EUS-guided gallbladder drainage (EUS-GBD) is currently a rescue procedure for malignant distal biliary obstruction after failed endoscopic retrograde cholangiopancreatography (ERCP) or other EUS-guided techniques in patients with a patent cystic duct 1 . However, the efficacy varies from 78 % to 90 % 2 3 . Therefore, for a group of patients this approach might be insufficient.
An 86-year-old man presented with jaundice secondary to malignant distal biliary obstruction caused by pancreatic adenocarcinoma ( Fig. 1 ). ERCP and EUS-assisted rendezvous (extra- and intrahepatic) attempts failed. After identifying a markedly distended gallbladder, a rescue EUS-GBD was performed from the gastric antrum with a 15 × 10-mm cautery-enhanced lumen-apposing metal stent (LAMS) ( Fig. 2 ).
Fig. 1.
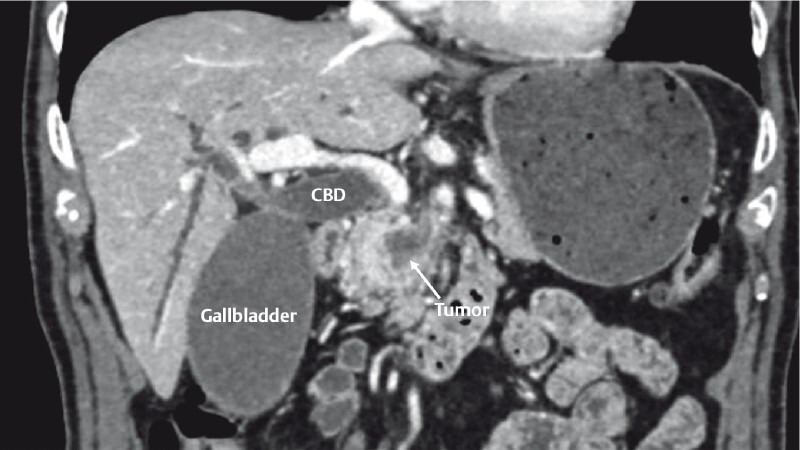
Abdominal computed tomography scan showing pancreatic head tumor with retrograde dilatation of the intra- and extrahepatic bile duct with a distended gallbladder. CBD: common bile duct.
Fig. 2.
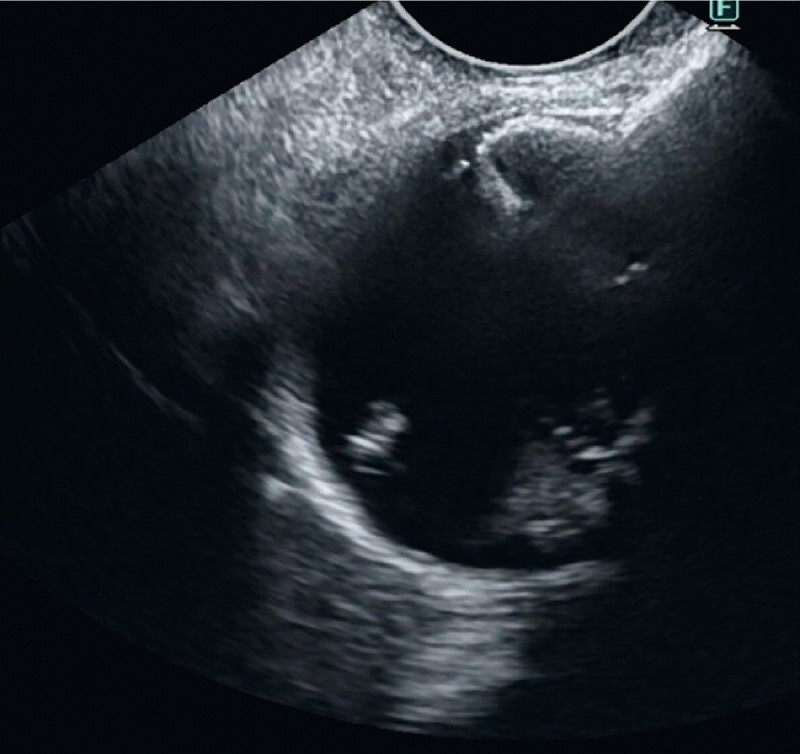
Ultrasound view of the distal flange of lumen-apposing metal stent after deployment in the gallbladder.
