Abstract
Objective
Sparse patterns in fixed-terrestrial broadband internet access are predominantly observed among older adults and low income areas, which are interrelated factors also associated with low center-based cardiac rehabilitation (CR) utilization in the United States (US). Telehealth CR is proposed to increase CR utilization under an assumption that fixed-terrestrial broadband internet access is readily available nationwide and parallels CR utilization demand. We aimed to characterize national, geographical, and urban-rural patterns in fixed-terrestrial broadband internet access, CR eligibility rates, and center-based utilization throughout the US.
Methods
Centers for Disease Control data were used to estimate CR eligibility rates and center-based utilization for 2017-2018 among Medicare fee-for-service beneficiaries aged ≥65 years. Census Bureau data for 2018 were used to estimate fixed-terrestrial broadband internet access among households of adults aged ≥65 years.
Results
Southern states exhibited the highest percentage of households without broadband internet [median (IQR): 32% (24-39)] coupled with the highest CR eligibility rates [per 1,000 beneficiaries, median (IQR): 18 (15-21)] and lowest participation rates [percentage completing ≥1 session, median (IQR): 25% (17-33)]. Compared with urban areas, rural areas demonstrated significantly higher eligibility rates [15.5 (13.2-18.4) vs. 17.4 (14.5-21.0)], participation rates [30.6% (22.0-39.4) vs. 34.6% (22.6-48.3)], and percentage of households without broadband internet [23.8% (18.1-29.2) vs. 31.6% (26.5-37.6)], respectively.
Conclusion
Overlapping patterns in fixed-terrestrial broadband internet access and CR eligibility rates and center-based utilization suggest telehealth CR policies need to account for the possibility that lack of broadband-quality internet access could be a barrier to accessing telehealth CR delivery models.
Keywords: Digital health, Home-based cardiac rehabilitation, Remote cardiac rehabilitation, Hybrid cardiac rehabilitation, Telehealth, Virtual cardiac rehabilitation
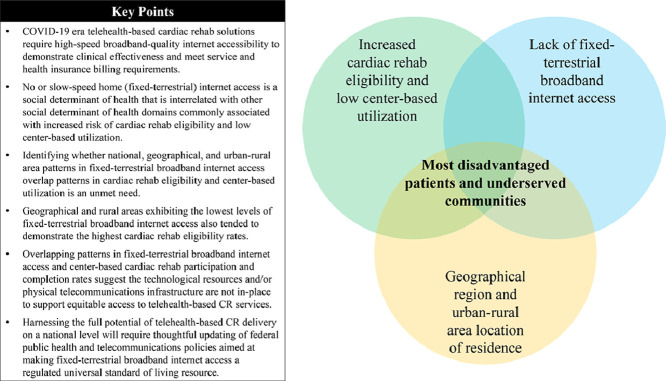
Graphical abstract
1. Introduction
The extraordinary circumstances of the COVID-19 pandemic has left patients who have experienced major heart events facing unpredictable barriers to accessing important outpatient center-based cardiac rehabilitation (CR) heart care [1]. The rapid reaction to the suddenness of inaccessible center-based CR has been to focus on identifying non-center-based telehealth solutions [1], [2], [3], [4], [5], [6], [7], [8]. Proponents of telehealth CR delivery methods have proposed, even before the COVID-19 pandemic, that remote digital health technologies can be used to address many of the well-known barriers predictive of low center-based CR utilization [9,10]. However, to advance the telehealth-based CR initiative in the United States (US) so that it proves beneficial for all patients, there is an urgent need to improve the understanding of national, geographical, and urban-rural disparities in fixed-terrestrial (i.e., home) broadband internet access among adults aged ≥65 years. Patients of this age strata commonly demonstrate an increased risk of coronary artery disease and associated social determinants of health that limit their ability to access and prioritize preventive healthcare [[8], [10], [11], [12], [13], [14], [15], [16], [17]]. Historical trends in secondary cardiovascular disease prevention and center-based CR uptake commonly illustrate patients aged ≥65 years utilize CR less than the already suboptimal levels exhibited by younger counterparts [10,13,18,19].
Contemporary internet capable technologies that are suggested to be pragmatic and generalizable to patients who are eligible to enroll in CR are fundamentally constructed on the need for high-bandwidth strength internet accessibility in order to demonstrate clinical effectiveness and to allow for regulatory requirements to be met. The importance of this digital technological requirement is directly reflected in the key stipulation of the temporary Hospitals without Walls initiative outlined by the US Centers for Medicare & Medicaid Services (CMS) which requires prospective telehealth-based CR enrollees to demonstrate an ability to reliably accommodate real-time two-way audio and video (A/V) telecommunication with qualified healthcare providers for the supervision of exercise sessions [20], [21], [22]. What remains missing from this recent telehealth CR policy is acknowledgement that broadband quality internet inaccessibility has been identified as a type of social determinant of health that is interlinked with well-known factors characterizing low socioeconomic status [11,12,23]. No provisions in current policy outline telehealth CR solutions for patients unable to self-furnish broadband quality internet access.
