Abstract
Apical membrane antigen 1 (AMA1) is considered one of the leading candidates for inclusion in a vaccine against blood stages of Plasmodium falciparum. Although the ama1 gene is relatively conserved compared to those for some other potential vaccine components, numerous point mutations have resulted in amino acid substitutions at many sites in the polypeptide. The polymorphisms in AMA1 have been attributed to the diversifying selection pressure of the protective immune responses. It was therefore of interest to investigate the impact of sequence diversity in P. falciparum AMA1 on the ability of anti-AMA1 antibodies to inhibit the invasion of erythrocytes in vitro by P. falciparum merozoites. For these studies, we used antibodies to recombinant P. falciparum 3D7 AMA1 ectodomain, which was prepared for testing in early clinical trials. Antibodies were raised in rabbits to the antigen formulated in Montanide ISA720, and human antibodies to AMA1 were isolated by affinity purification from the plasma of adults living in regions of Papua New Guinea where malaria is endemic. Both rabbit and human anti-AMA1 antibodies were found to be strongly inhibitory to the invasion of erythrocytes by merozoites from both the homologous and two heterologous lines of P. falciparum. The inhibitory antibodies targeted both conserved and strain-specific epitopes within the ectodomain of AMA1; however, it appears that the majority of these antibodies reacted with strain-specific epitopes in domain I, the N-terminal disulfide-bonded domain, which is the most polymorphic region of AMA1.
Plasmodium falciparum infections in malaria-naïve individuals can lead to severe morbidity, which may be life threatening if untreated. Continued exposure to infection leads to a degree of immunity, and consequently, older children and adults living in areas of endemicity are protected from the severe clinical consequences of infection with P. falciparum. The effector mechanisms that mediate naturally acquired immunity to malaria are not completely understood, but antibodies to the asexual blood stage parasites play a role. This has been most clearly demonstrated by the reduction of parasitemias following the passive immunization of children with clinical malaria with immunoglobulin G (IgG) from malaria-immune adults (6, 7, 32).
Antigens recognized by antibodies that are active in passive-immunization experiments are prime candidates for testing in a vaccine. Studies with an assay for antibody-dependent cellular inhibition have identified antibodies to MSP3 as an active component of passively transferred human IgG (28), but much evidence indicates that other merozoite antigens are capable of inducing antibodies that limit parasite development (13–15, 17, 26, 29, 33, 34).
One of the prime candidate antigens for inclusion in a malaria vaccine is apical membrane antigen 1 (AMA1). AMA1 is an 83-kDa antigen that is synthesized in mature stages of the parasite and is initially localized in the necks of the rhoptry organelles (9, 30). At about the time of merozoite release, the full-length 83-kDa molecule is localized at the apical pole, and an N-terminally processed form of 66 kDa can be detected distributed around the merozoite surface (27, 30). Although the biological function of AMA1 is unknown, its location and stage specificity suggest that it may be involved in the process of erythrocyte invasion.
AMA1 is one of only a few asexual blood stage antigens that have been identified in all Plasmodium species examined (42), and this has enabled the vaccine potential of AMA1 to be investigated using various animal models. Active immunization of monkeys or mice with either native (11) or recombinant (2, 8) forms of AMA1 has protected these animals against simian and rodent parasites, respectively. Much evidence indicates that anti-AMA1 antibodies mediate protection. Monoclonal antibodies raised against P. falciparum AMA1 and against PK66, the Plasmodium knowlesi homologue of AMA1, inhibit merozoite invasion in vitro (20, 35). Furthermore, passive immunization of AMA1-specific polyclonal antibodies into Plasmodium chabaudi-infected mice prevented lethal parasitemias (2). These protective antibodies react with conformational epitopes stabilized by disulfide bonds, as immunization with the reduced and alkylated AMA1 failed to protect mice against challenge with P. chabaudi (10).
The sequence of AMA1 is relatively conserved among various Plasmodium spp., with the level of amino acid sequence identity exceeding 50% in pairwise comparisons among all known sequences (5, 12, 24, 25, 31, 42). AMA1 lacks the sequence repeats and marked polymorphisms found in other malaria antigens, such as the merozoite surface antigens MSP1 and MSP2 (3). However, some sequence variation, resulting from point mutations, is observed among alleles of AMA1 in P. falciparum (25, 30, 36), P. knowlesi (43), Plasmodium vivax (5), and P. chabaudi (10), and studies with the P. chabaudi-mouse model indicate that this variation is immunologically significant. Mice immunized with AMA1 or receiving passively transferred anti-AMA1 antibodies were not protected from a heterologous strain of P. chabaudi parasites, indicating that the protective antibodies recognized strain-specific epitopes.
Early clinical trials with AMA1 have commenced, and it is important to determine the effect of sequence diversity on the efficacy of the recombinant AMA1 as a vaccine against P. falciparum. In this study, we demonstrate that immunization of rabbits with the refolded P. falciparum AMA1 ectodomain (the vaccine molecule) induces antibodies that inhibit merozoite invasion in vitro. The refolded antigen has also been used to affinity purify AMA1-specific antibodies from the plasma of individuals who have been exposed to chronic malaria infections. These naturally occurring human antibodies were also able to inhibit the invasion of erythrocytes by P. falciparum merozoites.
MATERIALS AND METHODS
Abbreviations.
AMA1, apical membrane antigen 1; AMA1B, apical membrane antigen 1 ectodomain; ABTS, 2,2′-azino-bis(3-ethylbenzthiazoline-6-sulfonic acid); BSA, bovine serum albumin; ELISA, enzyme-linked immunosorbent assay; IFA, immunofluorescence assay; Mr, relative molecular mass; MSP1, merozoite surface protein 1; MSP2, merozoite surface protein 2; MSP3, merozoite surface protein 3; PBS, phosphate-buffered saline; SDS-PAGE, sodium dodecyl sulfate-polyacrylamide gel electrophoresis.
Preparation of recombinant AMA1 ectodomain.
The ectodomain of AMA1 from the 3D7 strain of P. falciparum was expressed in Escherichia coli with an N-terminal hexa-His tag to allow purification by Ni-chelate chromatography. Nucleotide sequences corresponding to the ectodomain (AMA1B) were amplified from genomic 3D7 DNA by using Pfu DNA polymerase and oligonucleotide primers consisting of nucleotides 73 to 91 and 1422 to 1437. The amplified products were digested with BamHI and PstI, purified after agarose gel electrophoresis with the Magic PCR Preps purification system (Promega, Madison, Wis.), ligated into pDS56/RBS11/6xHis (Roche, Basel, Switzerland), and transformed into E. coli strain JPA101. Bacterial colonies containing inserts with the correct AMA1B sequence were identified by sequencing plasmid DNA prepared from individual colonies. (It was subsequently found that the sequence of the selected clone of 3D7 AMA1B differed from the published AMA1 sequence [24] in two sites: nucleotide 362 was changed from A to G [codon change GAA to GGA], resulting in a glycine residue at position 121 in the protein sequence, and nucleotide 1611 was changed from G to A [codon change GAA to AAA], resulting in a substitution of K for E at position 537 in the protein sequence.) Selected colonies were shown to be expressing the AMA1B recombinant protein by reactivity on immunoblots with a pool of plasma derived from adult Papua New Guinean blood donors.
