Abstract
Objectives:
As of 2016, 1.4 million people in the United States were identified as transgender. Transgender people face health disparities and may be at high risk for cardiovascular disease (CVD). The objective of this study was to examine the odds of CVD for those who report a transgender identity compared with cisgender.
Methods:
We used logistic regression to examine whether transgender identity was associated with CVD after accounting for factors commonly associated with CVD. Data were obtained from the Behavioral Risk Factor Surveillance Survey for the years 2015 through 2019.
Results:
Of the participants, 93.1% reported no CVD and 6.9% reported CVD. For participants with female sex recorded at birth, those identifying as transgender had 2.66 times higher odds of CVD (95% confidence interval [CI]: 1.60–4.41) than those identifying as cisgender. For participants with male sex recorded at birth, the odds of CVD were not statistically significantly different for transgender identity compared with cisgender identity; however, those who were gender nonconforming had 2.21 times higher odds of CVD (95% CI: 1.04–4.70) compared with those with cisgender identity. Additional significant predictors of CVD were age, race, body mass index, alcohol consumption, exercise, and smoking status.
Conclusion:
Participants who were female sex recorded at birth had statistically significant increased odds of CVD for those reporting transgender identity compared with cisgender identity. However, transgender identity did not change the odds of CVD compared with cisgender identity for participants who were male sex recorded at birth.
Keywords: cardiovascular disease, cisgender, health disparities, transgender
Introduction
Sex and gender—although often used interchangeably—are two distinct terms. Sex—male, female, or intersex—is reported at birth based on genitalia.1 Gender, typically referring to a person's gender identity, refers to the internal sense of self—which is most commonly classified as woman, man, gender nonconforming (GNC), gender nonbinary, gender androgynous, or many others.1 For many people, their sex recorded at birth is in accordance with their gender identity (cisgender). However, the term transgender, or trans, refers to individuals whose gender identity is different from their recorded sex at birth.2 As of 2016, ∼0.6% of the population in the United States, 1.4 million adults, identify themselves as transgender.3,4 Although identifying as transgender does not necessarily indicate a person will alter their physical body (e.g., vocal surgery to alter the voice, body contouring procedures to alter body shape), recent data show that 80% of transgender people have either utilized or have plans to take gender-affirming hormone therapy.5
One of the most pervasive barriers faced by transgender people is in seeking and accessing culturally competent medical care.6–8 Evidence shows that many who identify as transgender avoid seeking medical treatment out of fear of discrimination or lack of culturally competent knowledge by their providers.8 As a result, the transgender population faces a higher burden of disease owing to increased rates of depression, suicide, sexually transmitted infections, chronic disease, disabilities, and some cancers compared with the general population.9,10 There is also an elevated risk of cardiovascular disease (CVD) and CVD risk factors among transgender individuals—however, this relationship has not yet been widely studied.6
A report based on data from the transgender discrimination survey showed high rates of HIV infection, alcohol use, smoking, postponing medical care, and being refused medical care in transgender people.11 Another reported that transgender men and women have a higher risk of heart attack—up to more than four times in some cases—than do people who identify as cisgender.6 Even after adjusting for CVD risk factors such as age, high blood pressure, diabetes, and exercise habits, researchers found that transgender men (female sex recorded at birth but identify as men) had more than four times the rate of heart attack as cisgender women (female sex recorded at birth and identify as women).6 Transgender men also had more than twice the rate of a heart attack as cisgender men (recorded male sex at birth and identify as men).6
Although this body of evidence is still growing, one researcher identified this elevated risk in CVD among individuals in the transgender population could be owing to the hormone therapy that patients take for masculinization or feminization.12 However, this relationship between endogenous sex hormones and heart disease is very complex: for transgender women, there appeared to be an increased risk for CVD events because of hormone therapy, whereas data for transgender men are unclear.12 Previous literature corroborates that estrogen therapy for transgender women increases the risk of deep venous thrombosis, or blood clotting, more than estrogen therapy increases the risk in cisgender women.12 A 2018 cohort study examined the relationship between hormone use and venous thromboembolism (VTE), ischemic stroke, and myocardial infarction in transgender persons, and found that rates of VTE and ischemic stroke among transgender women surpassed the increased risk in cisgender women who used estrogen therapy.13 Transgender women had more than a twofold increased rate of VTE compared with cisgender women, but rates were not significantly different compared with cisgender men.5
Other studies cite gender-affirming hormone therapy as the culprit of potentially worsening CVD risk factors such as elevated blood pressure, insulin resistance, and lipid derangements—especially for transgender women.14 However the paucity of prospective cohort studies limits any true knowledge of the associations between cross-sex hormone therapy and CVD.
