Background:
COVID-19 challenged U.S. trauma centers to grapple with demands for expanded services with finite resources while also experiencing a concurrent increase in violent injuries.
Objective:
The purpose of this study was to describe the impact of COVID-19 on the roles and duties of U.S. hospital-based injury prevention professionals.
Methods:
This descriptive cross-sectional survey study of hospital-based injury prevention professionals was conducted between June 2021 and August 2021. Participants were recruited from six organizational members of the national Trauma Prevention Coalition, including the American Trauma Society, Emergency Nurses Association, Injury Free Coalition for Kids, Safe States Alliance, Society for Trauma Nurses, and Trauma Center Association of America. Results were analyzed using descriptive and inferential statistics.
Results:
A total of 216 participants affiliated with 227 trauma centers responded. The following changes were reported during 2020: change in injury prevention position (range = 31%–88%); change in duties (range = 92%–100%); and change to hospital-based injury prevention programs (range = 75%–100%). Sixty-one (43%) single-center participants with a registered nurse license were reassigned to clinical duties compared with six (10%) nonlicensed participants (OR = 5.6; 95% CI [1.96, 13.57]; p < .001). Injury prevention programs at adult-only and combined adult and pediatric trauma centers had higher odds of suspension than pediatric-only trauma centers (OR = 3.6; 95% CI [1.26, 10.65]; p < .017).
Conclusion:
The COVID-19 response exposed the persistent inequity and limited prioritization of injury prevention programming as a key deliverable for trauma centers.
Keywords: COVID-19, Hospital-based, Injury prevention, Trauma center, Violence prevention
COVID-19 posed unprecedented challenges and continues to impact U.S. health care systems. During the early months of the pandemic and subsequent “waves” of SARS-CoV-2 virus outbreaks, hospitals responded to increased demand for patient care by changing infrastructure, reallocating hospital personnel, and prioritizing resources to support the rapid influx of critically ill patients (Uppal et al., 2020). As COVID-19 continued into its second year, hospitals began to grapple with stressors of ongoing demands for expanded services within the context of finite resources (Barbash & Kahn, 2021). A concurrent increase in violent injuries was also seen impacting trauma centers across the United States (Abdallah et al., 2021; Hatrchimonji et al., 2020; Klutts et al., 2022).
During this time, when hospital-based injury prevention resources should have been focusing on strategies to reduce and respond to community violence, there were modifications to job responsibilities, duties, and program capacity. The American Trauma Society revealed during an informal discussion group of professional and personal impacts of the pandemic on organization members, noting suspension of hospital-based injury prevention programs, reduction in programs, and injury prevention staff furloughed or reassigned to clinical duties (personal communication, May 8, 2020). A survey conducted by Safe States Alliance supported these reports, which found hospital and injury prevention providers reported that 87% of programs, training, and technical assistance were negatively impacted by COVID-19 (Safe States, 2021).
KEY POINTS
This study found an overall reduction of U.S. hospital-based injury and violence prevention programming during the COVID-19 pandemic response.
COVID-19 highlighted the inequity and limited prioritization of injury prevention programming as a key deliverable for trauma centers.
Trauma centers have an institutional commitment to recognize and overcome barriers and facilitate organized and effective approaches to injury prevention.
OBJECTIVE
The purpose of this study was to describe the impact of COVID-19 on the roles and duties of U.S. hospital-based injury prevention professionals.
METHODS
This study used a descriptive cross-sectional survey design using a 10-item electronic self-reporting survey of hospital-based injury prevention professionals. Purposive sampling was used to recruit participants through six organizational members of the national Trauma Prevention Coalition. This study was deemed not human subjects' research by the University of California, Davis, Institutional Review Board (IRB #1754547-1).
