Abstract
Purpose:
Earlier literature has reported on the utility of diagnostic codes and demographic information for identifying transgender patients. We aim to assess which method identifies the most transgender patients utilizing readily available tools from within the electronic health record (EHR).
Methods:
A de-identified patient database from a single EHR that allows for searching any discrete data point in the EHR was used to query International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) diagnostic codes and demographic data specific to transgender patients from January 2011 to April 2019.
Results:
Demographic data and ICD-10 codes yielded 1494 individual EHRs with transgender-specific data domains. ICD-10 diagnostic codes alone identified 942 (63.05%) unique EHRs. Demographics alone identified 218 (14.59%) unique EHRs. A total of 334 (22.36%) unique EHRs had both ICD-10 and demographic identifiers. Of those identified by transgender-specific demographic data (552), 294 (53.26%) were trans masculine, 215 (38.95%) were trans feminine, and 43 (7.79%) were nonbinary. Of the 552 demographic-identified transgender patients, 141 (25.86%) were identified by a two-part gender identity demographic question.
Conclusions:
ICD-10 diagnostic codes, not demographic data, identified the most transgender patient records, but neither diagnostic codes alone nor demographic data captured the full population. Only 26.36% of the charts identified as transgender patients had both ICD-10 codes and demographic data. We recommend that when identifying transgender populations through EHR domains, a combination of diagnostic codes and demographic data be used. Furthermore, research is needed to optimize disclosure and collection of demographic information for gender minority populations.
Keywords: electronic health records, nonbinary, sexual orientation gender identity data, transgender
Introduction
The collection of sexual orientation and gender identity (SOGI) data is an ongoing effort to improve the health of sexual and gender minorities (SGM) including lesbian, gay, bisexual, transgender, and queer populations. The National Academy of Medicine (formerly Institute of Medicine), the National Healthy People 2020 initiative, and the National Institutes of Health have called for the collection of SOGI data as a means of combating SGM health disparities.1–3 The capacity to collect SOGI data has been certified as a Stage 3 requirement of Promoting Interoperability (previously Meaningful Use) by The Centers for Medicaid and Medicare Services.4 SOGI data collection allows for SGM populations to become clinically visible for epidemiological research and aid the implementation of best clinical care practices for SGM populations.1,5–8
SOGI data research has demonstrated that a majority of patients endorse the importance of asking SOGI questions and believe current best practice answer options allow an accurate reflection of their identity.2 When attitudes toward SOGI data collection were assessed, a minority of patients (10.3%) stated they would be offended by the routine collection of sexual orientation (SO) data.9 However, a majority of documented provider attitudes toward SOGI data collection differ from those of patients. Eighty percent of providers in one study felt that asking SO questions would offend patients and another study showed that 77.8% of clinicians thought patients would refuse SO data collection.9,10 Thus, despite established best practices and documentation of patient willingness to answer and question comprehension, barriers remain to comprehensive SOGI data collection.