There are potential biological pathways relating sex recorded at birth (i.e., male or female) and autonomic functioning, which underpins gender as a social determinant for cardiovascular health.15 The idea that CVD health trajectories differ by biological sex often conflates sex and gender. This contributes to the idea that these are consistent among all individuals—when in reality, gender is socially produced.15 Gender guides one's cognition to adopt certain norms, roles, behaviors, and social relations, and is a fluid construct that can vary across one's lifetime depending on the person, place, or life stage. For example, excessive alcohol consumption is a known risk factor for CVD.16 Thus, the socialization of boys as teenagers that discourages expressing emotions and promotes antisocial behaviors to cope—such as drinking—shapes CVD health from a young age.15 These odds of CVD are even worse for those who identify as transgender, because they face social discrimination and limited access to health care as well.17 It is paramount for clinicians, researchers, and policymakers to continue seeking better methods for detecting and preventing CVD early in transgender patients, address the barriers in access to care, and improve care coordination and cultural competency for the transgender community.9
The aims of this study were to (1) compare the odds of CVD between transgender and cisgender participants, controlling for important demographic and behavioral covariates; and (2) discuss systemic causes for this health disparity and areas for future research.
Methods
The Behavioral Risk Factor Surveillance System (BRFSS) survey instrument has included survey items about sexual and gender minorities since 2014. Using data from 2015 to 2019, we evaluated the association between identifying as transgender and reporting a history of myocardial infarction or CVD. BRFSS 2014 data were not included because the CVD question changed between the 2014 and 2015 survey administrations. We built a logistic regression model to study the association between CVD and transgender identity, and adjusted for sociodemographic and CVD health behavior risk factors including age, sex recorded at birth, educational attainment, smoking, alcohol use, smoking status, body mass index (BMI), and exercise.
Study population and sampling procedure
BRFSS is a survey of U.S. adults conducted monthly using random sampling by the state health departments and Centers for Disease Control and Prevention (CDC). CDC began this survey to collect prevalence data on risk behaviors and health practices that can affect an individual's health status. Participants for this study were an aggregated composition of respondents from the BRFSS survey from 2015 (n=441,456), 2016 (n=486,303), 2017 (n=450,016), 2018 (n=437,437), and 2019 (n=418,268). Of the 2,233,479 observations, 913,154 had complete data for all the variables of interest. Of the complete cases, 908,709 reported being cisgender (99.5%), 3428 reported being transgender (0.4%), and 1017 reported being GNC (0.1%). No human subjects approval was needed; the data were publicly available.
Measures of interest
The outcome variable of interest was CVD comparing those who reported having ever had coronary heart disease or myocardial infarction with those who reported not having heart disease or myocardial infarction. The other variable of interest was the transgender identity variable. Participants answered the question, “Do you consider yourself to be transgender?” and could answer: (1) yes, male-to-female (MTF), (2) yes, female-to-male (FTM), (3) yes, gender nonconforming (GNC), or (4) no, cisgender. We collapsed the gender identity variable into three categories: transgender, GNC, and cisgender.
We controlled for other demographic covariates (sex recorded at birth, education level, BMI, race, and age), as well as other related health behaviors—such as exercise (measured by answering “Yes” to the question of “Have you exercised any in the past month?”), alcohol use (number of days drinking alcohol in the last 30 days), and smoking status (ever or never). The question for obtaining participant sex changed during the period of interest. In 2015, the instructions for the interviewer were, “Indicate sex of respondent. Ask only if necessary.”18 In 2016 and 2017 the question was: “Are you …1=Male, 2=Female, 9=Refused.”19,20 In 2018, the question had two formats: “Format 1: What is your sex?” and “Format 2: What was your sex at birth?” with the instruction that “States may adopt one of the two formats of the question. If second format is used, read options.”21 Finally, in 2019, it was “What was your sex at birth? Was it male or female?”22
Because years 2015–2018 were unclear in asking for current sex or sex recorded at birth, we examined the intersection of sex and transgender identity. We found 677 participants who had reported being female sex and selected “yes, male-to-female (MTF)” transgender identity and 625 participants who reported being male sex and selected “yes, female-to-male (FTM)” for the gender identity question. We recoded the 677 participants reporting to be female sex and selected “yes, male-to-female (MTF)” for the gender identity question as male sex recorded at birth. We recoded the 625 participants reporting to be male sex and “yes, female-to-male (FTM)” as female sex recorded at birth. For the remainder of this article when we refer to sex, we are referring to sex recorded at birth.
