Objective:
This study aims to examine the indications, techniques, and outcomes of choledochoscopy during laparoscopic bile duct exploration and evaluate the results of the wiper blade maneuver (WBM) for transcystic intrahepatic choledochoscopy.
Summary of Background Data:
Choledochoscopy has traditionally been integral to bile duct explorations. However, laparoscopic era studies have reported wide variations in choledochoscopy availability and use, particularly with the increasing role of transcystic exploration.
Methods:
The indications, techniques, and operative and postoperative data on choledochoscopy collected prospectively during transcystic and choledo- chotomy explorations were analyzed. The success rates of the WBM were evaluated for the 3 mm and 5 mm choledochoscopes.
Results:
Of 935 choledochoscopies, 4 were performed during laparoscopic cholecystectomies and 931 during 1320 bile duct explorations (70.5%); 486 transcystic choledochoscopies (52%) and 445 through choledochotomies (48%). Transcystic choledochoscopy was utilized more often than blind exploration (55.7%% vs 44.3%) in patients with emergency admissions, jaundice, dilated bile ducts on preoperative imaging, wide cystic ducts, and large, numerous or impacted bile duct stones. Intrahepatic choledochoscopy was successful in 70% using the 3 mm scope and 81% with the 5 mm scope. Choledochoscopy was necessary in all 124 explorations for impacted stones. Twenty retained stones (2.1%) were encountered but no choledochoscopy related complications.
Conclusions:
Choledochoscopy should always be performed during a chol- edochotomy, particularly with multiple and intrahepatic stones, reducing the incidence of retained stones. Transcystic choledochoscopy was utilized in over 50% of explorations, increasing their rate of success. When attempted, the transcystic WBM achieves intrahepatic access in 70%-80%. It should be part of the training curriculum.
Keywords: basket in catheter technique, bile duct exploration, choledochoscopy, choledochotomy, complications, laparoscopic cholecystectomy, transcystic, wiper blade maneuver
Laparoscopic common bile duct exploration (LCBDE) is increasingly recognized as the preferred method of bile duct clearance during laparoscopic cholecystectomy (LC) where the expertise and equipment exist.1,2 Although training courses and programs enable more surgeons to perform bile duct explorations, the availability of facilities for intraoperative cholangiography (IOC) and specialized instruments, such as the choledochoscope, remain an obstacle in many units. Many studies suggest that blind basket trawling can achieve duct clearance in a significant percentage of patients. We demonstrated that 31% of patients with abnormal IOC had transystic clearance of stones using blind basket trawling or their cholangiographic abnormalities resolved using glucagon administration and duct flushing.3 Some studies reported exceptionally high success rates using this approach. Czerwonko et al4 attempted 500 transcystic explorations (TCEs), completing 469 (93.8%) without choledochoscopy.
The primary aim of this study was to analyze the indications, frequency, and success rates of choledochoscopy in a large single surgeon series of LCBDEs. The secondary aims were to evaluate criteria suggestive of successfully using choledochoscopic TCE over blind basket trawling, to compare TCE choledochoscopy and CBDE choledochoscopy, to evaluate our wiper blade maneuver (WBM) for transcystic intrahepatic choledochoscopy and to describe techniques for optimizing stone extraction and avoiding stone impaction, retained stones and damage to the instrument.
Methods
We reviewed prospectively collected data from 1320 bile duct explorations performed by a single surgeon (AHMN) over 28 years. The transition from open to LC preserved the traditional single session management of all fit patients with common bile duct stones (CBDS); performing routine IOC and when necessary LCBDE. The surgeon had already acquired wide choledochoscopy experience during open ductal explorations. The biliary service received most biliary emergencies including all patients with suspected CBDS from all departments, and 17% were transferred from or performed at other hospitals.5 Patient demographics, type of admission, clinical presentation, preoperative investigations, operative details, postoperative complications, and follow-up were stored on a Microsoft Access database. Data analysis was conducted with emphasis on LCBDEs utilizing choledochoscopy.
Informed consent was obtained from all patients, emphasizing the specialization of the unit in single session management of CBDS. Institutional review board approval was not required as the management protocols were consistent with the recommendations of national and international societies.
Techniques
All patients undergoing elective or urgent LC had a 4-port approach in the American position with 1 infraumbilical 10–12 mm port inserted by modified open access and three 5-mm ports; midline epigastric, right subcostal in the midclavicular line, and right flank in the anterior axillary line. The subcostal port is inserted in line with the longitudinal axis of the cystic duct (CD) to facilitate inserting the cholangiography catheter and, if necessary, the choledochoscope. We have previously described our cholangiography technique.6 Once stones were confirmed the surgeon proceeded to LCBDE, initially utilizing the transcystic approach unless the number or size of stones, CD diameter, or its anatomy indicated a choledochotomy.
TCE was initially performed using blind basket trawling. The first author later introduced the ‘‘basket in catheter’’ technique7 (Supplemental Media 1, http://links.lww.com/SLA/D100. Failure to retrieve stones after 3 attempts indicated choledochoscopy. IOC may indicate mandatory choledochoscopy where blind exploration could result in intramural CD stone impaction (Supplemental Data File 1, http://links.lww.com/SLA/D94). A choledochoscope (most TCEs are carried out using a 3 mm Choledocho-Fiberscope, Karl Storz, Tuttlingen, Germany) is inserted within a guide tube (Karl Storz) via the right subcostal port. The guide reduces scope looping, helps to direct and stabilize it, and prevents its damage. A 5 mm scope is inserted directly through the disposable 5 mm port.
Choledochoscope orientation and movements are checked after introduction before manipulation into the CD/CBD without trying to push it using graspers as this may crush the instrument. The scope should be kept straight as bending it at weak points causes damage or obstruction to the advancement of baskets. It should not be flexed onto the tip of its introducer or the access cannula and should be withdrawn completely into its introducer under vision before removal. Care must be taken during handling, placement onto instrument trays, and during storing or sterilizing the scopes.
