Abstract
Background
To capture various social determinants of health, recent analyses have used comprehensive measures of socioeconomic disadvantage such as deprivation and vulnerability indices. Given that studies evaluating the effects of social deprivation on total joint arthroplasty (TJA) have yielded mixed results, a systematic review of this relationship might help answer questions about usage, complications, and results after surgery among patients in different socioeconomic groups and help guide targeted approaches to ensure health equity.
Questions/purposes
We asked: How is social deprivation associated with TJA (1) usage, (2) adverse events including discharge deposition and length of stay, and (3) patient-reported outcome measures (PROMs)?
Methods
A comprehensive review of the PubMed, EBSCO host, Medline, and Google Scholar electronic databases was conducted to identify all studies that evaluated social deprivation and TJA between January 1, 2000, and March 1, 2022. Studies were included if they evaluated comprehensive measures of socioeconomic deprivation rather than individual social determinants of health. Nineteen articles were included in our final analysis with a total of 757,522 patients. In addition to characteristics of included studies (such as patient population, procedure evaluated, and utilized social deprivation metric), we recorded TJA usage, adverse events, and PROM values as reported by each article. Two reviewers independently evaluated the quality of included studies using the Methodological Index for Nonrandomized Studies (MINORS) tool. The mean ± SD MINORS score was 13 ± 1 of 16, with higher scores representing better study quality. All the articles included are noncomparative studies. Given the heterogeneity of the included studies, a meta-analysis was not performed and results were instead presented descriptively.
Results
Although there were inconsistencies among the included articles, higher levels of social deprivation were associated with lower TJA usage even after controlling for various confounding variables. Similarly, there was agreement among studies regarding higher proportion of nonhome discharge for patients with more social deprivation. Although there was limited agreement across studies regarding whether patients with more social deprivation had differences in their baseline and postoperative PROMs scores, patients with more social deprivation had lower improvements from baseline for most of the included articles.
Conclusion
These findings encourage continued efforts focusing on appropriate patient education regarding expectations related to functional improvement and the postoperative recovery process, as well as resources available for further information and social support. We suggest linking patient data to deprivation measures such as the Area Deprivation Index to help encourage shared decision-making strategies that focus on health literacy and common barriers related to access. Given the potential influence social deprivation may have on the outcome and utilization of TJA, hospitals should identify methods to determine patients who are more socially deprived and provide targeted interventions to help patients overcome any social deprivation they are facing. We encourage physicians to maintain close communication with patients whose circumstances include more severe levels of social deprivation to ensure they have access to the appropriate resources. Additionally, as multiple social deprivation metrics are being used in research, future studies should identify a consistent metric to ensure all patients that are socially deprived are reliably identified to receive appropriate treatment.
Level of Evidence
Level III, therapeutic study.
Introduction
Despite the increased usage of and clinical success associated with total joint arthroplasty (TJA) [3, 5, 40, 58], the quality of TJA care varies across patient populations [41]. Recently, there has been an increased interest in how factors such as low income and social determinants of health are associated with perioperative TJA outcomes and quality of care [51, 55]. Specifically, recent analyses have demonstrated disparities in TJA usage and outcomes based on race [2, 21, 61], income [4, 54], education [18, 51], and insurance type [12, 45]. Despite the increased awareness regarding how these social factors contribute to health inequities, inconsistency exists regarding which social determinants of health should be evaluated perioperatively [8, 41].
To capture various social determinants of health, recent analyses have used comprehensive measures of socioeconomic disadvantage such as deprivation and vulnerability indices [8, 59]. These multidimensional metrics frequently incorporate a wide variety of factors such as income, education, and housing quality to generate scores representing relative neighborhood and socioeconomic disadvantage [38]. These measures frequently have been used to capture the association of social determinants of health on outcomes for surgical procedures generally [47], and evaluations of this relationship for TJA have been performed with increasing frequency.
However, studies evaluating the association of social deprivation on TJA have yielded mixed results. It has become increasingly important to determine the relationship of social deprivation and TJA to develop interventions to reduce disparities in orthopaedic care. Because of the differences across studies, a systematic review of studies exploring this relationship might settle controversies about differences in usage, complications, and validated outcomes scores across socioeconomic groups and so might help guide targeted approaches to ensure health equity.
Therefore, our systematic review sought to evaluate how socioeconomic disadvantage is associated with the outcomes of TJA. Specifically, we asked: How is social deprivation associated with TJA (1) usage, (2) adverse events including discharge deposition and length of stay, and (3) patient-reported outcome measures (PROMs)?
Materials and Methods
Search Strategy
We conducted a comprehensive review of the PubMed, EBSCO host, Medline, and Google Scholar electronic databases to identify all studies that evaluated social deprivation and TJA between January 1, 2000, and March 1, 2022 (Appendix 1; http://links.lww.com/CORR/A942). The following keywords and MeSH terms were utilized in combination with “AND” or “OR” Boolean operators: “Arthroplasty, Replacement [MeSH],” “Arthroplasty, Replacement, Hip [MeSH],” “Arthroplasty, Replacement, Knee [MeSH],” “Social Determinants of Health [MeSH],” “Social Deprivation [MeSH],” “Healthcare Disparities [MeSH],” “total hip arthroplasty,” “total knee arthroplasty,” “total joint arthroplasty,” “THA,” “TKA,” “TJA,” “social determinants,” “social deprivation,” and “healthcare disparities.”
Eligibility Criteria
Articles were included if full-text articles in the English language were available; the study described primary TJA; and the study reported on the relationship between social deprivation and usage, adverse events, or PROMs. Specifically, we included studies evaluating comprehensive measures of socioeconomic deprivation rather than individual social determinants of health such as education or income. The following were excluded from our analysis: case reports, systematic reviews, abstracts, unpublished articles, and articles reporting on revision TJA as well as duplicate studies among databases.