Classifying alcohol use relies on sex, with definitions of moderate and heavy drinking being different for males and females.23 There is currently no consistent guidance on whether sex recorded at birth or gender identity should be considered for the purpose of classifying alcohol use.24 We examined the mean number of drinks per week by gender identity and sex and found that those with male recorded sex at birth had a higher mean number of drinks per week across all gender identity categories. Based on this, we used sex recorded at birth to assign alcohol use classifications. We categorized alcohol use as: no alcohol use (n=58,406), infrequent drinker (n=0), light drinker (n=281,343), moderate drinker (n=417,879), and heavy drinker (n=155,526).22 We chose the demographic and behavioral covariates based on previous evidence suggesting significant relationships to CVD.25
Statistical analysis
We conducted logistic regression in R version 3.6.3 using the following R statistical packages: tidyverse,26 car,27 ROCR,28 survey,29 spatstat,30 tidyr,31 and sjstats.32 For all analysis (include frequencies and percentages already reported), we used the overall survey weights recommended by BRFSS (i.e., LLCPWT) modified as recommended for data sets that combine data from multiple BRFSS survey administrations. The first model contained the demographic variables. The second model included demographic variables plus health behaviors and risks. The third model included all previous variables and transgender identity. The fourth model included all previous variables and an interaction between sex and transgender identity. When the interaction term was statistically significant, we stratified the fourth model by sex recorded at birth and reported the stratified models as the final models.
For the final models, all assumptions for logistic regression were met.33 We used variance inflation factors scores to test multicollinearity; they were all lower than 2, meeting this assumption. The assumption of independence of observations was met through the sampling methods. We transformed the age variable, which did not initially meet the linearity assumption. Because the age distribution was somewhat different for male and female sex, we used slightly different transformations in each group. After the transformations, the variable met the linearity assumption.
We identified influential observations using Cook's Distance plots, removed them from the data, and estimated the models again to examine any changes in coefficient values and significance, model significance, and model fit. Removing the five observations with the greatest Cook's Distances did not make a notable change in any aspect of the models, so results reported are for all observations.
Results
The sample had a total of 850,063 (93.1%) participants without CVD and 63,091 (6.9%) participants with CVD (Table 1). More participants were female (n=461,870; 50.6%) compared with male (n=451,284; 49.4%). Fewer were black, indigenous, and people of color (BIPOC) (n=310,386; 34%) compared with White (Table 1). There were statistically significant bivariate associations with CVD for age, sex, race-ethnicity, educational attainment, BMI, smoking status, alcohol use, exercise, and transgender identity (p<0.05; Table 1).
Table 1.
Characteristics of the 913,154 Survey Participants by Cardiovascular Disease Status
| Overall, n = 913,154 | No CVD, n = 850,063 | CVD, n = 63,091 | p | ||||
|---|---|---|---|---|---|---|---|
| Age (median, IQR) | |||||||
| Years | 49 | 33–63 | 57 | 42–68 | 69 | 61–77 | <0.001 |
| n | % | n | % | n | % | ||
|---|---|---|---|---|---|---|---|
| Sex | |||||||
| Male |
451,284 |
49.42 |
413,538 |
91.64 |
37,746 |
8.36 |
<0.001 |
| Female |
461,869 |
50.58 |
436,525 |
94.51 |
25,344 |
5.49 |
|
| Race-ethnicity | |||||||
| White |
602,769 |
66.01 |
555,945 |
92.23 |
46,824 |
7.77 |
<0.001 |
| BIPOC |
310,385 |
33.99 |
294,118 |
94.76 |
16,267 |
5.24 |
|
| Educational attainment | |||||||
| Some college or college degree |
541,295 |
59.28 |
510,617 |
94.33 |
30,678 |
5.67 |
<0.001 |
| High school, GED, or less |
371,859 |
40.72 |
339,447 |
91.28 |
32,412 |
8.72 |
|
| BMI | |||||||
| Normal or underweight |
305,962 |
33.51 |
290,764 |
95.03 |
15,198 |
4.97 |
<0.001 |
| Overweight or obese |
607,191 |
66.49 |
559,299 |
92.11 |
47,892 |
7.89 |
|
| Smoking status | |||||||
| Current of former |
377,705 |
41.36 |
338,626 |
89.65 |
39,079 |
10.35 |
<0.001 |
| Never smoker |
535,450 |
58.64 |
511,438 |
95.52 |
24,012 |
4.48 |
|
| Alcohol use | |||||||
| None |
58,406 |
6.4 |
55,700 |
95.37 |
2,706 |
4.63 |
<0.001 |
| Light |
281,343 |
30.81 |
267,253 |
94.99 |
14,090 |
5.01 |
|
| Moderate |
417,880 |
45.76 |
379,204 |
90.74 |
38,676 |
9.26 |
|
| Heavy |
155,526 |
17.03 |
147,907 |
95.1 |
7,619 |
4.9 |
|
| Exercise in the past month | |||||||
| No |
230,157 |
25.2 |
205,839 |
89.43 |
24,318 |
10.57 |
<0.001 |
| Yes |
682,998 |
74.8 |
644,225 |
94.32 |
38,773 |
5.68 |
|
| Gender identity | |||||||
| Cisgender |
908,709 |
99.51 |
846,029 |
93.1 |
62,680 |
6.9 |
<0.001 |
| Transgender |
3,428 |
0.38 |
3,094 |
90.26 |
334 |
9.74 |
|
| Gender nonconforming | 1,017 | 0.11 | 941 | 92.53 | 76 | 7.47 | |
p-Values are from χ2 analyses for categorical covariates and Mann–Whitney U-test for age (data source: weighted 2015–2019 BRFSS).
