Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) using a lumen-apposing metal stent (LAMS) is a novel endoscopic technique for treating gastric outlet obstruction and represents an alternative to stenting or surgery 1 2 . EUS-GE is minimally invasive and compares favorably with long-term surgical outcomes 1 2 . Several studies report a high degree of technical and clinical success, despite a considerable rate of complications 1 3 .
A 65-year-old woman with generalized breast cancer presented with signs of gastric outlet obstruction, with a tight duodenal stenosis caused by malignant abdominal lymphadenopathy. EUS-GE was performed using LAMS (20 mm Hot Axios Stent; Boston Scientific, Marlborough, Massachusetts, USA), resulting in immediate resumption of oral intake ( Fig. 1 , Video 1 ). Correct positioning of the stent in the small intestine was documented endoscopically and radiologically.
Fig. 1.
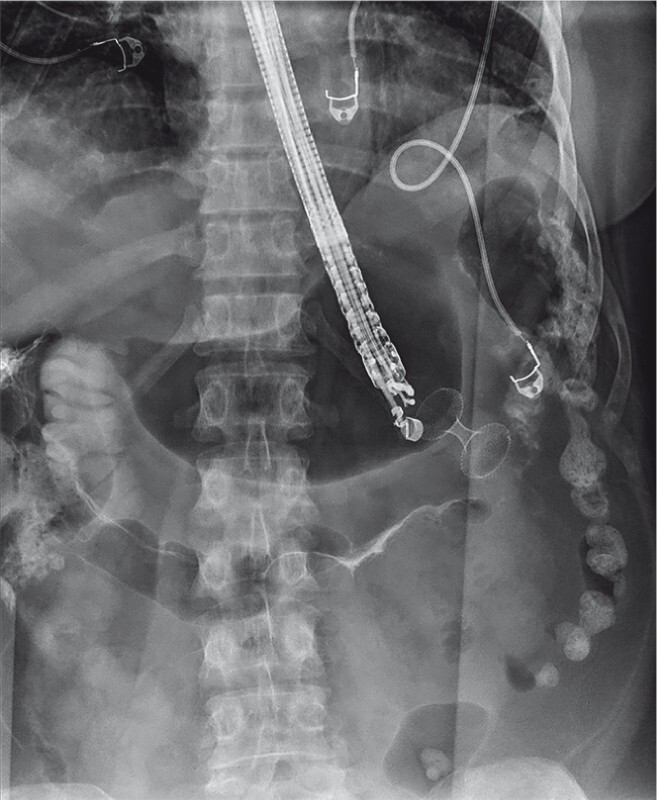
Fluoroscopy image showing the correct placement of a lumen-apposing metal stent during endoscopic ultrasound-guided gastroenterostomy. The anastomosis was created between the stomach and the proximal jejunum.
Video 1 Gastrojejunocolic fistula as an unusual late complication of endoscopic ultrasound-guided gastroenterostomy.
However, 4 months later, the patient complained of dyspeptic symptoms. Gastroscopy was performed, revealing a normal anastomosis with two jejunal loops ( Fig. 2 , Video 1 ). Then, 2 months later, gradual development of anorexia, diarrhea, and fecal vomiting was observed. A computed tomography scan indicated possible communication of the stent with the colon ( Fig. 3 , Video 1 ). Gastroscopy showed a patent anastomosis between the stomach and jejunum as well as the large intestine. We extracted the LAMS and closed the gastric orifice of the anastomosis with an over-the-scope clip (OTSC; Ovesco Endoscopy GmbH, Tübingen, Germany), through-the-scope clips, and endoloop ( Video 1 ), leading to immediate remission of vomiting and significant improvement in diarrhea. Due to ongoing oncological treatment and regression of abdominal lymphadenopathy, restoration of gastrointestinal tract continuity was not necessary. Although an improvement in condition enabled chemotherapy for an additional 3 months, the patient eventually died of disease progression.
Fig. 2.