Survey Development
The survey was developed by a collaborative workgroup of the Trauma Prevention Coalition comprising injury prevention representatives from the American Trauma Society, Emergency Nurses Association, Injury Free Coalition for Kids, Safe States Alliance, Society for Trauma Nurses, and Trauma Center Association of America. After drafting and reviewing the initial survey questions, feedback was solicited and incorporated from members of the injury prevention committees within the respective organizations. A sample of hospital-based injury prevention professionals from diverse trauma centers across the United States beta-tested the validity of the survey for clarity of question, content, flow, and usability. The authors analyzed these preliminary results for systematic errors in data collection. The Trauma Prevention Coalition workgroup subsequently reviewed and approved the revised survey for dissemination using Qualtrics XM (Provo, UT).
Survey Structure
The final survey comprised nine questions categorized into three domains: (1) trauma center profile; (2) hospital-based injury prevention professional's position description and clinical licensure; and (3) impact of COVID-19 on hospital staff position, injury prevention job duties, and hospital-based injury prevention program. Response options were limited to numerical or multiple-choice with “not applicable (NA)” and free-text options for “other” responses. Respondents could provide multiple responses to questions asking to describe responses specific to changes related to position, job duties, and injury prevention programs. A copy of the survey is provided as Supplemental Digital Content (available at: http://links.lww.com/JTN/A79).
Survey Dissemination
The Trauma Prevention Coalition administrator sent an initial study recruitment email to the leadership of the six participating trauma organizations. The message included an introductory paragraph describing the purpose of the survey, an invitation to participate with a link to the online survey, and a request to forward the invitation to all organizational members associated with hospital-based injury prevention. The researchers did not utilize a reward-based system to encourage higher participation or completion results. Concurrently, members of the collaborative workgroup posted the invitation and survey link on their respective organizational social media platforms. After 1 month of data collection, the Trauma Prevention Coalition administrator sent a follow-up email to the trauma program manager members of each organization, requesting the invitation be forwarded to any individuals who were formerly in the role of injury prevention professional at the start of COVID-19 but had since left their position. The survey was open to responses from June 7, 2021, to August 31, 2021.
Statistical Analyses
The initial questions of the survey asked the respondent to best describe their injury prevention job position in January 2020, prior to the start of COVID-19, and in which state their trauma center injury prevention job was located. These questions allowed the authors to exclude those respondents who were not in a formal injury prevention position prior to COVID-19 to be best able to describe the impact of COVID-19 on the role and duties of hospital-based injury prevention professionals.
The respondents were stratified into five groups based on dedicated injury prevention professionals' position at a single trauma center (Groups 1–3), injury prevention job duties only at a single trauma center (Group 4), or dedicated injury prevention position at multiple trauma centers (Group 5) for the descriptive analyses (Tables 1–3). Group 1–3 divisions were based on trauma center level (I, II, and III–IV, respectively).
Table 1. Study Groups by Trauma Center Type and Level (N = 216).
| Adult-Only TC | Pediatric-Only TC | Adult and Pediatric TC | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Dedicated IPP at a single TC (n = 176) | |||||||
| Group 1 (Level I TC, n = 73) | 33 | 45 | 13 | 18 | 27 | 37 | |
| Group 2 (Level II TC, n = 71) | 59 | 83 | 4 | 6 | 8 | 11 | |
| Group 3 (Level III–IV TC, n = 32) | 12 | 37 | 2 | 6 | 18 | 57 | |
| IP duties only at a single TC (n = 24) | |||||||
| Group 4 (Level I TC, n = 5) | 3 | 60 | 1 | 20 | 2 | 20 | |
| Group 4 (Level II TC, n = 6) | 4 | 66 | 1 | 17 | 2 | 17 | |
| Group 4 (Level III–IV TC, n = 3) | 8 | 66 | 0 | 0 | 3 | 34 | |
| Dedicated IPP at multiple TCs (16 IPPs, n = 37 TCs) | |||||||
| Group 5 (Level I TC, n = 10) | 6 | 60 | 3 | 30 | 1 | 10 | |
| Group 5 (Level II TC, n = 8) | 7 | 88 | 1 | 12 | 0 | 0 | |
| Group 5 (Level III–V TC, n = 19) | 14 | 70 | 0 | 0 | 5 | 30 | |
Note. IP = injury prevention; IPP = injury prevention professional; TC = trauma center.