To date, evidence does not support the assumption that fixed-terrestrial broadband internet is universally available, affordable, and reliable at quality levels that meet or exceed the industry standard of 25 megabits per second (Mbps) and upload rate of 3 Mbps needed for reliable high quality A/V telecommunications services [11,12,23]. Modern US data signals there is sporadic fixed-terrestrial broadband internet accessibility within low income and underserved communities [11,12,23]. The US Federal Communications Commission (FCC) also does not consider marketplace availability of cellular-based internet technologies an adequate like-for-like substitution for fixed-terrestrial broadband internet accessibility and capabilities [11,12,23]. Thus, given these limitations, it is possible that by hurriedly expanding standard- of-care CR to include telehealth services without simultaneously improving the understanding of whether patterns in fixed-terrestrial broadband internet access overlap with those for CR eligibility and utilization, low income patients residing in underserved communities could be left further behind in their ability to achieve healthcare equity. Other consequences could include less than expected improvements in national CR utilization levels and slowed progress made towards developing federal healthcare policies and services aimed at supporting those who require subsidized forms of high-bandwidth internet resources to access telehealth CR services.
In this study we aimed to characterize national, geographical, and urban-rural patterns in fixed-terrestrial broadband internet access, CR eligibility rates, and center-based CR utilization throughout the US.
2. Methods
In this cross-sectional and observational study, we ascertained CR data focused on eligibility rate (per 1,000 beneficiaries) and center-based utilization metrics, including participation rate (% of those eligible who initiated CR by participating in ≥1 session), adherence (mean number of sessions completed within 365 days of a qualifying event), and completion rate (% of enrollees who participated in ≥36 sessions) for Medicare FFS beneficiaries aged ≥65 years who in 2017 to 2018 experienced at least one primary or secondary CR qualifying event described by CMS [24,25]. All CR data analyzed for this study were originally sourced from CMS claims database warehouses by the Centers for Disease Control (CDC), who then generated cleaned datasets as spatially smoothed county-level estimates for all US states and the District of Columbia [25]. Sub-classification criteria used by the CDC to ascertain how patients should be counted towards specific CR metrics were those described in the latest American College of Cardiology and American Heart Association report on CR clinical performance and quality measures [24,25]. No patient-level identifying data describing specific CR qualifying event types and demographic characteristics are provided in CDC public use datasets [25]. Data on the number of hospitals per county offering center-based CR services were also ascertained from the CDC database [25]. All CR data analyzed and reported in this study are publically accessible on the CDC website at no cost to users [25].
We acquired data on internet access/connectivity for occupied housing units where household member(s) were surveyed as part of the ongoing annual US Census Bureau American Community Survey (ACS) [26]. The ACS defines internet that is accessed via cellular carrier and mobile device a form of broadband internet access, but one that is not fixed-terrestrial [26].
Internet access referred to in this study reflects the percentage of households within a given county where ACS respondents provided “YES” or “NO” answers to questions about home computer and internet availability. In brief, a home computer that was available and could be used by anyone residing in the household was defined as any of the following: desktop or laptop, smartphone, tablet or other portable wireless computer, or some other type of computer [26]. A classification of “no home computer” meant an answer of “NO” was given for anyone residing in the household being able to access any computer type. Households of adults aged ≥65 years were defined in this study as exhibiting no fixed-terrestrial broadband internet access if there was either no access to a home computer (as defined above) or dial-up service was the only type of internet access present.
The ACS reports internet access data in 1-year estimates, and in periods where data for a given year of interest is estimated based on rolling 5-year averages [27]. The Census Bureau specifies data reported as periods provide the most reliable datasets and are inclusive of all US counties regardless of population size. Alternatively, ACS data reported in 1-year estimates are described as most recent relative to the year of interest, but also least reliable in accuracy and precision while excluding geographical areas with population sizes <65,000 [27]. Therefore, to optimally match the precision and national representation of county-level data available for CR utilization metrics generated by the CDC [25], we studied internet access data that the Census Bureau estimated for 2018 based on rolling multi-year averages of the 5-year period from 2014 to 2018 [26,27].
No Institutional Review Board review of this study was required since it meets the requirements for exempt status described by the Department of Health and Human Services in 45 Code of Federal Regulations §46.104, subpart A.
2.1. Data processing
We merged CR and internet access datasets based on matching county codes defined in both datasets according to Census 2010 classifications. Geographical boundaries set for county location relative to either the Midwest, Northeast, South, or West region were also those defined by Census 2010 classifications [26]. The classification of county location as representing either a urban or rural area was based on 2013 codes defined by the CDC [28]. A small number of counties (n=111) were excluded from the data merge because not all counties within the US demonstrated large enough populations of Medicare FFS beneficiaries aged ≥65 years and enough CR qualifying events or occurrences for a particular metric for the CDC to generate reliable data estimates for CR eligibility rate, participation rate, adherence, and/or completion rate [25].
2.2. Statistical analyses
We report data as median (IQR) or n (%) where appropriate. General linear model analyses were used to evaluate differences between geographical regions and/or urban-rural areas for dependent variables of interest. General linear modeling utilized either a negative binomial or poisson distribution and log link function, either of which could be determined to provide an optimal fit of the data when the goodness-of-fit chi-square test was not statistically significant at an alpha level of 0.05 coupled with the Hessian convergence criterion limit of 0.0001 not being exceeded. Relying solely on the Hessian convergence criterion to determine model goodness-of-fit can be misleading since not exceeding the limit of 0.0001 only provides information on whether the model fit is generally adequate and converged, not necessarily optimal. Tukey-Kramer post-hoc testing was performed to evaluate pairwise differences only when the Wald Type 3 statistic was significant.
Both univariable and multivariable associations between a particular CR metric and fixed-terrestrial broadband internet access were evaluated using incident rate ratios (IRR) derived from parameter estimates generated from poisson or negative binomial regression analyses. Multivariable regression analyses included evaluating associations between a particular CR metric and the interaction between broadband internet access and either the geographical region or urban-rural area variable. The presence of the interaction term tested whether an association between a particular CR metric and broadband internet access differed by either geographical region or urban-rural area.
