Abstract
Autoantibodies can be used in the early diagnosis and treatment of atherosclerosis-related diseases. Using ProtoArray® screening of samples from patients with atherosclerosis, the present study identified thiosulfate sulfurtransferase-like domain-containing 2 (TSTD2) as a novel atherosclerosis antigen. The serum TSTD2 antibody levels were then quantified using an amplified luminescent proximity homogeneous assay-linked immunosorbent assay. This demonstrated the levels of TSTD2 antibodies (TSTD2-Abs) to be significantly higher in patients with acute cerebral infarction or chronic kidney disease than in healthy donors. The TSTD2-Ab levels were also found to be higher in males, older adults, smokers, in those who consumed alcohol regularly, and in those with hypertension. Furthermore, Spearman's rank correlation analysis revealed TSTD2-Ab levels to be strongly associated with measures of atherosclerosis severity, including plaque scores, intima-media thickness of the carotid artery and the cardio-ankle vascular index. Thus, TSTD2-Abs may thus be a promising novel biomarker for atherosclerosis-related cerebral infarction and kidney disease.
Keywords: autoantibody, thiosulfate sulfurtransferase-like domain-containing 2, atherosclerosis, acute cerebral infarction, chronic kidney disease
Introduction
Ischemic stroke is one of the most common vascular disorders worldwide and, despite notable advancements being made in treatments and diagnostic imaging techniques, it is still associated with high mortality and morbidity rates (1,2). Chronic kidney disease (CKD) is also a serious public health concern with a high incidence rate (3). Atherosclerosis is the main cause of both ischemic stroke and CKD (4,5). The immune response to atherosclerosis causes the production of autoantibodies in the sera of patients (6). These can potentially be used as biomarkers for preventive diagnosis and for the identification of the disease type of atherosclerosis-related diseases. Recent studies have demonstrated that serum autoantibodies play a critical role in various diseases (7,8). In previous studies, the authors identified several autoantibodies associated with ischemic stroke, including RPA2, PDCD11, ATP2B4, BMP-1, MMP1, CBX1, DNAJC2, AP3D1, DIDO1 and SERPINE 1 (9-15). These may all be applied to diagnosis and treatment. The present study examines the use of the anti-thiosulfate sulfurtransferase-like domain-containing 2 (TSTD2) autoantibody as a novel biomarker for atherosclerosis-related cerebral infarction and CKD in the sera of patients with atherosclerosis.
Materials and methods
Patient samples
Serum samples were obtained from patients who suffered an ischemic stroke and from healthy donors (HDs). The present study analyzed 684 serum samples, including 275 from patients with acute ischemic stroke (AIS), 300 from patients with CKD and 109 from HDs. The AIS group consisted of 196 patients with acute cerebral infarction (aCI) and 79 patients with transient ischemic attack (TIA). The serum samples of the patients with aCI and TIA were collected at Chiba Prefectural Sawara Hospital, Chiba Rosai Hospital, and Chiba Aoba Municipal Hospital. The aCI samples were collected within 2 weeks of the diagnosis of atherothrombotic brain infarction. The median (range) of age in years of the HD, aCI and TIA subjects were 60 (45-90), 77 (58-85) and 73 (26-90), respectively. The subject information of the Sawara stroke cohort is summarized in Table SI.
The CKD serum samples were obtained from the Kumamoto cohort (16,17), which included 145 samples from patients with type-1 (diabetic kidney disease), 32 with type-2 (nephrosclerosis) and 123 with type-3 (glomerulonephritis) CKD. The HD serum samples were collected from the Chiba Prefectural Sawara Hospital, and Port Square Kashiwado Clinic (Chiba, Japan). The HDs were individuals with no history of ischemic stroke or CKD, and no abnormalities upon a physical examination or brain magnetic resonance imaging. Those with autoimmune diseases were excluded from the study. The median (range) of age in years of the HDs, type-1 CKD, type-2 CKD and type-3 CKD subjects were 57 (44-76), 65 (38-93), 79 (54-90) and 63 (28-89), respectively. The subject information of the CKD cohort is summarized in Table SII. Each sample was centrifuged at 3,000 x g for 10 min at 4˚C, and the supernatant was stored at -80˚C until use. Repeated thawing and freezing were avoided.
The present study was conducted in accordance with the principles of the 1913 revision of the Declaration of Helsinki and with the approval of the Ethical Review Committee of Chiba University, Graduate School of Medicine and cooperative hospitals (approval no. 2018-320). The research on recombinant DNA was conducted with the permission of the Graduate School of Medicine, Chiba University, and following Japanese regulations. Each participant provided written informed consent to participation and publication.
ProtoArray® screening
The initial screening was performed using ProtoArray® Human Protein Microarrays v.4.0 (Thermo Fisher Scientific, Inc.), which are loaded with 9,480 proteins, as previously described (18). A total of 20 serum samples (10 each from HDs and patients with atherosclerosis) were used to select antigenic proteins specifically recognized by serum immunoglobin G (IgG) antibodies. The results were analyzed using Prospector (Thermo Fisher Scientific, Inc.) software based on M-statistics. When comparing the two groups, a positive cutoff value corresponds to relative fluorescence units above the M-statistic signal threshold established for each antigenic protein. The percentage of the samples in each group that exhibited an immune response above the cutoff value was determined and the P-value for the significance of the difference between the two groups was calculated, as previously described (19).
