Abstract
TINF2 is a critical subunit of the shelterin complex, which protects and maintains the length of telomeres. Pathogenic missense and truncating TINF2 mutations are causative for dyskeratosis congenita (DC), a rare, dominantly inherited bone marrow failure syndrome characterized by mucocutaneous abnormalities and cancer predisposition. Recent reports indicate that specific TINF2 truncating mutations act as high penetrance cancer predisposition alleles outside DC context, including breast cancer in their tumor spectrum. Here, we have evaluated the role of germline mutations in TINF2 and other shelterin genes in inherited breast cancer susceptibility using exome sequencing data from 98 Northern Finnish breast cancer cases with indication of inherited disease predisposition as a discovery cohort. A single protein truncating variant, TINF2 p.Tyr312Ter, was identified in one of the cases (1/98), and four more carriers were observed in the subsequently genotyped unselected breast cancer cohort (4/1904). None of the carriers were reported to have DC. TINF2 p.Tyr312Ter resulted in stable short form of mRNA transcript, and normal telomere length has been indicated by a recent report. Although recurrent in cases (total of 5/2095), TINF2 p.Tyr312Ter is also present in Finnish population controls (8/12,517), and the observed 4-fold higher frequency in cases falls at most into the range of moderate breast cancer risk alleles (OR 3.74, 95% CI 1.22–11.45, p = 0.029). Current results indicate that not all TINF2 truncating variants are high cancer risk alleles and add further evidence that different TINF2 mutations can have very diverse effects on the disease phenotype.
Supplementary information
The online version contains supplementary material available at 10.1007/s10689-022-00295-z.
Keywords: Breast cancer, Hereditary predisposition, TINF2, Dyskeratosis congenita
Introduction
TINF2 (TERF1 Interacting Nuclear Factor 2) is a critical subunit of the shelterin complex, which protects telomere ends and maintains the telomere length by cooperating with telomerase [1]. The shelterin complex allows cells to differentiate between telomeres and damaged DNA by blocking the activation of double-strand break repair pathways and prohibiting hyper-resection at telomeres [2]. The shelterin complex consists of six proteins, TINF2, TERF1, TERF2, TERF2IP, ACD, and POT1, of which TINF2 and ACD mediate the complex assembly [1]. Pathogenic missense [3] and truncating mutations [4] of TINF2 are causative for dyskeratosis congenita (DC), a rare, dominantly inherited bone marrow failure syndrome characterized by mucocutaneous abnormalities and cancer predisposition, most commonly head and neck cancers, anorectal squamous cell carcinoma, and stomach and lung cancer [5]. At cellular level, these TINF2 mutations result in short telomere length, which is a molecular hallmark for DC caused by defects in telomere maintenance [3].
Recently, a truncating germline TINF2 mutation, p.Trp198fs, was reported in a large family with several papillary thyroid carcinoma and melanoma cases, and it showed complete disease co-segregation. The telomere length was significantly longer in the identified mutation carriers, which is contrary to that previously reported in DC patients [6]. Following report revealed another two TINF2 truncating mutations, p.Glu202fs/p.Leu170fs and p.Ser186fs, in altogether four cancer-prone families, where six TINF2 mutation carriers developed numerous malignancies, including three papillary thyroid carcinomas, two melanomas and three breast carcinomas. In all four families, confirmed mutation carriers had at least one first-degree relative with breast cancer. At cellular level, both TINF2 mutations also resulted in excessive telomere elongation [7]. Based on these reports, TINF2 acts as a haploinsufficient tumor suppressor also outside the DC context, and specific truncation mutations resulting in long germline telomeres cause inherited cancer predisposition with high penetrance and severity [6, 7].
Here, we have evaluated the role of TINF2 and other shelterin complex gene mutations in inherited breast cancer susceptibility. As a result, we report a recurrent TINF2 truncation mutation, p.Tyr312Ter, which based on case-control comparisons is at highest a moderate-risk allele for breast cancer. This adds yet another feature for TINF2 germline mutations that seem to result in remarkably distinct outcomes.
Materials and methods
Identification of rare truncating variants in shelterin complex genes
Variant calls from exome sequencing data of 98 Northern Finnish breast cancer cases with indication of hereditary disease susceptibility [8] were assessed for rare and potentially deleterious variants in the six shelterin complex genes: TINF2, TERF1, TERF2, TERF2IP, ACD, and POT1. The filtering criteria used was: (1) inclusion of variants with predicted protein truncations (nonsense, frameshift and splice site variants) and (2) inclusion of variants with minor allele frequency, MAF < 0.01 in dbSNP, Ensembl, GnomAD and SISu databases. This discovery cohort included (1) index cases from families with 3 ≤ breast and/or ovarian cancer cases in 1st or 2nd degree relatives (n = 83), (2) index cases from families with two cases of breast, or breast and ovarian cancer in 1st or 2nd degree relatives, of which at least one with early disease onset (< 35 years), bilateral disease or multiple primary tumors (n = 7), and (3) breast cancer cases diagnosed at or below the age of 40 (n = 8).
