Abstract
Background
Cancer diagnosis and treatment can cause fatigue, stress and anxiety which can have a detrimental effect on patients, families and the wider community. Mindfulness‐based interventions appear to have positive effects on managing these cancer‐related symptoms.
Objective
To investigate the efficacy of mindfulness on cancer related fatigue (CRF) and psychological well‐being in female cancer patients.
Methods
Five databases (CINHAL, Ovid Medline, Ovid Psych Info, Scopus, and Cochrane), and two trial registers (WHO and Clinicaltrials.gov) were searched for randomised control trials from inception to April 2021 and updated in August 2022. Meta‐analysis was performed using Review Manager 5.4. The standardised mean difference (SMD) and 95% confidence intervals (CI) were used to determine the intervention effect. Subgroup analysis was performed for adaptation to types of mindfulness, length of intervention and types of comparator used.
Results
Twenty‐one studies with a total of 2326 participants were identified. Mindfulness significantly improved CRF (SMD −0.81, 95% CI −1.17 to −0.44), depression (SMD−0.74, 95% CI −1.08 to −0.39) and anxiety (SMD −0.92, 95% CI −1.50 to −0.33). No effect was observed for quality of life (SMD 0.32, 95% CI −0.13–0.87) and sleep (SMD −0.65, 95% CI −1.34–0.04). Subgroup analysis revealed that there was little difference in SMD for adapted type of mindfulness (p = 0.42), wait list control compared to active comparator (p = 0.05) or length of intervention (p = 0.29).
Conclusion
Mindfulness appears to be effective in reducing CRF and other cancer related symptoms in women. Adaptations to mindfulness delivery did not have negative impact on results which may aid delivery in the clinical settings.
Keywords: cancer, meta‐analysis, mindfulness, mindfulness‐based cognitive therapy, mindfulness‐based stress reduction, oncology, psycho‐oncology, systematic review, women
1. BACKGROUND
Worldwide there are an estimated 8.5 million women with cancer, while in the UK there are more than 182,000 new cases per year. 1 , 2 Symptoms associated with diagnosis and treatment of cancer include depression, anxiety, sleep deprivation and fatigue. Cancer‐related fatigue (CRF) prevalence is higher in females and it is rated as the fourth most common unmet need among those living with and beyond gynaecology cancer. 3 , 4 , 5 , 6
The definition of CRF provided by the National Comprehensive Cancer Network illustrates its pervasiveness, as it is deemed to be a persistent feeling of tiredness that is physical and cognitive, it is not related to activity level and is not relieved by sleep. 7 CRF is multifaceted in nature and presentation, hence the interventions to manage this symptom need to be reflective of this. However, currently, the advice to manage CRF continues to be keeping active, eating a healthy diet and sleep hygiene. 8 However, research suggests that interventions such as exercise have mixed results for managing CRF, with some studies showing little or no effect. 9 , 10 , 11 , 12 , 13 , 14 Furthermore, it seems that exercise alone may not successfully target all aspects of CRF, for example, emotional or cognitive fatigue, may actually hinder participants' engagement in interventions such as exercise. 15 , 16 , 17 Diet and sleep hygiene although have evidence that may impact CRF, there remains a lack of studies that incorporate the role of diet in the direct management of CRF or sleep interventions that improve sleep substantially. 18 This lack of improvement in sleep can directly or indirectly effect CRF, this is known as a phenomena called ‘cluster symptoms’ where more than one symptom cluster together and effect each other positively or negatively, for CRF the symptoms identified include sleep, anxiety and depression. 19 The presence of these symptoms can lead to stress which may also lead to a further increase in the cluster symptoms. 20 The reduction of stress for cancer patients may be a factor in enhancing the management of CRF and interventions that can have the mind‐body impact that may result in improvements in lifestyle include interventions like mindfulness.
Mindfulness has been described as the intention of being aware of the present moment without judgement. 21 And the research for cancer in this area has seen exponential growth over the last 10 years. However, the majority of this research has focused on reduction of depression, anxiety and stress symptoms associated with CRF. 22 , 23 , 24 , 25 Practising mindfulness has been shown to help emotional self‐regulation, the development of positive coping mechanisms, and stress reduction, leading to improved quality of life (QoL) in women with breast cancer. 26 , 27 Mindfulness alone may be helpful in managing CRF or it can be the starting point that will allow individuals to access interventions that may further enhance the management of CRF.
Previous systematic reviews have evaluated the impact of mindfulness on psychological wellbeing, 28 , 29 , 30 showing a moderate effect on reducing anxiety and depression. However, some of these reviews were restricted in terms of the types of mindfulness for example, mindfulness‐based stress reduction (MBSR) or mindfulness‐based cognitive therapy (MBCT), and others only included certain cancer population, for example, breast cancer. 28 , 29 , 31 , 32 The reviews that evaluated mindfulness in relation to CRF have also focused on specific types of mindfulness or have only included certain populations or types of cancer. 33 , 34 However, a recent review 34 reported the positive effects that mindfulness had on both CRF and vitality, the authors of this review assessed CRF as tiredness and exhaustion and vitality as energy and levels of function, each was evaluated separately. This review included any type of cancer, males and females, at any stage of cancer and any type of mindfulness. To date, no systematic review has evaluated research studies that included women with cancer, any type of mindfulness and its impact on CRF. Hence, the aim of this review was to assess evidence for the impact of any type of mindfulness on CRF in women with cancer. The secondary aim was to consider the impact of mindfulness on psychological wellbeing, which was defined in the current review as depression, anxiety, and sleep, all of which are described as part of the symptom cluster of CRF.
2. METHOD
2.1. Search strategy
This review followed the preferred reporting of items of systematic reviews and meta‐analysis (PRISMA) statement. 35 The protocol was registered in PROSPERO CRD42021240439. 36 A systematic search was conducted using the Cochrane Central Register of Controlled Trials (CENTRAL), the Cochrane Database of Systematic Reviews, Ovid MEDLINE(R), EBSCO Cumulative Index to Nursing and Allied Health Literature (CINAHL), Ovid PsycINFO and, Scopus from inception until April 2021 and updated in August 2022. Trials registries were also searched, clinicaltrials. gov and WHO ICRTP along with Open Grey for grey literature. Hand searching and citation searching were also performed of eligible studies to identify any missing studies that databases may have missed. Each database was searched with a combination of MeSH and Keywords (1) cancer or neoplasm, (2) fatigue or tiredness or lethargy, and (3) mindfulness or meditation. (Additional search strategy provided in supporting material).
2.2. Inclusion and exclusion criteria
Studies were eligible for inclusion if they were randomised control trials (RCT) testing a mindfulness based intervention (e.g., MBSR, mindfulness‐based cognitive therapy (MBCT), mindfulness‐based art therapy (MBAT)), participants were female, over 18 with a diagnosis of cancer, fatigue was measured at baseline and one other timepoint post intervention, and studies were published in English. Comparison groups included treatment as usual/waitlist control or active treatments such as supportive care or education. Studies were excluded if mindfulness was not the main component (e.g., Acceptance and Commitment Therapy) and if reported as poster and or conference reports or abstracts.
2.3. Study selection
Studies were initially screen by titles and abstracts and excluded if they did not focus on fatigue and women with cancer. Full text articles were retrieved and checked for eligibility, by a team of reviewers and any disagreements resolved by consensus. RefWorks bibliography software was used to export, manage and deduplicate search results, with additional hand removal of duplicates.
2.4. Data extraction
Data were individually extracted (KMCC) and checked, by a team of reviewers, and any discrepancies were resolved through discussion. Data extracted included: author, year of publication, country of origin, age, stage of cancer, type of cancer, treatment status, intervention arms, outcomes, measures, eligibility criteria, assessment timepoints, the results such as the mean and standard deviations (effect size) for CRF, anxiety, depression, sleep and QoL and adverse events. An Excel spreadsheet was designed to capture these data.
2.5. Risk of bias assessment
The risk of bias was assessed for all 23 using the Cochrane risk‐of‐bias tool for randomised trials (RoB 2) 37 which includes 5 domains: randomisation, deviations from interventions, outcome measures, missing outcome data, reporting of results all of which are judged as low, some concerns and high with a summarised overall risk. This was completed by (KMCC) and 21% independently checked by other reviewers any discrepancies were discussed and consensus reached within the team.