BIPOC, black, indigenous, and people of color; BMI, body mass index; BRFSS, Behavioral Risk Factor Surveillance System; CVD, cardiovascular disease; IQR, interquartile range.
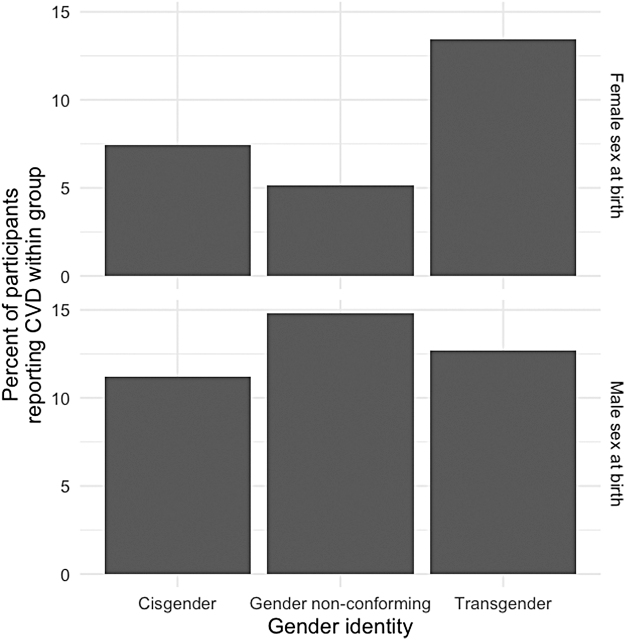
The final models (Table 2) predicting CVD from demographics, health behaviors, and transgender status were statistically significantly better than the baseline at explaining CVD for female sex participants [χ2(11)=31,429.3; p<0.05] and male sex participants [χ2(11)=42,983.8; p<0.05]. For participants who recorded as female sex at birth, those who identified as transgender had 2.66 times higher odds to report CVD (95% confidence interval [CI]: 1.60–4.41) than those identifying as cisgender. For participants who recorded male sex at birth, odds of CVD were not statistically significantly different than for transgender identity compared with cisgender identity; however, those who were GNC had 2.21 times higher odds of reporting CVD (95% CI: 1.04–4.70) compared with those with cisgender identity. A visualization of CVD by gender identity and sex (Fig. 1) demonstrates the relationship well.
Table 2.
Adjusted Odds of Cardiovascular Disease by Demographic Characteristics and Health Behaviors in 913,154 Participants in the 2015–2019 Behavioral Risk Factor Surveillance System Survey Administrations
| |
Female sex recorded at birth, n=499,987 |
Male sex recorded at birth, n=413,167 |
||
|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | |
| Transformed age in years | 2.29 | 2.22–2.36 | 18.05 | 16.68–19.54 |
| Race-ethnicity | ||||
| White | Ref. | Ref. | ||
| BIPOC | 1.10 | 1.04–1.17 | 0.87 | 0.82–0.93 |
| Formal educational attainment | ||||
| Some college or college degree | Ref. | Ref. | ||
| High school, GED, or less | 1.36 | 1.29–1.43 | 1.21 | 1.15–1.26 |
| BMI category | ||||
| Underweight or normal weight | Ref. | Ref. | ||
| Overweight or obese | 1.34 | 1.27–1.42 | 1.29 | 1.27–1.36 |
| Smoking status | ||||
| Ever smoker | Ref. | Ref. | ||
| Never smoker | 0.52 | 0.50–0.55 | 0.55 | 0.53–0.58 |
| Alcohol use | ||||
| Heavy | Ref. | Ref. | ||
| Moderate | 0.89 | 0.75–1.06 | 0.94 | 0.84–1.06 |
| Light | 1.20 | 1.03–1.40 | 1.16 | 1.03–1.30 |
| Never | 1.97 | 1.70–2.28 | 1.60 | 1.43–1.79 |
| Exercise | ||||
| No | Ref. | Ref. | ||
| Yes | 0.67 | 0.63–0.70 | 0.76 | 0.73–0.80 |
| Gender identity | ||||
| Cisgender | Ref. | Ref. | ||
| Gender nonconforming | 1.22 | 0.60–2.48 | 2.21 | 1.04–4.70 |
| Transgender | 2.66 | 1.60–4.41 | 1.18 | 0.89–1.55 |
aOR, adjusted odds ratio; CI, confidence interval.
