Abstract
Objective:
To examine the association between preconception diet quality, sedentary behavior, and physical activity with gestational weight gain (GWG) among Hispanic/Latina women
Methods:
This was a prospective cohort study of participants from visits 1 (2008–2011) and 2 (2014–2017) of the Hispanic Community Health Study/Study of Latinos and singleton pregnancies between the 2 visits. Diet quality (alternative healthy eating index/AHEI-2010), sedentary behaviors, and physical activity (Global Physical Activity Questionnaire) were measured at visit 1 and accounted for preconception health behaviors. GWG was evaluated as a continuous and categorical variable according to the 2009 Institute of Medicine guidelines (inadequate, adequate, excessive). Linear and generalized logit survey regressions were used to study the association between health behaviors and GWG, using adequate GWG as the reference.
Results:
Of the 457 women included, deliveries occurred at 3.2 years (mean) from visit 1; 48.7% of women had excessive GWG. Mean AHEI-2010 scores were <45% for women of all Hispanic/Latina backgrounds. Sedentary behavior was 269.5 (SE 9.7) minutes/day and total physical activity was 122.8 (SE 9.3) minutes/day. There was no association between each 10-unit increase in AHEI-2010 or a 500kcal/day increase in energy intake for mean and categorical GWG. There was no association between 30 minutes/day higher sedentary behavior, 30 minutes/day higher total physical activity, or meeting the 2008 US physical activity guidelines for mean and categorical GWG.
Conclusions:
We did not find associations between diet quality, sedentary behavior, and physical activity measured at visit 1 with GWG in pregnancies occurring between visits 1 and 2. We noted widespread poor diet quality as measured by the AHEI-2010, high sedentary behavior, and low physical activity among Hispanic/Latina women.
Background
The amount of weight gained during pregnancy, also referred to as gestational weight gain (GWG) is associated with important short- and long-term health outcomes. Both inadequate and excessive GWG negatively influence fetal development and may contribute to chronic diseases later in life. While non-Hispanic Black women and Hispanic/Latina women have lower mean GWG than whites, 36–51% of non-Hispanic Black women and Hispanic/Latino women also experience excessive GWG (Brawarsky et al., 2005; Chasan-Taber et al., 2008; Siega-Riz & Hobel, 1997; Walker, Hoke, & Brown, 2009).
Pre-pregnancy body mass index (BMI) is the most important risk factor for GWG. Approximately two-thirds of women with obesity exceed the Institute of Medicine (IOM) recommendations of 11–20 pounds of GWG, compared with almost half of normal-weight women who exceed the recommendation of 25–35 pounds of GWG (Bodnar et al., 2010). The prevalence of obesity is particularly high among Hispanic/Latina women in the US compared with non-Hispanic whites, increasing their risk for excessive GWG (Hales et al., 2020). Similarly, BMI is also related to inadequate GWG, such that 39% of women with an underweight pre-pregnancy BMI had inadequate GWG in a cross-sectional population-based US study in 2015 (Deputy et al., 2015) In general, health behaviors (e.g., diet, physical activity) are associated with weight status and they are also considered modifiable risk factors for GWG. Other social, economic and structural factors also contribute to GWG. For example, culture and acculturation, race-ethnicity, parity, marital status, partner and family support, depression, and stress are associated with GWG (Institute of Medicine, 2009). Health behaviors are important because they can be targeted at an individual level through weight management interventions. Several studies have examined physical activity and diet during pregnancy and their association with GWG in Hispanic/Latina women (Dolin et al., 2020; Tovar et al., 2009). Some of these studies have reported mean daily caloric intake and selected dietary variables and the proportion of participants meeting physical activity recommendations (Dolin et al., 2020; Tovar et al., 2009). The limitations of these studies include a focus on health behaviors during pregnancy as opposed to preconception and a focus on GWG in the context of gestational diabetes screening. Other studies that have examined physical activity prior to pregnancy found low adherence to recommendations and no differences among women from Puerto Rican or Dominican backgrounds (Chasan-Taber et al., 2010; Chasan-Taber et al., 2014). Although diet, sedentary behavior, and physical activity are associated with weight gain in non-pregnant individuals, our knowledge is limited by the association between these factors and GWG among women of diverse Hispanic/Latina backgrounds.
The association between preconception health behaviors and GWG has not been extensively examined in Hispanic/Latina women. Within the context of a cohort study, we examined the association of preconception diet, sedentary behavior, and physical activity with GWG among Hispanic/Latina women who gave birth over a 6-year period. We hypothesized that suboptimal diet, higher sedentary behavior, and lower physical activity in the preconception period would be associated with not meeting GWG goals during pregnancy and would vary among Hispanic/Latina backgrounds.
Methods
The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) is a prospective cohort study of individuals who self-identified as having Hispanic/Latino ethnicity. The HCHS/SOL methodology has been previously described (Lavange et al., 2010). The four communities included in HCHS/SOL are located in the Bronx, NY, Chicago, IL, Miami, FL, and San Diego, CA. Probability sampling within these areas was used to ensure a broad representation of the target population and to minimize the various sources of bias that may otherwise enter into the cohort selection and recruitment process (Lavange et al., 2010). Individuals were eligible to participate in the cohort study if they were 18–74 years old, able to give informed consent, not planning to move in the next 3 years, not currently pregnant, and spoke English or Spanish. The 16,415 participants completed a survey and health assessment between 2008–2011 (visit 1). HCHS/SOL participants were followed up in 2014–2017 (visit 2), at which time they reported lifetime pregnancy complications. The sampling methods for SOL study are available in Table 1 of Lavange et al. (2010). All participants provided written informed consent. The Institutional Review Board of each site approved this study, which was registered at clinicaltrials.gov as NCT02060344.
Table 1.
Preconception maternal characteristics by gestational weight gaina, HCHS/SOL (2008–2017).