2.6. Quality of assessment
The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) was performed to assess the quality of evidence of the included studies. This assessment goes beyond the risk of bias and includes 5 domains for assessment: risk of bias, inconsistency of the results, indirectness, imprecision, and publication bias possible ratings include high, moderate, low and very low. 38 GRADEpro was used to perform this assessment, and data for each outcome generated a ‘Summary of Findings Table’ with associated footnotes that explained any decisions on downgrading of the quality of evidence.
2.7. Data analysis
Review Manager software (RevMan version 5.4) was used to conduct the meta‐analysis, using a random‐effects (inverse variance method) as heterogeneity in treatment effects was anticipated due to between‐study variations in clinical factors (e.g., content of intervention). 39 Effects sizes were calculated as standardised mean differences (SMDs) with 95% confidence intervals (CIs) indicating the difference in means between groups divided by the pooled standard deviation (SD). Effect sizes were categorised by Cohen's classifications: SMD 0.2–0.5 small effect, SMD 0.5–0.8 medium effect, and SMD >0.8 large effect. 40 A negative SMD for CRF, depression, anxiety and sleep indicated a larger improvement in these outcomes due to the mindfulness intervention. For QoL a positive SMD indicated a larger reduction. Heterogeneity was evaluated using the I 2 statistics with values of 0%–40% representing might not be important, 30%–60% representing moderate, 50%–90% representing substantial and 75%–100% considerable heterogeneity. 41 Data was extracted for pre, post and first follow up for both intervention and control groups. Effect sizes were calculated for pre to post‐treatment and for pre‐treatment to last follow up.
2.8. Subgroup analysis
Subgroup analysis was intended for types of intervention (MBSR v non‐MBSR), length of intervention (8 weeks v > than 8 weeks) and active comparator (AC) versus wait‐list control (WLC) and usual care (UC).
2.9. Addressing missing data
In those studies that did not provide all the required data, authors were contacted via email to request SDs and means. If it was possible to calculate this from other data provided such as standard error (SE), CIs, or t‐values, then this was performed. Where it was not possible to access SDs and mean, these were excluded from the meta‐analysis.
2.10. Sensitivity analysis
Sensitivity analysis was carried out to ensure the robustness of the effect. For studies with a high risk of bias, all removal of these studies was performed to determine sensitivity to the results. If substantial or considerable heterogeneity was evident while performing meta‐analysis, then sensitivity analysis was also performed to explore reasoning. This may be performed by removing outliers with effect sizes that are two standard deviations from the pooled effect size. 42
3. RESULTS
3.1. Studies included
Electronic databases searching identified 1843 records. After deduplication, 1328 records were screened using the title, and the abstracts of these 1239 were excluded. This left 89 records, of which one report was unable to be retrieved. Following screening of the full text of 88 records 67 were excluded leaving 21 publications searching of reference lists and forward citations found, 2 additional eligible papers, resulting in a total of 23 eligible papers. Of the 23 papers, 20 were original RCT studies, and 3 were secondary publications of studies already included. Of the 23 records examined, 20 included sufficient evidence for analysis (Figure 1 PRISMA flow diagram).
FIGURE 1.
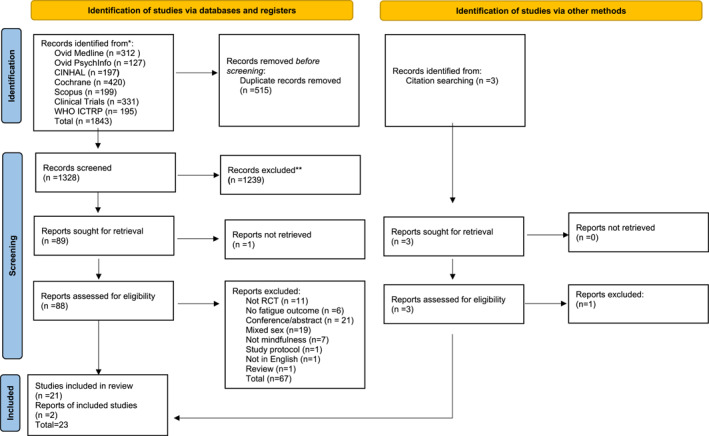
PRISMA flow diagram
3.2. Study characteristics
A total of 2326 participants were identified with an average of 116 per study (range 24–322). The mean age of the sample was 51 (range 41–64). The percentage of participants with breast cancer was 97%, and the remaining were gynaecology cancer (0.95%), Heamatology malignancy (0.65%), neuro‐oncology (0.25%), rectal carcinoma (0.30%) and other (0.85%). Most studies (n = 8, 42%) 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 adopted MBSR as the type of mindfulness programme. For many of the studies the intervention was greater than 8 weeks (n = 15, 79%) 43 , 47 , 48 , 49 , 50 , 51 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 duration. The comparator used was mainly (n = 11, 52%) 43 , 44 , 45 , 46 , 49 , 52 , 55 , 56 , 58 , 60 , 61 , 62 , 63 waitlist control or UC with only (n = 8, 38%) 47 , 48 , 50 , 51 , 53 , 54 , 57 , 59 , 64 using an AC. Only one study 49 assessed fatigue at baseline and stated fatigue severity score as an inclusion criteria. Very few (n = 5, 25%) 43 , 51 , 57 , 60 reported adverse events, and those studies that did report stated that there were no adverse events (Table 1).
TABLE 1.
Table of characteristics
| Sample size | Mean age | Race & ethnicity | Stage of cancer | Intervention features | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author year | Fatigue eligibility criteria | MBI | Control | MBI | Control | MBI | Control | Type of cancer | MBI | Control | Origin | MBI (type) | Control |
| Bower 2015 | N/A | 39 | 32 | 46.1 (28.4–60) | 47.7 (31.1–59.6) | White 29, African American1, Asian 5, other 1 | White 25, African American 1, Asian 5, other 1 | Breast | NR | NR | USA | (MAP) 6 weeks, 2 h per week | Wait list control. |
| Bower 2021 | N/A | 85 | 81 | 44.5 (7.7) | 45.8 (5.6) | White 75, black 3, Asian 5, other 2, hispanic 10 | White 126, black 16, Asian 15, other 3, hispanic 14 | Breast | NR | NR | USA | (MAP) 6 weeks, 2 h per week | SE 6 weeks |
| Carlson 2013 & 2006 | N/A | 134 | 118 | 55.12 (9.84) | 54.14 (10.23) | NR | NR | Breast | 0–5 (3.7), I‐56 (41.8), II‐51 (38.1), III‐17 (12.7), IV‐1 (0.7), Unkown‐4 (3.0) | (N9%) 0–2 (1.7), I‐49 (41.5), II‐42 (35.6), III‐16 (13.6), IV‐2 (1.7), Unknown‐7 (5.9) | Canada | MBSR 8 weeks group sessions, 90 min each | SET 12 weeks 1.5 h each. SMS 1 day |
| Chu 2020 | N/A | 42 | 42 | 54.6 (5.7) | 54.9 (6.3) | NR | NR | Breast | NR | NR | China | MBCT 8 weeks, 2 h per week | Usual care |