Expression and purification of glutathione-S-transferase-tagged antigenic proteins
The expression plasmid of the TSTD2 protein tagged with glutathione-S-transferase (GST) was constructed by recombining the cDNA sequence into a pGEX-4T-1 (Cytiva) plasmid vector. The competent Escherichia coli (E. coli) BL-21 cells was obtained from Nippon Gene, Co. Ltd. pGEX-4T-1-TSTD2 (0.2 µg in 1 µl) was mixed with the BL-21 cells (5x108 cells in 20 µl), incubated for 5 min at 0˚C, incubated for 45 sec at 42˚C, and plated on agar-Luria broth plate containing 50 µg/ml ampicillin according to the instructions of Nippon Gene, Co. Ltd. The transformed cells were cultured in 200 ml Luria broth and treated with 0.1 mM isopropyl β-D-1-thiogalactopyranoside (IPTG) reagent for 3 h. The cells were then harvested, washed with phosphate-buffered saline (PBS), and sonicated in BugBuster Master Mix (Merck KGaA). The cell lysates were centrifuged at 13,000 x g for 10 min at 4˚C, and the precipitates containing recombinant proteins were dissolved in 8 M urea in TED buffer [50 mM Tris-HCl (pH 8.0), 1 mM ethylenediaminetetraacetic acid (EDTA) and 1 mM dithiothreitol]. The samples were then sequentially dialyzed in steps of 2 h each against 4 and 2 M urea in TED buffer. The samples were then dialyzed against TED buffer for 15 h to remove the urea and centrifuged at 10,000 x g for 30 min at 4˚C. The GST-fused recombinant protein recovered in the supernatant fraction was directly purified by affinity chromatography using glutathione-Sepharose (Cytiva) according to the manufacturer's instructions. The purified protein was filtered using Amicon Ultra-15 (Merck) centrifugal filter equipment to concentrate it (9,20-22). The concentration of the purified protein was quantified by Bradford method using Bio-Rad Protein assay (#5000001JA, Bio-Rad Laboratories, Inc.). The proteins were subjected to sodium dodecyl sulfate-polyacrylamide (11%) gel electrophoresis (SDS-PAGE) followed by staining with 0.05% Coomassie Brilliant Blue (Nakalai Tesque, Inc.) in 10% methanol (FUJIFILM Wako Pure Chemical Corporation) and 50% methanol (FUJIFILM Wako Pure Chemical Corporation) for 1 h at 25˚C and destaining in 7.5% acetic acid and 5% methanol for longer than 16 h at 25˚C. The purity was calculated using Personal Density Scanning Imager (Molecular Dynamics, Inc.).
Western blot analysis
The GST and GST fusion proteins (0.3 µg) were separated by SDS-PAGE (11% polyacrylamide) and transferred to nitrocellulose membranes (cat. no. 1620112, Advantec Toyo Kaisha, Ltd.). The membranes were blocked with blocking solution [0.5% skim milk powder in a buffer consisting of 20 mM Tris-HCl (pH 7.6), 137 mM NaCl, and 0.1% Tween-20], and subjected to specific primary antibodies, i.e., 1:5,000-diluted antibodies against GST (cat. no. 600-101-200, Rockland Immunochemicals, Inc.) or 1:1,000-diluted sera from subjects. Following incubation with 1:30,000-diluted horseradish peroxidase (HRP)-conjugated secondary antibodies [donkey anti-goat (cat. no. sc-2056), or anti-human IgG (cat. no. sc-2453); both from Santa Cruz Biotechnology, Inc.], immunoreactivity was measured using Immobilon Western HRP Substrate (Merck KGaA) and LuminoGraph II (ATTO Co, Ltd.). The results were detected as previously described (21,23).
Quantification of antibodies using amplified luminescent proximity homogenous assay-linked immunosorbent assay (AlphaLISA)
AlphaLISA was used for the quantitative measurement of serum antibodies to purified proteins. Subsequently, 2.5 µl serum diluted 1:100 in AlphaLISA buffer [25 mM hydroxyethyl piperazine ethane sulfonic acid (Thermo Fisher Scientific, Inc.), pH 7.4, 0.1% casein (Merck KGaA), 0.5% Triton X-100 (FUJIFILM Wako Pure Chemical Corporation), 1 mg/ml dextran-500 (Merck KGaA) and 0.05% Proclin-300 (Merck KGaA)] and 2.5 µl GST or GST-fused TSTD2 proteins (10 µg/ml) was placed in 384-well microtiter plates (white opaque OptiPlate, PerkinElmer, Inc.) and used for the experiments. The reaction mixture was incubated at room temperature for 6-8 h, after which anti-human IgG-conjugated acceptor beads (2.5 µl, 40 µg/ml; PerkinElmer, Inc.) and glutathione-conjugated donor beads (2.5 µl, 40 µg/ml; PerkinElmer, Inc.) were added. The mixture was incubated for 7-21 days at room temperature in the dark. Chemiluminescence was read on an EnSpire Alpha (PerkinElmer, Inc.) microplate reader (PerkinElmer, Inc.), as previously described (13,22).
Statistical analyses
The Dunn's multiple comparison test following a Kruskal-Wallis test was used to analyze continuous variables using JMP Pro 14.2.0 software (SAS Institute Inc.). Correlations between TSTD2 antibody levels and each clinical and demographic parameter were evaluated using Spearman's correlation analysis. The cutoff TSTD2 antibody level for predicting ischemic stroke was assessed to maximize the sum of the sensitivity and specificity rates using a receiver operating characteristic (ROC) curve analysis. Clinical and demographic factors, including sex, age, smoking and alcohol drinking habits, and the presence of medical conditions such as hypertension, diabetes, cardiovascular disease, hyperlipidemia and obesity [based on body mass index (BMI)] were examined in relation to the serum TSTD2 antibody levels using a Mann-Whitney U test. Spearman's correlation analyses, ROC analysis and analysis using the Mann-Whitney U test were performed using GraphPad Prism 5 software (GraphPad, Inc.). All the tests were two-tailed, and a P-value <0.05 was considered to indicate a statistically significant difference.
Results
Identification of the TSTD2 antibody using ProtoArray screening
The screening of ProtoArray® loaded with 9,480 proteins identified TSTD2 antibodies (accession no. NM_139246.3) in eight of the 10 serum samples from patients with atherosclerosis and in two of the 10 serum samples from the HDs. The expression of GST-fused TSTD2 protein was successively induced in E. coli containing pGEX-4T-1-TSTD2 following treatment with IPTG (Fig. 1, lanes 1 and 2 of the CBB blot). Affinity-purified GST and GST-TSTD2 proteins were also subjected to SDS-PAGE followed by staining with Coomassie Brilliant Blue (Fig. 1, lanes 3 and 4 of the CBB blot). The purity of GST-TSTD2 protein was ~80%.
Figure 1.
