Abstract
Purpose:
To describe the development of the United States Air Force's (USAF) telehealth program from fall 2017 through fall of 2020 in response to the unique challenges associated with providing care for a global transgender military population.
Methods:
Telehealth visit completion rates were monitored at time of encounters and through electronic health record reports. Patient satisfaction data were obtained by immediate postvisit survey, across provider care received, logistics of setting up the appointment, and quality of the virtual health system connection. Patient cases highlighting opportunities for transgender telehealth were summarized.
Results:
Between September 9, 2019 and October 28, 2020, 99 telehealth encounters with video-to-video connection occurred. Twenty-three of the encounters were for gender-affirming hormone therapy, 17 for mental health visits, and 59 for speech therapy. Thirty-five surveys were collected from 20 patients. Overall patients were “satisfied” or “very satisfied” with providers' ability to manage their chief complaint through this modality (average 4.9 out of 5 on 1 to 5 scale with 1 being “very dissatisfied” and 5 being “very satisfied”) and “strongly agree” that telehealth is an effective means to accomplish care (average score 4.8 on 1 to 5 scale with 1 being “strongly disagree” and 5 “strongly agree”). Services provided spanned 11 USAF bases worldwide.
Conclusions:
Telehealth is successful in ensuring ongoing transgender health care services for a global military population. The success of this program may have implications for future military and civilian endeavors to bridge care gaps for transgender patients in resource-poor or distant-site locations.
Keywords: access, gender, military, telehealth, telemedicine, transgender
Background
In October of 2016, the United States Department of Defense (DoD) implemented new policy allowing transgender service members to openly serve. Each service was charged with developing a team to oversee the gender-affirming medical care for any members seeking an in-service military gender marker change.1 The United States Air Force (USAF) opted to create a single, centralized team, the Medical Multidisciplinary Team (MMDT) in policy directives.2 Initially the goal was for the MMDT to provide oversight and case management services remotely. Direct care for mental health (MH) services, gender-affirming hormones, surgical care, and other services such as speech therapy (ST) were to be done directly in the patient's clinic or “military treatment facility” (MTF), or referred off-base for care in the civilian health care system. Unfortunately, two issues prevented this from occurring across the USAF. First, Primary Care Managers were reluctant to provide care in an unfamiliar care area. Indeed, national deficits in transgender education in health care training programs are a known issue3,4 and a study in 2017 among USAF family physicians reflected similar findings.5 Second, several service members in small civilian communities were without specialty care resources. This concern is compounded for patients stationed in overseas locations, where all care is typically done at the on-base clinic. By fall of 2017, it was clear to MMDT providers and USAF medical leadership that if transgender patients were going to remain as operationally effective as their cisgender peers, these health care disparities would need to be addressed.
At that time, telehealth had already been utilized by some military specialties across the DoD. Telepsychiatry was an early user of telemedicine,6 with advances in telemedicine for radiology, dermatology, and pathology as well. As a result, a USAF Telehealth Program Office (USAFTPO) was already functioning to provide systems support for treatment facilities. Because virtual telecommunication (VTC) technology had already been installed in at least one clinic at each MTF across the USAF to support telepsychiatry, the MMDT opted to launch telemedicine as a means to provide direct patient care services for transgender service members in resource-poor, distant locations. The purpose of this article is to present visit completion rates, patient satisfaction data, and case vignettes from the MMDT telehealth program development efforts, as well as showcase successful provision of varying transgender services across this medium.
Methods
Setting
The MMDT consists of nursing case managers, MH providers, adolescent medicine specialists, endocrinologists, speech-language pathologists (SLPs), and surgical subspecialists. In 2017, most AF members with gender dysphoria were just starting gender-affirming medical care; therefore, the initial goal was to ensure direct virtual health services were available for MH, gender-affirming hormone therapy, and ST. The MMDT is located within one of the USAF's largest MTFs and thus was sufficiently resourced to support the global telehealth initiative.
