Abstract
Objective
To compare clinical and patient‐reported outcomes when providing maxillary overdentures on four and six splinted implants placed in the posterior region during a 10‐year follow‐up period.
Materials and Methods
Sixty‐six edentulous participants with functional maxillary denture complaints and insufficient bone volume to allow implant placement were scheduled for a bone augmentation procedure. After healing, participants were randomized to receive either four or six implants in the posterior maxilla. After 3 months of osseointegration, a bar overdenture was constructed. Implant survival, overdenture survival, clinical scores, peri‐implant bone height changes, and patient satisfaction were assessed.
Results
Forty‐six participants completed the 10‐year follow‐up. Implant survival was 100% in the 4‐implant group and 96.7% in the 6‐implant group. Seven new overdentures were made in the 4‐implant group and 12 new overdentures were made in the 6‐implant group due to excessive wear of the denture base and teeth. Clinical parameters did not differ significantly between groups. Mean marginal bone loss compared to baseline was 0.41 ± 0.37 mm in the 4‐implant group and 0.70 ± 1.07 mm in the 6‐implant group. Overall, patient satisfaction improved significantly, but did not differ between groups.
Conclusion
From this 10‐year follow‐up trial, it was concluded that bar maxillary overdentures on four or six implants in the posterior region of an augmented maxilla resulted in a comparable treatment outcome with high implant survival, limited loss of peri‐implant marginal bone, and high patients' satisfaction. (Clinical trial registration number: NTR9729).
Keywords: dental implants, edentulous, healthy aging, maxilla, overdenture
1. INTRODUCTION
The removable overdenture is not restricted to patients with a compromised situation in which fixed‐implant prostheses are not feasible. The removable overdenture is considered an equally good alternative treatment option to the fixed denture design (Zitzmann & Marinello, 1999). Clinical outcomes were similar if a screw‐retained fixed bridge was compared with a removable bar overdenture (Zitzmann & Marinello, 2000). For patients with persistent maxillary denture complaints, implant support diminishes these problems. Results from systematic reviews and clinical studies on maxillary implant‐supported overdenture treatment are consistent and favorable on various outcome parameters, such as improved oral function and Oral Health‐Related Quality of Life as well as patient satisfaction in general (Boven et al., 2015; Fonteyne et al., 2021; Fromentin et al., 2010; Van Assche et al., 2012). Implant survival rate is generally high (Di Francesco et al., 2021; Raghoebar et al., 2014; Roccuzzo et al., 2012; Sadowsky & Zitzmann, 2016; Slot et al., 2010). However, the present knowledge on maxillary overdenture therapy is hampered by the fact that studies generally do not encompass a long evaluation period. In addition, relevant practical information related to the ideal position and implant number and the attachment type is often unclear (Di Francesco et al., 2021; Roccuzzo et al., 2012; Sadowsky & Zitzmann, 2016; Slot et al., 2010). In a recent systematic review, no fewer than four implants were recommended (Di Francesco et al., 2019; Messias et al., 2021). Studies evaluating maxillary overdenture treatment with dentures supported by either four or six splinted implants demonstrate similar results for both biological and functional outcomes after a short period of time (Ferrigno et al., 2002; Sanna et al., 2009). If sufficient bone is present in the anterior region and sufficient space is available in the overdenture to cover an attachment system, placing implants in the anterior region is advantageous. In this situation, extensive bone augmentation procedures (maxillary sinus floor elevation surgery with bone from the iliac crest) can be avoided, resulting in less morbidity and less treatment time (Kalk et al., 1996; Slot et al., 2014). However, patients with poor retention and stability of their conventional maxillary denture often have limited bone volume to place implants. Therefore, these implants often have to be positioned in the posterior part of the maxilla, preceded by or in conjunction with a bone augmentation procedure.
High‐quality data from randomized clinical trials are needed to decide whether or not the fewer number of implants and placed in augmented bone in the posterior region would also suffice clinically and from a patients' perspective after a long‐term evaluation period.
Therefore, this research reports on the 10‐year clinical and patient‐reported outcomes of a randomized controlled clinical trial with a parallel study design on edentulous participants with persistent denture complaints with maxillary four‐ or six‐implant bar overdentures. All implants were placed in posterior maxillae following sinus augmentation procedures.
2. MATERIALS AND METHODS
Surgical and prosthodontic treatment procedures and measures of evaluation were described before and are summarized below (Slot et al., 2014). The trial was approved by the Medical Ethics Committee of the University Medical Center Groningen (ABR NL32503.042.11). The 10‐year follow‐up trial, since it took part during regular scheduled routine control visits, without collection of extra data, was not considered a clinical research with test subjects as meant in the Medical Research Involving Human Subjects Act (WMO) (METc communication M18.224571). The 10‐year follow‐up trial was registered in a trial register (www.trialregister.nl: NTR_NL9729). CONSORT guidelines for reporting clinical trials were followed.
2.1. Patient selection
Participants in this randomized controlled trial were selected from edentulous patients referred to the Department of Oral and Maxillofacial Surgery (University Medical Center Groningen, the Netherlands) suffering from a lack of retention and stability of their complete maxillary and mandibular dentures based on the following inclusion criteria: at least 18 years of age, capable of understanding and giving informed consent, at least 1 year of edentulism in the maxilla and mandible, and insufficient volume of bone of the maxilla (<3 mm in width, and <5 mm in height) for inserting implants. Panoramic radiographs, lateral cephalograms, and postero‐anterior oblique radiographs were made to assess the volume of the maxillary alveolar bone, the dimensions of the maxillary sinus, and the anteroposterior relationship of the maxilla to the mandible.
Excluded were patients with an American Society of Anesthesiologists score ≥ III (Smeets et al., 1998), those currently smoking, and those with a history of radiotherapy in the head and neck region or a history of pre‐prosthetic surgery and previous implant placement or sinus pathology.
2.2. Treatment procedure
All surgical procedures were performed by one experienced oral and maxillofacial surgeon (G.M.R.). The prosthodontic procedures were conducted by three experienced prosthodontists, and manufacturing of the superstructure was done by a single experienced dental laboratory.