Variant genotyping in additional cohorts
One variant, TINF2 p.Tyr312Ter, passing the filtering was genotyped further in breast cancer cohorts collected from same geographical area, defined as hereditary (n = 93) and unselected breast cancer cohort (n = 1904). The hereditary cohort (n = 93) consisted of BRCA1/2 and PALB2 mutation negative breast cancer index cases from (1) 44 families with 3 ≤ breast cancer cases in 1st or 2nd degree relatives, (2) 17 families with two cases of breast cancer in 1st or 2nd degree relatives, of which at least one had early disease onset (< 35 years), bilateral disease or multiple primary tumors including breast cancer, and (3) 32 families with two cases of breast cancer in 1st or 2nd degree relatives. The unselected cohort consisted of 1904 consecutive breast cancer cases diagnosed at the Oulu University Hospital during the years 2000–2019, unselected for their family history of cancer and age at disease onset. Tumor characteristics for the cases were obtained from pathology reports. This study included informed consent from all participating individuals. Genotyping was done using high-resolution melt analysis (CFX96, Bio-Rad) and Sanger sequencing (ABI3130xL, Applied Biosystem). Data from Finnish individuals (GnomAD, https://gnomad.broadinstitute.org/ and SISu, http://www.sisuproject.fi/) was used as control for comparisons.
Statistical analyses
Carrier frequencies between cases and controls were compared using Fisher’s exact test (IBM SPSS Statistics 26.0 for Windows). All p-values were two-sided.
Transcript analysis
RNA was extracted from patient-derived lymphoblastoid cell-lines using RNeasy Mini Kit (Qiagen) and reverse transcribed into cDNA with iScript cDNA synthesis Kit (Bio-Rad). PCR amplified (Table S1) fragments targeting both short and long isoforms were separated on agarose gel, extracted using UltraClean GelSpin DNA Extraction Kit (MO BIO) and Sanger sequenced (ABI3500xL).
Results
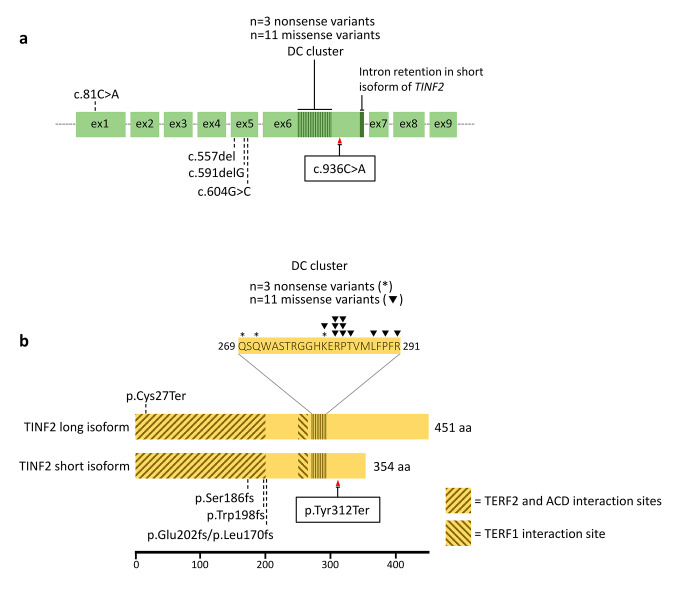
Analysis of 98 breast cancer cases for shelterin complex gene mutations (Table S2) revealed only one protein truncating variant, TINF2 p.Tyr312Ter (c.936 C > A, rs201677741). The carrier was diagnosed with breast cancer at the age of 27 years and had both breast and ovarian cancer in 3rd degree relatives (Table S3). Although there were no additional DNA samples from the family to study the disease segregation, the position and mutation type of the variant suggested that it could be a pathogenic mutation analogous to other previously reported variants in the gene (Fig. 1). To support this, the variant was globally rare with MAF of 0.0003 in European populations (both non-Finnish and Finnish, GnomAD), and had also equivalent MAF (0.00038) in Northern Finland, Northern Ostrobothnia (SISu).
Fig. 1.
