Abstract
Background
Women residents are underrepresented in orthopaedic surgery. The causes of the deficit of women in orthopaedic surgery are multifactorial, but by identifying the perceptions of women in orthopaedic residency training and comparing them with the perceptions of men, we can improve our understanding of ways to enhance the recruitment of qualified and diverse candidates.
Questions/purposes
(1) What differences exist in the perceived experiences of residents identifying as women and men regarding professional, social, and personal interactions during residency training? (2) Are there differences in the percentage of women and men residents who have experienced harassment or discrimination in preresidency interviews, and are there differences in the type of harassment or discrimination experienced?
Methods
A survey was generated using Academy of Critical Care: Development, Evaluation, and Methodology guidelines. Two focus groups with seven attending orthopaedic surgeons who participate in the Collaborative Orthopaedic Education Research Group and who are experts on gender diversity in orthopaedics were held to improve survey validity. The survey included binary-response, Likert, and free-text questions on the perception of professional, social, and personal interactions held by the resident being surveyed. The questions focused on a respondent’s perception of interactions with staff members, patients, resident colleagues, and attending surgeons, as well as sexual harassment. Program directors at 10 selected Accreditation Council for Graduate Medical Education (ACGME)–accredited orthopaedic residency programs that participate in the Collaborative Orthopaedic Education Research Group shared the survey with residents at their institutions. There were 95 programs in the Collaborative Orthopaedic Education Research Group at the time this survey was distributed. In this program, directors or other interested teaching faculty in orthopaedic residency programs voluntarily participate to discuss and develop quality research on resident and fellow education. These 95 programs account for 46% of the ACGME-accredited programs in the United States at the time the survey was created and distributed. The 10 residency programs had a total of 232 enrolled residents; 15% (34) identified as women. This gender distribution models the national sample of orthopaedic residents. Survey reliability was assessed by calculating the Cronbach alpha after determining the variance in each relevant (nondemographic) survey item. The final survey was found to have excellent internal reliability (alpha = 0.95). Responses from residents identifying as women and those identifying as men were compared using Fisher exact tests for all categorical data, and two-tailed independent t-tests were used for all continuous data. Differences in each survey category (professional interactions, social interactions, personal interactions, and sexual harassment in preresidency interview experiences) were calculated.
Results
Women reported experiencing microaggressions (left undefined to the survey respondent, but generally considered to be subtle, stunning, often automatic, and nonverbal exchanges that are “put downs”) at work more frequently than men did (40% [six of 15] versus 5% [four of 74]; p < 0.001). Specifically, women perceived being interrupted (53% [eight of 15] versus 5% [four of 75]); p < 0.001) by men colleagues, called by their first name (67% [10 of 15] versus 4% [3 of 72]; p < 0.001), and given administrative tasks (27% [four of 15] versus 1% [one of 75]; p = 0.004) more often than men. More women than men perceived that patients (33% [five of 15] versus 0 of 74 [0%]; p < 0.001) and hospital staff (27% [four of 15] versus 7% [five of 74]; p = 0.01) respected their opinion less than that of men. More women than men perceived that group humor negatively targeted their gender (47% [seven of 15] versus 1% [one of 75]; p < 0.001) and that criticism of their surgical skill was based on their gender rather than their ability (33% [five of 15] versus 5% [four of 78]; p = 0.005). In residency or subinternship interviews, 20% of women reported experiencing sexual harassment as defined by a listing of known types of harassment in the question stem, compared with 0% of men (p = 0.004). Women reported harassment in the form of verbal remarks of a sexual nature and obscene images in the workplace, whereas men did not report any form of harassment during interviews.
Conclusion
These findings suggest that the greatest discrepancies in the perceived experiences of women and men residents lie in professional interactions, and women residents are more likely to experience sexual harassment and disparaging humor than men residents.
Clinical Relevance
Addressing these discrepancies, particularly in the professional setting, will help to create a more inclusive work environment and attract more women to orthopaedic surgery. Annual distribution of the survey used in this study by program directors to residents in their programs can help to identify discrepant perceptions that, coupled with the collection of objective data, can be targeted for improvement.
Introduction
Women residents and attending physicians are underrepresented in the educational and professional ranks of orthopaedic surgery. Despite increased representation of women in other surgical specialties [7], the same trend has not been seen in orthopaedic surgery. Orthopaedics has the lowest percentage of women residents among all surgical specialties; currently, only 13% to 14% of all orthopaedic residents are women [16, 26, 28]. Orthopaedic residency is challenging for all residents, and women may encounter additional stresses related to their gender. Women often lack same-gender mentors and professional allies [6, 13, 19, 20], they may struggle to be perceived as an equal to men [18, 21], and some face the complex decision of whether to become pregnant or face the logistics of being pregnant in a demanding work environment [9, 15].