2.3. Surgical procedures
Participants were randomly allocated to one of the treatment groups by lot with the use of sealed envelopes. Thirty‐three notes with the words “4 implants” and 33 notes with the words “6 implants” were put into 66 identical, sequentially numbered, non‐transparent envelopes. No stratification was performed. All envelopes were irreversibly sealed, only to be opened prior to the fabrication of the surgical template.
A maxillary sinus floor augmentation with bone from the iliac crest was performed on both sides (Raghoebar et al., 1997, 2001), and autogenous blocks were fixed on the lateral wall with screws to reconstruct the bone width. After a 3‐month healing period, the screws were removed and either four or six dental implants (Straumann Standard SLA® implants with 2.8 mm polished collar; Ø 4.1 mm, length 12 mm, RN; Institut Straumann AG), depending on the randomization group, were inserted in the maxilla in a single‐step procedure. The implants were placed into the grafted sites in predefined positions (positions 16, middle of 15/14, 13, 23, middle of 24/25, 26 in the 6‐implant group and positions 16, 13, 23, 26 in the 4‐implant group) using a template designed for semi‐guided implant placement. Because all patients were also edentulous in the mandible, four implants for overdenture treatment were placed simultaneously in the mandible. In all cases, the design of their old complete maxillary denture could be used for diagnostics and could also be adjusted after surgery to serve as a provisional denture during the healing period. For 2 weeks after surgery, the patient was not allowed to wear the denture. Then, acrylic resin was removed from the denture in those areas which could contact the grafted sites or implants, whereafter the denture was relined with a resilient liner (Soft liner; GC Corporation).
2.4. Prosthodontic procedures
Prosthodontic procedures commenced after 3 months of undisturbed healing. The final attachment system consisted of a milled titanium split bar and an overdenture with built‐in cobalt chromium reinforcement structure and gold retentive clips (Figure 1a,b). Resilient egg‐shape bars (width 2.19 mm) were used (ES Healthcare NV). The overdentures were designed with full coverage of the alveolar process, but without palatal coverage in the maxilla (Slot et al., 2012). Acrylic resin artificial teeth (Ivoclar SR Orthotyp DCL and Ivoclar Vivodent PE; Ivoclar Vivadent AG) were selected and arranged on the record base for a trial arrangement. A bilateral balanced occlusion concept was followed. Simultaneously with the maxillary overdenture, participants also received a four‐implant overdenture in the mandible. Participants were instructed about hygiene procedures associated with the dentures and the bars. They were advised to remove the overdenture at night. Subsequently, the participants were scheduled for routine yearly maintenance appointments with a prosthodontist, combined with a dental hygienist.
FIGURE 1.
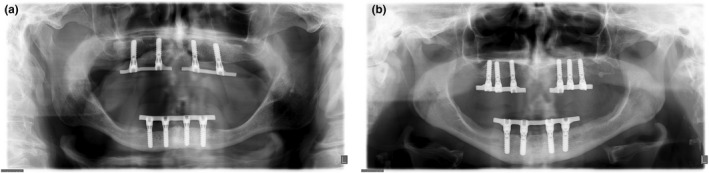
(a) Ten‐year panoramic radiograph of a patient with four implants connected with a bar in the posterior region of the maxilla. (b) Ten‐year panoramic radiograph of a patient with six implants connected with a bar in the posterior region of the maxilla.
2.5. Outcome measures
The primary outcome measure was peri‐implant bone height changes. The secondary outcome measures were implant survival, overdenture survival, and soft tissue conditions (plaque index, presence of calculus, gingival index, sulcus bleeding index and pocket probing depth). These parameters were scored at placement of the overdenture and 5 and 10 years after loading. All measurements were taken by a single examiner (W.S.). Patients' satisfaction was also scored before treatment and 5 and 10 years after loading.
2.6. Change of radiographic bone level
Standardized intraoral radiographs were taken at placement of the overdenture, after 5 years and at 10 years after placement. The radiographs were taken according to a long‐cone paralleling technique with an individualized X‐ray holder described by Meijndert et al. (2004). The digital images were analyzed using computer software (Biomedical Engineering, University Medical Center Groningen, the Netherlands) to perform linear measurements on digital radiographs. The known implant dimension was used as a reference to transform the linear measurements into millimeter. The reference point for linear measurements was the neck of the implant. Peri‐implant bone height change was defined as the difference in bone height between the X‐ray taken at overdenture placement and after 1, 5, and 10 years. Data of radiographic bone level change were presented at patient level; outcomes of the implants within the same patients were averaged. Data collection and analysis of the radiographs were done by the same observer. The worst score per implant of the clinical and radiographic parameters was used in the data analysis. Reproducibility of the specific analysis method was evaluated by Telleman et al. (2013). The intraclass correlation coefficient for average measures was 0.867 for the radiographic interobserver agreement (Cronbach's α = 0.867), which can be interpreted as almost perfect agreement.
2.7. Clinical parameters
For the presence of plaque, the index according to Mombelli et al. (1987) was used. The presence of calculus (score 1) or the absence of calculus (score 0) was scored. To qualify the degree of peri‐implant inflammation, the modified Löe and Silness index Löe and Silness (1963) was used. For bleeding, the bleeding index according to Mombelli et al. (1987) was used. Probing depth was measured at four sites of each implant (mesial, labial, distal, and lingual) by using a manual periodontal probe (Williams Colour‐Coded Probe; Hu‐Friedy).
Peri‐implant mucositis and peri‐implantitis were calculated at patient level. As a definition for peri‐implant mucositis and peri‐implantitis, the consensus reached at the Seventh European Workshop on Periodontology was used (Lang & Berglundh, 2011):
peri‐implant mucositis (radiographic bone loss <2 mm): bleeding on probing and/or suppuration and
peri‐implantitis: bleeding on probing and/or suppuration in combination with marginal bone loss ≥2 mm.