Study Selection
In accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines, two reviewers (AK, RJB) independently assessed the eligibility of each article for inclusion in our review. Disagreements were discussed and a third independent reviewer (AJA) was consulted to achieve consensus. The initial query yielded 429 publications, which were then screened for appropriate studies that aligned with the purpose of our review. After removing duplicates and reading each abstract, we selected 62 studies for further consideration. The full text of each article was then reviewed, 19 of which fulfilled our inclusion criteria. A thorough review of each studies’ reference list did not yield any additional articles (Fig. 1). The study characteristics included study design, patient population, procedure (THA, TKA, or both), and social deprivation measure, and factors controlled for in each analysis were documented.
Fig. 1.
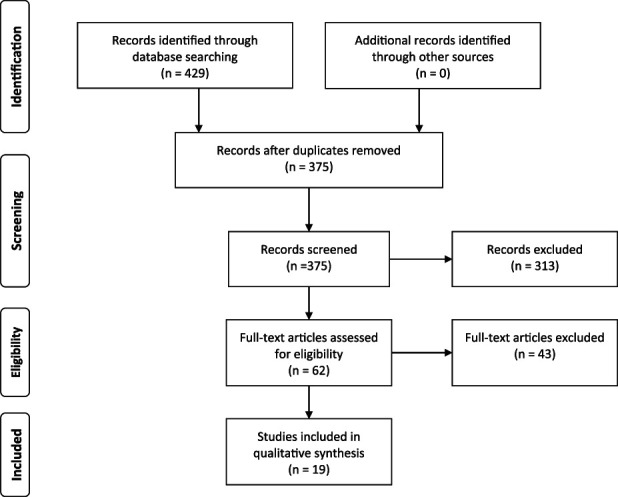
This PRISMA diagram depicts the selection process for article inclusion.
Data Collection
A collaborative online spreadsheet (Google Sheets), arranged by two reviewers (AK, RJB) before starting, facilitated data extraction. Reviewers performed data extraction in duplicate, and they compared findings for verification. We documented details regarding study design, methodology, patient demographics, surgical procedure, and social deprivation index. Complications, utilization, 30- and 90-day readmission, length of stay, cost, discharge disposition, and PROMs constituted the outcomes of interest.
Methodological Quality Assessment
Two reviewers (AK, CJH) independently evaluated the quality of included studies using the Methodological Index for Nonrandomized Studies (MINORS) tool [57], which is a validated assessment tool that grades noncomparative studies from 0 to 16 based on eight criteria and comparative studies from 0 to 24 based on 12 categories related to study design, outcomes assessed, and follow-up. Across these domains, each item is scored 0 if not reported, 1 when reported but inadequate, and 2 when reported and adequate, such that higher scores represent better study quality. Any discrepancies in grading were resolved by discussion with a third reviewer (AJA).
Included Studies
The final analysis included 19 studies (Table 1). In the 17 articles reporting on sample size, 757,522 patients were included. Of the 19 studies, 14 were retrospective, three were cross-sectional, and two were prospective. All the studies were noncomparative and had a mean ± SD MINORS score of 13 ± 1 of 16. Nine different deprivation indices were used across included articles (Table 2). The most common indices were the English Index of Multiple Deprivation (n = 4) and Area Deprivation Index (ADI) (n = 4). The studies were conducted across four countries: United Kingdom (n = 10), United States (n = 7), New Zealand (n = 1), and France (n = 1).
Table 1.
Studies included in final analysis
| Article | Study design | Country | Data source | Deprivation metric | Procedure | Sample size, n | Gender, women |
MINORS scorea |
| Clement et al. [11] | Prospective | United Kingdom | Hospital-specific | Carstairs Score | THA | 1312 | N/A | 14 |
| Clement et al. [10] | Prospective | United Kingdom | Hospital-specific | Scottish Index of Multiple Deprivation |
TKA | 996 | 56.40% | 14 |
| Diaz et al. [14] | Retrospective | United States | Medicare provider analysis and review and CDC Social Vulnerability Index dataset | CDC/ATSDR Social Vulnerability Index |
Both | 70,840 | 61.60% | 12 |
| Dixon et al. [15] | Retrospective | United Kingdom | Hospital Episode Statistics of England | Townsend Index of Deprivation | Both | N/A | 12 | |
| Dixon et al. [16] | Retrospective | United Kingdom | Hospital Episode Statistics of England | English Index of Multiple Deprivation | Both | 83,871 | N/A | 12 |
| Edwards et al. [19] | Retrospective | United Kingdom | National Joint Registry for England, Wales, Northern Ireland, and the Isle of Man; National Health Service England Patient Reported Outcome Measures; and Hospital Episode Statistics of England | English Index of Multiple Deprivation | TKA | 66,769 | 56.50% | 14 |
| Harcombe et al. [24] | Retrospective | New Zealand | New Zealand Ministry of Health’s National Minimum Dataset | New Zealand Deprivation Index | TKA | 62,907 | 54.17% | 12 |
| Hartnett et al. [25] | Retrospective | United States | New York Statewide Planning and Research Cooperative System (SPARCS) database | Social Deprivation Index | THA | 142,681 | 58.60% | 12 |
| Holbert el al. [27] | Retrospective | United States | Administrative database of 16 surgeons | CDC/ATSDR Social Vulnerability Index |
Both | 11,451 | 57.60% | 12 |
| Jenkins et al. [29] | Retrospective | United Kingdom | Regional arthroplasty database | Scottish Index of Multiple Deprivation |
THA | 1620 | 36.7% | 12 |
| Judge et al. [31] | Retrospective | United Kingdom | Hospital Episode Statistics of England | English Index of Multiple Deprivation | Both | N/A | 12 | |
| Judge et al. [32] | Cross-sectional | United Kingdom | Hospital Episode Statistics of England | English Index of Multiple Deprivation | Both | N/A | 14 | |
| Khlopas et al. [36] | Retrospective | United States | Hospital-specific | Area Deprivation Index | TKA | 3928 | 60.50% | 14 |
