Abstract
Background
Demographic factors have been implicated in THA and TKA outcome disparities. Specifically, patients’ racial backgrounds have been reported to influence outcomes after surgery, including length of stay, discharge disposition, and inpatient readmissions. However, in the United States, health-impacting socioeconomic disadvantage is sometimes associated with racial differences in ways that can result in important confounding, thereby raising the question of whether race-associated post-THA/TKA adverse outcomes are an independent function of race or a byproduct of confounding from socioeconomic deprivation, which is potentially addressable. To explore this, we used the Area Deprivation Index (ADI) as a proxy for socioeconomic disadvantage, since it is a socioeconomic parameter that estimates the likely deprivation associated with a patient’s home address.
Questions/purposes
The goal of this study was to investigate (1) whether race (in this study, Black versus White) was independently associated with adverse outcomes, including prolonged length of stay (LOS > 3 days), nonhome discharge, 90-day readmission, and emergency department (ED) visits while controlling for age, gender, BMI, smoking, Charlson comorbidity index (CCI), and insurance; and (2) whether socioeconomic disadvantage, measured by ADI, substantially mediated any association between race and any of the aforementioned measured outcomes.
Methods
Between November 2018 and December 2019, 2638 underwent elective primary THA and 4915 patients underwent elective primary TKA for osteoarthritis at one of seven hospitals within a single academic center. Overall, 12% (742 of 5948) of patients were Black and 88% (5206 of 5948) were White. We included patients with complete demographic data, ADI data, and who were of Black or White race; with these criteria, 11% (293 of 2638) were excluded in the THA group, and 27% (1312 of 4915) of patients were excluded in the TKA group. In this retrospective, comparative study, patient follow-up was obtained using a longitudinally maintained database, leaving 89% (2345 of 2638) and 73% (3603 of 4915) for analysis in the THA and TKA groups, respectively. For both THA and TKA, Black patients had higher ADI scores, slightly higher BMIs, and were more likely to be current smokers at baseline. Furthermore, within the TKA cohort there was a higher proportion of Black women compared with White women. Multivariable regression analysis was utilized to assess associations between race and LOS of 3 or more days, nonhome discharge disposition, 90-day inpatient readmission, and 90-day ED admission, while adjusting for age, gender, BMI, smoking, CCI, and insurance. This was followed by a mediation analysis that explored whether the association between race (the independent variable) and measured outcomes (the dependent variables) could be partially or completely attributable to confounding from the ADI (the mediator, in this model). The mediation effect was measured as a percentage of the total effect of race on the outcomes of interest that was mediated by ADI.
Results
In the THA group, after adjusting for age, gender, BMI, smoking, CCI, and insurance, White patients had lower odds of experiencing an LOS of 3 days or more (OR 0.43 [95% confidence interval (CI) 0.31 to 0.59]; p < 0.001) and nonhome discharge (OR 0.39 [95% CI 0.27 to 0.56]; p < 0.001). In mediation analysis, ADI partially explained (or mediated) 37% of the association between race and LOS of 3 days or more (-0.043 [95% CI -0.063 to -0.026]; p < 0.001) and 40% of the association between race and nonhome discharge (0.041 [95% CI 0.024 to 0.059]; p < 0.001). However, a smaller direct association between race and both outcomes was observed (LOS 3 days or more: -0.075 [95% CI -0.13 to -0.024]; p = 0.004; nonhome discharge: 0.060 [95% CI 0.016 to 0.11]; p = 0.004). No association was observed between race and 90-day readmission or ED admission in the THA group. In the TKA group, after adjusting for age, gender, BMI, smoking, CCI, and insurance, White patients had lower odds of experiencing an LOS of 3 days or more (OR 0.41 [95% CI 0.32 to 0.54]; p < 0.001), nonhome discharge (OR 0.44 [95% CI 0.33 to 0.60]; p < 0.001), 90-day readmission (OR 0.54 [95% CI 0.39 to 0.77]; p < 0.001), and 90-day ED admission (OR 0.60 [95% CI 0.45 to 0.79]; p < 0.001). In mediation analysis, ADI mediated 19% of the association between race and LOS of 3 days or more (-0.021 [95% CI -0.035 to -0.007]; p = 0.004) and 38% of the association between race and nonhome discharge (0.029 [95% CI -0.016 to 0.040]; p < 0.001), but there was also a direct association between race and these outcomes (LOS 3 days or more: -0.088 [95% CI -0.13 to -0.049]; p < 0.001; nonhome discharge: 0.046 [95% CI 0.014 to 0.078]; p = 0.006). ADI did not mediate the associations observed between race and 90-day readmission and ED admission in the TKA group.
Conclusion
Our findings suggest that socioeconomic disadvantage may be implicated in a substantial proportion of the previously assumed race-driven disparity in healthcare utilization parameters after primary total joint arthroplasty. Orthopaedic surgeons should attempt to identify potentially modifiable socioeconomic disadvantage indicators. This serves as a call to action for the orthopaedic community to consider specific interventions to support patients from vulnerable areas or whose incomes are lower, such as supporting applications for nonemergent medical transportation or referring patients to local care coordination agencies. Future studies should seek to identify which specific resources or approaches improve outcomes after TJA in patients with socioeconomic disadvantage.
Level of Evidence
Level III, therapeutic study.
Introduction
THA and TKA are common orthopaedic procedures with projected growth in the United States of up to 70% and 182%, respectively, from 2014 to 2030 [22]. Despite the relative standardization of perioperative and intraoperative arthroplasty care (with steps like preoperative health management, consistent intraoperative techniques, and postoperative rehabilitation pathways), contemporary studies continue to cite substantial disparities in adverse event rates among patients of different racial backgrounds. Non-White race has been associated with longer length of stay (LOS) after THA and TKA [23, 33]; LOS may be 10% and 8% longer for Black patients after THA and TKA, respectively, compared with White patients [2]. Black race has been associated with 25% to 30% higher odds of readmission after THA and TKA [2]. Black patients have been reported to be less likely to have a home discharge after TKA (36% versus 46% compared with White patients), and similarly, an 11% higher likelihood of nonhome discharge after THA [2]. Furthermore, Black race has been specifically associated with a higher odds of complications after TJA (3.6% versus 2.3% for White race) [2] and a 1.5 times higher risk of infectious and noninfectious complications after TKA [11].