2.8. Patient satisfaction
Patient‐Reported Outcome Measures were assessed using a validated questionnaire (Vervoorn et al., 1988). Items were functional problems of the upper denture, functional problems complaints in general, problems concerning facial aesthetics, items concerning accidental lip, cheek, and tongue biting (“neutral space”) and items concerning esthetics of the denture.
The severity of each complaint could be expressed on a four‐point rating scale (0 = no complaints, 1 = little, 2 = moderate, and 3 = severe complaints).
All participants were requested to fill out a “chewing ability” questionnaire (Stellingsma et al., 2005). In this questionnaire, participants gave their opinion about the ability to chew nine different kinds of food on a three‐point rating scale (0 = good, 1 = moderate, 2 = bad). The items were grouped into three scales: soft food, tough food, and hard food. In addition to these questionnaires, the patients' overall denture satisfaction was expressed on a 10‐point rating scale (1 = very bad to 10 = excellent).
Patients' satisfaction was scored before treatment and 5 and 10 years after placement of the overdenture.
2.9. Statistical analysis
It was assumed that an implant‐supported overdenture on four implants was not inferior to one supported by six implants (non‐inferiority hypothesis). The sample size was calculated with the program G*power version 2 (Erdfelder et al., 1996). Peri‐implant bone changes were regarded as the primary outcome for the power analysis. A difference of at least 0.4 mm in bone height (measured on standardized radiographs, with a standard deviation of 0.5 mm) between the 4‐implant group and 6‐implant group after 12 months was expected to differentiate between the two groups, based on the findings of a study on maxillary implant supported overdentures (Raghoebar et al., 2003). A t‐test given α = .05 with a power of 90% combined with the expected effect size for two independent means returns a sample size of 28 persons in each group. To deal with withdrawal of individuals in the trial, the number of participants was set at 33 persons per group.
Data were analyzed using the Statistical Package for Social sciences (version 23 VA, SPSS; IBM Corporation). In all tests, a significance level of .05 was used. To test whether the result from the frequency analyses differed significantly from a normal distribution, qq‐normal plots and the Shapiro–Wilk test were carried out. For normally distributed data, differences between groups were tested with an independent Student's t‐test. For non‐normally distributed data, Mann–Whitney tests were used. For comparisons over time, Wilcoxon signed‐rank tests were applied.
3. RESULTS
Between January 2006 and December 2009, consecutive patients fulfilling the criteria were included. Eight participants died during the follow‐up period (three participants in the 4‐implant group and five participants in the 6‐implant group). Three participants of the 4‐implant group and six participants in the 6‐implant group did not attend the 10‐year evaluation because of severe illness. One patient in the 4‐implant group and one patient in the 6‐implant group moved abroad. One patient in the 6‐implant group moved without leaving an address. So, totally 46 participants completed the 10‐year evaluation (Figure 2). No implants were lost in the 4‐implant group, while four implants were lost in the 6‐implant group (three implants in one patient). The 10‐year implant survival rate was 100% in the 4‐implant group and 96.7% in the 6‐implant group. Ten‐year' survival rate of overdentures was 73.1% in the 4‐implant group and 40.0% in the 6‐implant group.
FIGURE 2.
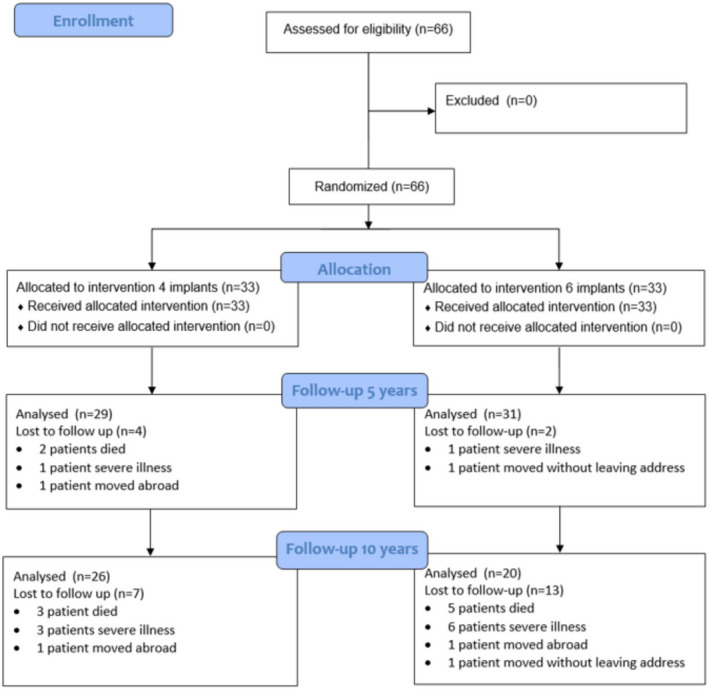
Flow diagram of the study
Mean loss of peri‐implant bone between baseline and the 10‐year evaluation was 0.66 ± 0.58 mm in the 4‐implant group and 0.73 ± 0.90 in the 6‐implant group and did not significantly differ between the groups (p = .728) (Table 1). Frequency analysis of indices for plaque, calculus, gingiva, and bleeding was very low after 10 years of loading and again did not significantly differ between the groups, nor did the mean scores for pocket probing depth (Table 2). In the present trial, incidence at patient level of peri‐implant mucositis was 34.6% in the 4‐implant group and 65.0% in the 6‐implant group. Incidence at patient level of peri‐implantitis was 38.5% in the 4‐implant group and 20.0% in the 6‐implant group. Mean scores of the questionnaires focusing on denture complaints, chewing ability, and overall satisfaction score of participants are listed in Table 3, with no significant differences between the groups, except for eating hard food (p = .024). The surgical and prosthodontic aftercare during 10 years of follow‐up revealed a small number of events, mostly repair of the denture base or teeth (Table 4). In 24% of the participants, a new bar was made, and in 41% of the participants, a new overdenture was made.
TABLE 1.
