Abstract
South Asian (SA) individuals, particularly those that reside in the United States and other Westernized countries, are at an elevated risk for ASCVD and mortality related to ASCVD. The 2018 ACC/AHA/Multi-society Cholesterol guideline listed SA as a high-risk ethnicity, underscoring the importance of treating modifiable risk factors to reduce ASCVD burden. Coronary artery calcium (CAC), a highly specific marker of subclinical atherosclerosis, may be a useful test to improve risk stratification among SA individuals. CAC testing is a cost-effective, highly reproducible, and specific marker of subclinical atherosclerosis, shown to improve ASCVD risk assessment across all racial/ethnic groups, thereby serving as a guide for initiating or deferring preventive therapies. In this White Paper we will discuss the use of CAC scoring to optimize risk stratification and delivery of preventive therapies to individuals of SA ethnicity.
Keywords: South Asian, Coronary artery calcium, Prevention, Statin, Lipid
1. Introduction
South Asian (SA) individuals make up a diverse ethnic milieu of individuals that trace their roots back to the Southern part of Asia including the Indian subcontinent. The term SA refers collectively to individuals with ancestry from the countries of Bangladesh, Bhutan, India, the Maldives, Nepal, Pakistan, and Sri Lanka. SAs are a rapidly growing ethnic group within and outside of the United States due to Western migration. Despite the growth and socioeconomic success of this group, Western acculturation has uncovered new challenges with regard to cardiometabolic health.
As an ethnicity, SA individuals are at high risk for atherosclerotic cardiovascular disease (ASCVD). The first reports of elevated ASCVD risk came from Singapore in 1959 [1]. Over the last several decades, a growing body of knowledge on ASCVD in SA individuals has pointed to a higher burden, earlier onset, and greater mortality of ASCVD within the SA community when compared to Non-Hispanic Whites (NHWs) [2], [3], [4], [5].
Notably, SA individuals, particularly those that reside in the United States and other Westernized countries, are at an even greater risk for ASCVD and mortality related to ASCVD. The mortality burden from ischemic heart disease among SA individuals is reflected by the proportional mortality rates. The proportional mortality rates in Asian Indian men and women are 1.43 and 1.12 respectively and are substantially elevated, when compared with NHW men (1.08) and women (0.92) [6]. Acknowledging this burden of heart disease, SA ethnicity is now listed as a ‘risk-enhancing’ factor, a factor that is thought to confer an elevated risk for ASCVD, in the 2018 American College of Cardiology (ACC)/ American Heart Association (AHA)/ Multi-society Guideline on the management of Blood Cholesterol [7,8].
While the ASCVD burden among SA individuals is multifactorial, the greatest need lies in appropriate risk stratification, prevention, and management of disease. A number of challenges lie in clinical risk stratification in these individuals using currently available risk calculators, namely due to either the overestimation or underestimation of risk. In this White paper, we will discuss the utility of noninvasive imaging with coronary artery calcium (CAC) scoring and coronary computed tomography (CT) to assist in “leveling the playing field” with regard to assessment of ASCVD risk.
2. Drivers of ASCVD among South Asians
The drivers of the elevated ASCVD burden among SA individuals residing in the United States include a broad variety of biological mechanisms and non-biological social and health-related behaviors. Insulin resistance, impaired glucose tolerance, metabolic syndrome (MetS), and type II diabetes mellitus collectively are some of the most common risk factors among SA individuals when compared to NHWs. Type II diabetes prevalence is at least 2-fold higher among SA individuals when compared to NHW [9]. Overall, the prevalence of type II diabetes and prediabetes is estimated at 29% and 37% respectively among Asian Indians [10]. Obesity, particularly abdominal adiposity and increased waist circumference is highly prevalent among SAs and contributes to increased cardiometabolic risk [11]. The World Health Organization and American Diabetes Association have recommended lower body mass index (BMI) cutoffs for individuals of SA ethnicity such that a normal BMI is 18.5–22.9 kg/m2, an overweight BMI is 23.0–27.4 kg/m2, and an obese BMI is ≥27.5 kg/m2 [11]. The lower cut points encourage healthy eating and weight management earlier on and trigger screening for cardiovascular disease risk factors, which become more prevalent at a lower BMI among SA individuals [12]. Dyslipidemia including elevated triglycerides, low HDL-C, potentially dysfunctional HDL-C, and smaller, lower density LDL particles are also notable contributors to the increased ASCVD risk [13]. Higher serum levels of lipoprotein(a) have also been reported among SA individuals and reflect a genetically inherited component to ASCVD risk [14]. Other ASCVD risk factors that elevate the risk include hypertension, which is more prevalent amongst SA individuals compared to NHW, and smoking [15]. While traditional tobacco use (i.e. cigarette smoking) is lower among SA individuals, clinical questionnaires and assessments often do not take into account other forms of cultural tobacco use that may be more commonly used (i.e. bidis, paan, paan masala, gutka, hookah, for example) and which influence ASCVD risk [16,17].