One such barrier is workforce training and protocol variations. Variation in how SOGI questions are asked and the presence of local and institutional nondiscrimination protections are also limitations. There is clear consensus that the SOGI data collection must be coupled with comprehensive staff training for safe and effective data collection.2,4,5,11 The importance of training has also been emphasized for transgender patients and gender identity (GI) data collection.1,3,12,13 However, even with training, shortcomings in translation to practice can negatively impact GI data collection.14–16 There is no consensus about when in the workflow SO and/or GI data should be collected, and by whom, complicating SOGI data collection.17,18 And although one study showed that nonverbal self-report was both patient- and provider-preferred method for SO collection,9 multiple methods of SOGI data inclusion into electronic health records (EHRs) have been documented alongside geographic and professional discipline variation in prevalence and methodology of collecting SOGI data.19–21
The need to assess the utility of collected data stems from both the barriers to SOGI data collection described above as well as the dynamic nature of SO and GI data. One recommendation to validate data is to compare data collected before a clinical encounter to data collected during a clinical encounter,20,22 although in some clinical settings these two data collection points may overwrite one another in the EHR. There is a need to ensure that EHRs reflect the percentage of SO and GI categories within the populations they document. For instance, in a text-mining study of home health nursing charts SOGI data, the percentage of lesbian, gay, bisexual, and transgender patients was 0.1% as compared with an estimated U.S. population percentage of 3.8%.21
Using discrete data points in the EHR allows for rapid identification of transgender patients across a large population of patients.23–25 Low cost and efficient means of identifying transgender patients in a large EHR have shown that “transgender status” can be identified through keywords, diagnostic codes, or their combination.23 Roblin et al. note that keyword-based identification alone would have overestimated the number of transgender patients, and that roughly one-third of transgender patients would not be identified with diagnostic codes only.23 Proctor et al. demonstrated that 90% of patients with International Statistical Classification of Diseases and Related Health Problems (ICD)-9 codes specific to medical transitions were able to be validated as transgender patients.25
Our goal was to characterize the utility of different EHR data types to identify transgender individuals. The EHR data types we use are (1) transgender-specific diagnostic codes, and (2) transgender demographic data. Our analysis does not seek to reinforce the use of these terms but rather to assess their efficacy in the current EHR and clinical landscape.
Methods
Chart review
Institutional Review Board approval to access data and abstract data without patient consent was obtained from NYU Langone Health and maintained throughout study period. We performed a chart review study of patients with health care encounters at an urban quaternary care academic hospital system that provides gender affirming surgery, fertility services, pediatric gender affirming care, and a child and adolescent psychiatry mental health gender clinic. We used data derived from the patient EHR. A database with all discrete data points from the EHR was searched using Boolean logic and the time parameters January 2011 to April 2019.26 The database also allows searching for number of distinct patients within a set of search terms, as well as demographic data including age, race, ethnicity, and language spoken. Patient information in the database is de-identified with a proprietary algorithm by a third-party provider, i2b2.26 Patient information is de-identified and dates associated with patient data are randomly offset 1–90 days forward within the database to further de-identify.
Clinical collection and training; information technology/field options
GI demographic data is input into the EHR during or after a clinical encounter by physicians, nurse practitioners, physician assistants, nurses, and mental health care providers with a doctorate. Patients who have a clinical encounter gender-affirming surgical providers may enter their own GI demographic data as well through a survey in the patient portal (MyChart) at any time once they have patient portal access. This is applicable to patients at age 13 years and older who did not provide patient portal proxy access to parents or guardians. For all routes of data input, the GI demographic categories are “sex assigned at birth” (SAB) and “current gender identity.” The most recent input overwrites previous input and no record of changes is retained by the system if data are overwritten.
Our institution provides a one-time online SOGI data collection-specific module training required by all providers with specific submodules based on clinic role (front desk/registration, emergency department, inpatient and procedure area, other clinical roles). Providers are not mandated to ask SOGI questions at our institution. Our institution's EHR is epic, and an institutionally customized SOGI data collection upgrade was instituted in December 2017.
The SAB prompt reads “What was your sex assigned at birth” and one of the following answer options can be chosen: “Male,” “Female,” and “Choose not to disclose.” Of note, legal sex data input is a separate data point used for billing purposes and filled based on patient legal documentation and does not populate the SAB fields. The GI prompt reads “What is your gender identity” and one of the following options can be chosen: male, female, transgender female, transgender male, nonbinary, other, and choose not to disclose. These align with established best practices for asking GI.2 Selecting the response “Other” prompts a free response. The entered text was not visible to our query using the database searched.