FIG. 1.
Percentage of the 913,154 survey participants who reported CVD by sex and gender identity (data source: weighted 2015–2019 BRFSS). BRFSS, Behavioral Risk Factor Surveillance System; CVD, cardiovascular disease.
We also found several of the demographic characteristics and health behaviors to be statistically significantly associated with CVD (Table 2). The odds of CVD increased significantly as age increased for participants of both sexes. Participants of both sexes who were overweight or had obesity had significantly higher odds of CVD compared with normal weight and underweight participants. The odds of CVD for a participant who was a never smoker were lower than the odds for ever smokers for female and male sex participants. Participants of both sexes with high school, a GED, or less educational attainment had significantly higher odds of CVD than those with more education. Participants of both sexes who exercised had significantly lower odds of CVD than those who did not exercise. For females and males, odds for CVD were significantly higher for light drinkers and never drinkers than heavy drinkers. Odds for CVD were not statistically significantly different for moderate drinkers compared with heavy drinkers for female or male participants. The only notable difference between the female and male sex stratified models, other than the gender identity results, was that BIPOC participants had significantly higher odds of CVD than whites in the model for female sex participants and significantly lower odds of CVD than whites in the model for male sex participants.
Model fit and model diagnostics
We compared model fit across all four models using the akaike information criterion (AIC). Model fit increased from model 1 to model 2, from model 2 to model 3, and from model 3 to model 4. After stratifying model 4 by female and male sex recorded at birth, we removed the outlying observations from the model based on Cook's Distances and found no significant model fit improvement or notable changes in odds ratios without these observations; final stratified models retained all observations with complete data. For those who wish to reproduce our analyses or check statistical models, the R statistical code used to perform all analyses is available as Supplementary Data. For participants who were female sex, model 4 correctly predicted 463,053 of 463,074 those who did not have CVD but only 10 of 36,913 who did have CVD for a Count-R2 of 92.6% correctly predicted. For participants who were male sex, model 4 correctly predicted 365,103 of 365,120 those who did not have CVD but only 15 of 48,047 who did have CVD for a Count-R2 of 88.4% correctly predicted.
Discussion
For participants who were female sex recorded at birth, we found statistically significant higher odds of reporting CVD for those identifying as transgender compared with cisgender after accounting for demographic and behavioral characteristics. This relationship did not hold for participants who were male sex recorded at birth; however, among participants who were male sex at birth, those who reported being GNC had significantly higher odds of CVD than those reporting being cisgender. Our results also confirmed known associations between CVD and smoking, exercise, BMI, and age. The difference between sexes in the odds of CVD by race is not well studied, but there is some evidence that race and gender intersect to influence CVD risk34; our finding and the limited related evidence suggest this is an area for further study. Our findings were inconsistent with prior research suggesting heavy alcohol use increases CVD risk16 ; however, other research on alcohol use and CVD risk implies a complex relationship between the two.35,36 One possible reason for the difference between our results and prior research is that we did not have a measure of prior alcohol use and former alcohol users are different from never users when it comes to cardiovascular outcomes.37
There is evidence that men with transgender identity have a much higher rate of smoking than cisgender men and transgender individuals of both sexes are more likely to smoke daily than cisgender individuals who smoke.38 Transgender men and women are also less likely to meet exercise recommendations than cisgender men and women.39 By virtue of participating in risky health behaviors at higher rates, transgender individuals may be at even higher CVD risk compared with their cisgender counterparts.