Participants
There are ∼75 MTFs across the AF and most are responsible for the medical care of at least one transgender member stationed at that base. All active-duty USAF transgender patients were eligible to receive direct video and audio virtual visits starting September 1, 2019. Providers hosting virtual video encounters included one MMDT licensed clinical social worker, one adult endocrinologist, one adolescent medicine provider, and two SLPs with expertise in voice.
Development of telehealth service
Systems set-up
In fall of 2017, MMDT leadership requested support from the USAFTPO for a transgender virtual telehealth service initiative. Hardware consisted of web cameras installed at each MTF. Initially, the USAFTPO installed two web cameras within the MMDT clinic. Remote transgender patients were then able to connect to their MMDT provider through a camera within their MTF. The USAF subsequently purchased several stand-alone monitors with embedded cameras (i.e., CISCO DX80) capable of using “one-touch” telehealth connection technology between MTFs with compatible devices.
DISA GVS was a Skype-like, HIPPA-compliant, secure room software initially utilized for these encounters. With the onset of the coronavirus disease 2019 (COVID-19) pandemic, the USAF approved the use of other civilian VTC platforms, such as Adobe Connect, Skype, FaceTime, and Google Duo, to ensure patient care during shelter-in-place orders.7 Additionally, MMDT providers reported Doximity to be a useful VTC modality as the application could be utilized over the patient's cell phone without prior account creation by the patient. Although the initial goal was to connect with patients MTF to MTF, some patient encounters were hosted on the alternative platforms listed above.
Credentialing
USAF providers are required to have state licensure; however, as they are often stationed at several bases throughout their careers, the military allows practice privileges across any federal military installation regardless of where the provider resides. Therefore, to move the telehealth initiative forward, telehealth-only “privileging-by-proxy” requests were granted. Early on these requests were coupled with several delays for each requesting provider; however, USAF leadership eventually streamlined the process.8,9 After that, once medical leadership at the patient's MTF site identified a need for particular transgender health services, the MMDT was able to establish telehealth privileging-by-proxy for each provider within a 2-week period.
Appointment booking
Once systems set-up and privileging-by-proxy were established at the patient's MTF, a clinical point of contact (POC) was identified to assist in scheduling and the logistical handling of the appointment itself. This POC coordinated with MMDT nursing for scheduling between the patient and provider. During appointments, the MTF clinical POC established the VTC connection, collected vitals, and administered appropriate screeners and consent forms. The POC would then leave the room for the remainder of the encounter. As needed, aftercare surveys were administered and uploaded into the military's electronic medical record (EMR) systems along with the provider's clinical documentation. The military medical record is universal across the DoD, allowing viewing of nursing and provider notes at any location.
For the encounters not conducted in the MTF and instead over civilian VTC platforms through the patient's personal smart devices, the MTF POC still liaised scheduling needs and sent out all relevant screeners, consents, and surveys before and after the visit.
Legal process
As per Defense Health Agency guidelines,9 before receiving telehealth services, patients are required to sign a consent form that reviews the risks and benefits of VTC services as well as procedures, should the technology fail resulting in a loss of the encounter. Additional information was collected from the patients not being seen within their MTF, including physical location and an emergency contact in case medical assistance was needed.
Data collection and analysis
Visit outcome information and demographics were captured by the military's EMR system and verified by compliance visit counts. Completed visits were defined as those in which patients were seen over audio and visual modalities. Noncompleted visits were defined as no-shows.
The MMDT developed a VTC-specific patient satisfaction survey in anticipation of launching telehealth services. The survey consisted of 14 satisfaction questions related to appointment logistics, MMDT provider service, VTC connection, and thoughts on telehealth overall as a means of accessing care (Table 1). While every provider sent out the survey following the initial encounter, frequency of administration beyond that was service specific. For example, patients were provided surveys following each MH and hormone visit while ST sent out the survey at minimum monthly due to the higher encounter frequency.