Two-tailed significance was determined using an alpha level set at .05. Analyses were performed using SAS v.9.4 (SAS Institute, Cary, NC), from March 2022 to December 2022.
3. Results
3.1. Geographical region disparities
Overall, households of adults aged ≥65 years made up a significantly larger proportion of all households located in Midwestern and Northeastern regions as compared with the Southern region (Table 1). The Midwestern and Northeastern regions also listed the most counties where center-based CR was offered by at least one hospital, which were significantly more frequent in number than that observed for the Southern region (Table 1). Similarly, fixed-terrestrial broadband internet access among households of adults aged ≥65 years was significantly more prevalent throughout Midwestern and Northeastern states as compared with the lowest levels observed across Southern states (Table 1).
Table 1.
Cardiac rehabilitation eligibility, center-based utilization and availability, and fixed-terrestrial broadband internet access.
| Geographical Region | ||||||
|---|---|---|---|---|---|---|
| Entire US | Midwest | Northeast | South | West | P-value | |
| Eligibility rate, median (IQR), per 1000 beneficiaries | 17 (14-20) | 17 (15-20) | 15 (13-18) | 18 (15-21) | 14 (11-16) | <.0001a |
| Counties estimated, No. (%) | 3,031 (97) | 933 (31) | 317 (11) | 1374 (45) | 407 (13) | <.0001 |
| Participation rate, median (IQR), % | 33 (22-44) | 44 (33-55) | 31 (23-41) | 25 (17-33) | 34 (22-44) | <.0001b |
| Counties estimated, No. (%) | 2353 (75) | 842 (36) | 295 (13) | 949 (40) | 267 (11) | <.0001 |
| Mean sessions completed, median (IQR), n | 25 (22-28) | 25 (21-28) | 25 (22-27) | 26 (23-28)c | 25 (21-27) | <.0001 |
| Counties estimated, No. (%) | 2353 (75) | 842 (36) | 295 (13) | 949 (40) | 267 (11) | <.0001 |
| Completion rate, median (IQR), % | 35 (24-46) | 33 (24-45)e | 30 (20-39) | 38 (28-49)d | 31 (18-43) | <.0001 |
| Counties estimated, No. (%) | 1268 (40) | 432 (34) | 180 (14) | 508 (40) | 148 (12) | <.0001 |
| Counties with no hospitals offering center-based CR, No. (%) | 1534 (51) | 329 (35) | 99 (31) | 878 (64)d | 228 (56) i | <.0001 |
| Households per county, median (IQR), n | 10520 (4746-27089) |
9114 (4191-19546)f |
24739 (9160-78594) |
9875 (5151-23594)g |
10017 (3707-37645) |
<.0001 |
| Households of adults ≥65 years of age | ||||||
| Proportion of households, median (IQR), % |
17.9 (15.5-20.5) |
18.2 (16.2-20.4) |
18.5 (16.2-20.7) |
17.6 (15.2-20.0)h |
17.5 (13.7-22.1) |
.0053 |
| Proportion with no fixed-terrestrial BIA, median (IQR), % |
28.8 (22.5-35.1) |
29.3 (25.1-33.6) |
26.4 (20.1-31.4) |
31.7 (24.0-38.7) |
20.6 (15.7-27.1) |
<.0001a |
Abbreviation: BIA, broadband internet access; CR, cardiac rehabilitation; US, United States.
The total number of counties recognized by United States (US) Census 2010 classifications was 3,142. The maximum number of counties where any of the four cardiac rehabilitation (CR) utilization metrics could be estimated for Medicare fee-for-service (FFS) beneficiaries aged ≥65 years was 3,031. For counties where CR utilization data estimates could not be generated for Medicare FFS beneficiaries aged ≥65 years this was because of inadequate population size and/or not enough qualifying events occurred during 2017-2018.
All pairwise differences between regions were significant after Tukey-Kramer post-hoc testing.
All pairwise differences between regions were significant except for Northeast vs. West after Tukey-Kramer post-hoc testing.
South vs. Midwest and West, significantly different after Tukey-Kramer post-hoc testing.
South vs. all regions, significantly different after Tukey-Kramer post-hoc testing.
Midwest vs. Northeast, significantly different after Tukey-Kramer post-hoc testing.
Midwest vs. Northeast and West, significantly different after Tukey-Kramer post-hoc testing.
South vs. Northeast and West, significantly different after Tukey-Kramer post-hoc testing.
South vs. Midwest and Northeast, significantly different after Tukey-Kramer post-hoc testing.
West vs. all regions, significantly different after Tukey-Kramer post-hoc testing.
Medicare FFS beneficiaries aged ≥65 years in the Southern region demonstrated CR eligibility rates that were significantly higher than those of the other geographical regions (Table 1). The highest completion rates also occurred among enrollees in Southern states, and the mean number of sessions completed per enrollee in the Southern region were also among the highest in the country. Alternatively, the lowest overall participation rates occurred in the Southern region.
3.2. Urban-rural disparities
Households of adults aged ≥65 years made up a significantly larger proportion of households located in rural areas as compared with urban areas (Table 2), and this was consistent across geographical regions. Similarly, the proportion of households of adults aged ≥65 years reporting no fixed-terrestrial broadband internet access was significantly larger in rural areas than urban areas (Table 2), regardless of geographical region. There were also significantly more counties in rural areas than urban areas where center-based CR was not offered by at least one hospital (Table 2).
Table 2.