Non-biological mechanisms are also though to play a significant role in ASCVD risk and the development of its risk factors. Western acculturation of traditional dietary patterns to incorporate a higher proportion of foods that are higher in saturated fats and sugars and lower in nutritional value and low physical activity rates compared to other racial and ethnic minorities further elevate the risk of ASCVD through non-biological mechanisms [15,18].
3. Current guideline recommendations for coronary artery calcium scoring
The 2018 ACC/AHA Cholesterol Guideline and 2019 ACC/AHA Primary Prevention Guideline recommends the use of the Pooled Cohort Equations (PCEs) to stratify patients into low, borderline, intermediate and high ASCVD risk [19,20]. Screening recommendations using the PCE begin at the age of 40 years. Per the guidelines, CAC scoring may be considered in individuals at borderline or intermediate risk in whom the benefit of statin use may be unclear. In younger adults, ages 20–39 years, a lifetime risk assessment is recommended and statin therapy may be considered in those with a strong family history of ASCVD or in those with significantly elevated LDL-C (including familial hypercholesterolemia).
4. Limitations of traditional risk stratification algorithms and current guideline recommendations in South Asians
Risk assessment is a fundamental aid for ASCVD risk reduction counseling. The 2018 ACC/AHA Guideline on the Management of Blood Cholesterol listed SA as a high-risk ethnicity and a risk-enhancing factor, thereby recommending that SA individuals at borderline (5- <7.5% 10-year ASCVD risk) or intermediate (≥7.5%- <20% 10-year ASCVD risk) risk or higher per the PCEs as candidates for consideration of statin initiation or intensification [19]. While these recommendations and other risk prediction tools acknowledge the elevated risk at a population level the elevated risk among SA individuals, there are limitations to risk prediction, discrimination, and calibration in these individuals (summarized in Table 1). First, available guidelines recommend risk algorithms have not been derived from or prospectively validated in SA adults; second, SA (and other ethnicities) are recommended to be classified as ‘White’ race (underestimating risk using the Pooled Cohorts Equations); third, crude adjustment factors to calculate ASCVD risk fail to accurately capture risk (using the UK based QRISK2 and QRISK Lifetime3rd Joint British Societies’ Risk Calculator); fourth, limited considerations have been given for native versus migrant populations; and finally, there is paucity of disaggregated data, which masks meaningful ASCVD health differences in SA subgroups. Overall, the PCEs have reasonable functionality in SA individuals (majority Asian Indian population) in the US who are at the extremes of risk (<5% and >20%), however, systematic consideration of statin treatment in these individuals at borderline and intermediate risk may result in overtreatment with statin therapy [21]. More refined means of risk stratification are needed for SA individuals, particularly for those who carry higher ASCVD risk compared to Asian Indians and who are underrepresented in current research studies such as those of Pakistani and Bangladeshi origin.
Table 1.
Limitations of the Pooled Cohort Equations Among South Asians.
|
|
|
|
|
There is robust evidence demonstrating significant ASCVD burden in younger SA individuals, particularly before the age of 45 years [22]. Per current screening recommendations, many younger SA individuals may be misclassified as low-risk by the PCEs and would remain inadequately screened and treated [23]. Comprehensive screening with cardiovascular imaging and blood biomarkers did not reduce the risk of death in a majority White population, leaving the role of population level cardiovascular screening in SA individuals less clear, and unlikely to be recommended at this time.
5. Coronary calcium scoring in South Asians
Substantial variability exists in the CVD prevalence, incidence, risk, and health‐seeking behavior among SA subgroups [5,6,[24], [25], [26], [27]]. In addition to frequent and universal screening for traditional risk factors and metrics, the use of CAC, a highly specific marker of subclinical atherosclerosis, therefore may be a useful test to improve risk stratification in SA individiuals [28]. CAC testing is a cost-effective, highly reproducible, and specific marker of subclinical atherosclerosis, proven to improve ASCVD risk assessment across all racial/ethnic groups, thereby serving as a guide for initiating or deferring preventive therapies [29]. An elevated CAC score has been shown to be independently associated with ASCVD and further stratifies ASCVD risk while CAC score of 0 does not further stratify ASCVD risk [30].