| Overall %(95%CI) n=457 | Inadequate GWG %(95%CI) n=111 | Adequate GWG %(95%CI) n=124 | Excessive GWG %(95%CI) n=222 | p-value | |
|---|---|---|---|---|---|
| Maternal age at the time of delivery in years, mean | 29.0 (28.5–29.6) | 29.7 (28.6–30.9) | 29.0 (28.0–30.1) | 28.7 (27.9–29.5) | 0.35 b |
| Age at Visit 1 in years, mean | 25.8 (25.3–26.3) | 26.5 (25.3–27.7) | 26.1 (25.2–26.9) | 25.3 (24.5–26.1) | 0.21 b |
| < 35 years | 94.6 (92.4–96.8) | 21.7 (16.4–27.0) | 28.9 (23.1–34.6) | 49.4 (42.8–56.1) | 0.003 |
| ≥ 35 years | 5.4 (3.2–7.6) | 44.7 (29.3–60.2) | 18.8 (8.8–28.8) | 36.5 (21.6–51.3) | |
| Hispanic/Latino background | 0.31 | ||||
| Mexican | 52.5 (46.2–58.8) | 25.1 (17.9–32.2) | 28.1 (20.6–35.6) | 46.8 (38.3–55.3) | |
| Cuban | 14.3 (9.7–19.0) | 10.0 (1.6–18.5) | 40.9 (22.2–59.5) | 49.1 (29.0–69.1) | |
| Puerto Rican | 9.2 (6.3–12.0) | 25.4 (10.8–39.9) | 23.4 (9.2–37.6) | 51.2 (35.1–67.4) | |
| Dominican | 10.3 (6.5–14.1) | 34.8 (15.9–53.7) | 14.7 (0.6–28.9) | 50.5 (29.9–71.0) | |
| Central American | 7.3 (4.7–10.0) | 17.4 (7.1–27.7) | 25.0 (9.8–40.1) | 57.6 (42.6–72.6) | |
| South American | 3.7 (1.8–5.7) | 22.7 (0.0–45.5) | 35.6 (17.7–53.5) | 41.7 (20.9–62.4) | |
| Other | 2.7 (1.2–4.2) | 12.3 (0.0–30.0) | 33.4 (7.2–59.6) | 54.2 (26.5–82.0) | |
| Site | 0.11 | ||||
| Bronx | 27.2 (20.6–33.7) | 34.3 (20.6–47.9) | 20.7 (11.0–30.4) | 45.0 (29.7–60.3) | |
| Chicago | 18.6 (14.6–22.7) | 23.7 (15.1–32.4) | 27.2 (18.4–35.9) | 49.1 (40.6–57.6) | |
| Miami | 21.6 (15.8–27.4) | 12.8 (4.7–20.8) | 35.1 (21.9–48.3) | 52.1 (36.5–67.8) | |
| San Diego | 32.6 (25.9–39.3) | 19.8 (11.9–27.8) | 30.8 (21.0–40.6) | 49.4 (39.4–59.3) | |
| Education | 0.12 | ||||
| Less than high school | 25.2 (20.2–30.2) | 21.7 (12.8–30.7) | 25.2 (15.8–34.7) | 53.0 (41.7–64.3) | |
| High school or equivalent | 30.5 (25.3–35.7) | 28.3 (18.1–38.5) | 20.5 (11.8–29.1) | 51.2 (40.7–61.7) | |
| Greater than high school or equivalent | 44.3 (38.6–50.1) | 20.0 (13.3–26.6) | 35.4 (26.9–43.9) | 44.6 (35.2–54.0) | |
| Marital Status | 0.59 | ||||
| Single | 43.5 (37.8–49.2) | 26.1 (17.0–35.2) | 25.1 (17.8–32.5) | 48.8 (39.8–57.7) | |
| Married | 52.4 (46.6–58.1) | 19.8 (13.8–25.7) | 30.8 (22.6–39.0) | 49.4 (40.4–58.4) | |
| Separated, divorced, widow | 4.1 (2.2–6.1) | 30.0 (9.0–51.1) | 30.0 (9.9–50.2) | 39.9 (14.6–65.2) | |
| Household Income | 0.48 | ||||
| Less than $30,000 | 62.7 (56.8–68.5) | 25.6 (19.0–32.2) | 28.1 (21.5–34.8) | 46.3 (38.3–54.3) | |
| $30,000 or more | 29.0 (23.4–34.6) | 19.7 (12.3–27.2) | 25.9 (16.3–35.5) | 54.4 (43.0–65.7) | |
| Not reported | 8.4 (5.0–11.7) | 14.5 (1.5–27.5) | 37.9 (15.4–60.4) | 47.6 (26.7–68.5) | |
| Average daily sleep duration (hours) | 8.3 (8.1–8.5) | 8.0 (7.7–8.4) | 8.3 (8.0–8.7) | 8.5 (8.2–8.7) | 0.13 b |
| Employment | 0.72 | ||||
| Full time | 24.7 (19.7–29.6) | 24.7 (15.5–33.9) | 30.4 (19.7–41.1) | 44.9 (33.7–56.0) | |
| Part time | 23.7 (19.1–28.3) | 26.0 (14.9–37.0) | 29.9 (19.3–40.5) | 44.1 (32.0–56.3) | |
| Not retired and not currently employed | 51.7 (46.0–57.3) | 20.7 (14.2–27.3) | 26.6 (18.8–34.3) | 52.7 (44.2–61.1) | |
| Health Insurance Coverage | 0.33 | ||||
| No coverage at baseline | 51.6 (45.5–57.6) | 19.8 (13.7–25.9) | 30.5 (23.1–37.9) | 49.7 (41.2–58.2) | |
| Coverage at baseline | 48.3 (42.2–54.3) | 26.4 (18.9–34.0) | 25.7 (17.9–33.6) | 47.8 (39.3–56.4) | |
| Language Preference | 0.43 | ||||
| Spanish | 71.8 (66.6–77.0) | 24.6 (18.7–30.5) | 28.7 (21.8–35.6) | 46.7 (38.6–54.8) | |
| English | 28.2 (23.0–33.4) | 18.7 (10.4–27.0) | 27.3 (18.6–36.1) | 53.9 (44.0–63.9) | |
| Nativity/Years in the US | 0.25 | ||||
| Born in U.S. | 30.5 (25.2–35.8) | 18.3 (10.5–26.1) | 28.8 (19.5–38.1) | 52.9 (43.1–62.7) | |
| 10 years or greater | 30.8 (25.0–36.6) | 19.5 (11.5–27.5) | 27.4 (18.1–36.7) | 53.1 (43.0–63.1) | |
| 0–10 years | 38.7 (32.6–44.8) | 29.4 (20.7–38.1) | 28.6 (19.4–37.9) | 42.0 (32.0–52.0) | |
| Immigration age not reported/missing | 30.5 (25.2–35.8) | 18.3 (10.5–26.1) | 28.8 (19.5–38.1) | 52.9 (43.1–62.7) | |
| Pre-pregnancy BMI | <0.001 | ||||
| Underweight/Normal (< 25 kg/m2) | 36.8 (31.4–42.2) | 37.6 (28.4–46.8) | 28.2 (19.2–37.3) | 34.2 (23.5–44.8) | |
| Overweight (25-< 30 kg/m2) | 30.6 (25.6–35.6) | 16.7 (8.7–24.7) | 26.0 (16.4–35.6) | 57.2 (46.8–67.7) | |
| Obese (≥ 30 kg/m2) | 32.6 (27.4–37.8) | 12.3 (6.1–18.4) | 30.6 (20.9–40.2) | 57.2 (47.2–67.2) | |
| Gravidity, median (refers to pregnancies prior to Visit 1) | 0.65 | ||||
| 0 previous pregnancies | 31.4 (25.6–37.3) | 19.8 (11.8–27.8) | 33.4 (22.2–44.6) | 46.8 (35.4–58.2) | |
| 1 previous pregnancy | 27.7 (22.7–32.7) | 26.5 (16.6–36.4) | 27.1 (17.6–36.6) | 46.4 (35.7–57.1) | |
| 2 or more previous pregnancies | 40.9 (34.8–47.0) | 23.0 (15.8–30.2) | 25.2 (17.3–33.2) | 51.8 (41.4–62.1) | |
| Gestational age at delivery | 0.95 b | ||||
| < 37 weeks | 10.5 (7.4–13.7) | 24.2 (10.8–37.7) | 26.0 (12.1–40.0) | 49.7 (33.9–65.6) | |
| ≥ 37 weeks | 89.5 (86.3–92.6) | 22.8 (17.2–28.4) | 28.6 (22.7–34.5) | 48.6 (41.7–55.5) | |
| Gestational age at delivery, mean | 38.8 (38.6–39.1) | 39.0 (38.6–39.4) | 38.8 (38.3–39.2) | 38.8 (38.4–39.1) | 0.61 b |
| Years between Visit 1 and delivery | 3.2 (3.0–3.5) | 3.2 (2.8–3.6) | 3.0 (2.6–3.3) | 3.4 (3.0–3.8) | 0.25 b |
| CESD10, mean | 6.9 (6.2–7.5) | 7.2 (6.1–8.3) | 7.0 (5.7–8.3) | 6.7 (5.7–7.6) | 0.77 b |
| STAI10, mean | 17.7 (17.0–18.4) | 17.7 (16.5–18.8) | 17.6 (16.3–19.0) | 17.7 (16.5–18.8) | 0.99 b |
Gestational weight gain defined as 28–40 pounds for pre-pregnancy BMI <18.5 kg/m2, 25–35 pounds for pre-pregnancy BMI 18.5–24.9 kg/m2, 15–25 pounds for pre-pregnancy BMI 25.0–29.9 kg/m2, and 11–20 pounds for pre-pregnancy BMI ≥ 30kg/m2.
