Abstract
Objectives
In addition to being home to more than seven million HIV-infected individuals, South Africa also has a high burden of COVID-19 and related comorbidities worldwide. We aimed to identify the most influential “beliefs” and “attitudes” on vaccine decision-making behavior.
Study design
This study used panel data from cross-sectional surveys.
Methods
We used the data from Black South Africans who participated in the “COVID-19 Vaccine Surveys” (November 2021 and February/March 2022) in South Africa. Besides standard risk factor analysis, such as multivariable logistic regression models, we also used the modified version of population attributable risk percent and estimated the population-level impacts of beliefs and attitudes on vaccine decision-making behavior using the methodology in multifactorial setting.
Results
A total of 1399 people (57% men and 43% women) who participated in both surveys were analyzed. Of these, 336 (24%) reported being vaccinated in survey 2. Overall low perceived risk, concerns around efficacy, and safety were identified as the most influential factors and associated with 52%–72% (<40 years) and 34%–55% (40+ years) of the unvaccinated individuals.
Conclusion
Our findings highlighted the most influential beliefs and attitudes on vaccine decision-making and their population-level impacts, which are likely to have significant public health implications exclusively for this population.
Keywords: COVID-19, Vaccine, South Africa, Vaccine acceptability, Population attributable risk
Introduction
In addition to being home to more than seven million HIV-infected individuals, South Africa also has a high burden of COVID-19 and related comorbidities worldwide.1, 2, 3 Furthermore, evidence suggests significant disparities in vaccine coverage in African countries.4 , 5 Similar to other low- and middle-income countries, South Africa also experienced delays in vaccine allocation and delivery where vaccination programs officially started approximately 1 year after vaccine approval (February 2021). As of July 2022, only 37.3% of South Africans received at least one dose compared with 66.9% of the global average.6 High vaccine coverage is crucial to reducing COVID-19-related severe adverse events.7 , 8 This is particularly important in South Africa, where multiple variants of COVID-19 were prevalent, including Beta (B.1.351) and the fast-spreading Omicron and its subvariants (BA.4 and BA.5), which were first identified in the country in November 2021.9, 10, 11
Vaccine acceptability directly impacts vaccine uptake. There has been extensive research to investigate the potential barriers associated with the intention to get vaccinated and uptake of vaccination worldwide.12, 13, 14 These studies, which were mostly conducted before the COVID-19 vaccines were approved and available for use, reported high acceptability rates, ranging from 67% to 91%.15, 16, 17 In February/March 2021, more than 80% of adult South Africans reported that they “they intend to get vaccinated” when the vaccines become available. This proportion was 71% in a nationally representative cohort of South Africans in June 2021.18 The most common reason for those who did not intend to get vaccinated was due to side-effects and concerns about the effectiveness of the vaccines.14 , 19 , 20
Despite undisputable evidence indicating that COVID-19 vaccines prevent severe adverse events, including hospitalization, and death, there is an emerging concern around vaccine hesitancy, which has increased over time in many countries.3 , 14 Consequently, studies continue to collect timely data to track vaccine acceptability and uptake in many countries, including South Africa. Most recently, vaccine knowledge, beliefs, and attitudes were assessed in South African adults who participated in the “COVID-19 Vaccine Surveys (CVACS)”. The CVACS was carried out twice, once in November 2021 and again in February/March 2022.21 , 22
This study aimed to investigate the population-level impacts of certain beliefs and attitudes and their interplay with vaccine decision-making in South African adults who participated in both “CVACS.” After developing a risk scoring algorithm to predict individuals’ vaccine decision-making behavior, we also quantified the degree to which the relative contributions of beliefs and attitudes influenced vaccination status. This is the first study to present empirical results for the most influential beliefs and attitudes on vaccine decision-making in the era of the widely available COVID-19 vaccines. Our findings collectively provide the most recent snapshot of the intention to get the vaccination and actual vaccination status and their significant contributors in Black South Africans. This information can potentially be used to improve the effectiveness of the current COVID-19 vaccine promotion and delivery programs/campaigns on vaccine uptake.
Methods
Survey population
The present study used the panel data from a cohort of the South Africans who participated in the “CVACS” from the nine provinces and 52 districts across the country. The surveys were implemented by the Southern Africa Labour and Development Research Unit. The details of the surveys and the populations were previously described.21 , 22 Briefly, a multistage stratified cluster sampling was used to select the households. Respondents were interviewed telephonically in two time points. Survey 1 participants were unvaccinated as of November 2021 (i.e. approximately 9 months after the first dose of vaccine roll-out). A total of 3,510 adults (aged ≥18 years) participated in survey 1. A follow-up survey was conducted in February to March 2022 (survey 2). A total of 1,772 individuals participated in both survey 1 and survey 2. Of these, 1,399 (80%) identified themselves as Black South Africans and were included in the present study. Owing to the low response rates for the other ethnic groups, we only included (self-identified) Black men and women in this analysis.