The perceived experiences of women residents in orthopaedic surgery and the stereotypes of the specialty and people in orthopaedic surgery can influence a medical student’s belonging in and desire to pursue a career in orthopaedic surgery [8, 11], and the slow growth in gender diversity in orthopaedic surgery has been attributed, in part, to these perceptions. One study surveyed medical students and found that perceptions of long hours, high physical demands, and the predominance of men in the field were deterrents to pursuing careers in orthopaedic surgery for women [2]. Rohde et al. [22] found similar results, with students noting concerns about the ability to achieve work-life balance in orthopaedic surgery.
It has also been shown that most women residents in orthopaedic surgery are likely to report experiencing microaggressions (defined as subtle, stunning, often automatic, and nonverbal exchanges that are “put downs”) at some point during their training and are more likely to face these than fellows or practicing orthopaedic surgeons [23]. Another study [29] found that more than two-thirds of women orthopaedic residents reported facing some form of sexual harassment during training. Individuals who experienced these behaviors are more likely to demonstrate markers of burnout [12], which can not only impact mental health but also lead to attrition from the field.
It is important to understand the experiences of women residents and directly compare them to the experiences of men residents so that gender diversity can be improved in orthopaedic surgery. Although the perceptions of orthopaedic surgery training held by women students have been documented [11], no prior study, to our knowledge, has evaluated the perceptions of women residents in orthopaedic surgery with regard to their professional and social environments and directly compared them with those of men residents or assessed the percentage of women and men experiencing harassment, as well as the type of harassment, even before residency. These perceptions are important to identify, not only to attract more women into the field but also to improve the wellbeing and retention of women currently in training.
We asked: (1) What differences exist in the perceived experiences of residents identifying as women and men regarding professional, social, and personal interactions during residency training? (2) Are there differences in the percentage of women and men residents who have experienced harassment or discrimination in preresidency interviews, and are there differences in the type of harassment or discrimination experienced?
Materials and Methods
Development and Pretesting
A closed survey instrument from a pilot study on this topic conducted in 2018 was validated using Academy of Critical Care: Development, Evaluation, and Methodology guidelines [4]. The original survey was created and reviewed by two medical students (MS and JT, who are not authors of this study) and two attending orthopaedic surgeons (ADS, MKM). The survey design ensured that issues related to item generation, question composition and formatting, bias avoidance, survey administration, and response rates were considered and applied. Pilot data from 132 men and women orthopaedic surgery residents allowed us to assess the survey’s reliability. Questions that contributed to decreasing reliability were eliminated. Two experts in the field of gender and diversity in orthopaedic surgery (KJT and SEA) revised the survey to improve its validity. Finally, two focus groups, which included seven attending orthopaedic surgeons (three in one group and four in the other) from several geographic regions in the United States, each with backgrounds in resident education and diversity, were conducted. This resulted in question-by-question feedback regarding inclusive wording, response enhancement, and greater instrument validity. This process yielded a 22-question anonymous online survey.
Recruitment Process
This survey was distributed to the program directors at 10 Accreditation Council for Graduate Medical Education (ACGME)–accredited orthopaedic surgery residency programs. These programs were selected based on the program director’s involvement in the Collaborative Orthopaedic Education Research Group as well as their voluntary commitment to distributing the survey to the residents in their program. There were 95 programs in the Collaborative Orthopaedic Education Research Group at the time this survey was distributed. In this organization, program directors or other interested teaching faculty in orthopaedic residency programs voluntarily participate to discuss and develop quality research on resident and fellow education. Geographic diversity (including programs from all four United States Census regions) and size diversity of the programs (inclusion of postgraduate class smaller than six residents or six and more) was considered in order to create a pool of potential respondents whose responses could be generalized to the national resident pool. At the time of survey creation and distribution, there were 208 ACGME-accredited orthopaedic surgery residency programs in the country; thus, Collaborative Orthopaedic Education Research Group membership included 46% of all possible programs. An email to the program directors contained instructions to forward the survey to all residents in their programs. Follow-up emails were sent 3, 6, and 10 weeks later to encourage further participation.