Table 1.
Survey Questions. Survey Questions Regarding the Quality of the Health Care Visit; Each Item Was Rated by Participants on a 5-Point Likert Scale
| Survey questions: Likert Scale 1 (least) to 5 (best) quality of experience |
|---|
| (1) Scheduling the telehealth appointment with the MMDT |
| (2) Scheduling the telehealth appointment with the MTF |
| (3) Nursing/tech support for telehealth at MTF |
| (4) Ease of completing any encounter follow-up instructions |
| (5) Provider's professionalism |
| (6) Provider's interaction with webcam |
| (7) Provider's cultural sensitivity |
| (8) Provider's ability to manage my chief complaint |
| (9) Provider's inclusion of me in developing my treatment plan |
| (10) Ability to understand the provider |
| (11) Clarity of picture/visuals |
| (12) System Connection (degree of “sticking” or “freezes”) |
| (13) Telemedicine is an effective means to accomplish my care |
| (14) I would recommend this to other of my diagnosis |
MMDT, Medical Multidisciplinary Team; MTF, military treatment facility.
Surveys were collected by the MTF POC for the visit and e-mailed to the MMDT case manager, who then uploaded the results to the MMDT restricted access/encrypted drive on the MMDT hospital server for later analysis. Descriptive statistics were used to tabulate survey results, with averages shown for the service as a whole and each subspecialty service individually.
Patient cases highlighting type of care provided through telehealth were decided upon by author consensus and included to showcase various challenges and benefits of transgender VTC health care services. Patient names were replaced by pseudonyms. The Wilford Hall Ambulatory Surgical Center (WHASC) Institutional Review Board deemed the telehealth service and patient satisfaction surveys to be quality improvement and did not require formal review.
Results
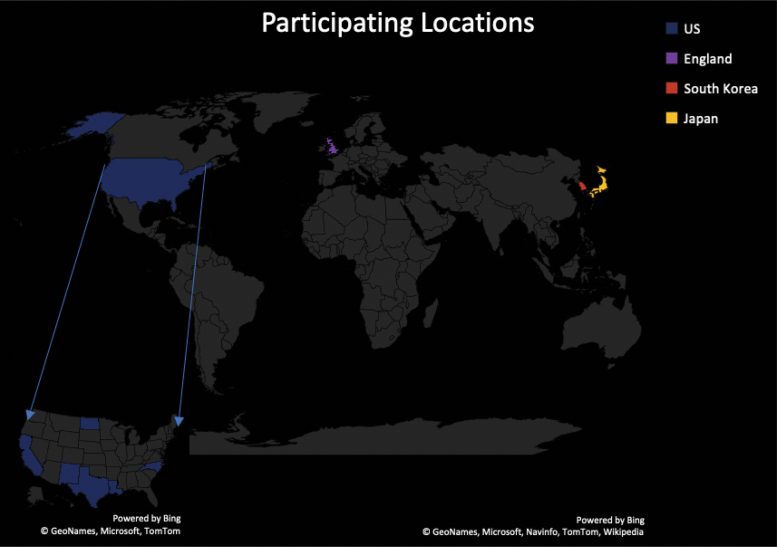
The first USAF transgender patient seen by MMDT VTC services occurred on September 9, 2019. Between then and October 28, 2020, the team completed 99 encounters for 20 patients across 11 bases worldwide (Fig. 1). The average age of patient was 28.4 years with range from 19 to 42 (median age 28). Sixteen patients were trans women, whereas four were trans men. Seven patients received more than one type of service by VTC. Thirty-five patient surveys were collected over this time (14 for hormone management encounters, 10 for MH, and 11 for ST). No-shows were minimal; there were a total of 4 across the 99 visits conducted and were all for patients forgetting when their scheduled appointment was to be held.
FIG. 1.