Measurements
Data from the survey 1 and survey 2 were merged by unique participant identification numbers. Our analysis included age (<35, 35–49, 50–59, and ≥60 years), employment status (yes/no), education (grade 12 completed vs not), residential area (urban, traditional, farm), marital/cohabitation status, monthly household income (in quartiles), and medical aid/insurance (yes/no). In survey 1, participants' COVID-19 risk perceptions, beliefs, and attitudes were measured by asking (1) Do you think you will get very sick with COVID-19 in the next 12 months? (yes, no, don’t know); (2) Do you believe the COVID-19 vaccine will prevent you from getting COVID-19? (yes, no, don’t know); (3) Do you believe the COVID-19 vaccine will help prevent you dying from COVID? (yes, no, don’t know)”. In survey 1, participants were also asked their reasons for not getting vaccinated in survey 1. These questions included (4) “I don’t trust vaccine/Vaccine has side effects” and (5) “Vaccine will kill (yes/no)”; (6) “Already had COVID-19”; (7) “Don’t know where to go”; (8) “Vaccination site is too far”; (9) “Travel cost is high”; (10) “May not be able to work after vaccine (yes/no); (11) “Don’t have time”. In addition, (12) religious and (13) health-related reasons for not getting vaccinated were derived from the participants' free text narratives for the question: what is the single biggest reason that you are not yet vaccinated? The study participants were also asked, “Regarding the COVID-19 vaccine, do you plan to”: (a) get it as soon as possible, (b) going to wait, (c) only if required, (d) definitely not get it. The primary outcome was self-reported vaccination status in survey 2 (unvaccinated vs vaccinated).
Statistical analysis
Characteristics of the population were described by vaccination status using frequencies and percentages and compared using Chi-squared test. Using the data from the individuals who participated in both surveys, we developed a risk scoring algorithm to predict the vaccination status in survey 2. After adjusting for potential confounders identified in descriptive analysis, we fitted logistic regression model and presented the weighted-rounded regression coefficients (i.e. and multiplying the logarithms of the odds ratio by 10) for the self-perception, beliefs questionnaires reported in survey 1.23 Total risk score for each participant was derived by adding up the final weighted scores for each item considered in the model. The total score was categorized using the deciles where “lowest” (1st decile) “to highest” (10th decile) risk for not getting vaccinated. We evaluated the internal validity of the primary outcome model using a bootstrapping analysis and generated 500 and 1000 test data sets by random selection with replacement (Stata 16.0 macro called rhsbsampler). The calibration of the model was visually assessed using pmcalplot and tested using the Hosmer–Lemeshow goodness-of-fit test, plotting the agreement between the predicted and observed probabilities of vaccination status. Statistically acceptable threshold was determined to predict those who would not get vaccinated with high sensitivity/specificity and discriminatory power. We also hypothesized that “intention to get vaccination” (i.e. as soon as possible vs other) in survey 1 and vaccine decision-making behavior in survey 2 will be strongly correlated. Therefore, it can potentially be considered as a proxy for vaccination status in survey 2. As a secondary analysis, we refitted the 7-item risk scoring algorithm to predict those who did not intend to receive the vaccine immediately in survey 1. Discriminative power of all models was assessed using the standard statistical measures, such as sensitivity, specificity, and area under the curve. The goodness-of-fits of our models were assessed using the Hosmer and Lemeshow test; non-significant p-values (P > 0.05) were interpreted as an acceptable fit. We also estimated the population-level impacts of these factors on vaccine decision-making behavior using the methodology in multifactorial setting.24 This analysis was also conducted among those who were aged <40 and ≥40 years, which was identified as the cut-point for median. Methodology, SAS codes, and access to the Macro were presented in Appendix.
Results
A total of 1399 individuals (803, 57% men and 596, 43% women) who participated in both surveys were analyzed. Of these, 336 (24%) reported being vaccinated in survey 2. The overall mean age was 39 years (standard deviation: 16; median age: 36 years [interquartile range: 30–50]). The characteristics of the study population in survey 1 are compared by their vaccination status in survey 2 (Table 1 ). Age and gender distributions were not statistically significant between the two groups. Overall, 63% of the study population resided in urban areas, with significant difference between the vaccinated and unvaccinated groups. Unvaccinated survey participants had higher education and income levels, and they also more to report having medical aid and owning a vehicle compared with those who were vaccinated.
Table 1.
Demographic and socio-economic characteristics of study population by vaccination status.