| Dodds 2015 | N/A | 16 | 17 | 54.7 (12.1) | 55.8 (9.7) | White 11 (92), non‐white 1 (8) | White 12 (75), non‐white 4 (25) | Breast | I‐3 (25), II‐5 (42), III‐4 (33), IV‐0 (0) | I‐1 (6), II‐9 (56), III, 4 (25), IV‐2 (13) | USA | CBCT 8 weeks, 2 h classes | Wait list control |
| Franco 2019 | N/A | 19 | 17 | 41.27 (9.76) | Not reported | NR | NR | Breast | NR | NR | Spain | Flow meditation 7 weeks, 2 h per week | Not stated |
| Gok Metin 2019 | N/A | 32 | 31 (PMR) 29 (CG) | 48.21 (10.23) | PMR 46.67 (10.06) CG 52.86 (11.70) | NR | NR | Breast | I‐4 (12.5), II‐16 (50), III‐12 (37.5) | PMR‐I‐4 (12.9), II‐19 (61.3), III‐8 (25.8) CG I‐1 (4), II‐16 (55.2), III‐12 (41.4) | Turkey | Mindfulness meditation daily once a day for 12 weeks | PMR (progressive muscle relaxation) daily once a day for 12 weeks |
| Hoffman 2012 | N/A | 12 | 12 | 49 (9.26) | 50.1 (9.14) | NR | NR | Breast | 0–11 (10), 1–34 (30), II‐47 (41), III‐22 (20) | 0–6 (5), I‐45 (39), II‐47 (41), III‐17 (15) | UK | MBSR 8 weeks 2 h per week, first session 2.25 h | Wait list control |
| Jang 2016 | N/A | 12 | 12 | 51.75 (5.32) | 51.42 (6.33) | NR | NR | Breast | NR | NR | Korea | MBAT 12 weeks 45 min each | Wait list control |
| Kenne 2017 | N/A | 62 | 52 (active controls) 52 (non‐MBSR) | 57.2 (10.2) | 57.2 (10.2) | NR | NR | Breast | NR | NR | Sweden | MBSR 8 weeks 2 h per week | Active control‐8 weeks self‐instruct MBSR, CG |
| Lengacher 2009 & 2012 | NA | 41 | 43 | 57.1 | 58.0 | White 36 (87.8), hispanic 6 (14.6), black‐ 2 (4.9) other 3 (7.3) | White 34 (79.1), hispanic 3 (7), black 8 (18.6), other 1 (2.3) | Breast | 0–5 (12.2), I‐26 (63.4), II‐7 (17.1), III‐3 (7.3) | 0–9 (20.9), I‐19 (44.2), II‐12 (27.9), III‐3 (7) | USA | MBSR 6 weeks, 2 h per week. | Wait list control |
| Mattes 2019 | N/A | 10 | 15 | 64.2 (9.1) | 62.9 (9.1) | NR | NR | Breast | Stage I‐III no breakdown | Stage I‐III no breakdown | Germany | MBSR 8 weeks | Nordic walking 8 weeks |
| Monti 2006 | N/A | 56 | 55 | 53.1 (12.4) | 54.1 (10.7) | Caucasian 45 (80), African American 10 (18), Asian 1 (2), hispanic 0, | Caucasian 38 (69), African American 13 (24), Asian 1 (2), hispanic 2 (4), other 1 (2) | Breast 51 (46), gynaecology 19 (17), haematology 13 (12), neuro 5 (5), rectal 6 (5), other 17 (15) | 29−0,I, II, 27‐III, IV | 28−0, I, II, 27‐III, IV | USA | MBAT 8 weeks, 2.5 h | Wait list control |
| Monti 2013 | N/A | 98 | 93 | 56.9 (12.4) | 56.4 (10.7) | Caucasian 59 (60), African American 35 (36), Asian/Other 0 | Caucasian 54 (58), African American 37 (40), Asian/Other 2 (2) | Breast | 0‐I (1), I‐36 (37), II‐25 (26), III‐11 (11), IV‐3 (3), unkown‐22 (22) | 0–1 (1), I‐39 (42), II‐23 (25), III‐5 (5), IV‐2 (2), unkown‐23 (2) | USA | MBAT 8 weeks | 8 weeks meeting weekly. |
| Park 2020 | N/A | 38 | 36 | 53.21 (8.4) | 54.19 (9.27) | N/A | N/A | Breast | 0–9 (23.7), I‐13 (34.2), II‐14 (36.8), III‐2 (5.3) | 0–6 (16.7), I‐14 (38.9), II‐15 (41.7), III‐1 (2.7) | Japan | MBAT 8 week, 2 h per week | Wait list control |
| Rahmani 2014 | NR | 12 | 12 (MCT) 12 (UC) | 43.25 (3.08) | MCT 44.92 (1.83) UC 44.92 (1.8) | NR | NR | Breast | NR | NR | Iran | MBSR 8 weeks, 2 h sessions per week | Metacognition (MCT) 8 sessions. |
| Rahmani 2015 | Fatigue severity at baseline | 12 | 12 | 43.25 (3.07) | 44.8 (28) | NR | NR | Breast | NR | NR | Iran | MBSR 8 weeks, 2 h sessions | None |
| Reich 2017 & Lengacher 2016 | N/A | 167 | 155 | 56.5 (10.2) | 57.6 (9.2) | Caucasian 112 (67.1), black 21 (12.6), hispanic 19 (11.4), other 15 (9) | Caucasian 110 (71.0), black 16 (10.5), hispanic 14 (9.1), other | Breast | 0–21 (12.6), I‐53 (31.7), II‐61 (36.5), III‐32 (19.2) | 0–19 (12.3), I‐56 (36.1), II‐54 (34.8), III‐26 (16.8) | USA | MBSR (BC) 6 weeks 2 h per week | Usual care |
| Van der gucht 2020 | N/A | 18 | 15 | 43.89 (6.03) | 47.4 (5.45) | NR | NR | Breast | NR | NR | Belgium | MBSR/MBCT 8 weeks × 4 3 h sessions | Wait list control |
| Witek Janusek 2019 | N/A | 96 | 96 | 55 (10.1) | 55.2 (10.1) | Caucasian 80.8, African American 11.5, hispanic 2.6, PI/Asian 1.3, other 1.3 | Caucasian 72.5, African American 15.8, hispanic 6.6, PI/Asian 1.3, other 2.6 | Breast | 0–22.9, I‐51.8, II‐16.9, III‐8.4, | 0–24.4, I‐62.2, II‐11.0, III‐2.4 | USA | MBSR 8 weeks 2.5 h per week | Active control condition (ACC) 8 week |
Abbreviations: CBCT, Compassion based cognitive therapy; MAPS, mindfulness awareness practice; MBAT, mindfulness‐based art therapy; MBCT, mindfulness‐based cognitive therapy; MBSR, mindfulness‐based stress reduction; MBSR (BC), mindfulness‐based stress reduction breast cancer; MCT, metacognition therapy; PMR, Progressive muscle relaxation; SET, Supportive Expressive therapy; SE, Survivorship Education; SMS, Stress management seminar.
3.3. Pooled effects at post‐intervention
A forest plot for effect size of CRF is shown in Figure 2 17 studies were included in this analysis. As shown in Table 2 mindfulness significantly improved CRF post‐intervention with the effect size being large (SMD −0.81). In addition, mindfulness had a significant effect on the secondary outcomes of depression and, anxiety with effect sizes being large (depression; SMD −0.74; anxiety; SMD −0.92). However, mindfulness did not have a significant effect on both QOL and sleep.
FIGURE 2.
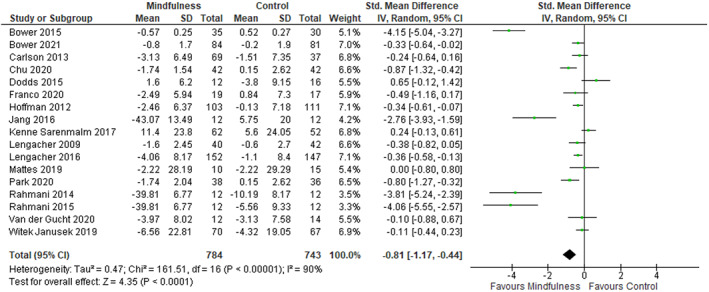
Forest Plot for fatigue‐post intervention effect size
TABLE 2.
Outcomes measures pooled effects for post intervention and follow up
| Outcome | Sample size | Effect size a | Heterogeneity b | ||||
|---|---|---|---|---|---|---|---|
| Post‐intervention: | K | N | SMD | 95% CI | p | I2 | p |
| Fatigue | 17 | 1527 | −0.81 | −1.17 to −0.44 | <0.0001 | 90% | <0.00001 |
| Anxiety | 7 | 1017 | −0.92 | −1.50 to −0.33 | 0.002 | 95% | <0.00001 |
| Depression | 12 | 1347 | −0.74 | −1.08 to −0.39 | <0.0001 | 88% | <0.00001 |
| QOL | 10 | 925 | 0.37 | −0.13 to –0.87 | 0.15 | 91% | <0.00001 |
| Sleep | 5 | 597 | −0.65 | −1.34 to 0.04 | 0.06 | 92% | <0.0001 |
| Follow‐up | |||||||
| Fatigue | 12 | 1141 | −0.55 | −0.86 to −0.25 | 0.0003 | 80% | <0.00001 |
| Anxiety | 4 | 675 | −0.59 | −0.93 to −0.25 | 0.007 | 76% | 0.006 |
| Depression | 8 | 1052 | −0.28 | −0.58 to 0.01 | 0.06 | 80% | <0.00001 |
| QOL | 8 | 791 | −0.06 | −0.65 to 0.53 | 0.85 | 92% | <0.00001 |
| Sleep | 4 | 504 | 0.04 | −0.47 to 0.55 | 0.89 | 83% | 0.0006 |
Note: Bold values indicate statistical significance.