Table 3. Professional Licensure (N = 216).
| RN Only | EMS Only | RN and EMS | Other/None | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Dedicated IPP at a single TC (N = 176 IPPs representing 176 TCs) | ||||||||
| Group 1 (Level I, n = 73) | 36 | 49 | 14 | 19 | 1 | 2 | 22 | 30 |
| Group 2 (Level II, n = 71) | 49 | 69 | 3 | 4 | 11 | 16 | 8 | 11 |
| Group 3 (Levels III–IV, n = 32) | 23 | 72 | 3 | 9 | 1 | 3 | 5 | 16 |
| IP duties only at a single TC (N = 24 IPPs representing 24 TCs) | ||||||||
| Group 4 (n = 24) | 9 | 56 | 1 | 6 | 0 | 0 | 6 | 38 |
| Dedicated IPP at multiple TCs (N = 16 IPPs representing 37 TCs) | ||||||||
| Group 5 (IPP, n = 16) | 9 | 83 | 1 | 4 | 0 | 0 | 6 | 8 |
Note. EMS = emergency medical service; IP = injury prevention; IPP = injury prevention professional; RN = registered nurse; TC = trauma center.
All analyses were completed using Stata, Release 17 (StataCorp, College Station, TX). Frequency distributions were used to summarize the categorical data. Logistic regression was used to compare category responses between groups, trauma center type, trauma center level, and verification status. An α of .5 was used for determining statistical significance (p < .05).
RESULTS
A total of 324 individuals from 44 states responded to the survey, of whom 74 (22.8%) did not complete the survey, and 25 (7.7%) respondents were not in a formal injury prevention position or a role with injury prevention duties in January 2020 and were thus excluded. Of the 74 respondents who did not complete the survey, 35 opened the survey link but did not progress beyond the introduction describing the purpose of the survey. An additional 36 respondents were automatically forwarded to the end of the survey through skip-logic mechanism in Question 3: “Which one of the following best describes your injury prevention job position prior to the start of the COVID-19 pandemic?” after selecting the response “I was not working in any trauma center position related to injury prevention.” We otherwise did not ascertain any consistent pattern of exiting among the remaining 15 participants who did not complete the survey. There were no missing data across survey items among participants completing the survey. Analyses were conducted with 216 individuals representing 227 trauma centers across the United States (Figure 1). Because of the electronic snowball sampling recruitment technique, the number of individuals who received the survey invitation is unknown.
Figure 1.
Respondent flow chart.
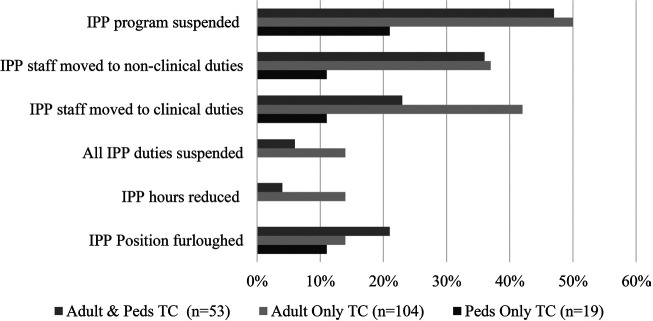
Most trauma centers represented by the five study groups were “adult-only” and “Level I or II” (Table 1), verified by the American College of Surgeons (ACS) or both ACS and state (Table 2). More than half of all groups held a registered nurse (RN) license (Table 3). Most respondents in Groups 1–3 reported some type of change to their injury prevention position (response range = 31%–88%), duties (response range = 92%–100%), and hospital-based injury and violence prevention program (response range = 75%–100%) during 2020 (Figure 2). The most notable impacts on position, duties, and programs reported were furloughing positions (response range = 14%–25%), shifting to clinical duties (response range = 19%–50%), working from home (response range = 13%–78%), transitioning to virtual delivery of injury and violence prevention programs (response range = 13%–100%), and suspending hospital-based injury and violence prevention programs (response range = 14%–75%).