The tip of the scope is inserted into the CD opening, initially pushing against the posterior wall before flexing it anteriorly to lift the CD anterior wall and advancing it in small ‘‘snake-like’’ movements of the tip of the scope with low irrigation until it enters the CBD (Supplemental Media 2, http://links.lww.com/SLA/D101). It is advantageous to advance the 5 mm port cannula towards the CD, reducing scope looping and facilitating its progress into the CBD. Advancing the choledochoscope through the CD may occasionally need to be done under vision to negotiate CD valves and reach the CD/CBD junction
Once in the CBD it is important to maintain low irrigation to prevent proximal stone migration. A suitable basket is introduced through the scope channel and stones are engaged. The choledocho- scope is then withdrawn keeping the stone under vision a short distance from the tip. This keeps the CBD lumen in view to avoid missing other stones and avoids scope damage. The process is repeated until the CBD is clear. Large, difficult to deliver, stones can be pulled into the CD stump, crushed with curved dissectors, and retrieved in fragments. Alternatively, a longitudinal incision is made on the CD towards the CBD, not reaching the junction, to help stone extraction. Stones that are too hard to crush or too large to deliver are pushed back into the CBD and other measures are used for fragmentation, for example, laser lithotripsy.
A 5-mm choledochoscope is used if the CD was wide enough. When difficulty is encountered a 5 Fr cholangiography catheter may be inserted into the choledochoscope channel, passed under vision into the intramural CD, and used as a guide over which the chol- edochoscope is advanced.
‘‘Intrahepatic choledochoscopy may be necessary to confirm clearance or to capture stones that are not floating or are too numerous to manipulate into the distal CBD. The WBM8 is attempted to deflect the choledochscope into the proximal ducts and requires favorable anatomy of the CD/CBD junction and moderate dilatation of the CBD, easily assessed on the IOC. With the choledochoscope visualizing the lower CBD it is withdrawn gradually and, at the same time, the tip is deflected towards the anterior wall. The scope is rotated anticlockwise until the light at its tip is visible through the anterior CBD wall. The head of the scope is then rotated 180 degrees in the same direction while firmly holding the lever in position, maintaining the tip in flexion. The tip of the introducer is then moved below the CD opening directing the scope towards the common hepatic duct and, at the same time, straightening the tip and advancing the scope into the duct. A slight anticlockwise rotation will usually allow the scope into the right hepatic duct. The right duct system is inspected, advancing then withdrawing the scope from smaller ducts. The scope is again withdrawn to the confluence of the right and left hepatic ducts (which can be confirmed on seeing the light at the tip on the laparoscopic view or visualizing the lumen of the left hepatic duct). A slight clockwise rotation will allow the scope to advance into the left duct system with selective duct by duct inspection facilitated by subtle inward/outward movements and tip deflection (Supplemental Media 3, http://links.lww.com/SLA/D102). The WBM can occasionally be performed using only the choledochscopic view, subject to favorable anatomy. The scope is withdrawn until the junction of the CD/CBD is visible. The same moves are then performed to deflect the tip of the scope into the common hepatic duct. A reverse WBM is used on rare occasions when the default direction of the scope upon entering the CD is towards the intrahepatic ducts.’’
Choledochoscopy confirms clearance, visualizes difficult large or impacted stones, and helps to retrieve intrahepatic stones, It is also essential if transcystic removal of stents is required, saving occasional choledochotomies (as stents can prevent stone extraction via TCE) or later endoscopic removal (Supplemental Data File 2, http://links.lww.com/SLA/D95).
Before concluding CBD inspection a half open basket may be passed through the ampulla under vision to exclude impacted ampullary stones. Choledochoscope passage into the duodenum is occasionally possible and may be used to transfer engaged stones to the duodenum rather than attempting transcystic extraction (Supplemental Media 4, http://links.lww.com/SLA/D103). This is particularly useful in patients who had a previous sphincterotomy and it avoids negotiating stone removal from the CD.
Following choledochotomy exploration the 5 mm choledocho- scope is used to inspect the opening of the intramural CD into the CBD while passing a cholangiography catheter, a basket or a 3 mm choledochoscope (Fig. 1) transcystically through the subcostal port. This will occasionally extract CD stump or intramural stones that may have migrated during the exploration (Supplemental Media 5, http://links.lww.com/SLA/D104). This may also be done by passing the scope retrogradely from the CBD into the CD (subject to favorable anatomical configuration) to inspect the CD lumen, allowing the irrigation fluid, a catheter or a basket to emerge from its opening under laparoscopic vision, confirming clearance (Supplemental Media 6, http://links.lww.com/SLA/D105).
Figure 1.
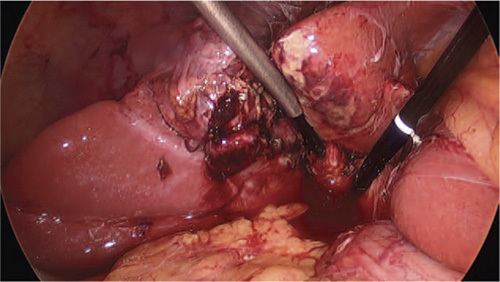
The opening of the CD into the CBD is inspected with a 5 mm choledochsocpe through the choledochotomy while a 3 mm scope is passed into the CD to exclude intramural stones. CBD indicates common bile duct;CD, cystic duct. the scope retrogradely from the CBD into the CD (subject to favorable anatomical configuration) to inspect the CD lumen, allowing the irrigation fluid, a catheter or a basket to emerge from its opening under laparoscopic vision, confirming clearance (Supplemental Media 6, http://links.lww.com/SLA/D105).
A final passage of the choledochoscope is recommended should completion cholangiography be equivocal.
Should the surgeon choose to place a transcystic biliary drain the choledochoscope is used to check the position of the tip of the tube, ensuring it remains above the ampulla rather than pass into the duodenum. Although transcystic biliary drainage is our preferred method we have used T-tubes, primary closure, and internal stenting, subject to case by case selection. The vertical choledochotomy is closed using interrupted 3/0 Vicryl on ski needles. Should a T-tube be used the sutures are placed above it. A subhepatic drain will always be inserted when a choledochotomy has been performed.
Statistical analysis
Qualitative data were given as frequency and percentages. Pearson uncorrected Chi-Square test was calculated in Statpages to calculate P-value and odds ratio with 95% confidence interval. P-value of <0.05 was considered to be statistically significant.
Results
A total of 1320 LCBDEs were performed between 1992 and 2020; 872 (66%) TCEs, and 448 (34%) via choledochotomy.
Of 935 choledochoscopies performed over this period, 931 (70.5%) were done during bile duct explorations including 486 TCE and 445 choledochotomies. Four choledochoscopies were performed during LCs but not recorded as ductal exploration as they had no bile duct stones. Two had impacted CD stones, 1 a CD/CBD junction stricture and 1 a failed IOC.