Participating locations World Map. The Country of each participating MTF is highlighted in a unique color. The blue arrows point to a detailed Map of the United States with the State of each participating MTF highlighted in a unique color. Produced in Office 365 PowerPoint Maps. MTF, military treatment facility.
Overall, telemedicine for transgender care was positive for patients. All patients indicated they “agree” or “strongly agree” that “Telemedicine is an effective means to accomplish my care (average score 4.8 on 1 to 5 scale with 1 being “strongly disagree” and 5 “strongly agree”)” and “I would recommend this to others with my diagnosis (average score 4.9 on same scale).” Generally, MMDT providers were rated highly across all surveys. Patients rated providers' interaction with the webcam and ability to manage the chief complaint as overall “very satisfied” (average 4.9 out of 5).
Postvisit surveys that evaluated the system-related aspects of telemedicine were similarly rated as “very satisfied.” Patients were “very satisfied” with their ability to understand the provider during the visit (4.9 out of 5), with the clarity of the picture/visuals (4.6 out of 5), and degree of “freezes” in the connection (4.6 out of 5).
Survey questions asking about satisfaction with appointment scheduling were similarly positive overall, but not as high. For example, while overall patients were “very satisfied” with scheduling the virtual appointment with the MMDT (4.7 out of 5), they were largely “satisfied” with scheduling the appointment through their own local MTF (4.3 out of 5), and comparably indicated “satisfied” with nursing and tech support for telehealth at their MTF (4.2 out of 5).
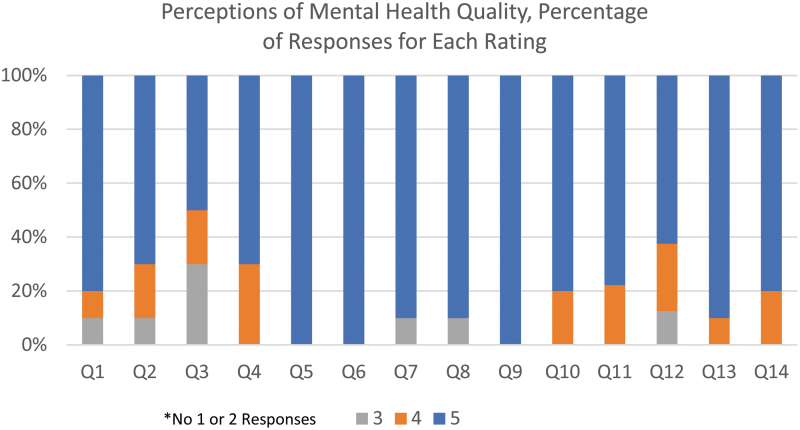
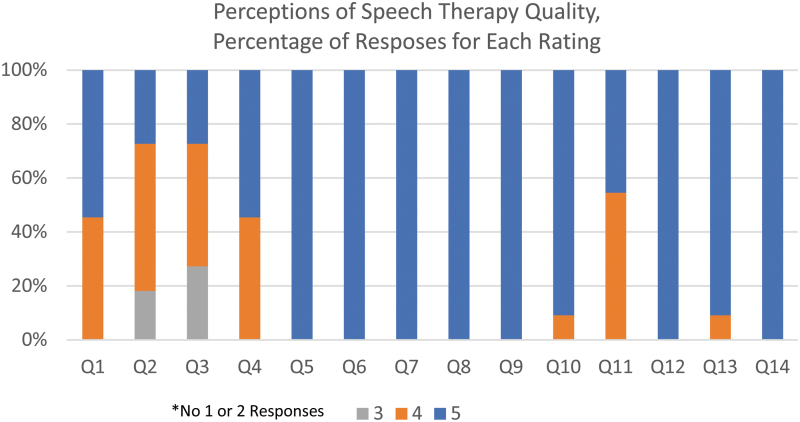
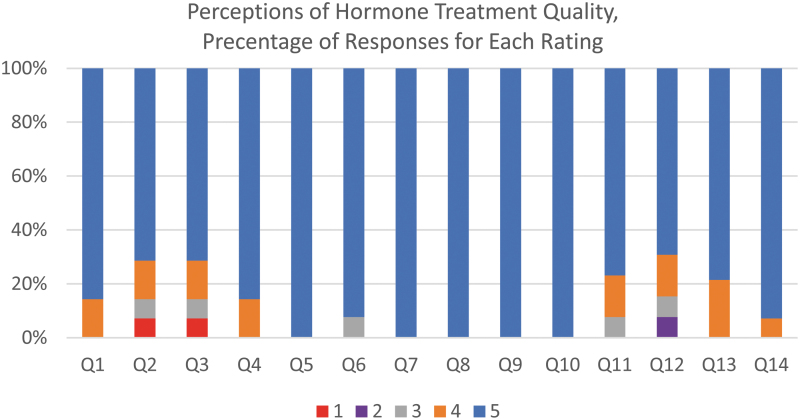