In early studies, a procedure essentially the same as that described for the extraction of P. chabaudi antigen from washed inclusion bodies was used for the purification of P. falciparum 3D7 AMA1B (1). Recently, a modified procedure, which will be described in detail elsewhere (V. Murphy, A. N. Hodder, P. E. Crewther, and R. F. Anders, unpublished data), has been developed, with a significant improvement in the yield of purified refolded protein. In this modified procedure, the induced E. coli cell pellet was solubilized in 6 M guanidine-HCl, pH 8.0, and after clarification by centrifugation, the supernatant was initially incubated in batch mode for 2 h with Ni-nitrilotriacetic acid resin (Qiagen GmbH, Hilden, Germany). The fall-through, containing unbound proteins, including approximately 50% of the expressed AMA1, was incubated overnight with a second batch of Ni-nitrilotriacetic acid resin. After a series of washes (10 column volumes each) with 6 M guanidine-HCl (pH 8.0, 6.3, and 5.9), the bound AMA1 was eluted with 6M guanidine-HCl (pH 4.5) buffer. The protein was then refolded by dilution in a buffer containing 1 mM reduced glutathione and 0.25 mM oxidized glutathione as previously described (2). The refolded protein was purified further by anion-exchange chromatography followed by reversed-phase high-performance liquid chromatography or gel permeation chromatography.
Preparation of rabbit antisera.
Rabbit antisera were raised to recombinant refolded AMA1B or reduced and alkylated AMA1B by immunization with 100 to 200 μg of the antigen emulsified in Montanide ISA720 (SEPPIC, Paris, France). The primary immunization was intramuscular, and subsequent immunizations were subcutaneous. Individual or pooled rabbit sera were heat inactivated at 56°C for 20 min and then sterilized by filtration through a 0.22-μm-pore-size filter.
IgG was affinity purified from pooled rabbit sera using protein G-Sepharose (Pharmacia Biotech, Uppsala, Sweden). Bound IgG was eluted with 0.1 M glycine (pH 2.6), neutralized, and then dialyzed against PBS. The antibody solution was sterilized by passage through a 0.22-μm-pore-size filter, adjusted to 5 mg/ml, and stored at 4°C.
Parasite culture.
Various strains of P. falciparum were cultivated in vitro using erythrocytes of blood group O+ according to the method of Trager and Jensen (39). The parasites were grown in RPMI 1640 supplemented with 25 mM HEPES, 24 mM NaHCO3, 25 mg of gentamycin/ml, 50 mg of hypoxanthine/liter, 0.25% (wt/vol) lipid-rich BSA (AlbuMax II cell culture grade 11021-045; Gibco-BRL, Life Technologies, Auckland, New Zealand), and 5% (vol/vol) heat-inactivated nonimmune human serum from O+ clotted blood (complete medium) at a 4% hematocrit. The origins of the P. falciparum isolates have been described previously (25).
Inhibition of merozoite invasion in vitro.
P. falciparum cultures were synchronized by treatment with sorbitol (23). Late-trophozoite or early-schizont-stage parasites were purified from synchronous cultures by centrifugation on 80-60-50-40% layered Percoll (Pharmacia Biotech) as described by Aley et al. (1). The parasites were diluted with uninfected erythrocytes to give a parasitemia of 2% and a hematocrit of 2% in complete medium unless otherwise specified.
Parasites were aliquoted (180 μl) into sterile flat-bottomed 96-well microtiter plates (Falcon 3072; Becton-Dickson, Lincoln Park, N.J.) to which 20 μl of test antibody was added. Instead of antibody solution, 20 μl. PBS was added to control wells. Cultures were incubated at 37°C in 5% CO2 and 1% O2 in N2. After 24 h, a thin smear was made from each well, fixed in methanol, stained with Giemsa's stain, and examined by oil immersion light microscopy. The number of ring-stage parasites in at least 2,000 erythrocytes was determined and expressed as a percentage. The percentage of inhibition was calculated as follows: [1 − percent parasitemia with test antibodies/percent control parasitemia] × 100%. The mean value of percent inhibition and the standard error of each mean were calculated from triplicate experiments.
Preparation of affinity matrices.
AMA1 ectodomain and BSA were coupled to CNBr-activated Sepharose 4B as recommended by the manufacturer (Pharmacia Biotech), using a ratio of 1 mg of protein to 1 ml of CNBr-activated Sepharose. The remaining active groups on the support were blocked with an excess of Tris-HCl.
Affinity purification of human anti-AMA1 IgG from pooled hyperimmune plasma.
Pooled outdated plasma obtained from the Papua New Guinea Red Cross blood bank was heat inactivated at 56°C for 20 min and then sterilized by passage through a 0.22-μm-pore-size filter. Human IgG from 20 ml of heat-inactivated plasma was purified using protein G Sepharose (Pharmacia Biotech) according to the manufacturer's instructions. The eluted IgG was dialyzed against PBS and then sterilized by passage through a 0.22-μm-pore-size filter.
The IgG preparation was further purified using an AMA1-Sepharose 4B affinity matrix after passage over a BSA-Sepharose 4B column to decrease background binding. The antibodies were eluted at pH 2.6 as described above, neutralized, and exchanged into PBS using PD-10 columns (Pharmacia Biotech). The preparation was concentrated using Centricon-30 concentrators (Amicon, Beverly, Mass.), passaged through a 0.22 μm-pore-size filter, and stored at 4°C.
IFAs.
Synchronized 3D7 schizonts at 4% parasitemia and 4% hematocrit were pelleted from culture and washed three times with RPMI 1640–25 mM HEPES–24 mM NaHCO3 buffer. Thin smears for analysis of parasite morphology were prepared as described elsewhere (4). Thick smears were prepared on 12-well multitest microscope slides (ICN, Aurora, Ohio). The dried smears were fixed in ice-cold acetone for 2 min and then air dried. If they were not used immediately, the acetone-fixed air-dried smears were stored with desiccant at −20°C.