Sixty-four percent were female, the mean age was 63 years (range 8–91) and 80% were emergency admissions. The admission diagnosis was obstructive jaundice with or without cholangitis in 565 patients (60.6%), acute biliary pain in 136 (14.5%), pancreatitis in 94 (10%), and acute cholecystitis in 51 (5.4%). Ultrasound scanning showed multiple gallbladder stones in 788 (84%) and dilated bile ducts in 563 (60%). Preoperative magnetic resonance cholangiopancreatography was done in 189 patients (20.2%) and endoscopic retrograde cholangiopancreatography (ERCP) in 96 (10.2%). Eight hundred thirty-three patients (89%) were, therefore, suspected of having CBDS.
Transcystic Choledochoscopy Versus Blind Basket Exploration
TCE was carried out in 872 patients, choledochoscopy being used in 486 (55.7%). These were more likely to be emergency admissions with obstructive jaundice or acute biliary pain whose ultrasound scans (and, if carried out, magnetic resonance cholangiopancreatography) showed dilated bile ducts. There were significantly more patients with risk factors for CBDS in this group than in patients whose explorations were performed using the basket alone technique. Blind basket explorations (44.3%) were more common in females, elective admissions, or with chronic biliary colic (Table 1).
Table 1.
Preoperative Characteristics Associated With Using Choledochoscopy Versus Blind Basket Transcystic Exploration
| Characteristics | Choledochoscopy (n = 486) | Blind Basket (n = 386) | P-value | OR (95% CI) |
|---|---|---|---|---|
| Median age (range) | 57 (8–89) yr | 55 (16–90) yr | <0.001 | |
| Female sex | 298 (61.3%) | 283 (73.3%) | <0.001 | 0.577 (0.432, 0.771) |
| Emergency admission | 392 (80.7%) | 243 (63.0%) | <0.001 | 2.454 (1.808, 3.331) |
| Admission diagnosis | ||||
| Jaundice | 259 (53.3%) | 119 (30.8%) | <0.001 | 2.560 (1.935, 3.387) |
| Acute pain | 302 (62.1%) | 181 (46.9%) | <0.001 | 1.859 (1.417, 2.438) |
| Chronic biliary pain | 102 (21.0%) | 138 (35.8%) | <0.001 | 0.477 (0.353, 0.645) |
| Cholangitis | 42 (8.6%) | 10 (2.6%) | <0.001 | 3.557 (1.761, 7.185) |
| Acute Pancreatitis | 72 (14.8%) | 48 (12.4%) | 0.311 | 1.225 (0.827, 1.813) |
| Acute Cholecystitis | 35 (7.2%) | 39 (10.1%) | 0.127 | 0.690 (0.428, 1.113) |
| Ultrasound scan | ||||
| Multiple stones | 423 (87.0%) | 367 (95.1%) | <0.001 | 0.348 (0.204, 0.592) |
| Contracted/thick GB | 94 (19.3%) | 62 (16.1%) | 0.209 | 1.253 (0.881, 1.783) |
| Dilated CBD | 243 (50.0%) | 94 (24.4%) | <0.001 | 3.106 (2.318, 4.162) |
| MRCP | 97 (20.0%) | 28 (7.3%) | <0.001 | 3.188 (2.045, 4.972) |
| CT scan | 57 (11.7%) | 21 (5.4%) | 0.001 | 2.309 (1.374, 3.882) |
| ERCP | 24 (4.9%) | 9 (2.3%) | 0.045 | 2.176 (0.999, 4.738) |
| CBD stone Risk | 416 (85.6%) | 242 (62.7%) | <0.001 | 3.536 (2.551, 4.902) |
Data in parentheses are 95% confidence intervals.
CBD indicates common bile duct; CT, computerized tomography; ERCP, endoscopic retrograde cholangiopancreatography; GB, gallbladder; MRCP, magnetic resonance cholangiopancreatography.
A comparison between the operative data and postoperative outcomes in choledochoscopic versus blind TCE is shown in Table 2. The operative difficulty grade, a wide CD, and the need for biliary drainage were all significantly higher in patients requiring choledochoscopy. All impacted stones occurred in the choledochoscopy group reflecting the fact that disimpaction or fragmentation always needed to be carried out under vision.
Table 2.
Operative and Postoperative Data of Transcystic Exploration Using Choledochoscopy Versus Blind Basket Exploration
| Characteristics | Choledochoscopy (n = 486) | Blind Basket (n = 386) | P-value | OR (95% CI) |
|---|---|---|---|---|
| Difficulty grading | ||||
| I | 76 (15.6%) | 96 (24.9%) | 0.001 | 0.560 (0.400, 0.784) |
| II | 131 (27.0%) | 127 (32.9%) | 0.056 | 0.753 (0.562, 1.008) |
| III | 151 (31.1%) | 97 (25.1%) | 0.053 | 1.343 (0.995, 1.812) |
| IV | 104 (21.4%) | 60 (15.5%) | 0.028 | 1.479 (1.042, 2.100) |
| V | 24 (4.9%) | 6 (1.6%) | 0.006 | 3.290 (1.331, 8.131) |
| Wide cystic duct | 205 (42.2%) | 88 (22.8%) | <0.001 | 2.450 (1.8181, 3.301) |
| Cystic duct stones | 155 (31.9%) | 141 (36.5%) | 0.151 | 0.814 (0.614, 1.078) |
| Number of CBD stone | 2 (1–50) | 2 (1–30) | <0.001 | |
| Size of CBD stone | 8 (2–22) mm | 6 (3–15) mm | <0.001 | |
| Impacted CBD stone | 43 (8.8%) | 0 | <0.001 | |
| Use of glucagon | 248 (51.0%) | 252 (65.3%) | <0.001 | 0.554 (0.421, 0.729) |
| operative time (mins) | 95 (42–285) | 75 (40–@265) | 0.965 | 1.008 (0.719, 1.412) |
| Transcystic biliary drain | 91 (18.7%) | 38 (9.8%) | <0.001 | 2.110 (1.407, 3.163) |
| Open Conversions | 1 (0.2%) | 2 (0.5%) | 0.434 | 0.396 (0.036, 4.382) |
| Retained stones | 5 (1.0%) | 6 (1.6%) | 0.490 | 0.658 (0.199, 2.174) |
| Complications | 48 (9.9%) | 40 (10.4%) | 0.813 | 0.948 (0.609, 1.476) |
| Reoperation | 2 (0.4%) | 1 (0.3%) | 0.703 | 1.591 (0.144, 17.610) |
| Readmissions | 25 (5.1%) | 23 (6.0%) | 0.600 | 0.856 (0.478, 1.533) |
| Number of episodes | 1 (1–5) | 1 (1–4) | 0.129 | |
| Total hospital stay | 6 (1–160) d | 5 (1–49) d | <0.001 | |
| Presentation to resolution interval | 1 (1–112) wk | 1 (1–72) wk | 0.515 |
Data in parentheses are 95% confidence intervals.