| Assessment at survey #2 | ||||
|---|---|---|---|---|
| Assessments at survey #1 | % | Vaccinateda, N = 336 (24%) | Unvaccinated, N = 1,063 (76%) | p-value |
| Age | 0.237 | |||
| <35 years | 46% | 48% | 45% | |
| 35–49 years | 28% | 24% | 29% | |
| 50–59 years | 15% | 17% | 14% | |
| ≥60 years | 11% | 11% | 12% | |
| Sex | 0.194 | |||
| Female | 43% | 46% | 41% | |
| Male | 57% | 54% | 59% | |
| Area of residency | 0.037 | |||
| Traditional | 13% | 13% | 14% | |
| Urban | 63% | 57% | 65% | |
| Farm | 23% | 28% | 21% | |
| Level of education | 0.015 | |||
| Less than grade 12 | 40% | 46% | 39% | |
| Grade 12 or more | 60% | 54% | 61% | |
| Tertiary education completed | 0.031 | |||
| No | 55% | 60% | 53% | |
| Yes | 45% | 39% | 47% | |
| Employment (last week) | 0.212 | |||
| No | 59% | 62% | 58% | |
| Yes | 41% | 38% | 42% | |
| Income (in quartiles) | 0.100 | |||
| First quartile (<1,700 ZARb) | 25% | 30% | 24% | |
| Second quartile (1,700 to <3,000 ZARb) | 27% | 27% | 27% | |
| Third quartile (3,000 to <8000 ZARb) | 23% | 25% | 22% | |
| Fourth quartile (≥8,000 ZARb) | 25% | 18% | 27% | |
| Medical aid/health insurance | 21% | 18% | 22% | 0.033 |
| Water/pipe in dwelling | 83% | 80% | 84% | 0.196 |
| Household has electronic device(s) | 65% | 62% | 65% | 0.436 |
| Household has vehicle | 39% | 30% | 43% | <0.001 |
| Why didn’t you get vaccinated? | ||||
| Self-perceived risk: no risk | 60% | 54% | 62% | 0.007 |
| Vaccine will not prevent COVID-19 | 46% | 29% | 51% | <0.001 |
| Vaccine will not prevent dying from COVID-19 | 48% | 29% | 54% | <0.001 |
| Don’t trust vaccinec | 57% | 43% | 61% | <0.001 |
| Vaccine may kill you | 40% | 32% | 42% | 0.012 |
| Religious reasons | 6% | 3% | 7% | 0.004 |
| Pre-existing health conditionsd | 8% | 6% | 9% | 0.040 |
| I already had COVID-19 | 47% | 47% | 47% | 0.206 |
| Don’t know where to go | 17% | 20% | 16% | <0.001 |
| Vaccination site is too far | 18% | 24% | 17% | <0.001 |
| Travel cost is high | 20% | 24% | 20% | 0.012 |
| May not be able to work after vaccine | 48% | 46% | 49% | 0.745 |
| Don’t have time | 30% | 39% | 27% | <0.001 |
| Are you going to get vaccinated? | <0.001 | |||
| I will get it as soon as possible | 38% | 61% | 30% | |
| I will wait | 22% | 19% | 24% | |
| Definitely not get it | 23% | 6% | 18% | |
| Other/missing | 21% | 14% | 28% | |
At least one dose.
1 South African Rand; 1 ZAR = 0.064 US Dollar (January 2022).
Vaccine has severe side-effects.
Including diabetes, hypertension, allergy.
Reasons for being unvaccinated in survey 1
Overall, 60% of the study population indicated that they were not at risk of getting infected by COVID-19, which was the most common reason for not being vaccinated (Table 1). A significantly higher proportion of individuals in the unvaccinated group indicated that they were not at risk for COVID-19 compared with the vaccinated group (62% vs 54%, respectively, p-value = 0.007). Unvaccinated individuals were also more likely to believe that vaccine is not effective (i.e. would not prevent infections and death due to COVID-19) and not safe (i.e. severe side-effects and death). Religion and pre-existing health conditions were reported in <10% of the study population in survey 1; however, these two reasons were significantly more common in the unvaccinated group. Meanwhile, other factors including “not knowing where to go for vaccination,” “travel costing and distance,” and “lack of time” were all significantly more common among those who got vaccinated in survey 2. More than 60% of the vaccinated participants also indicated that “they will get vaccinated as soon as possible” compared with 30% in the unvaccinated group.
A risk prediction model for vaccination status
In our risk prediction model, seven reasons for being unvaccinated from the survey 1 were identified as the most influential predictors for vaccination status in survey 2 (Table 2 ). Individuals with low perceived risk for COVID-19 were also significantly more likely to be unvaccinated compared with those who perceived themselves at high risk (adjusted odds ratio [aORs] from 1.74, 95% confidence interval [CI]: 1.24, 2.45). Similar trends were observed among those who did not believe in the vaccine’s efficacy and safety. For example, those who believed that the vaccine will not prevent them from getting infected or dying from COVID-19 were more than three times more likely to be unvaccinated than those who believed in the effectiveness of the vaccine. These factors had the highest risk scores (11 and 12, respectively) to predict unvaccinated individuals because of their high odds ratios (aOR: 3.10 and 3.45, respectively). Individuals who believed that the vaccine is associated with severe side-effects and deaths in survey 1 were also significantly more likely to be unvaccinated in survey 2 (aOR: 2.10 and 1.55, respectively).
Table 2.