Abbreviation: QOL, Quality of life.
ES = SMD, fatigue, anxiety, depression and sleep negative values indicates a favourable response. For QOL a positive value indicates a positive result. Values: small (0.2–0.5), moderate (0.5–0.8), large (>0.8).
p values <0.1 taken to suggest heterogeneity. I 2 statistics: 0% (no heterogeneity), 25% (low heterogeneity), 50% (moderate heterogeneity), and 75% (high heterogeneity).
There was evidence of considerable heterogeneity between studies for change in CRF (p = <0.00001, I 2 = 90%) depression (p = <0.00001, I 2 = 88%), anxiety (p = <0.00001, I 2 = 95%) QoL (p = <0.00001, I 2 = 91%) and sleep (p = <0.00001, I 2 = 92%). Sensitivity analysis was performed by removing outliers, which reduced the heterogeneity for CRF, anxiety and sleep from considerate to moderate or not being present, but did not appear to change the levels of heterogeneity for depression or QoL (See Table 2). The removal of outliers also reduced the pooled effect size from large to between moderate or small for all outcomes. Further sensitivity analysis was performed by removing studies with poor study quality which resulted in a reduction in heterogeneity from considerate to where it may not be considered important for CRF, anxiety and sleep but resulted in little change in heterogeneity for depression. Although the pooled effect size was also reduced from large to moderate or small for all outcomes (Table 2).
3.4. Sub‐group analysis
Sub group analysis was performed for type the of mindfulness, length of intervention and comparator used.
The effects of the mindfulness intervention were analysed as two groups, those studies that used MBSR as the mindfulness intervention compared with studies that used other types of mindfulness that were non‐MBSR (MBCT, MBAT, MBCR, Flow and CBCT). Both groups showed positive effect of mindfulness on CRF (non‐MBSR; SMD −0.93; MBSR; SMD −0.62) but there was no significant differences between groups (p = 0.42). There were significant differences for depression and anxiety, with non‐MBSR showing a greater pooled effect than MBSR (Table S1 in supporting materials for further information). There were no significant sub‐group differences for QoL or sleep, however given that there was only one study in the non‐MBSR sleep group, this sub‐group analysis result should be interpreted with caution.
Heterogeneity remained considerable for sub‐groups in the outcome of fatigue, depression, anxiety and QOL. For depression and anxiety the level of heterogeneity was reduced to low and very low in the MBSR group within the sub‐group analysis (Supporting materials Table S1).
In terms of length of intervention, studies of 8 weeks duration in length were compared to those that were less than 8 weeks. One study was of 12 weeks duration as this was considered an outlier, it was omitted from the analysis. For CRF, anxiety, and depression, there appeared to be no significant difference between sub‐groups with both showing a favourable response to mindfulness (SMD range −0.56 to −1.03). Mindfulness did not have a significant effect on QOL and sleep (Table S1 in supporting materials).
In the comparator analysis studies that used a WLC or UC were grouped together, and studies that used what was defined as AC were grouped together. For CRF, and anxiety this analysis indicated no significant difference between groups however, the pooled effect and overall effect showed a favourable response to the WLC group (CRF WLC; p = <0.0001 anxiety WLC; p = 0.03) with little or no effect for AC groups (CRF AC p = 0.13; anxiety AC p = 0.08) heterogeneity remained considerable for both these outcomes. Although there was a statistical significant between groups for depression the favourable response like the other outcomes, of CRF and anxiety, remained large for WLC (SMD −1.14) whereas AC showed little or no effect and demonstrated no heterogeneity within in this analysis (Table S1 in supporting materials). The subgroups for depression differed in the number of studies and number of participants suggesting that subgroup analysis may not be able to detect differences. For QOL and sleep both groups did not show a favourable response to mindfulness.
3.5. Pooled effects at follow up
Only (n = 12) studies provided data that could be included in an analysis Table 2 shows mindfulness 43 , 45 , 47 , 49 , 50 , 51 , 52 , 55 , 56 , 60 , 61 , 63 continued to show a significant pooled effect for CRF at follow up (SMD −0.55) and for the secondary outcomes of depression and anxiety (depression; SMD −0.28; anxiety; SMD −0.59). For QoL, and sleep the follow up remained non‐significant and continued to show little or no effect. The follow up periods for the studies included in this analysis were between 4 weeks and 6 months this variation along with the differing characteristics of the included types and durations of mindfulness may have contributed to the considerable heterogeneity that was shown in the analysis (Table 2).
3.6. Risk of bias
Results indicated that over 50% of studies were, assessed as having high overall risk of bias, mainly due to lack of blinding associated with outcome measures (domains 4) and deviations from intended interventions (domain 2). However, it must be noted due to the nature of these intervention studies, blinding is a common issue as it is difficult to blind participants and outcome assessors to interventions as quite often the outcomes are patient reported. The domain with the lowest risk of bias assessed missing outcome data (domain 3), with 14 out of the 20 studies assessed as low. This was expected, as most of the studies accounted for missing data through intention‐to‐treat analysis. Risk of bias from the randomisation process was also low (domain 1), as most studies provided adequate descriptions, however, many of the studies failed to adequately describe the allocation. The level of some concern was also high for reporting of studies, as very few trials were either pre‐registered or had a pre‐defined analysis plan (See Figure 3).
FIGURE 3.
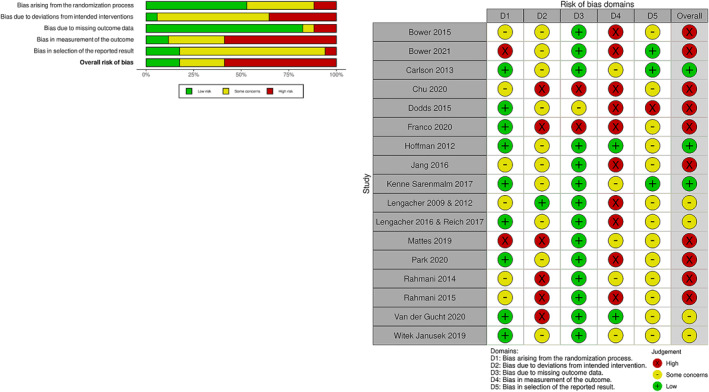
Risk of bias for fatigue outcome
3.7. Grading of recommendations, assessment, development and evaluation
Using GRADE the overall quality of evidence was rated as low or very low suggesting a low level of confidence in the effect estimate. The level of evidence for RCT was downgraded from high to low for sleep and anxiety and very low for fatigue, depression and QoL. This reduction from high to low or very low was due to serious concerns regarding levels of heterogeneity, risk of bias and publication bias. Overall, no serious concern were found for inconsistency or indirectness (See Table S2 Summary of findings table in supporting materials).
3.8. Publication bias
Publication bias was assessed using funnel plots for fatigue and, QoL, outcome measures that have fewer than 10 studies were not assessed as a minimum of 10 studies is required for a funnel plot to detect bias. 65 The funnel plots demonstrated asymmetry which would be suggestive of publication bias (Figure S1 in supporting material).
4. DISCUSSION
To our knowledge this is the first study to conduct a meta‐analysis on the impact of mindfulness on fatigue for women with cancer. The results of this meta‐analysis suggest that mindfulness led to a reduction in CRF post intervention and at follow up. For the secondary aim, mindfulness reduced anxiety and depression post intervention, with slight reductions at follow up, however no significant improvements were noted in sleep or QoL. The analysis showed that there was considerable heterogeneity between studies for all outcomes an attempt to account for this was performed through sensitivity analysis and removal of outliers although there was some reduction it continued to be considerable (Table S1 in supporting material).
