Abstract
Background/purpose
Splinting mobile teeth is a choice to improve the patient's oral comfort. The purpose of this study was to assess the survival and stability of mobile anterior mandibular teeth after splinting in patients with periodontitis undergoing supportive periodontal therapy (SPT).
Materials and methods
Patients with splinted mobile anterior mandibular teeth were assessed retrospectively. Periodontal statuses were recorded at baseline and follow-up visits. Tooth and splint survival as well as splint repairs were recorded. Multilevel Cox regression analyses were performed to evaluate patient- and tooth-related factors that might have influenced the survival rates of splints.
Results
Sixty-one patients, collectively having 161 splints, were followed for an average of 5.44 years. On average, probing depth (PD) of splinted teeth decreased from 4.31 mm to 2.93 mm and clinical attachment loss (CAL) decreased from 5.02 mm to 4.58 mm. Alveolar bone was stable in the follow-up period. None of the splinted teeth were extracted, The overall survival rate of the splints was 65.2%. Splints made of composite resin alone were associated with a higher risk of breakage when compared to splints composed of composite resin with mesh grid strips.
Conclusion
Splinting showed long-term survival and splinting combined with periodontal supportive treatment is a feasible option to maintain mobile mandibular anterior teeth.
Keywords: Splint, Long-term effect, Periodontitis, Periodontal therapy
Introduction
Periodontal disease is a chronic inflammatory disease characterized by gingival inflammation as well as connective tissue and alveolar bone destruction (1). As periodontal disease progresses, tooth mobility tends to increase due to deterioration in these support structures. In periodontal patients with severe horizontal bone loss, after periodontal debridement and occlusion adjustment treatment, periodontal inflammation can be effectively controlled, but continuing tooth mobility can still affect functions including speaking and chewing as well as aesthetics. Splinting mobile teeth is a choice that allows re-distribution of forces from mobile teeth to their immobile neighbor teeth in order to improve the patient's oral comfort and reduce occlusal forces (2,3). The 2017 World Workshop on the Classification of Periodontal Diseases confirmed that teeth with progressive mobility may require splint treatment (4). Besides prolonging the life expectancy of the mobile teeth, splinting also may postpone tooth extraction and subsequent complex and costly prosthodontic treatments.
Currently, there are a variety of splinting methods and materials used for short-term and medium-term temporary splinting in a clinical setting: unidirectional pre-impregnated glass fibers, open weave glass fibers, and fiber-reinforced composite splints are the most commonly-used options (5, 6, 7, 8). Though there have been some long-term studies of splinted teeth in periodontitis patients (9,10), the survival rate results have been inconsistent or even contrary (11, 12, 13) so the prognosis for splinted mobile teeth has remained unclear. The aim of this study is to evaluate the periodontal status of splinted mandibular anterior teeth treated with different splint materials and to compare their stability during a long term regular maintenance therapy period. Further, factors that might influence the survival rates of splints were also tested and analyzed to provide more evidence for clinical applications.
Materials and methods
Study design
This study was designed and performed as a retrospective study of patients with a history of periodontitis. It was approved by the Institutional Review Board of Peking University School and Hospital of Stomatology (approval number PKUSSIRB-202163053).
Patients
All participants were recruited at the department of periodontology, first clinical division, Peking University School and Hospital of Stomatology. All participants were medically healthy and were diagnosed with stage III or IV periodontitis according to the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. The inclusion criteria were: 1) 30–65 years of age before treatment at baseline; 2) no history of systemic diseases; 3) no cross-bites in the anterior teeth and no known oral parafunctions. 4) All participants were Eichner classification A1-B1 and had at least three occlusal support areas (14); 5) existence of at least one tooth with a mobility of degree II or III according to the Lindle and Nyman classification (Degree I: mobility in labio-oral direction of 0.2–1 mm; Degree II: mobility of 1–2 mm; Degree III: mobility more than 2 mm) combined with a CAL ≥5 mm at at least one site of the mobile tooth and a bone loss ≥50% at baseline (15); 6) completed active periodontal treatment (APT) and had supportive periodontal treatment (SPT) for ≥5 years with 2–3 visits per year and radiographic records at both the time of splint treatment and follow up. In total, 61 patients were enrolled in the study.