All ICD-9 codes, including transgender-specific codes, were converted to equivalent ICD-10 codes in 2015 and included in all queries. Diagnoses entered into the EHR as ICD-9 codes are only visible as their equivalent ICD-10 codes since this conversion. ICD-10 diagnostic codes specific to transgender patients included gender identity disorder (GID) in adolescence and adulthood (F64.0), dual-role transvestism (F64.1), GID unspecified (F64.9), GID of childhood (F64.2), other GID (F64.8), and personal history of sex reassignment (PHSR; Z87.890). F64.0 and F64.1 are grouped as a single output in our query because following ICD-10 code implementation, a provider diagnosis of “gender dysphoria” is mapped to either code in our system for billing purposes. ICD-10 codes that were active, resolved, or deleted were queried. ICD-10 codes generated from admission diagnosis, billing, clinical encounters, and clinician problem lists were all queried. The psychiatric diagnosis of “gender dysphoria” maps to F64.0. The previously utilized psychiatric diagnosis of “gender identity disorder” was mapped to either F64.0, F64.2, or F64.8 before the Diagnostic and Statistical Manual of Mental Disorders, Version 5 publication and adoption.30
Data analysis
All data extraction and analyses were completed in April 2019. The search database tallies the number of unique patients that meet search criteria, thus the results of searches are automatically counted. The database's count results are accurate to plus or minus three unique patients. Percentages were calculated manually.
Results
Two-step gender identity questions: SAB and current gender identity
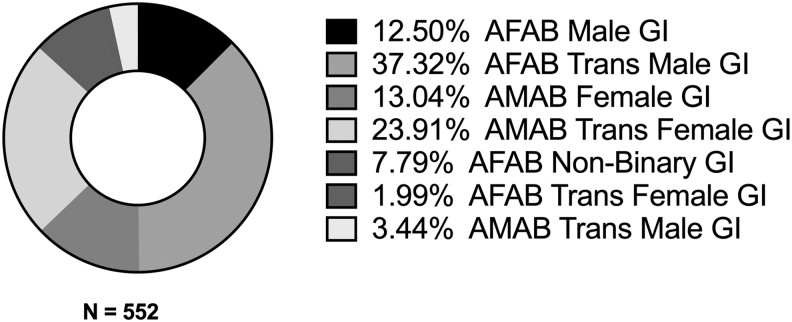
Demographic data identified 552 patients as transgender (Table 1). Of these 552 patients, 294 (53.26%) were trans masculine and 215 (38.95%) were trans feminine. Of these 552 patients, 509 (92.21%) patients were either male or female identified and 43 (7.79%) were nonbinary (Fig. 1). These do not include respondents with “other” input (n=19 total unique patients) for current GI.
Table 1.
Rates of Gender Identity Question Response Options Based on a Two-Step Question (Sex Assigned at Birth and Gender Identity)
| SAB | GI | Patients (N=552) | % of demographic-identified patients (N=552) |
|---|---|---|---|
| Female | Male | 69 | 12.50 |
| Transgender male | 206 | 37.32 | |
| Transgender female | 11 | 1.99 | |
| Nonbinary | 43 | 7.79 | |
| Other | 19 | 3.44 | |
| Choose not to disclose | 166 | 30.07 | |
| Male | Female | 72 | 13.04 |
| Transgender female | 132 | 23.91 | |
| Transgender male | 19 | 3.44 | |
| Nonbinary | 0 | 0 | |
| Other | 0 | 0 | |
| Choose not to disclose | 85 | 15.40 |
GI, gender identity; SAB, sex assigned at birth.
FIG. 1.
Breakdown of demographic-domain identified individuals by binary and nonbinary.
We determined that 141 (25.86%) of these 552 demographic-identified transgender patients were identified by the two-step question (male SAB and female GI, or female SAB and male GI; Fig. 2; Table 1). This refers to patients whose GI did not explicitly state transgender male or female (trans male or trans female), but whose GI (either male or female) was discordant with their SAB.
FIG. 2.
Breakdown of demographic-domain identified individuals by SAB and current GI. AMAB and AFAB designate SAB. AFAB, assigned female at birth; AMAB, assigned male at birth; SAB, sex assigned at birth.
When only charts with completed demographic data (SAB and current GI) are queried (n=70,048), the percentage of patients identified as transgender is 0.784% (552 of 70,048). Binary transgender patients comprised 0.723% (509 of 70,048), and nonbinary transgender patients comprised 0.061% (43 of 70,048).