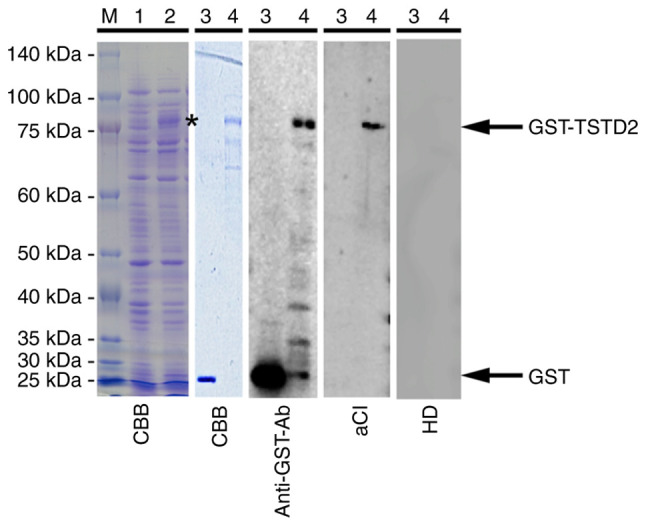
Western blot analysis. Escherichia coli BL-21 cells containing the pGEX-4T-1-TSTD2 were treated without (lane 1) or with 0.1 mM isopropyl β-D-1-thiogalactopyranoside (lane 2) for 3 h at 42˚C in Luria broth. The whole cell extract was electrophoresed with sodium dodecyl sulfate-polyacrylamide (11%) gels followed by staining with CBB. The asterisk represents GST-tagged full-length TSTD2 (GST-TSTD2) protein in the whole cell extract. Affinity-purified GST (lane 3) and GST-TSTD2 proteins (lane 4) were electrophoresed similarly and then stained with CBB or used for western blotting with anti-GST antibodies or the serum antibodies of a patient with aCI and those of a HD. Electrophoresed molecular weight markers are also shown in lane M, with the sizes shown on the left. CBB, Coomassie Brilliant Blue; GST, glutathione-S-transferase; aCI, acute cerebral infarction; HD, healthy donor.
Elevated TSTD2 antibody levels in patients with AIS
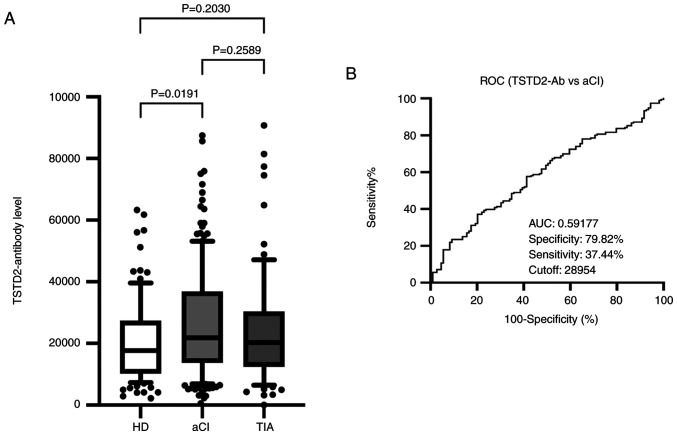
To investigate the association between TSTD2 autoantibodies and AIS, serum TSTD2 antibody levels were examined in the HD, aCI and TIA groups using AlphaLISA. Compared with the HD group, the aCI group exhibited significantly higher TSTD2 antibody levels (P=0.0191); however, no significant difference was observed between the TIA and HD groups (P=0.2030), or between the TIA and aCI groups (P=0.2589) (Fig. 2A).
Figure 2.
Comparison of the serum levels of TSTD2 antibodies in HDs, and in patients with aCI and TIA. (A) The figure illustrates the levels of serum TSTD2-Abs examined using amplified luminescence proximity homogeneous assay (Alpha)-linked immunosorbent assay. Antibody levels are represented by Alpha photon counts and shown in a box-whisker plot. The horizontal lines represent medians, and the boxes represent the 25 and 75th percentiles. The whiskers represent the 10 and 90th percentiles, and the dots represent outliers. P-values were calculated using the Kruskal-Wallis test. A ROC curve analysis was performed to assess the ability of serum TSTD2-Abs to detect aCI. (B) The numbers in the graph are the AUC, specificity, sensitivity and cutoff values for the marker levels. TSTD2, thiosulfate sulfurtransferase-like domain-containing 2; TSTD2-Ab, TSTD2 antibody; HD, healthy donor; aCI, acute cerebral infarction; TIA, transient ischemic attack; ROC, receiver operating characteristic; AUC, area under the curve.
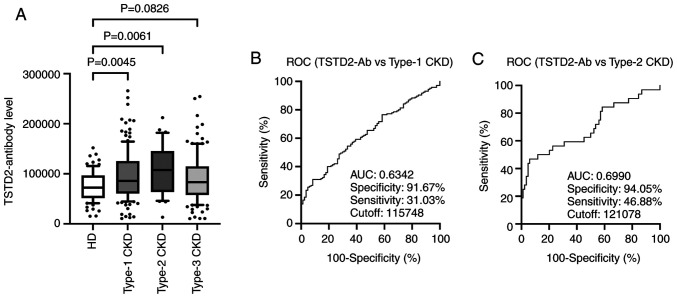
Elevation of TSTD2 antibody levels in patients with CKD
The present study then examined antibody levels in the sera of patients with CKD. This group was divided into three subgroups according to CKD type as follows: Type-1 (diabetic kidney disease), type-2 (nephrosclerosis) and type-3 (glomerulonephritis). The type-1 and type-2 CKD subgroups had significantly higher serum TSTD2-Ab levels than the HDs. The type-3 CKD subgroup exhibited higher levels than the HD group, although the difference was not significant (P=0.0826) (Fig. 3A).
Figure 3.
Comparison of serum TSTD2 antibody levels in HDs, and patients with type-1, -2 and -3 CKD. (A) Serum TSTD2 antibody levels were quantified using amplified luminescence proximity homogeneous assay-linked immunosorbent assay and compared between the HD group and the type-1 (diabetic kidney disease), type-2 (nephrosclerosis) and type-3 (glomerulonephritis) CKD subgroups. TSTD2 antibody levels are depicted in a box-whisker plot. (B and C) The TSTD2 antibody levels were analyzed using a ROC curve to compare type-1 and type-2 CKDs. The numbers in the graphs indicate the AUC, specificity, sensitivity and cutoff values. TSTD2, thiosulfate sulfurtransferase-like domain-containing 2; CKD, chronic kidney disease; ROC, receiver operating characteristic; AUC, area under the curve.
ROC analysis of TSTD2 antibody levels in patients with aCI and type-1 and type-2 CKDs
A ROC analysis of the TSTD2 antibody levels in aCI and type-1 and type-2 CKDs was also performed. The cutoff values for these levels in aCI and type-1 and type-2 CKDs were 28,954 (sensitivity, 37.4%; specificity, 79.8%), 11,5748 (sensitivity, 31.03%; specificity, 91.67%) and 12,1078 (sensitivity, 46.88%; specificity, 94.05%), respectively (Figs. 2B and 3B and C). The area under the curve (AUC) values were 0.592, 0.6342 and 0.6990 for aCI and type-1 and type-2 CKDs, respectively (Figs. 2B, 3B and C). The AUC value for type-2 CKD was higher than that for type-1 CKD, although the sample numbers examined diffed.