The Survey and its Administration
The survey (Supplemental Digital Content 1; http://links.lww.com/CORR/A967) was created and distributed using Qualtrics (Qualtrics XM Inc), and responses were blinded so no collected data could be used to identify the individual responding or the program in which they were training. Questions consisted of a combination of multiple choice, free text, and Likert scales and focused on the enrollment demographics and faculty characteristics of the residency program; the respondent’s perception of the program’s professional and social environments; their interactions with colleagues, hospital staff, and patients; and biases experienced. Sexual harassment was the focus of two questions and was defined as any of the following: unwanted touching; sexual assault or rape; verbal remarks of a sexual nature (including jokes) directed toward a resident or in their presence; gestures of a sexual nature, including exposure of any private parts; lustful staring at a resident or a part of their body; messages of a sexual nature sent to the resident via email, direct messaging, or on social media; obscene images in the workplace, including calendars, desktop screens, and posters; stalking, including online or physically; sexual coercion, in which a person promises or hints at enhanced career prospects in return for a sexual favor, or threatens adverse career impact if the recipient does not respond favorably; or persistent and unwanted invitations of a sexual nature. Of note, the term “microaggression” used in the survey was not defined explicitly in the survey given that it is defined similarly in major dictionaries without meaningful difference between sources.
Response Percentages and Demographics
Ninety-seven responses were obtained. This represented 42% of potential respondents (232 total residents). Two respondents did not indicate their gender and were not included. One respondent was a fellow and thus was not included, leaving 94 responses. Eighty-three percent (78 of 94 respondents) identified as men, 16% (15 of 94) identified as women, and 1% (one of 94) identified as gender-nonconforming. Gender was examined in a binary framework for the statistical analysis because of the limited number of gender-nonconforming individuals responding to the survey and in orthopaedics in general. Thus, the gender-nonconforming respondent was not included in this analysis. Of the potential respondents, 44% (15 of 34) of women and 39% (78 of 198) of men responded, with no difference in the proportion of responses based on gender (p = 0.70). There were no differences in the proportions of geographic divisions (p = 0.18) or class sizes (p = 0.052) represented by the responding men and women.
The mean total number of women reported in each residency program was 2.8 ± 4.0 (range 0 to 20). A total of 7.5% (seven) of respondents were in programs with no women residents, and 43% (40) were in programs with only one woman resident. Twenty-two percent of respondents (21) were in programs that had no women faculty with frequent interactions with the residents in their program, and an additional 22% (21 respondents) had exposure to only one woman faculty member. The mean number of women faculty members who had frequent interactions with residents (for example, were on teaching staff or were part of a clinical rotation) was 2.1 ± 2.3 per program (range 0 to 10), and the mean number of women faculty in leadership positions (such as program director, associate program director, fellowship director, chairperson, or division chief) in these residency programs was 0.95 ± 1.2 (range 0 to 5).
Ethical Approval
We obtained approval from the institutional review board at Tulane University, New Orleans, LA, USA (number 2021-120).
Statistical Analysis
Survey responses from women and men were compared. Fisher exact tests were used to compare and evaluate all categorical data, and two-tailed independent t-tests were used to compare responses regarding all continuous data. A p value < 0.05 was considered significant. To assess the reliability of the pilot and final surveys, the Cronbach alpha was calculated after determining the variance of each relevant (nondemographic) survey item, and the final survey was found to have excellent internal reliability (alpha = 0.95).
Results
Differences Between Men and Women Residents Regarding Professional, Social, and Personal Interactions During Residency
Professional Interactions
There were gender-based differences in the professional environment in both the surgical and administrative aspects of orthopaedic residency training. Overall, six of 15 women reported that they believed they had been the target of microaggressions from hospital staff members more frequently than coresidents of a different gender had, while only 5% (four of 74) of men agreed with this statement (p < 0.001).
More women than men reported they believed they were provided fewer opportunities to participate in complex procedures than residents of a different gender from their own (14% [two of 14] versus 0% [0 of 75]; p = 0.02). However, there was no difference between men and women in the perceived frequency of invitation to participate in procedures in general (1% [one of 74] versus 7% [one of 14]; p = 0.28). In addition, women reported they were given more administrative or nonclinical tasks than men did (27% [four of 15] versus 1% [one of 75]; p = 0.004). Furthermore, a greater proportion of women than men perceived that criticism of their surgical skill or decision-making was based on their gender rather than their ability (33% [five of 15] versus 5% [four of 78]; p = 0.005). Despite this, there was no difference between women and men regarding their perception that they had equality in terms of operative independence (73% [11 of 15] versus 79% [62 of 78]; p = 0.60).
Women also experienced differences in verbal communication in a professional setting compared with men. Women reported they were interrupted more often by colleagues of a different gender than men were (53% [eight of 15] versus 5% [four of 75]; p < 0.001). Furthermore, more women than men agreed with the statement, “I am referred to by my first name rather than my title of doctor more frequently” (67% [10 of 15] versus 4% [three of 72]; p < 0.001).