Active and supportive periodontal treatments (APT and SPT)
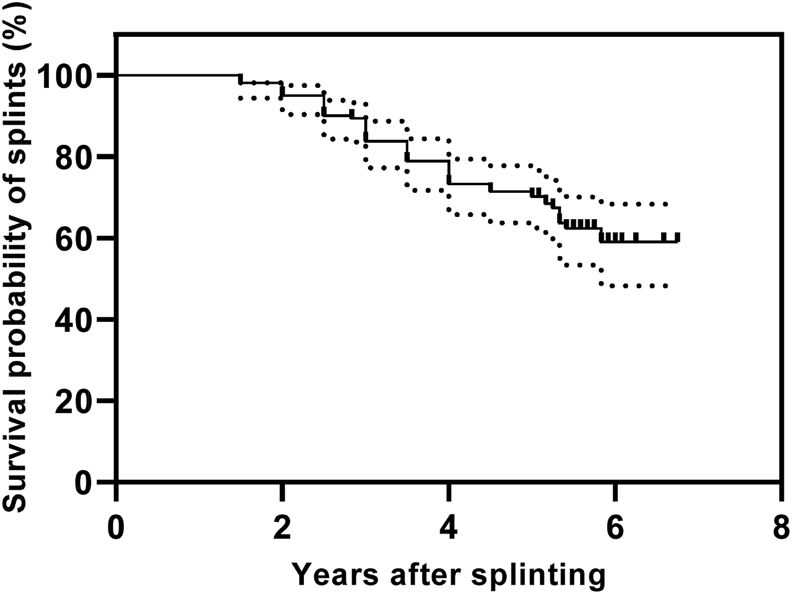
At baseline and follow-up visits, patients received a periodontal examination. All splinted teeth were measured with a 10-mm manual periodontal probe (PCP10-SE, Hu-Friedy, Chicago, USA) and results were rounded up to the nearest millimeter. Plaque index (PI), bleeding on probing (BOP), probing depth (PD), and clinical attachment level (CAL) were measured at 6 sites per tooth. During the measurement of PD, a periodontal probe was inserted to the base of the sulcus or pocket with a force of 20–25 g. BOP was present if the probed site bled about 20 s after probing. Relative bone loss (RBL) was assessed using peri-apical radiographic images at baseline and follow-up visits by one examiner. The ratio of alveolar bone height to root length was used to assess the RBL (RBL = alveolar bone height [distance between the cement-enamel junction to the most apical extension of the alveolar crest]/root length [distance between the cement-enamel junction to the radiographic apex of the root]) (Fig. 1). All measurements were performed by the same examiner (Y.Z.). We calculated the RBL at the mesial and distal surfaces of splinted teeth and used the mean value of the mesial and distal results.
Figure 1.
Measurement of relative bone loss (RBL). RBL = alveolar bone height (distance between the CEJ [cement-enamel junction] to the alveolar crest)/root length (distance between the CEJ to the root apex).
APT includes oral hygiene instruction and motivation (Bass tooth brushing method, application of dental floss, and interdental brushes), supragingival cleaning with ultrasonic instruments and polishing teeth with rotating rubber cups using polishing paste, and subgingival cleaning and root planing (SRP) with ultrasonic and hand instruments, under local anesthesia if needed. After completion of APT, patients received supportive periodontal therapy (SPT) 2–3 times per year. SPT included oral hygiene assessments (PI and BOP) and periodontal status assessments (PD and CAL), re-instruction and motivation to optimize individual oral plaque control, supragingival cleaning and polishing all teeth and subgingival scaling and root planing (SRP) at the sites with PD ≥ 5 mm and bleeding on probing.
Splinted teeth
Teeth were splinted in case of mobility and bone loss determined by a dentist in accordance with patients’ preferences (the mobility of teeth was degree II or III combined with a bone loss ≥50% or the mobility of teeth was degree I combined with a bone loss ≥67%).
In both groups, the splinted teeth on the labial and lingual surfaces were cleaned and polished with rubber wheels, the splints were made of composite splint materials: 27 patients were splinted using composite resin with mesh grid strips (BiosplintTM Reinforcement Ribbon, Acteon, Merignac, France and Filtek Supreme XT Flowable Restorative, 3 M ESPE, MN, USA) and 34 patients were splinted using composite resin only (4-methacryloloxyethyl trimellitate anhydride/methyl methacrylate/tri-n-butyl borane (4-META/MMA/TBB), Sun Medical Co Ltd., Shiga, Japan) according to the adhesion protocols provided by the manufacturers. For the patients were splinted using composite resin with mesh grid strips, the teeth were etched with 35% phospshoric acid (Gluma Etch 35 Gel, Heraeus Kulzer GmbH, Hanau, Germany) for 60s, self-etching adhesive (Clearfil SE-Bond, Kuraray Medical Inc, Okayama, Japan) was applied gently air-dried and photo-polymerized for 30 s (Mini LED Satelec, Satelec Acteon Group, Merignac, France; light intensity: 1200 mW/cm2). A thin layer of composite resin (3 M ESPE) was applied on the enamel surfaces and left unpolymerized. Then, mesh grid strip (Acteon) was placed in the bed of the composite resin and gently pressed towards the composite resin (3 M ESPE) on splinted teeth. Each segment of splint was photo-polymerized for 30 s (Satelec Acteon Group) and during polymerization, the rest of the splint was shielded with composite resin (3 M ESPE). Second layer of composite resin was applied on splint and each segment was photo-polymerized (Satelec Acteon Group) for 45 s, finishing and polishing. For the patients were splinted using composite resin only, the teeth were etched with 35% phospshoric acid for 60 s (Sun Medical Co Ltd.), the catalyst (TBB, Sun Medical Co Ltd.) was added to the monomer liquid (4-META and MMA, Sun Medical Co Ltd.) to prepare an activated monomer liquid, the polymer powder and activated monomer liquid were mixed to apply the splinting, finishing and polishing. In our study, splints were made to both sides of adjacent tooth and there were no splinting extensions. We did adjustments of occlusion in case of premature contact, adjustments of interdental brushes and other cleaning instructions. After splinting, the mobilities of the splinted teeth were reduced to better than degree I and all splints remained stable during the follow up period. Any loss of teeth and instances of splint breakage (fracture or de-bonding) were recorded. Fracture or de-bonding of the splint was defined as endpoint for splint survival. Patient satisfaction with splinting was evaluated using a visual analogue scale (VAS) method before splinting at baseline and at follow up visits.