Whereas we focused on demographics and health behavior, some studies examining CVD for transgender individuals have also examined the relationship between hormone therapy drugs and cardiovascular events,12 which is likely an important piece of the puzzle. For example, a meta-analysis of cardiovascular outcomes and hormone therapy drugs found statistically significant changes in biomarkers suggesting higher CVD risk for transgender men and transgender women.40 However, Defreyne et al. suggested that, owing to recent changes in hormone therapy, many existing studies of this relationship are no longer valid and new research is needed.41 More recently, Scheres et al. found that transgender women who have used gender-affirming hormone therapy have changes in coagulation that likely contribute to higher VTE risk.42
The majority of studies of transgender identity and CVD have identified increased CVD risk for transgender individuals compared with cisgender individuals.6,13,43,44 In the study most similar to ours, the researchers found that transgender individuals had statistically significantly higher odds of myocardial infarction than cisgender individuals after adjusting for race, ethnicity, and age.44 Getahun et al. found transgender women had a higher incidence of VTE than cisgender men and cisgender women.13 Likewise, Alzahrani et al. found that transgender women had higher odds of myocardial infarction than cisgender women (but not higher than cisgender men) and transgender men also had higher odds of myocardial infarction than cisgender men and cisgender women.6 In addition, Nota et al. found that transgender women and transgender men had higher risk of myocardial infarction than cisgender women and that transgender women had higher incidence of stroke and VTE than cisgender men and cisgender women.43 Our study adds the stratification of these relationships between gender identity and CVD by sex recorded at birth to capture how sex and gender identity together influence the odds CVD.
Limitations
Because BRFSS study data relies on self-reported measures, there are limitations of recall bias—a systematic error caused by difficulty in accurately remembering events in the past—and social desirability bias, which influences participants to ascribe themselves traits that are viewed as favorable. The survey is also a cross-sectional study design, so the questions are phrased as snapshots in time (e.g., “Has a doctor, nurse, or other health professionals EVER told you that you had coronary heart disease or a myocardial infarction?”). However, in previous studies, these types of survey questions have been validated with 81–98% agreement to official medical records.45,46 The sex question wording was evolving during the five survey administrations we examined, which may have introduced some incorrect assignment of sex, especially in 2015 when the interviewer was instructed to only ask sex if necessary and to otherwise select the sex of the participant without asking. In addition, when asked about their sex, participants may not be listing their sex recorded at birth given the nonspecific wording of the question for all participants 2015 through 2017 and for those in states where the first format of the question was used and did not specify birth sex.
In addition, we removed the 59.1% of observations missing values for one or more of the modeled variables, thus introducing bias in nonresponse. Furthermore, because of the lack of data on participants' cardiovascular medications or hormone replacement therapy—if any—it is not possible to make a definitive conclusion about the relationship between CVD and identifying as transgender. However, these biases would likely shift odds ratio estimates away from the null, meaning our model likely underestimates the true odds of CVD associated with being transgender. Our model was also not accurate in predicting CVD cases, which we expected owing to the small number of cases compared with those not reporting CVD.
Conclusion
Although given more attention in recent years, transgender health has not been widely studied.47 Many social, economic, and health disparities exist for transgender people compared with cisgender people.17,48 A 2015 survey found greater rates of poverty and unemployment, increased avoidance in seeking medical care because of financial constraints or lack of trust with their medical provider, and higher reports of discrimination in the workplace and health care settings among transgender individuals.49 Another survey of transgender adults in the United States reported 63% of participants experienced a serious act of discrimination owing to bias such as job loss, school bullying or harassment, eviction, physical assault, homelessness, loss of relationship with their partner or children because of gender identity or expression, denial of medical services, or incarceration.11 Not only do these injustices discriminate at the societal level, but they also have serious implications on a person's health status, making this a nuanced and transdisciplinary public health problem. Understanding and addressing health disparities, like the higher odds of CVD among transgender men found in this study, will require better interventions and more attention to measurement and data collection that is inclusive of transgender and other gender identities.
Supplementary Material
Abbreviations Used
- AIC
akaike information criterion
- aOR
adjusted odds ratio
- BIPOC
black, indigenous, and people of color
- BMI
body mass index
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CI
confidence interval
- CVD
cardiovascular disease
- FTM
female-to-male
- GNC
gender nonconforming
- IQR
interquartile range
- MTF
male-to-female
- VTE
venous thromboembolism
Author Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
Supplementary Material
Cite this article as: Howerton I, Harris JK (2022) Transgender identity and cardiovascular disease, Transgender Health 7:5, 407–415, DOI: 10.1089/trgh.2020.0188.
References
- 1. Nguyen HB, Chavez AM, Lipner E, et al. Gender-affirming hormone use in transgender individuals: impact on behavioral health and cognition. Curr Psychiatry Rep. 2018;20:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Safer JD, Tangpricha V. Care of the transgender patient. Ann Intern Med. 2019;171:ITC1–ITC16. [DOI] [PubMed] [Google Scholar]
- 3. Flores AR, Brown TN, Herman J. Race and Ethnicity of Adults Who Identify as Transgender in the United States. Los Angeles, CA: Williams Institute, UCLA School of Law, 2016. [Google Scholar]
- 4. Connelly PJ, Marie Freel E, Perry C, et al. Gender-affirming hormone therapy, vascular health and cardiovascular disease in transgender adults. Hypertension. 2019;74:1266–1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Grant J, Mottet L, Tanis J, et al. National transgender discrimination survey report on health and health care. 2010. Available at: https://cancer-network.org/wp-content/uploads/2017/02/National_Transgender_Discrimination_Survey_Report_on_health_and_health_care.pdf Accessed June 23, 2021.