CBD indicates common bile duct.
When transcystic choledochoscopy was performed the 3 mm choledochoscope was used in 381 patients (78.4%) and the 5 mm scope in 105 (21.6%). However, the 5-mm scope was preferred if the CD was wide enough. Only distal choledochoscopy was necessary in 201 patients with few lower CBD stones, completion cholangiography showing no indication for intrahepatic inspection. Intrahepatic choledochoscopy using the WBM was attempted in 285/486 (58.6%) of TCEs and was successful in 207 (72.6%). When attempted with the 5 mm scope the WBM was achieved in a higher percentage (52/ 64, 81%) than with the 3 mm scope (155/221, 70%) (Table 3).
Table 3.
Patients Undergoing Transcystic Choledochoscopy. Rates of Attempted and Successful WBM Using 3 mm Versus 5 mm Scopes
| Choledochoscope | 3 mm scope (n = 381) | 5 mm scope (n = 105) | P-value | OR (95% CI) |
|---|---|---|---|---|
| CBD only - intrahepatic NOT indicated | 160 (42.0%) | 41 (39.0%) | 0.587 | 1.130 (0.727, 1.758) |
| Intrahepatic attempted | 221 (58.0%) | 64 (61.0%) | 0.587 | 0.885 (0.569, 1.376) |
| Intrahepatic successful WBM | 155 (70.1%) | 52 (81.3%) | 0.079 | 0.542 (0.272, 1.081) |
Data in parentheses are 95% confidence intervals.
CBD indicates common bile duct.
Transcystic Choledochoscopy Versus Transcholedochal Choledochoscopy
A 5 mm choledochoscope was used in 445 transcholedochal explorations. The median age, sex, and type of admission of those patients were the same as those undergoing transcystic choledochoscopy. The clinical presentations, radiological investigations, and CBD stone risk are shown in Table 4. Choledochoscopy facilitated the extraction of stones and the insertion of transcystic biliary drains in 167 patients and stents on 16 occasions where internal drainage was indicated. The removal of stents that may have been left during a preoperative ERCP usually required a choledochotomy. However, in this series transcystic removal of biliary stents was achieved in 6 cases under choledochoscopic control, visualizing the upper end of the stent and engaging it with a basket.
Table 4.
Preoperative Characteristics Predictive of Utilizing Transcholedocal Versus Transcystic Choledochoscopy
| Characteristics | Transcystic Choledochoscopy (n = 486*) | Transcholedocal Choledochoscopy (n = 445) | P-value | OR (95% CI) |
|---|---|---|---|---|
| Median age (range) | 57 (8–89) yr | 73 (17–91) yr | <0.001 | |
| Female sex | 298 (61.3%) | 297 (66.7%) | 0.085 | 0.790 (0.604, 1.033) |
| Emergency admission | 392 (80.7%) | 356 (80.0%) | 0.801 | 1.043 (0.754, 1.441) |
| Admission diagnosis | ||||
| Jaundice | 259 (53.3%) | 293 (65.8%) | <0.001 | 0.592 (0.454, 0.771) |
| Acute pain | 302 (62.1%) | 246 (55.3%) | 0.034 | 1.328 (1.022, 1.725) |
| Chronic biliary pain | 102 (21.0%) | 112 (25.2%) | 0.130 | 0.790 (0.582, 1.072) |
| Cholangitis | 42 (8.6%) | 60 (13.5%) | 0.018 | 0.607 (0.400, 0.921) |
| Acute pancreatitis | 72 (14.8%) | 22 (4.9%) | <0.001 | 3.344 (2.036, 5.493) |
| Acute cholecystitis | 35 (7.2%) | 16 (3.6%) | 0.016 | 2.081 (1.135, 3.815) |
| Ultrasound scan | ||||
| Multiple stones | 423 (87.0%) | 361 (81.1%) | 0.013 | 1.562 (1.095, 2.229) |
| Contracted/Thick GB | 94 (19.3%) | 69 (15.5%) | 0.124 | 1.307 (0.929, 1.838) |
| Dilated CBD | 243 (50.0%) | 320 (71.9%) | <0.001 | 0.391 (0.297, 0.513) |
| MRCP | 97 (20.0%) | 92 (20.7%) | 0.786 | 0.957 (0.695, 1.317) |
| CT scan | 57 (11.7%) | 42 (9.4%) | 0.258 | 1.275 (0.837, 1.943) |
| ERCP | 24 (4.9%) | 73 (16.4%) | <0.001 | 0.265 (0.164, 0.428) |
| CBD stone risk | 416 (85.6%) | 415 (93.3%) | <0.001 | 0.430 (0.274, 0.673) |
Data in parentheses are 95% confidence intervals.
Four more transcystic choledochoscopies were not recorded as duct explorations.
CBD indicates common bile duct; CBDE, common bile duct exploration; CT, computerized tomography; ERCP, endoscopic retrograde cholangiopancreatography; GB, gallbladder; MRCP, magnetic resonance cholangiopancreatography; TC, transcystic.
The operative and postoperative characteristics of transcystic and transcholedochal choledochoscopy showed significantly more LC difficulty grades IV, CD stones, impacted CBD stones, and biliary drains in the choledochotomy group. As would be expected the utilization of biliary drains, open conversions, morbidity, and reoperations were also significantly higher (Table 5). However, such parameters were unrelated to the use of choledochoscopy.
Table 5.
