A 44-year-old man went to the local hospital with a 3-day history of nausea, vomiting, abdominal pain, and difficulty eating after drinking. Gastrointestinal endoscopy showed a kidney-shaped bezoar obstructing the esophagus at 30 cm from incisors. On esophagography, the esophageal walls were seen to be stretched thin by the large bezoar ( Fig. 1 ). Computed tomography scanning showed that the bezoar, which was located in the lower esophagus, was about 30-mm wide, 25 mm in the anteroposterior direction, and 53 mm in length ( Fig. 2 a, b ). Multiplanar reformation showed that the bezoar was close to the major blood vessels and heart ( Fig. 2 c ).
Fig. 1.
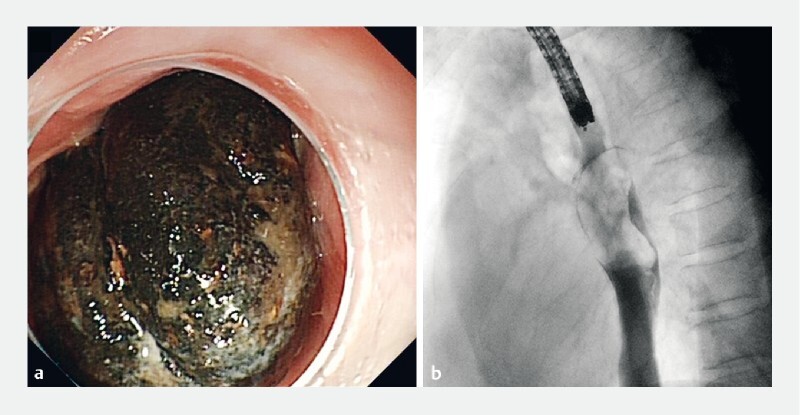
A large kidney-shaped bezoar that was obstructing the esophagus is seen on: a endoscopy; b fluoroscopy.
Fig. 2.
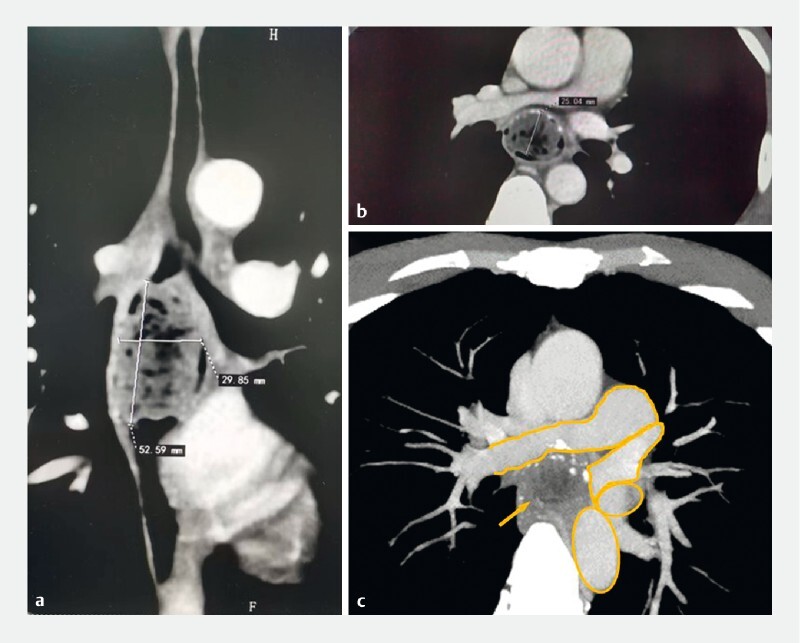
Computed tomography scan images showing: a, b a large bezoar (about 30 × 25 × 53 mm) in the lower esophagus; c on multiplanar reformation (MPR), that the bezoar was very close to the major blood vessels and heart (circled in orange, from top to bottom: right pulmonary trunk; left superior pulmonary vein; left atrium; thoracic aorta).