| Mehta et al. [44] | Retrospective | United States | Pennsylvania Health Care Cost Containment Council | Area Deprivation Index | THA | 84,931 | 55% | 12 |
| Michel et al. [46] | Cross-sectional | France | French hospital national database | French Version of the European Deprivation Index | TKA | 77,597 | 62.80% | 12 |
| Murray et al. [49] | Retrospective | United Kingdom | Hospital-specific (multicenter) | Townsend Index of Deprivation | TKA | 2506 | N/A | 14 |
| Neuburger et al. [50] | Retrospective | United Kingdom | Patient-reported outcome measures program of England | English Index of Multiple Deprivation | Both | 121,983 | 57.90% | 12 |
| Rahman et al. [53] | Cross-sectional | United States | Maryland Health Services Cost Review Commission datasets | Area Deprivation Index | THA | 21,475 | N/A | 12 |
| Shaw et al. [56] | Retrospective | United States | Michigan Arthroplasty Registry Collaborative Quality Initiative (MARCQ) | Area Deprivation Index | TKA | 2655 | N/A | 12 |
MINORS scores range from 0 to 24 for comparative studies and 0 to 16 for noncomparative studies, with higher scores corresponding to lower bias.
Table 2.
Description of included social deprivation tools
| Social deprivation metric | Components included |
| Carstairs Score | Low income, lack of car ownership, overcrowding, and unemployment of men |
| Scottish Index of Multiple Deprivation | Employment, income, crime, housing, health, education, and access to services |
| CDC/ATSDR Social Vulnerability Index | Fifteen factors grouped according to social factors, household composition and disability, racial group, language, housing type, and transportation |
| Townsend Index of Deprivation | Unemployment, lack of car ownership, lack of home ownership, and overcrowding in household |
| New Zealand Deprivation Index | Home internet access, aged 18 to 64 years receiving a means-tested benefit, living in equivalized households with income below a threshold, unemployment, aged 18 to 64 without any qualifications, living in a place other than their own home, aged younger than 65 years living in a single-parent family, living in equivalized households below a bedroom occupancy threshold, living in dwellings that are always damp and/or always have mold greater than A4 size |
| Social Deprivation Index | Income, education, employment, housing, household characteristics, transportation, and demographics |
| English Index of Multiple Deprivation | Income, employment, education, health, crime, barriers to housing and services, and living environment |
| Area Deprivation Index | Seventeen factors grouped according to poverty, housing, employment, and education |
| French version of the European Deprivation Index | Social exclusion, household data, basic amenities of housing, home ownership, car ownership, marital status, year of birth, gender, employment status, education level, and occupation |
ATSDR = Agency for Toxic Substances and Disease Registry.
Given the heterogeneity of the included studies, we did not perform a meta-analysis, and we have presented the results descriptively.
Primary and Secondary Study Outcomes
Our primary study goal was to determine the association between social deprivation and TJA utilization [15, 16, 24, 25, 31, 32, 46, 53] (Table 3). Of the studies included, eight articles evaluated TJA utilization. Our secondary goal was to investigate the association between social deprivation with adverse events and PROMs after TJA. Seven articles evaluated the association between social deprivation and adverse events [11, 14, 19, 27, 36, 44, 56] (Table 4). Six articles reported on the relationship between PROMs and social deprivation [10, 11, 19, 29, 49, 50] (Table 5).
Table 3.
Studies evaluating social deprivation and TJA use
| Study | Key findings | Factors controlled for |
| Dixon et al. [15] | Patients with the highest level of social deprivation (as measured by the Townsend Index of Deprivation) had the lowest utilization of primary TJA | Age, gender |
| Dixon et al. [16] | No correlation between deprivation quintile and utilization of THA and TKA | Correlation only |
| Judge et al. [31] | There was an association between THA and TKA use and social deprivation, with more-deprived groups having lower access to TJA care | Age, gender, rurality, ethnicity |
| Rahman et al. [53] | The THA utilization per 100,000 patients was lower in more socioeconomically disadvantaged communities as measured by the Area Deprivation Index | Age, gender, race or ethnicity, distance to nearest hospital |
| Judge et al. [32] | Patients with the highest levels of social deprivation had higher utilization of TKA but lower utilization of THA | Age, gender, race, rurality, distance to nearest hospital, hospital characteristics |
| Michel et al. [46] | TKA utilization was higher for patients in less socioeconomically deprived communities. As deprivation increased, use decreased | Age, gender |
| Harcombe et al. [24] | People in the most deprived groups had a higher utilization of TJA than the least socioeconomically deprived group | Age, race or ethnicity |
| Hartnett et al. [25] | Patients with a higher level of social deprivation, as measured by the Social Deprivation Index, had decreased odds of THA | Age, gender, race, payer, CCI |
CCI = Charlson comorbidity index.
Table 4.
