI] [PubMed] [Google Scholar]
- 2. Gadodia A, Seith A, Sharma R, Thakar A. Congenital salivary fistula of accessory parotid gland: imaging findings. J. Laryngol. Otol. 2008; 122: e11. [DOI] [PubMed] [Google Scholar]
- 3. Kulkarni CD, Mittal SK, Katiyar V, Pathak O, Sood S. Accessory parotid gland with ectopic fistulous duct‐‐diagnosis by ultrasonography, digital fistulography, digital sialography and CT fistulography. A case report and review of current literature. J. Radiol. Case Rep. 2011; 5: 7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sun Z, Sun L, Zhang Z, Ma X. Congenital salivary fistula of an accessory parotid gland in Goldenhar syndrome. J. Laryngol. Otol. 2012; 126: 103–7. [DOI] [PubMed] [Google Scholar]
- 5. Hah JH, Kim BJ, Sung MW, Kim KH. Chemocauterization of congenital fistula from the accessory parotid gland. Clin. Exp. Otorhinolaryngol. 2008; 1: 113–5. [DOI] [PMC free article] [PubMed] [Google Scholar]