ICD-10 diagnostic codes
ICD-10 diagnostic codes specific to transgender patients identified 1346 patients. ICD-10 codes specific to mental health diagnosis (F64.0–F64.9) identified 1276 unique patients. The ICD-10 code PHSR (Z87.890) identified 144 unique patients.
The most common ICD-10 diagnostic code was “GID in adolescence and adulthood” (996), followed by “GID, unspecified” (364). “GID of Childhood” identified 104 patients. “Other GID” was the least common ICD-10 GID code (26). (Table 2). Of the 144 individuals with an ICD-10 code of Z87.890, 74 also had an F64 ICD10 (i.e., a psychiatric diagnosis-generated) code and only 70 had just Z87.980.
Table 2.
Breakdown of Subcategories within Transgender-Specific International Statistical Classification of Diseases and Related Health Problems, 10th Revision, Psychiatric Codes
| ICD-10 psychiatric diagnosis codes | N=1276 total | Prevalence (%) within ICD10 psychiatric codes (N=1276) |
|---|---|---|
| GID in adolescence and adulthood (F64.0) or dual role transvestism (F64.1)* | 996 | 78.06% |
| GID of childhood (F64.2) | 104 | 8.15% |
| GID unspecified (F64.9) | 364 | 28.53% |
| Other GID (F64.8) | 26 | 2.04% |
F64.0 and F64.1 are grouped because a provider diagnosis of “gender dysphoria” maps to either code in our system for billing purposes.
GID, gender identity disorder; ICD-10, International Statistical Classification of Diseases and Related Health Problems, 10th Revision.
Comparing demographics and ICD-10 diagnostic codes
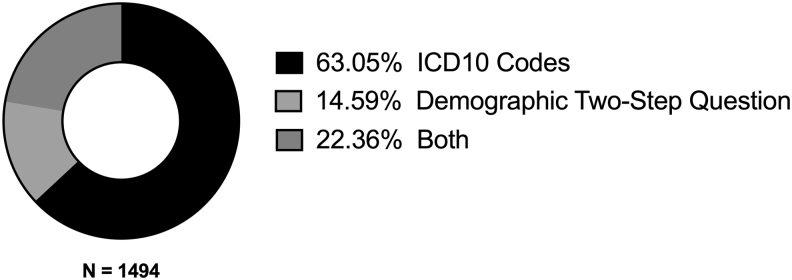
In total, 1494 individual EHRs with transgender demographics and/or ICD10 diagnostic codes were identified. ICD-10 diagnostic codes alone identified 942 (63.05%) unique EHRs. Demographics alone identified 218 (14.59%) unique EHRs. A total of 334 (22.36%) unique EHRs had both ICD-10 and demographic identifiers.
Discussion
The analysis seeks to characterize the utility of different domains within an EHR to identify medical records of patients with transgender identity or experience (henceforth transgender patients). The routine clinical collection of GI data in a two-step question format has been established as best practice,2 but to our knowledge no prior research has sought to describe collected data's utility and reliability in identifying transgender patients. This novel step in data analysis is critical to implementing these data as a tool for epidemiological study and improvement of clinical practice.3,5,20
ICD-10 diagnostic codes and demographic data were identified as EHR domains that had input specific to transgender patients in our system. ICD-10 diagnostic codes were the most reliable EHR domain, with 63.05% of transgender charts identified by ICD10 codes alone and another 22.36% identified by a combination of ICD-10 codes and demographics (Fig. 3). Demographic data alone identified 14.59% of all transgender patient charts. Overall, the total percentage of the transgender population estimated by demographic questions alone within our EHR (0.784%) is higher than recent national population estimates (0.58%) of the transgender population, and it is consistent with population percentage for younger age demographics (0.7% 13–17 years old, 0.7% 18–24 years old).28,29
FIG. 3.
EHR domain category and combination breakdown used to identify transgender charts. EHR, electronic health record.