Mean values and standard deviations of marginal bone loss in millimeter, frequency distribution of bone loss at 5 and 10 years after placement of the overdenture of the four‐ and six‐implant groups, and significance level (p value) of differences (p < .05) between the groups
| 5 years | 10 years | |||||
|---|---|---|---|---|---|---|
| 4‐Implant group (n = 29) | 6‐Implant group (n = 31) | p Value | 4‐Implant group (n = 26 implants) | 6‐Implant group (n = 20 implants) | p Value | |
| Mean (SD) | 0.58 mm (0.51) | 0.60 mm (0.58) | p = .871 | 0.66 mm (0.58) | 0.73 mm (0.90) | p = .728 |
| 0–0.5 mm | 45% | 58% | 58% | 59% | ||
| >0.5–1.0 mm | 38% | 13% | 16% | 15% | ||
| >1.0–1.5 mm | 17% | 19% | 11% | 14% | ||
| >1.5–2.0 mm | 0% | 7% | 7% | 3% | ||
| >2.0 mm | 0% | 3% | 8% | 9% | ||
TABLE 2.
Frequency distribution of plaque, calculus, gingival and bleeding indices and mean and standard deviation (SD) of probing depth in mm, at placement of the overdenture (T0), and 5 years (T60) and 10 years (T120) after placement of the overdenture, and significance level (p value) of differences between groups at three time points (p < .05 was considered significant)
| T0 | T60 | T120 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 4‐Implant group (n = 33) | 6‐Implant group (n = 33) | Sign | 4‐Implant group (n = 29) | 6‐Implant group (n = 31) | Sign | 4‐Implant group (n = 26) | 6‐Implant group (n = 20) | Sign | |
| Plaque index (%) | |||||||||
| 0 | 87.9 | 90.9 | 1.000 | 62.1 | 51.6 | .475 | 53.8 | 55.0 | .485 |
| 1 | 12.1 | 9.1 | 20.7 | 25.8 | 7.7 | 30.0 | |||
| 2 | 0 | 0 | 17.2 | 22.6 | 61.5 | 15.0 | |||
| 3 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| Calculus index (%) | |||||||||
| 0 | 97.0 | 100 | 1.000 | 96.6 | 96.8 | 1.000 | 92.3 | 90.0 | .957 |
| 1 | 3.0 | 0 | 3.4 | 3.2 | 7.3 | 10.0 | |||
| Gingival index (%) | |||||||||
| 0 | 87.9 | 97.0 | .355 | 48.3 | 54.8 | .462 | 61.5 | 65.0 | .783 |
| 1 | 12.1 | 3.0 | 41.4 | 41.9 | 26.9 | 20.0 | |||
| 2 | 0 | 0 | 10.3 | 3.3 | 11.6 | 15.0 | |||
| 3 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| Bleeding index (%) | |||||||||
| 0 | 72.7 | 72.3 | 1.000 | 51.7 | 38.7 | .268 | 46.1 | 45.0 | 1.000 |
| 1 | 24.3 | 27.3 | 37.9 | 41.9 | 42.3.9 | 40.0 | |||
| 2 | 3.0 | 0 | 10.4 | 19.4 | 11.6 | 15.0 | |||
| 3 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| Probing depth in mm (SD) | 4.5 (0.8) | 4.1 (1.1) | .157 | 4.3 (1.0) | 4.2 (0.8) | .765 | 4.8 (1.1) | 4.2 (0.9) | .337 |
TABLE 3.
Mean score of five scales concerning the denture complaints (possible range 0–3), mean scores of chewing ability of soft, tough, and hard food (possible range 0–2) and overall satisfaction score (possible range 1–10) before and 5 and 10 years after treatment and significance level of differences (p < .05) between the groups
| Pre‐treatment | 5 years | 10 years | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 4‐Implant group (n = 33) | 6‐Implant group (n = 33) | p Value | 4‐Implant group (n = 29) | 6‐Implant group (n = 31) | p Value | 4‐Implant group (n = 26) | 6‐Implant group (n = 20) | p Value | |
| Functional complaints about upper denture (SD) | 1.5 (0.6) | 1.7 (0.5) | 0.099 | 0.1 (0.1) | 0.2 (0.2) | 0.212 | 0.2 (0.2) | 0.3 (0.5) | 0.305 |
| Functional complaints in general (SD) | 1.0 (0.5) | 1.1 (0.5) | 0.132 | 0.1 (0.1) | 0.1 (0.1) | 0.106 | 0.1 (0.2) | 0.2 (0.5) | 0.258 |
| Facial aesthetics (SD) | 1.1 (0.9) | 1.1 (1.0) | 0.828 | 0.1 (0.3) | 0.4 (0.7) | 0.052 | 0.3 (0.4) | 0.3 (0.7) | 0.914 |
| “Neutral Space” (SD) | 0.6 (0.6) | 0.5 (0.7) | 0.408 | 0.4 (0.4) | 0.2 (0.4) | 0.055 | 0.5 (0.4) | 0.3 (0.5) | 0.215 |
| Aesthetics (SD) | 0.4 (0.3) | 0.4 (0.4) | 0.877 | 0.1 (0.2) | 0.1 (0.2) | 0.508 | 0.2 (0.3) | 0.2 (0.5) | 0.607 |
| Soft food (SD) | 0.4 (0.4) | 0.4 (0.4) | 0.632 | 0.0 (0.0) | 0.0 (0.1) | 0.338 | 0.0 (0.1) | 0.1 (0.2) | 0.422 |
| Tough food (SD) | 1.0 (0.5) | 1.2 (0.6) | 0.332 | 0.1 (0.3) | 0.1 (0.3) | 0.688 | 0.1 (0.2) | 0.1 (0.4) | 0.823 |
| Hard food (SD) | 1.8 (0.4) | 1.8 (0.5) | 0.730 | 0.2 (0.5) | 0.4 (0.5) | 0.140 | 0.2 (0.4) | 0.5 (0.7) | 0.024 |
| Overall satisfaction score (SD) | 4.4 (1.7) | 3.9 (1.5) | 0.188 | 8.6 (0.7) | 8.8 (0.9) | 0.467 | 8.7 (0.8) | 8.6 (1.6) | 0.699 |
Note: Differences between study groups were tested with the independent Student's t test.