Analysis of correlations between TSTD2 antibody levels and clinical and demographic parameters in the stroke cohort
Spearman's correlation analyses to identify the correlations between the TSTD2 antibody levels, and the clinical and demographic variables in the Sawara stroke cohort. The patient information is presented in Table SI, which included hematological examination results, smoking status and alcohol consumption status, age, sex, height, weight, BMI and intima-media thickness (IMT) of the carotid artery. Positive correlations were found between the TSTD2 antibody levels and maximum IMT (Rho=0.1703, P=0.0028), C-reactive protein levels (Rho=0.1395, P=0.0221), blood sugar (Rho=0.1542, P=0.039), smoking duration (Rho=0.1938, P=0.0002) and alcohol consumption frequency (Rho=0.1174, P=0.0241). Negative correlations were found between the TSTD2 antibody levels and cholinesterase levels (Rho=-0.1960, P=0.0009), albumin levels (Rho=-0.1727, P=0.0007) and total cholesterol (Rho=-0.1567, P=0.0046) (Table I).
Table I.
Spearman's correlation analysis for the correlation between the serum TSTD2 antibody levels and clinical features of patients with aCI.
| Variables | Spearman's rank correlation coefficient (Rho) | P-value |
|---|---|---|
| Age, years | 0.0954 | 0.0624 |
| BMI | 0.0193 | 0.7075 |
| Maximum IMT | 0.1703 | 0.0028 |
| AST | 0.0054 | 0.9161 |
| ALT | -0.0428 | 0.4051 |
| ALP | 0.0647 | 0.228 |
| LDH | 0.086 | 0.0986 |
| tBil | -0.0226 | 0.6642 |
| CHE | -0.1960 | 0.0009 |
| γ-GTP | 0.0586 | 0.2677 |
| TP | -0.0910 | 0.0797 |
| ALB | -0.1727 | 0.0007 |
| BUN | 0.034 | 0.5082 |
| Creatinine | -0.0079 | 0.8783 |
| eGFR | -0.0124 | 0.8154 |
| UA | 0.069 | 0.2558 |
| AMY | -0.0764 | 0.2537 |
| T-CHO | -0.1567 | 0.0046 |
| HDL-C | -0.0673 | 0.3106 |
| TG | -0.1109 | 0.0814 |
| Na | -0.0139 | 0.7877 |
| K | -0.0994 | 0.054 |
| Cl | -0.0989 | 0.055 |
| CRP | 0.1395 | 0.0221 |
| WBC | 0.0905 | 0.0783 |
| RBC | -0.0673 | 0.1912 |
| HGB | -0.0564 | 0.2737 |
| HCT | -0.0626 | 0.2243 |
| PLT | -0.0481 | 0.3503 |
| BS | 0.1542 | 0.0039 |
| HbA1c | -0.0250 | 0.6695 |
| Smoking duration (years) | 0.1938 | 0.0002 |
| Frequency of alcohol consumption (times/week) | 0.1174 | 0.0241 |
A correlation analysis was performed to identify the correlation between TSTD2 antibody levels and the clinical features of patients with ischemic stroke. Correlation coefficients (Rho) and P-values were calculated using Spearman's correlation analysis. Significant correlations (P<0.05) are marked in bold font. aCI, acute cerebral infarction; TSTD2, thiosulfate sulfurtransferase-like domain-containing 2; BMI, body mass index; IMT, intima-media thickness; AST, aspartate aminotransferase; ALT, alanine aminotransferase; ALP, alkaline phosphatase; LDH, lactate dehydrogenase; tBil, total bilirubin; CHE, choline esterase; γ-GTP, γ-glutamyl transpeptidase; TP, total protein; ALB, albumin; BUN, blood urea nitrogen; eGFR, estimated glomerular filtration rate; UA, uric acid; AMY, amylase; T-CHO, total cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglyceride; CRP, C-reactive protein; WBC, white blood cell count; RBC, red blood cell count; HCT, hematocrit; PLT, platelet count; BS, blood sugar; HbA1c, hemoglobin A1c.
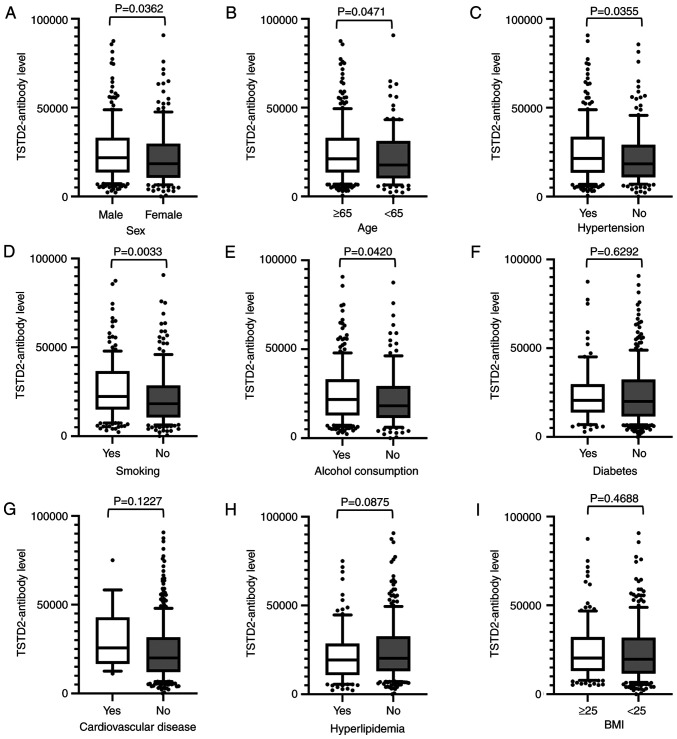
Antibody levels were compared between two groups using the Mann-Whitney U test using the cutoff values determined by ROC analysis, and were found to be significantly higher in males than in females (P=0.036), those who were ≥65 years of age compared with those <65 of age (P=0.047), in those with hypertension compared with those without this condition (P=0.036), in smokers compared with non-smokers (P=0.003), and in those who consumed alcohol compared with those who did not (P=0.042) (Fig. 4).
Figure 4.
Associations between TSTD2 antibody levels and clinical and demographic variables in the serum of acute cerebral infarction patients. The associations between TSTD2 antibody levels and (A) sex, (B) age, (C) hypertension, (D) smoking status, (E) alcohol consumption, (F) diabetes, (G) cardiovascular disease, (H) hyperlipidemia, and (I) BMI were examined in the acute cerebral infarction cohort. The TSTD2 antibody levels obtained using amplified luminescence proximity homogeneous assay-linked immunosorbent assay are shown in box-whisker plots. The P-values were calculated using Mann-Whitney U tests. TSTD2, thiosulfate sulfurtransferase-like domain-containing 2; BMI, body mass index.