Predictive model for unvaccinated participants: population-level impact of self-perception on COVID-19 uptake as reported in Survey #2 Black South Africans only (outcome: unvaccinated vs vaccinated).
| Assessments at Survey #1 | Adjusteda odds ratio (95% CI) | p-value | β×10 | Score |
|---|---|---|---|---|
| Self-perceived risk for COVID-19: | ||||
| I am at risk for COVID-19 | 1 | 0 | 0 | |
| I am not at risk for COVID-19 | 1.74 (1.24, 2.45) | 0.001 | 5.6 | 6 |
| Don’t know | 1.40 (0.96, 2.05) | 0.084 | 3.4 | 3 |
| COVID-19 vaccine effectiveness: | ||||
| Vaccine will prevent COVID-19 | ||||
| Yes | 1 | 0 | ||
| No | 3.10 (2.23, 3.89) | <0.001 | 10.8 | 11 |
| Don’t know | 1.94 (1.34, 2.81) | <0.001 | 6.6 | 7 |
| Vaccine will prevent dying from COVID-19 | ||||
| Yes | 1 | 0 | 0 | |
| No | 3.45 (2.62, 4.56) | <0.001 | 12.4 | 12 |
| Don’t know | 2.22 (1.50, 3.28) | <0.001 | 8.0 | 8 |
| COVID-19 vaccine safety | ||||
| Vaccine is not safeb | ||||
| No | 1 | 0 | ||
| Yes | 2.10 (1.63, 2.68) | <0.001 | 7.4 | 7 |
| Vaccine may kill | ||||
| No | 1 | |||
| Yes | 1.55 (1.20, 2.03) | 0.001 | 4.4 | 4 |
| Other barriers | ||||
| Religious believes (txt) | ||||
| No | 1 | 0 | 0 | |
| Yes | 2.69 (1.37, 5.25) | 0.004 | 9.9 | 10 |
| Presence of health issuesc | ||||
| No | 1 | |||
| Yes | 1.75 (1.05, 2.91) | 0.031 | 5.6 | 6 |
CI, confidence interval.
Odds ratios were adjusted for age, sex, area of residency, level of education, medical insurance.
Severe side-effects.
Including HIV, tuberculosis, diabetes, hypertension, and allergy.
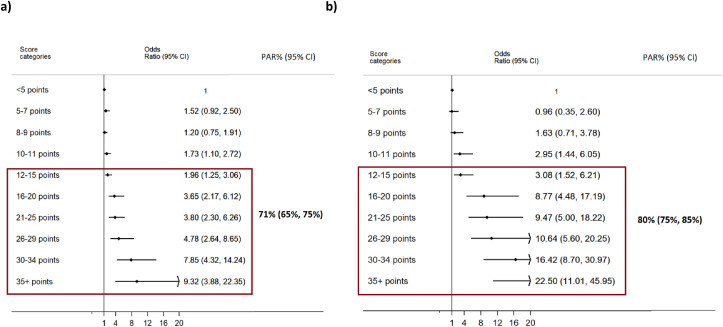
Fig. 1a presented the aORs across the deciles of the risk scores of being unvaccinated (Fig. 1a). There was a linear trend between the individuals’ increasing risk score and the odds of being unvaccinated (Ptrend <0.001). In our secondary outcome, similar increasing trends in odds ratios were observed to predict those who indicated not to get vaccinated in survey 1 (Fig. 1b). Performance of the risk prediction models for several cut-points is presented in Table 3 for the development and the internal validation data sets. A score of 12 or more had high sensitivity. Participants who scored 16–20 points were approximately four times more likely to be unvaccinated in survey 2. They were also almost nine times more likely to be vaccine hesitant in survey 1. Sensitivity/specificity and the discriminative power of those with a score ≥16 points, which requires at least two items from the risk prediction model and also falls into the sixth deciles of the total risk score, were statistically acceptable. Modifying of scores 12 or more would have prevented 71% of the unvaccinated individuals, and 80% of the vaccine-hesitant participants would also be prevented. (Fig. 2 )
Fig. 1.
Odds ratios (95% confidence intervals) of risk score (in deciles): test for trend in odds ratios were <0.001 (for both outcomes). (a) Primary outcome: unvaccinated vs vaccinated. (b) Secondary outcome: intention to get vaccinated (No vs Yes). PAR%, population attributable risk percent.
Table 3.
Performance of the risk scoring algorithm for different cut-points for not getting vaccinated: development and internal validation datasets.
|
Score |
Model: outcome= unvaccinated vs vaccinated AUCa(95% CI): 75% (95% CI: 72%, 78%) |
|
|
Median (IQR) |
25 (12-35) points |
|
|
Cut points |
Sensitivity (Specificity) |
Correctly classified |
| ≥ 10 points | 88% (29%) | 72% |
| ≥ 11 points | 86% (30%) | 72% |
| ≥ 12 points | 85% (36%) | 71% |
| ≥ 13 points | 84% (39%) | 70% |
| ≥ 14 points | 83% (40%) | 70% |
| ≥ 15 points | 82% (41%) | 69% |
| ≥ 16 points | 81% (43%) | 68% |
| ≥ 17 points | 80% (45%) | 67% |
| ≥ 18 points | 78% (45%) | 66% |
|
Internal validationb= unvaccinated vs vaccinated AUC a (95% CI): 71% (95% CI: 69%, 74%) |
||
| Score |
Sensitivity (Specificity) |
Correctly classified |
| ≥ 10 points | 94% (20%) | 57% |
| ≥ 11 points | 91% (23%) | 61% |
| ≥ 12 points | 88% (45%) | 64% |
| ≥ 13 points | 87% (40%) | 65% |
| ≥ 14 points | 85% (47%) | 63% |
| ≥ 15 points | 81% (50%) | 60% |
| ≥ 16 points | 78% (55%) | 59% |
| ≥ 17 points | 76% (58%) | 55% |
| ≥ 18 points | 76% (63%) | 50% |
AUC, Area Under the curve.