p-value as determined by ANOVA testing, all other p-values are from Chi-square tests
GWG gestational weight gain
BMI body mass index
US United States
CESD10 Center for Epidemiologic Studies Depression Scale
STAI10 Spielberger anxiety scale
For this analysis, women were included if they participated in both visits 1 and 2 and had one or more singleton pregnancies between these visits that resulted in a live birth. For women who had more than one pregnancy between visits 1 and 2, only the first pregnancy was included in the analysis. Women who did not report GWG or were missing BMI at visit 1 were excluded. The primary outcome of self-reported weight gain was measured according to the response to the question, “How much weight did you gain during this pregnancy?” as collected at visit 2. The distribution of GWG was checked using QQ plots. GWG was analyzed both as a continuous variable (pounds) and categorized according to recommendations from the IOM Guidelines (28–40 pounds for pre-pregnancy BMI <18.5 kg/m2, 25–35 pounds for pre-pregnancy BMI 18.5–24.9 kg/m2, 15–25 pounds for pre-pregnancy BMI 25.0–29.9 kg/m2, and 11–20 pounds for pre-pregnancy BMI ≥ 30 kg/m2) (Institute of Medicine, 2009). Categories of GWG included inadequate (below GWG guidelines), adequate (met GWG guidelines), and excessive (higher than GWG guidelines) based on the GWG and pre-pregnancy BMI. Similar to Savitz et al (2011), gestational age at delivery was accounted for by calculating the weekly rate of GWG (weeks of gestation at delivery divided by total weight gain), multiplied by 40 to estimate the amount of weight gain projected had the pregnancy lasted 40 weeks, and used the same category cut points as for GWG among term births. This adjustment was done for all participants, regardless of whether the delivery was pre-term. Because BMI immediately before conception was not available, we used BMI from visit 1 as a proxy for pre-pregnancy BMI.
At visit 1, two 24-hour dietary recalls were typically collected, one in person and then one over the phone, usually within a month of the first. For dietary data, we used the scores for the alternative healthy eating index (AHEI-2010) calculated from a 24-hour dietary recall using the National Cancer Institute method to predict usual intake to measure diet quality (Guenther et al., 2013; Siega-Riz et al., 2014). The AHEI-2010 is derived from 11 components (whole fruits, total vegetables, whole grains, sugar-sweetened beverages and fruit juice, nuts and legumes, fresh red meat, processed meat, fish, unsaturated fatty acid rich foods, alcohol, sodium), each taking a value of 0 (worst) to 10 (best) with final scores ranging from 0 to 110, with higher scores signified healthier diet quality. Additionally, mean total energy intake (kcal) per day was calculated.
Physical activity was assessed at visit 1 with the Global Physical Activity Questionnaire, which has acceptable reliability and validity with other physical activity measures (Bull et al., 2009). Self-reported minutes/day of total moderate to vigorous physical activity from a typical week were calculated from work, transportation, and leisure activities. Total physical activity was also categorized as to whether participants met the 2008 US physical activity guidelines of at least 150 minutes/week of moderate-intensity activity, at least 75 minutes/week of vigorous intensity activity, or an equivalent combination of the two (US Department of Health and Human Services, 2008). Self-reported minutes/day in sedentary behavior on a typical day was evaluated from a single question on time spent sitting or reclining.
Visit 1 characteristics included self-reported age, self-reported type of Hispanic/Latina background or heritage (Cuban, Central American, Dominican, Mexican, Puerto Rican, South American, and other), site, education, marital status, household income, sleep duration, employment, health insurance, language of interview, nativity (born in the 50 United States vs. born in a United States territory or foreign country), immigration age if applicable, anxiety (measured with Spielberger trait anxiety scale (Spielberger C, 1983)), and depressive symptoms (measured with the Center for Epidemiologic Studies Depression Scale, CES-D-10 (Radloff, 1977)). Height and weight were measured at visit 1, and these values were used to calculate pre-pregnancy (or pre-conception) BMI. At visit 2, women self-reported the number of pregnancies before visit 1 (gravidity), and all pregnancies after visit 1 that lasted at least six months including length of gestation (in weeks or months), and the date when each pregnancy ended.
Analysis was performed using SAS version 9.4 (SAS Institute, Cary, NC) and accounted for the complex sample design in which visit 2 weights, cluster sampling, and stratification are all considered in the analysis.
Descriptive statistics on maternal demographics and other covariates for the study sample by GWG categories were calculated and compared with Chi-square tests. Mean AHEI-2010, energy intake, moderate to vigorous physical activity, meeting 2008 physical activity guidelines, and sedentary behavior with standard errors (SE) by GWG category were calculated and compared with analysis of variance (ANOVA) or Chi-squared tests, as appropriate. Differences in health behaviors were also compared by background and the three GWG categories. Tests for interactions between GWG and background were done with ANOVA tests. A p-value <0.05 was considered statistically significant.
Linear and generalized logit survey regression analyses were then conducted to quantify the association between diet, sedentary behavior, and physical activity separately with continuous GWG and GWG categories using adequate GWG as the reference. After an evaluation of LOESS plots and restricted cubic splines, we opted to use linear measures of diet and physical activity since all p-values were <0.05. For diet, the association of a 10-unit increase of AHEI-2010 and 500 kcal/day increase of total energy intake with continuous GWG and by GWG category were calculated. For sedentary behavior and physical activity, the association of continuous measures of total sedentary behavior and physical activity in minutes/day with continuous GWG and with GWG category were calculated. Models for diet, sedentary behavior, and physical activity were separately adjusted for age at the time of delivery, Hispanic/Latina background, marital status, years in the United States, BMI at visit 1, gravidity (number of previous pregnancies) (model 1). Model 2 covariates included model 1 covariates in addition to education, household income, anxiety (Spielberger scale), depression (CES-D 10), length of gestation, and time between visit 1 and delivery to separately account for social, economic and structural factors. Beta coefficients or odds ratios (OR) with 95% CI were reported. To account for the time lapse from visit 1 and subsequent pregnancy, a sensitivity analysis was performed limiting the participants to women who delivered within 2 years of visit 1.