This large effect of mindfulness on CRF (SMD −0.81) is in keeping with other reviews that also demonstrated similar pooled effects for CRF (Xie 2020) 33 (SMD −0.89), Zhang 2016 66 (SMD −0.88). However, in contrast, some reviews have demonstrated a smaller or even a larger pooled effect size than the current review demonstrated, regardless, these reviews have all shown a favorable response for mindfulness in improving CRF (Lin et al. 2022), 67 (SMD −0.56), Zhang et al. 2019 29 (SMD −0.66), Haller et al. 2017 31 (SMD −0.28), Xunluin et al. 2020. 30 (SMD 0.48) Schell et al. 2019 32 (SMD −0.50). Indeed in a recent meta‐analysis, 68 that examined the effect of psychosocial interventions on CRF demonstrated that MBSR had the largest impact when compared to other types of interventions. These conflicting results may have been due to differences in the types of mindfulness, types of cancer, outcomes and aims within these reviews. Reviews on mindfulness and CRF have to date focused on either a specific type of mindfulness (MBSR) or specific cancers, such as breast, additionally reviews that have included many types of mindfulness have included various types and stages of cancer. 32 , 33 , 34 To date no review has assessed whether any type of mindfulness has an effect on CRF for women with cancer, therefore, this review has contributed new knowledge in this area.
Psychological well‐being, which included depression and anxiety, showed that mindfulness improved this symptom in this review. Many of the included studies had the primary aim of psychological well‐being. 43 , 44 , 45 , 46 , 48 , 52 , 53 , 54 , 55 , 58 , 59 , 63 , 69 Improvement in the symptoms of anxiety and depression may directly or indirectly effect other symptoms, such as CRF or sleep. Indeed, Reich et al., (2017) 52 examined the symptom cluster and identified that fatigue, sleep, and psychological well‐being were part of the cluster, suggesting they are interrelated and that they may impact each other. This interrelation of symptoms on CRF was also demonstrated in a mindfulness intervention of 249 women with breast cancer. 70 Within this study, mindfulness had the biggest effect on CRF directly but also indirectly by relieving or preventing anxiety, depression and sleep disturbance. However, these relationships between CRF and sleep was not demonstrated in other research, Carlson and Garland, 2005, 71 found a significant relationship between stress and fatigue which suggested that a reduction in stress affected fatigue. MBSR has been well documented for reducing and helping in the management of stress which may lead to an effect on fatigue, many of the studies in this review assessed this outcome as part of psychological well‐being. 44 , 45 , 46 , 51 , 52 , 59 , 63 Other reviews also demonstrated an effect on depression and anxiety although the magnitude of the effect differed from large to small. 29 , 30 , 31 , 66 , 72
Neither sleep nor QoL showed a significant effect when data were pooled for this review. This was also reflected in previous reviews, Zhang et al., 2016 29 found women with breast cancer reported some improvement in sleep after a mindfulness intervention, but this was not statistically, which is in contrast to the findings of Cillessen et al., 2019. 72 Few previous systematic reviews have assessed sleep as part of the review aims, indeed, within this review, only 5 studies post intervention and 4 at follow up assessed this as outcome, therefore the impact of mindfulness on sleep is difficult to interpret. Regarding QoL, previous systematic reviews have differed in the impact of mindfulness on this variable, with Cillessen et al. 2019, 72 finding no significant impact, and Haller et al., 2017, 31 reporting a small but significant effect. Within the current review the results there were no significant effects of mindfulness on QoL, however, the CI (SMD 0.37, 95% CI −0.13–0.87) was compatible with a slight improvement and little or no effect suggesting some improvement even though it was not statistically significant. Whether this was due to the variability of the outcome measures used in the included studies or other variables, it is difficult to ascertain, and further research for this symptom maybe warranted.
Few of the studies in this review assessed fatigue as a primary aim. Whilst Gok Metin et al., 2019, 57 stated that fatigue was an outcome of primary interest, this study could not be included in the meta‐analysis, as the data presented within the paper did not allow for this, and the author was contacted but did not respond. This study did demonstrate a significant result for the reduction in fatigue following the interventions of progressive muscle relaxation or mindfulness meditation. It also suggested that the positive emotional effect of mindfulness may also have an effect on energy levels. Reviews that have attempted to examine the relationship of the effect of mindfulness with participants who have fatigue at base line have suggested a larger effect for participants that enter studies with fatigue than those studies that do not assess participant levels at entry. 73 , 74 Whether this is seen as an inevitable result as there may be more scope for improvement if participants pre scores are large for a symptom, or if mindfulness may truly be able to treat symptoms such as fatigue remains to be further investigated.
Studies that reported follow up at least at one time point after post‐intervention were analysed and showed that there was a continued favorable response for improvement for fatigue, depression and anxiety after a mindfulness intervention. However, the pooled effect was smaller at follow up than post intervention for all outcomes. Few reviews have examined the effects at follow up and those that did show the effect of mindfulness at follow up varied. For example, Cillessen et al., 2019, 72 and Haller et al., 2017 31 found that anxiety and depression continued to show improvement but CRF was not statistically significant. Johns et al., 2021, 34 findings for CRF were similar to this review and continued to show effect for CRF but the effect size was smaller than at post intervention. These variations and some reduction in pooled effect sizes for outcome measures may be because some studies failed to report these data, but may also be a result of differences in the length of follow‐ups being, weeks or several months after the intervention.
Five studies made reference to their being no adverse events associated with their interventions, the remaining 75% of studies ignored this as part of their reporting. Even though the likelihood of adverse events for mindfulness is viewed as being low, this should be reported in all studies, as mindfulness can have a negative impact on people with anxiety disorders. 75 Most of the included studies in this review had exclusion criteria associated with mental health contraindications for participating in mindfulness. 43 , 44 , 45 , 46 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 However, this may suggest that recruitment into mindfulness studies to ameliorate CRF may not be representative of the general cancer population and this has implications for clinical practice as discussed below.
4.1. Limitations
Among the strengths of this current review are its emphases on CRF and the inclusion of all types of mindfulness. This allowed for the inclusion of a wide variety of studies, and the focus on women with cancer alone also further gave rise to establishing knowledge in this area. However, the wide variety of studies may have resulted in considerable heterogeneity as the study intervention characteristics were many and varied. Attempts were made to explain this heterogeneity through sensitivity analysis and sub group analysis however, not all could be explained and may be a result of other variables that could not be accounted for. Also the review was limited to English which has excluded those studies from another language that may have been included.
4.2. Clinical implications
Future implications would include a more diverse population in terms of types and stages of cancer as well as ethnic diversity. Unfortunately, studies of this type tend to attract a particular participant profile that tends to be highly motivated. Within this review, the majority of participants were Caucasian (72.42%), had breast cancer (97.42%) and the level of education or socioeconomic background was difficult to establish, as few studies report these details. As this review was gender specific it was able to demonstrate the positive effects of mindfulness on outcomes for women but also highlighted that other types of female cancer such as gynaecology cancer (0.95%) are underrepresented within the literature. Female cancer and its treatment may result in biological process such as the menopause occurring sooner or quicker, which could result in symptoms like fatigue, mood changes and sleep disturbance that are similar to those already experienced by cancer and possibly add further to them. This review has shown some evidence that may help women to manage these symptoms however, it has also demonstrated the need for more research in female specific cancers. Other reviews have also suggested the need for more research regarding race, ethnic group and types of cancer. 34
Currently, nearly all the studies within this review were performed face to face, but as this review shows, adaptations to types and duration of mindfulness interventions did not have a detrimental effect on the overall effect, which may make it feasible to further adapt this type of intervention to a digital platform. Covid‐19 has resulted in a trigger for the use of online services to manage health and has been received in the most part positively however, it still has its issues such as poor bandwidth and users technology skills. 76 Never the less the delivery of mindfulness interventions through these types of platforms would be worth further investigations as it would permit scalability and the ability to reach a larger population especially those in hard to reach rural area. 77 Alongside this, the need for more robust studies with active comparators such as exercise that focus on outcomes such as CRF are needed.
