Background:
Penile enlargement surgery is the second most desired cosmetic procedure in men worldwide. The mainstay of penile lengthening procedures is a partial release of the penile suspensory ligament system. Concerns regarding erect penis stability after this procedure have been raised by the surgical community. This study describes the anatomical features of the penile suspensory ligament system and explores the stability mechanisms of the penis.
Methods:
This study is subdivided in two parts: an anatomical analysis and a clinical analysis. The anatomical part consists of a dissection of eight male cadavers to describe the anatomy and test the stability after sectioning successively the suspensory ligaments. The clinical part consists of an analysis of 30 patients with micropenis operated on for penile lengthening by a penile suspensory ligament release and lipofilling.
Results:
The suspensory apparatus consists of four distinct ligamentous structures: fundiform, suspensory, dense vertical, and arcuate ligaments. These different structures are lax superficially but become firm and tense posteriorly. The section of the fundiform and suspensory ligaments did not destabilize the penis.
Conclusion:
Penile lengthening by way of cautious suspensory ligament release can be performed without erection instability.
Takeaways
Question: Detailed anatomic description of the penile suspensory system.
Findings: Four ligaments constitute a complex system.
Meaning: We concluded that the loose nonstabilizing ligaments constituted by the fundiform and the suspensory ligaments can be safely severed.
INTRODUCTION
Penile enlargement surgery is the second most desired cosmetic procedure in men worldwide.1 Surgical division of the suspensory system is considered the mainstay in penile aesthetic surgery, but has raised extensive concerns about erection stability.2–6 The aim of this study is to describe the anatomy of the suspensory ligament system and to explore the stability mechanisms of the penis.
METHODS
Descriptive Anatomy Study
We dissected two male cadavers embalmed following the Thiel method,7–9 70 and 72 years of age at time death, scar-free in the perineal region.
Dynamic Anatomic Study
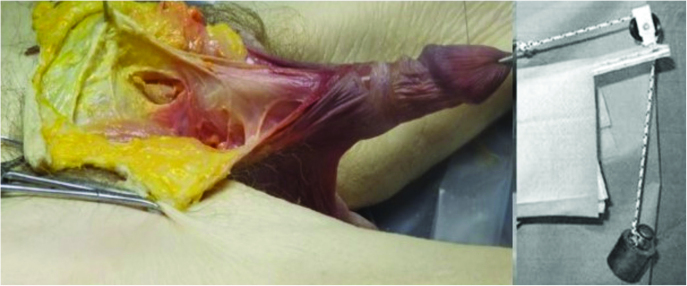
We then dissected six male cadaveric subjects aged from 64 to 70 years old, scar-free in the perineal region, frozen within 10 hours of death and preserved for 3 months without formalin fixation, by injection of 20 L of glycero-pheno-alcohol solution (mixture of 40 L of glycerol, 84 L of alcohol, 60 L of water, and 25 kg of phenol). We inserted one no. 19 scalp needle into the right corporum cavernosum, and connected it to an infusion pump. We then performed a progressive section from the superficial to the deep planes of the different parts of the suspensory system. After each section, an erection was obtained by the induction of a 100 mL per minute flow. In an erect position, after having sectioned progressively each component, we assessed the erected penis stability, placing the organ on an incline under 150 g of traction (Fig. 1). The traction wire passes through a pulley sliding on a hoop. When the erection was induced, if there was stability, the penis remained in the center of the hoop; if the ligament section caused instability, the penis tilted to one side or on the subject’s abdomen.
Fig. 1.
Descriptive anatomy of the fundiform ligament.
Clinical Application to Micropenis
We reviewed our cases of patients with micropenis operated on from January 2018 to December 2018. Micropenis was defined as a normally formed penis, having a stretched penile length (SPL) that falls two SDs below normal for a patient’s age and race. These patients must not have penile dysmorphophobia disorder.10 A psychiatric evaluation was requested only in the case of doubt of dysmorphophobia. We collected selected demographic data. We also performed pre- and postoperative physical examination including an assessment of the flaccid SPL, measured from the pubic penile skin junction to the meatus under the maximal extension of the penis.