Internal validation was conducted using 500 test datasets generated with replacement.
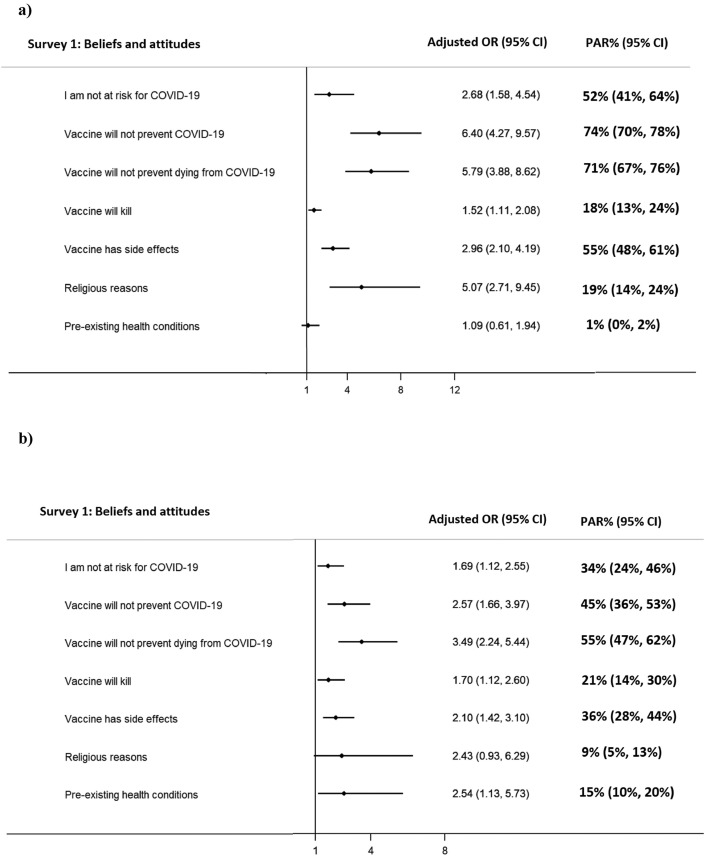
Fig. 2.
Individual and population-level impacts of beliefs and attitudes on unvaccinated individuals: (a) Age: <40 years (full §: 83%, 95% CI: 79%, 87%). CI, confidence interval; PAR%, population attributable risk percent.
Population-level impacts of perceived risk and beliefs: age-specific analysis
In an age-specific analysis, we estimated the population-level impacts of all seven beliefs and attitudes on vaccine uptake when they were considered individually and collectively. Overall, three items: (1) low perceived risk, (2) vaccine will not prevent COVID-19, and (3) vaccine will not prevent dying from COVID-19 were all identified as the most influential beliefs and attitudes on vaccine decision-making. After adjusting and accounting for their correlation structure, their population-level impacts ranged from 50% to 60% and 34% to 55% for younger (aged <40 years) and older (≥40 years). Modifying these three attitudes would have prevented (at least theoretically) 78% and 62% of the unvaccinated individuals in the younger and older groups, respectively (data not shown).
We also observed age-related disparities where 15% of the unvaccinated individuals in the older age group were exclusively associated with those who indicated to have had pre-existing health conditions, whereas only 2% of the unvaccinated younger individuals attributed to pre-existing conditions. The population-level impact of all seven items on vaccination status were estimated as 83% (95% CI: 79%, 87%; <40 years) and 72% (95% CI: 66%, 78%; ≥40 years all). These seven beliefs also had a substantial impact on vaccine hesitancy in both age groups, where lower self-perceived risk and vaccine confidence were identified as the most influential factors in the decision-making process.
Discussion
Our findings provided compelling evidence for a high proportion of unvaccinated adults in a cohort of Black South Africans who participated in two consecutive rounds of national surveys conducted in November 2021 and February to March 2022. More than half of the survey 1 participants indicated that they would get vaccinated; however, only 24% of the study participants reported being vaccinated in survey 2. While age and sex distributions did not differ significantly by vaccination status, unvaccinated individuals appeared to have higher socio-economic status with higher levels of education and income. Some of these findings have been reported previously in other populations including South Africa. For example, vaccine acceptability was associated with higher education in South Africa.18 , 20 However, this link was not consistently confirmed in other populations where higher socio-economic conditions and higher education were reported to be associated with high rates of vaccine acceptability.26 This trend has been documented with childhood vaccination, where parents of higher socio-economic status were more likely to be hesitant in vaccinating their child.27 , 28 These results may be interpreted as increasing vaccine hesitancy in adults who had higher socio-economic conditions.