Studies evaluating social deprivation and perioperative outcomes after TJA
| Study | Key findings | Factors controlled for |
| Clement et al. [11] | Patients with the most severe levels of social deprivation who underwent TJA had increased odds of dislocation and 90-day mortality | Age, gender, CCI, BMI |
| Khlopas et al. [36] | Higher area deprivation (as measured by the Area Deprivation Index) was associated with increased risk of all-cause readmissions, prolonged LOS, and nonhome discharge after TKA | Age, gender, race, BMI, smoking, CCI |
| Holbert et al. [27] | Patients within Maryland Health Enterprise Zones (underserved areas) had an increased risk of nonhome discharge as well as a higher incidence of 90-day ED visits after TJA | Age, gender, anesthesia type |
| Shaw et al. [56] | No association with Area Deprivation Index and 90-day postoperative ED visits after TKA | Age, gender, BMI, ASA class, comorbidities (diabetes, depression), preoperative ED visit |
| Edwards et al. [19] | Greater area deprivation was associated with a lower risk of any complication after TKA | Age, gender, living arrangements, symptom duration, comorbidity burden, baseline PROMs |
| Mehta et al. [44] | Patients with higher Area Deprivation Index values (less affluent areas) had a higher incidence of discharge to a facility after THA. No association seen with Area Deprivation Index and readmission | Age, gender, insurance, ECI, facility volume |
| Diaz et al. [14] | No differences in postoperative complications, mortality, or readmissions for patients undergoing TJA when comparing Social Vulnerability Index scores | Age, gender, race, ECI, hospital teaching status, year |
CCI = Charlson comorbidity index; LOS = length of stay; ED = emergency department; ASA = American Society of Anesthesiologists; ECI = Elixhauser comorbidity index.
Table 5.
Studies evaluating the relationship between social deprivation and PROMs
| Study | Key findings | Factors controlled for |
| Clement et al. [11] | Lower improvements in Oxford hip scores at 1 year associated with more-deprived areas as measured by the Carstairs Score | Age, comorbidity burden, baseline PROMs, LOS |
| Clement et al. [10] | Social deprivation, as measured by the SMID, was not associated with 1-year Oxford knee or SF-12 scores | Age, gender, comorbidity burden, baseline PROMs |
| Jenkins et al. [29] | Patients with the most severe levels of social deprivation who underwent THA had lower baseline, 6-month, and 18-month HHS and SF-36 physical and mental scores | Age, gender |
| Edwards et al. [19] | Greater area deprivation was associated with lower improvements in Oxford knee scores at 6 months | Age, gender, living arrangements, symptom duration, comorbidity burden, baseline PROMs |
| Neuburger et al. [50] | Higher postoperative improvements in the Oxford hip and knee scores were seen for more socially deprived patients. Patients in the most socially deprived cohorts had an increased odds of reporting no improvement after THA and TKA | Age, gender, ethnicity, comorbidity burden, revision rate, primary diagnosis, baseline PROMs |
| Murray et al. [49] | No association between deprivation (as measured by the Townsend score) and KSS or QoL scores | None listed |
LOS = length of stay; SMID = Scottish Index of Multiple Deprivation; HHS = Harris hip score; KSS = Knee Society score; QoL = quality of life.
Results
Arthroplasty Usage
There were mixed data regarding how social deprivation is associated with TJA usage. However, of the eight articles evaluating TJA usage [15, 16, 24, 25, 31, 32, 46, 53], six found that higher levels of social deprivation were associated with lower TJA utilization, even after controlling for various confounding variables including age, gender, rurality, ethnicity, distance to hospital, hospital characteristics, payer, and comorbidity burden (Table 3). All eight studies were retrospective and used a large national database, which allowed them to report on large patient populations. Dixon et al. [16] was the only study that found no association between social deprivation and TJA utilization when they compared different regions within England rather than individual patient characteristics.
Adverse Events
Among the seven studies that evaluated the association between social deprivation and adverse events, there was disagreement about whether social deprivation was associated with readmission and various complications. However, all seven studies evaluating discharge reported higher nonhome discharge for patients with higher levels of social deprivation [11, 14, 19, 27, 36, 44, 56]. These studies were all retrospective, and each had a study population of more than 10,000 participants. However, the study with the highest level of evidence was a prospective study performed by Clement et al. [11], who reported that the most socially deprived THA patients had increased odds of dislocation and 90-day mortality (Table 4).
Patient-reported Outcome Measures
There was limited agreement among the six studies that reported on the link between PROMs and social deprivation about whether patients with more social deprivation had differences between their baseline and postoperative PROMs score. However, four of the included studies found that patients with more social deprivation had smaller improvements from baseline at final follow-up. This ranged from 6 to 18 months postoperatively across studies (Table 5). The highest power studies were prospective studies both performed by Clement et al. [10, 11]. In 2011, Clement et al. [11] utilized the Carstairs Score to measure deprivation and found patients in more deprived areas had lower improvements after THA. In 2013, Clement et al. [10] reported that social deprivation was not associated with 1-year outcomes after TKA when utilizing the Scottish Index of Multiple Deprivation.
Discussion
As orthopaedic surgeons become more cognizant of the social factors that may influence perioperative TJA care, a growing interest has focused on comprehensive measures of social deprivation rather than more granular social determinants of health. Our analysis sought to summarize the current studies evaluating how combined socioeconomic disadvantage among patients undergoing TJA is associated with usage, adverse events, and PROMs. Although there was limited agreement among included studies, we found that patients with more social deprivation frequently have lower TJA utilization than those who are more affluent. Additionally, the frequency of nonhome discharge was greater among patients with more-severe social deprivation. Although it remains unclear whether social deprivation is associated with baseline PROM scores for these patients, socioeconomic disadvantage appears to limit the ability to achieve functional improvements compared with patients who are less deprived. Based on these findings, surgeons should be encouraged to incorporate early screening methods into clinical practice that identify patients with substantial social deprivation, for example, using a questionnaire during preoperative visits to assess for social determinants of health or linking patient data to specific social deprivation metrics. Identifying these patients during the early stages of the treatment process will allow surgeons to provide timely interventions and ensure patients receive adequate support and resources for a successful treatment course. The addition of optional virtual or in-person visits during the perioperative period can also ensure close patient monitoring. Furthermore, care should be provided by a multidisciplinary healthcare team, including social workers, who can connect the patient to community resources and address any social barriers that interfere with access to healthcare. Lastly, policymakers should continue to address areas of social deprivation, such as lack of transportation, which is a major barrier for socially deprived patients. Implementing transportation programs that offer free or reduced rates to and from healthcare facilities may increase access to care and mitigate disparities in people living in deprived areas.