Among asymptomatic Asian Indians without diabetes who were borderline risk in the MASALA cohort, 54% had an absence of CAC (score of 0). Among Asian Indians without diabetes who were at intermediate risk, 30% had an absence of CAC, but 70% had a CAC score that was >0. The prevalence of CAC was higher among Asian Indians at intermediate risk than at borderline risk [19,21]. In these individuals at borderline or intermediate risk who are asymptomatic and free of diabetes, CAC may provide additional value in ASCVD risk stratification. It is important to note that this cohort was enriched in Asian Indians and had very few Pakistani and Bangladeshi Americans, both of which are higher risk SA subgroups. Additional considerations for the use of CAC to further assess ASCVD risk include individuals who are at low risk by the PCE (who would otherwise not qualify for statin therapy) but have a family history premature ASCVD. In these patients, the use of CAC, and particularly early screening beginning around the ages of 30 or 40 years may identify higher risk individuals in whom preventive therapies may be initiated earlier on despite the lack of traditional risk factors assessed by the PCEs. However, it is important to note that the absence of CAC particularly in younger adults with an elevated lifetime risk does not diminish the importance of healthy lifestyle behaviors [31]. Prediabetes and MetS are highly prevalent among SA indiviiduals and increase ASCVD risk. In a study conducted using the MESA cohort, the addition of CAC improved risk classification of individuals with MetS, suggesting an additional potential role of CAC screening [32].
Racial and ethnic differences: With regard to CAC progression, SA men have greater CAC progression when compared to Chinese, Black and Latino men after adjustment for age, diabetes mellitus, hypertension, and statin use, but no difference was noted SA and White men [33]. SA women appear to have a similarly elevated CAC burden when compared to other racial and ethnic groups (African America, Latino, and Chinese Americans), but older SA women, ≥70 years, were noted to have a higher CAC burden compared to other racial and ethnic groups [34]. In one study of Asian-Indians, the presence of CAC in individuals <50 years was 46%, which was higher than other racial and ethnic groups [35]. CAC was found among 97% of Asian-Indian individuals >60 years pointing to the high burden of CAC among this ethnic group [35]. These findings correspond with the high prevalence of CAD in this group.
The presence of a family history of coronary heart disease (CHD) in SA individuals compared to those of other race/ethnicities is associated with CHD (OR 1.71 [95% CI 1.21, 2.42]; p = 0.002) and severe subclinical atherosclerosis (CAC >300) [36,37] With respect to biomarkers [Lp(a)], tumor necrosis factor-alpha, adiponectin, and leptin], no association was found with CAC presence or severity in the MASALA Study, suggesting markers of inflammation and cardiometabolic risk are independent of CAC in SA individuals, similar to other race/ethnicities [38]. CAC may help identify those SA adults who would best qualify for aggressive lifestyle optimization and anti-hypertensive pharmacotherapy [38,39]. For example, more than half of all SA adults qualified for lifestyle modifications and 17% were recommended anti-hypertensive pharmacotherapy by 2017 ACC/AHA Hypertension Guideline compared to 8% by JNC7 (chi-square p<0.001) [38]. It is important to note that many of the studies that assessed the use of CAC among SA adults were highly enriched in Asian Indians. While CAC has been shown to be a reliable marker among other racial and ethnic groups, additional studies are needed among SA individuals beyond just Asian Indians.
Taken together, when compared to available risk markers, CAC scoring is a useful noninvasive modality for further risk refinement and guide other preventive therapy in SA adults.
6. Coronary computed tomography angiography in South Asians
Coronary CT angiography has been used to identify high risk patients. While current data in SA adults using coronary CT angiography is limited, quantitative analysis of the coronary arteries by CT showed that SA adults had smaller normalized proximal LAD luminal diameters when compared with Caucasians and also had more severe CAD including a higher number of diseased vessel segments and greater mean percent stenosis in the proximal LAD and RCA [40]. Notably, SA individuals with type II diabetes mellitus have a higher prevalence and extent of asymptomatic coronary artery disease when compared to matched Caucasian patients [41]. Furthermore, SA individuals may have differential non-calcified plaque given the higher prevalence of elevated Lp(a) and MetS. Future studies should evaluate this as potential tool for diagnosis and treatment.