Indeed, contemporary research is rife with “independent” statistical associations between race and a variety of post-TJA adverse outcomes after adjusting for various socioeconomic modifiers/confounders. Although these claims may at times seem methodologically sound, one must question this because they are both biologically and physiologically implausible. Such a dissonance may, in part, stem from the dual nature of “race” as a potentially biologic determinant and a social one; in addition, it has a complex relationship to a multitude of socioeconomic factors. Even though it is possible to statistically account for known socioeconomic confounders, it is critical to realize that this process is imperfect and potential modifiers almost always will remain unadjusted for, poorly unadjusted for, or yet-to-be identified altogether. For example, Leopold et al. [15] recently outlined that the biological aspect of race is highly unlikely to be the independent driver of race-associated outcomes after orthopaedic interventions, based on our understanding of the United States as a “genetic blender.” Instead, social constructs that may be incorrectly attributed to race, such as poor education, limited access to care, and socioeconomic disadvantage (including low income and residence in predominantly in a high-poverty areas), are all more common among Black patients compared with their White counterparts [21]. Socioeconomic disadvantage, in turn, has been associated with increased all-cause mortality [30], as well as an elevated risk of acute adverse medical events (such as pulmonary embolism, hemorrhagic anemia, and cardiac complications), readmission, and early mortality after THA [1, 34] and TKA [24] and is likely the main culprit among the identifiable confounders to the association between race and adverse post-TJA outcomes.
With associations separately reported for race and socioeconomic disadvantage as risk factors for adverse outcomes after THA and TKA, and the known connection between race and socioeconomic disadvantage, we sought to better understand the relationship among race, socioeconomic disadvantage, and outcomes, such as LOS, discharge disposition, ED readmission, and inpatient readmission [1, 2, 11, 21, 23, 24, 30, 33, 34]. To explore this, we used the Area Deprivation Index (ADI) as a proxy for socioeconomic disadvantage, since it is a socioeconomic parameter that estimates the likely deprivation associated with a patient’s home address; it is considered a good surrogate measurement of socioeconomic disadvantages [10, 18, 25].
With that as background, we asked: (1) whether race (in this study, Black versus White) was independently associated with adverse outcomes, including prolonged LOS (LOS of 3 days or more), nonhome discharge, 90-day readmission, and emergency department (ED) visits while controlling for age, gender, BMI, smoking, Charlson comorbidity index (CCI), and insurance; and (2) whether socioeconomic disadvantage, measured by ADI, substantially mediated any association between race and any of the aforementioned measured outcomes.
Patients and Methods
Study Design and Setting
This is a retrospective, comparative study that drew from a longitudinally maintained institutional database. We considered potentially eligible all patients who underwent primary elective unilateral THA or TKA at one of seven large, urban hospitals in Ohio and Florida within a tertiary healthcare system between November 2018 and December 2019 [19, 20]. Data were obtained via a previously described and validated institutional data collection system [6, 19]. This system captures more than 97% of elective orthopaedic surgical interventions and records baseline patient demographics, comorbidities, perioperative and postoperative details, as well as 90-day readmissions in the healthcare system.
Study Population
Patients were considered for inclusion if they underwent primary THA or TKA for osteoarthritis between November 2018 and December 2019. During this period, a total of 2638 patients underwent THA and 4915 underwent TKA. Patients were excluded if they had a documented race that was not White or Black, were missing demographic data, or were missing ADI data. Inclusion of only Black and White race categories was necessary because of the small number of patients from racial groups other than the two that were included here. Nevertheless, such categorization was deemed sufficient for the purposes of the present study given that the greatest magnitude of racial disparity in the measured outcomes has been consistently demonstrated to be between Black and White patients [2, 11, 23, 33]. Race was provider-recorded and captured by the Orthopaedic Minimal Data Set Episode of Care (OME) institutional data collection system. In the THA group, 6% (148 of 2638) of patients were excluded for missing demographic data, 4% (99 of 2638) for missing ADI data, and 2% (46 of 2638) for non-Black or non-White race, yielding a sample of 2345 patients (Fig. 1A). In the TKA group, 7% (328 of 4915) of patients were excluded for missing demographic data, 18% (885 of 4915) for missing ADI data, and 2% (99 of 4915) for non-Black or non-White race, yielding a sample of 3603 patients (Fig. 1B). Ninety-day follow-up was obtained using a longitudinally maintained database that captures all readmissions occurring within 90 days after THA/TKA at any of the hospitals within an integrated healthcare care system, leaving 89% (2345 of 2638) and 73% (3603 of 4915) for analysis in the THA and TKA groups, respectively.
Fig. 1.
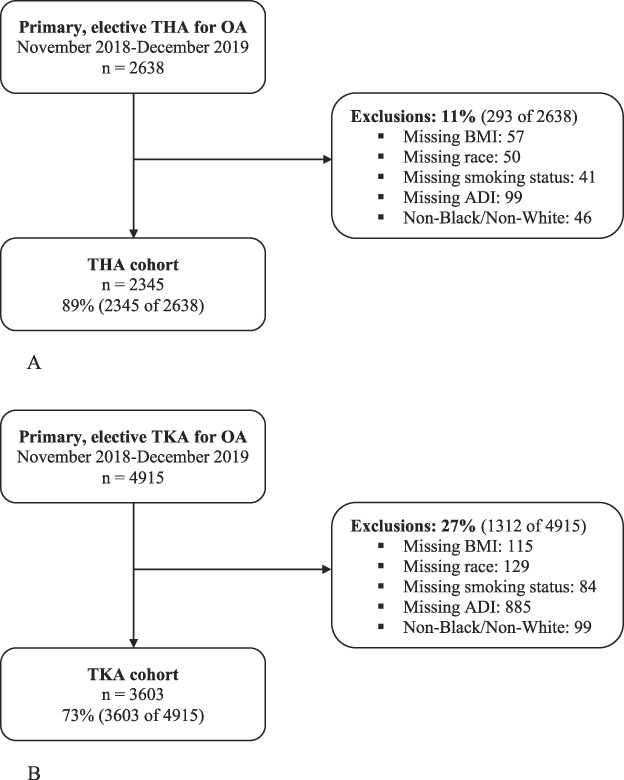
A-B These STROBE diagrams illustrate the reasons for exclusion for patients in the (A) THA and (B) TKA groups; OA = osteoarthritis.