Statistical analysis
The SPSS statistical program (Version 21.0; SPSS Inc., Chicago, IL, USA) was used to analyze the data. Mean with standard deviation was used to describe the variables of the background characteristics. Independent t-tests were used to evaluate the differences between the two groups. Survival rates of splinted teeth and stability of splints were calculated applying a Kaplan–Meier test with 95% confidence interval (CI). Cox regression was used to determine the association between the stability of splints and predictors (gender, baseline BOP, PI, PD, RBL, CAL, mobility degree, type of splint material). Statistical significance was defined as P < 0.05.
Results
A total of 61 participants (25 male and 36 female) were enrolled in the study. Their mean age was 54.1 years old. At baseline, all 61 patients were diagnosed as having stage III or IV periodontitis. A total of 37 posterior regions (across 26 patients) had received surgical therapy, 23 posterior regions (across 19 patients) underwent modified Widman flap surgery, and 14 posterior regions (across 11 patients) underwent guided tissue regeneration (GTR) with bone graft surgery. None of the anterior regions studied underwent surgical therapy. In 5 individuals, splints were inserted after supragingival cleaning and the rest were inserted after APT. The mean number of splinted teeth per patient as 2.6 teeth per patient. In 8 patients, 1 tooth was splinted; in 16 patients, 2 teeth were splinted; in 27 patients, 3 teeth were splinted; in 10 patients, 4 teeth were splinted. The total number of splinted teeth was 161. Composite resin with mesh grid strips was the splinting material used in 67 teeth (across 27 patients), while 94 teeth (across 34 patients) were splinted using only composite resin. At baseline, 43 patients had at least one tooth with a mobility degree of II and 15 patients had at least one tooth with a mobility degree of III. The demographic and clinical characteristics of all participants are presented in Table 1.
Table 1.
Characteristics of study participants.
| Characteristics of the participants | |
|---|---|
| Number of patients (male/female) | 61 (25/36) |
| Mean age ± SD (median; range) | 54.05 ± 5.77 (56; 34–66) |
| Observation time in years (mean ± SD) | 5.44 ± 0.42 |
| Smoking status | 13 smokers (all ≥10 cigarettes/day), 6 former smokers, 42 non-smokers |
| Number of splints | 161 |
| Eichner classification of patients: | A1: 13, A2: 16, A3: 24, B1: 8 |
| Mobility of splinted teeth (degree I/II/III) | 22/105/34 |
| Number of patients with 1/2/3/4 splints | 8/16/27/10 |
| Location of splints (42/41/31/32) | 35/53/47/26 |
| Splinting material: Composite resin with mesh grid strips | 27 patients, 67 teeth |
| Splinting material: Composite resin only | 34 patients, 94 teeth |
| SD, standard deviation | |
The oral hygiene of all patients remained as good as before splinting after an average of 5.44 years of supportive periodontal treatment. (Fig. 2). At baseline, before splint treatments, the mean PI and BOP were 2.7 and 85% respectively. After splinting and more than 5 years of SPT, the PI and BOP were 0.9 and 13%. These values were significantly lower compared to the PI and BOP levels recorded at baseline (Table 2).
Figure 2.
Clinical photography and radiography of patients splinted using composite resin with mesh grid strips (case 1, 2, 3 and 4) and composite resin only (case 5 and 6). In the case 1, after splinting and maintenance care, alveolar bone density in the proximal area of 31 and 41 were increased and crestal lamina dura in the proximal area of 31 and 41 appeared (yellow arrows), in the case 2, the alveolar bone density in the mesial part of 31 was also increased (yellow arrow).