TABLE 4.
Surgical and prosthodontic aftercare (number of events) of the 4‐implant group and the 6‐implant group during two follow‐up periods (0–5 years and 5–10 years)
| Follow‐up‐period | 0–5 years | 5–10 years | ||
|---|---|---|---|---|
| Group | 4‐implant group (n = 29) | 6‐implant group (n = 31) | 4‐implant group (n = 26) | 6‐implant group (n = 20) |
| Removal of hyperplasia | 2 | 3 | 0 | 0 |
| Surgical treatment of peri‐implantitis | 0 | 0 | 1 | 0 |
| Clip repair | 0 | 0 | 0 | 0 |
| Repair denture base/teeth | 13 | 18 | 4 | 18 |
| Relining overdenture | 0 | 1 | 0 | 0 |
| Readjustment occlusion | 1 | 2 | 3 | 0 |
| New bar | 0 | 1 | 4 | 6 |
| New overdenture | 0 | 3 | 7 | 9 |
4. DISCUSSION
This randomized clinical trial shows that both four and six dental implants connected with a bar, placed in the posterior region of the edentulous maxilla, can effectively support of an overdenture during 10 years of follow‐up. No significant differences were found between the group with an overdenture supported by four implants and the group with an overdenture supported by six implants.
Ten‐year survival rate of the implants was high in both groups (100% and 96.7%, respectively). These results are in line with the cumulative 10‐year implant survival rates reported by Ferrigno et al. (2002) and Sanna et al. (2009), although it must be noted that these implants were mainly placed in the anterior region. The survival rate in the present trial was much higher than in the study of Visser et al. (2009), with an actual 10‐year rate of only 86.1%, in which the study‐machined surface dental implants were placed in the posterior region. In the present trial, dental implants with a roughened surface were placed in the posterior region, in contrast to the latter study. Possibly with machined surface implants, osseointegration is less successful in sites in which extensive bone augmentation procedures have been performed. This rather low implant survival rate when using a machined implant surface in the edentulous maxilla was also reported in the 5‐year studies of Watson et al. (1997), and Bergendal and Engquist (1998), being, respectively, 72.4% and 79%.
Mean peri‐implant bone loss between baseline (placement of the overdenture) and the 10‐year evaluation was very small in both groups. Comparison with the studies of Ferrigno et al. (2002) and Visser et al. (2009) is not possible because marginal bone level changes were not mentioned or could not be distracted. In the study of Sanna et al. (2009), bone level changes were calculated in frequencies, reporting an annual bone loss of ≤0.15 mm in the vast majority of the cases. Mean indices for plaque, calculus, gingiva, and bleeding were very low at the 10‐year evaluation, and the probing depth was not deviating. There were no differences in outcome between the 4‐ and 6‐implant group. Some extra effort in performing hygiene tasks might be required from participants with six implants, but this did not appear to affect the results.
Incidence of peri‐implantitis was calculated according the definition VII European Workshop on Periodontology (Lang & Berglundh, 2011). In the present trial, incidence at the patient level of peri‐implant mucositis was 34.6% in the 4‐implant group and 65.0% in the 6‐implant group, whereas this number was, respectively, 27.3% and 39.4% at the 5‐year evaluation (Slot et al., 2019). Incidence of peri‐implantitis at patient level after 10 years was 38.5% and 20.0% in the 4‐ and 6‐implant group, respectively. At the 5‐year evaluation, this number was, respectively, 17.2% and 9.7% (Slot et al., 2019). This means that the risk of getting peri‐implant mucositis or peri‐implantitis does not stop after a number of years and new patients are infected. For the maxilla, there are no comparable 10‐year studies on this outcome variable, but for mandibular overdentures, comparable percentages of peri‐implant mucositis and peri‐implantitis are reported (Meijer et al., 2014). Peri‐implant mucositis and peri‐implantitis are infectious diseases caused by the bacterial biofilm. Existing studies have demonstrated clearly that edentulism per se is no protection from peri‐implant disease and that continuous supportive care is essential in maintaining peri‐implant health (De Waal et al., 2013).
Patients' satisfaction improved significantly when wearing implant‐supported maxillary overdentures, and results showed to be favorable at both the 5‐ and 10‐year evaluation. The scores at 10 years are in agreement with data reported by Sanna et al. (2009) for an overdenture supported by four implants. Krennmair et al. (2008) mentioned in their case series that patients with an overdenture on four or six implants in the maxilla were equally satisfied after 5 years. In other words, patients' satisfaction seemed to be irrespective of whether the bar was supported by four or six implants in the posterior maxillary region. The high satisfaction might be due to the fact that the overdenture is supported by a bar with the same length in both groups, which gives a comparable stability for both treatment options. The four and six implants are more or less placed in the same area, leading to the fact that the length of the bar is comparable in both groups. The high satisfaction with maxillary overdentures, including opinions on speech, resemble the results of Heydecke et al. (2003) in which favorable results of an overdenture were displayed compared with a fixed‐implant prosthesis.
A paradox can be noted as very high percentages of peri‐implant mucositis were calculated (Table 2), whereas the incidence of hyperplasia was low (Table 4). This could be clarified by the fact that mean bleeding scores were very low, meaning that there was, indeed, some bleeding at some sites in patients, scored as peri‐implant mucositis at patient level. But this low bleeding scores did not lead to a high infection rate, possibly resulting in hyperplasia. Prosthodontic complications related to treatment were mainly restricted to repair of the denture base and teeth. Mangano et al. (2011) reported that the majority of complications were related to the weakness of the attachment system connecting the bar and overdenture. In contrast, in the present trial, no clip repairs were observed. The absence of problems with the attachment system could be caused by a built‐in cobalt chromium reinforcement structure and gold retentive clips attached to this structure (Slot et al., 2012). The minimum number of relines needed could be caused by the fact that physiological resorption was minimal once the denture was supported by implants; a phenomenon that was also seen in the mandible (Kordatzis et al., 2003). At 10 years, in 41% of the participants, a new overdenture was made. After 5 years, this was only in 5% of the participants. Apparently, because of wear of the acrylic parts of the overdenture, new overdentures are needed in a considerable amount of participants. It must be said that the kind of maintenance and the number of events during 10 years is restricted to the combination of a maxillary and mandibular bar overdenture and does not count for other restorations or a natural dentition in the mandibular arch.