Tools for Quantifying Socioeconomic Disadvantage and Comorbidity Burden: ADI and CCI
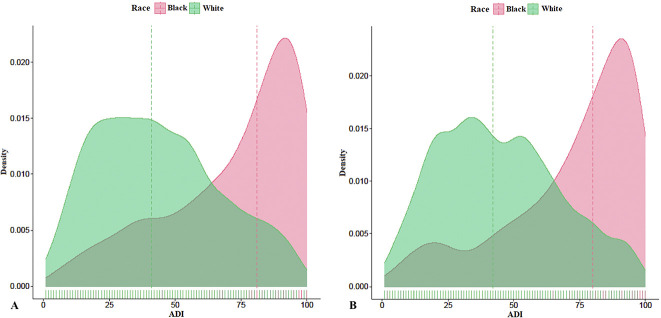
The ADI quantifies a patient’s relative socioeconomic disadvantage based on the patient's home address on the day of surgery. The ADI is scored from 1 to 100, with higher scores suggesting increased socioeconomic disadvantage. We used ADI data from 2018 to 2019, analyzing it as a continuous variable. The ADI has been used as a proxy for socioeconomic disadvantage in arthroplasty research [18, 25] and other healthcare research [10]. The distribution of ADI scores was separated by race for both the THA and TKA groups. A larger proportion of high ADI scores was observed in Black patients compared with White patients for both the THA and TKA groups (Fig. 2).
Fig. 2.
A-B These density plots represent ADI by Black or White race in patients undergoing (A) THA and (B) TKA. A color image accompanies the online version of this article.
The CCI was first described by Charlson et al. [4] in 1987 and was utilized to predict a patient’s likelihood of 10-year mortality based on their comorbidity burden. The index has been refined since the original publication, and we utilized the quan-10 age-unadjusted scoring system [26]. Data on comorbidities was acquired from our institutional data collection system.
Patient Demographics
Among the THA sample, 12% (273 of 2345) of patients were identified as Black and 88% (2072 of 2345) were identified as White. Among the TKA sample, 13% (469 of 3603) were identified as Black and 87% (3134 of 3603) were identified as White. Black patients in general had markedly higher ADI scores (suggesting they lived in areas of higher socioeconomic disadvantage), slightly higher BMIs, and were more likely to be current smokers in the THA group (Table 1). Similar findings were observed in the TKA group, with the additional finding that there was a moderately higher proportion of Black women (Table 2).
Table 1.
Demographic characteristics of the THA group stratified by Black or White race
| Variable | Black (n = 273) | White (n = 2072) | p value |
| Age in years | 64 (56-70) | 67 (60-73) | < 0.001 |
| Women | 55 (149) | 58 (1192) | 0.39 |
| BMI in kg/m2 | 31 (27-37) | 29 (26-34) | < 0.001 |
| Noncommercial insurance | 71 (195) | 63 (1312) | 0.01 |
| Smoking | |||
| Never | 46 (125) | 53 (1101) | < 0.001 |
| Quit | 35 (96) | 38 (778) | |
| Current | 19 (52) | 9 (193) | |
| CCI | 1 (0-2) | 0 (0-2) | < 0.001 |
| ADI | 81 (55-93) | 41 (25-59) | < 0.001 |
Data presented as median and IQR (25th-75th) or % (n). Race was provider-recorded and captured by an institutional data collection system. CCI = Charlson comorbidity index scores represent quan-10 age-unadjusted comorbidity burden with increasing values implying higher comorbidity burden; ADI = Area Deprivation Index quantifies a patient’s relative socioeconomic disadvantage based on his or her home address, with increasing values implying more severe socioeconomic disadvantage.
Table 2.
Demographic characteristics of the TKA group stratified by Black or White race
| Variable | Black (n = 469) | White (n = 3134) | p value |
| Age in years | 64 (57-71) | 67 (61-73) | < 0.001 |
| Women | 72 (336) | 59 (1843) | < 0.001 |
| BMI in kg/m2 | 34 (30-39) | 32 (28-37) | < 0.001 |
| Smoking | |||
| Never | 54 (253) | 54 (1705) | < 0.001 |
| Quit | 33 (156) | 39 (1224) | |
| Current | 13 (60) | 7 (205) | |
| CCI | 1 (0-2) | 0 (0-2) | < 0.001 |
| ADI | 80 (58-92) | 42 (26-61) | < 0.001 |
Data presented as median and IQR (25th-75th) or % (n). Race was provider-recorded and captured by an institutional data collection system. CCI = Charlson Comorbidity Index scores represent quan-10 age-unadjusted comorbidity burden with increasing values implying higher comorbidity burden; ADI = Area Deprivation Index quantifies a patient’s relative socioeconomic disadvantage based on his or her home address, with increasing values implying more severe socioeconomic disadvantage.
Multivariable regression and mediation analyses were used sequentially to adjust for confounding demographic variables, such as age, gender, BMI, smoking, CCI, and insurance (described in more detail in Statistical Analysis).
Primary Study Outcomes
The primary outcomes of the study were an LOS of 3 or more days, nonhome discharge disposition, 90-day inpatient readmission, and 90-day ED admission.
Ethical Approval
We obtained ethical review board approval for this study.
Statistical Analysis
Continuous variables were summarized using means and SD or medians and interquartile ranges, when appropriate. Categorical variables were displayed using counts and percentages. We conducted a univariate analysis to compare proportions between patient demographics and race. Numerical variables were analyzed with paired t-tests, and categorical variables were analyzed using Pearson chi-square tests or Fisher exact tests. To assess associations between race and the study outcomes, multivariable logistic regression models were developed for THA and TKA with age, gender, BMI, insurance, smoking, and CCI included as covariates. Each model’s performance ability was calculated using Tjur R-squared [32] values (range 0 to 1, the higher the better). Mediation analysis was then utilized to assess if ADI mediated any observed associations between race and outcomes. To investigate this, three additional steps were needed according to the following premises and requirements, as described by Mascha et al. [17]: Firstly, “race must be associated with ADI.” Multivariable linear regression was built to test associations between race and ADI, while adjusting for age, gender, BMI, smoking, CCI, and insurance. A significant association of race onto the mediator (ADI) was a prerequisite for mediation being possible. Secondly, “ADI must be associated with the measured outcomes, independent of race.” Multivariable logistic regression was built to test associations between ADI and outcomes, adjusting for race and age, gender, BMI, smoking, CCI, and insurance. A significant association of ADI on the outcome of interest was also an essential precondition for claiming mediation; and lastly, “mediation must be significant.” The significance of mediation was estimated by bootstrapping using R “mediation” package [31]. A nonparametric bootstrap resampling method with 1000 samples was used to generate the confidence interval and p value. Odds ratios and estimates were provided with 95% confidence intervals (CIs). The estimates from mediation analysis represent the proportion of the effect on the dependent variables (outcomes of interest) that may be attributed to the independent variable (race) and the mediator (ADI). The proportion of the total effect that is attributed to the mediator is used to calculate the percent mediation.