Results
Of the 16,415 HCHS/SOL participants at visit 1, 9835 were women. Of the 11,623 participants at visit 2, 7324 were women. For the current study, 557 women participated in both visit 1 and visit 2 and had one or more singleton pregnancies between visit 1 and visit 2 that resulted in a live birth. For women who had more than one pregnancy between visit 1 and 2, only the first pregnancy was included in the analysis (n=539 women). Women who did not report GWG or were missing BMI were excluded (n=60). For the 60 women excluded due to missing GWG or BMI, we noted higher energy intake (1665.2 kcal/d, SE 50.5 vs. 1789.5 kcal/d, SE 20.9; p=0.02), but no other difference in health behaviors (AHEI-2010 scores, sedentary behavior, total physical activity, and meeting 2008 physical activity guidelines) compared with those who were included in the analysis. In addition, 22 participants were excluded from analyses because of missing data on pregnancy length, time elapsed between visit 1 and delivery, diet, physical activity, or other covariates. Thus, these analyses are based on data from 457 participants (Figure 1).
Figure 1:
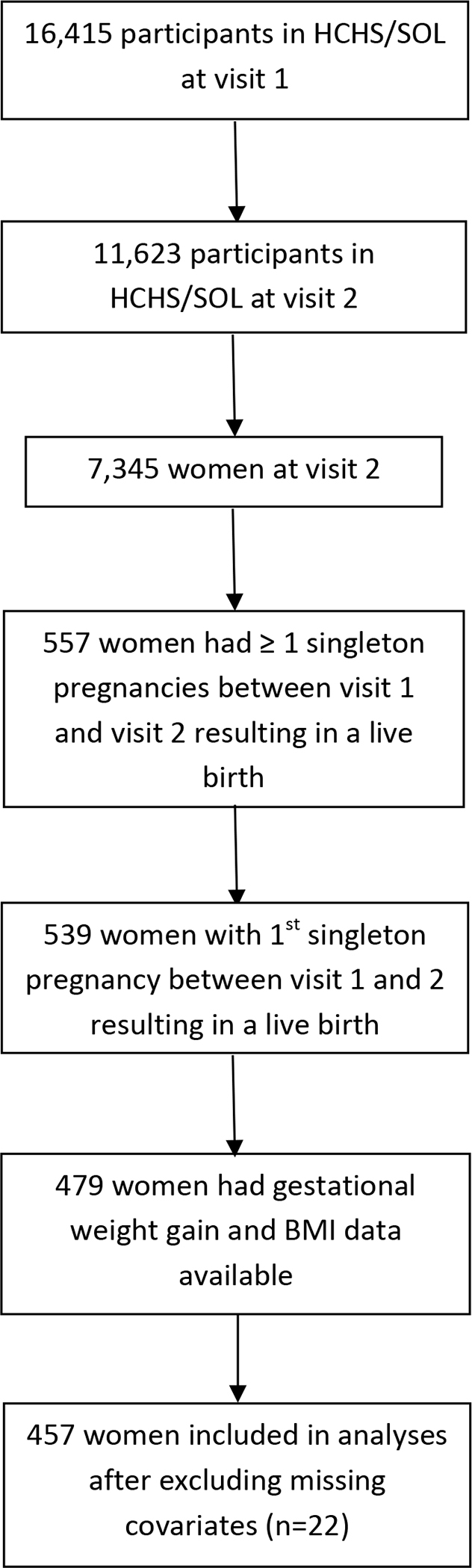
Flow diagram of participant selection
In the target population, we estimated 23.0%, 28.3%, and 48.7% of women had inadequate, adequate, and excessive GWG, respectively (Table 1). About half of the women were of Mexican background (52.5%), followed by Cuban (14.3%), Dominican (10.3%), and Puerto Rican (9.2%). At visit 1, 31.4% of all women were nulligravida and 32.6% had a BMI ≥ 30 kg/m2. Overall, the mean gestational age at delivery was 38.8 weeks. The deliveries occurred at a mean of 3.2 years (range 0.5–8.9 years) after visit 1.
We found no differences in maternal sociodemographic (age at delivery, Hispanic/Latina background, site, education, marital status, household income, employment, health insurance coverage, language preference) across the three GWG categories (p>0.05 for all comparisons, Table 1). However, we found tdifferences in age categories; women ≥ 35 years had higher frequency of inadequate GWG compared with women <35 years, p=0.003. Additionally, women with overweight or obesity at visit 1 had a higher frequency of excessive GWG compared with women who were underweight or normal weight (p<0.001).
Preconception Diet and GWG
Overall, mean energy intake was 1798 (SE 23) kcal/d and was highest for women with adequate GWG, but mean energy intake was not statistically different among the three GWG categories (p=0.33). Mean energy intake did vary by background (p<0.001 for each of the three GWG categories), with Dominican women having the lowest energy intake in the inadequate and excessive GWG categories (Table 2). The total AHEI-2010 scores were low (e.g., mean values of 44.0–44.1 for all GWG categories). The scores did not differ statistically across the GWG categories, but were different among background, with Mexican women having the highest AHEI-2010 scores in all GWG categories (p<0.001) (Table 2). Tests for interactions between background and GWG for energy intake and AHEI-2010 were not statistically significant (p>0.05 for both comparisons).
Table 2.
Mean preconception total energy intake and AHEI-2010 by gestational weight gain categories and by Hispanic/Latino background.