Limitations
This study has limitations. There was wide heterogeneity across included studies regarding what additional factors were controlled for when exploring the association of social deprivation on the evaluated outcome measures, and inconsistency in how these were measured and controlled for may influence reported findings. However, most of the studies controlled for factors that might influence social deprivation and the outcomes of TJA such as age, gender, race, and comorbidity. An important limitation relates to how social deprivation was measured in each article and the fact that we did not use a definition or set of criteria for identifying a social deprivation index. Although Cheng et al. [8] recently found that national ADI and healthcare insurance were the most effective metrics to capture social deprivation, alternative measures of socioeconomic disadvantage were commonly used which may be specific to the countries they were used in. Furthermore, we included studies from different countries with widely disparate healthcare systems. However, many of the social determinants of health are universal and our results may be seen as more generalizable by including data from multiple countries.
Additionally, although we analyzed more-global measurements of deprivation, it is possible that individual social determinants of health or factors such as healthcare insurance or income level could have influenced the evaluated outcomes. However, most of these individual factors are interdependent, and therefore, assessing outcomes through a social deprivation metric may provide a more comprehensive view of the relationship between social determinants of health and patient outcomes after TJA. Furthermore, we were not able to comment on the association between social deprivation and aspects of social identity such as age, gender, and race. Despite these limitations, our systematic review provides the first summary of the available literature on social deprivation and TJA utilization and patient-reported and surgical outcomes.
Arthroplasty Usage
Most of the included studies found that patients with more social deprivation had lower utilization of TJA compared with those with less social deprivation. This has likewise been demonstrated in studies evaluating specific social determinants of health, with lower usage reported among patients with lower income and education, those who live alone, and those who are resource limited [1, 6, 20, 23]. Various theories for the causes of these socioeconomic disparities have been postulated, including concerns regarding inequitable knowledge regarding osteoarthritis or about the potential benefits derived from TJA [63]. Similarly, socially disadvantaged patients may be less willing to undergo these elective procedures because of concerns related to costs, social support for recovery, and difficulties associated with transportation to follow-up appointments [7, 26]. Conversely, primary care providers might expect this patient population to have comparably poorer outcomes and subsequently may be less likely to refer these patients for surgery [6, 9]. Although this issue is likely multifaceted, a large contributing factor is probably the decreased involvement in medical decision-making that has been demonstrated for patients with social deprivation [22, 48]. Therefore, we believe that implementing global measures of social deprivation in clinical practice may help physicians better understand which patients are susceptible to potentially delayed TJA care, and subsequently, address related concerns. Specifically, we suggest linking patient data to deprivation measures such as the ADI to help encourage shared decision-making strategies that focus on health literacy and common barriers related to access [17, 39, 62]. This also highlights the importance of primary care physicians in educating and recommending patients for TJA to increase utilization.
Adverse Events
Although there was general disagreement regarding how social deprivation is associated with outcomes such as readmission [14, 36, 44], general complications [14, 19], and mortality [11, 14], patients who are more socially disadvantaged consistently had increased nonhome discharge. Similar to proposed explanations behind reduced usage among this patient population, nonhome discharge may be driven by patient and provider concerns regarding access to immediate postoperative care, transportation needs, or general social support [7, 26]. However, because home discharge has been shown to be associated with improved postoperative outcomes, such as shorter length of stay, fewer readmissions, and reduced overall costs of care [13, 43], further efforts at improving the proportion of home discharge may help reduce disparities in complications demonstrated in some of the included articles. Previously mentioned shared decision-making interventions that include a multidisciplinary team of nursing staff, social workers, and case managers may help set postoperative expectations, review postoperative instructions and protocols, as well as address patient concerns related to social support after discharge [33, 52, 60]. Given their recently demonstrated potential, mobile applications and messaging services could be implemented to help reduce emergency department visits and readmissions among socially vulnerable patients who are discharged home [34, 36, 37, 64]. However, it is important that discussions related to adequate education and postoperative support begin early [35], preferably when assessing the willingness of patients with more severe levels of social deprivation to proceed with surgical management.
Patient-reported Outcome Measures
Although there were some discrepancies regarding how social deprivation is associated with preoperative PROM scores and gross values postoperatively, most of the included studies found that higher social deprivation was associated with lower functional improvements from baseline. Patients with more severe social deprivation may have more severe arthritis because of delayed access to care [29]. Conversely, the lower functional improvement in patients who are less affluent may be explained by patient expectations postoperatively, where it has been shown that patients with lower expectations report lower functional outcomes. This has been demonstrated previously when focusing on specific social determinants of health, with studies reporting higher expectations among patients with less education and those with lower income [30, 42]. Therefore, in addition to ensuring that patients receive endstage arthritis care in appropriate timeframes, interventions should be implemented that target the expectations of patients with social deprivation. A thorough discussion with the patient regarding access to care and postoperative expectations should be incorporated during preoperative evaluation to improve patient expectations of surgical outcomes. Having these conversations should encourage adherence to the treatment plan and improve functional outcomes. These discussions should focus on what socioeconomic barriers may limit the rehabilitation process and must also include patient counseling regarding the typical duration of recovery, common residual symptoms, and the level of functional improvement patients may receive from joint replacement [28]. Shared decision-making strategies that include discussions with patients regarding their level of social deprivation and its association with comparably lower improvements may help ensure that expectations are appropriately managed among this patient population and resources are provided to improve outcomes after TJA.