Urban-rural area differences in cardiac rehabilitation eligibility, center-based utilization and availability, and fixed-terrestrial broadband internet access.
| Urban areas | Rural areas | P-value | |
|---|---|---|---|
| Eligibility rate, median (IQR), per 1000 beneficiaries | 15.5 (13.2-18.4) | 17.4 (14.5-21.0) | <.0001 |
| Counties estimated, n (%) | 1154 (38) | 1877 (62) | <.0001 |
| Participation rate, median (IQR), % | 30.6 (22.0-39.4) | 34.6 (22.6-48.3) | <.0001 |
| Counties estimated, n (%) | 1057 (45) | 1296 (55) | <.0001 |
| Mean sessions completed, median (IQR), n | 25.3 (22.6-27.5) | 25.0 (21.1-28.2) | .0661 |
| Counties estimated, n (%) | 1057 (45) | 1296 (55) | <.0001 |
| Completion rate, median (IQR), % | 31.3 (22.0-41.5) | 39.8 (28.6-50.0) | <.0001 |
| Counties estimated, n (%) | 748 (59) | 520 (41) | <.0001 |
| Counties with no hospitals offering center-based CR, No. (%) | 428 (37) | 1106 (59) | <.0001 |
| Households per county, median (IQR), n | 97183 (32267-220265) |
16829 (8384-32529) |
<.0001 |
| Households of adults ≥65 years of age | |||
| Proportion of households, median (IQR), % |
16.1 (13.6-18.3) | 19.0 (16.8-21.6) | <.0001 |
| Proportion with no fixed-terrestrial BIA, median (IQR), % |
23.8 (18.1-29.2) | 31.6 (26.5-37.6) | <.0001 |
Abbreviation: BIA, broadband internet access; CR, cardiac rehabilitation; US, United States. Urban and rural area categories reflect United States (US) Census 2010 geography and urban-rural classification structure defined in 2013 by the National Center for Health Statistics (NCHS). The total number of counties recognized by United States (US) Census 2010 classifications was 3,142. The maximum number of counties where any of the four cardiac rehabilitation (CR) utilization metrics could be estimated for Medicare fee-for-service (FFS) beneficiaries aged ≥65 years was 3,031. For counties where CR utilization data estimates could not be generated for Medicare FFS beneficiaries aged ≥65 years this was because of inadequate population size and/or not enough qualifying events occurred during 2017-2018.
As a whole, Medicare FFS beneficiaries aged ≥65 years residing in rural areas demonstrated significantly higher CR eligibility rates than levels observed for urban areas (Table 2). Rural area residing patients also demonstrated significantly higher participation (initiation) rates and completion rate as compared with levels observed for urban area residents. However, the mean number of sessions completed per enrollee did not significantly differ between urban areas and rural areas.
3.3. Associations between cardiac rehabilitation and broadband internet access
On a national level, for every percentage unit increase in the proportion of households of adults aged ≥65 years reporting no fixed-terrestrial broadband internet access, this was associated with a 1.0 % rise in CR eligibility rate (IRR=1.009, 95%CI 1.000 to 1.011; χ2=344, P<.0001), a -0.34 % decrease in participation rate (IRR=0.997, 95%CI 0.994 to 0.999; χ2=7.85, P=.0051), and a 1.56 % increase in completion rate (IRR=1.016, 95%CI 1.012 to 1.019; χ2=95, P<.0001) among Medicare FFS beneficiaries aged ≥65 years. There was no association between broadband internet access and mean sessions completed (χ2=1.08, P=.2991).
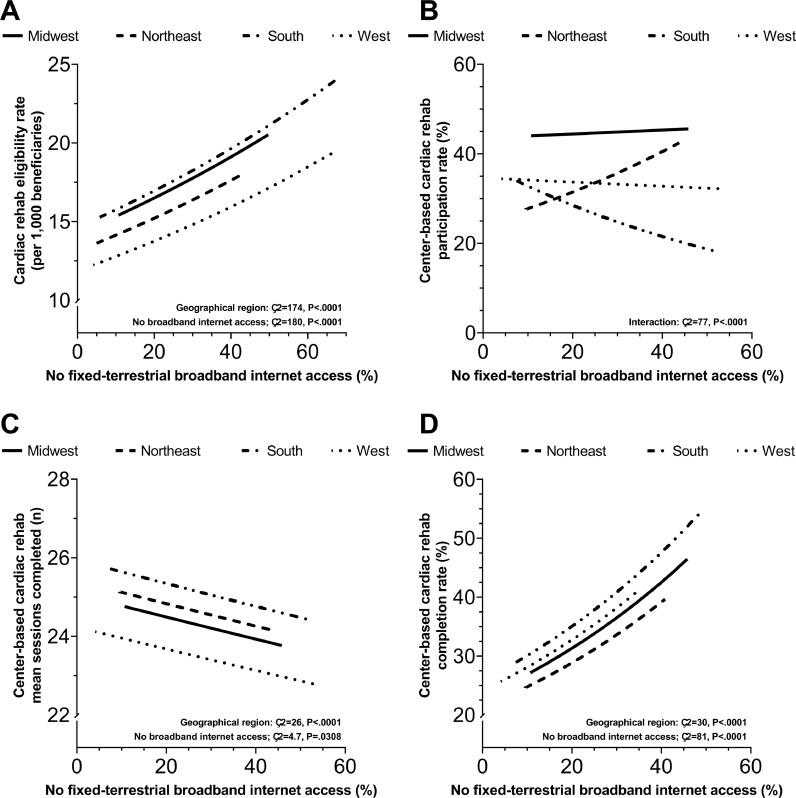
Significant associations between broadband internet access and CR eligibility rate, participation rate, and completion rate persisted after adjusting regressions for geographical region (Fig. 1a, b, and d, respectively). As opposed to the unadjusted regression, the association between broadband internet access and mean sessions completed was significant after adjusting for geographical region (Fig. 1c). However, participation rate was the only CR metric where the significant association with broadband internet access differed by geographical region (Fig. 1b).