The present study showed that COVID-19 vaccine hesitancy could be predicted by individuals’ self-perceptions with statistically acceptable robustness and accuracy. We identified the seven most influential beliefs and attitudes for not being vaccinated and their combined population-level impacts and implications on vaccine uptake. In our risk prediction model, low-risk self-perception, lack of trust, and concerns around safety, religion, and pre-existing health conditions were all determined to be the most significant predictors of not being vaccinated, with weighted scores ranging from 4 to 12. Although these factors have been well recognized and reported as the most common reasons for vaccine hesitancy in other worldwide, their population-level influence on vaccine decision-making using weighted and clustering impacts are unique to the present study.
Despite undisputable evidence for vaccine protection against COVID-19-related adverse health outcomes and death, approximately half of the study population had concerns regarding the vaccine efficacy and lack of trust, that is, “vaccine will not prevent COVID-19” and “Vaccine will not prevent dying from COVID-19.” Meanwhile, 60% of the study population reported that they were not at risk of COVID-19. These three factors were identified as the most influential beliefs on vaccine decision-making and were collectively associated with 76% (<40 years) and 62% (≥40 years) of the unvaccinated individuals. Considering the impact of concerns around the safety of the vaccines and the other factors, including “religion” and “pre-existing conditions,” increased the population attributable risk percent to 83% (<40 years) and 72% (≥40 years), respectively. These relatively modest increases were primarily because of the strong correlations between these beliefs and attitudes, which is not surprising. Despite having significant odds ratios, the population-level impact of “religion” on vaccination status was substantially lower compared with the other factors. This was because of the very low prevalence (6%) associated with this factor. These estimates can be translated into 869 more vaccinated individuals (940 × 83% = 780 and 123 × 72% = 89 for <40 and ≥40 years, respectively). Therefore, if it was possible to change these factors (at least theoretically), the proportion of vaccinated individuals would increase from 24% (336/1399) to 86% [(336 + 869)/1399]. Meanwhile, “pre-existing health conditions” only had a modest impact among the older participants. Other factors including “lack of knowledge where to go” and “travel difficulties and expenses” were reported in ≤20% of the study population in survey 1; however, these individuals were significantly more likely to get vaccinated compared with those who knew where to go and did not indicate any difficulties in traveling.
Our findings provide empirical evidence for a substantial shift in vaccine acceptability over time in South Africa, which was also reported in other countries. For example, less than 40% of the survey 1 participants indicated that “they would get vaccinated as soon as possible” in survey 1, which is substantially lower than reported in national surveys conducted before vaccine development and availability. For example, 82% of the South Africans who participated to in the “COVID-SCORE Global Survey,” which was conducted 3 months after the COVID-19 was declared as pandemic, indicated that “they intend to get vaccinated when vaccines become available” (June 2020) (Lazarus et al., 2020; NDoH 2021). High vaccine acceptability rates were also reported in “The Council for Medical Schemes (CMS)” (82%) and “National Income Dynamic Survey-Coronavirus Rapid Mobile Survey” (NIDS-CRAM)” (71%), which were both conducted before/during vaccine approval and roll-out in South Africa (February/March 2021).31 , 32 These estimates were comparable with the other countries, including China (91.3%), the United Kingdom (79.2%), the United States (67%) and other European countries (74%) which were all reported approximately at the same time periods.15, 16, 17 , 26
More than two-and-half years into the pandemic, South Africa continues to have a high burden of infections where the country has already faced multiple variants of COVID-19 infections. However, as of July 2022, <40% of the South Africans had at least one dose compared with 66.9% global average.6 The reasons for low vaccination rates in Black South Africans are likely to be different from other countries, with implications exclusively for this population. One of the marked results from our study is the impact of vaccine-related misconceptions, such as the vaccine will prevent getting “infected” and “dying” from COVID-19. Although these two concepts are different from each other, 83% of the study population who indicated that the vaccine would not prevent getting infected also believe that the vaccine would not prevent dying from COVID-19. There is an undisputable evidence for the vaccines’ key role in reducing COVID-19 and preventing related severe adverse events, including hospitalization and deaths.32 , 33 These findings have significant clinical and public health implications in South Africa where more than 300,000 excess deaths occurred over the past 12 months (June 2021 to June 2022) were reported to be primarily attributed to the COVID-19 infections.30
Limitations
Our study has several limitations. We only included the subset of the data from Black African men and women due to the low proportion of the other population groups. We were only able to analyze the available data. All the characteristics, beliefs, and attitudes were self-reported, including the vaccination status, therefore subject to recall bias. Risk scoring model was developed using cross-sectional data, which shares the same limitations associated with this design. Among those who participated in survey 1, only 1,772 (50%) of them also participated in survey 2. Therefore, the results cannot be generalized to the target population. However, our findings are exclusively unique to the Black South African men and women with the highest burden of other comorbidities, including HIV and tuberculosis.