Table 2. Study Groups by Trauma Center Verification Type (N = 216).
| ACS Only | State Only | ACS/State | None | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Dedicated IPP at a single TC (n = 176) | ||||||||
| Group 1 (Level I, n = 73) | 37 | 50 | 6 | 8 | 27 | 40 | 3 | 2 |
| Group 2 (Level II, n = 71) | 30 | 43 | 11 | 15 | 28 | 40 | 2 | 2 |
| Group 3 (Levels III–IV, n = 32) | 7 | 22 | 14 | 44 | 11 | 34 | 0 | 0 |
| IP duties only at a single TC (n = 24) | ||||||||
| Group 4 (n = 24) | 3 | 12 | 7 | 30 | 13 | 54 | 1 | 4 |
| Dedicated IPP at multiple TCs (16 IPP, n = 37 TCs) | ||||||||
| Group 5 (TC, n = 37) | 10 | 27 | 10 | 27 | 17 | 46 | 0 | 0 |
Note. ACS = American College of Surgeons; IP = injury prevention; IPP = injury prevention professional; TC = trauma center.
Figure 2.
Changes to injury prevention programs and duties by trauma center type. IPP = injury prevention program; TC = trauma center.
Sixty-one (43%) single-center participants with an RN license were reassigned to clinical duties, compared with six (10%) nonlicensed participants (OR = 5.6; 95% CI [1.96, 13.57]; p < .001). Injury prevention programs at adult-only and combined adult and pediatric trauma centers had higher odds of suspension than pediatric-only trauma centers (OR = 3.6; 95% CI [1.26, 10.65]; p < .017). Similarly, pediatric-only trauma centers reported fewer changes to injury prevention duties and programs than adult-only and combined adult and pediatric centers (Figure 2). No statistically significant differences were found in hospital-based injury prevention program elimination by trauma center level (OR = 0.41; 95% CI [0.06, 2.84]; p < .34) or verification (OR = 3.75; 95% CI [0.47, 29.36]; p < 0.21) or suspension by trauma center level (OR = 1.08; 95% CI [0.86, 1.36]; p < .48) or verification (OR = 1.03; 95% CI [0.76, 1.34]; p < .84).
DISCUSSION
Most injury and violence prevention professionals reported a change in their position, job duties, and program capacity, resulting in an overall reduction in hospital-based injury prevention programming during the COVID-19 response. The role of injury prevention was mandated by the American College of Surgeons Committee on Trauma (ACS COT) in the 2006 edition of Resources for Optimal Care of the Injured Patient for verification of hospitals as Level I and II trauma centers (ACS COT, 2006). The recognition of prevention as a key method to reducing the burden of trauma within the United States was validated in the 2014 update (ACS COT, 2014). Currently, the 2022 version requires that each trauma center have a designated individual whose job description contains requirements for injury prevention responsible for implementing at least two activities addressing separate major causes of injury within that trauma center (ACS COT, 2022). Within Level I trauma centers, this person must be separate from the trauma program manager or performance improvement personnel.
Despite the presence of this external mandate, the results of our study demonstrate that 26% (n = 13) of injury prevention professionals employed by Level I trauma centers prior to COVID-19 were furloughed during the response and 4% (n = 2) were eliminated entirely. This pattern was notably less significant in the pediatric-only trauma centers, leading the researchers to question what specific factors influenced this response for future research.
An additional requirement placed on trauma centers by the ACS to satisfy trauma center verification is that the trauma center must have an organized and effective approach to injury prevention, prioritizing those efforts on local epidemiological and trauma registry data when choosing evidence-based programs for implementation. This approach to injury prevention should include and track partnerships with other community organizations (ACS COT, 2014).