Table 2.
Periodontal condition of splinted teeth at baseline and follow-up visit.
| Baseline | Follow-up | |
|---|---|---|
| Plaque index (PI) | 2.68 ± 0.47 | 0.93 ± 0.49a |
| Bleeding on probing (BOP, %) | 85 ± 14 | 13 ± 7a |
| Probing depth (PD, mm) | 4.31 ± 0.36 | 2.93 ± 0.38a |
| Clinical attachment level (CAL, mm) | 5.02 ± 1.03 | 4.58 ± 0.67a |
| Relative bone loss (RBL, %) | 33.89 ± 7.53 | 33.38 ± 7.41 |
| Visual analogue scale (VAS) score | 3.27 ± 2.53 | 7.92 ± 3.26a |
Significant difference compared to baseline (∗P < 0.05).
At baseline, the mean PD and CAL of the splinted teeth were 4.31 mm and 5.02 mm respectively. After APT and SPT, mean PD and CAL measurements decreased to 2.93 mm and 4.58 mm. Both PD and CAL were significantly lower at follow-up compared to the PD and CAL measured at baseline. Regarding alveolar bone height level, the mean RBL at the splinted teeth was 33.9% at baseline, and alveolar bone height levels remained stable in the follow-up period. There were no significant differences in mean RBL between the baseline and follow up visits (Table 2).
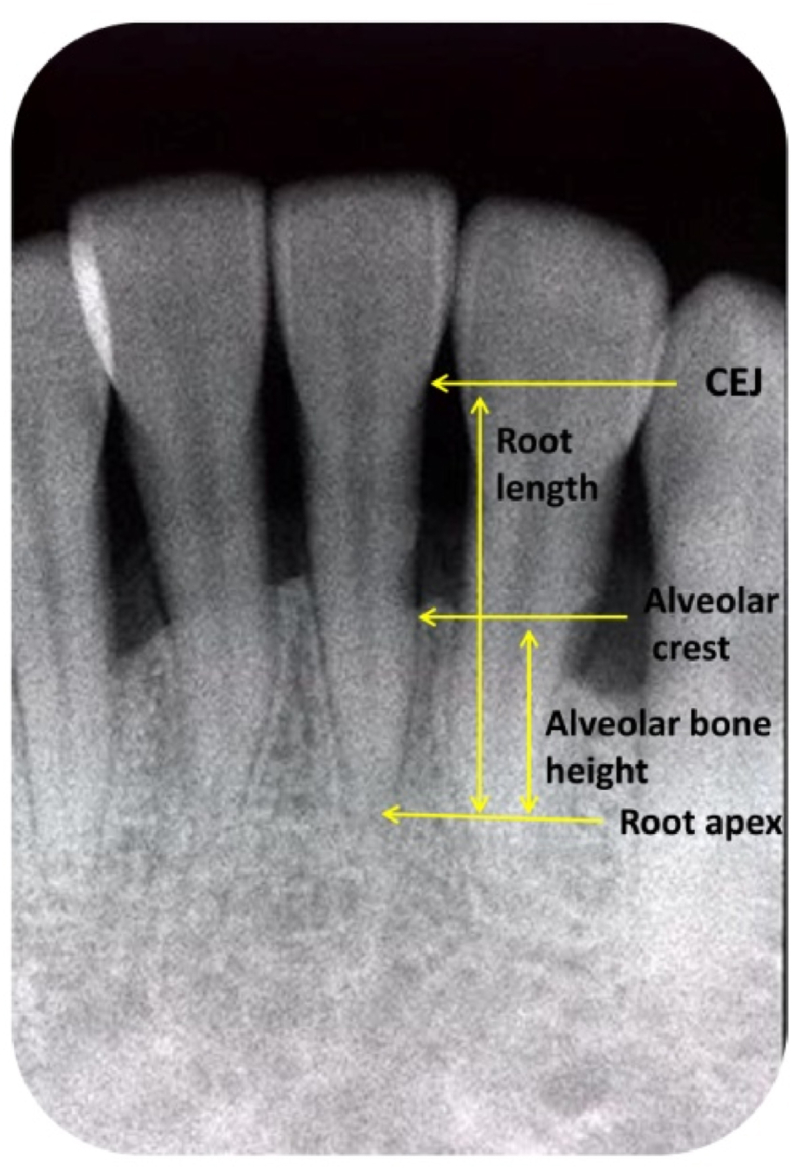
During SPT after splinting, 3 splinted teeth received endodontic treatment because of pulp necrosis or periapical periodontitis. None of the splinted teeth were extracted after more than 5 years. Within the study sample, one year after splinting, survival rate of splints was 100%; three years after splinting, 26 splints showed breakages (22 splints showed de-bonding, 3 splints showed fracture and 1 splint showed both de-bonding and fracture) and survival rate of splints was 83.9%; five years after splinting, 48 splints showed breakages (37 splints showed de-bonding, 7 splints showed fracture and 4 splints showed both de-bonding and fracture) and survival rate of splints was 70.2%; during follow-up period, 56 splints showed breakages (40 splints showed de-bonding, 9 splints showed fracture, and 7 splints showed both de-bonding and fracture), the overall survival rate of the studied splints was 65.2%. A Kaplan–Meier estimation of the survival rate of splints until broken (fracture or de-bonding) is shown in Fig. 3. 34.8% of the splinted teeth (56/161) required a repair during the follow-up period with a mean of 0.9 per patient. The mean annual number of repairs per patient was 0.2. The mean of patient-reported satisfaction VAS scores at baseline was 3.3. After splinting and more than 5 years of SPT, patients reported feeling more satisfied with the application of splints as evidenced by a significantly higher mean VAS score of 7.9 at the follow-up visit (Table 2).