In the present trial, autogenous bone, with the iliac crest as donor site, has been used as grafting material for the sinus floor elevation procedure. Since the start of the clinical trial, some systematic reviews have been published which concluded that xenographic grafting materials only, as well as xenographic materials mixed with autogenous bone, resulted in comparable successful outcomes (Raghoebar et al., 2019; Rickert et al., 2012). If the iliac crest is no longer needed as a donor site for large amounts of bone, this would obviously lead to less morbidity.
At the start of this trial, cone beam computed tomography (CBCT) was not available at our Medical Center. The bone volume was, therefore, estimated by analyzing conventional two‐dimensional radiographs. Nowadays, the bone volume of the maxilla would have been measured by CBCT, which provides more accuracy in diagnosing the amount of bone necessary for the sinus floor surgery or this could even prevent this procedure.
Some limitations have to be addressed. First, when determining the group size at the start of the trial, it was calculated that 28 participants would be needed per group to detect a possible difference in marginal bone level change (Slot et al., 2014). After 10 years, 26 participants could be analyzed in the 4‐implant group and 20 participants in the 6‐implant group, meaning that the conclusions on marginal bone level change have lost some power. However, marginal bone level was rather comparable between the groups, indicating that both approaches are feasible. Second, this was a university‐based trial with experienced professionals and dedicated participants to a strict hygiene protocol, consisting of information, checking, and reinstruction of dental hygiene procedures at yearly visits. The patients were carefully selected to fit in the research protocol. Thus, the results of the present trial may deviate from those achieved by a general practice.
5. CONCLUSION
In spite of these limitations, it is concluded from this 10‐year randomized clinical trial that maxillary bar overdentures on four or six implants in the posterior region of augmented maxillae resulted in a comparable treatment outcome with high implant survival, limited loss of peri‐implant marginal bone, high patient satisfaction, and minimal prosthodontic maintenance, when opposing a mandibular 4‐implant overdenture.
AUTHOR CONTRIBUTIONS
Wim Slot: conceptualization (equal); data curation (lead); investigation (lead); methodology (lead); project administration (lead); formal analysis (lead); validation (lead); visualization (lead); writing – original draft (lead). Gerry Raghoebar: conceptualization (lead); data curation (equal); investigation (equal); methodology (equal); writing – review and editing (equal). Marco Cune: writing – review and editing (equal). Arjan Vissink: formal analysis (lead); visualization (equal); writing – review and editing (equal). Henny Meijer: conceptualization (lead); data curation (equal); investigation (equal); methodology (lead); project administration (equal); supervision (lead); validation (equal); writing – review and editing (lead).
FUNDING INFORMATION
Funding for the 1‐year clinical trial was obtained by an unrestricted grant from Institut Straumann AG, Basel, Switzerland.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Supporting information
Appendix S1
Slot, W. , Raghoebar, G. M. , Cune, M. S. , Vissink, A. , & Meijer, H. J. A. (2022). Maxillary bar overdentures on four or six posterior implants: 10‐year results from a randomized clinical trial. Clinical Oral Implants Research, 33, 1147–1156. 10.1111/clr.13997
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Bergendal, T. , & Engquist, B. (1998). Implant‐supported overdentures: A longitudinal prospective study. The International Journal of Oral & Maxillofacial Implants, 13, 253–262. [PubMed] [Google Scholar]
- Boven, C. , Raghoebar, G. M. , Vissink, A. , & Meijer, H. J. A. (2015). Improving masticatory performance, bite force, nutritional state and patient's satisfaction with implant overdentures: A systematic review of the literature. Journal of Oral Rehabilitation, 42, 220–233. 10.1111/joor.12241 [DOI] [PubMed] [Google Scholar]
- De Waal, Y. C. M. , Van Winkelhoff, A. J. , Meijer, H. J. A. , Raghoebar, G. M. , & Winkel, E. G. (2013). Differences in peri‐implant conditions between fully and partially edentulous subjects: A systematic review. Journal of Clinical Periodontology, 40, 266–286. [DOI] [PubMed] [Google Scholar]
- Di Francesco, F. , De Marco, G. , Capcha, E. B. , Lanza, A. , Cristache, C. M. , Vernal, R. , & Cafferata, E. A. (2021). Patient satisfaction and survival of maxillary overdentures supported by four or six splinted implants: A systematic review with meta‐analysis. BMC Oral Health, 21, 247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Francesco, F. , De Marco, G. , Gironi Carnevale, U. A. , Lanza, M. , & Lanza, A. (2019). The number of implants required to support a maxillary overdenture: A systematic review and meta‐analysis. Journal of Prosthodontic Research, 63, 15–24. 10.1016/j.jpor.2018.08.006 [DOI] [PubMed] [Google Scholar]
- Erdfelder, E. , Faul, F. , & Buchner, A. (1996). GPOWER: A general power analysis program. Behavior Research Methods, Instruments, & Computers, 28, 1–11. [Google Scholar]