Data management and analysis were performed using R (Version 4.0). All tests were two-sided, assuming an alpha level of 0.05.
Results
Associations Between Race and Length of Stay, Discharge Disposition, and Readmission
After adjusting for age, gender, BMI, smoking, CCI, and insurance, White patients were less likely than Black patients to have an LOS of 3 days or more (OR 0.43 [95% CI 0.31 to 0.59]; p < 0.001) and nonhome discharge (OR 0.39 [95% CI 0.27 to 0.56]; p < 0.001) after THA. No association was seen between race and 90-day readmission or ED admission in the THA group (Table 3).
Table 3.
Multivariable logistic regression evaluating associations between race and demographic variables with LOS of 3 or more days, nonhome discharge, 90-day readmission, and 90-day ED admission after THA
| LOS ≥ 3 days | Nonhome discharge | 90-day readmission | 90-day ED admission | |||||
| Variable | Estimate (95% CI) | p value | Estimate (95% CI) | p value | Estimate (95% CI) | p value | Estimate (95% CI) | p value |
| Race (White vs Black) | 0.43 (0.31-0.59) | < 0.001 | 0.39 (0.27-0.56) | < 0.001 | 0.84 (0.51-1.44) | 0.50 | 0.71 (0.46-1.11) | 0.12 |
| Age (IQR increase) | 1.57 (1.27-1.96) | < 0.001 | 2.61 (2.02-3.39) | < 0.001 | 1.38 (1.01-1.89) | 0.047 | 0.8 (0.61-1.06) | 0.11 |
| Gender (women vs men) | 1.59 (1.24-2.05) | < 0.001 | 1.96 (1.47-2.65) | < 0.001 | 1.07 (0.75-1.52) | 0.72 | 1.27 (0.92-1.78) | 0.16 |
| BMI in kg/m2 (IQR increase) | 1.41 (1.21-1.66) | < 0.001 | 1.79 (1.49-2.15) | < 0.001 | 1.27 (1.01-1.60) | 0.04 | 1.22 (0.99-1.50) | 0.06 |
| Smoking (quit vs never) | 0.79 (0.61-1.02) | 0.07 | 0.81 (0.60-1.08) | 0.15 | 1.09 (0.76-1.57) | 0.62 | 1.27 (0.90-1.80) | 0.18 |
| Smoking (current vs never) | 1.19 (0.78-1.79) | 0.41 | 1.48 (0.90-2.38) | 0.11 | 0.81 (0.38-1.56) | 0.56 | 1.46 (0.85-2.42) | 0.16 |
| CCI | 1.26 (1.19-1.35) | < 0.001 | 1.28 (1.19-1.37) | < 0.001 | 1.22 (1.12-1.32) | < 0.001 | 1.16 (1.07-1.26) | < 0.001 |
| Insurance (commercial vs noncommercial) | 0.52 (0.37-0.73) | < 0.001 | 0.39 (0.24-0.60) | < 0.001 | 0.82 (0.50-1.32) | 0.41 | 0.52 (0.34-0.80) | 0.003 |
| Intercept | 0.01 (0.00-0.03) | < 0.001 | 0 (0.00-0.00) | < 0.001 | 0.01 (0.00-0.04) | < 0.001 | 0.11 (0.02-0.57) | 0.01 |
Race was provider-recorded and captured by an institutional data collection system. CCI = Charlson comorbidity index scores represent quan-10 age-unadjusted comorbidity burden with increasing values implying higher comorbidity burden.
After adjusting for age, gender, BMI, smoking, CCI, and insurance, White patients were less likely than Black patients to have an LOS of 3 days or more (OR 0.41 [95% CI 0.32 to 0.54]; p < 0.001), nonhome discharge (OR 0.44 [95% CI 0.33 to 0.60]; p < 0.001), 90-day readmission (OR 0.54 [95% CI 0.39 to 0.77]; p < 0.001), and 90-day ED admission (OR 0.60 [95% CI 0.45 to 0.79]; p < 0.001) after TKA (Table 4).
Table 4.
Multivariable logistic regression evaluating associations between race and demographic variables with LOS 3 or more days, nonhome discharge, 90-day readmission, and 90-day ED admission after TKA
| LOS ≥ 3 days | Nonhome discharge | 90-day readmission | 90-day ED admission | |||||
| Variable | Estimate (95% CI) | p value | Estimate (95% CI) | p value | Estimate (95% CI) | p value | Estimate (95% CI) | p value |
| Race (White vs Black) | 0.41 (0.32-0.54) | < 0.001 | 0.44 (0.33-0.60) | < 0.001 | 0.54 (0.39-0.77) | < 0.001 | 0.60 (0.45-0.79) | < 0.001 |
| Age (IQR increase) | 2.07 (1.77-2.42) | < 0.001 | 3.56 (2.95-4.33) | < 0.001 | 1.58 (1.30-1.92) | < 0.001 | 0.91 (0.78-1.06) | 0.22 |
| Gender (women vs men) | 1.69 (1.35-2.12) | < 0.001 | 1.81 (1.39-2.37) | < 0.001 | 0.92 (0.70-1.22) | 0.57 | 1.12 (0.89-1.41) | 0.33 |
| BMI in kg/m2 (IQR increase) | 1.34 (1.18-1.53) | < 0.001 | 1.52 (1.30-1.77) | < 0.001 | 1.14 (0.95-1.35) | 0.16 | 1.1 (0.96-1.27) | 0.17 |
| Smoking (quit vs never) | 1.13 (0.90-1.40) | 0.29 | 0.88 (0.68-1.13) | 0.31 | 1.12 (0.84-1.48) | 0.44 | 1.26 (1.00-1.59) | 0.05 |
| Smoking (current vs never) | 1.27 (0.82-1.91) | 0.27 | 1.47 (0.89-2.34) | 0.12 | 1.28 (0.74-2.12) | 0.35 | 1.65 (1.12-2.39) | 0.009 |
| CCI | 1.18 (1.12-1.24) | < 0.001 | 1.17 (1.11-1.24) | < 0.001 | 1.15 (1.07-1.22) | < 0.001 | 1.12 (1.05-1.18) | < 0.001 |
| Intercept | 0 (0.00-0.00) | < 0.001 | 0 (0.00-0.00) | < 0.001 | 0 (0.00-0.02) | < 0.001 | 0.15 (0.05-0.45) | 0.001 |
Race was provider-recorded and captured by an institutional data collection system. CCI = Charlson comorbidity index scores represent quan-10 age-unadjusted comorbidity burden with increasing values implying higher comorbidity burden.