Analysis of correlations between TSTD2 antibody levels and clinical and demographic parameters in the CKD cohort
Subsequently, Spearman's correlation analysis was performed to identify the correlations between the serum TSTD2 antibody levels and the clinical features of patients in the Kumamoto CKD cohort. The patient information is presented in Table SII. Positive correlations were found between TSTD2 antibody levels and plaque scores (Rho=0.1608, P=0.0056), maximum IMT (Rho=0.1266, P=0.0295), cardio-ankle vascular index (CAVI) of the right side (Rho=0.1430, P=0.0165) and the left side (Rho=0.1472, P=0.0132), parathyroid hormone (Rho=0.1539, P=0.0076), aspartate aminotransferase (Rho=0.1654, P=0.0041), lactate dehydrogenase (Rho=0.1749, P=0.0024), and C-reactive protein (Rho=0.1638, P=0.0044) levels. A negative correlation was found between TSTD2 antibody levels and BMI (Rho=-0.1509, P=0.0089) (Table II).
Table II.
Spearman's correlation analysis of the correlation between the serum TSTD2 antibody levels and clinical features of patients with CKD.
| Variables | Spearman's rank correlation coefficient (Rho) | P-value |
|---|---|---|
| Age, years | 0.0545 | 0.3468 |
| Height | -0.0044 | 0.9401 |
| Weight | -0.1152 | 0.0461 |
| BMI | -0.1509 | 0.0089 |
| Plaque score | 0.1608 | 0.0056 |
| Maximum IMT | 0.1266 | 0.0295 |
| ABI (right) | -0.0122 | 0.8353 |
| ABI (left) | -0.0124 | 0.8319 |
| CAVI (right) | 0.1430 | 0.0165 |
| CAVI (left) | 0.1472 | 0.0132 |
| HbA1c | -0.0077 | 0.9260 |
| PTH | 0.1539 | 0.0076 |
| Fe | -0.0984 | 0.0889 |
| Ferritin | 0.1110 | 0.0547 |
| TSAT ratio | -0.0615 | 0.2882 |
| Kt/V | -0.0874 | 0.1308 |
| RBC | -0.0680 | 0.2406 |
| PLT | -0.0743 | 0.1994 |
| TP | -0.0568 | 0.3272 |
| ALB | -0.0758 | 0.1907 |
| UA | -0.0153 | 0.7912 |
| Na | 0.1010 | 0.0807 |
| K | -0.0112 | 0.8462 |
| Cl | 0.0522 | 0.3676 |
| Ca | 0.0130 | 0.8223 |
| IP | -0.0017 | 0.9770 |
| Mg | 0.0544 | 0.3476 |
| AST | 0.1654 | 0.0041 |
| ALT | 0.0975 | 0.0920 |
| LDH | 0.1749 | 0.0024 |
| γ-GTP | 0.0895 | 0.1219 |
| AP | 0.0557 | 0.3366 |
| tBil | -0.0105 | 0.8559 |
| AMY | -0.0448 | 0.4394 |
| Creatinin | -0.0354 | 0.5415 |
| T-CHO | -0.0300 | 0.6047 |
| HDL-C | -0.0741 | 0.2004 |
| LDL-C | -0.0058 | 0.9197 |
| TG | 0.0383 | 0.5086 |
| CRP | 0.1638 | 0.0044 |
A correlation analysis was performed to identify the correlation between TSTD2 antibody levels and the clinical features in patients with CKD. Correlation coefficient (Rho) and P-values were calculated using Spearman's correlation analysis. Significant correlations (P<0.05) are marked in bold font. TSTD2, thiosulfate sulfurtransferase-like domain-containing 2; CKD, chronic kidney disease; BMI, body mass index; maximum IMT, maximum intima-media thickness; ABI, ankle brachial pressure index; CAVI, cardio-ankle vascular index; HbA1c, glycated hemoglobin; W-PTH, whole parathyroid hormone; ARB, angiotensin II receptor blocker; ACE, angiotensin converting enzyme; PTA, prothrombin; TSAT ratio, transferrin saturation ratio; Kt/V, standardized urea clearance; RBC, red blood cell number; PLT, platelet number; TP, total protein; ALB, albumin; UA, uric acid; HGB, hemoglobin; HCT, hematocrit; UN, urea nitrogen; CRE, creatinine; IP, inorganic phosphate; AST, aspartate aminotransferase; ALT, alanine amino transferase; LDH, lactate dehydrogenase; γ-GTP, γ-glutamyl transpeptidase; AP, alkaline phosphatase; tBil, total bilirubin; AMY, amylase; T-CHO, total cholesterol; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; TG, triglyceride; and CRP, C-reactive protein.
The presence of autoantibodies against purified protein in the sera of aCI patients
Western blot analysis was performed to determine the presence of anti-TSTD2 antibodies in the serum samples. Both GST and GST-TSTD2 protein reacted with commercial anti-GST antibodies whereas GST-TSTD2, but not GST was recognized by antibodies in the sera of patients with aCI (Fig. 1, lanes 3 and 4 of the anti-GST-Ab, aCI, and HD blots). HD serum contained no TSTD2 antibodies.
Discussion
Atherosclerosis is one of the major causes of ischemic stroke (24) and the primary cause of CKD (5). Autoantibodies have been found to develop alongside atherosclerosis (13,14). Some of these autoantibodies may have causal or suppressive effects on disease development. For example, anti-GRP78 autoantibodies accelerate the development of atherosclerotic lesions (25). Therefore, the present study performed ProtoArray® screening and identified a novel autoantibody marker and selected the TSTD2 autoantibody as a candidate marker for atherosclerosis. AlphaLISA was then used to quantify anti-TSTD2 antibodies in patient sera, and a significant increase in the antibody levels was found in samples from patients with aCI and type-1 and type-2 CKD, as compared with those from the HDs (Figs. 2A and 3A). Western blot analysis was performed and this confirmed the presence of TSTD2 antibodies in aCI sera and their absence in HD sera (Fig. 1).