- Ferrigno, N. , Laureti, M. , Fanali, S. , & Grippaudo, G. (2002). A long‐term follow‐up study of non‐submerged ITI implants in the treatment of totally edentulous jaws. Part I: Ten‐year life table analysis of a prospective multicenter study with 1286 implants. Clinical Oral Implants Research, 13, 260–273. [DOI] [PubMed] [Google Scholar]
- Fonteyne, E. , Burms, E. , Matthys, C. , Van Lierde, K. , & De Bruyn, H. (2021). Four‐implant‐supported overdenture treatment in the maxilla. Part II: Speech‐ and oral health‐related quality of life in patients with implant‐supported overdentures in the maxilla‐a prospective 3‐year follow‐up. Clinical Implant Dentistry and Related Research, 23, 680–691. 10.1111/cid.13034 [DOI] [PubMed] [Google Scholar]
- Fromentin, O. , Lassauzay, C. , Abi Nader, S. , Feine, J. , & de Albuquerque Junior, R. F. (2010). Testing the retention of attachments for implant overdentures ‐ validation of an original force measurement system. Journal of Oral Rehabilitation, 37, 54–62. 10.1111/j.1365-2842.2009.02020.x [DOI] [PubMed] [Google Scholar]
- Heydecke, G. , Boudrias, P. , Awad, M. A. , De Albuquerque, R. F. , Lund, J. P. , & Feine, J. S. (2003). Within‐subject comparisons of maxillary fixed and removable implant prostheses: Patient satisfaction and choice of prosthesis. Clinical Oral Implants Research, 14, 125–130. [DOI] [PubMed] [Google Scholar]
- Kalk, W. W. , Raghoebar, G. M. , Jansma, J. , & Boering, G. (1996). Morbidity from iliac crest bone harvesting. Journal of Oral and Maxillofacial Surgery, 54, 1424–1430. 10.1016/s0278-2391(96)90257-8 [DOI] [PubMed] [Google Scholar]
- Kordatzis, K. , Wright, P. S. , & Meijer, H. J. (2003). Posterior mandibular residual ridge resorption in patients with conventional dentures and implant overdentures. The International Journal of Oral & Maxillofacial Implants, 18, 447–452. [PubMed] [Google Scholar]
- Krennmair, G. , Krainhöfner, M. , & Piehslinger, E. (2008). Implant‐supported maxillary overdentures retained with milled bars: Maxillary anterior versus maxillary posterior concept. A retrospective study. The International Journal of Oral & Maxillofacial Implants, 23, 343–352. [PubMed] [Google Scholar]
- Lang, N. P. , Berglundh, T. , & Working Group 4 of the Seventh European Workshop on Periodontology . (2011). Periimplant diseases: Where are we now? – Consensus of the seventh European workshop on periodontology. Journal of Clinical Periodontology, 38(Suppl), 178–181. 10.1111/j.1600-051X.2010.01674.x [DOI] [PubMed] [Google Scholar]
- Löe, H. , & Silness, J. (1963). Periodontal disease in pregnancy. II: Correlation between oral hygiene and periodontal condition. Acta Odontologica Scandinavica, 21, 533–551. [DOI] [PubMed] [Google Scholar]
- Mangano, C. , Mangano, F. , Shibli, J. A. , Ricci, M. , Sammons, R. L. , & Figliuzzi, M. (2011). Morse taper connection implants supporting “planned” maxillary and mandibular bar‐retained overdentures: A 5‐year prospective multicenter study. Clinical Oral Implants Research, 22, 1117–1124. 10.1111/j.1600-0501.2010.02079.x [DOI] [PubMed] [Google Scholar]
- Meijer, H. J. A. , Raghoebar, G. M. , De Waal, Y. C. , & Vissink, A. (2014). Incidence of peri‐implant mucositis and peri‐implantitis in edentulous patients with an implant‐retained mandibular overdenture during a 10‐years' follow‐up period. Journal of Clinical Periodontology, 41, 1178–1183. [DOI] [PubMed] [Google Scholar]
- Meijndert, L. , Meijer, H. J. A. , Raghoebar, G. M. , & Vissink, A. (2004). A technique for standardized evaluation of soft and hard peri‐implant tissues in partially edentulous patients. Journal of Periodontology, 75, 646–651. 10.1902/jop.2004.75.5.646 [DOI] [PubMed] [Google Scholar]
- Messias, A. , Nicolau, P. , & Guerra, F. (2021). Different interventions for rehabilitation of the edentulous maxilla with implant‐supported prostheses: An overview of systematic reviews. The International Journal of Prosthodontics, 34, s63–s84. 10.11607/ijp.7162 [DOI] [PubMed] [Google Scholar]
- Mombelli, A. , Van Oosten, M. A. C. , Schürch, E. , & Lang, N. (1987). The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiology and Immunology, 2, 145–151. [DOI] [PubMed] [Google Scholar]
- Raghoebar, G. M. , Meijer, H. J. , Slot, W. , Slater, J. J. , & Vissink, A. (2014). A systematic review of implant‐supported overdentures in the edentulous maxilla, compared to the mandible: How many implants? European Journal of Oral Implantology, 7, 191–201. [PubMed] [Google Scholar]
- Raghoebar, G. M. , Onclin, P. , Boven, G. C. , Vissink, A. , & Meijer, H. J. (2019). Long‐term effectiveness of maxillary sinus floor augmentation: A systematic review and meta‐analysis. Journal of Clinical Periodontology, 46(Suppl 21), 307–318. 10.1111/jcpe.13055 [DOI] [PubMed] [Google Scholar]
- Raghoebar, G. M. , Schoen, P. , Meijer, H. J. , Stellingsma, K. , & Vissink, A. (2003). Early loading of endosseous implants in the augmented maxilla: A 1‐year prospective study. Clinical Oral Implants Research, 14, 697–702. [DOI] [PubMed] [Google Scholar]
- Raghoebar, G. M. , Timmenga, N. M. , Reintsema, H. , Stegenga, B. , & Vissink, A. (2001). Maxillary bone grafting for the insertion of endosseous implants: Results after 12‐124 months. Clinical Oral Implants Research, 12, 279–286. [DOI] [PubMed] [Google Scholar]
- Raghoebar, G. M. , Vissink, A. , Reintsema, H. , & Batenburg, R. H. (1997). Bone grafting of the floor of the maxillary sinus for the placement of endosseous implants. British Journal of Oral and Maxillofacial Surgery, 35, 119–125. [DOI] [PubMed] [Google Scholar]