Another important use of coronary CT is to assess for differences in plaque characteristics. Plaque characteristics beyond the traditional CAC score may be helpful when assessing ASCVD risk. SA adults have a higher number of vessels with calcified plaque compared to other race/ethnicities [41,42]. Significant coronary artery disease (CAD) (>50% stenosis) was more frequent in the left anterior descending coronary artery among asymptomatic SA adults compared to NHW adults with diabetes mellitus [41]. Compared to NHW, SA have significantly lower CAC volume but higher CAC density when accounting for traditional risk factors [42]. As noted by the authors, higher CAC density may reflect stable plaque (less likely to rupture), which is influenced by statin use (pro-calcific effects) [42,43]. Both CAC volume and density appear to be correlated with ASCVD risk [44]. The long-term clinical and prognostic significance of this is currently unknown and remains an area for future investigation.
7. Beyond statins
Beyond categorizing individuals as statin candidates and those who are not in a binary fashion, the detection and assessment of plaque using CAC and coronary CT can assist with personalized allocation of preventive cardiometabolic therapies tailored to individual needs. CAC testing and specifically CAC>100 Agatston may guide Aspirin utilization in asymptomatic adults in primary prevention cohorts [45,46]. Additionally, more intensive lifestyle counseling and enhanced used of other cardiometabolic therapies that reduce the risk of ASCVD events, i.e. Glucagon-like peptide-1 receptor agonists (GLP-1 RA), Sodium-glucose cotransporter-2 (SGLT2) inhibitors, and icosapent ethyl (IPE) may be offered to those who may not otherwise qualify for these therapies.
8. Clinical implications
The evaluation and management of traditional risk ASCVD risk factors among SAs remains important. Targeted strategies are needed to comprehensively reduce ASCVD risk among SA individuals residing in Westernized countries including the United States as well as those living in their native countries. These include strategies such as enhancing access to basic preventive care with enhanced early detection and treatment of conditions that are highly prevalent among SA individuals (i.e. diabetes mellitus, dyslipidemia, and MetS), increasing health literacy and education, nutrition and physical activity counseling.
Outside of clinic settings, interventions focused on tackling poverty and reducing air pollution are important ways to help reduce ASCVD burden. Local and national cultural community organizations may also be leveraged to assist with spreading awareness of heart disease and its risk factors and to help facilitate access to care. It is equally important to address unique challenges and barriers to care that have arisen in diaspora countries that adversely impact access to care: socioeconomic status, language barriers, Islamophobia, racism, low access to care, lack of insurance, and stressors of migration.
Currently, there exist notable limitations to currently available clinical risk stratification algorithms that may inadequately estimate ASCVD risk in SA individuals. CAC testing is a cost-effective, actionable, and reproducible tool that can accurately detect subclinical atherosclerosis and thereby guide preventive therapies. CAC scoring in patients at intermediate risk of ASCVD in whom the decision about statin use is uncertain has been listed as a high-value care test [47]. Beyond traditionally recommended indications, CAC screening may be considered in individuals who are at a higher risk than that estimated by traditional risk stratification tools including those classified as low risk, but with a family history of premature ASCVD. These individuals as such may not qualify for statin and other preventive therapies based on stratification by the PCEs alone, but CAC scoring may further refine their classification. Additionally, individuals with medical comorbidities that are highly prevalent drivers of ASCVD such as prediabetes and MetS may be considered as candidates for CAC scoring to help identify those in whom a primary prevention statin and other preventive cardiometabolic therapies may be considered.
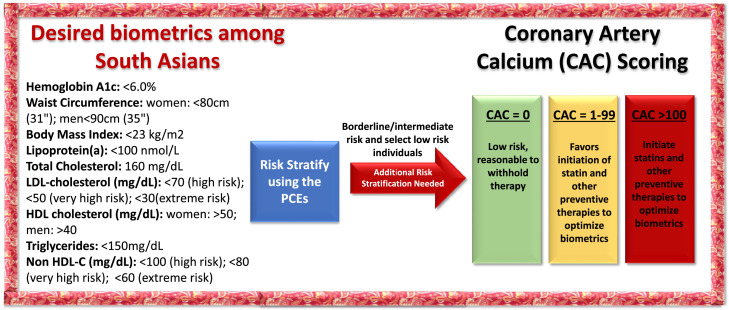
While traditional CAC scoring recommendations begin at the age of 45 years, the ASCVD burden among SA individuals begins roughly 10 years earlier than in other racial and ethnic groups and argues for earlier screening. As such, after risk assessment, implementation of CAC testing, particularly in those with significant risk factors or a family history of CHD may aid in the detection and management of subclinical atherosclerosis [48], [49], [50], [51]. Table 2 summarizes the key recommendations for CAC scoring in SA patients. There is a need for additional validation of CAC percentiles specific to SA individuals and those <45 years. Fig. 1 summarizes risk stratification among SA individuals, which has also been previously described (https://www.acc.org/latest-in-cardiology/articles/2021/12/06/13/32/how-many-south-asians-does-it-take) [15,52].