Subsequently, the correlation between clinical factors and anti-TSTD2 antibody levels was examined in the aCI cohort. A significant elevation in antibody levels was observed in males, and in those with hypertension, who were older, and with a smoking history and a history of alcohol consumption (Fig. 4), all of which are risk factors for atherosclerosis (26-28). These findings were consistent with the results of the Spearman's correlation analyses, which revealed a positive correlation between the serum TSTD2 antibody levels and maximum IMT and smoking (Table I). Maximum IMT, plaque score and CAVI (left and right) were also associated with serum TSTD2 antibody levels in the CKD cohort (Table II). IMT and plaque scores are widely accepted as indicators of atherosclerosis (29,30). Thus, the TSTD2 antibody may predominantly reflect the development of atherosclerosis, and may thus be associated with the presence of aCI and CKD.
Spearman's correlation analysis revealed that blood sugar, a typical diabetes mellitus (DM) marker, was related to the serum TSTD2 antibody levels (Table I). This correlation did not remain significant when the presence of DM was accounted for (Fig. 4F). The AUC of type-2 CKD (nephrosclerosis) was higher than that for type-1 CKD (diabetic kidney disease) (Fig. 3B and C). Consequently, it can be concluded that the serum TSTD2-Abs levels do not directly reflect DM, but may be related to DM-induced atherosclerotic disorders, including CKD. This is in contrast to anti-SH3BP5 antibody marker, which is mainly related to DM and, along with that, with type-1 CKD (31). Anti-DIDO1 antibody marker has been found to be equally associated with all three types of CKD, but has shown no association with DM (14).
TSTD2 is a thiosulfate sulfurtransferase (31). Although the function of TSTD2 has not yet been fully elucidated, its expression in the soleus feed artery can be upregulated by endurance exercise training (32). TSTD2 can function in the downstream region of the (pro)renin receptor signaling pathway (33). The renin-angiotensin system plays a key regulatory role in hypertension (34). This is consistent with the finding of the present study that the TSTD2 antibody levels were strongly associated with hypertension (Fig. 4C). If TSTD2 plays a causal role in the regulation of hypertension, it may be used as a therapeutic target to prevent the development of atherosclerosis. Among the other correlated factors in Fig. 4, the habit of smoking is one of the major risk factors for the development of atherosclerosis (35). Age may be indirectly associated with atherosclerosis as a confounding factor. The male sex and alcohol consumption may also be associated with the smoking habit and indirectly with atherosclerosis.
Reactive oxygen species (ROS) are considered to contribute to vascular inflammation in atherosclerosis as a result of mediating various signaling pathways (36,37). As a result, there are increasing reports that the excessive production of ROS is implicated in the pathogenesis of acute and chronic cardiovascular diseases and renal dysfunction (38-40). TSTD2 is one of the TST-like domains and is known as rhodanese (41). It is a mitochondrial enzyme that catalyzes sulfur transfer through multiple molecular pathways and is known for its ability to reduce the antioxidants glutathione and thioredoxin, detoxify ROS and regulate cellular homeostasis (42,43). Although, to the best of our knowledge, there have been no reports to date demonstrating a direct association between TSTD2 function and ROS, TST has antioxidant effects, and smoking, alcohol consumption, and hyperglycemia have the potential to cause vascular endothelial damage due to oxidative stress and the production of free radicals. It was hypothesized speculated that the levels of TSTD2, which is considered to contribute to the detoxification of ROS, are increased in blood, resulting in an elevation in the levels of anti-TSTD2 antibodies.
The early stages of atherosclerosis are usually accompanied by elevated autoantibody levels (44). Autoantibodies are stable and easy to detect in patients' sera (45). Hence, atherosclerosis-induced autoantibodies can be used for the early diagnosis of atherosclerosis-related diseases. The present study identified the TSTD2 antibody as a novel biomarker that may be used for the detection of atherosclerosis-related aCI and CKD. However, further research is required to evaluate the sensitivity and specificity using validation cohorts, including atherosclerosis-related diseases, as well as disease controls.
Supplementary Material
Acknowledgements
Not applicable.
Funding Statement
Funding: The present study was supported, in part, by research grants from the Japan Science and Technology Agency (Exploratory Research No. 14657335) and JSPS KAKENHI (grant nos. 20K17953, 22K09227, 17K16626, 22K07273 and 19K09451).
Availability of data and materials
All results of the ProtoArray® Human Protein Microarrays are available in the Figshre database (https://doi.org/10.6084/m9.figshare.21510009.v1).
Authors' contributions
MK, TMac, HK, YI and TH conceived and designed the study. MK, BSZ, SYL, HW and AAd performed the experiments and acquired the data. YY, TMac, SM, IK, TW, AAo, KK and HT contributed the reagents, materials, analysis tools or patient data. YY, AAd and TMat analyzed and interpreted the data. BSZ, TMat and HK performed the statistical analyses. MK, BSZ, SYL, TMac, YI and TH drafted the manuscript. SM, TW and HT confirm the authenticity of all the raw data. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
The present study was conducted in accordance with the principles of the 1913 revision of the Declaration of Helsinki and with the approval of the Ethical Review Committee of Chiba University, Graduate School of Medicine and cooperative hospitals (approval no. 2018-320). The research on recombinant DNA was conducted with the permission of the Graduate School of Medicine, Chiba University, and following Japanese regulations. Each participant provided written informed consent to participation and publication.
Patient consent for publication
Not applicable.
Competing interests
The present study was performed in collaboration with Fujikura Kasei Co., Ltd., and HK is an employee of Fujikura Kasei Co., Ltd.