The patient developed cholangitis and clinical deterioration. A computed tomography (CT) scan ruled out transmural drainage-related complications and showed a decrease of intra- and extrahepatic bile duct dilation. Complete biliary drainage via a transcystic rendezvous ERCP through the gallbladder was then scheduled ( Video 1 ). Using a gastroscope, a direct through-the-LAMS cholecystoscopy was performed. The gallbladder neck was occluded with a 10-mm balloon dilatation. Contrast was injected for visualization and distension of the cystic duct and bile duct, which facilitated passage of a catheter and 0.025-inch guidewire through the cystic duct and neoplastic stricture into the duodenum ( Fig. 3 ). The gastroscope was removed under endoscopic and fluoroscopic view. A duodenoscope was introduced identifying the guidewire through the papilla, which was used to access the bile duct with the parallel cannulation technique ( Fig. 4 ). Finally, sphincterotomy and insertion of a 10 × 60-mm covered self-expandable metal stent were performed ( Fig. 5 ). Cholestasis improved significantly, although unfortunately he died suddenly 10 days after the procedure due to decompensation of heart disease.
Fig. 3.
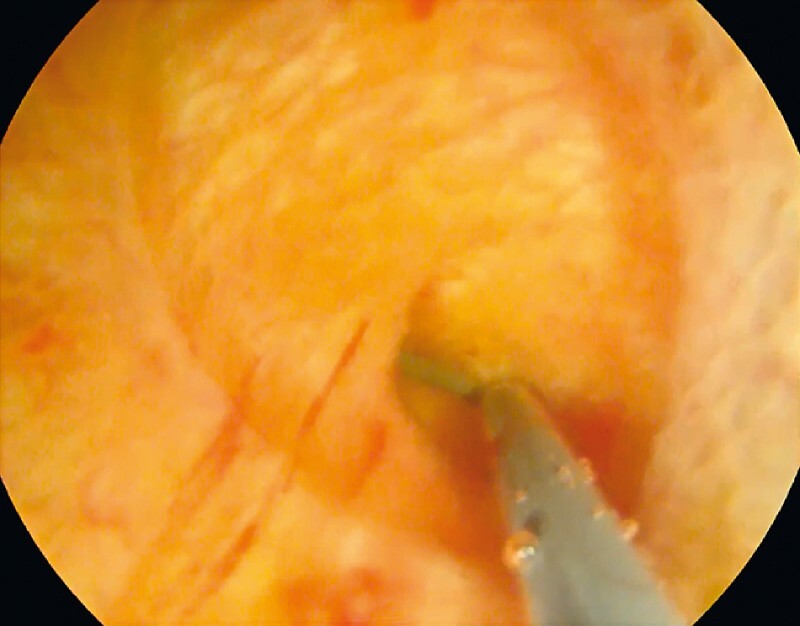
Endoscopic view of the cholecystoscopy from the gallbladder neck. Notice the cannulation of the cystic duct using a catheter and a 0.025” guidewire.
Fig. 4.

Endoscopic view of rendezvous endoscopic retrograde cholangiopancreatography (ERCP) with the “parallel cannulation technique” in which the sphincterotome is inserted to the bile duct through the papilla alongside the antegradedly placed guidewire.
Fig. 5.