Conclusion
Our systematic review found that patients with more social deprivation were less likely to receive TJA, be discharged home, and experience substantial improvements in functional outcomes than patients who were more affluent. These findings should encourage continued efforts at ensuring equitable care across socioeconomic groups. Efforts should focus on appropriate patient education regarding expectations related to functional improvement and the postoperative recovery process and making resources available for further information and social support. We suggest linking patient data to deprivation measures such as the ADI to help encourage shared decision-making strategies that focus on health literacy and common barriers related to access. Hospitals should identify methods to recognize patients whose circumstances involve more severe levels of social deprivation and provide additional targeted interventions to help patients overcome the social deprivation they might be facing. Additionally, shared decision-making between patients with social deprivation and their surgeons can improve the health literacy of these patients and subsequently ensure they have adequate access to quality care. With multiple social deprivation measures utilized in research, future studies should establish a consistent metric to ensure all patients who are socially deprived are reliably identified to receive appropriate treatment. In addition, more information is needed regarding the intersectionality between social deprivation and aspects of social identity such as age, gender, and race.
Footnotes
One of the authors (AFK) certifies receipt of personal payments or benefits, during the study period, in an amount of USD 10,000 to USD 100,000 from DePuy, a Johnson & Johnson Company; in an amount of USD 10,000 to USD 100,000 from Zimmer Biomet; in an amount less than USD 10,000 from Innomed; in an amount less than USD 10,000 from Proctor and Gamble; and in an amount less than USD 10,000 from Signature Orthopaedics.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was waived by the Cleveland Clinic Foundation, Cleveland, OH, USA.
Contributor Information
Amir Karimi, Email: ahk88@case.edu.
Robert J. Burkhart, Email: rjb246@case.edu.
Alexander J. Acuña, Email: aja127@case.edu.
References
- 1.Agabiti N, Picciotto S, Cesaroni G, et al. The influence of socioeconomic status on utilization and outcomes of elective total hip replacement: a multicity population-based longitudinal study. Int J Qual Health Care. 2007;19:37-44. [DOI] [PubMed] [Google Scholar]
- 2.Amen TB, Varady NH, Rajaee S, Chen AF. Persistent racial disparities in utilization rates and perioperative metrics in total joint arthroplasty in the U.S.: a comprehensive analysis of trends from 2006 to 2015. J Bone Joint Surg Am. 2020;102:811-820. [DOI] [PubMed] [Google Scholar]
- 3.Arthritis Foundation. Hip replacement success rates. Available at: https://www.arthritis.org/health-wellness/treatment/joint-surgery/after-surgery/hip-replacement-success-rates. Accessed September 19, 2020.
- 4.Bitar YF, Illingworth KD, Scaife SL, Horberg JV, Saleh KJ. Hospital length of stay following primary total knee arthroplasty: data from the Nationwide Inpatient Sample Database. J Arthroplasty. 2015;30:1710-1715. [DOI] [PubMed] [Google Scholar]
- 5.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brennan-Olsen S, Vogrin S, Holloway KL, et al. Geographic region, socioeconomic position and the utilisation of primary total joint replacement for hip or knee osteoarthritis across western Victoria: a cross-sectional multilevel study of the Australian Orthopaedic Association National Joint Replacement Registry. Arch Osteoporos. 2017;12:97. [DOI] [PubMed] [Google Scholar]
- 7.Carmichael H, Tran B, Velopulos CG. When more is less: urban disparities in access to surgical care by transportation means. Am J Surg. 2022;223:112-119. [DOI] [PubMed] [Google Scholar]
- 8.Cheng AL, McDuffie JV, Schuelke MJ, Calfee RP, Prather H, Colditz GA. How should we measure social deprivation in orthopaedic patients? Clin Orthop Relat Res. 2022;480:325-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clement N. Patient factors that influence the outcome of total knee replacement: a critical review of the literature. OA Orthopaedics. 2013;1:11. [Google Scholar]
- 10.Clement ND, Jenkins PJ, Macdonald D, et al. Socioeconomic status affects the Oxford knee score and Short-Form 12 score following total knee replacement. Bone Joint J . 2013;95:52-58. [DOI] [PubMed] [Google Scholar]
- 11.Clement ND, Muzammil A, Macdonald D, Howie CR, Biant LC. Socioeconomic status affects the early outcome of total hip replacement. J Bone Joint Surg Br. 2011;93:464-469. [DOI] [PubMed] [Google Scholar]
- 12.DeKeyser GJ, Anderson MB, Meeks HD, Pelt CE, Peters CL, Gililland JM. Socioeconomic status may not be a risk factor for periprosthetic joint infection. J Arthroplasty. 2020;35:1900-1905. [DOI] [PubMed] [Google Scholar]
- 13.DeMik DE, Carender CN, Glass NA, Callaghan JJ, Bedard NA. Home discharge has increased after total hip arthroplasty, however rates vary between large databases. J Arthroplasty. 2021;36:586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diaz A, Hyer JM, Barmash E, Azap R, Paredes AZ, Pawlik TM. County-level social vulnerability is associated with worse surgical outcomes especially among minority patients. Ann Surg. 2021;274:881-891. [DOI] [PubMed] [Google Scholar]