Operative and Postoperative Data of Transcystic Versus Transcholedocal Choledochoscopy
| Transcystic Choledochoscopy | Transcholedocal Choledochoscopy | |||
|---|---|---|---|---|
| Characteristics | (n = 486*) | (n = 445) | P-value | OR (95% CI) |
| Cholecystectomy difficulty grading | ||||
| I | 76 (15.6%) | 43 (9.7%) | 0.006 | 1.733 (1.163, 2.581) |
| II | 131 (27.0%) | 112 (25.2%) | 0.535 | 1.097 (0.818, 1.471) |
| III | 151 (31.1%) | 115 (25.8%) | 0.078 | 1.293 (0.971, 1.722) |
| IV | 104 (21.4%) | 148 (33.3%) | <0.001 | 0.546 (0.408, 0.732) |
| V | 24 (4.9%) | 27 (6.1%) | 0.449 | 0.804 (0.457, 1.416) |
| Wide cystic duct | 205 (42.2%) | 175 (39.3%) | 0.376 | 1.126 (0.866, 1.463) |
| Cystic duct stones | 155 (31.9%) | 102 (22.9%) | 0.002 | 1.575 (1.176, 2.109) |
| Number of CBD stone | 2 (1–50) | 5 (1–100) | <0.001 | |
| Size of largest CBD stone | 8 (2–22) mm | 15 (2–30) mm | <0.001 | |
| Impacted CBD stone | 43 (8.8%) | 81 (18.2%) | <0.001 | 0.436 (0.294, 0.647) |
| Use of glucagon | 248 (51.0%) | 97 (21.8%) | <0.001 | 3.738 (2.806, 4.980) |
| operative time (mins) | 95 (42–285) | 170 (55–630) | <0.001 | |
| Transcystic biliary drain | 91 (18.7%) | 167 (37.5%) | <0.001 | 0.384 (0.285, 0.517) |
| T-tubes | 5 (1.0%) | 218 (49.0%) | <0.001 | 0.011 (0.004, 0.027) |
| Open conversions | 1 (0.2%) | 13 (2.9%) | 0.001 | 0.069 (0.009, 0.526) |
| Retained stones | 5 (1.0%) | 15 (3.4%) | 0.014 | 0.298 (0.107, 0.827) |
| Complications | 48 (9.9%) | 106 (23.8%) | <0.001 | 0.350 (0.242, 0.507) |
| Reoperation | 2 (0.4%) | 11 (2.5%) | 0.007 | 0.163 (0.036, 0.740) |
| Readmissions | 25 (5.1%) | 74 (16.6%) | <0.001 | 0.272 (0.169, 0.437) |
| Mortality | 0 | 3 (0.7%) | 0.070 | |
| Number of episodes | 1 (1–5) | 2 (1–8) | <0.001 | |
| Total hospital stay | 6 (1–160) d | 14 (2–93) d | <0.001 | |
| Presentation to resolution interval | 1 (1–112) wk | 4 (1–72) wk | 0.009 |
Data in parentheses are 95% confidence intervals.
Four more transcystic choledochoscopies were not recorded as duct explorations.
CBD indicates common bile duct; CBDE, common bile duct exploration; TC, transcystic.
Choledochoscopy was necessary during 51 of 58 explorations for Mirizzi syndrome; 31 choledochotomies and 20 TCE.9 It was also used in all 124 patients with impacted stones; 81 during choledo- chotomy and 43 during TCE. It facilitated access, dislodgement under vision, and fragmentation using biopsy forceps or laser lithotripsy and only 3 patients in this group had retained stones.
Retained stones occurred in 20 patients (2.1%) who had a choledochoscopic exploration; 15 through choledochotomy and 5 a TCE.
No operative or postoperative complications, open conversions, readmissions, or reinterventions resulted from the use of the choledochoscope.
Discussion
Blind basket exploration was achieved in 44.3% of 872 TCEs in this study. However, large, multiple, or impacted stones rendered blind exploration either time consuming or impossible and subsequently the choledochoscope was used during most TCEs. Case selection for choledochoscopy was determined by a number of factors including the presence of numerous stones, intrahepatic stones, and the need to confirm complete clearance of the bile ducts when postexploration completion cholangiography remained equivocal.
Capagnacci et al10 compared the blind basket technique with choledochoscopy in a randomized trial. Although blind basket exploration achieved stone clearance in 77.5%, choledochoscopy was better in terms of higher stone removal rate and fewer minor complications despite a longer operation time.
Topal et al11 examined 113 LCBDEs in a prospective study comparing fluoroscopically guided stone removal with choledocho- scopic TCE. Choledochoscopy exploration had a shorter operating time but stone clearance and morbidity rates were similar. Their basket technique was used early in their experience and the longer time was probably a reflection of the learning curve rather than evidence that choledochoscopic exploration is faster. As we do not dilate the CD our exploration time is determined by many factors including whether negotiating the CD is difficult, stone fragmentation is necessary or the WBM is attempted. Our own experience is that the TCE operative time is less important than selecting the appropriate technique for the patient. There was no statistical difference in the surgery time between blind basket and choledochoscopsy TCE (Table 2).
TCE Choledochoscopy Technique
The introduction of even the narrow 3 mm scope into the CD may be difficult due to a small duct caliber or the presence of valves. Several authors reported techniques for dilating the CD either with forceps,12,13 balloon dilators14,15 or blunt flexible dilators16 to facilitate choledochoscope insertion. However, CD dilatation is not without problems. Zhang et al16 reported a ruptured CD resulting in open conversion. Carroll et al15 and Al-Habbal17 also reported CD laceration or avulsion resulting in failure. Railroading the scope over a floppy tipped guidewire has also been reported.17,18 Navaratne et al18 used trans-infundibular choledochoscopy when inflammation at the cystic pedicle made it difficult or impossible to access the CD for dilatation. All the above authors described CD dissection towards the lateral wall of the CBD to display a right angled junction. However, there was no mention of CD/CBD configurations, such as a CD entering the medial side of the CBD rendering that dissection impossible or undesirable.
The group of Martinez-Isla, Al-Musawi, and Navaratne18,19,20 described complete separation of the gallbladder from the liver, leaving it attached to the CBD only through the CD. They maintained that this achieves a right angled CD/CBD junction facilitating choledochoscope insertion and proximal access using our WBM.