- Rickert, D. , Slater, J. J. , Meijer, H. J. , Vissink, A. , & Raghoebar, G. M. (2012). Maxillary sinus lift with solely autogenous bone compared to a combination of autogenous bone and growth factors or (solely) bone substitutes. A systematic review. International Journal of Oral and Maxillofacial Surgery, 41, 160–167. 10.1016/j.ijom.2011.10.001 [DOI] [PubMed] [Google Scholar]
- Roccuzzo, M. , Bonino, F. , Gaudioso, L. , Zwahlen, M. , & Meijer, H. J. (2012). What is the optimal number of implants for removable reconstructions? A systematic review on implant‐supported overdentures. Clinical Oral Implants Research, 23(suppl. 6), 229–237. 10.1111/j.1600-0501.2012.02544.x [DOI] [PubMed] [Google Scholar]
- Sadowsky, S. J. , & Zitzmann, N. U. (2016). Protocols for the maxillary implant overdenture: A systematic review. The International Journal of Oral & Maxillofacial Implants, 31, 182–191. 10.11607/jomi [DOI] [PubMed] [Google Scholar]
- Sanna, A. , Nuytens, P. , Naert, I. , & Quirynen, M. (2009). Successful outcome of splinted implants supporting a “planned” maxillary overdenture: A retrospective evaluation and comparison with fixed full dental prostheses. Clinical Oral Implants Research, 20, 406–413. [DOI] [PubMed] [Google Scholar]
- Slot, W. , Raghoebar, G. M. , Cune, M. S. , Vissink, A. , & Meijer, H. J. (2019). Four or six implants in the maxillary posterior region to support an overdenture: 5‐year results from a randomized controlled trial. Clinical Oral Implants Research, 30, 169–177. 10.1111/clr.13403 [DOI] [PubMed] [Google Scholar]
- Slot, W. , Raghoebar, G. M. , Van Dijk, G. , & Meijer, H. J. (2012). Attachment of clips in a bar‐retained maxillary implant overdenture: A clinical report. Journal of Prosthetic Dentistry, 107, 353–357. 10.1016/S0022-3913(12)60088-2 [DOI] [PubMed] [Google Scholar]
- Slot, W. , Raghoebar, G. M. , Vissink, A. , Huddleston Slater, J. J. , & Meijer, H. J. (2010). A systematic review of implant‐supported maxillary overdentures after a mean observation period of at least 1 year. Journal of Clinical Periodontology, 37, 98–110. 10.1111/j.1600-051X.2009.01493.x [DOI] [PubMed] [Google Scholar]
- Slot, W. , Raghoebar, G. M. , Vissink, A. , & Meijer, H. J. (2014). A comparison between 4 and 6 implants in the maxillary posterior region to support an overdenture; 1‐year results from a randomized controlled trial. Clinical Oral Implants Research, 25, 560–566. 10.1111/clr.12118 [DOI] [PubMed] [Google Scholar]
- Smeets, E. C. , De Jong, K. J. , & Abraham‐Inpijn, L. (1998). Detecting the medically compromised patient in dentistry by means of the medical risk‐related history. A survey of 29.424 dental patients in The Netherlands. Preventive Medicine, 27, 530–535. 10.1006/pmed.1998.0285 [DOI] [PubMed] [Google Scholar]
- Stellingsma, K. , Slagter, A. P. , Stegenga, B. , Raghoebar, G. M. , & Meijer, H. J. A. (2005). Masticatory function in patients with an extremely resorbed mandible restored with mandibular implant‐retained overdentures: Comparison of three types of treatment protocols. Journal of Oral Rehabilitation, 32, 403–410. 10.1111/j.1365-2842.2005.01242.x [DOI] [PubMed] [Google Scholar]
- Telleman, G. , Raghoebar, G. M. , Vissink, A. , & Meijer, H. J. (2013). Short implants with a nanometer‐sized CaP surface provided with either a platform‐switched or platform‐matched abutment connection in the posterior region: A randomized clinical trial. Clinical Oral Implants Research, 24, 1316–1324. 10.1111/clr.12000 [DOI] [PubMed] [Google Scholar]
- Van Assche, N. , Michels, S. , Quirynen, M. , & Naert, I. (2012). Extra short dental implants supporting an overdenture in the edentulous maxilla: A proof of concept. Clinical Oral Implants Research, 23, 567–576. 10.1111/j.1600-0501.2011.02235.x [DOI] [PubMed] [Google Scholar]
- Vervoorn, J. M. , Duinkerke, A. S. H. , Luteijn, F. , & Van Der Poel, A. C. M. (1988). Assessment of denture satisfaction. Community Dentistry and Oral Epidemiology, 16, 364–367. [DOI] [PubMed] [Google Scholar]
- Visser, A. , Raghoebar, G. M. , Meijer, H. J. A. , & Vissink, A. (2009). Implant‐retained maxillary overdentures on milled bar suprastructures: A 10‐year follow‐up of surgical and prosthetic care and aftercare. International Journal of Prosthodontics, 22, 181–192. [PubMed] [Google Scholar]
- Watson, R. M. , Jemt, T. , Chai, J. , Harnett, J. , Heath, M. R. , Hutton, J. E. , Johns, R. B. , Lithner, B. , McKenna, S. , McNamara, D. C. , Naert, I. , & Taylor, R. (1997). Prosthodontic treatment, patient response, and the need for maintenance of complete implant‐supported overdentures: An appraisal of 5 years of prospective study. International Journal of Prosthodontics, 10, 345–354. [PubMed] [Google Scholar]
- Zitzmann, N. U. , & Marinello, C. P. (1999). Treatment plan for restoring the edentulous maxilla with implant‐supported restorations: Removable overdenture versus fixed partial denture design. Journal of Prosthetic Dentistry, 82, 188–196. 10.1016/s0022-3913(99)70155-1 [DOI] [PubMed] [Google Scholar]
- Zitzmann, N. U. , & Marinello, C. P. (2000). Treatment outcomes of fixed or removable implant‐supported prostheses in the edentulous maxilla. Part II: Clinical findings. Journal of Prosthetic Dentistry, 83, 434–442. 10.1016/s0022-3913(00)70038-2 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