Table 2.
Key Recommendations for Coronary Artery Calcium Scoring among South Asians.
| Key Recommendations for the use of Coronary Artery Calcium Scoring in South Asian adults |
|
|
|
|
Fig. 1.
Proposed biometrics and risk stratification of South Asian Individuals.
Future ACC/AHA guidelines and recommendations may consider novel indications for CAC scoring among SA adults and other high-risk groups as well as earlier screening ages to help allocate preventive cardiometabolic therapies. Comprehensive screening with cardiovascular imaging and blood biomarkers did not reduce the risk of death in a majority White population, leaving the role of population level cardiovascular screening in SA adults less clear, and unlikely to be recommended at this time [53]. However, currently available clinical data among SA individuals underscores the need for appropriate risk stratification and management in individuals at an elevated ASCVD risk [21,32].
Use of the Multi-Ethnic Study of Atherosclerosis (MESA) 10-year CHD risk calculator with coronary artery calcification may be considered for SA men. While a SA specific calculator does not currently exist, in the MESA calculator, SA men may be represented as “White” race given that CAC scores are similar in SA men and NHW men.
Cost and insurance reimbursement considerations are also important issues to consider for CAC scoring. Traditionally, CAC scoring has not been well covered by insurance. While out of pocket costs may range from $49-$400 per test nationally, this may be prohibitively expensive for individuals of lower socioeconomic status or may not be readily available to those with limited access to healthcare services. This may further increase disparities by not making this screening tool affordable or accessible to higher-risk, lower-income SA individuals.
Growing awareness of the unique challenges in SA cardiovascular health has led to the creation of specialty clinics around the United States uniquely focused on lowering the burden of heart disease among SA individuals [54].
9. Conclusion
Comprehensive and actionable risk stratification tools have great utility in tackling the burden of ASCVD among SA adults. Current data suggest that the use of CAC scoring is a cost effective and reproducible metric to detect subclinical atherosclerosis and further enhance ASCVD risk stratification in select individuals. While we have begun to understand the differences in the types and prevalence of risk factors, there is a need for further studies among SA individuals to understand the nuances and heterogeneity of risk even within this diverse group and standardized clinical guidelines that incorporate cultural practices and traditional beliefs to optimize care. Greater efforts are needed in raising awareness of heart disease and its risk factors using informative and culturally focused messaging from healthcare providers as well as through the community and cultural organizations as well as eliminating barriers to care (language, socioeconomic status, literacy etc.). Further studies are needed in disaggregated SA subgroups that have been traditionally underrepresented in Westernized studies, specifically Bangladeshi and Pakistani Americans.
Authorship contribution
Anandita Agarwala and Jaideep Patel drafted the manuscript. Michael Blaha, Miguel Cainzos-Achirica, Khurram Nasir, and Matthew Budoff edited and provided key feedback on the manuscript.
Funding
None.
Declaration of Competing Interest
None of the authors have any conflicts of interest relevant to this paper.