Again, despite this mandate, the results of our study revealed the suspension of hospital-based injury and violence prevention programming (response rate = 19%–44%). The concern this poses is that during this same time frame, when respondents reported a reduction in hospital-based injury prevention resources, the United States began to see a rise in injuries and violence within its communities. Researchers noted in the survey responses that trauma centers transitioned to virtual delivery of injury and violence prevention programs (response rate = 13%–100%) at varying rates.
The results of our study indicate the organizational commitment of hospitals and administrations to support the work of injury prevention remains inadequate. A 2017 survey by the Safe States Alliance and the National Association of County and City Health Officials (NACCHO) reported injury prevention programs across the United States were largely underfunded and understaffed, with insufficient opportunities for professional development (Keitt et al., 2018). A later survey of hospital-based injury prevention professionals confirmed a consistent lack of administrative support necessary to develop effective injury prevention initiatives (Adams et al., 2020). In a qualitative study of hospital-based injury prevention programs identifying factors that facilitate or serve as barriers to implementing evidence-based prevention programs, the analysis revealed that successful implementation was related to supportive institutional leadership and collaborative interdepartmental relationships; however, study participants indicated these factors were not the norm. Instead, limited training opportunities for staff orientation, professional development, funding availability, and program selection hindered program capacity (Newcomb et al., 2020).
The COVID-19 response further strained and highlighted the perpetuating inequity and limited prioritization of injury prevention programming as a key deliverable for trauma centers. Despite the external mandate of necessity for trauma center verification and a rising need for injury and violence prevention, most injury prevention professionals reported a change in their position, job duties, and program capacity, resulting in an overall reduction in hospital-based injury prevention programming. Those respondents who were RNs most dramatically felt this shift from prevention to a focus on clinical duties. Providing optimal care to the injured patient requires an appropriately designed and resourced trauma system along the public health model (ACS COT, 2014). This response is unachievable without recognizing the role of injury and violence prevention as essential criteria in the care of that patient and included within the national trauma system.
LIMITATIONS
Given the known general opinion highlighted by reports from injury prevention professionals revealing hospital-based injury prevention programs were being suspended or scaled back and injury prevention staff furloughed or reassigned to clinical duties, survey development was deemed the most efficient and effective means to gather objective data to measure the effectiveness of the COVID-19 response on hospital-based injury prevention professionals. Respondent bias may be present in both survey creation and participants' responses. The research team appreciated the potential inaccurate data generated by an imbalance in survey development or respondents.
The purposive sampling method was deemed the most feasible and appropriate to obtain more specific insight into and details of the status of hospital-based injury prevention programs. One limitation within this study is tied to the purposive sampling method chosen to recruit study participants, particularly the presence of sampling error. Of concern was the limited means to contact and include the responses of hospital-based injury prevention professionals who left the role, organization, or health care sector prior to dissemination of the survey and thus making them an unrepresented group within the survey analysis.
CONCLUSION
This study explores the impact of COVID-19 on the role and duties of hospital-based injury prevention professionals in the United States. The overwhelming majority of respondents reported a change to their position, duties, and hospital-based injury prevention program that could negatively impact the trauma center to respond to the burden of trauma within its community proactively. The local, regional, and national response to SARS-CoV-2 infection is critically important. However, the focus on safety through injury and violence prevention should not be absent, nor minimized from response efforts. Trauma systems must provide effective evidence-based injury and violence prevention efforts; accordingly, trauma centers have an institutional commitment to overcome barriers and facilitate organized and effective approaches to injury prevention within their communities.
Footnotes
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's website (WWW.JOURNALOFTRAUMANURSING.COM).
Contributor Information
Courtney Edwards, Email: courtney.edwards@phhs.org.
Sandra Strack Arabian, Email: sarabian@tuftsmedicalcenter.org.