Mediation of ADI on Associations Between Race and Measured Outcomes
In the THA group, ADI mediated 37% of the association between race and LOS of 3 days or more (-0.043 [95% CI -0.063 to -0.026]; p < 0.001) and 40% of the association between race and nonhome discharge (0.041 [95% CI 0.024 to 0.059]; p < 0.001). However, a direct association between race and LOS of 3 days or more (-0.075 [95% CI -0.13 to -0.024]; p = 0.004) as well as nonhome discharge (0.060 [95% CI 0.016 to 0.11]; p = 0.004) was observed (Table 5, Fig. 3)
Table 5.
Mediation analysis of ADI on associations observed between Black or White race with LOS 3 or more days and nonhome discharge in patients who underwent THA
| Association | Estimate (95% CI) | p value | % mediation |
| LOS > 3 days | |||
| Mediation (indirect) | -0.043 (-0.063 to -0.026) | < 0.001 | 37% |
| Direct | -0.075 (-0.13 to -0.024) | 0.004 | 64% |
| Total | -0.117 (-0.17 to -0.065) | < 0.001 | 100% |
| Nonhome discharge | |||
| Mediator (indirect) | 0.041 (0.024 to 0.059) | < 0.001 | 40% |
| Direct | 0.060 (0.016 to 0.109) | 0.004 | 60% |
| Total | 0.101 (0.053 to 0.149) | < 0.001 | 100% |
Mediation analysis explored the degree to which the observed relationship between race (independent variable) and LOS of 3 or more days/nonhome discharge (dependent variables) was completely or partially explained by ADI (mediator). The estimates from mediation analysis represent the proportion of the total effect on the dependent variables that may be attributed to the independent variable and the mediator. The mediation (indirect) effect divided by the total effect was used to calculate the percent mediation for each outcome. For example, the mediation effect of ADI on the effect of race on LOS of 3 days or more was -0.043, and the total effect of race on LOS of 3 days or more was -0.117. The percentage of the total effect of race on LOS of 3 days or more that is mediated by ADI was calculated as -0.043/-0.117 = 0.37 or 37%.
Fig. 3.
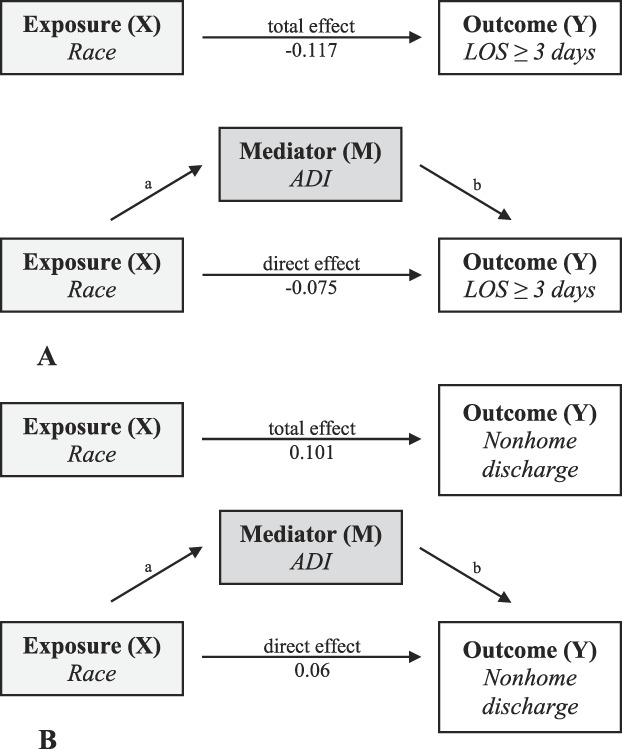
A-B Diagrams illustrating mediation analysis of ADI on associations observed between (A) Black or White race with LOS of 3 or more days and (B) nonhome discharge in patients who underwent THA.
In the TKA group, ADI mediated 19% of the association between race and LOS of 3 days or more (-0.021 [95% CI -0.035 to -0.007]; p = 0.004) and 38% of the association between race and nonhome discharge (0.029 [95% CI -0.016 to 0.04]; p < 0.001); however, a direct association between race and LOS of 3 days or more (-0.088 [95% CI -0.13 to -0.049]; p < 0.001) as well as nonhome discharge (0.046 [95% CI 0.014 to 0.078]; p = 0.006) was observed (Table 6, Fig. 4). ADI did not mediate the associations observed between race and 90-day readmission (0.00 [0.00 to 0.01]; p = 0.27) and 90-day ED admission (0.00 [0.00 to 0.01]; p = 0.33), respectively.
Table 6.
Mediation analysis of ADI on associations observed between Black or White race with LOS > 3 days and nonhome discharge in patients who underwent TKA
| Association | Estimate (95% CI) | p value | % mediation |
| LOS > 3 days | |||
| Mediation (indirect) | -0.021 (-0.035 to -0.007) | 0.004 | 19% |
| Direct | -0.088 (-0.126 to -0.049) | < 0.001 | 81% |
| Total | -0.109 (-0.146 to -0.072) | < 0.001 | 100% |
| Nonhome discharge | |||
| Mediator (indirect) | 0.029 (-0.016 to 0.04) | < 0.001 | 38% |
| Direct | 0.046 (0.014 to 0.078) | 0.006 | 62% |
| Total | 0.075 (0.042 to 0.106) | < 0.001 | 100% |
Mediation analysis explored the degree to which the observed relationship between race (independent variable) and LOS 3 or more days/nonhome discharge (dependent variables) was completely or partially explained by ADI (mediator). The estimates from mediation analysis represent the proportion of the total effect on the dependent variables that may be attributed to the independent variable and the mediator. The mediation (indirect) effect divided by the total effect was used to calculate the percent mediation for each outcome.