Conclusion
The present study brings significant insight into the previous research and provides the associations between self-perceptions, beliefs, and attitudes on vaccine decision-making using the first and the most recent data from South Africans following the vaccine roll-out. Our findings particularly highlighted the most influential concerns around vaccine efficacy and safety and their population-level impacts on vaccine decision-making, which are likely to have significant public health implications exclusively for this population. One of the most significant results from this study was the considerable drop in vaccine acceptability since the vaccines have become widely available. This is particularly worrisome, given the high excess mortality rates that have been documented in the region. Given the ongoing nature of the pandemic, widespread misinformation and disinformation, factors contributing to variations in coverage are likely to be complex and nuanced for any vaccine; the COVID-19 vaccine is no exception. Taken together, our findings suggest that vaccine promotion and delivery programs should include a focus on the key role of vaccines in preventing COVID-19-related severe illnesses, hospitalization, and death.
Author statements
Ethical approval
Approval for the primary study was granted by the Ethics Committee of the University of Cape Town. The present study is used an open access (publicly available) data set and does not require further ethical approval.
Funding
The present study used the secondary data did not receive funding. However, the original study was funded by the Bill & Melinda Gates Foundation. Surveys were undertaken by the Southern Africa Labour and Development Research Unit (University of Cape Town).
Competing interests
None declared.
Participant's involvement/informed consent
CVACS data were collected using telephone surveys. Therefore, a verbal consent obtained from the participants by asking if they want to participate the survey. Those who said “yes” were included in the surveys.
Data availability
Publicly available data can be requested and accessed via https://www.datafirst.uct.ac.za/
Availability of data and material (data transparency)
Appendix 2a and b presented the methodology and the SAS Macro developed by the first author of the present article to estimate the “Population Attributable Risk” in multifactorial settings.
Author contributions
H.W., C.V., S.N., and J.M. prepared the concept sheet. H.W. and T.R. extracted database. H.W. and T.R. analyzed the data. H.W. and C.V. prepared the first draft. All authors interpreted the results. All authors approved the final version.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2023.01.007.
Appendix A. Supplementary data
The following are the Supplementary data to this article.
References
- 1.Wand H., Morris N., Reddy T. Temporal and spatial monitoring of HIV prevalence and incidence rates using geospatial models: results from South African women. Spat Spatio-temporal Epidemiol. 2021;37 doi: 10.1016/j.sste.2021.100413. [DOI] [PubMed] [Google Scholar]
- 2.UNAIDS Report 2017. https://www.unaids.org/en/regionscountries/countries/southafrica Geneva, Switzerland.
- 3.Ngangue P., Pilabré A.H., Barro A., Pafadnam Y., Bationo N., Soubeiga D. Public attitudes towards COVID-19 vaccines in Africa: a systematic review. J Publ Health Afr. 2022;13(1):2181. doi: 10.4081/jphia.2022.2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sen-Crowe B., McKenney M., Elkbuli A. Disparities in global COVID-19 vaccination rates & allocation of resources to countries in need. Ann Med Surg. 2021;68 doi: 10.1016/j.amsu.2021.102620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rydland H.T., Friedman J., Stringhini S., Link B.G., Eikemo T.A. The radically unequal distribution of COVID-19 vaccinations: a predictable yet avoidable symptom of the fundamental causes of inequality. Humanit Soc Sci Commun. 2022;9:61. doi: 10.1057/s41599-022-01073-z. [DOI] [Google Scholar]
- 6.World Health Organization (WHO). COVID-19 vaccine tracker and landscape. (Accessed July 2022). https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines.
- 7.Zarębska-Michaluk D., Rzymski P., Moniuszko-Malinowska A., Brzdęk M., Martonik D., Rorat M., et al. Does hospitalization change the perception of COVID-19 vaccines among unvaccinated patients? Vaccines. 2022;10(3):476. doi: 10.3390/vaccines10030476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Plumb I.D., Feldstein L.R., Barkley E., Posner A.B., Bregman H.S., Hagen M.B., et al. Effectiveness of COVID-19 mRNA vaccination in preventing COVID-19–associated hospitalization among adults with previous SARS-CoV-2 infection — United States, June 2021–February 2022. MMWR Morb Mortal Wkly Rep. 2022;71:549–555. doi: 10.15585/mmwr.mm7115e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization (WHO) 2021. Classification of Omicron (B.1.1.529): SARS-CoV-2 variant of concern. Geneva, Switzerland (Accessed July 2022. [Google Scholar]
- 10.World Health Organization (WHO) 2021. Update on Omicron. Geneva, Switzerland: 2021 (Accessed July 2022) [Google Scholar]
- 11.Callaway H. Ledford. How bad is Omicron? What scientists know so far. Nature. 2021;600:197–199. doi: 10.1038/d41586-021-03614-z. [DOI] [PubMed] [Google Scholar]