The ICD-10 diagnostic codes used here have been shown to have a high rate of specificity to transgender patients.23–25 Not every transgender person who obtains medical care generates a transgender-specific diagnostic code. Thus, in theory, there should be more individuals identified by demographic data than diagnostic codes. Of note, only 22.36% of patients were identified as transgender by both ICD-10 codes and demographic data. And more than half (63.05%) of the cohort identified here was missing demographic data that identified them as a gender minority. This demonstrates that, in our EHR system and workflow input, demographic data are not routinely or accurately entered for all transgender patients. Even in a large academic health care setting with GI best practices and a staff training online module, demographic data have not yet reached its potential to be the most sensitive EHR domain to identify transgender patients.
To our knowledge we are the first to quantify the utility of the two-step question for GI by estimating the number of patients that would not be legible as having transgender experience without having two demographic questions (SAB, GI) by which to more accurately derive transgender experience. We determined that 25.86% of demographic-identified transgender patients were identified by the two-step question (assigned male at birth, female GI; assigned female at birth, male GI). Thus, we believe in the absence of a two-step question for GI data, roughly a quarter of transgender patients would not be clinically visible. This demonstrates the critical importance of implementing best practices for GI data collection to provide clinical standards of care to all patients and address the stark health disparities facing transgender patients, which are in part fostered by EHR systems.1
The two-step GI question also allowed us to characterize the number of nonbinary transgender versus binary transgender patients (92.21% vs. 7.79%). Nonbinary patients have been shown to have worse clinical outcomes,28 and we demonstrate the utility of the two-step question in disaggregating this population for the purpose of addressing its unique health disparities. It is likely our nonbinary population is underestimated given that GI responses of “other” were considered separately from nonbinary. The free text responses of patient and provider who input “other” as a response were not available in this query. It is possible terms entered could be considered under the nonbinary umbrella; however, this is speculative without free text analysis. To our knowledge, there are no data specifically studying GI question response attitudes of nonbinary populations, but we presume this population may select binary options to simplify insurance billing.
Our analysis also reveals the limitations of the current best practice two-step question for GI. The SAB demographic domain is designed to capture patient's anatomical baseline and serve as a basis for exploring an organ inventory, as described in best practices.1 About 1.99% of demographically identified transgender patients had female SAB and transgender female GI, and 3.44% had male SAB and transgender male GI (Table 1). In our analysis, these patients were included as binary (rather than nonbinary), given that nonbinary was another explicit option. A few reasons for these data may exist, including data entry errors either owing to workflow interface or lack of staff understanding of question response options. We believe that for the patients whose data accurately reflects their identities, they are most likely rejecting the notion of biologically determined sex. This prompts the need to continually examine best practice response options to maximize data accuracy and patient comfort.
Changes in policy and insurance landscapes can impact the utility of ICD codes in identifying clinical populations. This underscores the need for increasing future demographic data collection and understanding the potential utility of demographic data as compared with other EHR categories that can potentially identify transgender patients.
Limitations
Our analysis conflates medical diagnoses and/or conditions with a dynamic identity category based on gender. Of note, the diagnostic categories are not synonymous with the social identity categories captured by the demographic questions, and thus scope of our analysis' utility is limited to optimizing clinical care for patients of transgender experience.
The number of transgender patients estimated here is likely an underestimate. Because not every transgender patient has an ICD-10 diagnostic code and demographic data as a category was less sensitive then ICD-10 codes in identifying transgender patients, we believe there are transgender patients without ICD-10 codes who lack demographic data that identifies them as transgender. Thus, our analysis of transgender data percentage and demographics may be missing a significant portion of patients, emphasizing the need for increased GI data collection implementation. An analysis of this type is also limited by the discordance between ICD-10 codes and most recent Diagnostic and Statistical Manual language,27 a gap that continues to widen with pending ICD-11 code revisions that will move transgender-related codes out of conditions of mental health and into those of sexual health.30
In addition, our conclusions are limited in scope to large academic health centers that provide gender-affirming surgery, pediatric gender-affirming care, and a child and adolescent psychiatry mental health gender clinic. It is likely that the utility of diagnostic codes at health care institutions that do not offer these clinical services may vary, thus limiting the applicability of our findings. The reality of variation in clinical services available to transgender patients and possible variation in ICD-10 diagnostic code usage based on insurance and billing practices further underscores the need to improve the reliability and accuracy of demographic data as the standard for identifying transgender patients in EHRs.