Fig. 4.
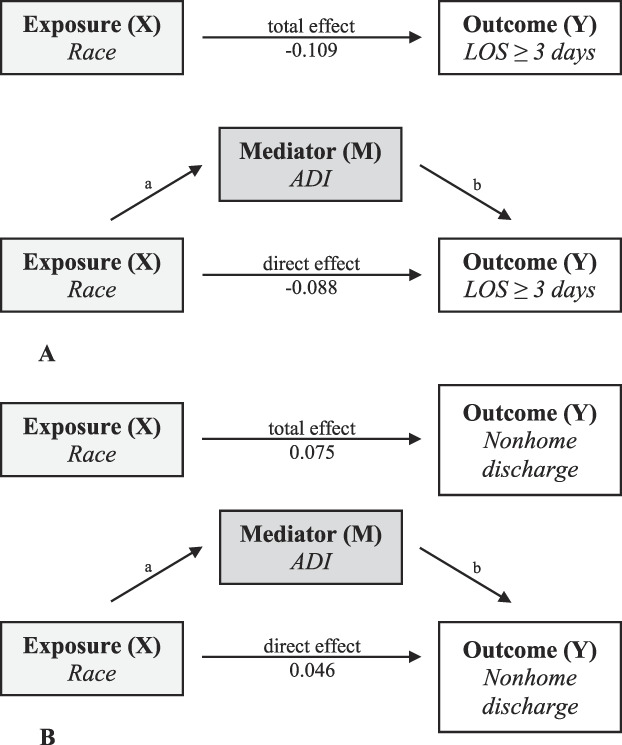
A-B Diagrams illustrating mediation analysis of ADI on associations observed between (A) Black or White race with LOS of 3 or more days and (B) nonhome discharge in patients who underwent TKA. The arrows labeled “a” and “b” represent the indirect effect of race on each outcome that is mediated by ADI.
Discussion
Black and non-White race have been reported to be associated with longer hospital stays, increased risk for infectious and noninfectious complications, and higher odds of readmission after TJA [2, 11, 23, 33]. However, race includes both biological and social components; therefore, claims of associations between adverse outcomes and race in arthroplasty research are problematic if they do not adjust for other important factors [13,14,15]. Most importantly, socioeconomic disadvantages have been associated with increased complications and readmissions after TJA [1, 24, 30, 34] and are more prevalent in patients of Black race compared with those of White race [21]. Therefore, we aimed to explore whether social factors, such as ADI—a surrogate measurement for socioeconomic disadvantage—instead of race, may account for the reported disparities in several important healthcare utilization outcomes (LOS, discharge disposition, ED readmission, and inpatient readmission) after TJA in Black and White patients. Primarily, ADI was found to partially explain observed associations between race and LOS of 3 days or more and nonhome discharge disposition after THA and TKA. These findings suggest that socioeconomic disadvantages, as measured by the ADI, may be implicated in a substantial proportion of the previously assumed race-driven disparity in healthcare utilization parameters after THA and TKA. Orthopaedic surgeons should attempt to identify potentially modifiable socioeconomic disadvantage indicators. This serves as a call to action for the orthopaedic community to consider specific interventions to support patients from vulnerable areas or whose incomes are lower, such as supporting applications for nonemergent medical transportation or referring patients to local care coordination agencies.
Limitations
This institutional comparative study has several limitations. Specifically, 90-day readmission and ED visit data were directly captured if the event occurred within one of the sites affiliated with our healthcare system or if it was reported to one of our institutional providers at a later date and subsequently recorded in the patients’ medical record. Therefore, it is possible that some patients may have required a 90-day readmission/ED visit at an outside institution that was not subsequently communicated to us by the patient or the outside provider. This may have introduced an extent of transfer bias despite having a 100% retrospective follow-up for 90-day outcomes; nevertheless, patients are routinely questioned for adverse events at follow-up visits and not recalling a readmission/ED visit event seems unlikely. We were unable to analyze patients from racial groups other than Black or White because of insufficient representation of individuals from other groups in our cohort; one therefore should not assume that our findings apply to other racial groups. Nevertheless, the current study aimed to highlight that sociodemographic factors are more likely be behind what had been race-associated post-TJA adverse events than is race, a finding that has been most extensively described when comparing White versus Black patients [2, 11, 23, 33]. Future investigations are needed to evaluate similar socioeconomic modifiers of TJA outcomes in patients with various ethnic and racial backgrounds using larger sample sizes. These studies should pay particular attention to capturing important socioeconomic parameters that may contribute to racial disparities such as income, healthcare insurance, housing insecurity, educational attainment, transportation, and nutrition [14]. This is critical given that less than 10% of orthopaedic randomized trials published in three high-tier orthopaedic journals within the last 20 years reported on race, and 80% of these failed to include important social factors [7]. In contrast, we were able to report on racial disparities among Black patients and raise awareness of how social factors, such as socioeconomic disadvantages, are highly important in studies reporting race. We believe our findings may be generalizable to Black and White patients undergoing THA and TKA at large academic centers within the Midwest and Southeastern regions of the United States, and others whose racial sociodemographic distributions are comparable to those reported on here.
We conducted a complete case analysis using multivariable regression and mediation models, which are not without limitations, including failure to account for unmeasured confounding, selection bias, and missing data. However, the proportion of missing data was small and likely missing at random. Furthermore, we used a robust methodology to evaluate associations between a nonmodifiable exposure, such as race, and a modifiable factor and potential mediator of outcomes, such as ADI. We acknowledge that a more detailed assessment of individual comorbidities was not feasible due to the extensive sample size that would be required to ensure adequate power in the multivariable regression model. However, the CCI score is a well-recognized measurement for comorbidity burden in arthroplasty research.