Fig. 1.
Associations between cardiac rehabilitation eligibility rate and center-based utilization among Medicare fee-for-service beneficiaries aged ≥65 years and fixed-terrestrial broadband internet access among households of adults aged ≥65 years adjusted for geographical region effects. Eligibility rate (per 1,000 beneficiaries) (A), participation rate (% of those eligible who participated in ≥1 session) (B), adherence (mean number of sessions completed within 365 days of qualifying event) (C), and completion rate (% of enrollees who participated in ≥36 sessions) (D).
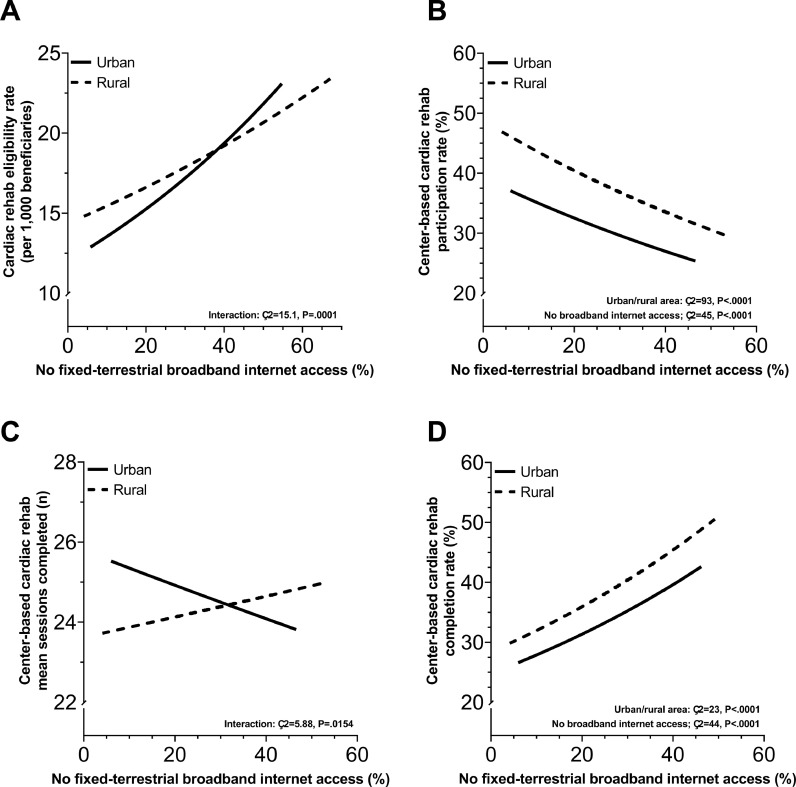
In multivariable regressions including the urban-rural area variable, the adjusted association between broadband internet access and each of the four CR metrics was significant (Fig. 2). In Fig. 2a and 2c it is further illustrated that associations between broadband internet access with eligibility rate and mean sessions completed, respectively, differed by urban-rural area.
Fig. 2.
Associations between cardiac rehabilitation eligibility rate and center-based utilization among Medicare fee-for-service beneficiaries aged ≥65 years and fixed-terrestrial broadband internet access among households of adults aged ≥65 years adjusted for urban-rural area effects. The urban-rural classification scheme for counties defined by the CDC National Center for Health Statistics was used for stratifications. Eligibility rate (per 1,000 beneficiaries) (A), participation rate (% of those eligible who participated in ≥1 session) (B), adherence (mean number of sessions completed within 365 days of qualifying event) (C), and completion rate (% of enrollees who participated in ≥36 sessions) (D).
4. Discussion
In this study we described patterns in fixed-terrestrial broadband internet access throughout the US to suggest national, geographical, and urban-rural disparities in access to this type of telecommunications resource are not rare among households of adults aged ≥65 years. Patterns in fixed-terrestrial broadband internet access tended to overlap those observed for CR eligibility rates to further suggest area-wide gaps in the availability of in-home high-speed internet technology may be symbolic of larger communitywide public health concerns, not just a limited ability to browse the internet. As the proportion of households reporting no fixed-terrestrial broadband internet access rose throughout the country we observed associated patterns of increasing CR eligibility rates overlap decreasing participation rates among Medicare FFS beneficiaries aged ≥65 years. Several of these overlapping patterns also resulted in associations that differed across geographical boundaries and urban-rural areas to highlight that it cannot be assumed at the national level that telehealth-based CR delivery is a pragmatic option currently generalizable to Medicare FFS beneficiaries aged ≥65 years. The associations characterized in our study suggest if available resources and infrastructure needed to support the nationwide expansion of fixed-terrestrial broadband internet access continue to remain out-of-step with the rapid rate at which broadband-dependent telehealth technologies develop, stagnant levels of fixed-terrestrial broadband internet access could play a meaningful role in setting absolute limits on what maximal effect telehealth-based CR delivery could have on making progress towards the CR utilization goals of the Million Hearts initiative [10].