On day 4 of admission, the patient underwent laser lithotripsy. After the bezoar had been partially broken up by the lithotripsy, we attempted removal with a wire-guided retrieval basket and snare, but neither were successful ( Video 1 ). Laser lithotripsy was performed again. The broken bezoar fragments were then pushed into the stomach and crushed by the wire-guided retrieval basket. Once the bezoar had been removed from the esophagus, multiple ulcers, including two large ones, were seen at 30–36 cm from the incisors ( Fig. 3 a ). Following the lithotripsy procedure, the patient was treated with sodium bicarbonate to facilitate dissolution of the bezoars. At follow-up 1 month later, gastroscopy showed that the bezoars had disappeared and the esophageal ulcers were well healed ( Fig. 3 b ).
Fig. 3.
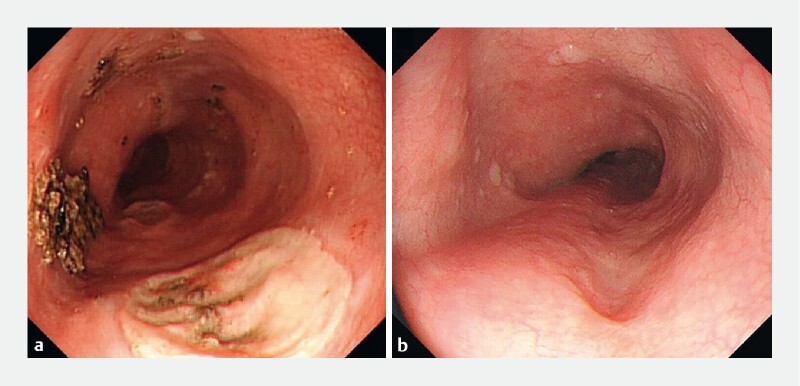
Endoscopic views showing: a two large ulcers in the esophagus; b good healing of the ulcers on follow-up 1 month later.
Video 1 Endoscopic laser lithotripsy is performed to remove a large esophageal bezoar.
Esophageal bezoars are rare, in contrast to the more common gastric bezoars. Esophageal bezoars are often associated with mechanical obstruction of the esophagus or reflux of gastric bezoars 1 2 . A bezoar that lodges in the esophagus often causes acute obstruction; its most acute onset can cause chest pain and difficulty in swallowing. If the bezoar is incarcerated in the esophagus for a longer time, the esophageal wall can ulcerate, bleed, and even perforate 3 . Usually, a wire-guided retrieval basket or snare is used as the first approach for foreign body removal in the esophagus 4 5 ; however, alternative methods to manage large foreign bodies should be considered. As in our case, the hard bezoar was huge and near to large blood vessels. The risk of esophageal perforation or blood vessel rupture meant that conventional treatment was difficult, which was the main reason we chose to use laser lithotripsy.
Endoscopy_UCTN_Code_TTT_1AO_2AL
Footnotes
Competing interests The authors declare that they have no conflict of interest.
Endoscopy E-Videos : https://eref.thieme.de/e-videos .
Endoscopy E-Videos is an open access online section, reporting on interesting cases and new techniques in gastroenterological endoscopy. All papers include a high quality video and all contributions are freely accessible online. Processing charges apply (currently EUR 375), discounts and wavers acc. to HINARI are available. This section has its own submission website at https://mc.manuscriptcentral.com/e-videos
References
- 1.Kim K H, Choi S C, Seo G S et al. Esophageal bezoar in a patient with achalasia: case report and literature review. Gut Liver. 2010;4:106–109. doi: 10.5009/gnl.2010.4.1.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hashmi S, Dimino J, Shady A et al. A case of megaesophagus secondary to a massive phytobezoar in a patient with achalasia. Cureus. 2022;14:e23061. doi: 10.7759/cureus.23061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hernandez P V, Snyder D L, Ghorab S et al. Removal of a large stone in the upper thoracic esophagus. Mayo Clin Proc Innov Qual Outcomes. 2020;4:105–108. doi: 10.1016/j.mayocpiqo.2019.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chirica M, Kelly M D, Siboni S et al. Esophageal emergencies: WSES guidelines. World J Emerg Surg. 2019;14:26. doi: 10.1186/s13017-019-0245-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birk M, Bauerfeind P, Deprez P H et al. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:489–496. doi: 10.1055/s-0042-100456. [DOI] [PubMed] [Google Scholar]