Lastly, we recognize that ADI, which is dependent on patient home address data, may not accurately measure socioeconomic disadvantages for all patients [9]. However, ADI is a validated tool that reflects necessities within a geographic region by factoring income, education, employment, and housing quality [12], and it has been inversely correlated with income [25].
Discussion of Key Findings
The present study observed that Black race (compared with White race) was associated with a higher odds of LOS of 3 days or more and nonhome discharge disposition after THA and a higher odds of LOS of 3 days or more, nonhome discharge, 90-day readmission, and 90-day ED admission after TKA. This is in line with commonly reported racial disparities in joint reconstructive surgery. Firstly, TKA utilization has been shown to be lower for minorities compared with White patients, even after controlling for socioeconomic disadvantage [29]. Black race has been claimed to be a risk factor for readmission after orthopaedic surgery [8] and has been associated with longer LOS compared with White patients after TJA [28]. Amen et al. [3] found that Black race was associated with longer LOS and a higher odds of discharge to a facility after THA and TKA while controlling for demographic factors, median household income, and healthcare insurance. Notwithstanding, a deeper look at the biological and social components of race in the United States leads us to believe these findings should be interpreted with caution [15]. Social determinants of health, such as education, access to care, and socioeconomic disadvantages—which may be unequally distributed among Black and White patients [21]—are more likely to explain these associations.
Our most important finding is that ADI was a partial mediator of the associations observed between race and LOS of 3 days or more and nonhome discharge disposition among Black and White patients undergoing THA and TKA. These results suggest that previous research which may have claimed that race has a causative role in arthroplasty outcomes is not only wrong in theory, but also wrong in practice. Different measurements of socioeconomic disadvantages have been previously associated with adverse outcomes after TJA, including higher healthcare utilization, complications, and readmissions [18, 27, 34]. Mehta et al. [18] found that patients from higher ADI communities were more likely to be discharged to a facility after elective THA in their analysis of 84,931 patients. Weiss et al. [34] reported that lower patient income was associated with an increased risk of early postoperative mortality and readmission within 90 days after THA. Patients with Medicaid insurance, a proxy for socioeconomic disadvantage, have been associated higher healthcare utilization after TKA compared with patients with private insurance [27]. The present study contributes new evidence that ADI, and likely socioeconomic disadvantage, is a partial mediator of the causal relationships that may be observed between race, LOS, and discharge disposition after TJA.
Our discoveries suggest that race should not be used as part of risk stratification algorithms in TJA [16]; rather, ADI and socioeconomic factors are more relevant variables. However, in doing so, it is important to be mindful that social factors do not cause biologic complications [13, 15]. According to our findings, ADI may help institutional software algorithms predict LOS and discharge disposition of patients undergoing THA and TKA. Previously, Martsolf et al. [16] found that including race or ethnicity and socioeconomic parameters in risk-adjusted algorithms had little effect when predicting the odds of hospital readmission after THA and TKA. In contrast, Courtney et al. [5] suggested that models for reimbursement after TJA should be adjusted by socioeconomctic parameters because more severe socioeconomic disadvantage was associated with increased LOS, increased risk of discharge to a facility, and 90-day readmission. Importantly, orthopaedic surgeons should recognize patients who live with socioeconomic disadvantage and facilitate their access to care. For example, orthopaedic surgeons may be able to connect patients to valuable resources, such as nonemergent medical transportation or a local care coordination agency. Considering the growing pressure to curtail healthcare costs in the United States and the recent increase in outpatient or short-stay THA and TKA, future healthcare economic policies and regulations should guarantee physicians the ability to provide patients who live with socioeconomic disadvantage the necessary level of care for successful joint replacement.
Conclusion
Our findings suggest that socioeconomic disadvantage may be implicated in a substantial proportion of the previously assumed race-driven disparity in healthcare utilization parameters after primary TJA. Orthopaedic surgeons should attempt to identify socioeconomic disadvantage indicators and be cognizant of the role socioeconomic disadvantage may have in patients undergoing THA and TKA. This study serves as a call to action for the orthopaedic community to consider specific interventions to support patients from vulnerable areas or whose incomes are lower, such as supporting applications for nonemergent medical transportation or referring patients to local care coordination agencies, when they undergo TJA. Future studies should seek to identify which specific resources or approaches may improve outcomes after TJA in patients with socioeconomic disadvantage, and further elucidate which sociodemographic factors actually drive outcomes after TJA.
Footnotes
The authors certify that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was obtained from the Cleveland Clinic, Cleveland, OH, USA (number 06-196).
Contributor Information
Matthew J. Hadad, Email: hadadm2@ccf.org.
Pedro Rullán-Oliver, Email: rullanp@ccf.org.
Daniel Grits, Email: gritsd@ccf.org.
Chao Zhang, Email: ZHANGC4@ccf.org.
Ahmed K. Emara, Email: emaraa2@ccf.org.
Robert M. Molloy, Email: molloyr@ccf.org.
Alison K. Klika, Email: klikaa@ccf.org.