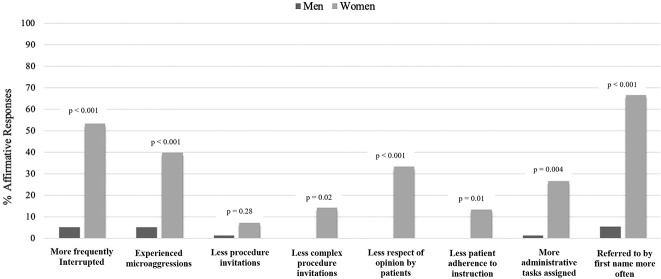
Additionally, men and women residents experienced differences in their interactions with hospital staff, such as scrub technicians or nurses, as well as with patients. A greater proportion of women than men felt their opinions were respected by hospital staff less frequently (27% [four of 15] versus 7% [five of 74]; p = 0.01). Women, more commonly than men, perceived that patients were less likely to adhere to their instructions (13% [two of 15] versus 0% [0 of 73]; p = 0.01) and respected their opinion less than that of men (33% [five of 15] versus 0% [0 of 74]; p < 0.001) (Fig. 1).
Fig. 1.
This bar chart demonstrates the percentage of men (black) and women (gray) resident respondents who agreed that their experiences in each interaction was different from that of the opposite gender.
Social Interactions
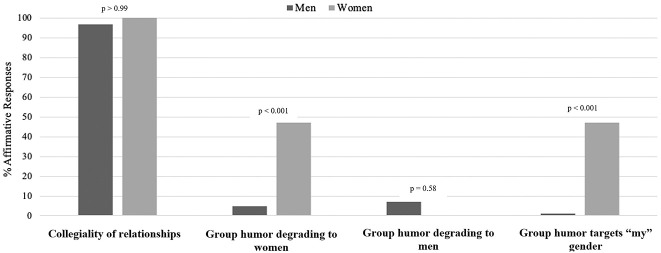
Overall, all women and most men believed their relationships with coresidents of a different gender were collegial (100% [15 of 15] versus 97% [72 of 74]; p > 0.99). Few women and men believed that junior residents ignored them in social settings (8% [one of 13] versus 3% [two of 70]; p = 0.43). Additionally, very few women and men felt they were socially ignored by coresidents of a different gender, and there was no difference between these groups (7% [one of 15] versus 4% [three of 72]; p > 0.99). However, seven of the 15 women felt that group jokes or dynamics often negatively targeted their gender, whereas only 1% (one of 75) of the men felt this way (p < 0.001). Additionally, more women than men perceived that group humor among colleagues was degrading to women (47% [seven of 15] versus 5% [four of 76]; p < 0.001). Most women and men did not believe that group humor was degrading to men (0% [0 of 15] versus 7% [five of 76]; p = 0.58) (Fig. 2).
Fig. 2.
This bar chart depicts differences in experiences between men (black) and women (gray) orthopaedic surgery residents regarding the social atmosphere of their residency program.
Personal Environment
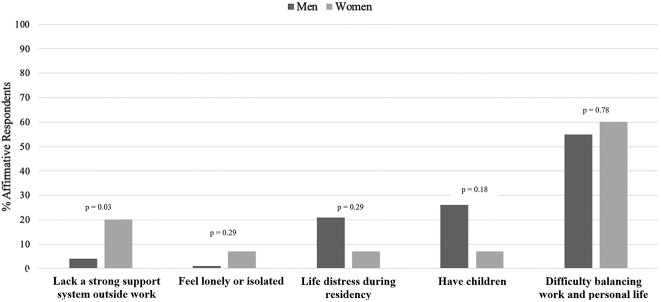
Most women and men indicated they did not feel lonely or isolated from other residents (93% [14 of 15] versus 99% [74 of 75]; p = 0.29). Three of these 15 women noted a lack of a strong support system outside of work, while only 3% (two of 77) of men noted this finding (p = 0.03). There was no difference in the proportion of men and women who had difficulties in balancing residency with personal life (55% [42 of 77] versus 60% [nine of 15]; p = 0.78) or those with substantial life distress during residency, such as divorce or break-up of a long-term relationship (21% [16 of 77] versus 7% [one of 15]; p = 0.29). There was no difference between men and women regarding having children (26% [20 of 78] versus 7% [one of 15]; p = 0.18) (Fig. 3).
Fig. 3.
This bar chart depicts the percentage of men (black) and women (gray) residents who experienced the described personal life events while in orthopaedic surgery residency.