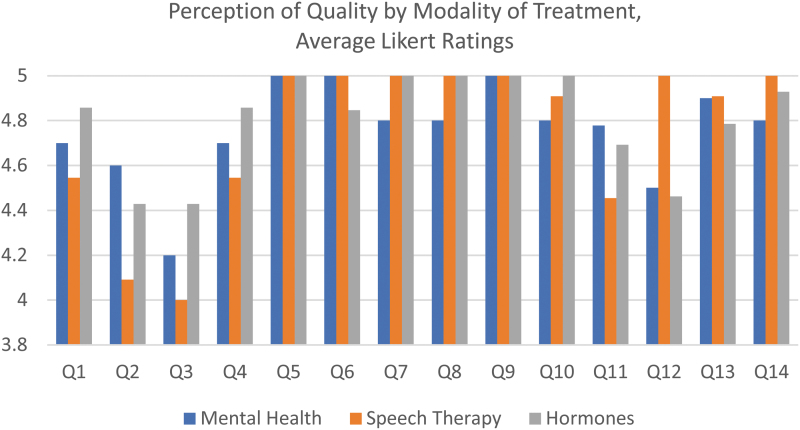
Specifics for each specialty area are listed below (Figs. 2–4) and show similar trends in patient feedback. The overall comparison of average ratings are demonstrated in Figure 5.
FIG. 2.
Perception of MH quality, percentage of responses for each rating. Each question referenced in Table 1 is represented on the X-axis and pertains to those visits held by MH. The Likert Scale ratings of 3, 4, or 5 are identified by a unique bar color, the height of which demonstrates the percentage of responses for that rating. No ratings of 1 or 2 occurred. MH, mental health.
FIG. 3.
Perception of ST quality, percentage of responses for each rating. Each question referenced in Table 1 is represented on the X-axis and pertains to those visits held by ST. The Likert Scale ratings of 3, 4, or 5 are identified by a unique bar color, the height of which demonstrates the percentage of responses for that rating. No ratings of 1 or 2 occurred. ST, speech therapy.
FIG. 4.
Perception of hormone treatment, percentage of responses for each rating. Each question referenced in Table 1 is represented on the X-axis and pertains to those visits held by hormone treatment providers. The Likert Scale ratings of 1, 2, 3, 4, or 5 are identified by a unique bar color, the height of which demonstrates the percentage of responses for that rating.
FIG. 5.
Perception of quality by modality of treatment, average Likert ratings. Each question referenced in Table 1 is represented on the X-axis. MH, ST, and hormone therapy visits are identified by a unique bar color, the height of which demonstrates the average Likert rating.
Patient cases
Brief patient cases exemplifying each type of transgender health service provided through VTC are noted below to demonstrate scope of care and highlight challenges and benefits.