Under general anesthesia, after a pubic inverted U incision, the first stage was the dissection of the fundiform and suspensory ligaments. These structures were constituted of superficial, loose, fibrofatty tissue. After the subperiosteal release of these ligaments, there was a clear boundary with an open space, then a very dense layer at the level of the dense vertical ligament. The surgical release must have stopped after entering this tinny open space between the nonstabilizing and the stabilizing structures.
The anterior ligaments were severed close to the pubic bone in a subperiosteal plane until all midline attachments have been freed. Incisions should be close to the anteroinferior border of the pubic symphysis, away from the dorsal aspect of the penis to avoid injury of the dorsal deep arteries, veins, and nerves. To preserve the deep part of this ligament, the depth of the incision should not reach beyond the anterior inferior border of the pubic arch. We closed the inverted U approach with a VY suture using resorbable sutures. A lipofilling was then performed. We instilled in the abdomen 500 mL of physiologic solution containing adrenalin (1:800,000) and 0.02 Xylocain (50 mL Xylocain 1% per 1 L of solution) through the supra pubic incision using an electric device (Osseo Doc, Bienair MOT300). Fat was harvested with a power-assisted system (MicroAire iP.A.L.TM; MicroAire Surgical Instruments LLC, Va.) by means of short or long 3-mm multiple-hole cannula attached to a handpiece and set to 0.5 bars and 0.5 atm. The fat was then centrifuged at 2000 rpm (400 G) for 2 minutes to obtain purified fat with almost nonexistent oily supernatant without compromising efficiency of the graft. The nanofat graft was obtained by shifting the fat with 10-mL syringes after 10 passes.11 We reinjected the nanofat via a punctiform proximal incision with deposition from distal to proximal. (See Video [online], which demonstrates the markings, the section of the fundiform and suspensory ligaments, and the fat grafting in two patients.) A light dressing was put over the incision. The patient could have a regular shower after 48 hours but no intercourse, no bath, no spa, and no swimming for 6 weeks.
Video 1. This video demonstrates the markings, the section of the fundiform and suspensory ligaments and the fat grafting in two patients.
RESULTS
Descriptive Anatomy Study and Dynamic Anatomic Study
We identified four distinct ligamentous structures separated by a loose fatty tissue: the fundiform, the suspensory, the dense vertical and the arcuate. They were lax superficially and became firm posteriorly.
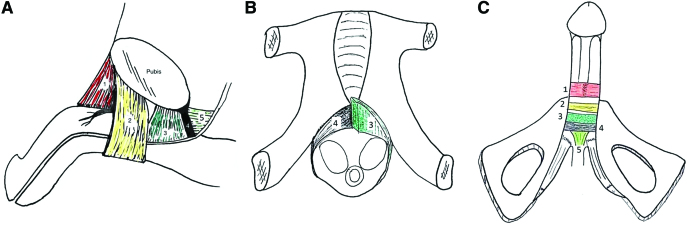
The four ligaments can be divided into two groups (Fig. 2):
Fig. 2.
Anatomical diagrams sagittal and frontal horizontal section. A, Sagittal view. B, Frontal view through the vertical dense ligament. Its right part is removed allowing to see the arcuate ligament. C, Underside view (the ischiocavernous muscles are encircled by the ligamentous structures at their distal part). Looser, nonstabilizing ties: (1) fundiform ligament, (2) suspensory ligament. Stabilizing ties: (3) vertical dense ligament, (4) arcuate ligament, (5) urethral ligament.
(1) The loose, nonstabilizing ties were constituted by the fundiform and the suspensory ligaments. These ligaments did not connect to the symphysis pubis or tunica albuginea. The transection of these two elements did not destabilize the erect penis.
(2) The stabilizing ties consisted of the dense vertical, the arcuate ligaments, which constituted a dense layer, and the ischiocavernous muscles. Due to their attachments to the pubic symphysis and tunica albuginea, they behaved as a major suspensory apparatus for the penis in erection. A complete section of the dense vertical ligament resulted in an instability of the erect penis (mobility).