Figure 3.
Kaplan–Meier estimator with 95% CI (confidence interval) of splints until fracture or de-bonding (splinting stability).
After Cox regression analysis, gender, baseline PI, BOP, PD, CAL, baseline mobility degree, and number of splinted teeth had no statistical influence on splint fracture or de-bonding probability (Table 3). Splint material, however, showed significant correlation with the survival of splints. Splints made of composite resin alone were associated with a significantly higher risk of breakage compared to splints made of composite resin and mesh grid strips (Hazard Ratio (HR) = 2.07, 95% CI: 1.33–3.01, P < 0.05). Although the difference was not significant, there was a visible correlation between splint location and splint survival. Splints located at the middle incisor area (31 and 41) showed a tendency towards higher risk of breakage compared to splints located at the lateral incisor area (32 and 42, HR = 1.26, 95% CI:0.96–1.48, P = 0.06). In contrast to the splint location, the RBL of splinted teeth seemed to be associated with a lower risk of splint breakage (HR = 0.93, 95% CI: 0.86–1.01, P = 0.06).
Table 3.
Estimates of the association between covariates and splint stability.
| aVariables | HR | 95% CI | P |
|---|---|---|---|
| Age (continuous) | 0.980 | 0.894–1.074 | 0.660 |
| Gender (reference: female) | 1.078 | 0.496–1.719 | 0.515 |
| Plaque index (PI) | 1.091 | 0.497–2.387 | 0.318 |
| Bleeding on probing (BOP) | 1.024 | 0.982–1.069 | 0.263 |
| Probing depth (PD) | 1.339 | 0.225–1.919 | 0.719 |
| Clinical attachment loss (CAL) | 1.028 | 0.543–1.946 | 0.632 |
| Relative Bone Loss (RBL) | 0.929 | 0.858–1.006 | 0.063 |
| Eichner classification A1 (reference) | 1 | ||
| Eichner classification A2 | 1.045 | 0.763–1.381 | 0.243 |
| Eichner classification A3 | 1.087 | 0.875–1.306 | 0.340 |
| Eichner classification B1 | 1.080 | 0.875–1.275 | 0.157 |
| One splinted tooth (reference) | 1 | ||
| Two splinted teeth | 1.149 | 0.568–1.689 | 0.179 |
| Three splinted teeth | 1.083 | 0.312–1.843 | 0.248 |
| Four splinted teeth | 1.180 | 0.271–1.978 | 0.358 |
| Splinting at lateral incisor area (reference) | 1 | ||
| Splinting at middle incisor area | 1.264 | 0.961–1.484 | 0.056 |
| Mobility degree Ⅰ (reference) | 1 | ||
| Mobility degree Ⅱ | 0.973 | 0.438–2.259 | 0.291 |
| Mobility degree Ⅲ | 1.046 | 0.276–2.852 | 0.409 |
| Composite resin with mesh grid strip splints (reference) | 1 | ||
| Composite resin only splints | 2.067 | 1.326–3.011 | 0.006∗∗ |
Cox regression analysis. HR, Hazard Ratio. CI, confidence interval. ∗∗P < 0.01.
Discussion
Tooth mobility is a common consequence of periodontitis, however bone loss and attachment loss can be reduced by eliminating trauma (2). Provided all relevant factors are considered, splinting helps to redistribute occlusal forces over a larger area and acts as an adjunct to periodontal treatment and maintenance. Periodontally compromised teeth with poor prognosis can also be retained for a longer period of time by using splints, (16,17) therefore splinting the mobile tooth is recommended (18).