Characteristics of mindfulness interventions particularly the type and duration did not demonstrate within this review a difference between groups. Although there appeared to be a slightly larger effect for the non‐MBSR and the less than 8 weeks in duration group all types of mindfulness demonstrated a favourable response to the outcomes of CRF, anxiety and depression. Cillessen et al., 2019, 72 also found that there was no difference in efficacy between types of mindfulness intervention and that all types were effective however, they did establish that there was a larger effect if adherence to the original protocol was maintained. These results may demonstrate that reducing the length of the intervention or adapting the type of mindfulness does not appear to have a detrimental effect on the overall effect and indeed may aid delivery in future clinical settings, as compliance may be easier with shorter interventions. This would also have financial implications for clinical settings and possibly reduce participant burden.
When assessing types of comparator, the analysis showed there were no differences between sub groups the comparison against WLC appears to show a greater favourable response in this review for all outcomes, which has also been identified in other reviews. This is not unexpected as studies that have a WLC or UC can result in a larger effect size in the intervention arms. 34 The small number of studies that used AC as the control arm in this review (n = 6, 32%) may have contributed to the findings. Other reviews also found similar findings where there were either too few studies to perform sub group analysis or the results were more favourable for the intervention groups compared to an AC group. 31 , 34 Furthermore, the type of AC may have an effect, as other reviews have suggested that if the comparator interventions are not developed for the management of particular symptoms, such as fatigue, then the results for these outcomes may not be reflective. 34 The use of specific interventions for control arms was demonstrated by Monti 2013 et al., in their 3 arm study with women with breast cancer and the effect of mindfulness or educational support on stress and QoL. They found that even though the MBAT maybe more beneficial for stress reduction and improved QoL than the support group or untreated group, the active control group was still beneficial and therefore still a worthy intervention in this population. Alongside this comparing or combining mindfulness with other interventions such as exercise 78 which is already supported by guidelines for managing fatigue, may provide evidence to enable health care professionals to make informed decisions with regard to interventions that could be offered to their patients.
5. CONCLUSION
In conclusion, there appeared to be a large effect of mindfulness on fatigue, anxiety and depression however, there was little or no effect on sleep and QoL. In terms of sub group analysis, there was little difference in the groups suggesting that all types of mindfulness and duration of intervention were effective. Follow up showed that the response was sustained although slightly reduced when compared to post intervention which may indicate the need for participants to continue practising. The demographics of the participants reported within the studies in this review show that certain types of cancer and ethnicity of the participants are underrepresented and further studies may aim to address this. Overall mindfulness is an intervention that is well received with few adverse events and is adaptable, which will make it a transferrable and scalable intervention within the clinical setting.
AUTHOR CONTRIBUTIONS
All authors contributed and approved the final manuscript.
CONFLICT OF INTEREST
The authors report no conflict of interest.
ETHICS STATEMENT
For this type of study formal ethical approval was not required.
Supporting information
Supporting Information S1
ACKNOWLEDGEMENTS
Kelly McCoo subject librarian. We would like to acknowledge funding from the Department for the Economy, Northern Ireland.
McCloy K, Hughes C, Dunwoody L, Marley J, Gracey J. Effects of mindfulness‐based interventions on fatigue and psychological wellbeing in women with cancer: a systematic review and meta‐analysis of randomised control trials. Psychooncology. 2022;31(11):1821‐1834. 10.1002/pon.6046
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analysed in this study.
REFERENCES
- 1. Cancer Statistics for the UK . 2015. Accessed June 8, 2022. https://www.cancerresearchuk.org/health‐professional/cancer‐statistics‐for‐the‐uk
- 2. World Cancer Research Fund . Ovarian Cancer Statistics; 2018. Accessed January 28, 2022.
- 3. Beesley V, Eakin E, Steginga S, Aitken J, Dunn J, Battistutta D. Unmet needs of gynaecological cancer survivors: implications for developing community support services. Psycho Oncol. 2008;17(4):392‐400. 10.1002/pon.1249 [DOI] [PubMed] [Google Scholar]
- 4. Sekse RJT, Hufthammer KO, Vika ME. Fatigue and quality of life in women treated for various types of gynaecological cancers: a cross‐sectional study. J Clin Nurs. 2015;24(3‐4):546‐555. 10.1111/jocn.12647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tian L, Lu H, Lin L, Hu Y, Lu HJ. Effects of aerobic exercise on cancer‐related fatigue: a meta‐analysis of randomized controlled trials. Support Care Cancer. 2016;24(2):969‐983. 10.1007/s00520-015-2953-9 [DOI] [PubMed] [Google Scholar]
- 6. Al Maqbali M, Al Sinani M, Al Naamani Z, Al Badi K, Tanash MI. Prevalence of fatigue in patients with cancer: a systematic review and meta‐analysis. J Pain Symptom Manag. 2020. [DOI] [PubMed] [Google Scholar]
- 7. Berger AM, Mooney K, Alvarez‐Perez A, et al. Cancer‐related fatigue, version 2.2015. J Natl Compr Cancer Netw. 2015;13(8):1012‐1039. 10.6004/jnccn.2015.0122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tiredness (fatigue) ‐ Macmillan Cancer Support . 2018. Accessed June 8, 2022. https://www.macmillan.org.uk/cancer‐information‐and‐support/impacts‐of‐cancer/tiredness
- 9. Courneya KS, Segal RJ, Mackey JR, et al. Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial. J Clin Oncol. 2007;25(28):4396‐4404. 10.1200/jco.2006.08.2024 [DOI] [PubMed] [Google Scholar]
- 10. Kim SH, Shin MS, Lee HS, et al. Randomized pilot test of a simultaneous stage‐matched exercise and diet intervention for breast cancer survivors. Oncol Nurs Forum. 2011;38(2):E97‐E106. 10.1188/11.onf.e97-e106 [DOI] [PubMed] [Google Scholar]
- 11. Cheville AL, Kollasch J, Vandenberg J, et al. A home‐based exercise program to improve function, fatigue, and sleep quality in patients with stage IV lung and colorectal cancer: a randomized controlled trial. J Pain Symptom Manag. 2013;45(5):811‐821. 10.1016/j.jpainsymman.2012.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lin K, Frawley HC, Denehy L, Feil D, Granger CL. Exercise interventions for patients with gynaecological cancer: a systematic review and meta‐analysis. Physiotherapy. 2016;102(4):309‐319. 10.1016/j.physio.2016.02.006 [DOI] [PubMed] [Google Scholar]
- 13. Kelley GA, Kelley KS. Exercise and cancer‐related fatigue in adults: a systematic review of previous systematic reviews with meta‐analyses. BMC Cancer. 2017;17(1):1‐17. 10.1186/s12885-017-3687-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wanchai A, Armer JM, Stewart BR. Nonpharmacologic supportive strategies to promote quality of life in patients experiencing cancer‐related fatigue: a systematic review. Clin J Oncol Nurs. 2011;15(2):203‐214. 10.1188/11.cjon.203-214 [DOI] [PubMed] [Google Scholar]
- 15. Bower JE. Cancer‐related fatigue—mechanisms, risk factors, and treatments. Nat Rev Clin Oncol. 2014;11(10):597‐609. 10.1038/nrclinonc.2014.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Naraphong W, Lane A, Schafer J, Whitmer K, Wilson BRA. Exercise intervention for fatigue‐related symptoms in Thai women with breast cancer: a pilot study. Nurs Health Sci. 2015;17(1):33‐41. 10.1111/nhs.12124 [DOI] [PubMed] [Google Scholar]