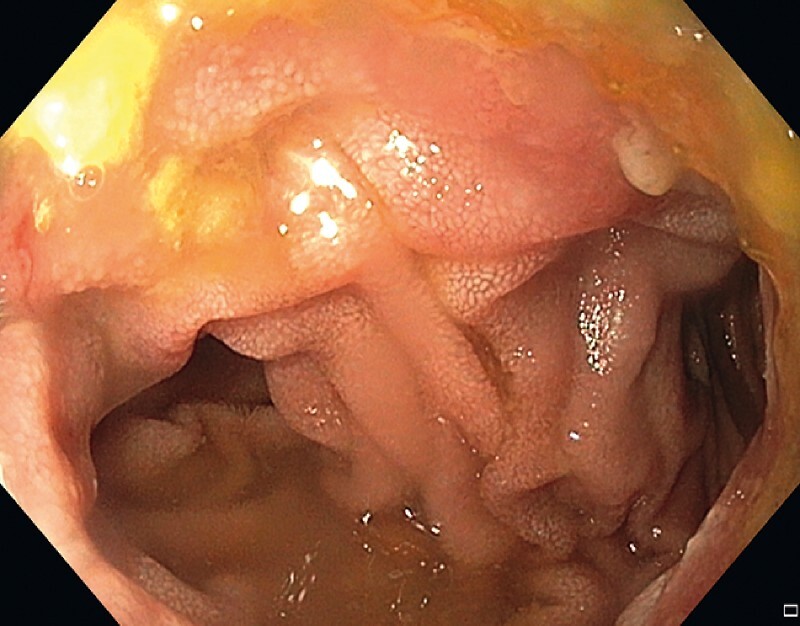
Endoscopic view from the stomach into two loops of the jejunum 4 months after creating the anastomosis.
Fig. 3.

Computed tomography scan showing communication between the stomach and colon (arrow).
Endoscopic closure of a gastrocolic fistula following EUS-GE has been successfully performed using a suturing device 4 . Another report described gastrojejunocolic fistula as a rare complication of surgical gastroenterostomy 5 . However, our report is the first to document gastrojejunocolic fistula following EUS-GE, which we successfully resolved with endoscopic treatment.
Endoscopy_UCTN_Code_CPL_1AH_2AD
Footnotes
Competing interests The authors declare that they have no conflict of interest.
Endoscopy E-Videos : https://eref.thieme.de/e-videos .
Endoscopy E-Videos is an open access online section, reporting on interesting cases and new techniques in gastroenterological endoscopy. All papers include a high quality video and all contributions are freely accessible online. Processing charges apply (currently EUR 375), discounts and wavers acc. to HINARI are available. This section has its own submission website at https://mc.manuscriptcentral.com/e-videos
References
- 1.Itoi T, Ishii K, Ikeuchi N et al. Prospective evaluation of endoscopic ultrasonography-guided double-balloon-occluded gastrojejunostomy bypass (EPASS) for malignant gastric outlet obstruction. Gut. 2016;65:193–195. doi: 10.1136/gutjnl-2015-310348. [DOI] [PubMed] [Google Scholar]
- 2.McCarty T R, Garg R, Thompson C C et al. Efficacy and safety of EUS-guided gastroenterostomy for benign and malignant gastric outlet obstruction: a systematic review and meta-analysis. Endosc Int Open. 2019;7:1474–1482. doi: 10.1055/a-0996-8178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kastelijn J B, Moons L MG, Garcia-Alonso F J et al. Patency of endoscopic ultrasound-guided gastroenterostomy in the treatment of malignant gastric outlet obstruction. Endosc Int Open. 2020;8:1194–1201. doi: 10.1055/a-1214-5659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pham K D, Havre R F. Endoscopic management of gastrocolic fistula after endoscopic ultrasound-guided gastrojejunostomy (EUS-GJ) Endoscopy. 2019;51:169. doi: 10.1055/a-0871-1629. [DOI] [PubMed] [Google Scholar]
- 5.Kece C, Dalgic T, Nadir I et al. Current diagnosis and management of gastrojejunocolic fistula. Case Rep Gastroenterol. 2010;4:173–177. doi: 10.1159/000314048. [DOI] [PMC free article] [PubMed] [Google Scholar]