Schematic presentation of TINF2 (a) gene and (b) protein, and localization of currently identified and previously discovered pathogenic variants for both DC and high cancer risk. TINF2 short isoform is a result of a small intron retention between exon 6 and 7 and the consequent stop codon [9]. Based on the cDNA analysis, c.936 C > A variant is stable only in this mRNA isoform. In exon 5, truncating variant c.591delG (p.Trp198fs) is associated with papillary thyroid carcinoma and melanoma [6], and a splice donor variant c.604G > C (with predicted truncations p.Glu202fs and p.Leu170fs) and c.557del (causing frameshift and a stop codon, p.Ser186fs) are proposed as high-risk alleles for multiple cancer types [7]. A majority of missense and truncating variants associated with DC localize to exon 6, specifically to a highly conserved area called DC cluster [3]. Variants associated with high cancer risk are shown under schematic gene and protein illustrations, and DC variants above (ClinVar database, https://www.ncbi.nlm.nih.gov/clinvar/). Variant c.936 C > A (p.Tyr312Ter) is pointed by a red arrow. TERF2, ACD and TERF1 interaction sites are marked with diagonal stripes
TINF2 p.Tyr312Ter was genotyped in further breast cancer case cohorts, and the variant prevalence is summarized in Table 1. No TINF2 p.Tyr312Ter carriers were identified in the additional cohort of BRCA1/2 and PALB2 mutation negative index cases with indication of inherited background for the disease. However, four more carries were identified from the unselected breast cancer cohort (4/1904, 0.21%, OR = 3.29, 95% CI = 0.99–10.49, p = 0.063). The mean age at disease onset for the unselected carriers was 61.3 years, which is similar to the mean for this cohort (58 years, range 28–93 years). When all breast cancer cases (5/2095, 0.24%) were compared to carriers reported in Finnish population (8/12,517, 0.06%), the frequency was 4 times higher with OR 3.74 (95% CI 1.22–11.45, p = 0.029).
Table 1.
Frequency of TINF2 p.Tyr312Ter in breast cancer cases and controls
| Cohort | N | WT | % | Mut | % | OR | 95% CI | p |
|---|---|---|---|---|---|---|---|---|
| Hereditary Bra | 191 | 190 | 99.48 | 1 | 0.52 | 8.23 | 1.02–66.12 | 0.127 |
| Unselected Br | 1904 | 1900 | 99.79 | 4 | 0.21 | 3.29 | 0.99–10.49 | 0.063 |
| All Br | 2095 | 2090 | 99.76 | 5 | 0.24 | 3.74 | 1.22–11.45 | 0.029 |
| Controlsb | 12,517 | 12,509 | 99.94 | 8 | 0.06 |
Br = Breast cancer, CI = Confidence interval, Mut = Mutation carrier, OR = Odds ratio, WT = Wild-type
a 98 exome-sequenced and 93 additionally genotyped index cases
b GnomAD European (Finnish) population
All four TINF2 p.Tyr312Ter carriers from the unselected cohort had family history of cancer, but only one of the families showed cancer types (one melanoma case) previously linked to TINF2-related cancer susceptibility [7]. Unfortunately, there were no samples available to study the mutation’s co-segregation with the cancer phenotype in the respective families (Table S3). The breast tumor characteristics of the TINF2 p.Tyr312Ter carriers are summarized in Table S4. Based on the reported cancer history and other diseases in the family, there were no indications of DC for any of the carriers or their family members.
The effect of the TINF2 p.Tyr312Ter variant at transcriptional level was studied with mRNA specific sequencing. The presence of the variant was confirmed only in the short form of TINF2 transcript, where it resides in the last coding exon (6/6) of the transcript and the created premature stop codon abolishes the last 42 amino acids of the short protein isoform. It was absent from the long transcript likely due to nonsense-mediated decay targeting the isoform with premature stop codon in exon 6/9 (Fig. 1, Fig. S1).
Discussion
Specific truncating mutations of TINF2 that encodes an integral member of the shelterin complex, critical for telomere protection, have previously been reported to cause a high risk for cancer [6, 7]. To evaluate the role of germline mutations in TINF2 and other shelterin encoding genes in inherited breast cancer susceptibility, we analyzed exome sequencing data from 98 Northern Finnish breast cancer cases with indication of hereditary disease susceptibility. There were no truncating germline mutations in the TERF1, TERF2, TERF2IP, ACD, and POT1 genes, whereas a single truncating variant in TINF2, p.Tyr312Ter, was observed.
Although TINF2 p.Tyr312Ter variant was recurrent in breast cancer cases, it is also reported in public databases in apparently healthy individuals. Based on the case-control comparisons, the frequency of TINF2 p.Tyr312Ter in breast cancer cases was 4-fold higher compared to controls, which falls at most into the range typical for moderate breast cancer risk alleles [10]. Even though TINF2 p.Tyr312Ter variant locates near the DC cluster of the protein, none of the currently identified cases or their family members were reported to have any of the symptoms of this disorder. This might be due to variant localizing closer to the C-terminal end of the protein than the DC causing truncation mutations in the same exon and therefore the functionality of the produced truncated protein from the short transcript is retained. In support of this, there is a recent case report of TINF2 p.Tyr312Ter variant carrier with normal telomere length. She suffered from herpes simplex virus 2 encephalitis but was otherwise healthy [11]. Thereby TINF2 p.Tyr312Ter does not seem to result in either elongated or shortened telomeres, the cellular level features associated with TINF2 mutations related to inherited high-risk cancer predisposition and DC, respectively.