- 6. Alzahrani T, Nguyen T, Ryan A, et al. Cardiovascular disease risk factors and myocardial infarction in the transgender population. Circ Cardiovasc Qual Outcomes. 2019;12:e005597. [DOI] [PubMed] [Google Scholar]
- 7. Cigna. LGBT health disparities. Cigna Health and Wellness, 2017. Available at: https://www.cigna.com/individuals-families/health-wellness/lgbt-disparities Accessed June 23, 2021.
- 8. Goedel WC, Regan SD, Chaix B, et al. Using global positioning system methods to explore mobility patterns and exposure to high HIV prevalence neighbourhoods among transgender women in New York. Geospat Health. 2019;14. Available at: https://pubmed.ncbi.nlm.nih.gov/31724385/ Accessed June 23, 2021. [DOI] [PMC free article] [PubMed]
- 9. Downing JM, Przedworski JM. Health of transgender adults in the US, 2014–2016. Am J Prev Med. 2018;55:336–344. [DOI] [PubMed] [Google Scholar]
- 10. White Hughto JM, Murchison GR, Clark K, et al. Geographic and individual differences in healthcare access for US transgender adults: a multilevel analysis. LGBT Health. 2016;3:424–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grant JM, Motter LA, Tanis J, et al. Injustice at every turn: a report of the national transgender discrimination survey. 2011. Available at: https://transequality.org/sites/default/files/docs/resources/NTDS_Report.pdf Accessed June 23, 2021.
- 12. Irwig MS. Cardiovascular health in transgender people. Rev Endocr Metab Disord. 2018;19:243–251. [DOI] [PubMed] [Google Scholar]
- 13. Getahun D, Nash R, Flanders WD, et al. Cross-sex hormones and acute cardiovascular events in transgender persons: a cohort study. Ann Intern Med. 2018;169:205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Streed Jr CG, Harfouch O, Marvel F, et al. Cardiovascular disease among transgender adults receiving hormone therapy: a narrative review. Ann Intern Med. 2017;167:256–267. [DOI] [PubMed] [Google Scholar]
- 15. O'Neil A, Scovelle AJ, Milner AJ, Kavanagh A. Gender/sex as a social determinant of cardiovascular risk. Circulation. 2018;137:854–864. [DOI] [PubMed] [Google Scholar]
- 16. Blosnich JR, Lehavot K, Glass JE, Williams EC. Differences in alcohol use and alcohol-related health care among transgender and nontransgender adults: findings from the 2014 Behavioral Risk Factor Surveillance System. J Stud Alcohol Drugs. 2017;78:861–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Winter S, Diamond M, Green J, et al. Transgender people: health at the margins of society. Lancet. 2016;388:390–400. [DOI] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Questionnaire. 2015. Available at: https://www.cdc.gov/brfss/questionnaires/pdf-ques/2015-brfss-questionnaire-12-29-14.pdf Accessed June 23, 2021.
- 19. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Questionnaire. 2016. Available at: https://www.cdc.gov/brfss/questionnaires/pdf-ques/2016_BRFSS_Questionnaire_FINAL.pdf Accessed June 23, 2021.
- 20. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Questionnaire. 2017. Available at: https://www.cdc.gov/brfss/questionnaires/pdf-ques/2017_BRFSS_Pub_Ques_508_tagged.pdf Accessed June 23, 2021.
- 21. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Questionnaire. 2018. Available at: https://www.cdc.gov/brfss/questionnaires/pdf-ques/2018_BRFSS_English_Questionnaire-508.pdf Accessed June 23, 2021.
- 22. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Questionnaire. 2019. Available at: https://www.cdc.gov/brfss/questionnaires/pdf-ques/2019-BRFSS-Questionnaire-508.pdf Accessed June 23, 2021.
- 23. Centers for Disease Control and Prevention. National Health Interview Survey glossary—alcohol. 2018. Available at: https://www.cdc.gov/nchs/nhis/alcohol/alcohol_glossary.htm Accessed June 23, 2021.
- 24. Gilbert PA, Pass LE, Keuroghlian AS, et al. Alcohol research with transgender populations: a systematic review and recommendations to strengthen future studies. Drug Alcohol Depend. 2018;186:138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cicero EC, Reisner SL, Merwin EI, et al. The health status of transgender and gender nonbinary adults in the United States. PLoS One. 2020;15:e0228765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wickham H, Averick M, Bryan J, et al. Welcome to the tidyverse. J Open Source Softw 2019;4:1686. [Google Scholar]
- 27. Fox J, Weisberg S, Adler D, et al. Package ‘car.’ Vienna: R Foundation for Statistical Computing, 2012.