- 15.Dixon T, Shaw M, Ebrahim S, Dieppe P. Trends in hip and knee joint replacement: socioeconomic inequalities and projections of need. Ann Rheum Dis. 2004;63:825-830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dixon T, Shaw ME, Dieppe PA. Analysis of regional variation in hip and knee joint replacement rates in England using hospital episodes statistics. Public Health. 2006;120:83-90. [DOI] [PubMed] [Google Scholar]
- 17.Durand MA, Carpenter L, Dolan H, et al. Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. PLoS One. 2014;9:e94670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dy CJ, Marx RG, Bozic KJ, Pan TJ, Padgett DE, Lyman S. Risk factors for revision within 10 years of total knee arthroplasty. Clin Orthop Relat Res. 2014;472:1198-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Edwards HB, Smith M, Herrett E, MacGregor A, Blom A, Ben-Shlomo Y. The effect of age, sex, area deprivation, and living arrangements on total knee replacement outcomes. JBJS Open Access. 2018;3:e0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edwards NM, Varnum C, Overgaard S, Pedersen AB. The impact of socioeconomic status on the utilization of total hip arthroplasty during 1995–2017: 104,055 THA cases and 520,275 population controls from national databases in Denmark. Acta Orthopaedica. 2020;92:29-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goodman SM, Mandl LA, Parks ML, et al. Disparities in TKA outcomes: census tract data show interactions between race and poverty. Clin Orthop Relat Res. 2016;474:1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greenberg CC, Schneider EC, Lipsitz SR, et al. Do variations in provider discussions explain socioeconomic disparities in postmastectomy breast reconstruction? J Am Coll Surg. 2008;206:605-615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hanchate AD, Zhang Y, Felson DT, Ash AS. Exploring the determinants of racial and ethnic disparities in total knee arthroplasty: health insurance, income, and assets. Medical Care. 2008;46:481-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harcombe H, Davie G, Derrett S, Abbott H, Gwynne-Jones D. Equity of publicly-funded hip and knee joint replacement surgery in New Zealand: results from a national observational study. N Z Med J. 2016;129:1442. [PubMed] [Google Scholar]
- 25.Hartnett DA, Brodeur PG, Kosinski LR, Cruz AI, Gil JA, Cohen EM. Socioeconomic disparities in the utilization of total hip arthroplasty. J Arthroplasty. 2022;37:213-218.e1. [DOI] [PubMed] [Google Scholar]
- 26.Hawker GA, Wright JG, Glazier RH, et al. The effect of education and income on need and willingness to undergo total joint arthroplasty. Arthritis Rheum. 2002;46:3331-3339. [DOI] [PubMed] [Google Scholar]
- 27.Holbert SE, Cheema M, Brennan JC, MacDonald JH, King PJ, Turcotte JJ. Patients from medically underserved areas are at increased risk for nonhome discharge and emergency department return after total joint arthroplasty. J Arthroplasty. 2022;37:609-615. [DOI] [PubMed] [Google Scholar]
- 28.Husain A, Lee GC. Establishing realistic patient expectations following total knee arthroplasty. J Am Acad Orthop Surg. 2015;23:707-713. [DOI] [PubMed] [Google Scholar]
- 29.Jenkins PJ, Perry PRW, Yew Ng C, Ballantyne JA. Deprivation influences the functional outcome from total hip arthroplasty. Surgeon. 2009;7:351-356. [DOI] [PubMed] [Google Scholar]
- 30.Jourdan C, Poiraudeau S, Descamps S, et al. Comparison of patient and surgeon expectations of total hip arthroplasty. PLoS One. 2012;7:e30195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Judge A, Welton NJ, Sandhu J, Ben-Shlomo Y. Geographical variation in the provision of elective primary hip and knee replacement: the role of socio-demographic, hospital and distance variables. J Public Health (Oxf). 2009;31:413-422. [DOI] [PubMed] [Google Scholar]
- 32.Judge A, Welton NJ, Sandhu J, Ben-Shlomo Y. Equity in access to total joint replacement of the hip and knee in England: cross sectional study. BMJ . 2010;341:c4092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kansagara D, Chan B, Harmon D, Englander H. Transitions of care: putting the pieces together. Virtual Mentor. 2013;15:145-149. [DOI] [PubMed] [Google Scholar]
- 34.Kee JR, Edwards PK, Barnes CL, Foster SE, Mears SC. After-hours calls in a joint replacement practice. J Arthroplasty . 2019;34:1303-1306. [DOI] [PubMed] [Google Scholar]
- 35.Kelmer GC, Turcotte JJ, Dolle SS, Angeles JD, MacDonald JH, King PJ. Preoperative education for total joint arthroplasty: does reimbursement reduction threaten improved outcomes? J Arthroplasty. 2021;36:2651-2657. [DOI] [PubMed] [Google Scholar]
- 36.Khlopas A, Grits D, Sax OC, et al. Neighborhood socioeconomic disadvantages associated with prolonged lengths of stay, nonhome discharges, and 90-day readmissions after total knee arthroplasty. J Arthroplasty. 2022;37:S37-S43.e1. [DOI] [PubMed] [Google Scholar]
- 37.Kim K, Pham D, Schwarzkopf R. Mobile application use in monitoring patient adherence to perioperative total knee arthroplasty protocols. Surg Technol Int. 2016;28:253-260. [PubMed] [Google Scholar]
- 38.Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible — the Neighborhood Atlas. New Engl J Med. 2018;378:2456-2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Klifto K, Klifto C, Slover J. Current concepts of shared decision making in orthopedic surgery. Curr Rev Musculoskelet Med. 2017;10:253-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508-1519. [DOI] [PubMed] [Google Scholar]