Plasma or affinity-purified antibodies were diluted in a threefold series using 0.5% BSA–PBS as the diluent. Aliquots (20 μl) of the diluted plasma or antibodies were placed in duplicate wells and allowed to incubate for 1 h at room temperature in a humidified atmosphere. Each slide was washed extensively in PBS, and then 20 μl of either sheep anti-rabbit Ig-fluorescein isothiocyanate conjugate (Silenus, Melbourne, Australia) or sheep-anti human Ig-fluorescein isothiocyanate conjugate (Silenus) at 1:200 in 0.5% BSA–PBS was added to each well and left to incubate for 1 h at room temperature in a moist atmosphere. The slides were washed extensively in PBS and allowed to dry shielded from direct light. Vectashield mounting medium (Vector Laboratories, Burlingame, Calif.) was placed under each coverslip to preserve the fluorescence, and the slides were left in an airtight container for 24 h before being examined by fluorescence microscopy.
ELISA procedure.
The titer of anti-AMA1 antibodies was determined by ELISA using microtiter plates (Dynex Technologies Inc., Chantilly, Va.) coated overnight at 4°C with P. falciparum 3D7 AMA1B diluted in PBS (2 μg/ml). After being coated, the plates were blocked by incubation for at least 60 min with 5% (wt/vol) skim milk in PBS, pH 7.3 (BLOTTO). Half-log10 serial dilutions of each serum sample were prepared in duplicate and incubated in the antigen-coated wells for 2 h at room temperature. After being washed (three times with PBS–0.05% [vol/vol] Tween 20 and then two times with water), a 1:1,000 dilution of horseradish peroxidase-conjugated sheep anti-rabbit IgG (Silenus) was added to each well. After a further 2-h incubation at room temperature and washing, bound antibody was visualized by the addition of ABTS substrate solution (1 mM ABTS [Sigma, St. Louis, Mo.] in 0.1 M citrate buffer [pH 4.2] activated with 0.03% [vol/vol] hydrogen peroxide). The absorbance at 414 nm was read 40 min after the addition of substrate. The titration end point was defined as the last dilution with an absorbance of >0.1.
SDS-PAGE and immunoblotting procedures.
Saponin-lysed parasites were solubilized in SDS-PAGE (22) sample buffer with or without β-mercaptoethanol as a reducing agent and then fractionated on 10% polyacrylamide discontinuous gels. Prestained Kaleidoscope molecular weight markers (BioRad, Hercules, Calif.) were used throughout. Proteins were electrophoretically transferred to nitrocellulose (Sartorius, Gottingen, Germany; 0.45-μm pore size) as described by Towbin et al. (38). Immunoblotting was performed using procedures described previously (9). The protein bands on the immunoblots were visualized using a chemiluminescent substrate (Pierce, Rockford, Ill.) according to the manufacturer's instructions.
RESULTS
Recombinant refolded P. falciparum AMA1B induces high-titer antibody responses in rabbits.
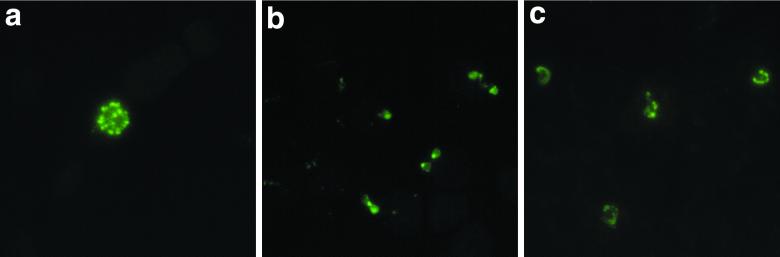
Immunization of rabbits with recombinant P. falciparum AMA1 induced high titers of anti-AMA1 antibodies (Table 1). When measured by ELISA on the immunogen, titers ranged from log10 4.5 to log10 6.0 after the first immunization and log10 6.0 to log10 6.5 after the third immunization. Indirect IFAs showed that these antibodies reacted with AMA1 in P. falciparum-infected erythrocytes, and the IFA titer also increased with the number of immunizations, reaching 1:81,000 to 1:243,000 after the third immunization. The punctate immunofluorescence pattern seen for schizont-stage parasites in the IFAs was consistent with the IF pattern previously reported for AMA1 (4, 26). In addition, the results from IFAs conducted on thin blood smears of asynchronous parasite cultures showed free merozoites with intense apical fluorescence and weaker surface fluorescence (Fig. 1b). Early-ring-stage parasites also fluoresced (Fig. 1c), consistent with other evidence suggesting that AMA1, or a processed form of AMA1, is carried into the erythrocyte with the invading merozoite (27).
TABLE 1.
Serological data for rabbits immunized with P. falciparum 3D7 AMA1B
| Rabbit no. | Bleed | % Inhibition of merozoite invasion (SEM) | Inverse ELISA titer (log10) | IFA titer |
|---|---|---|---|---|
| 3100 | Prebleed | −6.6 (5.9) | <3 | <1:1,000 |
| Post-V1 | 5.0 (2.9) | 4.5 | 1:3,000 | |
| Post-V2 | 15.2 (9.1) | 5.5 | 1:9,000 | |
| Post-V3 | 40.9 (2.9) | 6.0 | 1:243,000 | |
| 3103 | Prebleed | 7.7 (6.7) | <3 | <1:1,000 |
| Post-V1 | 23.6 (2.5) | 6.0 | 1:9,000 | |
| Post-V2 | 47.4 (2.0) | 6.5 | 1:81,000 | |
| Post-V3 | 60.2 (7.2) | 6.5 | 1:243,000 | |
| 3113 | Prebleed | 6.6 (2.1) | <3 | <1:1,000 |
| Post-V1 | 22.7 (8.9) | 5.5 | 1:9,000 | |
| Post-V2 | 40.0 (2.8) | 6.0 | 1:27,000 | |
| Post-V3 | 55.1 (6.3) | 6.5 | 1:81,000 |
FIG. 1.
IFA of the subcellular localization of AMA1 in mature schizonts (a), free merozoites (b), and ring stages (c) of P. falciparum 3D7 with rabbit anti-AMA1 antibodies. Note that control IFAs using antibodies isolated from the same rabbits prior to immunization with AMA1 gave negligible background fluorescence (data not shown).