Clinical Application to Micropenis
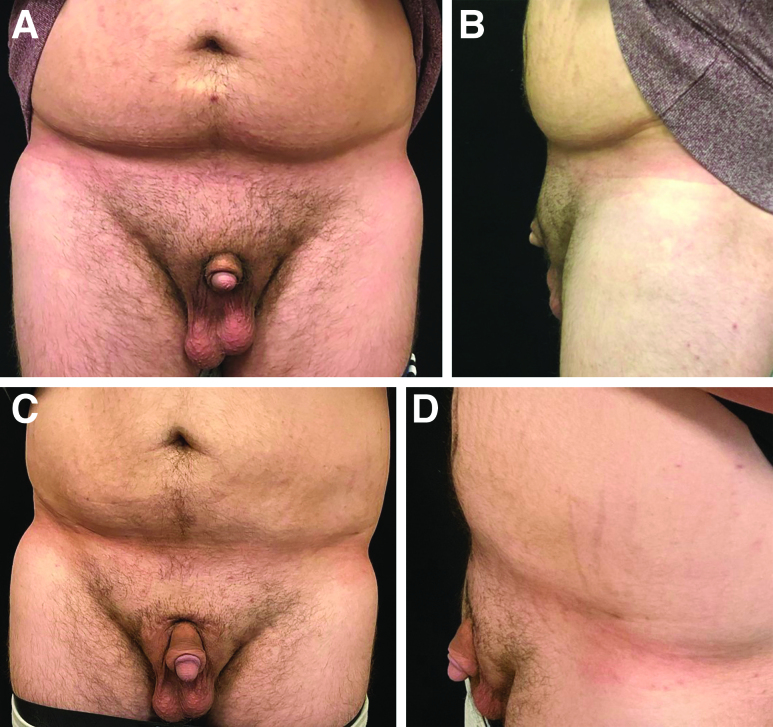
We studied 30 cases. The mean patient age was 37.4 years (range 21–65 years). The mean body mass index was 27.3 (range 21.8–33.8) (Fig. 3). Smokers accounted for 13.3% of patients (Table 1). Anxiety due to penile size and “locker room” embarrassment were the most common causes for consultation. Out of the 30 men, 10 had undergone an evaluation by a psychiatrist preoperatively to rule out body dysmorphic disorder. The average preoperative flaccid stretched length was 7.4 cm (range 1.5–10 cm) and at 1-year postoperative the average length was 10.7 cm (range 8–13 cm) (Fig. 4). The flaccid SPL increased significantly postoperatively to 3.4 cm (range 1,5–7 cm), which represented an average lengthening of 62.7% (range 20%–467%). A second enlargement procedure by nanofat lipofilling was requested by five patients and performed in four with a mean quantity of 66 cc injected. Complications consisted of wound infection with a wound breakdown in one patient, managed conservatively (serial alginate dressings and antibiotics). Two patients required a secondary circumcision because of a paraphymosis and three patients had granuloma and were treated by cortisone injection. All patients had normal sexual function and kept the penile stability (Table 2).
Fig. 3.
Enlargement of a micropenis (frontal and lateral views). Preoperative photographs: (A) front view and (B) lateral view. Postoperative photographs: (C) front view and (D) lateral view.
Table 1.
Demographic Data
| Characteristic | N | Percentage |
|---|---|---|
| Age (y) | ||
| <30 | 9 | 30 |
| 30–40 | 10 | 33.3 |
| 40–50 | 8 | 26.7 |
| 50–60 | 2 | 6.7 |
| >60 | 1 | 3.3 |
| Average: 37.4 [21–65] | ||
| Weight (kg) | ||
| 60–69.9 | 4 | 13.3 |
| 70–79.9 | 10 | 33.3 |
| 80–89.9 | 3 | 10 |
| 90–99.9 | 7 | 23.3 |
| 100–110 | 6 | 20 |
| Average: 85.8 [65.9–106.8] | ||
| Body mass index | ||
| 18.5–24.9 | 11 | 36.7 |
| 25–29.9 | 9 | 30 |
| 30–34.0 | 10 | 33.3 |
| Average: 27.3 [21.8–33.8] | ||
| Tobacco status | ||
| Yes | 4 | 13.3 |
| No | 26 | 86.7 |
| Circumcision status | ||
| Yes | 15 | 50 |
| No | 15 | 50 |
Fig. 4.