Case #1: MH
Jay is a 29-year-old trans woman who sought telehealth services after a history of in-person MH treatment with inconsistent attendance on the part of the patient. Initially, the patient was experiencing suicidal ideations without intent or plan and was very reserved, speaking of their concerns in vague terms and resisting attempts to elicit clarifying details. By the third session, the patient was diagnosed with adjustment disorder and cognitive behavioral therapy intervention was implemented.
Over the course of four additional sessions, Jay became significantly more engaged in the therapeutic process. They responded to therapy and reduced their suicidal ideations. The patient's scores on the Columbia Screener-Lifetime reflected a reduction of suicidal ideations starting in session 3 and maintained through session 7, which was the patient's most recent session with provider. Jay's feedback survey also reflects an increase in satisfaction with the telehealth modality. As per patient report, they feel better equipped to handle life stressors than they were before seeking telehealth MH services.
Case #2: ST
Sal is a 36-year-old trans woman who requested a referral to speech pathology for gender-affirming voice training. This was an unavailable service within her base's MTF; therefore, she was referred for VTC services. She demonstrated high levels of motivation throughout and was compliant with her home exercise programs and generalization tasks. At the time of this writing, she had been seen for seven VTC voice feminization training sessions targeting pitch, vocal loudness, resonance, intonation, and nonverbal communication. She reported being “very satisfied” with provider treatment delivery and the technological aspects of the telehealth encounters. Sal “strongly agreed” she would recommend telehealth to others.
Case #3: Hormone management
Andy is a 24-year-old trans man. His MTF was located overseas where transgender resources were limited for service members, so his leadership was concerned that he could not start gender-affirming medical care. Because Andy's chosen military career field was heavily tied to this particular region of the world, there were not many options for moving, effectively jeopardizing his future in the military.
Medical leadership at his location worked in conjunction with the MMDT to develop telehealth. Initially, MMDT providers could not order laboratories or meds for the patient as each MTF laboratory and medication ordering system is limited to the providers stationed there. This was circumvented by finding a provider in the clinic who ordered needed laboratories per MMDT recommendations. Andy signed up for Express Scripts, the Tricare mail delivery pharmacy service, which allows providers from any DoD MTF to fax in prescription orders. This allowed the patient to effectively start hormone therapy until MMDT providers were granted access to Andy's local ordering system. The successful launch of VTC services for transgender patients at Andy's MTF removed the limitations previously placed on transgender USAF members to work in that part of the world.
Discussion
Our initial data show that VTC services for gender-affirming care across several disciplines is well received by USAF transgender members. Satisfaction scores overall remain high for providers' ability to meet clinical needs and interact over the VTC medium, for the scheduling and logistics of setting up a telehealth appointment, and for the connection of the VTC system itself. This was consistent across our various specialty offerings as a whole and for each individual specialty service provided.
To some extent, favorable scores are to be expected. Given the recent advent of transgender members in the service and limitations in training programs nationally,3,4 a paucity of resources for providing transgender health care services still exists in some locations. This is especially true for sites that are located in more rural areas or overseas locations that lack an easy referral source in the civilian community. For some services, this is more evident than in others. For example, there are very few voice specialists in the field of Speech-Language Pathology, fewer that have the competencies to provide gender-affirming voice training, and fewer still that are employed within the military health system.10 As noted previously, among potential hormone providers in the military setting there is a lack of comfort to provide care for transgender patients.5 When it comes to specialty services like these, the military's resources, consequentially, are often proportionately small. As a result, provision of care through VTC with experienced gender-affirming providers is a choice between no health care service at all, or the use of virtual services. This may also explain the low no-show rates we saw. Not only is there more direct nursing coordination with the patient to facilitate appointment times across time zones between the MMDT provider and local MTF, but patients have little other options for care if they do not make their appointment. It is unclear what the impact may be on future use of transgender VTC services as MMDT and USAF medical leadership work to expand transgender-specific health care education.