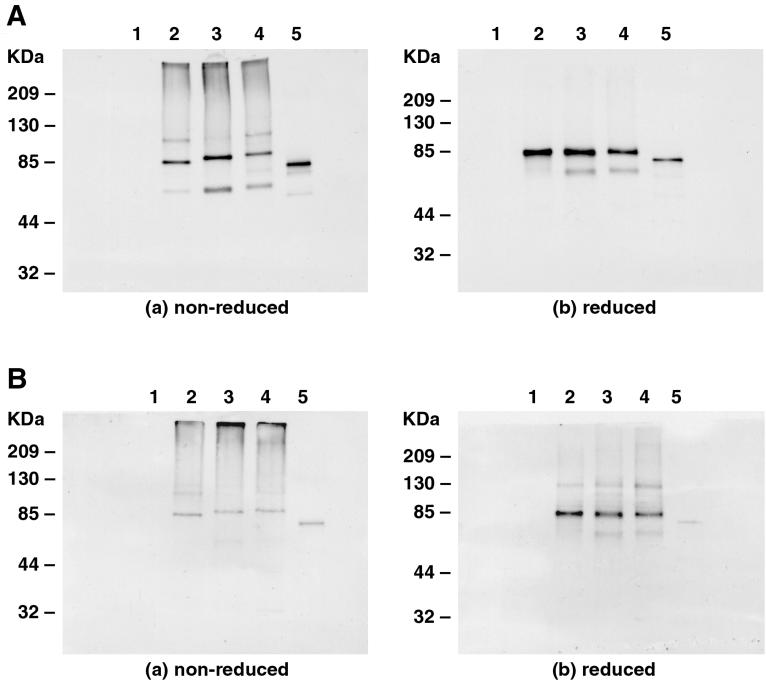
The reactivity of these rabbit anti-AMA1 antibodies with both parasite AMA1 and the recombinant AMA1B was confirmed by immunoblot analysis (Fig. 2A). Antibodies predominantly recognized parasite polypeptides of approximately 83,000 and 66,000 Mr, which are consistent with previously reported values for the full-length and processed forms of AMA1 seen in parasitized erythrocytes (9). In reduced samples, there was no size polymorphism evident for AMA1 in the different parasite lines studied. In contrast, the nonreduced form of 3D7 AMA1 was found to migrate faster than nonreduced forms of D10 and HB3. We attribute this behavior to differences in physicochemical properties among the three folded antigens arising from variation in the surface amino acid substitutions, as the predicted molecular masses of the three antigens are nearly identical. The anti-AMA1 antibodies also reacted with higher-Mr species in the parasite samples prepared in nonreducing sample buffer (Fig. 2A). An antigen of approximately 110,000 Mr was prominent in 3D7 and HB3 parasite extracts but was not seen clearly in D10. The identities of these higher-molecular-weight antigens are unknown, but reactivity with these antigens and the parasite AMA1 polypeptides was removed by absorption with recombinant AMA1 (data not shown).
FIG. 2.
Immunoblots of saponin-lysed parasite extracts electrophoresed under nonreducing (left) and reducing (right) conditions. The immunoblots were probed with either rabbit anti-refolded P. falciparum 3D7 AMA1B antibodies (A) or rabbit anti-reduced and alkylated P. falciparum 3D7 AMA1B antibodies. Lanes 1, saponin-lysed uninfected erythrocytes; lanes 2, saponin-lysed P. falciparum 3D7 schizonts; lanes 3, saponin-lysed P. falciparum D10 schizonts; lanes 4, saponin-lysed P. falciparum HB3 schizonts; lanes 5, recombinant P. falciparum 3D7 AMA1B.
The antibodies raised to the refolded recombinant AMA1 ectodomain reacted strongly in immunoblots with recombinant AMA1 electrophoresed under reducing and nonreducing conditions (Fig. 2A). Although these antibodies were raised to an antigen that was refolded by in vitro methods, the existence of some incompletely folded conformers may have resulted in the generation of antibodies to linear epitopes. Alternatively, limited refolding of the reduced antigen during SDS-PAGE and the immunoblotting procedure may reconstitute reactivity with conformation-dependent antibodies.
Rabbit antibodies to the reduced and alkylated AMA1 reacted poorly with the nonreduced samples of parasite AMA1 from different strains and the refolded recombinant AMA1 but reacted strongly with the equivalent samples electrophoresed in reducing sample buffer (Fig. 2B). This observation indicates that these antibodies are targeted predominantly toward linear epitopes that are not available in the refolded recombinant AMA1 or the native, parasite-derived AMA1 due to conformational restraints imposed by disulfide bonds.
Rabbit anti-AMA1 total IgG inhibits P. falciparum invasion of erythrocytes.
Initially, the ability of anti-AMA1 antibodies to block merozoite invasion in vitro was examined by supplementing culture medium with 10% rabbit serum. In these experiments, sera from all three rabbits immunized with refolded recombinant AMA1 inhibited merozoite invasion. The level of inhibitory activity in the rabbit sera increased with the number of immunizations, in parallel with the increase in titer of anti-AMA1 antibodies as determined by ELISA and IFA (Table 1).
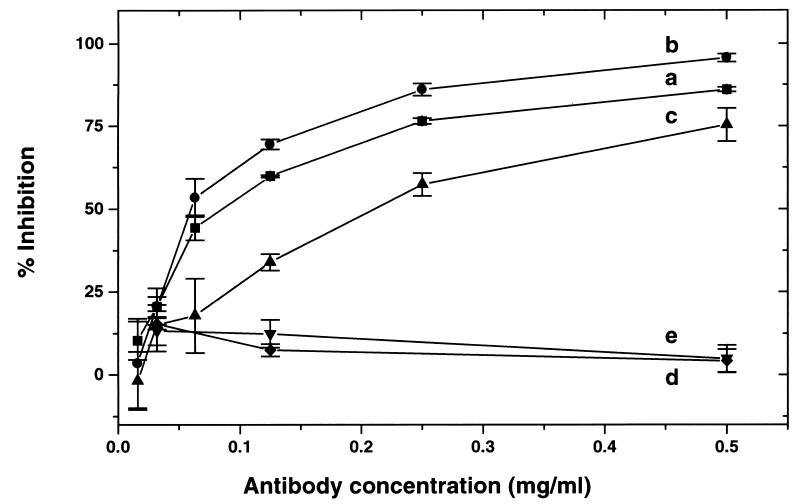
More-detailed investigations of the inhibitory activity of rabbit anti-AMA1 antibodies were carried out with IgG fractions isolated on protein G-Sepharose. Invasion of erythrocytes by merozoites from various strains of P. falciparum was inhibited in a concentration-dependent manner by IgG isolated from the sera of rabbits immunized with the refolded recombinant P. falciparum 3D7 AMA1B (Fig. 3, plots a, b, and c). The antibodies inhibited invasion by the homologous 3D7 line as well as two heterologous parasite lines (D10 and HB3). The lowest inhibition was observed for HB3, and of the two heterologous lines, the HB3 AMA1 sequence is the more distantly related to 3D7 AMA1. Unexpectedly, the degree of inhibition with D10 was greater than that observed with the homologous 3D7 parasite line. This has been a consistent observation in several experiments using total IgG from rabbits immunized with the refolded AMA1 ectodomain. Control IgG preparations from rabbits that were immunized with the reduced and alkylated AMA1, and from nonimmunized rabbits, were not inhibitory (Fig. 3, plots d and e).
FIG. 3.
Inhibition of merozoite invasion by rabbit anti-AMA1 antibodies (3D7 [plot a], D10 [plot b], and HB3 [plot c]). The effects on 3D7 of two control sera, rabbit anti-reduced and alkylated P. falciparum 3D7 AMA1B antibodies (plot d) and rabbit antibodies from a pool of prebleeds (plot e), are also shown. The data represent the means and standard errors of the mean for triplicate assays.