References
- 1.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, et al. Heart disease and stroke statistics-2020 update: A report from the american heart association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(e442) doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McClellan WM, Plantinga LC. A public health perspective on CKD and obesity. Nephrol Dial Transplant. 2013;28 (Suppl 4):iv37–iv42. doi: 10.1093/ndt/gft030. [DOI] [PubMed] [Google Scholar]
- 4.Baldassarre D, Castelnuovo S, Frigerio B, Amato M, Werba JP, De Jong A, Ravani AL, Tremoli E, Sirtori CR. Effects of timing and extent of smoking, type of cigarettes, and concomitant risk factors on the association between smoking and subclinical atherosclerosis. Stroke. 2009;40:1991–1998. doi: 10.1161/STROKEAHA.108.543413. [DOI] [PubMed] [Google Scholar]
- 5.Drüeke TB, Massy ZA. Atherosclerosis in CKD: differences from the general population. Nat Rev Nephrol. 2010;6:723–735. doi: 10.1038/nrneph.2010.143. [DOI] [PubMed] [Google Scholar]
- 6.Nilsson J, Hansson GK, Shah PK. Immunomodulation of atherosclerosis: implications for vaccine development. Arterioscler Thromb Vasc Biol. 2005;25:18–28. doi: 10.1161/01.ATV.0000149142.42590.a2. [DOI] [PubMed] [Google Scholar]
- 7.Miyashita K, Lutz J, Hudgins LC, Toib D, Ashraf AP, Song W, Murakami M, Nakajima K, Ploug M, Fong LG, et al. Chylomicronemia from GPIHBP1 autoantibodies. J Lipid Res. 2020;61:1365–1376. doi: 10.1194/jlr.R120001116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Obaid AH, Zografou C, Vadysirisack DD, Munro-Sheldon B, Fichtner ML, Roy B, Philbrick WM, Bennett JL, Nowak RJ, O'Connor KC. Heterogeneity of acetylcholine receptor autoantibody-mediated complement activity in patients with myasthenia gravis. Neurol Neuroimmunol Neuroinflamm. 2022;9(e1169) doi: 10.1212/NXI.0000000000001169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Machida T, Kubota M, Kobayashi E, Iwadate Y, Saeki N, Yamaura A, Nomura F, Takiguchi M, Hiwasa T. Identification of stroke-associated-antigens via screening of recombinant proteins from the human expression cDNA library (SEREX) J Transl Med. 2015;13(71) doi: 10.1186/s12967-015-0393-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoshida Y, Wang H, Hiwasa T, Machida T, Kobayashi E, Mine S, Tomiyoshi G, Nakamura R, Shinmen N, Kuroda H, et al. Elevation of autoantibody level against PDCD11 in patients with transient ischemic attack. Oncotarget. 2018;9:8836–8848. doi: 10.18632/oncotarget.23653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang H, Zhang XM, Tomiyoshi G, Nakamura R, Shinmen N, Kuroda H, Kimura R, Mine S, Kamitsukasa I, Wada T, et al. Association of serum levels of antibodies against MMP1, CBX1, and CBX5 with transient ischemic attack and cerebral infarction. Oncotarget. 2018;9:5600–5613. doi: 10.18632/oncotarget.23789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoshida Y, Zhang XM, Wang H, Machida T, Mine S, Kobayashi E, Adachi A, Matsutani T, Kamitsukasa I, Wada T, et al. Elevated levels of autoantibodies against DNAJC2 in sera of patients with atherosclerotic diseases. Heliyon. 2020;6(e04661) doi: 10.1016/j.heliyon.2020.e04661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li SY, Yoshida Y, Kobayashi E, Kubota M, Matsutani T, Mine S, Machida T, Maezawa Y, Takemoto M, Yokote K, et al. Serum anti-AP3D1 antibodies are risk factors for acute ischemic stroke related with atherosclerosis. Sci Rep. 2021;11(13450) doi: 10.1038/s41598-021-92786-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hiwasa T, Wang H, Goto KI, Mine S, Machida T, Kobayashi E, Yoshida Y, Adachi A, Matsutani T, Sata M, et al. Serum anti-DIDO1, anti-CPSF2, and anti-FOXJ2 antibodies as predictive risk markers for acute ischemic stroke. BMC Med. 2021;19(131) doi: 10.1186/s12916-021-02001-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kubota M, Yoshida Y, Kobayashi E, Matsutani T, Li SY, Zhang BS, Mine S, Machida T, Takizawa H, Hiwasa T, Iwadate Y. Serum anti-SERPINE1 antibody as a potential biomarker of acute cerebral infarction. Sci Rep. 2021;11(21772) doi: 10.1038/s41598-021-01176-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nishiura R, Fujimoto S, Sato Y, Yamada K, Hisanaga S, Hara S, Nakao H, Kitamura K. Elevated osteoprotegerin levels predict cardiovascular events in new hemodialysis patients. Am J Nephrol. 2009;29:257–263. doi: 10.1159/000157629. [DOI] [PubMed] [Google Scholar]
- 17.Komatsu H, Fujimoto S, Hara S, Fukuda A, Fukudome K, Yamada K, Sato Y, Kitamura K. Recent therapeutic strategies improve renal outcome in patients with IgA nephropathy. Am J Nephrol. 2009;30:19–25. doi: 10.1159/000197116. [DOI] [PubMed] [Google Scholar]
- 18.Hamanaka S, Nakagawa T, Hiwasa T, Ohta Y, Kasamatsu S, Ishigami H, Taida T, Okimoto K, Saito K, Maruoka D, et al. Investigation of novel biomarkers for predicting the clinical course in patients with ulcerative colitis. J Gastroenterol Hepatol. 2018;33:1975–1983. doi: 10.1111/jgh.14297. [DOI] [PubMed] [Google Scholar]
- 19.Vermeulen N, de Béeck KO, Vermeire S, Van Steen K, Michiels G, Ballet V, Rutgeerts P, Bossuyt X. Identification of a novel autoantigen in inflammatory bowel disease by protein microarray. Inflamm Bowel Dis. 2011;17:1291–1300. doi: 10.1002/ibd.21508. [DOI] [PubMed] [Google Scholar]
- 20.Nakashima K, Shimada H, Ochiai T, Kuboshima M, Kuroiwa N, Okazumi S, Matsubara H, Nomura F, Takiguchi M, Hiwasa T. Serological identification of TROP2 by recombinant cDNA expression cloning using sera of patients with esophageal squamous cell carcinoma. Int J Cancer. 2004;112:1029–1035. doi: 10.1002/ijc.20517. [DOI] [PubMed] [Google Scholar]