| N=457 | Energy Intake (kcal/d) | Energy Intake (kcal/d) by Hispanic/Latino Background | |||||||||||||||
| Mexican (n=244) | Cuban (n=40) | Puerto Rican (n=46) | Dominican (n=39) | Central American (n=49) | South American (n=24) | Other (n=15) | |||||||||||
| GWG Categories | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | P-valuea |
| Inadequate | 111 | 1760.7 (39.6) | 67 | 1813.3 (51.6) | 5 | 2082.5 (88.2) | 11 | 1649.0 (125.7) | 13 | 1558.4 (115.0) | 8 | 1588.5 (68.6) | 5 | 1614.2 (103.9) | 2 | 2275.1 (25.0) | <0.001 |
| Adequate | 124 | 1838.4 (40.1) | 68 | 1883.2 (51.9) | 15 | 1987.9 (62.4) | 10 | 1785.2 (121.7) | 5 | 1449.7 (141.8) | 12 | 1421.7 (127.4) | 9 | 1862.1 (98.3) | 5 | 1722.0 (52.7) | <0.001 |
| Excessive | 222 | 1792.7 (33.7) | 109 | 1828.3 (48.9) | 20 | 2016.4 (108.6) | 25 | 1676.9 (77.3) | 21 | 1457.7 (64.2) | 29 | 1740.3 (46.7) | 10 | 1777.1 (93.4) | 8 | 1845.5 (112.9) | <0.001 |
| P-value from ANOVA | 0.33 b | ||||||||||||||||
| N=457 | Total AHEI-2010 | AHEI-2010 by Hispanic/Latino Background | |||||||||||||||
| Mexican (n=244) | Cuban (n=40) | Puerto Rican (n=46) | Dominican (n=39) | Central American (n=49) | South American (n=24) | Other (n=15) | |||||||||||
| GWG Categories | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | P-valuea |
| Inadequate | 111 | 44.0 (0.7) | 67 | 46.9 (0.9) | 5 | 38.8 (2.1) | 11 | 37.3 (1.8) | 13 | 41.7 (1.2) | 8 | 41.7 (1.4) | 5 | 40.8 (0.8) | 2 | 41.5 (3.9) | <0.001 |
| Adequate | 124 | 44.1 (0.6) | 68 | 47.3 (0.6) | 15 | 39.0 (1.1) | 10 | 38.9 (1.2) | 5 | 45.1 (1.8) | 12 | 41.9 (0.8) | 9 | 42.6 (1.7) | 5 | 43.5 (2.9) | <0.001 |
| Excessive | 222 | 44.0 (0.5) | 109 | 46.4 (0.5) | 20 | 39.6 (1.8) | 25 | 39.6 (1.1) | 21 | 45.3 (0.9) | 29 | 42.2 (0.9) | 10 | 42.0 (1.4) | 8 | 41.3 (1.2) | <0.001 |
| P-value from ANOVA | 0.97 c | ||||||||||||||||
P-value pertains to ANOVA comparison for energy intake or AHEI-2010 and background within each GWG category
P-value pertains to ANOVA comparison for energy intake and GWG category
P-value pertains to ANOVA comparison for Total AHEI-2010 and GWG category
Ns are unweighted, proportions are weighted
Data presented as mean (SE)
ANOVA Analysis of variance
AHEI alternative healthy eating index
GWG Gestational weight gain
In linear regression analyses, we found no association between each 10-unit increase in AHEI-2010 and a 500kcal/day increase in energy intake for a continuous measure of GWG in models 1 and model 2 (Table 3). Similarly, in logistic regression analyses, we found no association between a 500kcal/day increase in energy intake and each 10-unit increase in AHEI-2010 in models 1 and 2 for the GWG categories. In a sensitivity analysis limited to women who delivered within 2 years of visit 1 (n=154), we similarly found no association between AHEI-2010 or energy intake and GWG as a linear or categorical measure (data not shown).
Table 3.
Linear and logistic regression analyses for the association between preconception diet, indexed by a 500 kcal/day increase in energy intake and each 10-unit increase in AHEI-2010 and change in adjusted gestational weight gain (pounds) and adjusted gestational weight gain category.
| Energy Intake (kcal/d) | Total AHEI-2010 | |||||
|---|---|---|---|---|---|---|
| Model | N | β | 95% CI | N | β | 95% CI |
| Unadjusted | ||||||
| Continuous GWG | 457 | −1.31 | −4.89,2.27 | 457 | −0.32 | −4.04,3.40 |
| Categorical GWG | OR | OR | ||||
| Inadequate | 111 | 0.74 | 0.49,1.12 | 111 | 0.96 | 0.54,1.71 |
| Adequate | 124 | Ref. | 124 | Ref. | ||
| Excessive | 222 | 0.84 | 0.55,1.26 | 222 | 0.96 | 0.60,1.53 |
| Model 1 | β | β | ||||
| Continuous GWG | 457 | −2.34 | −6.53,1.86 | 457 | 2.62 | −2.64,7.87 |
| Categorical GWG | OR | OR | ||||
| Inadequate | 111 | 1.02 | 0.62,1.69 | 111 | 0.50 | 0.24,1.07 |
| Adequate | 124 | Ref. | 124 | Ref. | ||
| Excessive | 222 | 0.96 | 0.62,1.51 | 222 | 0.96 | 0.53,1.72 |
| Model 2 | β | β | ||||
| Continuous GWG | 457 | −2.00 | −5.62,1.63 | 457 | 2.70 | −2.44,7.84 |
| Categorical GWG | OR | OR | ||||
| Inadequate | 111 | 1.21 | 0.71,2.07 | 111 | 0.43 | 0.19,0.95 |
| Adequate | 124 | Ref. | 124 | Ref. | ||
| Excessive | 222 | 1.06 | 0.65,1.73 | 222 | 0.88 | 0.48,1.63 |
Model 1. Adjusted for maternal age at the time of delivery, Hispanic/Latina background, marital status, years in the United States, body mass index, and gravidity (number of previous pregnancies).
Model 2. Adjusted for maternal age at the time of delivery, Hispanic/Latina background, education level, marital status, household income, years in the United States, anxiety (Spielberger scale), depression (CESD), body mass index, gravidity (number of previous pregnancies), length of gestation, and time lapse since visit 1
GWG gestational weight gain
AHEI alternative healthy eating index
Preconception Sedentary Behavior and Physical Activity
Overall sedentary behavior was 269.5 (SE 9.7) minutes/day and total physical activity was 122.8 (SE 9.3) minutes/day. We found no association between sedentary behavior and GWG, total physical activity and GWG, or meeting 2008 physical activity guidelines and GWG (Table 4). Sedentary behavior did vary by GWG categories and background for women with inadequate GWG (p=0.004), with Central American women having the lowest sedentary behavior (148.3, min SE 52.3). We noted wide variations in total physical activity by background. For example, within the inadequate GWG category, Puerto Rican women had the highest total physical activity (280.9 min, SE 96.6) and women of other background had the lowest physical activity (26.3 min, SE 6.5). Differences among physical activity and background for women with inadequate GWG and excessive GWG were found (Table 4). Tests for interactions between background and GWG for sedentary behavior, total physical activity, and physical activity goals were not statistically significant (p>0.05 for all comparisons).
Table 4.