When forced telehealth innovation had to occur without warning because of the suddenness of the COVID-19 pandemic this circumstance led to the rapid proliferation of high speed internet-dependent solutions that have in a short period of time grown to levels that are not reflective of a dated telecommunications infrastructure that has yet to be developed in the US to allow for widespread routine accessibility to high speed internet services [[2], [3], [4], [11], [12], [17], [23]]. Therefore, an inability to access fixed-terrestrial broadband internet services could be identified as a contemporary era barrier to non-center based CR uptake, and one which predominantly affects the individuals whose participation in CR is already likely to be impacted by other known social determinants of health [[10], [11], [12], [14], [17], [23], [29]]. As the telehealth evolution continues an essential part of this movement needs to include resources dedicated towards simultaneously closing the “digital divide” as a contemporary social determinant of health [11,12,23]. Not having the information, resources, and physical infrastructure in-place to support universal broadband-quality internet access jeopardizes both the present and future ability to leverage evolving telecommunications technologies to help address the role social disparities play in cardiovascular disease risk and accessing, utilizing, and prioritizing preventive healthcare [10,13,29,30].
Discussions and research studies to date that suggest technology driven telehealth CR delivery is urgently needed and a missing resource required to overcome barriers preventing CR utilization do not fully appreciate and acknowledge concern that universal fixed-terrestrial broadband internet access does not exist in the US [2], [3], [4], [5], [6], [7]. The lack of widespread fixed-terrestrial broadband internet access nationwide is particularly impactful to patients who live below the poverty threshold and in underserved communities since not having routine access to this technological resource eliminates telehealth CR delivery options, such as the model outlined in the current Hospitals without Walls initiative defined by CMS [20], [21], [22]. Continuing to move forward with telehealth CR models such as the Hospitals without Walls program without concurrently implementing new and complementary provisions that provide resources for free broadband internet access to impoverished patients threatens to entrench the effects of the digital divide as a social determinant of health [11,12,20,22,23]. Contemporary estimates suggest the median age of patients hospitalized because of primary acute coronary syndrome is 66.8 (95%CI 66.7 – 67.0) years with Medicare identified as the payer status for 56.8% of cases, and another 14.5% identified as extremely low income and receiving Medicaid benefits or uninsured altogether [30]. In this study we illustrate at least one-quarter to one-third of households of adults aged ≥65 years are affected by circumstances, socioeconomic or otherwise, where fixed-terrestrial broadband internet access is absent. In the present-to-medium term, it is unclear how current models [20], [21], [22] or proposals [2], [3], [4], [5], [6], [7] advocating for mainstream telehealth CR delivery offer translational assistance with overcoming barriers to accessing non-center-based CR, and are transformative and generalizable to the large segment of Medicare FFS beneficiaries aged ≥65 years who live below the poverty threshold and are either eligible for CR or at high risk for experiencing a qualifying event [9,10,13,29,30]. There has also been no commitment by CMS to continue supporting beyond the declared public health emergency period reimbursement for A/V monitored home-based CR exercise training sessions that are remotely supervised by physicians [22].
The absence of universal access to fixed-terrestrial broadband internet connectivity as part of standard of living in the US [23] neutralizes for many Medicare FFS beneficiaries aged ≥65 years the proposed CR accessibility benefits thought to be gained by emphasizing the utility and practicality of smartphone applications and wearable health solutions as progressive tools for creating a technology-based ecosystem specific for CR [2], [3], [4], [5], [6], [7]. In order to be effective and meet current requirements of CMS, technologies proposed for use in the telehealth CR environment are fundamentally reliant on reliable medium strength (or higher) bandwidth quality (i.e., download rate ≥25 Mbps and upload rate of ≥3 Mbps) broadband internet access for transmitting data and supporting live-action A/V telecommunications [20], [21], [22], [23]. Primarily relying on cellular-based subscriptions for broadband internet access is not pragmatic for the majority of the eligible or at-risk CR population since unlimited cellular data plans are cost prohibitive for low income households, fixed monthly data allowances are not suitable for accommodating up to 12 live-action A/V enhanced 1-hour supervised CR sessions per month, and concerns over cellular affordability and continuity of active service lines affect patients who are least likely to have fixed-terrestrial broadband internet access [[11], [12], [20], [21], [22], [23]]. The FCC also does not currently consider cellular-based internet technologies a like-for-like substitute for fixed-terrestrial internet access [11,12,21,23].
Paradoxically, it is the large segment of patients who are most vulnerable to experiencing the highest CR eligibility rates, hallmark barriers to CR utilization, and lack of fixed-terrestrial broadband internet access who in the present-to-near future stand to benefit the least from institutionalizing current [20], [21], [22] or proposed [2], [3], [4], [5], [6], [7] models of telehealth CR as part of current standard of care. Additionally, if CMS first requires large-scale randomized clinical trial evidence to endorse the clinical benefits of telehealth CR as an option for standard of care, acquiring such data in a representative patient cohort of diverse social and economic backgrounds could prove extremely challenging and biased without universal fixed-terrestrial broadband internet access already in-place. Equitable representation of patients exhibiting characteristics predictive of low socioeconomic status in randomized clinical trials is rare and an ongoing concern for the development of medical treatments and improving access to preventive healthcare [31], [32], [33].
4.1. Limitations
Causality cannot be established based on associations we report in this study. The internet access dataset from the Census Bureau did not exclusively represent the fixed-terrestrial broadband internet access status of CR eligible Medicare FFS beneficiaries aged ≥65 years. By reporting on fixed-terrestrial broadband internet access for all households of adults aged ≥65 years it is possible we over- or under-estimated our reported associations. However, to the best of our knowledge there is no data available that links national internet access status with CMS claims data focusing on CR eligible Medicare FFS beneficiaries aged ≥65 years. Additionally, separate bodies of evidence are available illustrating demographic factors and social determinants of health that are associated with the digital divide are also commonly observed to correlate with cardiovascular disease risk and CR utilization [[9], [10], [11], [12], [13], [29], [30]]. Thus, it is unlikely that fixed-terrestrial broadband internet access levels would be higher among CR eligible Medicare FFS beneficiaries aged ≥65 years than that of the general population.