Our cases demonstrate some of the challenges and benefits of transgender telehealth services. In addition to the increased access to care, the incorporation of services from the MMDT assures that patients are offered care that is affirming of their gender identity. In essence, interdisciplinary telehealth care allows for comprehensive end-to-end delivery of transgender-related services for military members.
Several advantages exist for launching a telehealth effort in the military setting. The use of the central USAFTPO means that system compatibility issues are kept to a minimum. The USAFTPO knows all software platforms in use across the USAF Medical Service and can leverage that information to ensure the chosen VTC platform will function optimally at each MTF. Furthermore, DoD's development of a universal protocol for telehealth privileging-by-proxy means that state-to-state care hurdles are minimized and providers can be credentialed at a patient's MTF within 2 weeks. The use of a standardized EMR across the DoD is beneficial in that documentation can be reviewed by both MMDT providers and the patient's MTF.
Challenges do remain in setting up telehealth services. Despite system compatibility and solutions for privileging, bringing care to an MTF that has not previously utilized the platform requires considerable administrative workload. MMDT staff liaise with multiple offices to verify system compatibility, push through privileging-by-proxy requests, ensure laboratory and medication ordering access, develop templates for provider appointments, and train MTF POCs on logistical procedures for scheduling, administering screeners, and taking vitals for various appointments. At first, navigating these hurdles required considerable time and explains the 2-year gap between when the MMDT first sought to provide VTC services and the first encounter in September 2019. However, as telehealth for the MMDT becomes more commonplace, onboarding new MTFs is becoming more efficient and new sites are often able to host a new patient appointment within a few weeks. As noted earlier, due to limitations of the COVID-19 pandemic, alternative civilian VTC platforms are also available for use. In some cases, this allows for faster care; however, without the MTF support this does introduce additional tasks for the patient and provider. It remains unclear at the time of this writing whether military policy will allow continued use of home virtual health services beyond the current pandemic.
There are some limitations of our data presented. One is that while 35 surveys were collected, they represent the feedback from 20 total patients seen. As a result, some patients completed the survey twice, although at different points in their care. In addition, despite generally high scores across the survey responses, there was a noted disparity between satisfaction with MMDT provider care and scheduling logistics and nursing/tech support at the patient's MTF. Unfortunately, few comments were written to highlight the specific concerns when lower scores were given, making correction of deficits at the local clinics difficult. Furthermore, as this particular survey instrument is not universally given across all Air Force clinics providing telehealth services (the definition of which may vary from clinic to clinic, i.e., audio to audio patient care versus with a visual component), it is unknown if similar concerns exist for telehealth services provided for other patient populations. Further use of this modality for patient care and refinement of the data collection tools used may clarify these concerns.
Another possible limitation is the makeup of the patient population. As Air Force members, our patients are subject to various policy requirements that may provide additional hurdles for clinical care that may influence the decision to use telehealth as a modality or not. Furthermore, the overall age of our patients tends to be younger. Consequently, this may represent a patient population that embraces VTC as a modality for care more than other patients may; therefore, increasing our ratings. Indeed, several qualitative studies exist that highlight the affinity transgender patients in general have for technological resources.11,12 Whether age of patients or the patient population itself had an impact may require further evaluation. Our data also only show patient satisfaction, and not any measures for efficacy of care delivered. For example, during VTC ST encounters, the “DevExtra's Voice Tools” application was downloaded by the patient. Various tools within the app were used during sessions, with the clinician providing guidelines for utilizing the application independently. Although the application was not biomedically calibrated, it provided an interim solution for test measures. In the future, these may be considered as outcome measures. More formal research comparing treatment effect in telehealth versus in-person clinic care is needed.
Conclusion
In summary, our team showed that a “proof-of-concept” quality improvement project to provide gender-affirming health care services to USAF transgender service members is a way to ensure care on a global scale. Patients showed high satisfaction scores across MH, ST, and gender-affirming hormone encounters. In our experience, this modality for health care has expanded readiness options for our USAF transgender members and may be applicable in reducing barriers to transgender medical services for any patient in distant or resource-poor settings.