- 28. Sing T, Sander O, Beerenwinkel N, Lengauer T. ROCR: visualizing classifier performance in R. Bioinformatics 21:3940–3941. [DOI] [PubMed] [Google Scholar]
- 29. Lumley T. Analysis of Complex Survey Samples. Journal of Statistical Software, 2004;9(1):1–19. R package version 2.2. [Google Scholar]
- 30. Baddeley A, Rubak E, Turner R. Spatial point patterns: methodology and applications with R. Chapman and Hall/CRC Press, 2015. Available at: https://www.routledge.com/Spatial-Point-Patterns-Methodology-and-Applications-with-R/Baddeley-Rubak-Turner/9781482210200 Accessed June 23, 2021.
- 31. Wickham H. Tidyr: tidy messy data. 2021. Available at: https://CRAN.R-project.org/package=tidyr Accessed June 23, 2021.
- 32. Lüdecke D. Sjstats: statistical functions for regression models (Version 0.18.1). DOI: 10.5281/zenodo.1284472, Available at: https://CRAN.Rproject.org/package=sjstats Accessed June 23, 2021.
- 33. Harris JK. Statistics with R: Solving Problems Using Real-World Data. Thousand Oaks, CA: SAGE Publications, 2020. [Google Scholar]
- 34. Walsemann KM, Goosby BJ, Farr D. Life course SES and cardiovascular risk: heterogeneity across race/ethnicity and gender. Soc Sci Med. 2016;152:147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhang X, Liu Y, Li S, et al. Alcohol consumption and risk of cardiovascular disease, cancer and mortality: a prospective cohort study. Nutr J. 2021;20:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ronksley PE, Brien SE, Turner BJ, et al. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Goel S, Sharma A, Garg A. Effect of alcohol consumption on cardiovascular health. Curr Cardiol Rep. 2018;20:1–10. [DOI] [PubMed] [Google Scholar]
- 38. Drope J, Liber AC, Cahn Z, et al. Who's still smoking? Disparities in adult cigarette smoking prevalence in the United States. CA Cancer J Clin. 2018;68:106–115. [DOI] [PubMed] [Google Scholar]
- 39. Jones BA, Haycraft E, Bouman WP, Arcelus J. The levels and predictors of physical activity engagement within the treatment-seeking transgender population: a matched control study. J Phys Act Health. 2018;15:99–107. [DOI] [PubMed] [Google Scholar]
- 40. Maraka S, Singh Ospina N, Rodriguez-Gutierrez R, et al. Sex steroids and cardiovascular outcomes in transgender individuals: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2017;102:3914–3923. [DOI] [PubMed] [Google Scholar]
- 41. Defreyne J, Van de Bruaene LDL, Rietzschel E, et al. Effects of gender-affirming hormones on lipid, metabolic, and cardiac surrogate blood markers in transgender persons. Clin Chem. 2019;65:119–134. [DOI] [PubMed] [Google Scholar]
- 42. Scheres LJ, Selier NL, Nota NM, et al. Effect of gender-affirming hormone use on coagulation profiles in transmen and transwomen. J Thromb Haemost. 2021;19:1029–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nota NM, Wiepjes CM, de Blok CJ, et al. Occurrence of acute cardiovascular events in transgender individuals receiving hormone therapy: results from a large cohort study. Circulation. 2019;139:1461–1462. [DOI] [PubMed] [Google Scholar]
- 44. Meyer IH, Brown TN, Herman JL, et al. Demographic characteristics and health status of transgender adults in select US regions: Behavioral Risk Factor Surveillance System, 2014. Am J Public Health. 2017;107:582–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tretli S, Lund-Larsen PG, Foss OP. Reliability of questionnaire information on cardiovascular disease and diabetes: cardiovascular disease study in Finnmark county. J Epidemiol Community Health. 1982;36:269–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Okura Y, Urban LH, Mahoney DW, et al. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57:1096–1103. [DOI] [PubMed] [Google Scholar]
- 47. Korpaisarn S, Safer JD. Gaps in transgender medical education among healthcare providers: a major barrier to care for transgender persons. Rev Endocr Metab Disord. 2018;19:271–275. [DOI] [PubMed] [Google Scholar]
- 48. Hafeez H, Zeshan M, Tahir MA, et al. Health care disparities among lesbian, gay, bisexual, and transgender youth: a literature review. Cureus. 2017;9:e1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. James SE, Herman J, Rankin JL, et al. The report of the 2015 U.S. transgender survey. 2016, Available at: https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf Accessed June 23, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.