Mean preconception sedentary behavior and physical activity by gestational weight gain categories and by Hispanic/Latino background
| N=457 | Sedentary Behavior (min) | Sedentary Behavior by Hispanic/Latino Background | ||||||||||||||||
| Mexican (n=244) | Cuban (n=40) | Puerto Rican (n=46) | Dominican (n=39) | Central American (n=49) | South American (n=24) | Other (n=15) | ||||||||||||
| GWG Categories | N | (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | P-valuea | |
| Inadequate | 111 | 234.4 (16.8) | 67 | 220.3 (15.5) | 5 | 323.7 (76.3) | 11 | 280.1 (69.6) | 13 | 221.6 (43.8) | 8 | 148.3 (52.3) | 5 | 320.3 (100.6) | 2 | 337.3 (84.7) | 0.004 | |
| Adequate | 124 | 281.1 (19.5) | 68 | 258.1 (29.4) | 15 | 353.1 (37.3) | 10 | 258.9 (48.2) | 5 | 312.4 (50.9) | 12 | 252.6 (58.0) | 9 | 254.8 (62.5) | 5 | 288.3 (131.8) | 0.48 | |
| Excessive | 222 | 279.3 (14.8) | 109 | 239.7 (18.5) | 20 | 319.4 (31.8) | 25 | 281.7 (38.1) | 21 | 349.2 (51.2) | 29 | 263.2 (34.6) | 10 | 310.5 (114.3) | 8 | 512.5 (147.8) | 0.11 | |
| P-value | 0.10 b | |||||||||||||||||
| N=457 | Total Physical Activity (min) | Physical Activity Guidelines 2008 | Total Physical Activity by Hispanic/Latino Background | |||||||||||||||
| Mexican (n=244) | Cuban (n=40) | Puerto Rican (n=46) | Dominican (n=39) | Central American (n=49) | South American (n=24) | Other (n=15) | ||||||||||||
| GWG Categories | N | Mean (SE) | N(%) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | N | Mean (SE) | P-valuea |
| Inadequate | 111 | 128.1 (20.4) | 78 (70.9%) | 67 | 110.2 (25.4) | 5 | 34.5 (20.9) | 11 | 280.9 (96.6) | 13 | 105.7 (24.7) | 8 | 223.4 (80.7) | 5 | 135.9 (30.4) | 2 | 26.3 (6.5) | 0.001 |
| Adequate | 124 | 116.8 (20.4) | 77 (65.7%) | 68 | 87.6 (21.1) | 15 | 167.0 (67.9) | 10 | 105.3 (45.5) | 5 | 182.9 (107.8) | 12 | 143.2 (53.9) | 9 | 87.5 (24.0) | 5 | 176.3 (93.3) | 0.73 |
| Excessive | 222 | 123.8 (12.6) | 156 (74.1%) | 109 | 125.5 (16.6) | 20 | 108.6 (49.2) | 25 | 173.0 (38.9) | 21 | 128.6 (43.3) | 29 | 125.5 (34.0) | 10 | 78.5 (36.1) | 8 | 35.1 (16.7) | 0.001 |
| P-value from ANOVA | 0.92 c (ANOVA) | 0.43 d (Chi-square) | ||||||||||||||||
P-value pertains to ANOVA comparison for sedentary behavior or total physical activity and background for each GWG category
P-value pertains to ANOVA comparison for sedentary behavior and GWG category
P-value pertains to ANOVA comparison for total physical activity and GWG category
P-value pertains to Chi-square comparison for meeting 2008 physical activity guidelines and GWG category
Ns are unweighted, proportions are weighted
Data presented as mean (SE) or n(%)
ANOVA Analysis of variance
GWG Gestational weight gain
SE standard error
Physical activity goals 2008: Percent of participants meeting the 2008 Physical Activity Goals
In linear regression analyses, we found no association between 30 minutes/day higher sedentary behavior, 30 minutes/day higher total physical activity, or meeting the 2008 US physical activity guidelines and GWG in models 1 or 2. Similarly, in logistic regression analyses, we found no association between 30 minutes/day higher sedentary behavior, 30 minutes/day higher total physical activity, and meeting the 2008 physical activity guidelines with the GWG categories in models 1 and 2 (Table 5). In a sensitivity analysis limited to women who delivered within 2 years after visit 1 (n=154), we similarly did not find an association between sedentary behavior or total physical activity and GWG as a linear or categorical measure (data not shown).
Table 5.
Linear and logistic regression analyses for the association between physical activity in the preconception period, indexed by a 30 mins/day increase in sedentary time, a 30 mins/day increase in total physical activity, and meeting 2008 Physical Activity Guidelines and change in adjusted gestational weight gain (pounds) and adjusted gestational weight gain category.
| Sedentary Behavior | Total physical activity | Meets 2008 physical activity guidelines | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Model | N | β | 95% CI | N | β | 95% CI | N | β | 95% CI |
| Unadjusted | |||||||||
| Continuous GWG | 457 | 0.14 | −0.21,0.50 | 457 | 0.11 | −0.35,0.56 | 457 | 3.35 | −1.16,7.86 |
| Categorical GWG | |||||||||
| Inadequate | 111 | 0.95 | 0.91,1.01 | 111 | 1.01 | 0.95,1.08 | 111 | 1.27 | 0.63,2.54 |
| Adequate | 124 | Ref. | 124 | Ref. | 124 | Ref. | |||
| Excessive | 222 | 1.00 | 0.96,1.04 | 222 | 1.01 | 0.95,1.07 | 222 | 1.50 | 0.79,2.84 |
| Model 1 | |||||||||
| Continuous GWG | 0.12 | −0.20,0.43 | 457 | 0.08 | −0.36,0.52 | 3.66 | −1.09,8.41 | ||
| Categorical GWG | |||||||||
| Inadequate | 111 | 0.98 | 0.93,1.04 | 111 | 1.00 | 0.94,1.07 | 111 | 1.12 | 0.55,2.28 |
| Adequate | 124 | Ref. | 124 | Ref. | 124 | Ref. | |||
| Excessive | 222 | 1.00 | 0.96,1.04 | 222 | 1.01 | 0.95,1.08 | 222 | 1.58 | 0.80,3.11 |
| Model 2 | |||||||||
| Continuous GWG | 457 | 0.16 | −0.11,0.43 | 457 | 0.13 | −0.31,0.56 | 457 | 3.86 | −0.71,8.43 |
| Categorical GWG | |||||||||
| Inadequate | 111 | 0.99 | 0.93,1.05 | 111 | 1.02 | 0.95,1.09 | 111 | 1.10 | 0.53,2.27 |
| Adequate | 124 | Ref. | 124 | Ref. | 124 | Ref. | |||
| Excessive | 222 | 1.00 | 0.96,1.05 | 222 | 1.03 | 0.97,1.09 | 222 | 1.63 | 0.82,3.21 |
Model 1. Adjusted for maternal age at the time of delivery, Hispanic/Latina background, marital status, years in the United States, body mass index, and gravidity (number of previous pregnancies).
Model 2. Adjusted for maternal age at the time of delivery, Hispanic/Latina background, education level, marital status, household income, years in the United States, anxiety (Spielberger scale), depression (CES-D), body mass index, gravidity (number of previous pregnancies), length of gestation, and time lapse since visit 1
GWG gestational weight gain
Discussion
In our study of 457 Hispanic/Latina women, we did not find an association between diet, sedentary behavior, or physical activity at visit 1 with GWG in pregnancies that occurred between visits 1 and 2 (approximately 6 years of follow-up). We noted widespread low diet quality as measured by AHEI-2010 and low total physical activity as measured by the Global Physical Activity Questionnaire. Less than 75% of all women met the 2008 physical activity recommendations across all GWG categories. When evaluating diet by background, differences in total energy intake and AHEI-2010 among all GWG categories were found (p < 0.001), but consistent trends among backgrounds and diet were not noted. We also noted differences in sedentary behaviors for women with inadequate GWG and in physical activity for women with inadequate and excessive GWG by background. In the unadjusted and adjusted models, we also did not find significant associations between diet, sedentary behavior, or physical activity and GWG as a continuous or categorical measure. We theorize that the lack of association between pre-conception health behaviors and GWG may be attributed to the overall low diet quality and low physical activity among all the women and therefore a lack of range in values. Lastly, social determinants of health such as access to care and food security are also known to be associated with health behaviors and weight, but they were not specifically measured in this study.