We did not have data on the proportion of CR eligible patients who did not receive physician referrals for CR enrollment since CMS does not collect this information. Although the lack of a physician referral can be a barrier to CR enrollment [10], we are unaware of evidence suggesting the number of missing CR referrals differs significantly between and within counties and from state-to-state or region-to-region on a national level.
5. Conclusions
Current levels of fixed-terrestrial broadband internet access are imbalanced between geographical regions and urban-rural areas among US households of adults aged ≥65 years. Geographical regions and rural areas exhibiting the lowest levels of fixed-terrestrial broadband internet access also demonstrate the highest CR eligibility rates among Medicare FFS beneficiaries aged ≥65 years. Offering telehealth CR as an alternative to center-based care may have the largest potential impact on improving CR utilization among a select segment of patients residing in areas supported by the combination of up-to-date physical broadband infrastructure and government backed financial resources needed to allow for widespread opportunities to access fixed-terrestrial broadband internet services. In order to support the universal viability and intended benefit of offering patients the option of telehealth CR delivery, the modern era of digitally connected healthcare requires actionable public health policy initiatives aimed at providing communities with the physical and financial resources required to support the availability and accessibility to fixed-terrestrial broadband internet as a standard of living resource for all.
Authorship confirmations/contributions
Erik H. Van Iterson: This author takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation
Luke J. Laffin: This author takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation
Leslie Cho: This author takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation
Each author contributed to study design, data analyses, writing of the manuscript, and provided final review. Each author takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Funding
None.
Disclosure
No private or public funding agency had a role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Declaration of Competing Interest
The authors report no relationships that could be construed as a conflict of interest.
Acknowledgements
None.
Data availability
References
- 1.Van Iterson EH, Laffin LJ, Crawford M, Mc Mahan D, Cho L, Khot U. Cardiac Rehabilitation Is Essential in the COVID-19 Era: DELIVERING UNINTERRUPTED HEART CARE BASED ON THE CLEVELAND CLINIC EXPERIENCE. J Cardiopulm Rehabil Prev. 2021;41(2):88–92. doi: 10.1097/HCR.0000000000000585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Babu AS, Arena R, Ozemek C, Lavie CJ. COVID-19: A Time for Alternate Models in Cardiac Rehabilitation to Take Centre Stage. Can J Cardiol. 2020;36(6):792–794. doi: 10.1016/j.cjca.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scherrenberg M, Wilhelm M, Hansen D, et al. The future is now: a call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. European journal of preventive cardiology. 2021;28(5):524–540. doi: 10.1177/2047487320939671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomas E, Gallagher R, Grace SL. Future-proofing cardiac rehabilitation: Transitioning services to telehealth during COVID-19. Eur J Prev Cardiol. 2020 doi: 10.1177/2047487320922926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epstein E, Patel N, Maysent K, Taub PR. Cardiac Rehab in the COVID Era and Beyond: mHealth and Other Novel Opportunities. Curr Cardiol Rep. 2021;23(5):42. doi: 10.1007/s11886-021-01482-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taylor RS, Dalal HM, McDonagh STJ. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nature reviews Cardiology. 2022;19(3):180–194. doi: 10.1038/s41569-021-00611-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Passantino A, Dalla Vecchia LA, Corra U, et al. The Future of Exercise-Based Cardiac Rehabilitation for Patients With Heart Failure. Front Cardiovasc Med. 2021;8(795) doi: 10.3389/fcvm.2021.709898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Iterson EH, Laffin LJ, Cho L. Expanding the availability of cardiac rehabilitation by offering a virtual option: Forecasting the financial implications. Am J Prev Cardiol. 2022;10 doi: 10.1016/j.ajpc.2022.100334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomas RJ, Beatty AL, Beckie TM, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation. 2019;140(1):e69–e89. doi: 10.1161/CIR.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 10.Ades PA, Keteyian SJ, Wright JS, et al. Increasing Cardiac Rehabilitation Participation From 20% to 70%: A Road Map From the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc. 2017;92(2):234–242. doi: 10.1016/j.mayocp.2016.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelley B, Sisneros L. Broadband Access and the Digital Divides. Policy Brief. Education Commission of the States. 2020 [Google Scholar]
- 12.Rachfal C, Gilroy A. Congressional Research Service. 2019. Broadband internet access and the digital divide: federal assistance programs. [Google Scholar]
- 13.Ritchey MD, Maresh S, McNeely J, et al. Tracking Cardiac Rehabilitation Participation and Completion Among Medicare Beneficiaries to Inform the Efforts of a National Initiative. Circ Cardiovasc Qual Outcomes. 2020;13(1) doi: 10.1161/CIRCOUTCOMES.119.005902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bachmann JM, Huang S, Gupta DK, et al. Association of Neighborhood Socioeconomic Context With Participation in Cardiac Rehabilitation. J Am Heart Assoc. 2017;6(10) doi: 10.1161/JAHA.117.006260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson AE, Zhu J, Garrard W, et al. Area Deprivation Index and Cardiac Readmissions: Evaluating Risk-Prediction in an Electronic Health Record. J Am Heart Assoc. 2021;10(13) doi: 10.1161/JAHA.120.020466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mathews L, Brewer LC. A Review of Disparities in Cardiac Rehabilitation: EVIDENCE, DRIVERS, AND SOLUTIONS. J Cardiopulm Rehabil Prev. 2021;41(6):375–382. doi: 10.1097/HCR.0000000000000659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Astley CM, Clarke RA, Cartledge S, et al. Remote cardiac rehabilitation services and the digital divide: implications for elderly populations during the COVID19 pandemic. Eur J Cardiovasc Nurs. 2021;20(6):521–523. doi: 10.1093/eurjcn/zvab034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martin BJ, Hauer T, Arena R, et al. Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation. 2012;126(6):677–687. doi: 10.1161/CIRCULATIONAHA.111.066738. [DOI] [PubMed] [Google Scholar]
- 19.Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship Between Cardiac Rehabilitation and Long-Term Risks of Death and Myocardial Infarction Among Elderly Medicare Beneficiaries. Circulation. 2010;121(1):63–70. doi: 10.1161/CIRCULATIONAHA.109.876383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Medicare & Medicaid Services (CMS) Health and Human Services (HHS). Waivers during Public Health Emergency (PHE), CMS Guidance to Delivering CR/ICR/PR Using Home as a Provider-Based Department (PBD). Vol 86 Federal Register 64996 (19 November 2021), pp. 65244-65250 (https://www.govinfo.gov/app/details/FR-2021-11-19/2021-23972): Office of the Federal Register, National Archives and Records Administration; 2022:65244-65250.