In our practice, we have not adopted CD dilatation as some configurations of the CD/CBD junction make it impossible to dilate the full length of the duct. Moreover, dilating the intramural part of the CD may be undesirable due to the risk of CBD disruption. When valves or a narrow caliber preclude scope passage our first approach is to perform further dissection and incise the CD closer to the CBD. This allows the 3 mm scope to pass into most CDs. As a medial low CD entry will make the WBM impossible choledochoscopy should be performed without prior attempts at blind trawling to avoid stones moving above the CD/CBD junction and a completion choledochoscopy carried out and used to obtain cholangiography confirming intrahepatic clearance (Supplemental Data File 3, http://links.lww.com/SLA/D96).
Achieving intrahepatic access is a measure of success of chol-edochscopic TCE. In our practice, it was only thought necessary and attempted in 59% of explorations, when initial or completion cholangiography showed intrahepatic stones. It may be clear from the IOC that the WBM would not be successful. A low or medial insertion of the CD would make it physically impossible to angle the scope at multiple points to reflect it upwards and achieve intrahepatic access. Our preliminary report on the WBM8 included 120 transcystic choledochoscopies in which transcystic intrahepatic access was successful in 49 (40.8%). The refinement of the technique and increasing experience have resulted in higher success rates. When indicated and attempted, the WBM was achieved in 81% using the 5 mm scope and 70% with the 3 mm scope, a trend towards significance (P = 0.79). Although the WBM was used in a number of studies19,21,22 the numbers were small and neither the size of choledochoscope nor the success rates were reported.
Choledochotomy
If a choledochotomy is made a choledochoscope should always be used to visualize the CBD. Some stones may simply be squeezed out of the choledochotomy or removed using the conventional methods of irrigation, balloon trawling, or basket retrieval. Others, particularly intrahepatic and impacted stones, will require removal under vision. The exploration should always be concluded with a choledochoscopy. The 5 mm scope is used, being easier to handle and less fragile than the 3 mm scope. The epigastric port is used for scope insertion, giving a better angle of access to both intrahepatic and extrahepatic ducts. Right subcostal port insertion may be preferred for multiple or impacted intrahepatic stones as it allows scope stability while the surgeon attends to positioning, basket manipulation, or laser use. The choledochoscopy mechanics remain as described.
Choledochoscopy and Impacted Stones
It is seldom possible to resolve impacted stones without choledochoscopic control. All methods of disimpaction or fragmentation must be carried out under vision to achieve successful extraction while avoiding injury to the bile ducts. Impacted intra- hepatic stones can be challenging and time consuming due to difficult choledochoscopic access and demanding fragmentation (Supplemental Data File 4, http://links.lww.com/SLA/D97). Open conversion, therefore, will seldom make the procedure any easier and most such patients may have already had multiple failed ERCP attempts. Distal CBD stone impaction is more likely in jaundiced patients in whom the ultrasound scan detects CBD stones. Even small stones can be challenging to remove as they often impact in a pouch which is eccentric to the CBD making it impossible to open a basket around the stone. Fogarty balloons passed through the subcostal port may be used alongside retrieval baskets through the choledochoscope, attempting to evert such a pouch, dislodge a stone, and engage it. This allows 2 instruments to be used simultaneously under vision within the bile duct (Supplemental Media 7, http://links.lww.com/SLA/D106). Early in the series we used biopsy forceps or ultrasound lithotripsy but later used laser to fragment stones (Supplemental Media 8A, B, and C, http://link- s.lww.com/SLA/D107, http://links.lww.com/SLA/D108, http://links.lww.com/SLA/D109). However, the consistency and the size of the stone can make this difficult and time consuming. Laser could be used to fragment and remove impacted intrahepatic stones which are almost impossible to disimpact and remove endoscopically or lower CBD stones which are a risk factor for ERCP complications. Navarro-Sanchez et al23 reported the laser assisted bile duct exploration by laparosendoscopy (LABEL) technique of laser fragmentation in complicated TCE. In another publication from the same group24 TCE was successful in two-thirds of patients and 16.2% required LABEL to achieve transcystic extraction. 7/31 (22.6%) of TCEs failed despite the use of laser. However, the LABEL group had more bile leaks requiring reintervention, longer operative times, and longer postoperative hospital stay. The group’s large percentage of explorations requiring laser is likely due to personal preference and experience as less than 1% of 1320 CBDEs in our series needed laser. Other large studies with high success rates of TCE also reported occasional laser use.4 It is our view, therefore, that routine use of laser can not be recommended on the basis of necessity or safety.
The use of electro-hydraulic lithotripsy to fragment impacted stones has also been reported.19
Special Uses of Choledochoscopy
Transcystic choledochoscopic retrieval of intrahepatic stones using the WBM has been used by the first author since 2002 and described in 2012.8 Once achieved, intrahepatic choledochoscopy should progress from the main ducts to their tributaries in a systematic fashion to avoid missing stones. It is often possible to identify the right hepatic duct and occasionally the left hepatic duct by observing the light at the tip of the choledochoscope through the duct wall on the laparoscopic view (Supplemental Media 9, http://links.lww.com/SLA/D110). This technique will also occasionally identify extrahepatic right hepatic or sectoral ducts, clarifying duct anatomy, avoiding such ducts during difficult gallbladder separation, and checking their integrity afterward.
Choledochoscopic Cholangiography
When insertion or the WBM are difficult to repeat it may be advantageous to confirm intrahepatic duct clearance before removing the choledochoscope. The C-Arm is positioned and contrast is injected through the choledochoscope channel obtaining a dynamic IOC (Fig. 2). The viscosity of the contrast material may allow intrahepatic stones to move down to the CBD. Choledochoscopy could also be used as a alternative to IOC in pregnant patients to avoid using x-rays, in patients who are allergic to contrast media, or when cholangiography is unavailable.
Figure 2.
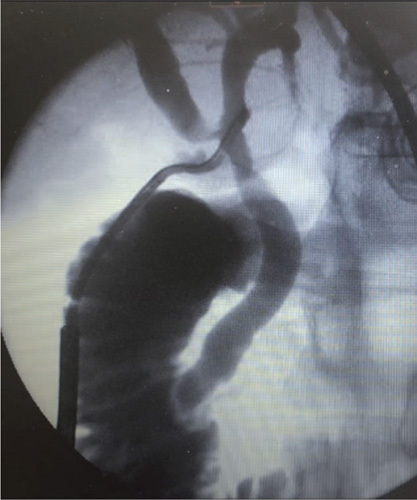
Choalngiography obtained through the choledochoscope channel to view intrahepatic ducts before concluding the WBM.