References
- 1.Danaraj T.J., Acker M.S., Danaraj W., Wong H.O., Tan B.Y. Ethnic group differences in coronary heart disease in Singapore: an analysis of necropsy records. Am Heart J. 1959;58:516–526. doi: 10.1016/0002-8703(59)90085-7. [DOI] [PubMed] [Google Scholar]
- 2.Donaldson L.J., Taylor J.B. Patterns of Asian and non-Asian morbidity in hospitals. Br Med J (Clin Res Ed) 1983;286(6369):949–951. doi: 10.1136/bmj.286.6369.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hughes L.O., Raval U., Raftery E.B. First myocardial infarctions in Asian and white men. BMJ. 1989;298(6684):1345–1350. doi: 10.1136/bmj.298.6684.1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marmot M.G., Adelstein A.M., Bulusu L. Lessons from the study of immigrant mortality. Lancet. 1984;1(8392):1455–1457. doi: 10.1016/s0140-6736(84)91943-3. [DOI] [PubMed] [Google Scholar]
- 5.Holland A.T., Wong E.C., Lauderdale D.S., Palaniappan L.P. Spectrum of cardiovascular diseases inAsian-American racial/ethnic subgroups. Ann Epidemiol. 2011;21(8):608–614. doi: 10.1016/j.annepidem.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jose P.O., Frank A.T., Kapphahn K.I., et al. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol. 2014;64(23):2486–2494. doi: 10.1016/j.jacc.2014.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grundy S.M., Stone N.J., Bailey A.L., et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation. 2018 CIR0000000000000625. [Google Scholar]
- 8.Agarwala A., Liu J., Ballantyne C.M., SS V. The Use of Risk Enhancing Factors to Personalize ASCVD Risk Assessment: Evidence and Recommendations from the 2018 AHA/ACC Multi-Society Cholesterol Guidelines. In. Curr Cardiol Risk Rep. 2019 doi: 10.1007/s12170-019-0616-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gujral U.P., Pradeepa R., Weber M.B., Narayan K.M., Mohan V. Type 2 diabetes in South Asians: similarities and differences with white Caucasian and other populations. Ann N Y Acad Sci. 2013;1281:51–63. doi: 10.1111/j.1749-6632.2012.06838.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanaya A.M., Wassel C.L., Mathur D., et al. Prevalence and correlates of diabetes in South asian indians in the United States: findings from the metabolic syndrome and atherosclerosis in South asians living in america study and the multi-ethnic study of atherosclerosis. Metab Syndr Relat Disord. 2010;8(2):157–164. doi: 10.1089/met.2009.0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Consultation WE Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 12.Shah A.D., Kandula N.R., Lin F., et al. Less favorable body composition and adipokines in South Asians compared with other US ethnic groups: results from the MASALA and MESA studies. Int J Obes (Lond) 2016;40(4):639–645. doi: 10.1038/ijo.2015.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bilen O., Kamal A., Virani S.S. Lipoprotein abnormalities in South Asians and its association with cardiovascular disease: Current state and future directions. World J Cardiol. 2016;8(3):247–257. doi: 10.4330/wjc.v8.i3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anand S.S., Yusuf S., Vuksan V., et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE) Lancet. 2000;356(9226):279–284. doi: 10.1016/s0140-6736(00)02502-2. [DOI] [PubMed] [Google Scholar]
- 15.Kalra D., Vijayaraghavan K., Sikand G., et al. Prevention of atherosclerotic cardiovascular disease in South Asians in the US: A clinical perspective from the National Lipid Association. J Clin Lipidol. 2021 doi: 10.1016/j.jacl.2021.03.007. [DOI] [PubMed] [Google Scholar]
- 16.Siddiqi K., Gupta P.C., Prasad V.M., Croucher R., Sheikh A. Smokeless tobacco use by south Asians. Lancet Glob Health. 2013;1(2):e71. doi: 10.1016/S2214-109X(13)70021-4. [DOI] [PubMed] [Google Scholar]
- 17.Hrywna M., Jane Lewis M., Mukherjea A., Banerjee S.C., Steinberg M.B., Delnevo C.D. Awareness and Use of South Asian Tobacco Products Among South Asians in New Jersey. J Community Health. 2016;41(6):1122–1129. doi: 10.1007/s10900-016-0208-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daniel M., Wilbur J., Fogg L.F., Miller A.M. Correlates of lifestyle: physical activity among South Asian Indian immigrants. J Community Health Nurs. 2013;30(4):185–200. doi: 10.1080/07370016.2013.838482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grundy S.M., Stone N.J., Bailey A.L., et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24):e285–e350. doi: 10.1016/j.jacc.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 20.Arnett D.K., Blumenthal R.S., Albert M.A., et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease. Circulation. 2019 CIR0000000000000678. [Google Scholar]