Conclusions
Although demographic data are the ideal way to identify transgender patients, we demonstrate the utility of multiple data points—demographic data and diagnostic codes—to identify a transgender population. We demonstrate the utility of a two-step question in identifying transgender patients whose GI is discordant from SAB, regardless of GI label including “transgender.”
Acknowledgments
The authors thank Joseph Nicholson for his assistance with the literature search.
Abbreviations Used
- AFAB
assigned female at birth
- AMAB
assigned male at birth
- EHR
electronic health record
- GI
gender identity
- GID
gender identity disorder
- ICD
International Statistical Classification of Diseases and Related Health Problems
- PHSR
personal history of sex reassignment
- SAB
sex assigned at birth
- SGM
sexual and gender minorities
- SO
sexual orientation
- SOGI
sexual orientation and gender identity
Author Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
Cite this article as: Dubin S, Cook T, Liss A, Doty G, Moore K, Greene R, Radix A, Janssen A (2022) Comparing electronic health record domains' utility to identify transgender patients, Transgender Health 7:1, 78–84, DOI: 10.1089/trgh.2020.0069.
References
- 1. Deutsch MB, Buchholz D. Electronic health records and transgender patients—practical recommendations for the collection of gender identity data. J Gen Intern Med. 2015;30:843–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cahill S, Singal R, Grasso C, et al. Do ask, do tell: high levels of acceptability by patients of routine collection of sexual orientation and gender identity data in four diverse American community health centers. PLoS One. 2014;9:e107104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Institute of Medicine Board on the Health of Select Populations. The National Academies Collection: Reports funded by National Institutes of Health. In: Collecting Sexual Orientation and Gender Identity Data in Electronic Health Records: Workshop Summary. Washington, DC: National Academies Press (US) National Academy of Sciences, 2013. [PubMed] [Google Scholar]
- 4. Cahill SR, Baker K, Deutsch MB, et al. Inclusion of sexual orientation and gender identity in stage 3 meaningful use guidelines: a huge step forward for LGBT health. LGBT Health. 2016;3:100–102. [DOI] [PubMed] [Google Scholar]
- 5. Cahill S, Makadon H. Sexual orientation and gender identity data collection in clinical settings and in electronic health records: a key to ending LGBT health disparities. LGBT Health. 2014;1:34–41. [DOI] [PubMed] [Google Scholar]
- 6. Deutsch MB, Keatley J, Sevelius J, Shade SB. Collection of gender identity data using electronic medical records: survey of current end-user practices. J Assoc Nurses AIDS Care. 2014;25:657–663. [DOI] [PubMed] [Google Scholar]
- 7. Donald C, Ehrenfeld JM. The opportunity for medical systems to reduce health disparities among lesbian, gay, bisexual, transgender and intersex patients. J Med Syst. 2015;39:178. [DOI] [PubMed] [Google Scholar]
- 8. Reisner SL, Deutsch MB, Bhasin S, et al. Advancing methods for US transgender health research. Curr Opin Endocrinol Diabetes Obes. 2016;23:198–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Haider AH, Schneider EB, Kodadek LM, et al. Emergency department query for patient-centered approaches to sexual orientation and gender identity: the EQUALITY Study. JAMA Intern Med. 2017;177:819–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maragh-Bass AC, Torain M, Adler R, et al. Risks, benefits, and importance of collecting sexual orientation and gender identity data in healthcare settings: a multi-method analysis of patient and provider perspectives. LGBT Health. 2017;4:141–152. [DOI] [PubMed] [Google Scholar]
- 11. Cahill S, Makadon HJ. Sexual orientation and gender identity data collection update: U.S. government takes steps to promote sexual orientation and gender identity data collection through meaningful use guidelines. LGBT Health. 2014;1:157–160. [DOI] [PubMed] [Google Scholar]