Differences in the Percentage of Residents Who Have Experienced Harassment or Discrimination in Preresidency Interviews and Type of Harassment or Discrimination Experienced
In analyzing differences specific to subinternship or residency interview experiences, more women than men reported they experienced sexual harassment in such environments (20% [three of 15] versus 0% [0 of 78]; p = 0.004). Sexual harassment was defined in the survey question stem according to a definition from a previous study [29]. The type of sexual harassment experienced by women included verbal remarks of a sexual nature (three of four descriptions) and obscene images in the workplace (one of four descriptions). One woman experienced both verbal remarks of a sexual nature and obscene images in the workplace. We could not subanalyze the types of sexual harassment experienced, given the small number of events in question. There was no difference between men and women in their perception of gender-based discrimination in interviews or subinternship experiences (5% [four of 78] versus 13% [two of 15]; p = 0.25).
Discussion
Previous studies have evaluated the impact of experiences in youth through medical school that result in the decisions of women to pursue careers in orthopaedic surgery [3, 11, 22, 25]. This decision is often informed by what they observe in the experiences of women in training as well as longstanding stereotypes that can affect feelings of belonging [8]. The environment faced by women while in medical and surgical training programs has been documented [18] and impacts not only the opinions of students regarding the field but also the wellbeing of women residents. This could contribute to attrition of women from orthopaedic surgery [12]. Although previously defined at other levels of training or practice in orthopaedic surgery [24] and in residency programs in fields outside orthopedic surgery, the current study demonstrates (based on the responses from a novel, validated survey instrument) that differences exist in the perceptions of women and men orthopaedic residents with regard to their professional and social interactions and their experiences of sexual harassment and discrimination as medical students during residency interviews. Specifically, we found that women residents, when comparing their experiences with those of men residents, reported more microaggressions from hospital staff members, fewer opportunities to participate in complex procedures, more administrative or nonclinical tasks, more criticism of surgical skill or decision-making based on their gender, more interruptions from colleagues of a different gender, more references by their first name rather than professional title, less respect from patients and hospital staff, and more group humor targeting their gender than men residents.
Limitations
First, the comparisons made in this study were based on data from a potential sample of 232 residents from 10 programs rather than a national sample of orthopaedic residents. This was intentional to limit nonresponder bias and was directed by feedback from our pilot study, which had a very low response proportion. We only surveyed residents via program directors from 10 select programs in the Collaborative Orthopaedic Education Research Group, who would assist in ensuring a high response proportion. Selecting a subset of residency programs allowed an appropriate calculation of the response percentage rather than sending the survey to all program directors and then not knowing which residents received the survey, avoiding the limitation of nonresponder bias. To help improve the generalizability of the data, we selected these 10 programs by considering their geography, class size, population territory (urban versus rural), and other features to model the national sample of residents, similar to how databases (such as the National Inpatient Sample or National Electronic Injury Surveillance System) select hospitals for reporting. Furthermore, our sample population represents all postgraduate years and women:men ratio of the national sample. Thus, although this survey yielded only 15 responses from women orthopaedic residents, our proportion of respondents who were women (16%) was similar to that of the total resident pool in the United States (14%). Additionally, the proportion of women who responded among all possible women respondents was not different from the proportion of men who responded, and there were no differences in the geography or class sizes of the two groups of respondents. Additionally, given that the survey asks questions about preresidency events, responses may be subject to recall bias, given the length of time from the recalled event to the survey’s administration. However, when respondents recalled whether such impactful and upsetting situations occurred (such as sexual harassment or discrimination), we expect that the memory of the occurrence would not be lost to recall. We also recognize there was no definition of the term “microaggression” in the question stem. This could have resulted in variable interpretation and loss of validity of the responses and our data.
Most importantly, this survey aimed to elicit the subjective response of residents. It was not structured to define objective differences in factors such as procedure volume and numbers of administrative tasks. This study design was selected to help us understand how residents perceive their experiences, because perception does not always reflect the true objective evidence. We believe a resident’s subjective perception drives the discussion between that resident and a medical student or prospective applicant about their residency experience and sparks or extinguishes interest in applying to orthopaedics. We also believe that subjective factors play strongly into a resident’s daily interpersonal interactions with other residents, attending surgeons, staff, and others during the resident’s day-to-day life.