- 21.Haque W., Grandhi G.R., Kanaya A.M., et al. Implications of the 2019 American College of Cardiology/American Heart Association Primary Prevention Guidelines and potential value of the coronary artery calcium score among South Asians in the US: The Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Atherosclerosis. 2021;334:48–56. doi: 10.1016/j.atherosclerosis.2021.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Volgman A.S., Palaniappan L.S., Aggarwal N.T., et al. Atherosclerotic Cardiovascular Disease in South Asians in the United States: Epidemiology, Risk Factors, and Treatments: A Scientific Statement From the American Heart Association. Circulation. 2018;138(1) doi: 10.1161/CIR.0000000000000580. CIR.00000000000. [DOI] [PubMed] [Google Scholar]
- 23.Agarwala A., Ballantyne C., Stone N.J. Primary Prevention Management of Elevated Lipoprotein(a) JAMA Cardiol. 2022 doi: 10.1001/jamacardio.2022.4063. [DOI] [PubMed] [Google Scholar]
- 24.Palaniappan L.P., Araneta M.R., Assimes T.L., et al. Call to action: cardiovascular disease in Asian Americans: a science advisory from the American Heart Association. Circulation. 2010;122(12):1242–1252. doi: 10.1161/CIR.0b013e3181f22af4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koirala B., Turkson-Ocran R.A., Baptiste D., et al. Heterogeneity of Cardiovascular Disease Risk Factors Among Asian Immigrants: Insights From the 2010 to 2018 National Health Interview Survey. J Am Heart Assoc. 2021;10(13) doi: 10.1161/JAHA.120.020408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Satish P., Vela E., Bilal U., et al. Burden of cardiovascular risk factors and disease in five Asian groups in Catalonia: a disaggregated, population-based analysis of 121 000 first-generation Asian immigrants. Eur J Prev Cardiol. 2021 doi: 10.1093/eurjpc/zwab074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Satish P., Sadaf M.I., Valero-Elizondo J., et al. Heterogeneity in cardio-metabolic risk factors and atherosclerotic cardiovascular disease among Asian groups in the United States. Am J Prev Cardiol. 2021;7 doi: 10.1016/j.ajpc.2021.100219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Al Rifai M., Cainzos-Achirica M., Kanaya A.M., et al. Discordance between 10-year cardiovascular risk estimates using the ACC/AHA 2013 estimator and coronary artery calcium in individuals from 5 racial/ethnic groups: Comparing MASALA and MESA. Atherosclerosis. 2018;279:122–129. doi: 10.1016/j.atherosclerosis.2018.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greenland P., Blaha M.J., Budoff M.J., Erbel R., Watson K.E. Coronary Calcium Score and Cardiovascular Risk. J Am Coll Cardiol. 2018;72(4):434–447. doi: 10.1016/j.jacc.2018.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mehta A., Vasquez N., Ayers C.R., et al. Independent Association of Lipoprotein(a) and Coronary Artery Calcification With Atherosclerotic Cardiovascular Risk. J Am Coll Cardiol. 2022;79(8):757–768. doi: 10.1016/j.jacc.2021.11.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miedema M.D., Dardari Z.A., Nasir K., et al. Association of Coronary Artery Calcium With Long-term, Cause-Specific Mortality Among Young Adults. JAMA Netw Open. 2019;2(7) doi: 10.1001/jamanetworkopen.2019.7440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Malik S., Zhao Y., Budoff M., et al. Coronary Artery Calcium Score for Long-term Risk Classification in Individuals With Type 2 Diabetes and Metabolic Syndrome From the Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol. 2017;2(12):1332–1340. doi: 10.1001/jamacardio.2017.4191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kanaya A.M., Vittinghoff E., Lin F., et al. Incidence and Progression of Coronary Artery Calcium in South Asians Compared With 4 Race/Ethnic Groups. J Am Heart Assoc. 2019;8(2) doi: 10.1161/JAHA.118.011053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kanaya A.M., Kandula N.R., Ewing S.K., et al. Comparing coronary artery calcium among U.S. South Asians with four racial/ethnic groups: the MASALA and MESA studies. Atherosclerosis. 2014;234(1):102–107. doi: 10.1016/j.atherosclerosis.2014.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hatwalkar A., Agrawal N., Reiss D.S., Budoff M.J. Comparison of prevalence and severity of coronary calcium determined by electron beam tomography among various ethnic groups. Am J Cardiol. 2003;91(10):1225–1227. doi: 10.1016/s0002-9149(03)00268-6. [DOI] [PubMed] [Google Scholar]