Acknowledgments
The authors would like to acknowledge Cecilia Sessions-Carpenter, MD; Phyllis Gallegos-Santillan, MS, CCC-SLP; and Andrea Alaniz, LVN, for their essential roles in the telehealth scale-up.
Abbreviations Used
- COVID-19
coronavirus disease 2019
- EMR
electronic medical record
- MH
mental health
- MMDT
Medical Multidisciplinary Team
- MTF
military treatment facility
- POC
point of contact
- SLPs
speech-language pathologists
- ST
speech therapy
- USAF
United States Air Force
- USAFTPO
USAF Telehealth Program Office
- VTC
virtual telecommunication
- WHASC
Wilford Hall Ambulatory Surgical Center
Authors' Contributions
J.M.S., J.M.L., C.J.M., and J.A.C. all contributed to the design of the project, participated in the collection of results, and contributed to the analysis and interpretation of the data. J.M.S. wrote the first draft of the article, and all authors contributed to its revision; all authors approved the submitted article.
Author Disclosure Statement
The authors have no conflicts of interest to declare. The views expressed are solely those of the authors and do not reflect the official policy or position of the U.S. Air Force, the Department of Defense, or the U.S. Government.
Funding Information
No funding was used in the design, execution, or completion of this study.
Cite this article as: Smalley JM, Lozano JM, McMahon CJ, Colburn JA (2022) Improving global access to transgender health care: outcomes of a telehealth quality improvement study for the air force transgender program, Transgender Health 7:2, 150–158, DOI: 10.1089/trgh.2020.0167.
References
- 1. Department of Defense Instruction (DoDI) 1300.28, Military Service by Transgender Persons and Persons with Gender Dysphoria. Washington, DC: US Department of Defense; 2020. [Google Scholar]
- 2. Air Force Policy Memorandum (AFPM) 2019-36-02, Military Service by Transgender Persons and Person's with Gender Dysphoria. Washington, DC: US Department of the Air Force; 2020. [Google Scholar]
- 3. Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender–related content in undergraduate medical education. JAMA. 2011;306:971–977. [DOI] [PubMed] [Google Scholar]
- 4. Safter JD, Coleman E, Feldman J, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016;23:167–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schvey NA, Blubaugh I, Morettini A, Klein DA. Military family physicians' readiness for treating patients with gender dysphoria. JAMA Intern Med. 2017;177:727–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nieves J. Telemental health for our soldiers: a brief review and a new pilot program. Mil Med. 2009;174:xxi–xxii. [PubMed] [Google Scholar]
- 7. Hogg DA. Memorandum. Subject: Use of Virtual Visits for Telehealth in the AFMS. Washington, DC: US Department of the Air Force Surgeon General; 2020. [Google Scholar]
- 8. Woodson J. Memorandum. Subject: Waiver of Restrictive Licensure and Privileging Procedures to Facilitate the Expansion of Telemedicine Services in the Military Health System. Washington, DC: US Department of Defense; 2012. [Google Scholar]
- 9. Defense Health Agency 6025.13, Procedures Manual. Washington, DC: Department of Defense; 2019. [Google Scholar]
- 10. Adler R. Peer reviewed article gender voice issues: voice and communication therapy for transsexual/transgender clients. Voice Speech Rev. 2007;5:293–299. [Google Scholar]
- 11. Cannon Y, Speddlin S, Avera J, et al. Transition, connection, disconnection, and social media: examining the digital lived experiences of transgender individuals. J LGBT Issues Couns. 2017;11:68–87. [Google Scholar]
- 12. Selkie E, Adkins V, Masters E, et al. Transgender adolescents' uses of social media for social support. J Adolesc Health. 2020;66:275–280. [DOI] [PubMed] [Google Scholar]