- 21.American Association of Cardiovascular Pulmonary Rehabilitation. Reimbursement Update. Medicare 2021 Final Physician and Hospital Outpatient Regulations and Payment Rates. https://www.aacvpr.org/Portals/0/Docs/Advocacy/Reimbursement%20Updates/2021/1.06.21%20AACVPR%20Reimbursement%20Update.pdf?ver=2021-01-19-101211-627, Accessed August 5, 2021 (https://www.aacvpr.org/Portals/0/Docs/Advocacy/Reimbursement%20Updates/2021/1.06.21%20AACVPR%20Reimbursement%20Update.pdf?ver=2021-01-19-101211-627).
- 22.Centers for Medicare & Medicaid Services (CMS) Health and Human Services (HHS). Medicare and Medicaid Programs: CY 2023 Payment Policies under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; Medicare and Medicaid Provider Enrollment Policies, etc. Vol 87 Federal Register 69404 (18 November 2022), pp. 69404-70700 (https://www.regulations.gov/document/CMS-2022-0113-24344): Office of the Federal Register, National Archives and Records Administration; 2023:69467-70700.
- 23.Federal Communications Commission. Inquiry Concerning Deployment of Advanced Telecommunications Capability to All Americans in a Reasonable and Timely Fashion, 2020 Broadband Deployment Report. Washington, D.C. April 24 2020. GN Docket No. 19-285.
- 24.Thomas RJ, Balady G, Banka G, et al. 2018 ACC/AHA Clinical Performance and Quality Measures for Cardiac Rehabilitation: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol. 2018;71(16):1814–1837. doi: 10.1016/j.jacc.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Interactive Atlas of Heart Disease and Stroke. http://nccd.cdc.gov/DHDSPAtlas, Accessed March 31, 2022 (http://nccd.cdc.gov/DHDSPAtlas).
- 26.American Community Survey. 2022. https://data.census.gov/cedsci/table?q=broadband%20internet&t=Physical%20Characteristics%3ATelephone,%20Computer,%20and%20Internet%20Access&g=0100000US%240400000_0200000US1,2,3,4&d=ACS%205-Year%20Estimates%20Detailed%20Tables&tid=ACSDT5Y2018.B28002&moe=false. Accessed March 31, 2022.
- 27.United States Census Bureau. American Community Survey - Understanding and Using ACS Single-Year and Multiyear Estimates. 2022; https://www.census.gov/content/dam/Census/library/publications/2020/acs/acs_general_handbook_2020_ch03.pdf. Accessed March 31, 2022.
- 28.Ingram DD, Franco SJ. 2013 NCHS Urban-Rural Classification Scheme for Counties. National Center for Health Statistics. Vital Health Stat. 2014;2(166) [PubMed] [Google Scholar]
- 29.Gaalema DE, Savage PD, Rengo JL, et al. Patient Characteristics Predictive of Cardiac Rehabilitation Adherence. J Cardiopulm Rehabil Prev. 2017;37(2):103–110. doi: 10.1097/HCR.0000000000000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Srivastava PK, Fonarow GC, Bahiru E, Ziaeian B. Association of Hospital Racial Composition and Payer Mix With Mortality in Acute Coronary Syndrome. J Am Heart Assoc. 2019;8(21) doi: 10.1161/JAHA.119.012831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alegria M, Sud S, Steinberg BE, Gai N, Siddiqui A. Reporting of Participant Race, Sex, and Socioeconomic Status in Randomized Clinical Trials in General Medical Journals, 2015 vs 2019. JAMA Netw Open. 2021;4(5) doi: 10.1001/jamanetworkopen.2021.11516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gabriel A, Zare H, Jones W, et al. Evaluating Depressive Symptoms Among Low-Socioeconomic-Status African American Women Aged 40 to 75 Years With Uncontrolled Hypertension: A Secondary Analysis of a Randomized Clinical Trial. JAMA Psychiatry. 2021;78(4):426–432. doi: 10.1001/jamapsychiatry.2020.4622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.LaPlante A, Yen RW, Isaacs T, et al. Enrollment, retention, and strategies for including disadvantaged populations in randomized controlled trials: a systematic review protocol. Syst Rev. 2021;10(1):233. doi: 10.1186/s13643-021-01790-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.