- 36.Patel J., Al Rifai M., Cainzos-Achirica M., et al. Family History of CHD Is Associated With Severe CAC in South Asians: Comparing the MASALA and MESA Studies. JACC Cardiovasc Imaging. 2017;10(8):958–960. doi: 10.1016/j.jcmg.2017.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mehta A., Patel J., Al Rifai M., et al. Inflammation and coronary artery calcification in South Asians: The Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Atherosclerosis. 2018;270:49–56. doi: 10.1016/j.atherosclerosis.2018.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Patel J., Mehta A., Rifai M.A., et al. Hypertension guidelines and coronary artery calcification among South Asians: Results from MASALA and MESA. Am J Prev Cardiol. 2021;6 doi: 10.1016/j.ajpc.2021.100158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Whelton P.K., Carey R.M., Aronow W.S., et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–1324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 40.Hasan R.K., Ginwala N.T., Shah R.Y., Kumbhani D.J., Wilensky R.L., Mehta N.N. Quantitative angiography in South Asians reveals differences in vessel size and coronary artery disease severity compared to Caucasians. Am J Cardiovasc Dis. 2011;1(1):31–37. [PMC free article] [PubMed] [Google Scholar]
- 41.Roos C.J., Kharagjitsingh A.V., Jukema J.W., Bax J.J., Scholte A.J. Comparison by computed tomographic angiography-the presence and extent of coronary arterial atherosclerosis in South Asians versus Caucasians with diabetes mellitus. Am J Cardiol. 2014;113(11):1782–1787. doi: 10.1016/j.amjcard.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 42.Al Rifai M., Kanaya A.M., Kandula N.R., et al. Distribution of calcium volume, density, number, and type of coronary vessel with calcified plaque in South Asians in the US and other race/ethnic groups: The MASALA and MESA studies. Atherosclerosis. 2021;317:16–21. doi: 10.1016/j.atherosclerosis.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Criqui M.H., Denenberg J.O., Ix J.H., et al. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA. 2014;311(3):271–278. doi: 10.1001/jama.2013.282535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Al Rifai M., Kanaya A.M., Kandula N.R., et al. Association of Coronary Artery Calcium Density and Volume With Predicted Atherosclerotic Cardiovascular Disease Risk and Cardiometabolic Risk Factors in South Asians: The Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study. Curr Probl Cardiol. 2022 doi: 10.1016/j.cpcardiol.2022.101105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ajufo E., Ayers C.R., Vigen R., et al. Value of Coronary Artery Calcium Scanning in Association With the Net Benefit of Aspirin in Primary Prevention of Atherosclerotic Cardiovascular Disease. JAMA Cardiol. 2021;6(2):179–187. doi: 10.1001/jamacardio.2020.4939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miedema M.D., Duprez D.A., Misialek J.R., et al. Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes. 2014;7(3):453–460. doi: 10.1161/CIRCOUTCOMES.113.000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kini V., Breathett K., Groeneveld P.W., et al. Strategies to Reduce Low-Value Cardiovascular Care: A Scientific Statement From the American Heart Association. Circ Cardiovasc Qual Outcomes. 2022 doi: 10.1161/HCQ.0000000000000105. HCQ0000000000000105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carr J.J., Jacobs D.R., Jr., Terry J.G., et al. Association of Coronary Artery Calcium in Adults Aged 32 to 46 Years With Incident Coronary Heart Disease and Death. JAMA Cardiol. 2017;2(4):391–399. doi: 10.1001/jamacardio.2016.5493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Okwuosa T.M., Greenland P., Ning H., Liu K., Lloyd-Jones D.M. Yield of screening for coronary artery calcium in early middle-age adults based on the 10-year Framingham Risk Score: the CARDIA study. JACC Cardiovasc Imaging. 2012;5(9):923–930. doi: 10.1016/j.jcmg.2012.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hecht H., Blaha M.J., Berman D.S., et al. Clinical indications for coronary artery calcium scoring in asymptomatic patients: Expert consensus statement from the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2017;11(2):157–168. doi: 10.1016/j.jcct.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 51.Mortensen M.B., Dzaye O., Bødtker H., et al. Interplay of Risk Factors and Coronary Artery Calcium for CHD Risk in Young Patients. JACC Cardiovasc Imaging. 2021 doi: 10.1016/j.jcmg.2021.05.003. [DOI] [PubMed] [Google Scholar]
- 52.Puri R., Mehta V., Iyengar S.S., et al. Lipid Association of India Expert Consensus Statement on Management of Dyslipidemia in Indians 2020: Part III. J Assoc Physicians India. 2020;68(11[Special]):8–9. [PubMed] [Google Scholar]
- 53.Lindholt J.S., Sogaard R., Rasmussen L.M., et al. Five-Year Outcomes of the Danish Cardiovascular Screening (DANCAVAS) Trial. N Engl J Med. 2022;387(15):1385–1394. doi: 10.1056/NEJMoa2208681. [DOI] [PubMed] [Google Scholar]
- 54.Kulkarni A. M.J, Deedwania P., Patel J. South Asian Cardiovascular Health: Lessons Learned from the National Lipid Association Scientific Statement. 2021.