References
- 1.Agabiti N, Picciotto S, Cesaroni G, et al. The influence of socioeconomic status on utilization and outcomes of elective total hip replacement: a multicity population-based longitudinal study. Int J Qual Health Care. 2007;19:37-44. [DOI] [PubMed] [Google Scholar]
- 2.Alvarez PM, McKeon JF, Spitzer AI, et al. Race, utilization, and outcomes in total hip and knee arthroplasty: a systematic review on health-care disparities. JBJS Rev. 2022;10:e21.00161. [DOI] [PubMed] [Google Scholar]
- 3.Amen TB, Varady NH, Rajaee S, Chen AF. Persistent racial disparities in utilization rates and perioperative metrics in total joint arthroplasty in the U.S. J Bone Joint Surg Am. 2020;102:811-820. [DOI] [PubMed] [Google Scholar]
- 4.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [DOI] [PubMed] [Google Scholar]
- 5.Courtney PM, Huddleston JI, Iorio R, Markel DC. Socioeconomic risk adjustment models for reimbursement are necessary in primary total joint arthroplasty. J Arthroplasty. 2017;32:1-5. [DOI] [PubMed] [Google Scholar]
- 6.Curtis GL, Tariq MB, Brigati DP, et al. Validation of a novel surgical data capturing system following total hip arthroplasty. J Arthroplasty. 2018;33:3479-3483. [DOI] [PubMed] [Google Scholar]
- 7.Cwalina TB, Jella TK, Manyak GA, Kuo A, Kamath AF. Is our science representative? A systematic review of racial and ethnic diversity in orthopaedic clinical trials from 2000 to 2020. Clin Orthop Relat Res. 2022;480:848-858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dailey EA, Cizik A, Kasten J, Chapman JR, Lee MJ. Risk factors for readmission of orthopaedic surgical patients. J Bone Joint Surg Am. 2013;95:1012-1019. [DOI] [PubMed] [Google Scholar]
- 9.Dalkin BH, Sampson LR, Novicoff WM, Browne JA. Zip codes may not be an adequate method to risk adjust for socioeconomic status following total joint arthroplasty at the individual surgeon level. J Arthroplasty. 2020;35:309-312. [DOI] [PubMed] [Google Scholar]
- 10.Hu J, Kind AJH, Nerenz D. Area Deprivation Index predicts readmission risk at an urban teaching hospital. Am J Med Qual. 2018;33:493-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ibrahim SA, Stone RA, Han X, et al. Racial/ethnic differences in surgical outcomes in veterans following knee or hip arthroplasty. Arthritis Rheum. 2005;52:3143-3151. [DOI] [PubMed] [Google Scholar]
- 12.Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible — the neighborhood atlas. N Engl J Med. 2018;378:2456-2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leopold SS. Editorial: Beware of studies claiming that social factors are “independently associated” with biological complications of surgery. Clin Orthop Relat Res. 2019;477:1967-1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leopold SS. Editor’s Spotlight/Take 5: Is our science representative? A systematic review of racial and ethnic diversity in orthopaedic clinical trials from 2000 to 2020. Clin Orthop Relat Res. 2022;480:843-847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leopold SS, Beadling L, Calabro AM, et al. Editorial: The complexity of reporting race and ethnicity in orthopaedic research. Clin Orthop Relat Res. 2018;476:917-920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martsolf GR, Barrett ML, Weiss AJ, et al. Impact of race/ethnicity and socioeconomic status on risk-adjusted hospital readmission rates following hip and knee arthroplasty. J Bone Joint Surg Am. 2016;98:1385-1391. [DOI] [PubMed] [Google Scholar]
- 17.Mascha EJ, Dalton JE, Kurz A, Saager L. Statistical grand rounds: understanding the mechanism: mediation analysis in randomized and nonrandomized studies. Anesth Analg. 2013;117:980-994. [DOI] [PubMed] [Google Scholar]
- 18.Mehta B, Goodman S, Ho K, Parks M, Ibrahim SA. Community deprivation index and discharge destination after elective hip replacement. Arthritis Care Res (Hoboken). 2021;73:531-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.OME Cleveland Clinic Orthopaedics. Implementing a scientifically valid, cost-effective, and scalable data collection system at point of care: the Cleveland Clinic OME cohort. J Bone Joint Surg Am. 2019;101:458-464. [DOI] [PubMed] [Google Scholar]
- 20.OME Cleveland Clinic Orthopaedics. Value in research: achieving validated outcome measurements while mitigating follow-up cost. J Bone Joint Surg. 2020;102:419-427. [DOI] [PubMed] [Google Scholar]
- 21.Reeves R, Edward R, Kneebone E. Five evils: multidimensional poverty and race in America. Available at: https://www.brookings.edu/wp-content/uploads/2016/06/reeveskneebonerodrigue_multidimensionalpoverty_fullpaper.pdf. Accessed August 2, 2022.
- 22.Schwartz AM, Farley KX, Guild GN, Bradbury TL. Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty. 2020;35:S79-S85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shah A, Memon M, Kay J, Wood TJ, Tushinski DM, Khanna V. Preoperative patient factors affecting length of stay following total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2019;34:2124-2165.e1. [DOI] [PubMed] [Google Scholar]
- 24.Shau D, Shenvi N, Easley K, Smith M, Guild G. Medicaid is associated with increased readmission and resource utilization after primary total knee arthroplasty: a propensity score–matched analysis. Arthroplast Today. 2018;4:354-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shaw JH, Wesemann LD, Ayoola AS, Les CM, Charters MA, North WT. Comparison of Area Deprivation Index, socioeconomic parameters, and preoperative demographics with postoperative emergency department visits after total knee arthroplasty. J Arthroplasty. 2021;36:2788-2794. [DOI] [PubMed] [Google Scholar]
- 26.Sinclair ST, McConaghy KM, Emara AK, Klika AK, Piuzzi NS. Reporting of comorbidities in total hip and knee arthroplasty clinical literature. JBJS Rev. 2021;9:e21.0028. [DOI] [PubMed] [Google Scholar]
- 27.Singh JA, Cleveland JD. Socioeconomic status and healthcare access are associated with healthcare utilization after knee arthroplasty: a U.S. national cohort study. Joint Bone Spine. 2020;87:157-162. [DOI] [PubMed] [Google Scholar]
- 28.Singh V, Realyvasquez J, Kugelman DN, Aggarwal VK, Long WJ, Schwarzkopf R. Does racial background influence outcomes following total joint arthroplasty? J Clin Orthop Trauma. 2021;19:139-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Skinner J, Zhou W, Weinstein J. The influence of income and race on total knee arthroplasty in the United States. J Bone Joint Surg Am. 2006;88:2159-2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stringhini S, Carmeli C, Jokela M, et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. Lancet. 2017;389:1229-1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. Mediation: R package for causal mediation analysis. J Stat Softw. 2014;59:1-38.26917999 [Google Scholar]
- 32.Tjur T. Coefficients of determination in logistic regression models—a new proposal: the coefficient of discrimination. Am Stat. 2009;63:366-372. [Google Scholar]
- 33.Weaver F, Hynes D, Hopkinson W, et al. Preoperative risks and outcomes of hip and knee arthroplasty in the veterans health administration. J Arthroplasty. 2003;18:693-708. [DOI] [PubMed] [Google Scholar]
- 34.Weiss RJ, Kärrholm J, Rolfson O, Hailer NP. Increased early mortality and morbidity after total hip arthroplasty in patients with socioeconomic disadvantage: a report from the Swedish Hip Arthroplasty Register. Acta Orthop. 2019;90:264-269. [DOI] [PMC free article] [PubMed] [Google Scholar]