Our findings confirm and extend other studies of Hispanic/Latina women during pregnancy. For example, Tovar et al. reported the results of a semi-quantitative food frequency questionnaire among 423 Hispanic pregnant women in the US with and without diabetes (Tovar et al., 2009). The mean daily caloric intake range was around 2500 kcal, but the relationship between diet and GWG could not be completely assessed because the weight gain was only accounted for up until the time of screening for gestational diabetes (i.e., < 28 weeks). Dolin et al. evaluated the relationship between diet with the 2005 Block Food Frequency Questionnaire and physical activity with the 2011 Behavioral Risk Factor Surveillance System questions in 508 Hispanic/Latina women in the US during pregnancy, the majority of whom were not able to meet the recommended daily intakes of selected dietary variables (<25% for dairy, vegetables, whole fruit, whole grains) or physical activity recommendations (32% met recommendations) (Dolin et al., 2020). Among these women, meeting physical activity recommendations of at least 150 min per week was associated with 1 kg lower total GWG (−1.00 kg; 95% CI −1.99, −0.03), but no associations between GWG and adhering to dietary recommendations were found.
Other studies of physical activity prior to pregnancy in Hispanic women also found low adherence to physical activity guidelines. Among 632 Hispanic women (Puerto Rican or Dominican Republican) who completed the Pregnancy Physical Activity Questionnaire (PPAQ) 1 year prior to pregnancy, 18.7% met the American College of Obstetricians and Gynecologists’ recommendations for physical activity (Chasan-Taber et al., 2010). Of further interest, the proportion of women meeting physical activity goals dropped to 5.2% when the PPAQ was completed early in the pregnancy (Chasan-Taber et al., 2010). In a separate study of 1160 Puerto Rican or Dominican women, no differences in type or intensity of physical activity and GWG, as assessed by the PPAQ prior to pregnancy, were found (Chasan-Taber et al., 2014).
With respect to BMI and GWG in general, we found that both pre-conception obesity and excessive GWG were common. Our findings are similar to other studies of GWG in Hispanic/Latina women. In a study of 282 Hispanic/Latina women, 45% had excessive GWG, 32% had inadequate GWG, and only 24% had adequate GWG (Sangi-Haghpeykar et al., 2014). Chasan-Taber et al reported that among 1359 Puerto Rican or Dominican women, 20.2% had inadequate, 27.3% had adequate, and 52.5% had excessive GWG in the total cohort (Chasan-Taber et al., 2016). We did not find significant differences in GWG among women from 7 Hispanic/Latina background groups. Nearly one-third of the women in our study had obesity at visit 1.
Limitations
We acknowledge several limitations to this study, including self-reported diet, sedentary behavior, and physical activity that were recorded a mean of 3.2 years (range 0.5–8.9 years) prior to delivery. These behaviors were not measured during pregnancy, so it was not possible to determine the extent to which they may have changed with pregnancy. Pre-pregnancy BMI category may have been misclassified if women changed BMI categories between visit 1 and conception. GWG was also based on maternal self-report. Although GWG misclassification based on maternal self-report may have occurred, evidence supports the reliability of this measure in the absence of birth certificate data or medical records (Hinkle et al., 2013), including a systematic review concluding that misclassification of GWG post-pregnancy was moderate and did not largely bias associations with birth outcomes (Headen et al., 2017). For some analyses, including those testing interactions between background and health behaviors, the sample size was small and a larger sample would be ideal to examine differences among Hispanic/Latina background.
Conclusions
Among diverse Hispanic/Latinas from four communities in the US, preconception diet, sedentary behavior, and physical activity were not associated with GWG. These reproductive-age women had low AHEI-2010 scores, indicating poor diet quality, as well as suboptimal physical activity and sedentary behavior. These findings need to be interpreted in the context of other factors that contribute to health behaviors and GWG, such as access to healthy food, opportunities for safe physical activity, and support from a partner and family. An opportunity for Hispanic/Latina women to improve both diet quality and daily physical activity prior to pregnancy. Although pregnancy and the preconception period are windows of opportunity to intervene for health behaviors, interventions need to consider to other specific systemic and structural factors that influence diet and physical activity among Hispanic/Latina women.
Acknowledgements
The authors thank the staff and participants of HCHS/SOL for their important contributions. Investigators website - http://www.cscc.unc.edu/hchs/. The HCHS/SOL is a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (HHSN268201300001I / N01-HC-65233), University of Miami (HHSN268201300004I / N01-HC-65234), Albert Einstein College of Medicine (HHSN268201300002I / N01-HC 65235), University of Illinois at Chicago – HHSN268201300003I / N01-HC-65236 Northwestern University), and San Diego State University (HHSN268201300005I / N01-HC-65237). The following Institutes/Centers/Offices have contributed to the HCHS/SOL through a transfer of funds to the NHLBI: National Institute on Minority Health and Health Disparities, National Institute on Deafness and Other Communication Disorders, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Neurological Disorders and Stroke, NIH Institution-Office of Dietary Supplements.
Footnotes
The authors declare that they have no conflicts of interest to report.
Contributor Information
Michelle A. Kominiarek, Department of Obstetrics and Gynecology, Northwestern University.
Christina Cordero, Department of Psychology, University of Miami, Coral Gables, Florida.
Alison M. Stuebe, Department of Obstetrics and Gynecology, University of North Carolina School of Medicine, Chapel Hill, NC.
Melissa Simon, Department of Obstetrics and Gynecology, Northwestern University.
Kelly R Evenson, Department of Epidemiology, Gillings School of Global Public Health, UNC, Chapel Hill, NC.
Krista M Perreira, Department of Social Medicine, UNC School of Medicine, Chapel Hill, NC 27599.
Linda C Gallo, Department of Psychology, San Diego State University.
Sheila F Castañeda, Department of Psychology, San Diego State University.
JoNell E. Potter, Department of Obstetrics, Gynecology and Reproductive Sciences, University of Miami Miller School of Medicine, Miami, Florida 33101
Donghong Wu, Institute for Minority Health Research, University of Illinois at Chicago.
Carmen R Isasi, Department of Epidemiology & Population Health. Albert Einstein College of Medicine, Bronx, NY.
Martha L Daviglus, Institute for Minority Health Research, University of Illinois at Chicago.