Differences Between Men and Women Residents Regarding Professional, Social, and Personal Interactions During Residency
Generally, there were many more instances of perceived differences between women and men with regard to professional interactions than in the social or personal categories. We found that women residents reported more microaggressions from hospital staff members, fewer opportunities to participate in complex procedures, more administrative or nonclinical tasks, more criticism of surgical skill or decision-making based on their gender, more interruptions from colleagues of a different gender, more references by their first name rather than professional title, and less respect from patients and hospital staff than men did. At the time of this survey’s distribution, to our knowledge, there had been no documented reports specifically comparing perceptions of the professional interactions of men and women residents; thus, we believe these are novel findings. Unfortunately, our findings are similar to the reported experiences of women in fields outside orthopaedic surgery. In general surgery, men and women residents noted differential opportunities for women, high rates of dismissal of the professional titles of women by patients, and negative stereotyping of women residents [18]. Another study [17] noted that women in general surgery (trainees and consultants) were more likely to have their opinions ignored or were more likely to be bullied in a professional setting. One further study [1] described the gender-related aspects of the “minority tax” and described that pressure for women to participate in more administrative tasks can have implications on their career.
In terms of social experiences, women were more likely to report group humor among their colleagues as being degrading toward women. This, along with women perceiving they were interrupted by colleagues more often than men, suggests that women have different interpersonal experiences than men do. This finding supports previous evidence that women generally feel more bullied than men in surgery and surgical subspecialties [5, 17]. These findings suggest that women experience a more hostile social environment than men do.
In terms of personal experiences, women felt less supported at home than men did. This finding agrees with the work of others who found that women orthopaedic and nonorthopaedic surgeons had more primary household responsibilities and lower career satisfaction than their men colleagues [10, 14]. However, we found there was no difference in the experience of distressing life events, such as divorce, during residency between men and women respondents. Unsurprisingly, women and men orthopaedic residents both experienced personal conflicts and difficulties in finding work-life balance overall. This can be more taxing on residents without a strong support system at home, suggesting that women may have a more difficult time on this front. Lack of support at work or at home is a large contributor to burnout, especially for women [27]. Fortunately, loneliness, often cited as a risk factor for burnout, was not frequently noted by the respondents in this study.
Differences in the Percentage of Residents Who Have Experienced Harassment or Discrimination in Preresidency Interviews and Type of Harassment or Discrimination Experienced
Three women and no men indicated they had experienced sexual harassment in residency or subinternship interviews, including sexual verbal remarks made toward them, although a subset of men perceived discrimination. One study [29] found that 68% of surveyed practicing women orthopaedic surgeons experienced sexual harassment while in residency training, and another found that 47% of surveyed women who were American Academy of Orthopaedic Surgeons members experienced sexual harassment in the workplace [24]. These data, in conjunction with our survey, suggest that sexual harassment occurs in residency interviews, and unfortunately may continue throughout a woman’s career. Although this finding does not detract from the gravity of this issue for women, men in our survey population also felt discriminated against. Although perceived discrimination against men was less frequent than that perceived by women, this has been documented in a survey of American Academy of Orthopaedic Surgeons members [24] and should be considered in the context of improving the environment for all parties.
Possible Solutions
Based on the findings of this study, we recommend that the first step to addressing these issues and working to create a more gender-equitable environment is to identify and acknowledge the perceived discrepancies on a program level. Having each orthopaedic surgery residency program self-administer the survey from this study and openly discuss the results in a manner that keeps respondent confidentiality can identify issues not previously expressed. This is a rapid option for internal quality improvement that program leadership can use to understand the concerns of residents and is not resource intensive. Subsequently, objective data should be collected. For example, residency programs should more actively, and on a recurring basis, track residents’ complex procedure volumes to identify differences between men and women residents. If differences exist, opportunities to enhance the experience of those with fewer complex procedures would be program-specific, although recognizing the pattern of underlying issues would help to correct this issue. In addition, the distribution of administrative tasks should be examined in order to assure gender equity. These objective data can help validate the subjective perceptions of residents, specifically in the professional environment, given the high number of discrepancies between what men and women perceive. Vocal leadership from residency program directors that highlights the differences in residency experiences based on gender and sets expectations of inclusivity can facilitate improved awareness among trainees and faculty to improve these experiences. Recruiting and promoting more women to academic roles can help address issues faced by women residents and medical students; however, the development of more training programs to promote social and cultural competency should not rely solely on the input of women faculty, because this is the responsibility of all orthopaedic surgery faculty, especially men in leadership positions. Additionally, the creation of formal mentorship programs in residency programs, graduate medical education departments, or hospital systems would enhance access and promote mutually beneficial relationships. Finally, training faculty and residents in identifying and appropriately responding to microaggressions and harassment in the workplace can help address these issues.