- 21.Matsutani T, Hiwasa T, Takiguchi M, Oide T, Kunimatsu M, Saeki N, Iwadate Y. Autologous antibody to src-homology 3-domain GRB2-like 1 specifically increases in the sera of patients with low-grade gliomas. J Exp Clin Cancer Res. 2012;31(85) doi: 10.1186/1756-9966-31-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li SY, Yoshida Y, Kobayashi E, Adachi A, Hirono S, Matsutani T, Mine S, Machida T, Ohno M, Nishi E, et al. Association between serum anti-ASXL2 antibody levels and acute ischemic stroke, acute myocardial infarction, diabetes mellitus, chronic kidney disease and digestive organ cancer, and their possible association with atherosclerosis and hypertension. Int J Mol Med. 2020;46:1274–1288. doi: 10.3892/ijmm.2020.4690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muto M, Mori M, Hiwasa T, Takiguchi M, Iwadate Y, Uzawa A, Uchida T, Masuda H, Sugimoto K, Kuwabara S. Novel serum autoantibodies against talin1 in multiple sclerosis: Possible pathogenetic roles of the antibodies. J Neuroimmunol. 2015;284:30–36. doi: 10.1016/j.jneuroim.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 24.Gutierrez J, Turan TN, Hoh BL, Chimowitz MI. Intracranial atherosclerotic stenosis: Risk factors, diagnosis, and treatment. Lancet Neurol. 2022;21:355–368. doi: 10.1016/S1474-4422(21)00376-8. [DOI] [PubMed] [Google Scholar]
- 25.Crane ED, Al-Hashimi AA, Chen J, Lynn EG, Won KD, Lhoták Š, Naeim M, Platko K, Lebeau P, Byun JH, et al. Anti-GRP78 autoantibodies induce endothelial cell activation and accelerate the development of atherosclerotic lesions. JCI Insight. 2018;3(e99363) doi: 10.1172/jci.insight.99363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Colafella KMM, Denton KM. Sex-specific differences in hypertension and associated cardiovascular disease. Nat Rev Nephrol. 2018;14:185–201. doi: 10.1038/nrneph.2017.189. [DOI] [PubMed] [Google Scholar]
- 27.Lechner K, von Schacky C, McKenzie AL, Worm N, Nixdorff U, Lechner B, Kränkel N, Halle M, Krauss RM, Scherr J. Lifestyle factors and high-risk atherosclerosis: pathways and mechanisms beyond traditional risk factors. Eur J Prev Cardiol. 2020;27:394–406. doi: 10.1177/2047487319869400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matsuda H. Health risk assessment of long-term weight history. Nihon Koshu Eisei Zasshi. 1990;37:817–824. [PubMed] [Google Scholar]
- 29.Nezu T, Hosomi N, Aoki S, Matsumoto M. Carotid intima-media thickness for atherosclerosis. J Atheroscler Thromb. 2016;23:18–31. doi: 10.5551/jat.31989. [DOI] [PubMed] [Google Scholar]
- 30.Ojima S, Kubozono T, Kawasoe S, Kawabata T, Miyata M, Miyahara H, Maenohara S, Ohishi M. Association of risk factors for atherosclerosis, including high-sensitivity C-reactive protein, with carotid intima-media thickness, plaque score, and pulse wave velocity in a male population. Hypertens Res. 2020;43:422–430. doi: 10.1038/s41440-019-0388-2. [DOI] [PubMed] [Google Scholar]
- 31.Cipollone R, Ascenzi P, Visca P. Common themes and variations in the rhodanese superfamily. IUBMB Life. 2007;59:51–59. doi: 10.1080/15216540701206859. [DOI] [PubMed] [Google Scholar]
- 32.Padilla J, Jenkins NT, Thorne PK, Martin JS, Rector RS, Davis JW, Laughlin MH. Transcriptome-wide RNA sequencing analysis of rat skeletal muscle feed arteries. II. Impact of exercise training in obesity. J Appl Physiol (1985) 2014;116:1033–1047. doi: 10.1152/japplphysiol.01234.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zaade D, Schmitz J, Benke E, Klare S, Seidel K, Kirsch S, Goldin-Lang P, Zollmann FS, Unger T, Funke-Kaiser H. Distinct signal transduction pathways downstream of the (P)RR revealed by microarray and ChIP-chip analyses. PLoS One. 2013;8(e57674) doi: 10.1371/journal.pone.0057674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang Z, Chen L, Zhong J, Gao P, Oudit GY. ACE2/Ang-(1-7) signaling and vascular remodeling. Sci China Life Sci. 2014;57:802–808. doi: 10.1007/s11427-014-4693-3. [DOI] [PubMed] [Google Scholar]
- 35.Siasos G, Tsigkou V, Kokkou E, Oikonomou E, Vavuranakis M, Vlachopoulos C, Verveniotis A, Limperi M, Genimata V, Papavassiliou AG, et al. Smoking and atherosclerosis: Mechanisms of disease and new therapeutic approaches. Curr Med Chem. 2014;21:3936–3948. doi: 10.2174/092986732134141015161539. [DOI] [PubMed] [Google Scholar]
- 36.Witztum JL. The oxidation hypothesis of atherosclerosis. Lancet. 1994;344:793–795. doi: 10.1016/s0140-6736(94)92346-9. [DOI] [PubMed] [Google Scholar]
- 37.Madamanchi NR, Vendrov A, Runge MS. Oxidative stress and vascular disease. Arterioscler Thromb Vasc Biol. 2005;25:29–38. doi: 10.1161/01.ATV.0000150649.39934.13. [DOI] [PubMed] [Google Scholar]
- 38.Ochoa CD, Wu RF, Terada LS. ROS signaling and ER stress in cardiovascular disease. Mol Aspects Med. 2018;63:18–29. doi: 10.1016/j.mam.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jha JC, Banal C, Chow BS, Cooper ME, Jandeleit-Dahm K. Diabetes and kidney disease: Role of oxidative stress. Antioxid Redox Signal. 2016;25:657–684. doi: 10.1089/ars.2016.6664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aranda-Rivera AK, Cruz-Gregorio A, Aparicio-Trejo OE, Pedraza-Chaverri J. Mitochondrial redox signaling and oxidative stress in kidney diseases. Biomolecules. 2021;11(1144) doi: 10.3390/biom11081144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nakajima T. Roles of sulfur metabolism and rhodanese in detoxification and anti-oxidative stress functions in the liver: Responses to radiation exposure. Med Sci Monit. 2015;21:1721–1725. doi: 10.12659/MSM.893234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Libiad M, Motl N, Akey DL, Sakamoto N, Fearon ER, Smith JL, Banerjee R. Thiosulfate sulfurtransferase-like domain-containing 1 protein interacts with thioredoxin. J Biol Chem. 2018;293:2675–2686. doi: 10.1074/jbc.RA117.000826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nandi DL, Horowitz PM, Westley J. Rhodanese as a thioredoxin oxidase. Int J Biochem Cell Biol. 2000;32:465–473. doi: 10.1016/s1357-2725(99)00035-7. [DOI] [PubMed] [Google Scholar]
- 44.Iseme RA, McEvoy M, Kelly B, Agnew L, Walker FR, Handley T, Oldmeadow C, Attia J, Boyle M. A role for autoantibodies in atherogenesis. Cardiovasc Res. 2017;113:1102–1112. doi: 10.1093/cvr/cvx112. [DOI] [PubMed] [Google Scholar]
- 45.Anderson KS, LaBaer J. The sentinel within: Exploiting the immune system for cancer biomarkers. J Proteome Res. 2005;4:1123–1133. doi: 10.1021/pr0500814. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All results of the ProtoArray® Human Protein Microarrays are available in the Figshre database (https://doi.org/10.6084/m9.figshare.21510009.v1).