References
- Bodnar LM, Siega-Riz AM, Simhan HN, Himes KP, & Abrams B (2010). Severe obesity, gestational weight gain, and adverse birth outcomes. American Journal of Clinical Nutrition, 91(6), 1642–1648. doi: 10.3945/ajcn.2009.29008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brawarsky P, Stotland NE, Jackson RA, Fuentes-Afflick E, Escobar GJ, Rubashkin N, & Haas JS (2005). Pre-pregnancy and pregnancy-related factors and the risk of excessive or inadequate gestational weight gain. International Journal of Gynaecology and Obstetrics, 91(2), 125–131. doi:S0020–7292(05)00474–1 [pii] 10.1016/j.ijgo.2005.08.008 [DOI] [PubMed] [Google Scholar]
- Bull FC, Maslin TS, & Armstrong T (2009). Global physical activity questionnaire (GPAQ): nine country reliability and validity study. Journal of Physical Activity and Health, 6(6), 790–804. doi: 10.1123/jpah.6.6.790 [DOI] [PubMed] [Google Scholar]
- Chasan-Taber L, Fortner RT, Gollenberg A, Buonnaccorsi J, Dole N, & Markenson G (2010). A prospective cohort study of modifiable risk factors for gestational diabetes among Hispanic women: design and baseline characteristics. Journal of Womens Health (Larchmt), 19(1), 117–124. doi: 10.1089/jwh.2009.1416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chasan-Taber L, Schmidt MD, Pekow P, Sternfeld B, Solomon CG, & Markenson G (2008). Predictors of excessive and inadequate gestational weight gain in Hispanic women. Obesity (Silver Spring), 16(7), 1657–1666. doi:oby2008256 [pii] 10.1038/oby.2008.256 [DOI] [PubMed] [Google Scholar]
- Chasan-Taber L, Silveira M, Lynch KE, Pekow P, Solomon CG, & Markenson G (2014). Physical activity and gestational weight gain in Hispanic women. Obesity (Silver Spring), 22(3), 909–918. doi: 10.1002/oby.20549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chasan-Taber L, Silveira M, Waring ME, Pekow P, Braun B, Manson JE, . . . Markenson G (2016). Gestational Weight Gain, Body Mass Index, and Risk of Hypertensive Disorders of Pregnancy in a Predominantly Puerto Rican Population. Maternal and Child Health Journal, 20(9), 1804–1813. doi: 10.1007/s10995-016-1983-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deputy NP, Sharma AJ, Kim SY, & Hinkle SN (2015). Prevalence and characteristics associated with gestational weight gain adequacy. Obstetrics and Gynecology, 125(4), 773–781. doi: 10.1097/AOG.0000000000000739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolin CD, Gross RS, Deierlein AL, Berube LT, Katzow M, Yaghoubian Y, . . . Messito MJ (2020). Predictors of Gestational Weight Gain in a Low-Income Hispanic Population: Sociodemographic Characteristics, Health Behaviors, and Psychosocial Stressors. International Journal of Environmental Research and Public Health, 17(1). doi: 10.3390/ijerph17010352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HA, Kuczynski KJ, . . . Krebs-Smith SM (2013). Update of the Healthy Eating Index: HEI-2010. Journal of the Academy of Nutrition and Dietetics, 113(4), 569–580. doi: 10.1016/j.jand.2012.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales CM, Carroll MD, Fryar CD, Ogden CL (2020). Prevalence of obesity and severe obesity among adults: United States, 2017–2018. Hyattsville, MD: National Center for Health Statistics [Google Scholar]
- Headen I, Cohen AK, Mujahid M, & Abrams B (2017). The accuracy of self-reported pregnancy-related weight: a systematic review. Obesity Reviews, 18(3), 350–369. doi: 10.1111/obr.12486 [DOI] [PubMed] [Google Scholar]
- Hinkle SN, Sharma AJ, Schieve LA, Ramakrishnan U, Swan DW, & Stein AD (2013). Reliability of gestational weight gain reported postpartum: a comparison to the birth certificate. Maternal Child Health Journal, 17(4), 756–765. doi: 10.1007/s10995-012-1057-0 [DOI] [PubMed] [Google Scholar]
- Lavange LM, Kalsbeek WD, Sorlie PD, Aviles-Santa LM, Kaplan RC, Barnhart J,. Elder JP (2010). Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Annals of Epidemiology, 20(8), 642–649. doi: 10.1016/j.annepidem.2010.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: a self-report depression scale for research in the general population Applied Psychological Measurement 1(33), 385–401. [Google Scholar]
- Macdorman MF, & Mathews TJ (2008). Recent trends in infant mortality in the United States. NCHS Data Brief(9), 1–8. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19389323 [PubMed]
- Institute of Medicine. (2009). Weight gain during pregnancy: reexamining the guidelines. Washington, DC [PubMed]
- Moore Simas TA, Doyle Curiale DK, Hardy J, Jackson S, Zhang Y, & Liao X (2010). Efforts needed to provide Institute of Medicine-recommended guidelines for gestational weight gain. Obstetrics and Gynecology, 115(4), 777–783. doi: 10.1097/AOG.0b013e3181d56e12 [DOI] [PubMed] [Google Scholar]
- Sangi-Haghpeykar H, Lam K, & Raine SP (2014). Gestational weight gain among Hispanic women. Maternal Child Health Journal, 18(1), 153–160. doi: 10.1007/s10995-013-1248-3 [DOI] [PubMed] [Google Scholar]
- Savitz DA, Stein CR, Siega-Riz AM, & Herring AH (2011). Gestational weight gain and birth outcome in relation to prepregnancy body mass index and ethnicity. Annals of Epidemiology, 21(2), 78–85. doi: 10.1016/j.annepidem.2010.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services. (2008). 2008 Physical activity guidelines for americans. Washington, D.C.: Availble at : https://health.gov/our-work/physical-activity/previous-guidelines/2008-physical-activity-guidelines
- Siega-Riz AM, & Hobel CJ (1997). Predictors of poor maternal weight gain from baseline anthropometric, psychosocial, and demographic information in a Hispanic population. Journal of the American Dietetic Association, 97(11), 1264–1268. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=9366864 [DOI] [PubMed] [Google Scholar]
- Siega-Riz AM, Sotres-Alvarez D, Ayala GX, Ginsberg M, Himes JH, Liu K, . . . Van Horn L (2014). Food-group and nutrient-density intakes by Hispanic and Latino backgrounds in the Hispanic Community Health Study/Study of Latinos. American Journal of Clinical Nutrition, 99(6), 1487–1498. doi: 10.3945/ajcn.113.082685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C GR, Lushene R, et al. (1983). Manual for the State-Trait Anxiety Inventory (STAI) Palo Alto, CA: Consulting Psychologists Press [Google Scholar]
- Tovar A, Must A, Bermudez OI, Hyatt RR, & Chasan-Taber L (2009). The impact of gestational weight gain and diet on abnormal glucose tolerance during pregnancy in Hispanic women. Maternal and Child Health Journal, 13(4), 520–530. doi: 10.1007/s10995-008-0381-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker LO, Hoke MM, & Brown A (2009). Risk factors for excessive or inadequate gestational weight gain among Hispanic women in a U.S.-Mexico border state. Journal of Obstetrics, Gynecologic, & Neonatal Nursing, 38(4), 418–429. doi:S0884–2175(15)30198–2 [pii] 10.1111/j.1552-6909.2009.01036.x [DOI] [PubMed] [Google Scholar]