- 12.Serwaa D., Lamptey E., Senkyire E.K. Increasing COVID-19 vaccine acceptance among the general population while maintaining autonomy. Hum Vaccines Immunother. 2021;17(12):5139–5141. doi: 10.1080/21645515.2021.1922265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris J.N., Mauro C., Andresen J.A., Zimet G.D., Rosenthal S.L. COVID-19 vaccine uptake and attitudes towards mandates in a nationally representative U.S. sample. J Behav Med. 2022 doi: 10.1007/s10865-022-00317-2. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooper S., van Rooyen H., Wiysonge C.S. COVID-19 vaccine hesitancy in South Africa: how can we maximize uptake of COVID-19 vaccines? Expert Rev Vaccines. 2020;20(8):921–933. doi: 10.1080/14760584.2021.1949291. [DOI] [PubMed] [Google Scholar]
- 15.Sethi S., Kumar A., Mandal A., Shaikh M., Hall C.A., Kirk J., et al. The UPTAKE study: a cross-sectional survey examining the insights and beliefs of the UK population on COVID-19 vaccine uptake and hesitancy. BMJ Open. 2021;11(6) doi: 10.1136/bmjopen-2021-048856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang J., Jing R., Lai X., Zhang H., Lyu Y., Knoll M.D., et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. 2020;8:482. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel J., et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21:977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burger R., Christian C., Maughan-Brown B., Rensburg R., Rossouw L. 2020. COVID-19 risk perception, knowledge and behaviour. National Income Dynamics Study- Coronavirus Rapid Mobile Survey.https://cramsurvey.org/wp-content/uploads/2020/07/Burger-COVID19-risk-perception-knowledge-and-behaviour.pdf (Cited 2022 June17). Available from: [Google Scholar]
- 19.Robinson E., Jones A., Lesser I., Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021;39(15):2024–2034. doi: 10.1016/j.vaccine.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wiysonge C.S., Ndwandwe D., Ryan J., Jaca A., Batouré O., Anya B.M., et al. Vaccine hesitancy in the era of COVID-19: could lessons from the past help in divining the future? Hum Vaccines Immunother. 2022;18(1):1–3. doi: 10.1080/21645515.2021.1893062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.COVID-19 vaccine survey (CVACS) 2021, Survey 1 [Dataset] DataFirst [Distributor]; Cape Town: 2022. Version 1.1.0. Cape Town: Bill and Melinda Gates Foundation [Funding Agency]. Cape Town: Southern Africa Labour and Development Research Unit [Producer], 2021. [DOI] [Google Scholar]
- 22.COVID-19 vaccine survey (CVACS) 2022, survey 2 [Dataset] DataFirst [Distributor]; Cape Town: 2022. Version 1. Cape Town: Bill and Melinda Gates Foundation [Funding Agency]. Cape Town: Southern Africa Labour and Development Research Unit [Producer], 2022. [DOI] [Google Scholar]
- 23.Wand H., Vujovich-Dunn C., Moodley J., Reddy T., Naidoo S. Developing and validating risk algorithm for hypertension in South Africa: results from a nationally representative cohort (2008–2017) High Blood Press Cardiovasc Prev. 2022 doi: 10.1007/s40292-022-00534-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spiegelman D., Hertzmark E., Wand H.C. Point and interval estimates of partial population attributable risks in cohort studies: examples and software. CCC (Cancer Causes Control) 2007;18(5):571–579. doi: 10.1007/s10552-006-0090-y. [DOI] [PubMed] [Google Scholar]
- 26.Swaney S.E., Burns S. Exploring reasons for vaccine-hesitancy among higher-SES parents in Perth, Western Australia. Health Promot J Aust. 2019;30(2):143–152. doi: 10.1002/hpja.190. [DOI] [PubMed] [Google Scholar]
- 27.Fielding J.E., Bolam B., Danchin M.H. Immunisation coverage and socioeconomic status - questioning inequity in the 'No Jab, No Pay' policy. Aust N Z J Publ Health. 2017;41(5):455–457. doi: 10.1111/1753-6405.12676. [DOI] [PubMed] [Google Scholar]
- 28.South African Medical Research Council (samrc.ac.za) Report on Weekly Deaths in South Africa | South African Medical Research Council (samrc.ac.za) (Accessed June 2022).
- 30.Narnia B., Roberts B., Alexander K., Runciman C., Mchunu N. 2021. A hesitant nation? Survey shows potential acceptance of a COVID-19 vaccine in South Africa. Maverick Citizen [Internet] (2021). (Accessed May 2022) [Google Scholar]
- 31.Runciman C., Alexander K., Bekker M., Bohler-Muller N., Roberts B., Mchunu N. 2021. SA survey sheds some light on what lies behind coronavirus vaccine hesitancy. Daily Maverick [Internet]. (Accessed May 2022). [Google Scholar] [Google Scholar]
- 32.Mohammed I., Nauman A., Paul P., Ganesan S., Chen K.H., Jalil S.M.S., et al. The efficacy and effectiveness of the COVID-19 vaccines in reducing infection, severity, hospitalization, and mortality: a systematic review. Hum Vaccines Immunother. 2022;18:1. doi: 10.1080/21645515.2022.2027160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lazarus J.V., Ratzan S., Palayew A., Billari F.C., Binagwaho A., Kimball S. COVID-SCORE: a global survey to assess public perceptions of government responses to COVID-19 (COVID-SCORE-10) PLoS One. 2020;15(10) doi: 10.1371/journal.pone.0240011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Publicly available data can be requested and accessed via https://www.datafirst.uct.ac.za/