Human AMA1-specific IgG inhibits P. falciparum invasion of erythrocytes.
Anti-AMA1 antibodies are found at high titer in the plasma or serum of individuals living in areas where malaria is endemic (37). Human anti-AMA1 antibodies were affinity purified from a pool of plasma obtained from Papua New Guinean blood donors who had previously been found to have high titers of antibodies to a variety of P. falciparum asexual blood-stage antigens. Quantitation of antibodies by ELISA with P. falciparum 3D7 AMA1 as the adsorbent showed that >99% of the anti-AMA1 antibodies were depleted from the pool by three passages over the immunosorbent and the majority of AMA1-specific antibodies were recovered in the combined eluates (data not shown).
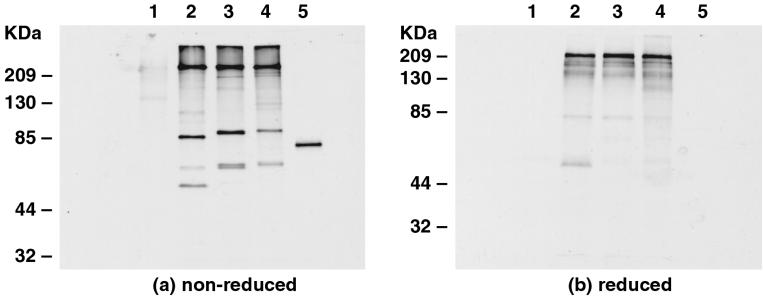
The affinity-purified human anti-AMA1 antibodies reacted in immunoblots with the parasite AMA1 from each P. falciparum line and the recombinant refolded P. falciparum 3D7 AMA1 ectodomain when these antigens were electrophoresed in the presence of nonreducing sample buffer. In contrast, these antibodies reacted poorly with the reduced forms of the proteins (Fig. 4). Hence, the refolded AMA1 ectodomain used for the production of the immunoadsorbent has allowed purification of antibodies that predominantly recognize AMA1 epitopes stabilized by disulfide bonds. The affinity-purified anti-AMA1 IgG also cross-reacted with some protein species having much higher relative molecular weights than those expected for AMA1 in both nonreduced and reduced sample buffer (Fig. 4). Because only a faint reactivity is observed for a similar loading of proteins derived from saponin-lysed uninfected human erythrocytes, it seems likely that the cross-reactivity is due to related parasite antigens or complexes containing AMA1.
FIG. 4.
Immunoblots of saponin-lysed parasite extracts electrophoresed under nonreducing (left) or reducing (right) conditions. The immunoblots were probed with human anti-AMA1B affinity-purified antibodies. See the legend to Fig. 2 for further details.
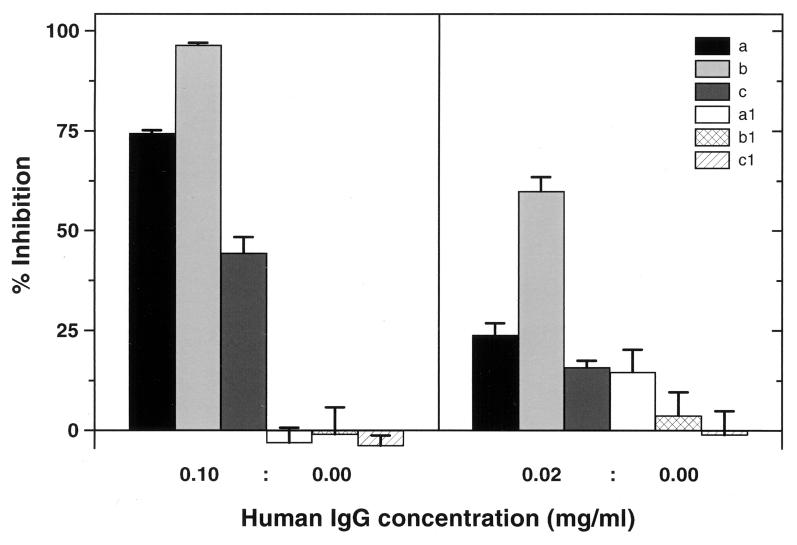
When tested in the in vitro merozoite invasion assay, the affinity-purified human anti-AMA1 antibodies inhibited the various strains of P. falciparum in a manner similar to that observed for rabbit IgG raised to the refolded P. falciparum 3D7 AMA1 ectodomain (Fig. 5). The inhibitory effect was dose dependent and strain specific, with HB3 the least inhibited, whereas as seen with the rabbit antibodies, D10 was more inhibited than the homologous 3D7 strain. At 20 μg/ml, little inhibition of merozoite invasion was observed for 3D7 and HB3, whereas at this low concentration of antibodies, D10 was still inhibited by more than 50%.
FIG. 5.
Inhibition of merozoite invasion by human anti-AMA1 antibodies (a, 3D7; b, D10; and c, HB3). In control experiments (a1, b1, and c1) PBS rather than affinity-purified IgG was added to the cultures. The data represent the means and standard errors of the mean for triplicate assays. The affinity-purified anti-AMA1 antibodies corresponded to ∼0.5% of the total IgG obtained from the pooled sera. In hyperimmune individuals, whose total IgG is estimated to be approximately 20 mg/ml, this would correspond to a physiological anti-AMA1 antibody concentration of 100 μg/ml. See Materials and Methods for further details.
DISCUSSION
AMA1 is regarded as a likely component of a malaria vaccine targeting the asexual blood stages of P. falciparum. This antigen is located on the surfaces of merozoites (27) and is relatively conserved compared to MSP1 and MSP2, two other vaccine candidates found in this location. AMA1 lacks the variable repeat sequences found in many malarial proteins, but numerous amino acid substitutions are present in P. falciparum AMA1. The distribution and nature of these amino acid substitutions is consistent with selection by protective immune responses (10). Since AMA1 is currently undergoing the first phase of evaluation in clinical trials, it is important to assess whether one form of the antigen can protect against lines of P. falciparum expressing antigenically diverse forms of AMA1. As part of this assessment, we have used inhibition of merozoite invasion in vitro to examine the anti-parasitic specificities of anti-AMA1 antibodies.