Paige Colburn-Hargis, Email: colburn-hargis.paige@scrippshealth.org.
Gina Duchossois, Email: duchossois@chop.edu.
Christy Adams, Email: cmadams@ucdavis.edu.
REFERENCES
- Abdallah H. O., Zhao C., Kaufman E., Hatchimonji J., Swendiman R. A., Kaplan L. J., Seamon M., Schwab C. W., Pascual J. L. (2021). Increased firearm injury during the COVID-19 pandemic: A hidden urban burden.Journal of the American College of Surgeons, 232(2), 159–168.e3. 10.1016/j.jamcollsurg.2020.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams C., Strack Arabian S., Edwards C., Tinkoff G. (2020). Hospital-based injury and violence prevention: Defining the role of injury prevention professionals at trauma centers in the United States. The American Surgeon, 3134820979161. 10.1177/0003134820979161 [DOI] [PubMed] [Google Scholar]
- Barbash I. J., Kahn J. M. (2021). Fostering hospital resilience—Lessons from COVID-10. JAMA, 326(8), 693–694. 10.1001/jama.2021.12484 [DOI] [PubMed] [Google Scholar]
- Committee on Trauma of the American College of Surgeons (ACS COT). (2006). Resources for optimal care of the injured patient. American College of Surgeons. [Google Scholar]
- Committee on Trauma of the American College of Surgeons (ACS COT). (2014). Resources for optimal care of the injured patient. American College of Surgeons. [Google Scholar]
- Committee on Trauma of the American College of Surgeons (ACS COT). (2022). Resources for optimal care of the injured patient: 2022 standards. American College of Surgeons. [Google Scholar]
- Hatrchimonji J. S., Swendiman R. A., Seamon M. J., Nance M. L. (2020). Trauma does not quarantine: Violence during the COVID-19 pandemic. Annals of Surgery, 272(2), e53–e54. 10.1097/SLA.0000000000003996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keitt S. H., Alonso J., McPhillips-Tangum C., Lezin N., Carr M. (2018). Advancing trauma center injury and violence prevention: Public health and health care working together. Journal of Public Health Management and Practice, 24(3), 292–295. 10.1097/PHH.0000000000000798 [DOI] [PubMed] [Google Scholar]
- Klutts G. N., Deloach J., McBain S. A., Jensen H., Sexton K. W., Kalkwarf K. J., Karim S., Bhavaraju A. (2022). Increases in violence and changes in trauma admissions during the COVID quarantine. The American Surgeon, 88(3), 356–359. 10.1177/00031348211050824 [DOI] [PubMed] [Google Scholar]
- Newcomb A. B., Zadnik M., Carlini A. R., Francis M. M., Frey K. P., Heins S. E., McNamara L., Staguhn E. D., Castillo R. C. (2020). Barriers and facilitators to the implementation of injury prevention programs: A qualitative exploration and model development. Journal of Trauma Nursing, 27(6), 335–345. 10.1097/JTN.0000000000000540 [DOI] [PubMed] [Google Scholar]
- Safe States. (2021). Crisis amidst COVID-19: The state of injury and violence prevention in health departments and hospitals. Safe States Alliance. https://cdn.ymaws.com/www.safestates.org/resource/resmgr/covid/Crisis_Amdist_COVID-19.pdf [Google Scholar]
- Uppal A., Silvestri D. M., Siegler M., Natsui S., Boudourakis L., Salway R. J., Parikh M., Agoritsas K., Cho H. J., Gulati R., Nunez M., Hulbanni A., Flaherty C., Iavicoli L., Cineas N., Kanter M., Kessler S., Rhodes K. V., Bouton M., Wei E. K. (2020). Critical care and emergency department response at the epicenter of the COVID-19 pandemic. Health Affairs, 39(8), 1443–1449. 10.1377/hlthaff.2020.00901 [DOI] [PubMed] [Google Scholar]