- 17. Poort H, de Rooij BH, Ezendam NPM, et al. Patterns and predictors of cancer‐related fatigue in ovarian and endometrial cancers: 1‐year longitudinal study. Cancer. 2020;126(15):3526‐3533. 10.1002/cncr.32927 [DOI] [PubMed] [Google Scholar]
- 18. Crowder SL, Playdon MC, Gudenkauf LM, et al. A molecular approach to understanding the role of diet in cancer‐related fatigue: challenges and future opportunities. Nutrients. 2022;14(7):1496. 10.3390/nu14071496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. He X, Ng MS, Wang X, et al. A dance program to manage a fatigue‐sleep disturbance‐depression symptom cluster among breast cancer patients receiving adjuvant chemotherapy: a feasibility study. Asia‐Pacific J Oncol Nurs. 2021;8(3):337‐339. 10.4103/2347-5625.308677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ando M, Kira H, Hayashida S, Ito S. Effectiveness of the mindfulness art therapy short version for Japanese patients with advanced cancer. Art Ther. 2016;33(1):35‐40. 10.1080/07421656.2016.1128764 [DOI] [Google Scholar]
- 21. Kabat‐Zinn J, Thich Nhat H. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain and Illness. Revised Edition ed. Bantam; 2013. [Google Scholar]
- 22. Lengacher CA, Johnson‐Mallard V, Fitzgerald S, et al. Feasibility of a mindfulness‐based stress reduction program for early‐stage breast cancer survivors. J Holist Nurs. 2011;29(2):107‐117. 10.1177/0898010110385938 [DOI] [PubMed] [Google Scholar]
- 23. Carlson LE, Tamagawa R, Stephen J, Drysdale E, Zhong L, Speca M. Randomized‐controlled trial of mindfulness‐based cancer recovery versus supportive expressive group therapy among distressed breast cancer survivors (MINDSET): long‐term follow‐up results. Psycho Oncol. 2016;25(7):750‐759. 10.1002/pon.4150 [DOI] [PubMed] [Google Scholar]
- 24. Johns SA, Brown LF, Beck‐Coon K, et al. Randomized controlled pilot trial of mindfulness‐based stress reduction compared to psychoeducational support for persistently fatigued breast and colorectal cancer survivors. Support Care Cancer. 2016;24(10):4085‐4096. 10.1007/s00520-016-3220-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Atreya CE, Kubo A, Borno HT, et al. Being Present: a single‐arm feasibility study of audio‐based mindfulness meditation for colorectal cancer patients and caregivers. PLoS One. 2018;13(7):e0199423. 10.1371/journal.pone.0199423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bruggeman Everts FZ, van der Lee ML, de Jager Meezenbroek E. Web‐based individual Mindfulness‐Based Cognitive Therapy for cancer‐related fatigue—a pilot study. Internet Interv Appl Inf Technol Ment Behavl. 2015;2(2):200‐213. 10.1016/j.invent.2015.03.004 [DOI] [Google Scholar]
- 27. Eyles C, Leydon GM, Hoffman CJ, et al. Mindfulness for the self‐management of fatigue, anxiety, and depression in women with metastatic breast cancer: a mixed methods feasibility study. Integr Cancer Ther. 2015;14(1):42‐56. 10.1177/1534735414546567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cramer H, Lauche R, Paul A, Dobos G. Mindfulness‐based stress reduction for breast cancer‐a systematic review and meta‐analysis. Curr Oncol. 2012;19(5):E343‐E352. 10.3747/co.19.1016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zhang Q, Zhao H, Zheng Y. Effectiveness of mindfulness‐based stress reduction (MBSR) on symptom variables and health‐related quality of life in breast cancer patients‐a systematic review and meta‐analysis. Support Care Cancer. 2019;27(3):771‐781. 10.1007/s00520-018-4570-x [DOI] [PubMed] [Google Scholar]
- 30. Xunlin NG, Lau Y, Klainin‐Yobas P. The effectiveness of mindfulness‐based interventions among cancer patients and survivors: a systematic review and meta‐analysis. Support Care Cancer. 2020;28(4):1563‐1578. 10.1007/s00520-019-05219-9 [DOI] [PubMed] [Google Scholar]
- 31. Haller H, Winkler MM, Klose P, Dobos G, Kümmel S, Cramer H. Mindfulness‐based interventions for women with breast cancer: an updated systematic review and meta‐analysis. Acta Oncol. 2017;56(12):1665‐1676. 10.1080/0284186x.2017.1342862 [DOI] [PubMed] [Google Scholar]
- 32. Schell LK, Monsef I, Wöckel A, Skoetz N. Mindfulness‐based stress reduction for women diagnosed with breast cancer. Cochrane Database Syst. Rev. 2019;3(3):CD011518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Xie C, Dong B, Wang L, et al. Mindfulness‐based stress reduction can alleviate cancer‐related fatigue: a meta‐analysis. J Psychosom Res. 2020:130. [DOI] [PubMed] [Google Scholar]
- 34. Johns SA, Tarver WL, Secinti E, et al. Effects of mindfulness‐based interventions on fatigue in cancer survivors: a systematic review and meta‐analysis of randomized controlled trials. Crit Rev Oncol Hematol. 2021;160:160. 10.1016/j.critrevonc.2021.103290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178‐189. 10.1016/j.jclinepi.2021.03.001 [DOI] [PubMed] [Google Scholar]
- 36. McCloy K, Gracey J, Hughes C, Dunwoody L, Marley J. Mindfulness based interventions for cancer related fatigue and psychological well being in female cancer patients. Prospero Int Prospect Regist Syst Rev. 2021. [Google Scholar]
- 37. Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC. Chapter 8: Assessing Risk of Bias in a Randomized Trial. 2022. handbook/current/chapter‐08. Accessed May 5, 2022.
- 38. Schünemann HJ, Higgins JPT, Vist GE, et al. Chapter 14: Completing ‘Summary of Findings’ Tables and Grading the Certainty of the Evidence. 2022. handbook/current/chapter‐14. Accessed May 5, 2022.
- 39. DerSimonian L. Meta‐analysis in clinical trials. Contr Clin Trials. 1986;7(3):177‐188. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 40. Cohen L, Warneke C, Fouladi RT, Rodriguez MA, Chaoul‐Reich A. Psychological adjustment and sleep quality in a randomized trial of the effects of a Tibetan yoga intervention in patients with lymphoma. Cancer. 2004;100(10):2253‐2260. 10.1002/cncr.20236 [DOI] [PubMed] [Google Scholar]
- 41. Deeks JJ, Higgins JPT, Altman DG. Chapter 10: Analysing Data and Undertaking Meta‐Analyses. 2022. handbook/current/chapter‐10. Accessed May 5, 2022.
- 42. Lipsey MW, Wilson D. Practical Meta‐Analysis. SAGE; 2001. [Google Scholar]
- 43. Lengacher CA, Johnson‐Mallard V, Post‐White J, et al. Randomized controlled trial of mindfulness‐based stress reduction (MBSR) for survivors of breast cancer. Psycho Oncol. 2009;18(12):1261‐1272. 10.1002/pon.1529 [DOI] [PubMed] [Google Scholar]
- 44. Hoffman CJ, Ersser SJ, Hopkinson JB, Nicholls PG, Harrington JE, Thomas PW. Effectiveness of mindfulness‐based stress reduction in mood, breast‐ and endocrine‐related quality of life, and well‐being in stage 0 to III breast cancer: a randomized, controlled trial. J Clin Oncol. 2012;30(12):1335‐1342. 10.1200/jco.2010.34.0331 [DOI] [PubMed] [Google Scholar]
- 45. Lengacher CA, Reich RR, Post‐White J, et al. Mindfulness based stress reduction in post‐treatment breast cancer patients: an examination of symptoms and symptom clusters. J Behav Med. 2012;35(1):86‐94. 10.1007/s10865-011-9346-4 [DOI] [PubMed] [Google Scholar]
- 46. Rahmani S, Talepasand S, Ghanbary‐Motlagh A. Comparison of effectiveness of the metacognition treatment and the mindfulness‐based stress reduction treatment on global and specific life quality of women with breast cancer. Iran J Cancer Prev. 2014;7(4):184‐196. [PMC free article] [PubMed] [Google Scholar]
- 47. Rahmani S, Talepasand S. The effect of group mindfulness ‐ based stress reduction program and conscious yoga on the fatigue severity and global and specific life quality in women with breast cancer. Med J Islam Repub Iran. 2015;29. [PMC free article] [PubMed] [Google Scholar]