Advanced tooth mobility is often observed in patients with periodontitis due to attachment loss and alveolar bone loss. As a therapeutic opinion, tooth splinting has been used widely, especially in the mandibular anterior tooth area (19). While splinting treatment redirects forces from mobile teeth to their immobile neighbors and reduces occlusal force, it can also affect oral hygiene measures in the interproximal area (3). Despite this, splinting has been studied for a long time. Some studies have reported that splinting treatment only stabilized mobile teeth and did not improve the periodontal situation, mobility may return once the splints have be removed, several studies focused on the long-term survival rate of splints have reported inconsistent or even contrary results and reported limited data on possible factors that might influence the survival rate of splints (12,20). In our study, we splinted 1/3 of the coronal portion of the mobile tooth, leaving enough space for oral hygiene measures and professional treatment. Our results show that, after splinting and SPT for an average of 5.4 years, PI (0.93) and BOP (13%) were observed to be at low levels and were significantly lower compared to those at baseline (PI 2.68 and BOP 85%). Splints only slightly affected patients' oral hygiene measures and were confirmed not to be a high risk factor of plaque accumulation, in accordance with other studies (13,21,22). At baseline, the PD and CAL of splinted teeth were 4.31 mm and 5.02 mm respectively. After splinting and SPT (along with good oral hygiene measures and decreased tooth mobility), the PD and CAL decreased to 2.93 mm and 4.58 mm. The observed decrease of 1.38 mm in mean PD and 0.44 mm in mean CAL were similar to results reported in Sonnenschein's study (23,24). Previous studies have reported that splinting can resulted in alveolar bone regeneration in the adjacent area (25). However, our results differed, most of the splinted teeth showed stable bone levels after SPT, alveolar bone density in the proximal area of some splinted teeth were increased, several splinted teeth showed continuing bone loss, and none of the splinted teeth showed significant bone gain. The RBL was not significantly different at the follow-up visit compared to the baseline level. The reason may be that our observation period was longer than in previous studies and our bone levels observed at baseline were lower (34%). These factors may have contributed to the our final results.
Baseline alveolar bone level was demonstrated to significantly contribute to tooth loss during long term SPT in patients with chronic periodontitis (26,27) although the RBL of splinted teeth at baseline was considerable lower, after an average of 5.4 years' observation after splinting, no splinted teeth were extracted and Kumbuloglu's investigation of tooth loss rate yielded similar results for the splinted teeth after a 4.5 year period (13). All of these results confirmed that the splinted teeth exhibited long-term survival and that splinting of periodontally-compromised anterior mandibular teeth combined with APT is a valid and valuable procedure to maintain these teeth. Patient satisfaction VAS scores at the follow up visit (7.9 on average) were significantly higher compared to the VAS scores taken at baseline (3.3 on average). This suggests that splints have a truly positive impact on periodontitis patients' oral quality of life.
During the follow-up period, the survival rate of splints was 83.9% after 3 years and 70.2% after 5 years, totally 47 splints showed de-bonding and 16 splints showed fracture, these were repaired over the observational period and the overall survival rate was 65.2%, which was similar to the Sonnenschein's result that the survival rate of splints was 74.4% after 3 years and 67.3% after 10 years (23). 34.8% of the splinted teeth required a repair during follow-up with a mean of 0.9 per patient, all of the splints needing repair exhibited a severe bone loss of RBL less than 30%, indicating that high bone loss areas may still be less able to suffer regular chewing forces and lead to de-bonding or fracture. Our results showed that relative bone level seemed to be related to the success rate of the splint, although the difference was not significant (HR = 0.929, P = 0.063). For cost-effectiveness, we had only splinted the mobile teeth to neighbor teeth. Determining whether extending the splint to more teeth with higher bone levels might help to diminish the chance of splint breakage will require further study to confirm.
Graetz investigated the success rates of different splinting materials (composite, composite reinforced with wired metal or glass fiber) and showed that different splint materials were not associated with the number of repairs (26) however in our study, after Cox regression analysis, splints made of only composite resin were associated with higher risk of splint breakage (fracture or de-bonding, HR = 2.067, P = 0.006). These different results maybe be attributed to the location of splints and bone levels of the splinted teeth. In the Graetz's study, they included upper and lower anterior teeth as well as posterior teeth. Our study only included lower anterior teeth. The bone level of splinted teeth in Graetz's study (61%) was distinctly higher compared to the bone levels of splinted teeth in our study (34%). The patients in our study were also Eichner class A1-B1 and had at least three occlusal support areas that might influence the occlusal distribution (17,28). All of these factors resulted in inconsistent success rates of splints and our data indicate that splinting with composite resin combined with mesh grid strips can enlarge the splinted area and enhance the bond strength. However, this does require a longer clinical operation time.
Different tooth locations showed different occlusal loading and Graetz's results showed that splints in the lower anterior teeth needed fewer repairs compared to the upper anterior teeth and posterior teeth, (9,26) our results showed that the location of splints may influence success rates and that splints at middle incisor area seemed to be at higher risk of being broken compared to splints in the lateral incisor area, although the difference was not significant (HR = 1.264, P = 0.056).