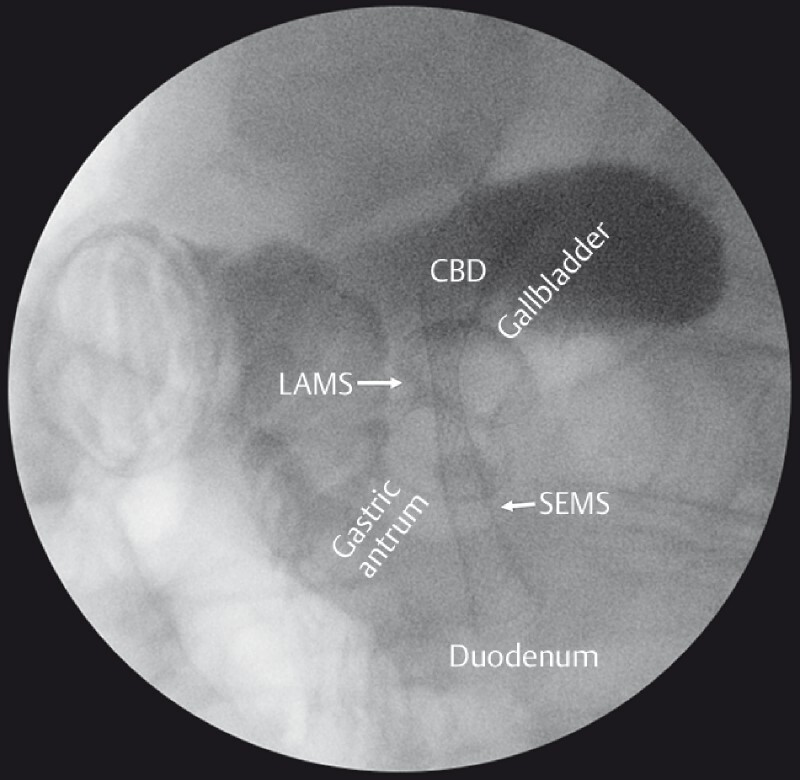
Fluoroscopic view of combined biliary drainage with cautery-enhanced lumen-apposing metal stent (LAMS) cholecystogastrostomy and self-expandable metal stent (SEMS) placement within the common bile duct (CBD).
Video 1 Fluoroscopic view of transcystic rendezvous. Cholecystoscopy through the lumen-apposing metal stent. A guidewire was advanced through the cystic duct and neoplastic distal biliary stricture through the ampulla to facilitate conventional endoscopic retrograde cholangiopancreatography.
Rendezvous ERCP via EUS-GBD has been used for other indications 4 5 . This approach could allow complete biliary drainage after rescue EUS-GBD in selected patients with distal malignant biliary obstruction when other options fail.
Endoscopy_UCTN_Code_CPL_1AL_2AD
Footnotes
Competing interests The authors declare that they have no conflict of interest.
Endoscopy E-Videos : https://eref.thieme.de/e-videos .
Endoscopy E-Videos is an open access online section, reporting on interesting cases and new techniques in gastroenterological endoscopy. All papers include a high quality video and all contributions are freely accessible online. Processing charges apply (currently EUR 375), discounts and wavers acc. to HINARI are available. This section has its own submission website at https://mc.manuscriptcentral.com/e-videos
References
- 1.van der Merwe S W, van Wanrooij R LJ, Bronswijk M et al. Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022;54:185–205. doi: 10.1055/a-1717-1391. [DOI] [PubMed] [Google Scholar]
- 2.Imai H, Kitano M, Omoto S et al. EUS-guided gallbladder drainage for rescue treatment of malignant distal biliary obstruction after unsuccessful ERCP. Gastrointest Endosc. 2016;84:147–151. doi: 10.1016/j.gie.2015.12.024. [DOI] [PubMed] [Google Scholar]
- 3.Chang J I, Dong E, Kwok K K. Endoscopic ultrasound-guided transmural gallbladder drainage in malignant obstruction using a novel lumen-apposing stent: a case series (with video) Endosc Int Open. 2019;7:E655–E661. doi: 10.1055/a-0826-4309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Law R, Baron T H. Endoscopic ultrasound-guided gallbladder drainage to facilitate biliary rendezvous for the management of cholangitis due to choledocholithiasis. Endoscopy. 2017;49:E309–E310. doi: 10.1055/s-0043-119351. [DOI] [PubMed] [Google Scholar]
- 5.Sanchez-Ocana R, de Benito Sanz M, Nájera-Muñoz R et al. Rendezvous ERCP via endoscopic ultrasound-guided gallbladder drainage to salvage a dislodged lumen-apposing metal stent during choledochoduodenostomy. Endoscopy. 2022;54:E65–E67. doi: 10.1055/a-1368-3985. [DOI] [PubMed] [Google Scholar]