Two types of anti-AMA1 antibodies have been used in these studies: (i) antibodies produced by immunizing rabbits with the vaccine being used in clinical trials (P. falciparum 3D7 AMA1B emulsified in Montanide ISA720) and (ii) antibodies affinity purified from the plasma of hyperimmune individuals living in a region of Papua New Guinea where malaria is endemic. In immunofluorescence assays, both types of antibodies gave the punctate fluorescence pattern on mature schizonts typical of AMA1 and other antigens located in the rhoptries (27). Both reagents stained the surfaces of merozoites with apical intensity, but the rabbit antibodies reacted more strongly with ring stages. Thus, there appear to be different anti-AMA1 specificities in the two polyclonal anti-AMA1 reagents. On immunoblots, rabbit and human anti-AMA1 antibodies reacted strongly with both parasite-derived full-length and processed forms of AMA1 and the recombinant antigen when these proteins were electrophoresed under nonreducing conditions. In contrast, the rabbit antibodies, but not the affinity-purified human antibodies, reacted strongly on immunoblots with AMA1 electrophoresed under reducing conditions, providing further evidence of a difference in fine specificity. The human antibodies reacted preferentially with conformational epitopes stabilized by disulfide bonds.
The rabbit, but more particularly the affinity-purified human, anti-AMA1 antibodies reacted on immunoblots with some higher-molecular-weight proteins in infected erythrocytes. It appears that at least some of these high-molecular-weight species were disulfide-bonded protein complexes, as they were not seen by the rabbit antibodies when samples were electrophoresed under reducing conditions. The detection of these high-molecular-weight species by anti-AMA1 antibodies may result from the presence of AMA1 in natural protein complexes, or it may reflect the presence of cross-reacting epitopes in other P. falciparum antigens, e.g., MAEBL (19). We cannot exclude the possibility that cross-reactions with these other antigens contributes to the inhibition seen in the merozoite invasion assay.
Both the rabbit and the affinity-purified human anti-AMA1 antibodies inhibited merozoite invasion of erythrocytes. Several lines of evidence support our conclusion that the inhibition seen in merozoite invasion assays was due to anti-AMA1 antibodies. First, the level of inhibitory activity in rabbit sera increased with the number of immunizations. Second, the inhibitory activity paralleled the antibody titers determined by ELISA on recombinant AMA1 and by IFA on infected erythrocytes. Third, inhibition was obtained with rabbit sera, rabbit IgG isolated on protein G-Sepharose, and affinity-purified human anti-AMA1 antibodies. Furthermore, IgG isolated from the sera of rabbits immunized with reduced and alkylated AMA1 ectodomain, formulated in the same adjuvant, did not inhibit merozoite invasion. This indication that the inhibitory antibodies react predominantly with conformational epitopes stabilized by disulfide bonds is consistent with the observation that mice immunized with the refolded but not the reduced and alkylated P. chabaudi AMA1 ectodomain were protected from parasite challenge (2).
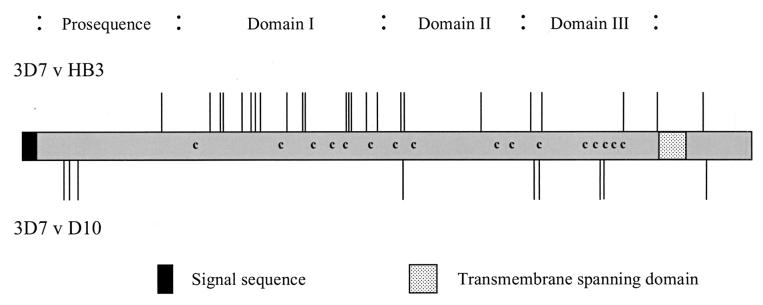
Rabbit and human anti-AMA1 antibodies inhibited the invasion of human erythrocytes by merozoites from both the homologous 3D7 strain and the heterologous D10 and HB3 strains of P. falciparum, in a dose-dependent manner. Thus, some of the inhibitory antibodies in these polyclonal reagents recognize conserved epitopes in the AMA1 ectodomain. This is consistent with the observation that inhibitory rat monoclonal antibodies recognize AMA1 epitopes found in all P. falciparum isolates examined and which are conserved in Plasmodium reichenowi (20, 21). However, HB3, one of the two heterologous parasite lines studied, was markedly less inhibited than was the homologous 3D7 line or D10, the other heterologous line. Although all P. falciparum AMA1 sequences are closely related (>95% identity), of the AMA1 alleles sequenced, HB3 is one of the most distant from the 3D7 sequence, with 23 amino acid differences in the ectodomain (Fig. 6). In contrast, only eight amino acid differences distinguish the 3D7 and D10 sequences (Fig. 6). The majority of the amino acid differences between 3D7 and HB3 (16 of 23) are located between the first and sixth conserved cysteine residues. In contrast, the 3D7 and D10 sequences are identical in this region of AMA1, which falls within the putative domain I (16). The total alignment of AMA1 sequences shows domain I to be the most diverse region of the molecule (25), and the relative inhibitions of the three lines of P. falciparum observed in this study indicate that many of the inhibitory antibodies recognize strain-specific epitopes in this region of AMA1.
FIG. 6.
Schematic showing the locations of amino acid differences between 3D7 and two other lines of P. falciparum. The AMA1 sequence for D10 differs from 3D7 by 9 amino acids, while the AMA1 sequence for HB3 differs by 24 amino acids. The domain structure for AMA1 is based on the disulfide bond pattern determined by Hodder et al. (16).
Unexpectedly, in several independent experiments, the degree of inhibition with D10, one of the heterologous lines studied, was greater than that seen with the homologous 3D7 parasite line. Of the eight amino acid differences between the AMA1 sequences of 3D7 and D10, three are found in the prosequence, one is found in domain II, and four are found in domain III. It is not obvious how these differences in the AMA1 sequences could explain an increased level of inhibition of the heterologous parasite line, and it is possible that some aspect of parasite biology that differs between the 3D7 and D10 lines (e.g., cytoadherence phenotype or invasion pathway) is modulating the inhibitory activity of the AMA1 antibodies.
Analysis of the pattern of mutations in AMA1 has led to the conclusion that at least some of the sequence diversity has arisen as a result of positive selection (10, 18, 40, 41). The present study, which has demonstrated that inhibitory rabbit and naturally occurring human anti-AMA1 antibodies recognize both strain-specific and conserved epitopes, provides strong evidence in support of the conclusion that AMA1 is a natural target of protective antibody responses.
In summary, this study has demonstrated that antibodies to one form of AMA1 are capable of inhibiting the invasion of erythrocytes by merozoites from three lines of P. falciparum expressing different forms of AMA1. Although clinical evaluation of the construct (AMA1B) used in these studies will continue, the results reported here indicate that an AMA1 construct lacking the most variable domain, domain I, may help to direct the immune response to a region(s) of the molecule that contains conserved epitopes found in all strains of P. falciparum.
ACKNOWLEDGMENTS
This work was supported by the Cooperative Research Center for Vaccine Technology, the UNDP-World Bank-WHO Special Program for Research and Training in Tropical Diseases, and the National Health and Medical Research Council (Australia).