However, there were some limitations to this study. Firstly, this was a retrospective study. There was no control group (for example one that did not receive splinting treatment with similar mobility of teeth and alveolar bone loss), and we only splinted the mandibular anterior teeth and excluded patients with cross-bites in the anterior teeth or oral parafunctions. Sonnenschein's study showed that patients without posterior and anterior antagonistic support of natural teeth may be more susceptible to splint fracture, (23) which indicates that functional loading may be an influencing factor in the survival of splints. Antagonistic loading should be considered before splint treatment. In this study, we took parallel projection periapical radiographs and measured the relative bone height variation; using stents or computer assisted densitometric image analysis (CADIA) might be a better choice to evaluate the change of alveolar bone. Lastly, although our results showed a considerable survival rate after more than five years, the splints we used in this study were still considered medium-term provisional splints that might need further treatment or repair due to their strength. All of these factors limit the applicable scope of this study.
In conclusion, we evaluated the periodontal condition of 61 patients for an average of 5.44 years after receiving splint treatment and supportive periodontal treatment. This was a considerable sample size and observation period. We analyzed possible factors that can influence the survival rate of splints. Our results indicate that splinting shows long-term survival and splinting combined with supportive periodontal treatment is a feasible option to maintain mobile mandibular anterior teeth in patients without a parafunction. Further studies are needed to determine if this would be true of this particular type of patients.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
The study was supported by National Natural Science Foundations of China (project number: 81800978).
Contributor Information
Yu Cai, Email: jessonjesson@hotmail.com.
Qingxian Luan, Email: kqluanqx@163.com.
References
- 1.Lang N.P., Bartold P.M. Periodontal health. J Clin Periodontol. 2018;45:S9–S16. doi: 10.1111/jcpe.12936. [DOI] [PubMed] [Google Scholar]
- 2.Fleszar T.J., Knowles J.W., Morrison E.C., Burgett F.G., Nissle R.R., Ramfjord S.P. Tooth mobility and periodontal therapy. J Clin Periodontol. 1980;7:495–505. doi: 10.1111/j.1600-051x.1980.tb02156.x. [DOI] [PubMed] [Google Scholar]
- 3.Kathariya R., Devanoorkar A., Golani R., Shetty N., Vallakatla V., Bhat M.Y. To splint or not to splint: the current status of periodontal splinting. J Int Acad Periodontol. 2016;18:45–56. [PubMed] [Google Scholar]
- 4.Jepsen S., Caton J.G., Albandar J.M., et al Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J Periodontol. 2018;89:S237–S248. doi: 10.1002/JPER.17-0733. [DOI] [PubMed] [Google Scholar]
- 5.Eminkahyagil N., Erkut S. An innovative approach to chairside provisional replacement of an extracted anterior tooth: use of fiber-reinforced ribbon-composites and a natural tooth. J Prosthodont. 2006;15:316–320. doi: 10.1111/j.1532-849X.2006.00125.x. [DOI] [PubMed] [Google Scholar]
- 6.Giordano R. Fiber reinforced composite resin systems. Gen Dent. 2000;48:244–249. [PubMed] [Google Scholar]
- 7.Mosedale R.F. Current indications and methods of periodontal splinting. Dent Update. 2007;34:168–176. doi: 10.12968/denu.2007.34.3.168. [DOI] [PubMed] [Google Scholar]
- 8.Vallittu P.K. Compositional and weave pattern analyses of glass fibers in dental polymer fiber composites. J Prosthodont. 1998;7:170–176. doi: 10.1111/j.1532-849x.1998.tb00200.x. [DOI] [PubMed] [Google Scholar]
- 9.Tokajuk G., Pawinska M., Stokowska W., Wilczko M., Kedra B.A. The clinical assessment of mobile teeth stabilization with fibre-kor. Adv Med Sci. 2006;51(1):225–226. [PubMed] [Google Scholar]
- 10.Cho Y.D., Kim S., Koo K.T., et al Rescue of a periodontally compromised tooth by non-surgical treatment: a case report. J Periodontal Implant Sci. 2016;46:128–134. doi: 10.5051/jpis.2016.46.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nabers C.L., Stalker W.H., Esparza D., Naylor B., Canales S. Tooth loss in 1535 treated periodontal patients. J Periodontol. 1988;59:297–300. doi: 10.1902/jop.1988.59.5.297. [DOI] [PubMed] [Google Scholar]