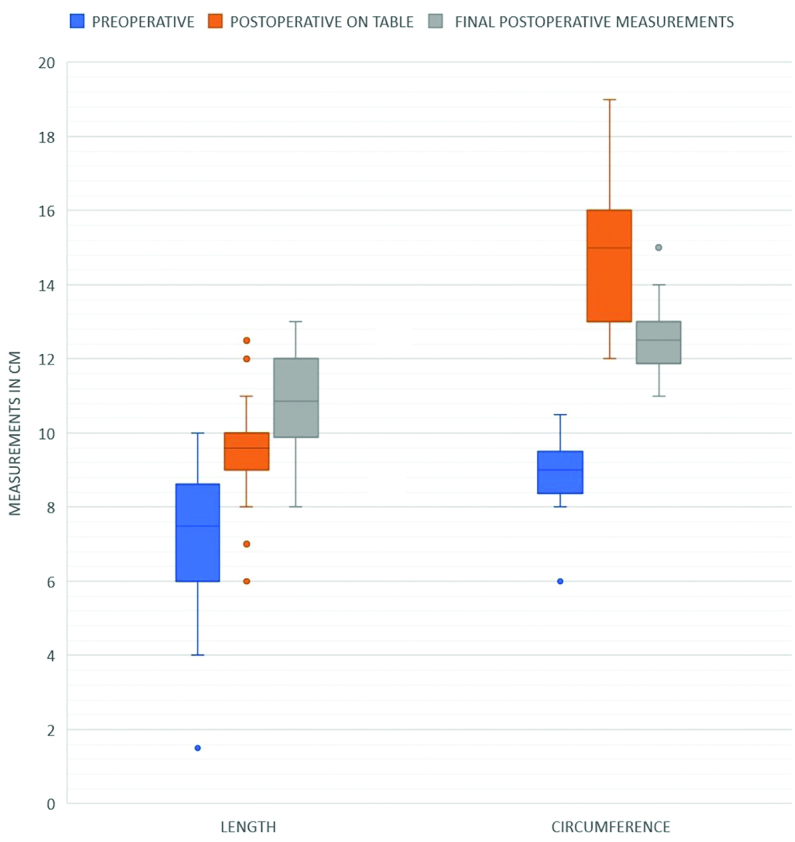
Outcomes of our series of patients on the penile enlargement in micropenises.
Table 2.
Outcomes
| Characteristic | N | Percentage |
|---|---|---|
| Average additional lengthening (cm) | +3.4 [2–5.8] | + 62.7 [20–467] |
| Average additional circumference (cm) | +3.7 [1.5–8] | + 43.5 [21–133.3] |
| Volume of lipofilling | 66 cc [49–80] | |
| Complications | 10 | 33.3 |
| Granuloma | 5 | 16.7 |
| Paraphymosis | 4 | 13.3 |
| Scarring complications (hypertrophic, discolored) | 3 | 10 |
| Infection with wound dehiscence | 1 | 3.3 |
| None | 20 | 66.7 |
| Revisions (under local anesthesia) | 9 | 30 |
| Complementary lipofilling (+average volume) | 5 (66 cc) | 16.7 |
| Secondary circumcision | 2 | 6.7 |
| Fragmentation of granuloma | 3 | 10 |
| None | 21 | 70 |
| Likert satisfaction scale (out of 5) | Average 4.8 [4–5] | |
| Sexual function | ||
| Normal | 30 | 100 |
| Handicapped | 0 | 0 |
DISCUSSION
Penile lengthening surgery is a subject of controversy with a range of methods.12–16 Initial descriptions treat the penile ligament system as one entity without separating it to its components.17–20 Its function during penile erection was emphasized as stabilizing due to the firm adhesion to the pubic bone.18 We dissected four entities in the suspensory system. As Hoznek et al,19 we found anteriorly the fundiform ligament with no function during erection. The absence of connection between the suspensory ligament and the tunica albuginea of the corpora cavernosa was confirmed by Chen et al.20 Posteroinferiorly to the suspensory ligament, we describe for the first time in medical literature a dense vertical ligament connecting the pubis symphysis to the tunica albuginea of the corpora cavernosa. The arcuate pubic ligament reinforces the attachments of the corpora cavernosa to the pubis symphysis, therefore having a similar function to the dense vertical ligament. The arcuate pubic ligament, the crura corpora cavernosa, and the ischiocavernosus muscles firmly attach the corpora cavernosa to the pubis and ischium, constituting the fixed apparatus of the penis. This stabilizes the penis at the specific angle required for sexual intercourse.