Choledochoscopic Suction
Recovery of intrahepatic stones or fragments into the CBD may be achieved using irrigation followed by suction to move the stones towards the choledochoscope to engage and remove them. Some stones may be transferred to the duodenum or occasionally crushed and fragmented. Although the 3 mm scope does not have a dedicated suction button or channel we have used a 3-way tap on the irrigation port to provide alternate irrigation and suction.
We have also used the choledochoscope to locate and remove spilled stones. The flexible instrument can reach the space lateral to the liver or the subphrenic space more readily than the laparoscope and facilitates basket stone retrieval (Supplemental Media 10, http://links.lww.com/SLA/D111).
Choledochoscopy Training
Acquiring and refining choledochoscopy skills are essential components of mastering LCBDE. Teitlebaum et al25 used a simulator allowing senior surgery residents to perform specific tasks before proceeding to simulated explorations. A 2 months curriculum of practicing procedural skills improved residents performance to the level of mastery. Resident assessment scores on inserting and manipulating the choledochoscopes improved significantly and were reflected in increased confidence in performing both transcystic and transcholedochal choledochoscopy. However, tissue dissection to simulate exposing and preparing the CBD was not possible on the synthetic model. Li et al26 used a 3D printed biliary tract model as a choledochoscopy training tool. The anatomically realistic model improved trainees ability to manipulate the scope. However, it could not reproduce tissue elasticity and the loss of normal texture affected tactile feedback.
Drissen et al27 designed a synthetic bile duct model which was assessed by experienced surgeons during a choledochoscopy hands- on course (Supplemental Data File 5, http://links.lww.com/SLA/D98). Although the model offered a realistic experience, the internal friction of the artificial CBD was high and the rating of the compliance, tactile characteristics, and color was lower than with animal tissue.
Navarro-Sanchez et al28 used a porcine aorta model concluding that although live animal models provided the most realistic experience they were expensive and raised ethical and regulatory issues. However, their model could not reproduce realistic transcystic choledochoscopy, or simulate intrahepatic duct anatomy or the WBM.
The first author conducted hands-on courses using cow liver models for over 20 years (Supplemental Data File 6A, B, and C, http://links.lww.com/SLA/D99). These provide realistic anatomy and tissue texture. Cholangiography, TCE, choledohotomy and choledochoscopy tasks are reproducible resulting in skills consolidation. Stones of various sizes can be inserted into the ducts to allow realistic stone retrieval practice. When cow livers were not available large sheep, goat or pig livers are used subject to local regulations.
Component Training
Our training protocol is based on consolidation of skills and the optimal use of choledochoscopy through hands-on LCBDE in 1 or 2-day courses. Clinical component training follows, progressing through IOC, TCE, and choledochotomy. Senior trainees are able to perform most LCBDE during their 6-month placements.29
Challenges of the Use, Maintenance, and Sterilization of the Choledochoscope
The sterilization of choledochoscopes usually occurs offsite, with a minimum 48-hour turnaround in the authors’ institutions. Centers performing high volume LCBDEs require a number of scopes in circulation to ensure their continued availability. The Ambu aScope (Ambu, Denmark) bronchoscope has been used as a cholecdoscope.30,31 Although it is not designed for fluid irrigation it is a useful alternative when the standard instruments are not available. Disposable ureteroscopes can be used for inspection but they are too long to allow the use of most available retrieval baskets.
Video choledochoscopes provide higher quality images than fibreoptic scopes and are easier to set up, having an integrated light source. However, they are more expensive to repair.
The SpyGlass Discover choledochoscope (Boston Scientific, Marlborough, MA) at 3.6 mm external diameter, is slightly larger than the fiberoptic scopes available. However, it has the advantage of 2 way tip defection and the ability to lock the scope’s position to facilitate stone capture. It also has separate irrigation and instrument channels, allowing good irrigation pressure when a basket is in use.
Conclusions
Although blind basket trawling is successful in clearing between 30% and 80% of stones during TCE, choledochoscopy is an essential tool for any unit adopting single session laparoscopic treatment of CBDS. Transcystic choledochoscopy is necessary in over half of TCEs and, when indicated, the WBM achieves intra- hepatic choledochoscopy to confirm stone clearance in 70–80%. Choledochoscopy should be routine when a trans-choledochotomy exploration is performed. It is essential for intrahepatic and impacted stone retrieval, reducing the incidence of failed LCBDE and retained stones.
Supplementary Material
Footnotes
Ahmad H.M. Nassar has directed laparoscopic bile duct exploration/choledocho- scopy hands-on courses supported by Karl Storz. There are no formal links or financial ties.
The authors report no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.annalsofsurgery.com.