REFERENCES
- 1.Aley S B, Sherwood J A, Marsh K, Eidelman O, Howard R J. Identification of isolate-specific proteins on sorbitol-enriched Plasmodium falciparum infected erythrocytes from Gambian patients. Parasitology. 1986;92:511–525. doi: 10.1017/s0031182000065410. [DOI] [PubMed] [Google Scholar]
- 2.Anders R F, Crewther P E, Edwards S, Margetts M, Matthew M L S M, Pollock B, Pye D. Immunization with recombinant AMA1 protects mice against infection with Plasmodium chabaudi. Vaccine. 1998;16:240–247. doi: 10.1016/s0264-410x(97)88331-4. [DOI] [PubMed] [Google Scholar]
- 3.Anders R F, Smythe J A. Polymorphic antigens in Plasmodium falciparum. Blood. 1989;74:1865–1875. [PubMed] [Google Scholar]
- 4.Bianco A E, Crewther P E, Coppel R L, Stahl H D, Kemp D J, Anders R F, Brown G V. Patterns of antigen expression in asexual blood stages and gametocytes of Plasmodium falciparum. Am J Trop Med Hyg. 1988;38:258–267. doi: 10.4269/ajtmh.1988.38.258. [DOI] [PubMed] [Google Scholar]
- 5.Cheng Q, Saul A. Sequence analysis of the apical membrane antigen 1 (AMA1) of Plasmodium vivax. Mol Biochem Parasitol. 1994;65:183–187. doi: 10.1016/0166-6851(94)90127-9. [DOI] [PubMed] [Google Scholar]
- 6.Cohen S, McGregor I A, Carrington S. Gamma-globulin and acquired immunity to human malaria. Nature. 1961;192:733–737. doi: 10.1038/192733a0. [DOI] [PubMed] [Google Scholar]
- 7.Cohen S, Butcher G A. Properties of protective malarial antibody. Immunology. 1970;19:369–383. [PMC free article] [PubMed] [Google Scholar]
- 8.Collins W E, Pye D, Crewther P E, Vandenberg K L, Galland G G, Sulzer A J, Kemp D L, Edwards S J, Coppel R L, Sullivan J S, Morris C L, Anders R F. Protective immunity induced in squirrel monkeys with recombinant apical membrane antigen 1 of Plasmodium fragile. Am J Trop Med Hyg. 1994;51:711–719. doi: 10.4269/ajtmh.1994.51.711. [DOI] [PubMed] [Google Scholar]
- 9.Crewther P E, Culvenor J G, Silva A, Cooper J A, Anders R F. Plasmodium falciparum: two antigens of similar size are located in different compartments of the rhoptry. Exp Parasitol. 1990;70:193–206. doi: 10.1016/0014-4894(90)90100-q. [DOI] [PubMed] [Google Scholar]
- 10.Crewther P E, Matthew M L S M, Flegg R H, Anders R F. Protective immune responses to apical membrane antigen 1 of Plasmodium chabaudi involve recognition of strain-specific epitopes. Infect Immun. 1996;64:3310–3317. doi: 10.1128/iai.64.8.3310-3317.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deans J A, Knight A M, Jean W C, Waters A P, Cohen S, Mitchell G H. Vaccination of rhesus monkeys with a minor, invariant, Plasmodium knowlesi 66 kDa merozoite antigen. Parasite Immunol. 1988;10:535–552. doi: 10.1111/j.1365-3024.1988.tb00241.x. [DOI] [PubMed] [Google Scholar]
- 12.Dutta S, Malhotra P, Chauhan V S. Sequence analysis of apical membrane antigen 1 (AMA1) of Plasmodium cynomolgii bastianelli. Mol Biochem Parasitol. 1995;73:267–270. doi: 10.1016/0166-6851(95)00112-e. [DOI] [PubMed] [Google Scholar]
- 13.Egan A F, Burghaus P, Druilhe P, Holder A A, Riley E M. Human antibodies to the 19 kDa C-terminal fragment of Plasmodium falciparum merozoite surface protein 1 inhibit parasite growth in vitro. Parasite Immunol. 1999;21:133–139. doi: 10.1046/j.1365-3024.1999.00209.x. [DOI] [PubMed] [Google Scholar]
- 14.Good M F, Kaslow D C, Miller L H. Pathways and strategies for developing a malaria blood-stage vaccine. Annu Rev Immunol. 1998;16:57–87. doi: 10.1146/annurev.immunol.16.1.57. [DOI] [PubMed] [Google Scholar]
- 15.Harnyuttanakorn P, McBride J S, Donachie S, Heidrich H-G, Ridley R G. Inhibitory monoclonal antibodies recognize epitopes adjacent to a proteolytic cleavage site on the RAP1 protein of Plasmodium falciparum. Mol Biochem Parasitol. 1992;55:177–186. doi: 10.1016/0166-6851(92)90138-a. [DOI] [PubMed] [Google Scholar]
- 16.Hodder A N, Crewther P E, Matthew M L S M, Reid G E, Moritz R L, Simpson R J, Anders R F. The disulfide bond structure of Plasmodium apical membrane antigen 1. J Biol Chem. 1996;271:29446–29452. doi: 10.1074/jbc.271.46.29446. [DOI] [PubMed] [Google Scholar]
- 17.Holder A A. Malaria vaccines. Proc Natl Acad Sci USA. 1999;96:1167–1169. doi: 10.1073/pnas.96.4.1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hughes M K, Hughes A L. Natural selection on Plasmodium surface proteins. Mol Biochem Parasitol. 1995;71:99–113. doi: 10.1016/0166-6851(95)00037-2. [DOI] [PubMed] [Google Scholar]
- 19.Kappe S H I, Noe A R, Fraser T S, Blair P L, Adams J H. A family of chimeric erythrocyte binding proteins of malaria parasites. Proc Natl Acad Sci USA. 1998;95:1230–1235. doi: 10.1073/pnas.95.3.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kochen C H M, van der Wel A M, Dubbeld A, Narum D L, van de Rijke F M, van Gemert G-J, van der Linde X, Bannister L H, Janse C, Waters A P, Thomas A W. Precise timing of expression of a Plasmodium falciparum-derived transgene in Plasmodium berghei is a critical determinant of subsequent subcellular localization. J Biol Chem. 1998;273:15119–15124. doi: 10.1074/jbc.273.24.15119. [DOI] [PubMed] [Google Scholar]
- 21.Kocken C H M, Narum D L, Massougbodji A, Ayivi B, Dubbeld M A, van der Wel A M, Conway D J, Sanni A, Thomas A W. Molecular characterization of Plasmodium reichenowi apical membrane antigen-1 (AMA-1), comparison with P. falciparum AMA-1, and antibody-mediated inhibition of red cell invasion. Mol Biochem Parasitol. 2000;109:147–156. doi: 10.1016/s0166-6851(00)00250-4. [DOI] [PubMed] [Google Scholar]