CONCLUSIONS
We conclude that penile lengthening with release of the nonstabilizing ties of the suspensory system offers a rational surgical aesthetic approach for patients reasonably unsatisfied with their penile length. When the penis is erect, the remaining stabilizing ties firmly fix the corpora cavernosa to the pubic symphysis, at the specific angle required for sexual intercourse.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Littara A, Melone R, Morales-Medina JC, et al. Cosmetic penile enhancement surgery: a 3-year single-centre retrospective clinical evaluation of 355 cases. Sci Rep. 2019;9:6323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dillon BE, Chama NB, Honig SC. Penile size and penile enlargement surgery: a review. Int J Impot Res. 2008;20:519–529. [DOI] [PubMed] [Google Scholar]
- 3.Li CY, Kayes O, Kell PD, et al. Penile suspensory ligament division for penile augmentation: indications and results. Eur Urol. 2006;49:729–733. [DOI] [PubMed] [Google Scholar]
- 4.Wessells H, Lue TF, McAninch JW. Complications of penile lengthening and augmentation seen at 1 referral center. J Urol. 1996;155:1617–1620. [PubMed] [Google Scholar]
- 5.Vardi Y, Har-Shai Y, Harshai Y, et al. A critical analysis of penile enhancement procedures for patients with normal penile size: surgical techniques, success, and complications. Eur Urol. 2008;54:1042–1050. [DOI] [PubMed] [Google Scholar]
- 6.ISAPS Global Survey Results 2018. Available at https://www.isaps.org/wp-content/uploads/2019/12/ISAPS-Global-Survey-Results-2018-new.pdf.
- 7.Thiel W. An arterial substance for subsequent injection during the preservation of the whole corpse. Ann Anat. 1992;174:197–200. [PubMed] [Google Scholar]
- 8.Thiel W. Die Konservierung ganzer Leichen in natürlichen Farben. Ann Anat. 1992;174:185–195. [PubMed] [Google Scholar]
- 9.Thiel W. Supplement to the conservation of an entire cadaver according to W. Thiel. Ann Anat. 2002;184:267–269. [DOI] [PubMed] [Google Scholar]
- 10.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (5th edWashington, DC: American Psychiatric Association: 2013. Available at 10.1176/appi.books.9780890425596. [DOI] [Google Scholar]
- 11.Tonnard P, Verpaele A, Peeters G, et al. Nanofat grafting: basic research and clinical applications. Plast Reconstr Surg. 2013;132:1017–1026. [DOI] [PubMed] [Google Scholar]
- 12.Campbell J, Gillis J. A review of penile elongation surgery. Transl Androl Urol 2017;6:69–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Austoni E, Guarneri A, Cazzaniga A. A new technique for augmentation phalloplasty: albugineal surgery with bilateral saphenous grafts—three years of experience. Eur Urol. 2002;42:245–253; discussion 252. [DOI] [PubMed] [Google Scholar]
- 14.Perovic SV, Djordjevic ML. Penile lengthening. BJU Int 2000;86:1028–1033. [DOI] [PubMed] [Google Scholar]
- 15.Austoni E, Guarneri A, Gatti G. Penile elongation and thickening—a myth? Is there a cosmetic or medical indication? Andrologia 1999;31(Suppl 1):45–51. [DOI] [PubMed] [Google Scholar]
- 16.Wessells H, Lue TF, McAninch JW. Penile length in the flaccid and erect states: guidelines for penile augmentation. J Urol. 1996;156:995–997. [PubMed] [Google Scholar]
- 17.Surraco LA, Lockhart J. Procesos Del Iigamento Suspensor. (Rosgal, ed.). Montevideo: Rosgal; 1946:1–89. [PubMed] [Google Scholar]
- 18.Bondil P, Wespes E. Anatomie et physiologie de l’érection. Muscles striés et érection. Rapport du 86ème Congrès de l’Association Française d’Urologie Progrès en Urologie. 1992:809. [Google Scholar]
- 19.Hoznek A, Rahmouni A, Abbou C, et al. The suspensory ligament of the penis: an anatomic and radiologic description. Surg Radiol Anat. 1998;20:413–417. [DOI] [PubMed] [Google Scholar]
- 20.Chen X, Wu Y, Tao L, et al. Visualization of penile suspensory ligamentous system based on visible human data sets. Med Sci Monit. 2017;23:2436–2444. [DOI] [PMC free article] [PubMed] [Google Scholar]