- 48. Lengacher CA, Reich RR, Paterson CL, et al. Examination of broad symptom improvement resulting from mindfulness‐based stress reduction in breast cancer survivors: a randomized controlled trial. J Clin Oncol. 2016;34(24):2827‐2834. 10.1200/jco.2015.65.7874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kenne Sarenmalm E, Mårtensson LB, Andersson BA, Karlsson P, Bergh I. Mindfulness and its efficacy for psychological and biological responses in women with breast cancer. Cancer Med. 2017;6(5):1108‐1122. 10.1002/cam4.1052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Reich RR, Lengacher CA, Alinat CB, et al. Mindfulness‐based stress reduction in post‐treatment breast cancer patients: immediate and sustained effects across multiple symptom clusters. J Pain Symptom Manag. 2017;53(1):85‐95. 10.1016/j.jpainsymman.2016.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mattes* JF. Effect of moderate running training and mindfulness based stress reduction on immune system and quality of life in women with breast cancer receiving aromatase inhibitors. Can Archit. 2019;1:1‐4. [Google Scholar]
- 52. Witek Janusek L, Tell D, Mathews HL. Mindfulness based stress reduction provides psychological benefit and restores immune function of women newly diagnosed with breast cancer: a randomized trial with active control. Brain Behav Immun. 2019;80:358‐373. 10.1016/j.bbi.2019.04.012 [DOI] [PubMed] [Google Scholar]
- 53. Monti DA, Peterson C, Kunkel EJ, et al. A randomized, controlled trial of mindfulness‐based art therapy (MBAT) for women with cancer. PSYCHO Oncol. 2006;15(5):363‐373. 10.1002/pon.988 [DOI] [PubMed] [Google Scholar]
- 54. Carlson LE, Doll R, Stephen J, et al. Randomized controlled trial of mindfulness‐based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer (MINDSET). J Clin Oncol. 2013;31(25):3119‐3126. 10.1200/jco.2012.47.5210 [DOI] [PubMed] [Google Scholar]
- 55. Monti DA, Moss A, Mathews M, et al. Psychosocial benefits of a novel mindfulness intervention versus standard support in distressed women with breast cancer. Psycho Oncol. 2013;22(11):2565‐2575. 10.1002/pon.3320 [DOI] [PubMed] [Google Scholar]
- 56. Dodds SE, Pace TWW, Bell ML, et al. Feasibility of Cognitively‐Based Compassion Training (CBCT) for breast cancer survivors: a randomized, wait list controlled pilot study. Support Care Cancer. 2015;23(12):3599‐3608. 10.1007/s00520-015-2888-1 [DOI] [PubMed] [Google Scholar]
- 57. Carlson LE, Tamagawa R, Stephen J, Drysdale E, Zhong L, Speca M. Randomized‐controlled trial of mindfulness‐based cancer recovery versus supportive expressive group therapy among distressed breast cancer survivors (MINDSET): long‐term follow‐up results. PSYCHO Oncol. 2016;25(7):750‐759. 10.1002/pon.4150 [DOI] [PubMed] [Google Scholar]
- 58. Jang S, Kang S, Lee H, Lee S. Beneficial effect of mindfulness‐based art therapy in patients with breast Cancerâ randomized controlled trial. Explor J Sci Heal. 2016;12(5):333‐340. 10.1016/j.explore.2016.06.003 [DOI] [PubMed] [Google Scholar]
- 59. Gok Metin Z, Karadas C, Izgu N, Ozdemir L, Demirci U. Effects of progressive muscle relaxation and mindfulness meditation on fatigue, coping styles, and quality of life in early breast cancer patients: an assessor blinded, three‐arm, randomized controlled trial. Eur J Oncol Nurs. 2019;42:116‐125. 10.1016/j.ejon.2019.09.003 [DOI] [PubMed] [Google Scholar]
- 60. Chu X, Lou Y, Wang Z, Xu Q. Effect of mindfulness based cognitive therapy on the mental health and quality of life in patients with breast cancer. Indian J Pharmaceut Sci. 2020;82:44‐48. 10.36468/pharmaceutical-sciences.spl.143 [DOI] [Google Scholar]
- 61. Park S, Sato Y, Takita Y, et al. Mindfulness‐based cognitive therapy for psychological distress, fear of cancer recurrence, fatigue, spiritual well‐being, and quality of life in patients with breast Cancerâ randomized controlled trial. J Pain Symptom Manag. 2020;60(2):381‐389. 10.1016/j.jpainsymman.2020.02.017 [DOI] [PubMed] [Google Scholar]
- 62. Van der Gucht K, Ahmadoun S, Melis M, et al. Effects of a mindfulness‐based intervention on cancer‐related cognitive impairment: results of a randomized controlled functional magnetic resonance imaging pilot study. Cancer. 2020;126(18):4246‐4255. 10.1002/cncr.33074 [DOI] [PubMed] [Google Scholar]
- 63. Bower JE, Crosswell AD, Stanton AL, et al. Mindfulness meditation for younger breast cancer survivors: a randomized controlled trial. Cancer. 2015;121(8):1231‐1240. 10.1002/cncr.29194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bower JE, Partridge AH, Wolff AC, et al. Targeting depressive symptoms in younger breast cancer survivors: the pathways to wellness randomized controlled trial of mindfulness meditation and survivorship education. J Clin Oncol. 2021;39(31):3473‐3484. 10.1200/jco.21.00279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ. Br Med J. 1997;315(7109):629‐634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Zhang J, Xu R, Wang B, Wang J. Effects of mindfulness‐based therapy for patients with breast cancer: a systematic review and meta‐analysis. Complement Ther Med. 2016;26:1‐10. 10.1016/j.ctim.2016.02.012 [DOI] [PubMed] [Google Scholar]
- 67. Lin L, Lin L, Tzeng G, et al. Effects of mindfulness‐based therapy for cancer patients: a systematic review and meta‐analysis. J Clin Psychol Med Settings. 2022;29(2):432‐445. 10.1007/s10880-022-09862-z [DOI] [PubMed] [Google Scholar]
- 68. Yuan Y, Lin L, Xie C, et al. Effectiveness comparisons of various psychosocial therapies for cancer‐related fatigue: a Bayesian network meta‐analysis. J Affect Disord. 2022. [DOI] [PubMed] [Google Scholar]
- 69. Franco C, Amutio A, Mañas I, Sánchez‐Sánchez LC, Mateos‐Pérez E. Improving psychosocial functioning in mastectomized women through a mindfulness‐based program: flow meditation. Int J Stress Manage. 2020;27(1):74‐81. 10.1037/str0000120 [DOI] [Google Scholar]
- 70. Ikeuchi K, Ishiguro H, Nakamura Y, Izawa T, Shinkura N, Nin K. The relation between mindfulness and the fatigue of women with breast cancer: path analysis. Biopsychosoc Med. 2020;14(1):1‐9. 10.1186/s13030-020-0175-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Carlson LE, Garland SN. Impact of mindfulness‐based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med. 2005;12(4):278‐285. 10.1207/s15327558ijbm1204_9 [DOI] [PubMed] [Google Scholar]
- 72. Cillessen L, Johannsen M, Speckens AEM, Zachariae R. Mindfulness‐based interventions for psychological and physical health outcomes in cancer patients and survivors: a systematic review and meta‐analysis of randomized controlled trials. Psycho Oncol. 2019;28(12):2257‐2269. 10.1002/pon.5214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Duong N, Davis H, Robinson PD, et al. Mind and body practices for fatigue reduction in patients with cancer and hematopoietic stem cell transplant recipients: a systematic review and meta‐analysis. Crit Rev Oncol‐Hematol. 2017;120:210‐216. 10.1016/j.critrevonc.2017.11.011 [DOI] [PubMed] [Google Scholar]
- 74. Haussmann A, Schmidt ME, Illmann ML, et al. Meta‐analysis of randomized controlled trials on yoga, psychosocial, and mindfulness‐based interventions for cancer‐related fatigue: what intervention characteristics are related to higher efficacy? Cancers. 2022;14(2016):2016. 10.3390/cancers14082016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Van Dam N T, van Vugt MK, Vago DR, et al. Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect Psychol Sci. 2018;13(1):36‐61. 10.1177/1745691617709589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Cottrell M, Burns CL, Jones A, et al. Sustaining allied health telehealth services beyond the rapid response to COVID‐19: learning from patient and staff experiences at a large quaternary hospital. J Telemed Telecare. 2021;27(10):615‐624. 10.1177/1357633x211041517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Wherton J, Greenhalgh T, Shaw SE. Expanding video consultation services at pace and scale in scotland during the COVID‐19 pandemic: national mixed methods case study. J Med Internet Res. 2021;23(10):e31374. 10.2196/31374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Cataldi S, Greco G, Mauro M, Fischetti F. Effect of exercise on cancer‐related fatigue: a systematic review. J Hum Sport Exerc. 2021;16(3):476‐492. 10.14198/jhse.2021.163.01 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.