- 12.Sekhar L.C., Koganti V.P., Shankar B.R., Gopinath A. A comparative study of temporary splints: bonded polyethylene fiber reinforcement ribbon and stainless steel wire + composite resin splint in the treatment of chronic periodontitis. J Contemp Dent Pract. 2011;12:343–349. doi: 10.5005/jp-journals-10024-1057. [DOI] [PubMed] [Google Scholar]
- 13.Kumbuloglu O., Saracoglu A., Ozcan M. Pilot study of unidirectional e-glass fibre-reinforced composite resin splints: up to 4.5-year clinical follow-up. J Dent. 2011;39:871–877. doi: 10.1016/j.jdent.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 14.Ikebe K., Matsuda K., Murai S., et al Validation of the eichner index in relation to occlusal force and masticatory performance. Int J Prosthodont. 2010;23:521–524. [PubMed] [Google Scholar]
- 15.Lindhe J., Nyman S. The effect of plaque control and surgical pocket elimination on the establishment and maintenance of periodontal health. a longitudinal study of periodontal therapy in cases of advanced disease. J Clin Periodontol. 1975;2:67–79. doi: 10.1111/j.1600-051x.1975.tb01727.x. [DOI] [PubMed] [Google Scholar]
- 16.Bernal G., Carvajal J.C., CA M. A review of the clinical management of mobile teeth. J Contemp Dent Pract. 2002;3:10–22. [PubMed] [Google Scholar]
- 17.Graetz C., Ostermann F., Woeste S., Salzer S., Dorfer C.E., Schwendicke F. Long-term survival and maintenance efforts of splinted teeth in periodontitis patients. J Dent. 2019;80:49–54. doi: 10.1016/j.jdent.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 18.Rühling A. Treatment strategies in the case of advanced attachment loss: part 2: extraction of critical teeth and dental restorations on movable abutments. Periodontal Practice Today. 2004;2:213–225. [Google Scholar]
- 19.Quirynen M., Mongardini C., Lambrechts P., et al A long-term evaluation of composite-bonded natural/resin teeth as replacement of lower incisors with terminal periodontitis. J Periodontol. 1999;70:205–212. doi: 10.1902/jop.1999.70.2.205. [DOI] [PubMed] [Google Scholar]
- 20.Alkan A., Aykac Y., Bostanci H. Does temporary splinting before non-surgical therapy eliminate scaling and root planing-induced trauma to the mobile teeth? J Oral Sci. 2001;43:249–254. doi: 10.2334/josnusd.43.249. [DOI] [PubMed] [Google Scholar]
- 21.Agrawal A.A., Chitko S.S. The use of silane-coated industrial glass fibers in splinting periodontally mobile teeth. Indian J Dent Res. 2011;22:594–596. doi: 10.4103/0970-9290.90307. [DOI] [PubMed] [Google Scholar]
- 22.Forabosco A., Grandi T., Cotti B. The importance of splinting of teeth in the therapy of periodontitis. Minerva Stomatol. 2006;55:87–97. [PubMed] [Google Scholar]
- 23.Sonnenschein S.K., Betzler C., Rutters M.A., Krisam J., Saure D., Kim T.S. Long-term stability of splinted anterior mandibular teeth during supportive periodontal therapy. Acta Odontol Scand. 2017;75:475–482. doi: 10.1080/00016357.2017.1340668. [DOI] [PubMed] [Google Scholar]
- 24.Sonnenschein S.K., Ziegler P., Ciardo A., Ruetters M., Krisam J., Kim T.S. The impact of splinting mobile mandibular incisors on oral health-related quality of life-preliminary observations from a randomized clinical trial. J Clin Periodontol. 2021;48:816–825. doi: 10.1111/jcpe.13454. [DOI] [PubMed] [Google Scholar]
- 25.Machtei E.E., Hirsch I. Retention of hopeless teeth: the effect on the adjacent proximal bone following periodontal surgery. J Periodontol. 2007;78:2246–2252. doi: 10.1902/jop.2007.070125. [DOI] [PubMed] [Google Scholar]
- 26.Graetz C., Plaumann A., Schlattmann P., et al Long-term tooth retention in chronic periodontitis - results after 18 years of a conservative periodontal treatment regimen in a university setting. J Clin Periodontol. 2017;44:169–177. doi: 10.1111/jcpe.12680. [DOI] [PubMed] [Google Scholar]
- 27.Checchi L., Montevecchi M., Gatto M.R., Trombelli L. Retrospective study of tooth loss in 92 treated periodontal patients. J Clin Periodontol. 2002;29:651–656. doi: 10.1034/j.1600-051x.2002.290710.x. [DOI] [PubMed] [Google Scholar]
- 28.Graetz C., Schwalbach M., Seidel M., Geiken A., Schwendicke F. Oral health-related quality of life impacts are low 27 years after periodontal therapy. J Clin Periodontol. 2020;47:952–961. doi: 10.1111/jcpe.13324. [DOI] [PubMed] [Google Scholar]