- 12. Maragh-Bass AC, Torain M, Adler R, et al. Is it okay to ask: transgender patient perspectives on sexual orientation and gender identity collection in healthcare. Acad Emerg Med. 2017;24:655–667. [DOI] [PubMed] [Google Scholar]
- 13. Tamar-Mattis S, Gamarel KE, Kantor A, et al. Identifying and counting individuals with differences of sex development conditions in population health research. LGBT Health. 2018;5:320–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Safer JD, Coleman E, Feldman J, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016;23:168–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goldhammer H, Maston ED, Kissock LA, et al. National findings from an LGBT healthcare organizational needs assessment. LGBT Health. 2018;5:461–468. [DOI] [PubMed] [Google Scholar]
- 16. Dichter ME, Ogden SN, Scheffey KL. Provider perspectives on the application of patient sexual orientation and gender identity in clinical care: a qualitative study. J Gen Intern Med. 2018;33:1359–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dunne MJ, Raynor LA, Cottrell EK, Pinnock WJA. Interviews with patients and providers on transgender and gender nonconforming health data collection in the electronic health record. Transgend Health. 2017;2:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. German D, Kodadek L, Shields R, et al. Implementing sexual orientation and gender identity data collection in emergency departments: patient and staff perspectives. LGBT Health. 2016;3:416–423. [DOI] [PubMed] [Google Scholar]
- 19. Cathcart-Rake EJ, Zemla T, Jatoi A, et al. Acquisition of sexual orientation and gender identity data among NCI Community Oncology Research Program practice groups. Cancer. 2019;125:1313–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. AHIMA Work Group. Improved patient engagement for LGBT populations: addressing factors related to sexual orientation/gender identity for effective health information management. J AHIMA. 2017;88:34–39. [PubMed] [Google Scholar]
- 21. Bjarnadottir RI, Bockting W, Yoon S, Dowding DW. Nurse documentation of sexual orientation and gender identity in home healthcare: a text mining study. Comput Inf Nurs. 2019;37:213–221. [DOI] [PubMed] [Google Scholar]
- 22. Grasso C, Keuroghlian AS, McDowell MJ, Goldhammer H. Planning and implementing sexual orientation and gender identity data collection in electronic health records. J Am Med Inform Assoc. 2018;26:66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Roblin D, Barzilay J, Tolsma D, et al. A novel method for estimating transgender status using electronic medical records. Ann Epidemiol. 2016;26:198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kauth MR, Shipherd JC, Lindsay J, et al. Access to care for transgender veterans in the veterans health administration: 2006–2013. Am J Public Health. 2014;104:S532–S534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Proctor K, Haffer SC, Ewald E, et al. Identifying the transgender population in the medicare program. Transgend Health. 2016;1:250–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Murphy SN, Mendis ME, Berkowitz DA, et al. Integration of clinical and genetic data in the i2b2 architecture. AMIA Annu Symp Proc AMIA Symp. 2006;2006:1040. [PMC free article] [PubMed] [Google Scholar]
- 27. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC: American Psychiatric Association, 2013. [Google Scholar]
- 28. Herman J, Flores A, Brown T, et al. Age of individuals who identify as transgender in the United States. TheWilliamsInstitute, 2017. https://williamsinstitute.law.ucla.edu/wp-content/uploads/TransAgeReport.pdf Accessed September 15, 2019.
- 29. Flores A, Herman J, Gates G, Brown T. How Many Adults Identify as Transgender in the United States? Los Angeles, CA: The Williams Institute, 2016. [Google Scholar]
- 30. World Health Organization. ICD-11 International Classification of Diseases for Mortality and Morbidity Statistics Eleventh Revision. 2019. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/411470068/mms/unspecified Accessed September 19, 2019.