Conclusion
We found that women residents were more likely to perceive differences in experiences related mostly to their professional environment, but also reported disparaging humor, being discounted as a physician, being given more administrative tasks than men residents, and more sexual harassment during preresidency interviews. All of these can lead women to feel they have a lack of support and that they do not belong in orthopaedic surgery, increasing the risk of burnout. Given that reported differences in professional interactions were more common than those in the social or personal areas, the focus should be on interventions to improve professional interactions. Differential and negative experiences may start before residency begins, because women reported sexual harassment in subinternship or residency interviews. However, improving the culture of orthopaedic surgery is everyone’s responsibility, especially that of men, because most faculty members are men, as are most members of department and program leadership. Acknowledging these different experiences between men residents and women residents is the first step to decreasing bias, creating a more inclusive and healthy work environment for women in orthopaedics and enhancing the pipeline for future generations.
Group Authorship
Participating Members of the Collaborative Orthopaedic Educational Research Group include: Gregory Vrabec, Brent Ponce, Daniel Wongworawat, Afshin Razi, Daniel Farber, Dawn Laporte, J. Milo Sewards, Lauren Geaney, and Jaysson Brooks.
Acknowledgments
We thank Margaret Smythe MD and Jeffrey Trojan MD for their contributions to the development of the pilot survey and data collection.
Footnotes
Members of the Collaborative Orthopaedic Educational Research Group are listed in an Appendix at the end of this article.
One of the authors (SEA) serves as Chair, Accreditation Council for Graduate Medical Education Residency Review Committee, Orthopaedic Surgery 2021 to 2024. One of the authors (KJT) has received honorarium for lectures, during the study period, in an amount of less than USD 10,000 and serves as an American Medical Association delegate from the American Academy of Orthopaedic Surgeons as well as a member of the National Institutes of Health-Office of Research on Women’s Health-Advisory Committee. One of the authors (MKM) serves in unpaid leadership positions on the following organizations: Arthroscopy Association of North America, American Orthopaedic Society of Sports Medicine, American Academy of Orthopaedic Surgeons, American Orthopaedic Association, and Ruth Jackson Orthopaedic Society.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was obtained from Tulane University, New Orleans, LA, USA (number 2021-120).
This work was performed at Tulane University School of Medicine, New Orleans, LA, USA.
Contributor Information
Tessa R. Lavorgna, Email: tlavorgn@tulane.edu.
S. Elizabeth Ames, Email: elizabeth.ames@med.uvm.edu.
Kimberly J. Templeton, Email: ktemplet@kumc.edu.
Mary K. Mulcahey, Email: mary.mulcahey.md@gmail.com.
Collaborators: Gregory Vrabec, Brent Ponce, Daniel Wongworawat, Afshin Razi, Daniel Farber, Dawn Laporte, J. Milo Sewards, Lauren Geaney, and Jaysson Brooks
References
- 1.Armijo PR, Silver JK, Larson AR, Asante P, Shillcutt S. Citizenship tasks and women physicians: additional woman tax in academic medicine? J Womens Health (Larchmt). 2021;30:935-943. [DOI] [PubMed] [Google Scholar]
- 2.Baldwin K, Namdari S, Bowers A, Keenan MA, Levin LS, Ahn J. Factors affecting interest in orthopedics among female medical students: a prospective analysis. Orthopedics. 2011;34:e919-e932. [DOI] [PubMed] [Google Scholar]
- 3.Bath MF, Harries RL, Gokani VJ. Medical students’ and interns’ interest in orthopedic surgery: the gender factor. J Surg Educ. 2017;74:1. [DOI] [PubMed] [Google Scholar]
- 4.Burns KEA, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians. Can Med Assoc J. 2008;179:245-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crebbin W, Campbell G, Hillis DA, Watters DA. Prevalence of bullying, discrimination and sexual harassment in surgery in Australasia. ANZ J Surg. 2015;85:905-909. [DOI] [PubMed] [Google Scholar]
- 6.Day CS, Lage DE, Ahn CS. Diversity based on race, ethnicity, and sex between academic orthopaedic surgery and other specialties. J Bone Joint Surg Am. 2010;92:2328-2335. [DOI] [PubMed] [Google Scholar]
- 7.Donaldson K, Callahan KE, Gelinne A, et al. Gender diversity in United States neurosurgery training programs. J Neurosurg. 2021;135:943-948. [DOI] [PubMed] [Google Scholar]