In conclusion, the results indicate that rare variants in shelterin complex genes do not play a major role in inherited breast cancer susceptibility, at least in the current study population. The only observed truncating mutation was TINF2 p.Tyr312Ter, and although it was more prevalent in cases compared to controls, it is unlikely a high cancer risk allele analogous to those TINF2 truncation mutations previously described in the literature [6, 7]. Our results provide additional evidence that TINF2 mutations in different gene positions can have remarkably diverse effects on individuals’ phenotype, ranging from severe congenital disorder to potentially moderately increased risk for breast cancer.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank all the patients and their family members for volunteering to participate in this study, and Biocenter Oulu Sequencing Center for providing sequencing services.
Contributions
K.P., T.M. conceived the study. S.K., S.V., T.M.M., A.T., T.K., T.M. performed experiments and analysis. R.W., K.P., O.K., J.M. provided patient samples. S.K., K.P. drafted manuscript, and all authors approved the final manuscript.
Funding
This work was supported by the Academy of Finland, the Cancer Foundation of Finland sr and the Sigrid Jusélius Foundation sr.
Open Access funding provided by University of Oulu including Oulu University Hospital.
Data Availability
The data to support the findings of this study is available on request from the corresponding author.
Declarations
Compliance with Ethical Standards
The study included informed consent from all participating individuals, and it was approved by the Ethical Board of the North Ostrobothnia Health Care District (100/2016).
Conflict of interest
The authors declare that there is no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Xin H, Liu D, Songyang Z. The telosome/shelterin complex and its functions. Genome Biol. 2008 doi: 10.1186/gb-2008-9-9-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Lange T (2018) Shelterin-Mediated Telomere Protection. 10.1146/annurev-genet-032918 [DOI] [PubMed]
- 3.Walne AJ, Vulliamy T, Beswick R, Kirwan M, Dokal I. TINF2 mutations result in very short telomeres: Analysis of a large cohort of patients with dyskeratosis congenita and related bone marrow failure syndromes. Blood. 2008;112(9):3594–3600. doi: 10.1182/blood-2008-05-153445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sasa GS, Ribes-Zamora A, Nelson ND, Bertuch AA. Three novel truncating TINF2 mutations causing severe dyskeratosis congenita in early childhood. Clin Genet. 2012;81(5):470–478. doi: 10.1111/j.1399-0004.2011.01658.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Savage SA, Alter BP (2009, April) Dyskeratosis Congenita. Hematol Oncol Clin N Am. 10.1016/j.hoc.2009.01.003 [DOI] [PMC free article] [PubMed]
- 6.He H, Li W, Comiskey DF, Liyanarachchi S, Nieminen TT, Wang Y, de La Chapelle A. A Truncating Germline Mutation of TINF2 in Individuals with Thyroid Cancer or Melanoma Results in Longer Telomeres. Thyroid. 2020;30(2):204–213. doi: 10.1089/thy.2019.0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmutz I, Mensenkamp AR, Takai KK, Haadsma M, Spruijt L, de Voer RM, de Lange T. Tinf2 is a haploinsufficient tumor suppressor that limits telomere length. eLife. 2020;9:1–20. doi: 10.7554/ELIFE.61235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koivuluoma S, Tervasmäki A, Kauppila S, Winqvist R, Kumpula T, Kuismin O, Pylkäs K. Exome sequencing identifies a recurrent variant in SERPINA3 associating with hereditary susceptibility to breast cancer. Eur J Cancer. 2021;143:46–51. doi: 10.1016/j.ejca.2020.10.033. [DOI] [PubMed] [Google Scholar]
- 9.Kaminker PG, Kim SH, Desprez PY, Campisi J. A novel form of the telomere-associated protein TIN2 localizes to the nuclear matrix. Cell Cycle. 2009;8(6):931–939. doi: 10.4161/cc.8.6.7941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hollestelle A, Wasielewski M, Martens JWM, Schutte M (2010, June) Discovering moderate-risk breast cancer susceptibility genes. Curr Opin Genet Dev. 10.1016/j.gde.2010.02.009 [DOI] [PubMed]
- 11.Hautala T, Chen J, Tervonen L, Partanen T, Winqvist S, Lehtonen J, Seppänen MRJ (2020) Herpes simplex virus 2 encephalitis in a patient heterozygous for a TLR3 mutation. Neurology: Genetics. Lippincott Williams and Wilkins. 10.1212/NXG.0000000000000532 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data to support the findings of this study is available on request from the corresponding author.