- 41.Li X, Galvin JW, Li C, Agrawal R, Curry EJ. The impact of socioeconomic status on outcomes in orthopaedic surgery. J Bone Joint Surg Am. 2020;102:428-444. [DOI] [PubMed] [Google Scholar]
- 42.Mancuso CA, Sculco TP, Salvati EA. Patients with poor preoperative functional status have high expectations of total hip arthroplasty. J Arthroplasty. 2003;18:872-878. [DOI] [PubMed] [Google Scholar]
- 43.Mayer MA, Pirruccio K, Sloan M, Sheth NP. Discharge home is associated with decreased early complications following primary total joint arthroplasty. J Arthroplasty. 2019;34:2586-2593. [DOI] [PubMed] [Google Scholar]
- 44.Mehta B, Goodman S, Ho K, Parks M, Ibrahim SA. Community deprivation index and discharge destination after elective hip replacement. Arthritis Care Res (Hoboken). 2021;73:531-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Menendez ME, Ring D, Barnes CL. Inpatient dislocation after primary total hip arthroplasty. J Arthroplasty. 2016;31:2889-2893. [DOI] [PubMed] [Google Scholar]
- 46.Michel M, Bryère J, Maravic M, Marcelli C. Knee replacement incidence and social deprivation: results from a French ecological study. Joint Bone Spine. 2019;86:637-641. [DOI] [PubMed] [Google Scholar]
- 47.Mora J, Krepline AN, Aldakkak M, et al. Adjuvant therapy rates and overall survival in patients with localized pancreatic cancer from high Area Deprivation Index neighborhoods. Am J Surg. 2021;222:10-17. [DOI] [PubMed] [Google Scholar]
- 48.Moret L, Anthoine E, Pourreau A, Beaudeau F, Leclère B. Inpatient satisfaction with medical information received from caregivers: an observational study on the effect of social deprivation. BMC Health Serv Res. 2017;17:769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Murray JRD, Birdsall PD, Sher JL, Deehan DJ. Deprivation and outcome of total knee replacement. Knee. 2006;13:98-101. [DOI] [PubMed] [Google Scholar]
- 50.Neuburger J, Hutchings A, Black N, van der Meulen JH. Socioeconomic differences in patient-reported outcomes after a hip or knee replacement in the English National Health Service. J Public Health (Oxf). 2013;35:115-124. [DOI] [PubMed] [Google Scholar]
- 51.Núñez-Cortés R, Chamorro C, Ortega-Palavecinos M, et al. Social determinants associated to chronic pain after total knee arthroplasty. Int Orthop. 2019;43:2767-2771. [DOI] [PubMed] [Google Scholar]
- 52.Pelt CE, Gililland JM, Erickson JA, Trimble DE, Anderson MB, Peters CL. Improving value in total joint arthroplasty: a comprehensive patient education and management program decreases discharge to post-acute care facilities and post-operative complications. J Arthroplasty. 2018;33:14-18. [DOI] [PubMed] [Google Scholar]
- 53.Rahman R, Canner JK, Haut ER, Humbyrd CJ. Is geographic socioeconomic disadvantage associated with the rate of THA in Medicare-aged patients? Clin Orthop Relat Res. 2021;479:575-585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ross TD, Dvorani E, Saskin R, Khoshbin A, Atrey A, Ward SE. Temporal trends and predictors of thirty-day readmissions and emergency department visits following total knee arthroplasty in Ontario between 2003 and 2016. J Arthroplasty. 2020;35:364-370. [DOI] [PubMed] [Google Scholar]
- 55.Rubenstein WJ, Harris AHS, Hwang KM, Giori NJ, Kuo AC. Social determinants of health and patient-reported outcomes following total hip and knee arthroplasty in veterans. J Arthroplasty. 2020;35:2357-2362. [DOI] [PubMed] [Google Scholar]
- 56.Shaw JH, Wesemann LD, Ayoola AS, Les CM, Charters MA, North WT. Comparison of Area Deprivation Index, socioeconomic parameters, and preoperative demographics with postoperative emergency department visits after total knee arthroplasty. J Arthroplasty. 2021;36:2788-2794. [DOI] [PubMed] [Google Scholar]
- 57.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index For Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [DOI] [PubMed] [Google Scholar]
- 58.Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100:1455-1460. [DOI] [PubMed] [Google Scholar]
- 59.Smith TO, Kamper SJ, Williams CM, Lee H. Reporting of social deprivation in musculoskeletal trials: an analysis of 402 randomised controlled trials. Musculoskeletal Care. 2021;19:180-185. [DOI] [PubMed] [Google Scholar]
- 60.Theiss MM, Wllison MW, Tea CG, Warner JF, Silver RM, Murphy VJ. The connection between strong social support and joint replacement outcomes. Orthopedics. 2011;34:357. [DOI] [PubMed] [Google Scholar]
- 61.Thirukumaran CP, Cai X, Glance LG, et al. Geographic variation and disparities in total joint replacement use for Medicare beneficiaries: 2009 to 2017. J Bone Joint Surg Am. 2020;102:2120-2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yen RW, Smith J, Engel J, et al. A systematic review and meta-analysis of patient decision aids for socially disadvantaged populations: update from the International Patient Decision Aid Standards (IDPAS). Med Decis Making. 2021;41:870-896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Youm J, Chan V, Belkora J, Bozic KJ. Impact of socioeconomic factors on informed decision making and treatment choice in patients with hip and knee OA. J Arthroplasty. 2015;30:171-175. [DOI] [PubMed] [Google Scholar]
- 64.Zheng QY, Geng L, Ni M, et al. Modern instant messaging platform for postoperative follow-up of patients after total joint arthroplasty may reduce re-admission rate. J Orthop Surg Res. 2019;14:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