- 8.Gerull KM, Parameswaran P, Jeffe DB, Salles A, Cipriano CA. Does medical students’ sense of belonging affect their interest in orthopaedic surgery careers? A qualitative investigation. Clin Orthop Relat Res. 2021;479:2239-2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hamilton AR, Tyson MD, Braga JA, Lerner LB. Childbearing and pregnancy characteristics of female orthopaedic surgeons. J Bone Joint Surg Am. 2012;94:e77. [DOI] [PubMed] [Google Scholar]
- 10.Higgins MJ, Kale NN, Brown SM, Mulcahey MK. Taking family call: understanding how orthopaedic surgeons manage home, family, and life responsibilities. J Am Acad Orthop Surg. 2021;29:e31-e40. [DOI] [PubMed] [Google Scholar]
- 11.Hill JF, Yule A, Zurakowski D, Day CS. Residents’ perceptions of sex diversity in orthopaedic surgery. J Bone Joint Surg Am. 2013;95:e1441-e1446. [DOI] [PubMed] [Google Scholar]
- 12.Hu Y-Y, Ellis RJ, Hewitt DB, et al. Discrimination, abuse, harassment, and burnout in surgical residency training. N Engl J Med. 2019;381:1741-1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jagsi R, Griffith KA, DeCastro RA, Ubel P. Sex, role models, and specialty choices among graduates of US medical schools in 2006-2008. J Am Coll Surg. 2014;218:345-352. [DOI] [PubMed] [Google Scholar]
- 14.Johnson HM, Irish W, Strassle PD, et al. Associations between career satisfaction, personal life factors, and work-life integration practices among US surgeons by gender. JAMA Surg. 2020;155:742-750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keene RR, Hillard-Sembell DC, Robinson BS, Novicoff WM, Saleh KJ. Occupational hazards to the pregnant orthopaedic surgeon. J Bone Joint Surg Am. 2011;93:e1411-e1415. [DOI] [PubMed] [Google Scholar]
- 16.Lattanza LL, Meszaros-Dearolf L, O’Connor MI, et al. The Perry Initiative’s medical student outreach program recruits women into orthopaedic residency. Clin Orthop Relat Res. 2016;474:1962-1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ling M, Young CJ, Shepherd HL, Mak C, Saw RPM. Workplace bullying in surgery. World J Surg. 2016;40:2560-2566. [DOI] [PubMed] [Google Scholar]
- 18.Myers SP, Hill KA, Nicholson KJ, et al. A qualitative study of gender differences in the experiences of general surgery trainees. J Surg Res. 2018;228:127-134. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen L, Amin NH, Vail TP, Pietrobon R, Shah A. Editorial: a paucity of women among residents, faculty, and chairpersons in orthopaedic surgery. Clin Orthop Relat Res. 2010;468:1746-1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’Connor MI. Medical school experiences shape women students’ interest in orthopaedic surgery. Clin Orthop Relat Res. 2016;474:1967-1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rabinowitz LG. Recognizing blind spots - a remedy for gender bias in medicine? N Engl J Med. 2018;378:2253-2255. [DOI] [PubMed] [Google Scholar]
- 22.Rohde RS, Wolf JM, Adams JE. Where are the women in orthopaedic surgery? Clin Orthop Relat Res. 2016;474:1950-1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Samora JB, Denning J, Haralabatos S, Luong M, Poon S. Do women experience microaggressions in orthopaedic surgery? Current state and future directions from a survey of women orthopaedists. Curr Orthop Pract. 2020;31:503-507. [Google Scholar]
- 24.Samora JB, Van Heest A, Weber K, Ross W, Huff T, Carter C. Harassment, discrimination, and bullying in orthopaedics: a work environment and culture survey. J Am Acad Orthop Surg. 2020;28:e1097-e1104. [DOI] [PubMed] [Google Scholar]
- 25.Segal D. Factors motivating medical students in selecting a career specialty: relevance for a robust orthopaedic pipeline. J Am Acad Orthop Surg. 2018;26:e48-e49. [DOI] [PubMed] [Google Scholar]
- 26.Sobel AD, Cox RM, Ashinsky B, Eberson CP, Mulcahey MK. Analysis of factors related to the sex diversity of orthopaedic residency programs in the United States. J Bone Joint Surg Am. 2018;100:e79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Templeton K, Bernstein CA, Sukhera J, et al. Gender-based differences in burnout: issues faced by women physicians. Available at: https://nam.edu/gender-based-differences-in-burnout-issues-faced-by-women-physicians/?gclid=EAIaIQobChMIl_3–L-m-gIVqGxvBB2BGQ5SEAAYASAAEgLW2vD_BwE. Accessed September 21, 2022.
- 28.Van Heest AE, Fishman F, Agel J. A. 5-year update on the uneven distribution of women in orthopaedic surgery residency training programs in the United States. J Bone Joint Surg Am. 2016;98:e64. [DOI] [PubMed] [Google Scholar]
- 29.Whicker E, Williams C, Kirchner G, Khalsa A, Mulcahey MK. What proportion of women orthopaedic surgeons report having been sexually harassed during residency training? A survey study. Clin Orthop Relat Res. 2020;478:2598-2606. [DOI] [PMC free article] [PubMed] [Google Scholar]