References
- 1.Internal Clinical Guidelines Team (UK) (2014). National Institute for Health and Care Excellence: Clinical Guidelines. Gallstone Disease: Diagnosis and Management of Cholelithiasis, Cholecystitis and Choledocholithiasis. National Institute for Health and Care Excellence, London. Available at: https://www.nice.org.uk/guidance/cg188/evidence/full-guideline-pdf-193302253. Accessed November 7, 2020. [PubMed] [Google Scholar]
- 2.Overby DW, Apelgren KN, Richardson W, et al. Society of American Gastrointestinal and Endoscopic Surgeons. SAGES guidelines for the clinical application of laparoscopic biliary tract surgery. Surg Endosc. 2010;24:2368–2386. [DOI] [PubMed] [Google Scholar]
- 3.Hamouda AH, Khan M, Nassar AH. Intraoperative cholangiography facilitates simple transcystic clearance of ductal stones in units without expertise for laparoscopic bile duct surgery. Surg Endosc. 2007;21:955–959. [DOI] [PubMed] [Google Scholar]
- 4.Czerwonko ME, Pekolj J, Uad P, et al. Laparoscopic transcystic common bile duct exploration in the emergency is as effective and safe as in elective setting. J Gastrointest Surg. 2019;23:1848–1855. [DOI] [PubMed] [Google Scholar]
- 5.Nassar AHM, Ng HJ, Ahmed Z, et al. Optimising the outcomes of index admission laparoscopic cholecystectomy and bile duct exploration for biliary emergencies: a service model. Surg Endosc. 2021;35:4192–4199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nassar AHM, Shallaly G, Hamouda A. Optimising laparoscopic cholangiography time using a simple cannulation technique. Surg Endosc. 2009;23:513–517. [DOI] [PubMed] [Google Scholar]
- 7.Qandeel H, Zino S, Hanif Z, et al. Basket-in-catheter access for transcystic laparoscopic bile duct exploration: technique and results. Surg Endosc. 2016;30:1958–1964. [DOI] [PubMed] [Google Scholar]
- 8.Gough V, Stephens N, Ahmed Z, et al. Intrahepatic choledochoscopy during trans-cystic common bile duct exploration; technique, feasibility and value. Surg Endosc. 2012;26:3190–3194. [DOI] [PubMed] [Google Scholar]
- 9.Nassar AHM, Nassar MK, Gil IC, et al. One-session laparoscopic management of Mirizzi syndrome: feasible and safe in specialist units. Surg Endosc. 2021;35:3286–3295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campagnacci R, Baldoni A, Baldarelli M, et al. Is laparoscopic fiberoptic choledochoscopy for common bile duct stones a fine option or a mandatory step? Surg Endosc. 2010;24:547–553. [DOI] [PubMed] [Google Scholar]
- 11.Topal B, Aerts R, Penninckx F. Laparoscopic common bile duct stone clearance with flexible choledochoscopy. Surg Endosc. 2007;21:2317–2321. [DOI] [PubMed] [Google Scholar]
- 12.Zhu JG, Han W, Guo W, et al. Learning curve and outcome of laparoscopic transcystic common bile duct exploration for choledocholithiasis. Br J Surg. 2015;102:1691–1697. [DOI] [PubMed] [Google Scholar]
- 13.Matsumura T, Komatsu S, Komaya K, et al. Dual common bile duct examination with transcystic choledochoscopy and cholangiography in laparoscopic cholecystectomy for suspected choledocholithiasis: a prospective study. Surg Endosc. 2021;35:3379–3386. [DOI] [PubMed] [Google Scholar]
- 14.Tokumura H, Umezawa A, Cao H, et al. Laparoscopic management of common bile duct stones: transcystic approach and choledochotomy. J Hepatobiliary Pancreat Surg. 2002;9:206–212. [DOI] [PubMed] [Google Scholar]
- 15.Carroll BJ, Fallas MJ, Phillips EH. Laparoscopic transcystic choledochoscopy. Surg Endosc. 1994;8:310–314. [DOI] [PubMed] [Google Scholar]
- 16.Zhang WJ, Xu GF, Huang Q, et al. Treatment of gallbladder stone with common bile duct stones in the laparoscopic era. BMC Surg. 2015;15:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Habbal Y, Reid I, Tiang T, et al. Retrospective comparative analysis of choledochoscopic bile duct exploration versus ERCP for bile duct stones. Sci Rep. 2020;10:14736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Navaratne L, Al-Musawi J, Mérida AA, et al. Trans-infundibular choledochoscopy: a method for accessing the common bile duct in complex cases. Langenbecks Arch Surg. 2018;403:777–783. [DOI] [PubMed] [Google Scholar]
- 19.Al-Musawi J, Navaratne L, Martinez-Isla A. Laparoscopic common bile duct exploration versus endoscopic retrograde cholangiopancreatography for chol- edocholethiasis found at the time of laparoscopic cholecystectomy. Am J Surg. 2019;217:188–189. [DOI] [PubMed] [Google Scholar]
- 20.Martinez-Isla A, Navaratne L, Quinones Sampedro J, et al. Efficacy of fibrincollagen sealant for reducing the incidence of biliary fistulae after laparoscopic exploration of the bile duct. Cir Esp. 2019;97:119–120. [DOI] [PubMed] [Google Scholar]
- 21.ElGhamry EE, ElSheikh M, Abdelhady H, et al. An auspicious experience with laparoscopic common bile duct exploration. Eg J Surg. 2019;38:459–470. [Google Scholar]
- 22.Elghamry EE, ElSkeikh MM, Mohamed HA. Evaluation of different methods of laparoscopic treatment of common bile duct stones. Int Surg J. 2019;6:2670–2676. [Google Scholar]
- 23.Navarro-Sanchez A, Ashrafian H, Segura-Sampedro JJ, et al. LABEL procedure: laser-assisted bile duct exploration by laparoendoscopy for choledo- cholithiasis: improving surgical outcomes and reducing technical failure. Surg Endosc. 2017;31:2103–2108. [DOI] [PubMed] [Google Scholar]
- 24.Jones T, Al Musawi J, Navaratne L, et al. Holmium laser lithotripsy improves the rate of successful transcystic laparoscopic common bile duct exploration. Langenbecks Arch Surg. 2019;404:985–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Teitelbaum EN, Soper NJ, Santos BF, et al. A simulator-based resident curriculum for laparoscopic common bile duct exploration. Surgery. 2014;156:880–890. [DOI] [PubMed] [Google Scholar]
- 26.Li A, Tang R, Rong Z, et al. The use of three-dimensional printing model in the training of choledochoscopy techniques. World J Surg. 2018;42:4033–4038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Driessen P, 2011. Designing a Realistic Anatomical Model for Training in Laparoscopic Bile Duct Exploration. Master Thesis ‘‘Integrated product design’’ Delft University of technology. Study No 1539469. Available at: https://repository.tudelft.nl/islandora/object/uuid:140b1868-b57c-48e3-84ec-8366a1a9ba34/datastream/OBJ. Accessed December 6, 2020. [Google Scholar]
- 28.Navarro-Sanchez A, von Roon AC, Thomas RL, et al. A new teaching model for laparoscopic common bile duct exploration: use of porcine aorta. Cir Esp. 2014;92:692–693. [DOI] [PubMed] [Google Scholar]
- 29.Jabbar SAA, Ahmed Z, Mirza A, et al. Laparoscopic training opportunities in an emergency biliary service. JSLS. 2019;23:e2019.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aawsaj Y, Light D, Brown J, et al. Use of the Ambu ® aScope 2™ in laparoscopic common bile duct exploration. Surg Endosc. 2016;30:5153–5155. [DOI] [PubMed] [Google Scholar]
- 31.Daniel C, Pereira J, Prudente C, et al. Laparoscopic choledochoscopy with Ambu ® aScope 3TM in the treatment of coledocholithiasis: a series of cases. J Surg Case Rep. 2018;2018:rjy046. [DOI] [PMC free article] [PubMed] [Google Scholar]