- 22.Laemmli U K. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970;277:680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- 23.Lambros C, Vanderberg J P. Synchronization of Plasmodium falciparum erythrocyte stages in culture. J Parasitol. 1979;65:418–420. [PubMed] [Google Scholar]
- 24.Marshall V M, Peterson M G, Lew A M, Kemp D J. Structure of the apical membrane antigen 1 (AMA1) of Plasmodium chabaudi. Mol Biochem Parasitol. 1989;37:281–283. doi: 10.1016/0166-6851(89)90160-6. [DOI] [PubMed] [Google Scholar]
- 25.Marshall, V. M., L.-X. Zhang, R. F. Anders, and R. L. Coppel. Diversity of the vaccine candidate AMA1 of Plasmodium falciparum. Mol. Biochem. Parasitol. 77:109–113. [DOI] [PubMed]
- 26.Miller L H, Hoffman S L. Research toward vaccines against malaria. Nat Med. 1998;4:520–524. doi: 10.1038/nm0598supp-520. [DOI] [PubMed] [Google Scholar]
- 27.Narum D L, Thomas A W. Differential localization of the full-length and processed forms of PF83/AMA-1 an apical membrane antigen of Plasmodium falciparum merozoites. Mol Biochem Parasitol. 1994;67:59–68. doi: 10.1016/0166-6851(94)90096-5. [DOI] [PubMed] [Google Scholar]
- 28.Oeuvre C, Bouharoun-Tayoun H, Gras-Masse H, Bottius E, Kaidoh T, Aikawa M, Filgueira M-C, Tartar A, Druilhe P. Merozoite surface protein-3: a malaria protein inducing antibodies that promote Plasmodium falciparum killing by cooperation with blood monocytes. Blood. 1994;84:1594–1602. [PubMed] [Google Scholar]
- 29.Pang X-L, Mitamura T, Horii T. Antibodies reactive with the N-terminal domain of Plasmodium falciparum serine repeat antigen inhibit cell proliferation by agglutinating merozoites and schizonts. Infect Immun. 1998;67:1821–1827. doi: 10.1128/iai.67.4.1821-1827.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peterson M G, Marshall V M, Smythe J A, Crewther P E, Lew A, Silva A, Anders R F, Kemp D J. Integral membrane protein located in the apical complex of Plasmodium falciparum. Mol Cell Biol. 1989;9:3151–3154. doi: 10.1128/mcb.9.7.3151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peterson M G, Nguyen-Dinh P, Marshall V M, Elliott J F, Collins W E, Anders R F, Kemp D J. Apical membrane antigen of Plasmodium fragile. Mol Biochem Parasitol. 1990;39:279–283. doi: 10.1016/0166-6851(90)90067-v. [DOI] [PubMed] [Google Scholar]
- 32.Sabchareon A, Burnouf T, Ouattara D, Attanth P, Bouharoun-Tayoun H, Chantavanich P, Foucault C, Chongsuphajaisiddhi T, Druilhe P. Parasitologic and clinical human response to immunoglobin administration in falciparum malaria. Am J Trop Med Hyg. 1991;45:297–308. doi: 10.4269/ajtmh.1991.45.297. [DOI] [PubMed] [Google Scholar]
- 33.Siddique A B, Iqbal J, Ahlborg N, Wahlin Flyg B, Perlmann P, Berzins K. Antibodies to nonrepeat sequences of antigen Pf155/RESA of Plasmodium falciparum inhibit parasite growth in vitro. Parasitol Res. 1998;84:485–491. doi: 10.1007/s004360050434. [DOI] [PubMed] [Google Scholar]
- 34.Theisen M, Soe S, Oeuvray C, Thomas A W, Vuust J, Danielsen S, Jepsen S, Druilhe P. The glutamate-rich protein (GLURP) of Plasmodium falciparum is a target for antibody-dependent monocyte-mediated inhibition of parasite growth in vitro. Infect Immun. 1998;66:11–17. doi: 10.1128/iai.66.1.11-17.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thomas A W, Deans J A, Mitchell G H, Alderson T, Cohen S. The Fab fragments of monoclonal IgG to a merozoite surface antigen inhibit Plasmodium knowlesi invasion of erythrocytes. Mol Biochem Parasitol. 1984;13:187–199. doi: 10.1016/0166-6851(84)90112-9. [DOI] [PubMed] [Google Scholar]
- 36.Thomas A W, Waters A P, Carr D. Analysis of variation in Pf83, an erythorcyte merozoite vaccine candidate antigen of Plasmodium falciparum. Mol Biochem Parasitol. 1990;42:285–288. doi: 10.1016/0166-6851(90)90172-i. [DOI] [PubMed] [Google Scholar]
- 37.Thomas A W, Trape J-F, Rogier C, Goncalves A, Rosario V E, Narum D L. High prevalence of natural antibodies against Plasmodium falciparum 83-kilodalton apical membrane antigen (PF83/AMA-1) as detected by capture-enzyme-linked immunoadsorbent assay using full-length baculovirus recombinant PF83/AMA-1. Am J Trop Med Hyg. 1994;51:730–740. doi: 10.4269/ajtmh.1994.51.730. [DOI] [PubMed] [Google Scholar]
- 38.Towbin H, Staehelin T, Gordon J. Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets. Procedure and some applications. Proc Natl Acad Sci USA. 1979;76:4350–4354. doi: 10.1073/pnas.76.9.4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Trager W, Jensen J B. Human malaria parasites in continuous cultures. Science. 1976;193:673–675. doi: 10.1126/science.781840. [DOI] [PubMed] [Google Scholar]
- 40.Verra F, Hughes A L. Natural selection on apical membrane antigen-1 of Plasmodium falciparum. Parasitologia. 1999;41:93–95. [PubMed] [Google Scholar]
- 41.Verra F, Hughes A L. Evidence for ancient balanced polymorphism at the apical membrane antigen (AMA-1) locus of Plasmodium falciparum. Mol Biochem Parasitol. 2000;105:149–153. doi: 10.1016/s0166-6851(99)00162-0. [DOI] [PubMed] [Google Scholar]
- 42.Waters A P, Thomas A W, Deans J A, Mitchell G H, Hudson D E, Miller L H, McCutchan T F, Cohen S. A merozoite receptor protein from Plasmodium knowlesi is highly conserved and distributed throughout Plasmodium. J Biol Chem. 1990;265:17974–17979. [PubMed] [Google Scholar]
- 43.Waters A P, Thomas A W, Mitchell G H, McCutchan T F. Intra-generic conservation and limited inter-strain variation in a protective minor surface antigen of Plasmodium knowlesi merozoites. Mol Biochem Parasitol. 1991;44:141–144. doi: 10.1016/0166-6851(91)90230-4. [DOI] [PubMed] [Google Scholar]